Patient Assessment
1/49
Earn XP
Description and Tags
To ensure a comprehensive understanding of the patient assessment process, this flash card assignment breaks down every section and its core components. You'll translate key concepts into organized, accessible learning tools.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms

operations
Functional Equipment
Sufficient Inventory
Proper Documentation
Wellbeing of Self & Others

Functional Equipment
Is it whole?
Is it ready?

Sufficient Inventory
Do i have what i should?

Proper Documentation
Does this need to be time stamped
Am i writing legibly
Am i writing somewhere appropriate
Is my chart complete
Has it been reviewed
Is it objective? Honest? Thorough?

Wellbeing of Self & Others
Does my Partner need to be checked?
Do i need to be checked?
Is this decision healthy?
Should this be debriefed?
Scene Size-up & Safety
Evaluate Dispatch
Scene Safety
PPE
# of patients
Triage
Need for additional resources

Evaluate Dispatch
MOI or NOI?
Is there anything unique about the location?
Could I need special resources?
Are thre flags on the address?
does this make sense?
GUT CHECK!

Scene Safety
Physical hazards
weather hazards
Violence or crowds
Unstable structures
Live wires or fire
Exposed roadway
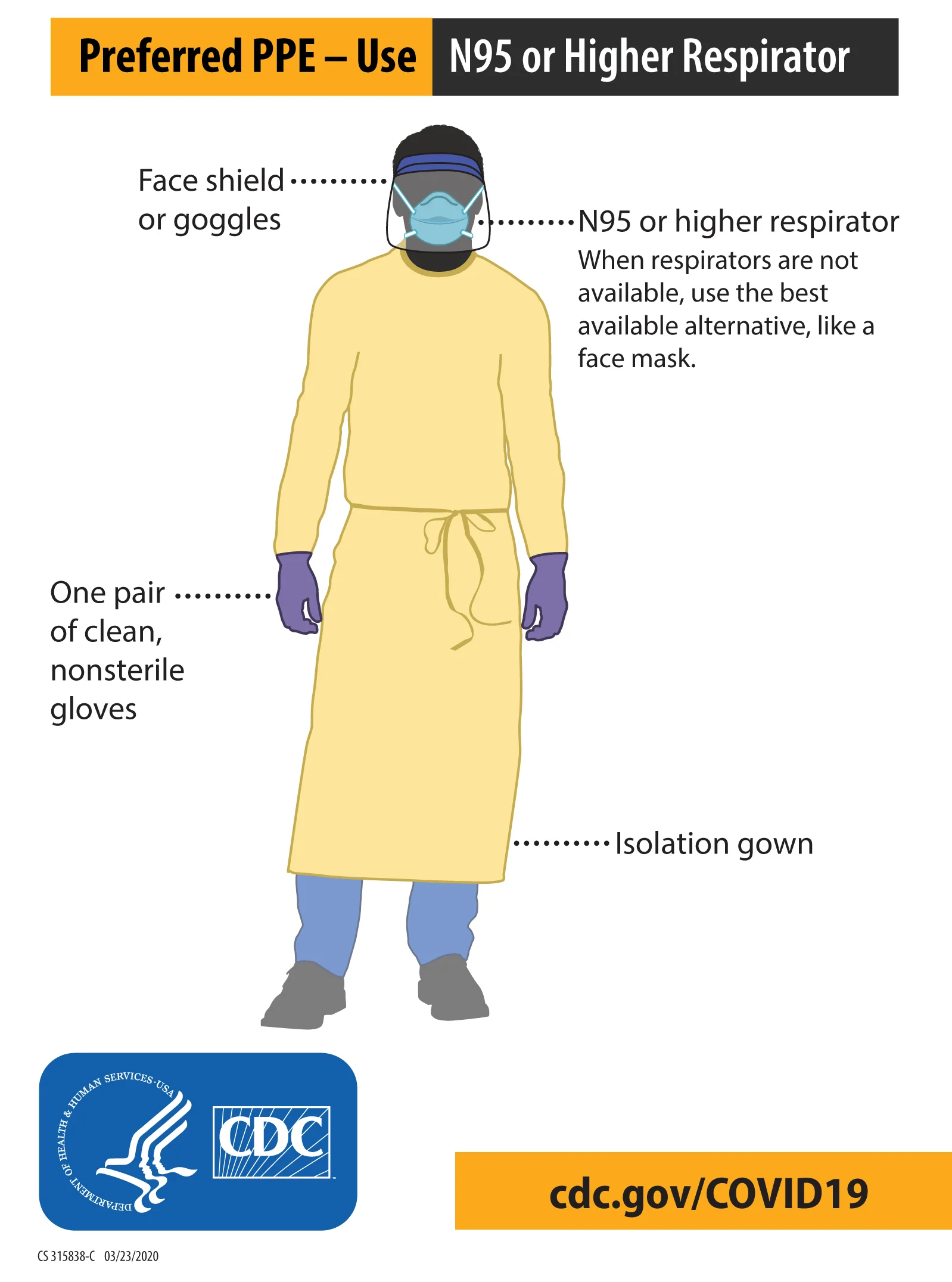
PPE
Gloves
Mask
Eye protection
Gown
Vest
Hair net & booties
Number of Patients
How many patients are there?
How many people are present?
Do I have the full picture?

