EP1 Pre-Work: AFib and AFL
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
True or False: AFL is considered a type of SVT.
True
AFL commonly coexists with what other arrythmia? Can it be paroxysmal, chronic, or both?
Commonly exists with AFib (in 25-35% of AFib patients). Can be paroxysmal in normal hearts AND chronic in diseased hearts
What two factors affect the severity or existence of symptoms in patients with AFL?
Ventricular rate during AFL, and LV function
Presence or absence of structural heart disease
What is the short-term non-invasive option for treating Atrial Flutter? Why should anticoagulation medications be simultaneously administered?
Option: cardioversion to re-establish sinus rhythm
Anticoagulation meds: help to prevent the formation of blood clots because during AFL, the atria have been quivering and less blood is circulating, so blood may have clotted. If cardioverted, the atria beat more forcefully and could potentially eject the blood clots, leading to potential arterial blockage and a stroke.
What is a short-term option for treating AFL in patients with pacemakers or CIEDs? What is a potential complication
Option: Overdrive atrial pacing - use the device to pace at a rate faster than AFL and re-establish NSR, then address underlying disease
Complication: Can convert AFL into AFib in the process.
Primary treatment option for chronic AFL?
Ablation
Two segments of the RA and what structures they involve
Anterior lateral, trabeculated RA - includes right free wall and right atrial appendage
Posterior smooth RA - includes IVC, SVC, and CS. Fossa ovalis, Sinus Node, and AV node are structures found in this part of the RA
Where is the sinus node located?
As an epicardial structure at the SVC/RA junction
What is the function of the crista terminalis, a smooth, lateral ridge in the RA?
It separates the posterior, smooth tissue from the anterior, pectinate muscle.
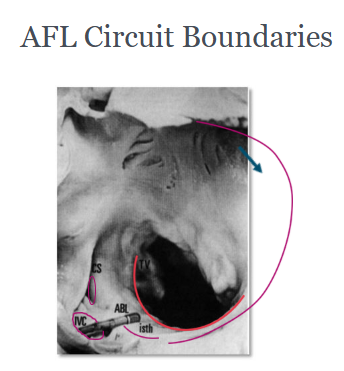
Describe the AFL Circuit Boundaries anterior and posterior
Anterior: tricuspid annulus (electrically inert fibrous tissue)
Posterior: crista terminalis at floor of the RA merging with Eustachian ridge/IVC, CS Ostium
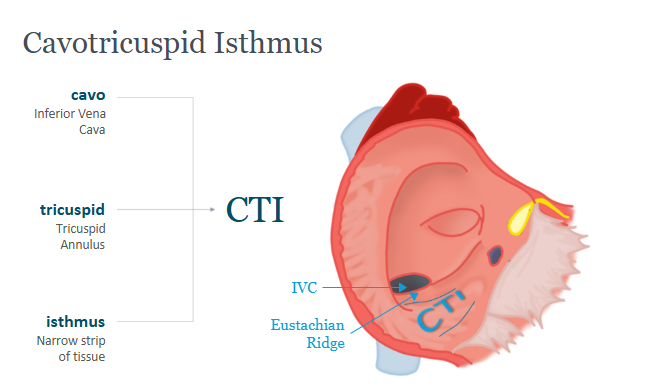
What is the CTI, what is its main characteristic, and what are its boundaries?
Cavotricuspid Isthmus - narrow strip of tissue
Characteristic: pathway of slow conduction, likely due to anisotropic muscles
Boundaries: IVC/Eustachian ride and annulus of the tricuspid valve
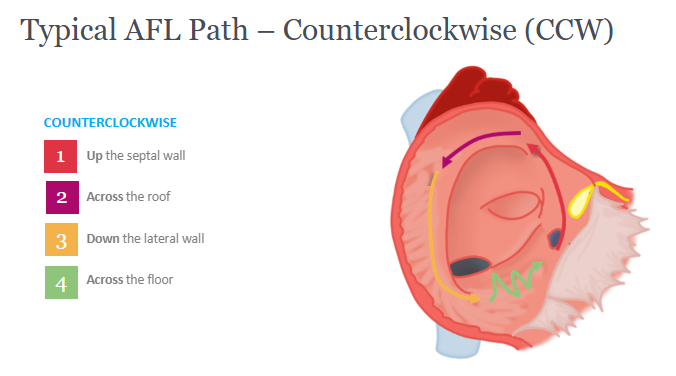
Key locations for CCW AFL
How do atrial signals in RA from AFL travel to LA?
