Neurodegenerative Conditions 😶🌫️
1/42
Earn XP
Description and Tags
ALS, MS, Huntington’s, Guillain Barre, Parkinson’s, Dementia
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
Akinesia
-freezing gait/ other movements
-teaching rocking is useful in helping clients initiate movement
Ataxia
-uncoordinated movements, tremors may be present
~you need to call “a taxi” because you’re uncoordinated
-tx: stabilize proximally to help distal movements; pt can use unaffected side over hand with tremor to help with fine motor tasks; orthoses like c-collar/wrist splints can help to reduce impact of tremors
Dyskinesias
Involuntary, non-repetitive movements that are associated with basal ganglia damage
Dystonia
-creates sustained abnormal postures/disruptions of ongoing movement
Dysmetria
decreased coordination of movements *dysmetria ~ off meter/ off beat
Festinating gait
Shuffling gait- small, quick steps from forward-tilted head and trunk posture
Special Evaluation Consideration for Neurodegenerative Conditions
-How pt’s disease may progress and/or have variable symptoms (e.g. symptoms that change during the day/week/month/seasons)
-Pt’s understanding/ level of acceptance of progressive nature of disease
General Neurodegenerative Disease OT Interventions
-Help client compensate/adapt as function declines
-Ex: cognitive compensatory strategies, energy conservation, environmental mods, adaptive equipment, exercise, caregiver training
Multiple Sclerosis (onset, diagnosis, symptoms, patterns, medical management)
-slowly progressing CNS disease of demyelination characterized by remissions and exacerbations of symptoms
Onset
most often in 30s (20-50)
Symptoms
Acute/beginning
weakness/clumsiness in leg or hand
paresthesia (in one or more extremities/trunk/face)
visual disturbances (diplopia, partial blindness, nystagmus, eye pain)
emotional disturbances (lability, depression, euphoria)
Long term is typically fatigue, general weakness, intention tremors
Balance issues/vertigo
Bowel/bladder/sexual dysfunction
Spasticity/increased reflexes/ataxia/tremors/pain
4 types: relapse remitting (best), secondary progressive (has some neurological dysfunction), primary progressive (no remission, neuro function worsens), progressive relapses (worse)
MS OT Intervention
-Gentle ROM is good, so is caregiver education
-Strengthening is usually a bad thing
-cognitive and physical abilities can vary throughout the day- try to time sessions when pt usually feels the most energized
-can benefit mentally/emotionally from group-therapy/CBT
-sitting with at least 90 hip flexion can help reduce spasticity
Amyotrophic Lateral Sclerosis (ALS) (Prognosis, Symptoms, Stages, Medications, Interventions)
-Motor neurons in CNS & PNS are replaced by scar tissue over time (plaques)
-AKA Lou Gehrig’s disease
-onset ~57 y.o.