Triage
Sort your patients
Sort your priorities

Additional Resources
Additional ambulances
ALS
Fire fighters
Rescue operations
Police
Bariatric ambulance
MD1
Supervisor / Incident management
Social services

Primary Assessment
Introduction
General impression
Level of consciousness
Airway
Breathing
Circulation
Disability
Exposure
Chief complaint
Baseline vitals
Transport decisions

Introductions
To the patient
To the family
To the other providers on scene
Set the tone
General Impression
Big sick
Little sick
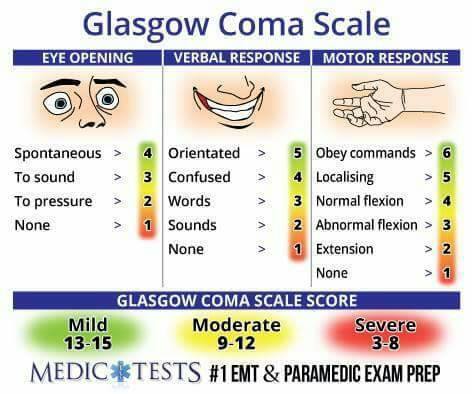
Level of Consciousness
AVPU
Alert: acknowledges you as you approach them
Verbal: acknowledges or reacts after you apply verbal stimulation
Painful: reacts to painfull stimulation
Unresponsive: does not respond to any stimulation
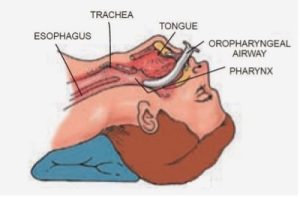
Airway
Is it patent?
if not, what can i do to open it?
If it is, can it remain open?
Breathing
Are they?
Is it adequate or inadequate?
if inadequate, why?
Does it need to be assisted?
How should i assist it?
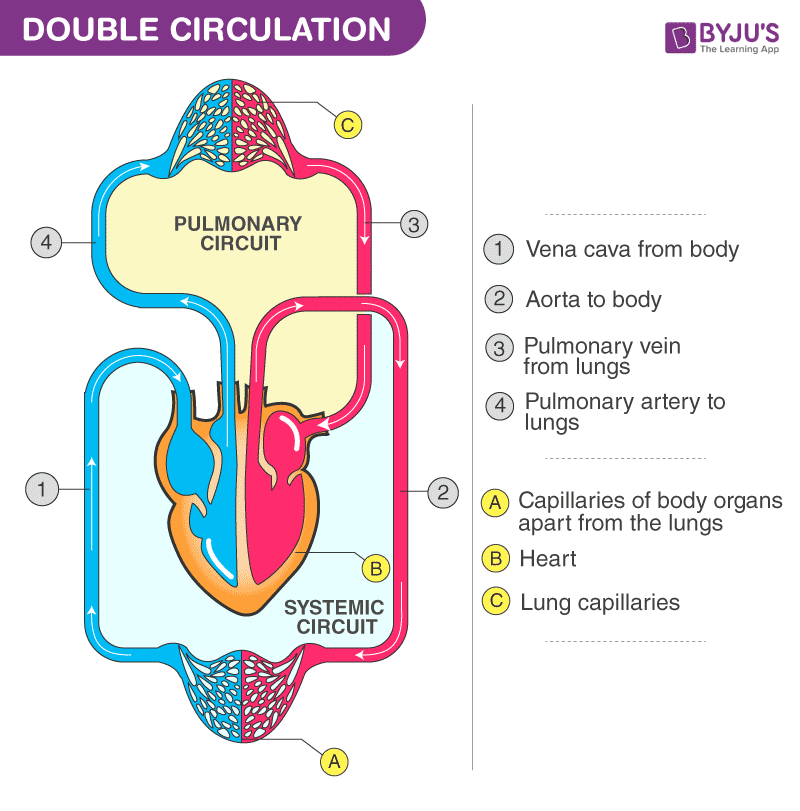
Circulation
Do they have a pulse?
What is the quality?
Is it too fast, or too slow?
Are they bleeding?
Are there signs of poor perfusion?
Disability
Is there an obvious cause for what i can see?
Is there something disabling my assessment?