Along interatrial septum → utilize crista terminalis to move across roof → down lateral wall of CT → along RA floor (CTI) between anterior and posterior boundaries.
Passively via Bachmann’s bundle, through fossa ovalis, and/or through septum by means of CS/LA connection
What do the sawtooth P waves of the AFL EKG represent?
Continuous activation of the atrium
Clockwise AFL (CW AFL) is only seen in about what percentage of clinical cases?
~10%
Considering leads II, III, and aVF, the inferior leads. What part of the circuit causes the upstroke and downstroke of the P waves?
Fast UPSTROKE as current travels down the lateral wall (CT) towards the CTI line
Slow DOWNSTROKE as the current travels along CTI line towards septum
A type of atypical AFL is perimetral flutter that uses the mitral annulus as its anterior boundary in the LA. If the activation is CCW vs CW, would the CS catheter be activated distal to proximal or vice versa?
CCW: CS proximal to distal
CW: CS distal to proximal
What is the primary cause for atypical AFL?
Surgical incisions or ablations in the RA or LA that act as obstacles to the circuit
4 most common catheters used when treating Atrial Flutter
CS catheter (decapolar) to monitor LA and LV signals
TA catheter (duodecapolar) wrapping around lateral wall to tricuspid annulus
Ablation catheter at CTI line
Sometimes, HIs catheter
Primary means of inducting AFL successfully 95% of the time? (Secondary option?)
Either atrial burst pacing from HRA or CS, or single/double atrial extrastimulus
*Secondary option would be to use Isuprel to induce the tachycardia
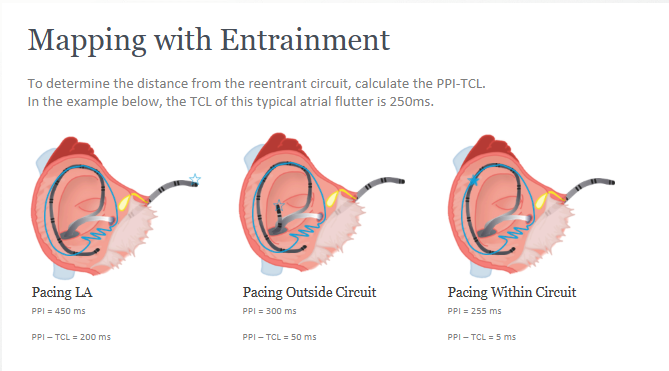
What is entrainment?
Continuous resetting of a macro reentrant circuit by a train of external stimuli
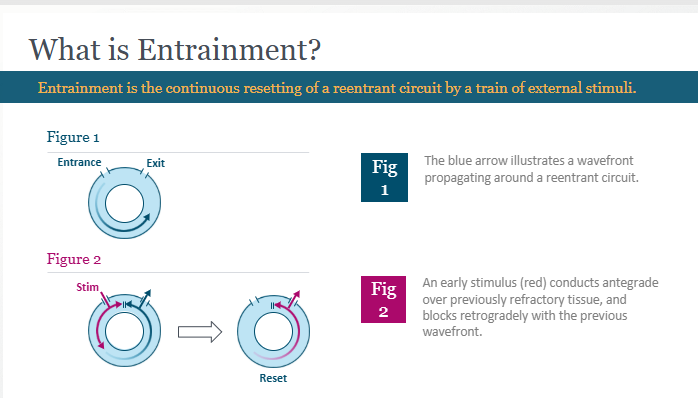
How is entrainment accomplished in the atrium? (6 steps)
Measure the TCL
Pace the atrium at 10-20 ms faster than TCL - overdrive suppression
Atrial rate should increase to pacing rate - confirm capture
Measure the post-pacing interval - time from end of pacing stimulus to propagate around circuit and back to pacing site
Take PPI - TCL, if < 30 ms, we are pacing from within the circuit.