-death in 2- 5 years after onset
Symptoms
muscle weakness/atrophy progresses distally to proximally
most common first symptoms are weakness in small hand muscles or asymmetrical foot drop
Muscle cramping at night- usually in calves
Corticospinal tract involvement symptoms: spasticity & hyperactive deep tendon reflexes
⚡️spinal & spasticity
Corticobulbar tract involvement
Dysarthria (slowed/slurred speech)
Dysphagia (difficulty swallowing)
⚡️difficult to talk/swallow with a bulb in your mouth
May eventually have difficulty breathing, requiring respiratory therapist to be on team
Sensation, vision, hearing, bowel/bladder usually NOT affected
Stages
Stages I-III
can walk, but growing weakness (some → moderate → severe)
Stage IV
requires W/C (d/t extreme weakness in LEs)
require some assistance with ADLs
Stage V
Dependent with ADLs (d/t extreme weakness in arms and legs)
Stage VI
unable to get out of bed
Medications- slightly slow disease progression/reduce negative impacts on functioning but have side effects
Riluzole/Rilutek- dizziness, fatigue, GI issues, liver issues
Edaravone (Radicava)- swelling, SOB
Interventions:
because it is progressive/degenerates a large part of functional skills, CAREGIVER education is really important for issues
early stage: try to keep some muscle, just dont overexert
middle stage: muscle loss will happen, better for ROM
late stage: ulcer prevention
W/C recs: often start with high backed, reclining, light weight, small turning radius, with head/trunk/extremity support then progress to power W/C with adaptable controls
Use voice operated/hands-free tech
Can extend ability to drive a car by using hand controls and adding W/C lift

Presbyopia
Decreased ability to focus clearly on close objects, and switching from near to far
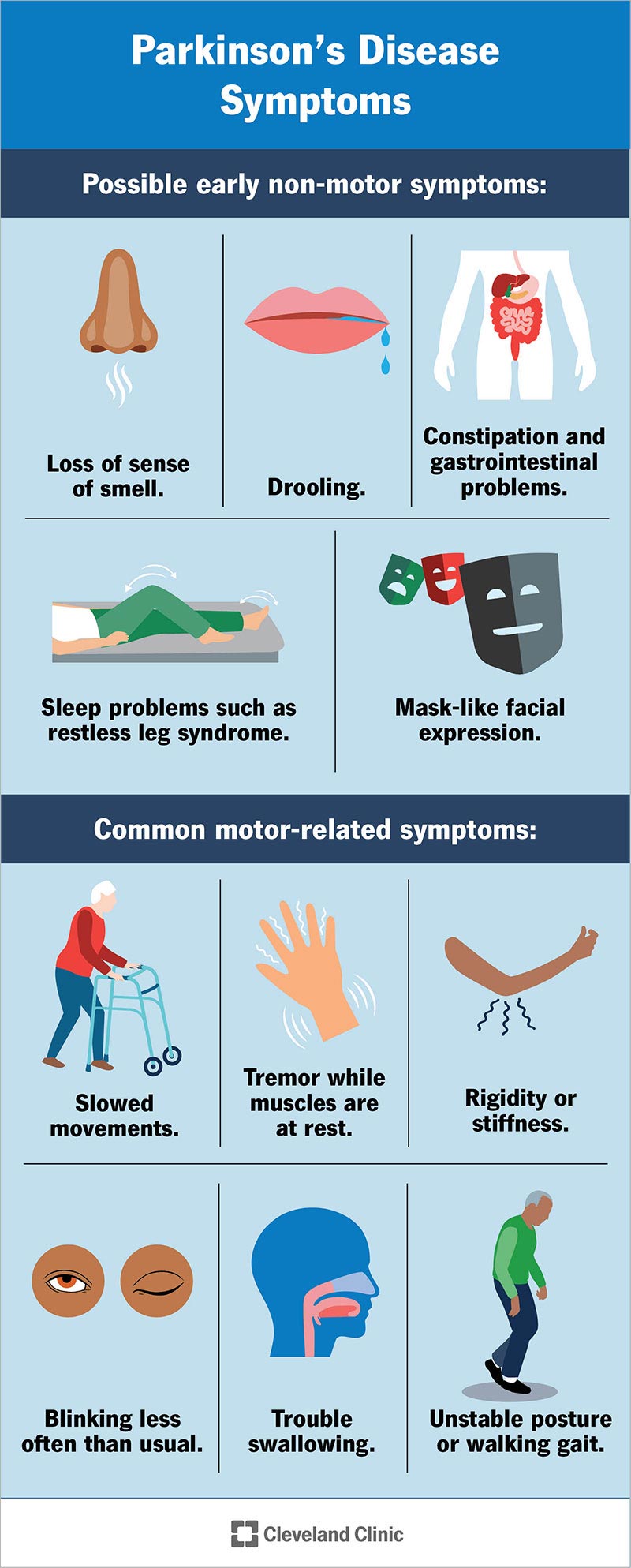
General Parkinson’s Info (Symptoms, Medications, Evaluation, Intervention)
-CNS movement disorder
-Symptoms
pill-rolling tremor in one hand- usual first sign
TRAP
Tremor
-resting tremors of hand (not usually present during sleep/voluntary mvmnts)
Rigidity
-muscle rigidity that is NOT velocity dependent during passive movement
Cogwheel or lead pipe rigidity
Akinesia- no/slow voluntary movements
Motoric freezing
Postural Instability
stooped posture, lack of arm swing, festinating gait, retropulsion (falling backward), falling forward (propulsion)
inc fall risk
-stress exacerbates symptoms
-life expectancy usually not impacted but QOL is
depression
Fatigue
Urinary/sexual dysfunction
Swallowing difficulties
Weight loss
Sensory symptoms
-Medications
Used to help with loss of dopamine
Levodopa
Carbidopa (Sinemet)
May see increased dyskinesia when medication is having peak effects; side effects are somewhat unpredictable
Help with rigidity/tremors
Benadryl
Arcane
Cogentin
Antiviral drug that helps with symptoms
Amantadine