Exposure
Can i get to my patient?
Can i perform my assessment?
Can i perform my treatment?
Is it safe to be here?
Is it SMART to be here?
Chief Complaint
What’s going on?
What happened?
Why am I here?
Why did you call 911 today?

Baseline Vitals
Pulse
RR
BP
Lung sounds
Pupils
Skin condition
SPO2
Pain
Transport Decision
Stay and play
Load and go

Secondary Assessment
History gathering
Focused physical assessment
Primary assessment
Differential diagnosis

Onset
Did it start suddenly?
Did this come over time?
Acute v chronic

Provocation / Palliation
Does anything make it feel better?
Does anything make it worse?
Have you taken anything for it?

Quality
What does it feel like?
Can you describe it to me?
If “shortness of breath”
Does it feel like you’re not getting enough air? or is it hard to breathe?

Region & Radiation
Can you point to where it hurts?
Does it travel anywhere else?
Does it hurt anywhere else?
Does it feel like it’s moving?
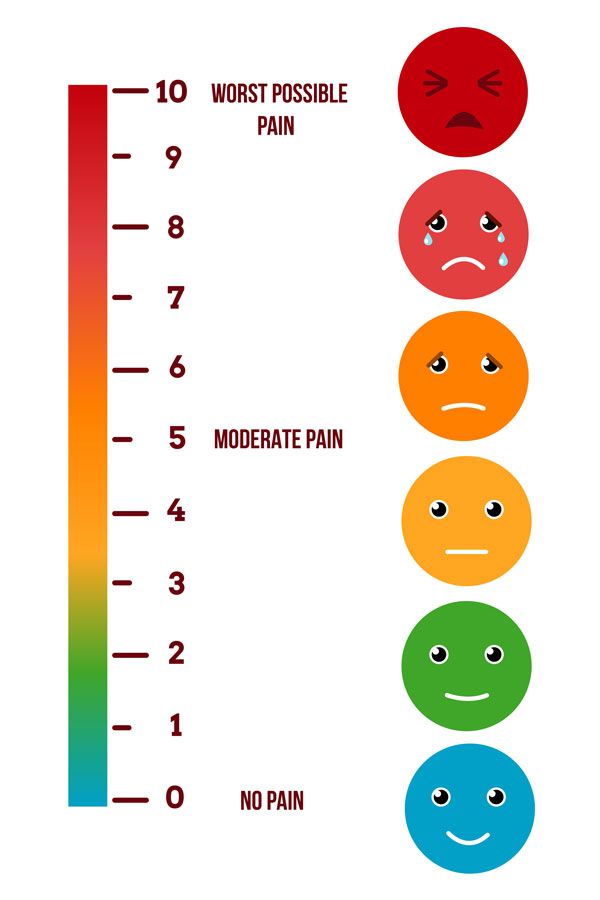
Saverity
On a scale of 0-10, 0 being no (complaint) at all, and 10 being the worst (complaint) you have ever experienced, what does it feel like?
Time
What time did all of this start?
If it was a while ago…
What caused you to wait, or prevent you you from seeking help sooner?

Associated Symptoms
Ask about symptoms that would confirm you differential diagnoses, or rule out another problem

Pertinent Negatives
symptoms that would rule out another problem

Signs / Symptoms
What do you see?
Signs
What are they complaining of?
Symptoms

Allergies
Are you allergic to anything?
Medications
Are you prescribed any medications?
Do you take your medications the way they are prescribed?
Do you take over the counter medication?
Are there medications that you are prescribed, that you’re not taking?
Have you had any recent changes on medications?
What do you take this medication for?