CHECK IF MANIFEST OR CONCEALED based on atrial activation sequence
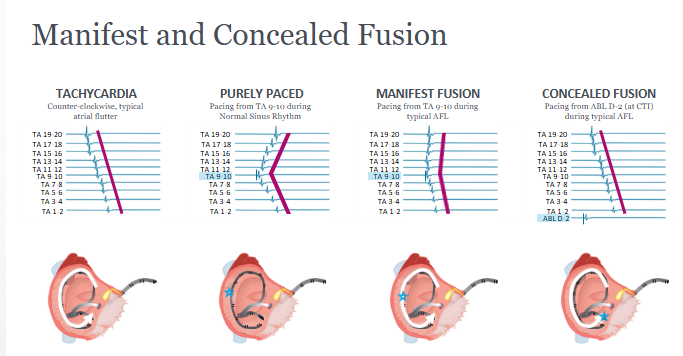
Describe the EGM patterns for a tricuspid annulus catheter when we have:
Basic CCW tachycardia
Purely paced in middle of catheter during NSR
Manifest fusion
Concealed fusion
Atrial signals are linear, from proximal to distal TA electrodes
Chevron atrial signals when paced from middle electrodes during NSR
Pacing from middle electrodes during typical AFL, slight chevron + slight linear = fusion
Pacing from distal catheter at CTI line, a place of low conduction, during typical AFL
True or False: each color of the time map is the same length of time
True (isochrone)
Where would you expect to see the highest concentration of colors in a time map?
At the CTI line, an area of slow conduction
What is the ideal ablation site for AFL?
CTI line - from 6 o’clock on the tricuspid annulus to the IVC, spanning across the CTI and connecting two electrically inert structures
The distal ablation EGM at the tricuspid valve shows a ____ atrial signal and ___ ventricular signal.
Small, large (1:4)
What are the two methods to confirm successful AFL ablation in patients whose tachycardia was 1) re-inducible or 2) not re-inducible?
1) Attempt to re-induce with atrial extrastimuli
2) Confirm bidirectional block for both CCW and CW directions
List the four methods to confirm bidirectional block
Evaluate activation sequence
Transisthmus time
Double potentials
3D Mapping
Bi-directional block: Activation sequence. Describe.
Atrial pacing during NSR, observe activation along TA catheter. Pace from either the medial or lateral side of the circuit, if we have chevron pattern then NO block, if we have linear pattern then YES block
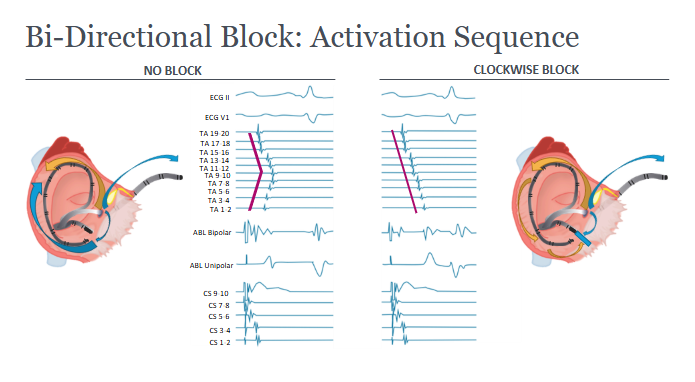
Bi-directional block: Transisthmus time. Describe.
The time it takes to cross the ablation line. It should be 150 ms or greater, or have increased by 50% after ablation. Use proximal CS as medial and ablation or TA catheter as lateral
Bi-directional block: Double Potentials. Describe.
Pacing at CS ostium. Observe atrial activation first on medial side, then on lateral side, after signal has traveled by force all the way around the TA. If > 110 ms, we have complete block. Should also check with pacing from the low lateral RA to confirm block in both directions.
Bi-directional block: 3D mapping. Describe.
See activation halt at the CTI line.
How would AFL have been initiated?
Unidirectional block in either the slow or fast pathways that were connected
Define atrial fibrillation
Supraventricular arrhythmia characterized by rapid and irregular activation of the atria without discrete P waves present on the ECG. Stimulate AFib by a premature atrial contraction. Also shows irregular ventricular responses with normal QRS complexes, as ventricular contraction is still controlled by the AV node.
What is the most common arrhythmia?