-Evaluation
COPM to find “empowering” goals, evaluate at multiple times of day to get accurate picture, may need to screen cognition/depression
-Intervention
freezing (avoid crowds/tight spaces/turns/rushing/clutter/distractions)
instruct on use of cane/walker
counting/singing/auditory cueing can help make movements smoother
Feeding
built-up/weighted utensils/spill guards
increased time to eat
distal wrist weights for tremors
put arms on table and keep items close to body to inc stability)
Movement (LSVT BIG for gross and fine motor coordination- need cert)
Active ROM against gravity that is occupation based can be good for cogwheel rigidity
E.g. reaching overhead for a box of cereal on a shelf when cogwheel rigidity is present in both shoulders
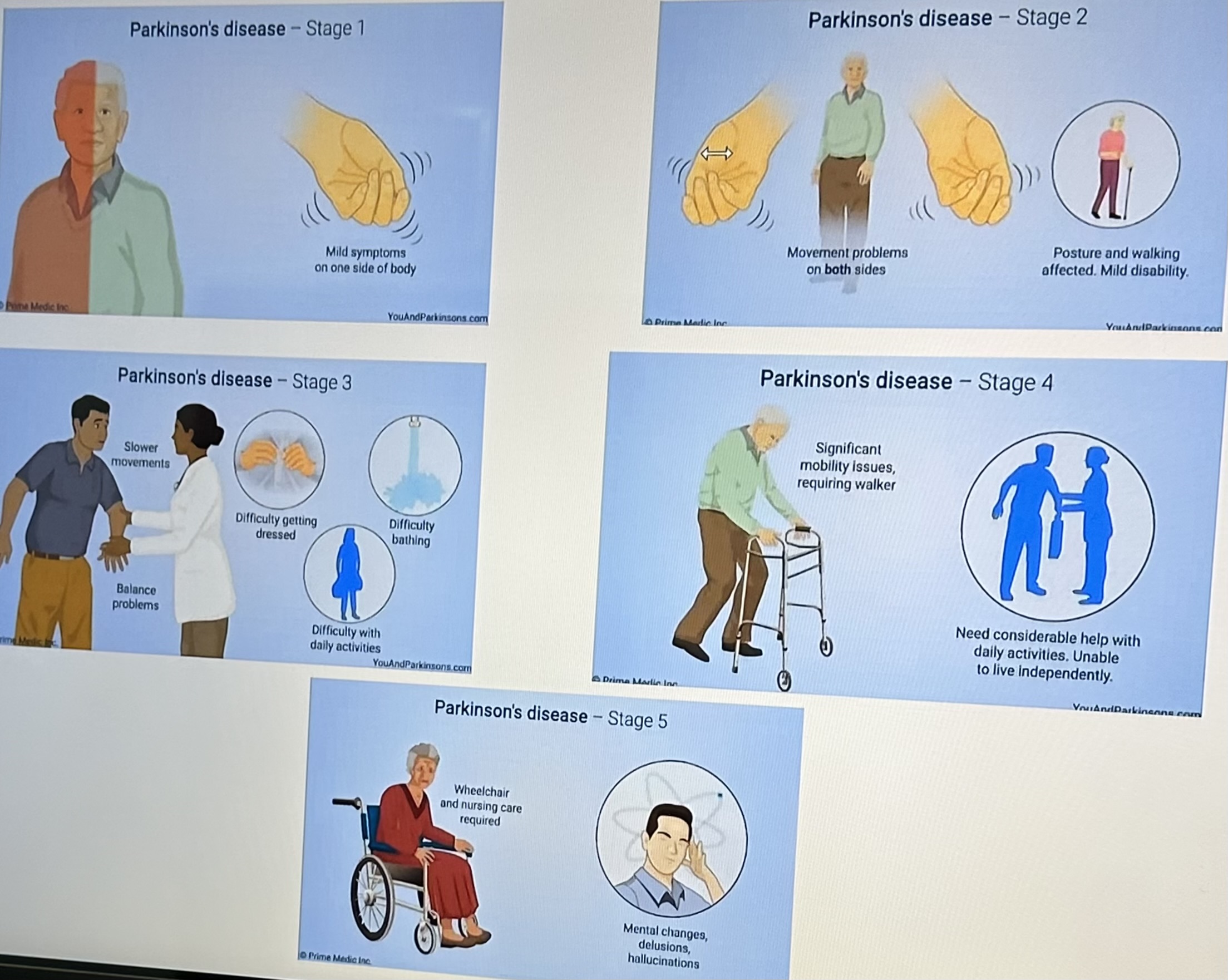
Stages of Parkinson’s Disease
Stage I
Unilateral tremor
Minimal-no functional impairment
Stage II
Bilateral tremor
Independent with ADL
No balance impairment
Stage III
first signs of impaired righting reflexes
onset of disability in ADL performance (min A)
can lead independent life
Start to see high fall risk
Stage IV
requires help with some or all ADL
Unable to live alone without some assistance
Able to walk/stand (with walker)
Stage V
Unable to stand/walk
Unable to perform ADLs
W/C and Max A are required
Extrapyramidal Syndrome
-movement disorders such as akathisia (cant stay still), dystonia (twisting motion), and parkinsonism (tremors) caused by antipsychotic drug therapy
-dangerous if working with tools
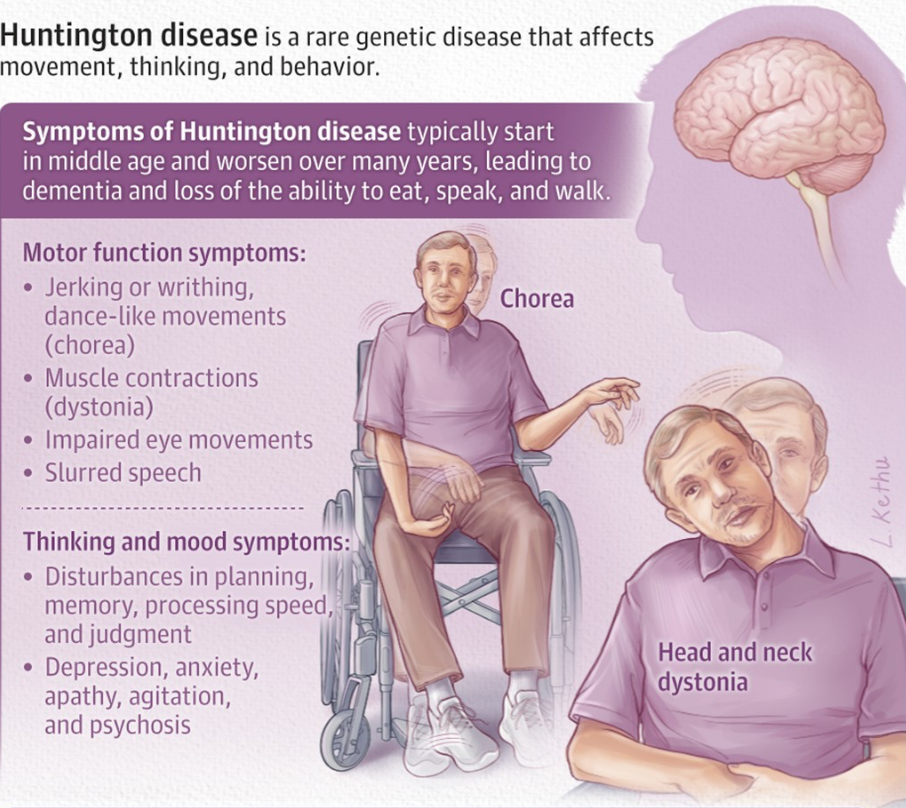
Huntington’s Disease AKA Huntington’s Chorea (Prognosis, Symptoms, Stages, Eval, Intervention)
-onset during early middle age (30s/40s)
-usually fatal ~20 years after the onset of symptoms
-hereditary components
Symptoms
characterized by uncontrollable body movements
Chorea (rapid, involuntary movements)
Akathisia (motor restlessness)
Dystonia (abnormal posturing, usually of arms)
Bradykinesia (slow movements)
Akinesia (lack of initiation)
Impaired walking/balance and decreased motor control (use AE)
Cognitive Decline
difficulty with some cognition (i.e. word retrieval skills)
Difficulty with problem solving skills
Dysphagia- difficulty swallowing
Psychosocial impacts/Emotional Disturbances
Usually significant depression/social isolation b/c it is often diagnosed during middle age
Some individuals die by suicide
Fatigue (use activity mod/breaks)
Stages
Early stages-
Stage 1 (Early Stage) & Stage 2 (Early Intermediate Stage)
some impacts at work and home from impacts on balance/motor/coordination, but mostly independent
Middle stages-
Stage 3 (Late Intermediate Stage)
difficulty with memory and decision making
work becomes difficult as well as IADLs
Later stages-
Stage 4 (Early Advanced Stage) & Stage 5 (Advanced Stage)
dysarthria makes speaking difficult