Pertinent Past Medical history
Have you ever had this problem before?
If so, what happened? What did they do for you? What did they diagnose you with? Did they tell you what to do if it happened again?
What kind of medical problems do you have?
Do you see a doctor for any medical problems?
Have you been diagnosed with any medical problems?

Last In / Last Out
Have you been eating regularly? If not, what is different, and for how long has it been different?
Have you been going to the bathroom regularly?
When is the last time you ate / went to the bathroom?

Events Leading Up
What were you doing when this started?
What were you doing earlier?
Did this start during that, or after?
Have you done this task before?

Focused Physical assessment
Perform a hands on assessment based on the patient’s area of complaint.

Primary Reassessment
General impression - reassess for changes, are they still what i initially thought?
Level of consciousness - has it improved , or worsened?
Airway - is it still patent? Did i fix it?
Breathing - are they still breathing adequately, do I need to try something else?
Circulation - has there been any positive improvement?
Disability - have i worked past it?
Exposure - do I need to expose more?
Chief complaint - has it changed, lessened, or increased?
Baseline vitals - trend vitals every 5/10 minutes
Transport decision - is my destination still appropriate

Differential Diagnosis
Based on the information you have gathered, what is going on with this patient?
Rule
Out
Worst case
Scenario
Patient Treatment & Transport
ABCS
Cardiovascular & Circulatory Management
Motion Restriction
Medications
Interventions
Transport
Transfer of Care
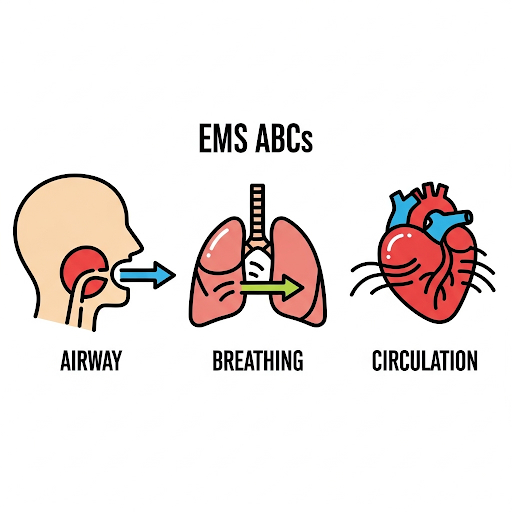
ABCs
Airway, Breathing, & Circulation should take priority when making treatment and transport decisions
They require constant reevaluation
There is no room for compromise
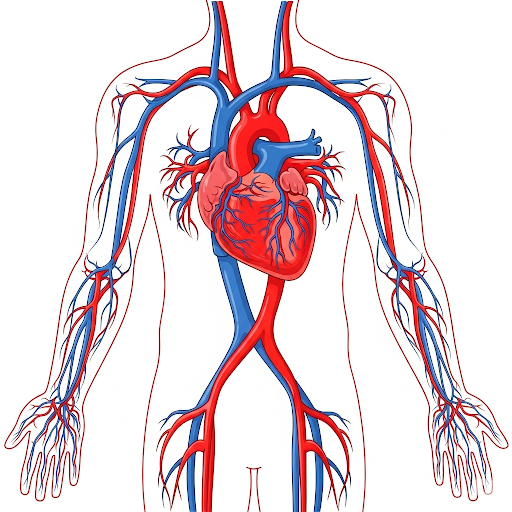
Cardiovascular / Circulatory Management
You won't always have the time or capacity to treat every single problem, clean every wound, or ask every question.
Trending Vitals:
Stable patients: every 10-15 minutes
Unstable patients: every 5 minutes
After any intervention or significant movement
Minimum of 2 sets on all patients
Gold standard = 3 sets on all patients
Motion Restriction
Modern EMS equipment has made lifting and moving patients significantly safer
Patients with serious conditions should not exert themselves further
Medications
Is there a medication I can give to help with this condition?
9 Rights of Medication Administration
Reassessment of efficacy

Interventions
Did the patient improve? Did they decline? Did my intervention work? Do I need to do more? Do I need to change my plan?

Transport
Do they need a specialty hospital?
Primary v Comprehensive Stroke
PCI Center
Trauma Center
Burn Center
Pediatric Center
Dialysis Capable
L&D w/ NICU
Do they need lights & sirens?
Do I know the safest route?
Is everyone, and everything secured?
Am I prepared to be on the road?

Transfer of care
LISBAR
SOAP
To someone of equal or higher medical authority capable of providing necessary care