Atrial fibrillation
3 technologies that can be used to detect AFib when the arrhythmia is not present
Holter Monitor (short-term), Implantable Cardiac Monitor, or Pacemaker/Defibrillator
4 classifications of arrhythmia
Recurrent: two or more episodes of AFib
Paroxysmal: AFib that terminates spontaneously or with intervention within 7 days of onset
Persistent AFib: sustained beyond 7 days
Permanent AFib: sustained beyond 1 year, no further attempts made to return to NSR
What are the three key risk factor categories for chronic AFib to develop?
triggering, atrial dilation, or lowered ratio of healthy to diseased tissue
Three methods of rhythm control/AFib correction
Cardioversion
Pharmacological Therapy - suppress triggering ectopic beats
Catheter Ablation - for patients who remain symptomatic after adequate drug therapy
Two methods for rate control for patients with AFib
Pharmacological treatment
AV node ablation with permanent pacemaker implantation
What are some common factors that trigger the onset of AFib?
PACs from PVs or non-PV trigger sites, LV posterior wall, AFL or a paroxysmal SVT
List the four mechanisms by which pulmonary veins can trigger and maintain AFib.
Autonomic
Focal
Wavelet
Composite
Pulmonary vein trigger mechanism #1: Autonomic. Describe.
Ganglionated plexuses at PV/LA junction that can initiate AFib via nervous system
Pulmonary vein trigger mechanism #1: Focal. Describe.
Foci found in pulmonary veins that propagate into atrium
Pulmonary vein trigger mechanism #1: Wavelet hypothesis. Describe.
Multiple, wandering wavelets in PVs that maintain AFib. These daughter wavelets stemmed from an initial wavelet
Pulmonary vein trigger mechanism #1: Composite. Describe.
Overlap of triggers (wavelet + foci + autonomic ganglion)
3 key non-pulmonary vein triggers of AFib
Musculature of the coronary sinus
SVC
Ligament of Marshall between left PVs and LAA
What is INR?
International normalized ratio, indicating how long it takes for blood to clot. Want to maintain at 2.0 - 3.0
What is ACT?
Activated clotting time when heparin is being administered during ablation procedure. Goal is to maintain 300 - 350 seconds
Cryoablation has a risk of damaging what structure when targeting right-sided veins?
Phrenic nerve
List the four ablation treatment strategies
Segmental
Circumferential
WACA
CFAE
Ablation Treatment Strategy #1: Segmental. Describe.
Ablation performed at the ostia of PVs only where PV vein-muscle potentials are identified
Ablation Treatment Strategy #1: Circumferential. Describe.
Ablate entire circumference of the PVs → GOLD standard

Ablation Treatment Strategy #1: WACA. Describe. What is the risk?
Ablation circumferentially around the sets of right and left PVs + connecting ablation line for superior and/or inferior PVs
Risk: complex procedures or can induce other arrythmias
Ablation Treatment Strategy #1: CFAE. Describe.
Ablation lesions targeting regions of long, low-voltage, fractionated signals (i.e. septum, LA roof, posterior wall, mitral annulus, etc.)
Describe entrance block as a post-ablation verification method for PV isolation.
Pace from somewhere in the LA and see if the signal propagates or does not propagate to the PVs. If it does not then we have achieved complete PV isolation.
Describe exit block as a post-ablation verification method for PV isolation.
Pace from somewhere in the PV or along the posterior wall and see if the signal propagates or does not propagate to the rest of the heart. If it does not, then we have achieved complete PV isolation.
Describe differential pacing as a post-ablation verification method for PV isolation.
Identify far-field vs near-field atrial signals. Use two catheters in LA. PVs are not isolated if pacing spike from LAA travels to PVs and triggers a potential
Describe how electrical anatomical mapping can be used as a verification for PV isolation.
Voltage - grey tissue near the PV/LA junction indicates dead, non-conducting tissue
Time - can indicate where there is a gap in isolation using Sparkle Map
4 major complications that could result during AFib ablation
Atrioesophageal Fistula - joining of esophagus and left atrium
Char/clot at location of ablation that could lead to stroke
Phrenic nerve injury - can result in diaphragm dysfunction
Pulmonary vein stenosis - narrowing of PV lumen - constricts blood circulation from lungs to LA
Define aberrant Atrial Fibrillation
Problem with the conduction system down the line (could be block, refractory) and AFib signals don’t conduct, so QRS complex may be wide
What are the two most common clinic risk factors for chronic AF (structural heart disease)?
Hypertension and ischemic heart disease
For CCW AFL, the interior leads have positive or negative P waves?
Negative (traveling away from interatrial septum