High risk for choking & falling
unable to work
needs major and eventually full assistance with care
Evaluation
Unified Huntington’s Disease Rating Scale- assesses motor, cognitive, functional, and behavioral changes
Intervention
Should be compensatory
Early on modifications should focus on activities that require fine motor skills (fastening zippers, buttons, hooks, etc.) since challenges are usually limited to fine motor coordination at the beginning
Community/support groups
Eating- may need modified diets, adaptive utensils, minimal distractions when eating
Maintain community mobility + safety in home
Maintain valued roles
May need to find a simpler job
Finance management
Can encourage auto payments
Environmental Mods
Guillain-Barré Syndrome (GBS) Overview (Onset, Prognosis, Diagnosis, Symptoms)
-Acute and rapidly progressing demyelination of the peripheral nerves and spinal roots
Onset- equal for all ages
Prognosis
Recovery generally happens after 2-4 weeks after onset
Long-term Impacts
Fatigue is most commonly reported residual symptom
80% are ambulatory within 6 months
50% have mild neurological deficits
15% have residual functional deficits
5% die from complications
Symptoms
acute, rapidly progressing symmetric muscular weakness
Weakness starts distally and progresses proximally
mild distal sensory loss/parasthesias
Often start in stocking-glove distribution
Loss of deep tendon reflexes
Respiratory failure and dysphagia in some cases (need to monitor vitals and have a respiratory therapist)
Acute Guillain-Barre Syndrome
-onset is sudden and rapidly progressing- usually starts with paralysis of feet that moves up
-most prominent factors is decreased strength of muscles which can lead to swallowing issues, fatigue (biggest pt complaint), and pain
-loss of deep tendon reflexes
Plateau Guillain-Barre Syndrome
-where symptoms are worse, may need ventilator
-paralysis of the muscles of the head and neck can affect speaking, swallowing
-OT eval often covers positioning to prevent skin breakdown, communication, control of phys env, comfort, and anxiety management
Intervention:
-train communication tools (signs/picture boards),
-adjust laying/sitting positions to optimize function/comfort and limit risk of skin breakdown (teach caregivers as well)
-Position client for trunk/head/ UE stability
-Educate pt/family about condition and anxiety-reduction techniques
Recovery Guillain-Barre Syndrome
-GBS has no cure but ~80% of pts can walk after 6 months, 60% get full strength back after a year
-OT eval focuses mobility, ADLs, communication, and community/work reintegration
Intervention:
-energy conservation/fatigue management good diet
-gradually increase tolerance of complexity of task
-dynamic splints can help maintain ROM for wrist/fingers/ankle i.e. hinged drop-foot orthosis
-Adapt modes of communication based on client (e.g. speech to text on phone)
Myasthenia Gravis
Rare condition caused by autoimmune attack on acetylcholine receptor
Onset
Younger women
Older men
Prognosis
varied, but progressive and disabling
Death may occur from respiratory complications
Symptoms
Episodic muscle weakness
Muscle fatigue after exercising
Proximal limb weakness
Weakness in muscles for swallowing/talking (dysphagia/dysarthria)
Difficulty breathing (may require ventilator)
Impacts on eyes
Ptosis (eyelid drooping)
Diplopia (double vision)
Anxiety
Tachypnea
Tachycardia
Restlessness
Medical Treatments
Cholinesterase inhibitors/anticholinergics
Immunosuppressive agents/corticosteroids

Dementia vs. Normal Aging
-If a change is noticed look deeper
-Treatable causes of change- mental health issue, physical health issue, medication complication, sensory change like hearing loss, new chronic condition like diabetes
Dementia vs. Alzheimer’s
Dementia- not a diagnosis, but a general umbrella term for deterioration of brain capacity (at least 2 parts of brain are dying)/cognitive decline that is constantly changing; consists of 85-90 different conditions; can’t be fixed/stopped at least right now
Alzheimer’s- most common form of dementia (~75%), associated with specific patterns of brain changes
4 A’s of Alzheimer’s (Amnesia, Apraxia, Aphasia, Agnosia)
Amnesia
loss of memories (facts, info, experiences)
Apraxia
loss of ability to map out motor actions in order to repeat them in functional activities
Aphasia
inability to comprehend/formulate language because of damage to specific brain regions
Agnosia
loss of ability to recognize objects, faces, voices, or places
Vascular Dementia
-from series of mini strokes
-2nd most common type of dementia after Alzheimer’s
-Cognitive deficits similar to Alzheimer’s but with better memory in tact
-Gait impairment
-Typically see sudden appearance/ abrupt worsening of symptoms
-Requires immediate emergency medical attention
Frontotemporal Dementia
-marked by behavioral changes such as impulsive, listless, inappropriate social, lack of empathy, loss of insight to behaviors, increased sex drive, progressive aphasia, symptoms similar to Parkinson’s
-Sudden onset
-Medical tx still in development
Dementia with Lewy Bodies
-Marked by visual hallucinations and parkinson’s-like motor symptoms
⚡️hallucinations~ ha”lewy”cinations
-gradual progression
Early Stage Dementia
-Difficulty with IADLs (money management, way-finding)
-Increased irritability, mood swings, sadness, anxiety
-More forgetful of recent events
-Signs can look similar to age-related memory loss
Middle Stage Dementia
-Confusion with time and place
May become lost in familiar places
-Moderate IADL issues
-Difficulty making choices (like with clothes)
May behave inappropriately e.g. wearing winter clothes on a hot day
-General confusion/difficulty recalling recent events
-Issues with judgement of direction, distance may increase falls
Difficulty executing simple movements
-May have visual/perceptual issues, difficulty with reading
-They may think they’re in an earlier stage of life
-May see/hear things that aren’t there
Late Stage Dementia
-Unable to remember events that happened a few minutes before
-Difficulties with posture and balance
Bed-bound
-Swallowing and chewing difficulties
-Speaking issues, may only say a few words
-Need help with feeding, washing, bathing, etc.
-May have uncontrolled movements
Random Dementia Pointers for the Exam
-Observation and interviewing family is good for assessment
-Most assessments likely too cognitively challenging
-Family can use locks, door/bed alarms, visual barriers for safety
-Visual cues are good for memory issues, as well as bathroom schedules for independence
Screening Tools for Cognition
-Mini Mental and BIMS are quick and good to start out with
-Use MOCA/SLUMS for early stages of Alzheimer’s as they are for executive functioning
Types of Skill Learning (Generalization vs. Transfer)
-Generalization: skill from one context to another
-Tranfer: strategy of one task to another
Motor Learning Key Words for the Exam
-doing the activity is a good answer
-any type of cueing is a good answer
General Interventions for Dementia (Environmental changes, Monitoring personal comfort, Providing security objects, Providing opportunities for exercise)
Environmental Changes
Create a safe environment
Prevent falls, avoid scatter rugs/clutter
Create a calm environment by reducing background distractions, stressors or clutter
Monitor Personal Comfort
Make sure room temp is comfortable
Monitor skin irritation
Provide Security Object
Give favorite blanket/book/anything comfortable that client is familiar with
Provide Opportunities for Exercise
Wandering is sometimes caused by need to move
Allen’s Cognitive Levels (Mnemonic & Overview)
⚡️All Players Must Get Extra Points
1- Automatic
2- Postural
3- Manual
4- Goal-directed
5- Exploratory
6- Purposeful
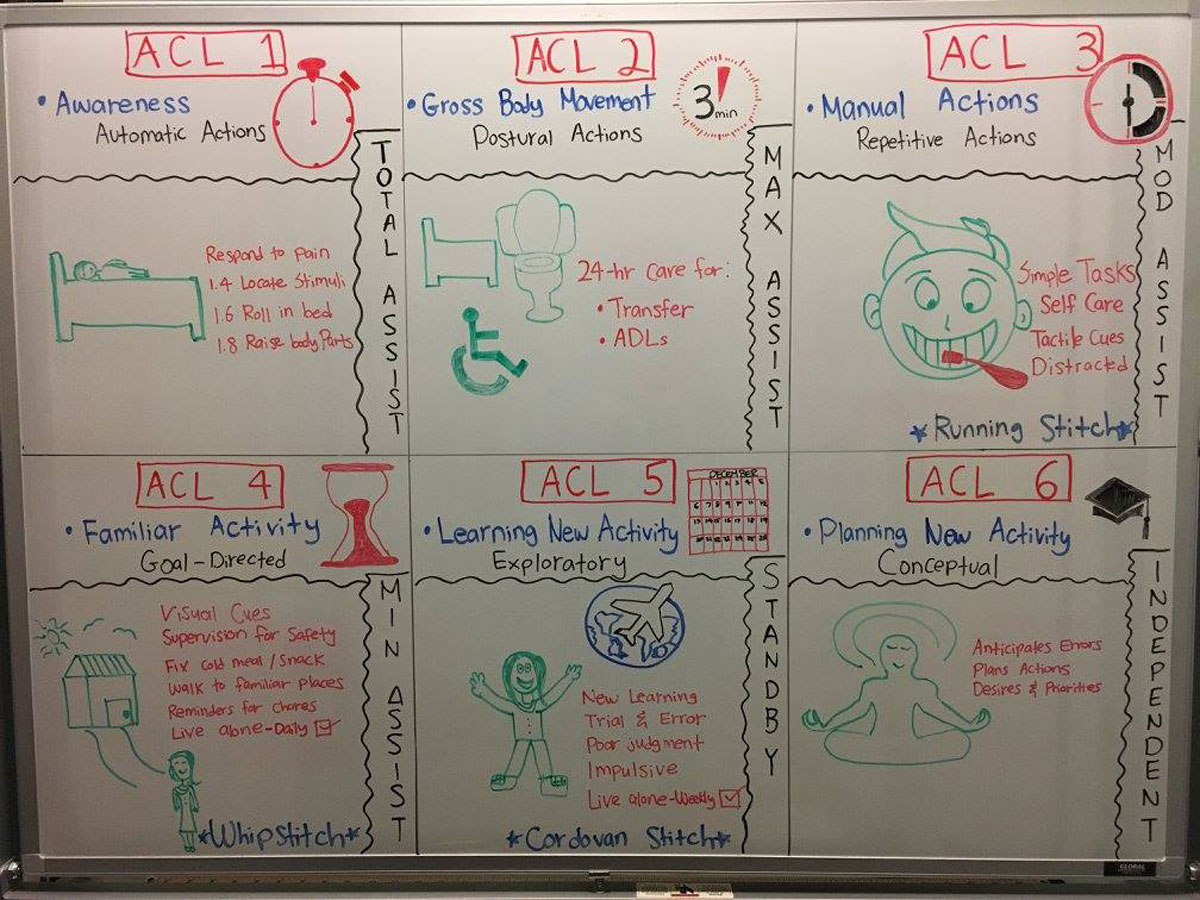
Allen’s Cognitive Level 1
Automatic/Awareness
Essentially in a coma
Automatic motor response
Total assistance with all activities and 24/7 care
Attention is fleeting and non-selective/not conscious
Focus on single sensory activities, bed mobility, skin integrity, passive mobility
1.4 location stimuli
1.6 rolling in bed
1.8 raising body part
Allen Cognitive Level 2
Postural/ Large Body Movements
Some awareness about posture, gross body movements, large objects in the room
Can overcome effects of gravity
(work on sitting and righting reactions)
Can imitate gross motor actions
ADLs can be accomplished by imitation
Max assistance 24/7 care
Need close on site-supervision
Risk of wandering (try to give client activity and implement safety measures)
Create a sensory rich environment that helps to give client sensory stimulation
2.0 overcoming gravity/sit
2.4 aimless walking
2.6 directed walking
Allen Cognitive Level 3
Manual actions/ Moderate assistance
Uses hands to manipulate objects
Can complete manual repetitive actions e.g. coloring
Need set up/supervision for ADLs; can perform familiar ADL tasks but may be distractible/unpredictable
May need tactile cues/ demonstration/ long-term repetitive training
Cause and effect emerges
Able to imitate running stitch (three stitches)
3.0 grasping objects
3.2 distinguishing objects
3.4 sustaining actions on objects
Allen Cognitive Level 4
Familiar Activity/ Min assistance
Able to perform purposeful short tasks (making sandwich, buying drink from a store)
May need visual cues (but no longer need tactile cues)
Needs supervision at lower levels, but can live alone at 4.6 with some check-ins
Needs assistance with new tasks
Able to imitate whip stitch (three stitches)
attention last up to an hour, can do goal directed actions e.g. putting a bird feeder together
4.0 sequencing familiar actions
4.2 differentiating features of objects
4.4 completing a goal
4.6 cut off for independent living
Allen Cognitive Level 5
Exploratory/ Learning new activity
New learning can occur
Learns through trial and error
Standby assist for ADLs
Poor organization and socialization
Able to imitate the single cordovan stitch using overt trial and error method for three stitches
5.2 live independently with weekly checks
5.4 self directed learning
5.6 can live independently with no checks; considering social standards
5.8 consulting with others
Allen Cognitive Level 6
Planned
No global cognitive impairment
Independent with all activities (No supervision needed)
New motor learning can be done safely
Plans new activities
Reflect on mistakes
May seek guidance
Reisberg Scale (Global Deterioration Scale)
Stage 1
no noticeable impairment
Stage 2
Memory impairment begins to be noticeable
might get memory confused with aging
Stage 3
Family members/health care providers notice mild decline with problem solving/remembering names/details
Stage 4 Alzheimer’s Stage I
Obvious difficulty with problem solving/remembering names/details
May withdraw from new social situations
Interventions: Visual aids, familiarity
Stage 5 [Alzheimer’s Stage II (Bashful)]
Patient will begin to need help with functional ADLs
May benefit from adult day care
Interventions: simplify tasks in familiar locations, make objects accesible, eliminate environment distractions, goal-directed with visuals and initiation cues (e.g. help select outfit), use personal photos to promote memories and social connection
Stage 6 [Alzheimer’s Stage III (Grumpy)]
Requires assistance with most ADLs
Personality begins to change
May become delusional/aggressive
Not oriented to time
Interventions: Caregiver training on routine/behavior management, structured tasks, home mods for safety (Audiovisual systems ~baby monitors, camouflage exits, hide knives), keep them active during the day to reduce night-time wandering
Stage 7 [Alzheimer’s Stage IV (Sleepy)]
Lose ability to walk/communicate
Dependent with all activities
Nursing home likely necessary
Interventions: quality of life training for caregivers, contracture/pressure sore prevention (splinting and positioning), sensory stimulation for comfort and contact with reality (soothing sounds, touch)
![<p>Stage 1</p><ul><li><p>no noticeable impairment</p></li></ul><p>Stage 2</p><ul><li><p>Memory impairment begins to be noticeable</p></li><li><p>might get memory confused with aging</p></li></ul><p>Stage 3</p><ul><li><p>Family members/health care providers notice mild decline with problem solving/remembering names/details</p></li></ul><p><strong>Stage 4 Alzheimer’s Stage I</strong></p><ul><li><p><strong>Obvious difficulty with problem solving/remembering names/details</strong></p></li><li><p><strong>May withdraw from new social situations</strong></p></li><li><p><strong>Interventions: Visual aids, familiarity</strong></p></li></ul><p><strong>Stage 5 [Alzheimer’s Stage II (Bashful)]</strong></p><ul><li><p><strong>Patient will begin to need help with functional ADLs</strong></p></li><li><p><strong>May benefit from adult day care</strong></p></li><li><p><strong>Interventions: simplify tasks in familiar locations, make objects accesible, eliminate environment distractions, goal-directed with visuals and initiation cues (e.g. help select outfit), use personal photos to promote memories and social connection</strong></p></li></ul><p><strong>Stage 6 [Alzheimer’s Stage III (Grumpy)]</strong></p><ul><li><p><strong>Requires assistance with most ADLs</strong></p></li><li><p><strong>Personality begins to change</strong></p></li><li><p><strong>May become delusional/aggressive</strong></p></li><li><p><strong>Not oriented to time</strong></p></li><li><p><strong>Interventions: Caregiver training on routine/behavior management, structured tasks, home mods for safety (Audiovisual systems ~baby monitors, camouflage exits, hide knives), keep them active during the day to reduce night-time wandering</strong></p></li></ul><p>Stage 7 [Alzheimer’s Stage IV (Sleepy)]</p><ul><li><p>Lose ability to walk/communicate</p></li><li><p>Dependent with all activities</p></li><li><p>Nursing home likely necessary</p></li><li><p>Interventions: quality of life training for caregivers, contracture/pressure sore prevention (splinting and positioning), sensory stimulation for comfort and contact with reality (soothing sounds, touch)</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/f6eab04e-8adb-412a-b933-9ba10881981f.jpg)