urinalysis 2
1/86
Earn XP
Description and Tags
hw, etc.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
time and speed for a centrifuge when preparing a urine specimen for microscopic examination?
5 min
2000 RPM
The minimum number of microscopic fields that should be evaluated under low power (10x) are_____________.
10
What type of epithelial cell is most frequently seen in urine sediment? Are they clinically significant?
squamous
no
squamous epithelial cell appearance
large flattened cells
formed elements which are looked for and quantified under low power (10x)
abnormal casts, hyaline cast, normal crystals, squamous epithelial cells, mucus
formed elements which are looked for and semi quantitated under high power (40x)
types of casts (oval fat bodies, hyaline casts, renal tubular epithelial cells), WBCs, RBCs, renal epithelial cells, epithelial cells by type, bacteria/yeast/other parasites, other miscellaneous items
If the specimen color appears red and pink and the clarity of the specimen is hazy or cloudy, look for
RBCs
If the specimen color is white and the clarity is hazy or cloudy, look for
WBCs
If the biochemical test shows a positive nitrate, look for
WBCs and bacteria
If the biochemical test shows positive leukocyte esterase, look for
WBCs, WBC casts, bacteria
If the biochemical test reveals a positive glucose,
look for yeast
If the biochemical test shows a positive protein,
look for casts
A freshly collected urine specimen appears to have pink dust, which settles upon standing, and is cloudy. What is it?
amorphous urate
What pH would support the observation of a freshly collected urine specimen appears to have pink dust, which settles upon standing, and is cloudy. (acidic or basic)?
acidic
microscopic findings would you expect to see in a freshly collected specimen that has:
Cloudy, positive leukocyte estersase, positive nitrite, positive hemoglobin
WBCs, bacteria, WBC casts, RBCs
Cloudy, positive leukocyte estersase, positive nitrite, positive hemoglobin
explain why it’s caused by WBCs, bacteria, WBC casts, RBCs
nitrite result can be due to WBCs and bacteria
hemoglobin result may be due to the presence of RBCs
leukocyte esterase may be due to the WBC, WBC casts, and bacteria.
RBCs may or may not be seen because they could be lysed and not visible for viewing under the microscope.
structures frequently confused with RBCs
yeast, oil, air bubbles, or calcium oxalate crystals.
why a MLS might see bacteria in the microscopic and not have a positive nitrite?
bacteria may be misidentified as an amorphous substance
bacteria may be gram-positive or a bacterium that doesn't convert nitrate to nitrite
patient doesn't eat enough nitrate, then the converted nitrite would not be detectable in the specimen
urine does not spend enough time in the bladder for the bacteria to properly convert nitrate to nitrite.
CSF specimen tube numbers
1- chem
2- micro
3-hematology
4-cytology
xanthochromia caused by
release of hemoglobin from hemolyzed RBCs two hours after a brain hemorrhage (subarachnoid hemorrhage).
xanthochromia looks like
pink with oxyhemoglobin, orange with a combination of colors, and yellow for bilirubin. This color remains even after centrifugation.
how to properly view xanthochromia
the color of the sample should be compared to distilled water with white paper in the background. This specimen should be examined within 1 hour or less to prevent false positives.
conditions where true xanthochromia is present
and why?
The subarachnoid hemorrhage releases hemoglobin from hemolyzed RBC, altering the color of CSF. This process is called erythrophagia.
Jaundice can cause yellow xanthochromia because of the presence of bilirubin in the CSF.
pigment carotene from elevated serum levels,
increased protein concentrations from blood-brain disorders,
melanoma pigment from meningeal melanosarcoma.
three ways to differentiate if blood in a CSF specimen is from a subarachnoid hemorrhage vs. a bloody spinal tap.
centrifuging the specimen,
detecting blood clots in the sample,
detecting how much blood is in the first sample tube compared to the others.
how come centrifuging a specimen helps differentiate subarachnoid hemorrhage vs. a bloody spinal tap?
the supernatant from a traumatic tap appears clear, but the supernatant from a remote hemorrhage/protein is "xanthochromic."
how come detecting blood clots in the sample helps differentiate subarachnoid hemorrhage vs. a bloody spinal tap?
this indicates that the sample is a bloody tap because a CNS hemorrhage does not have clots.
how come detecting how much blood is in the first sample tube compared to the others helps differentiate subarachnoid hemorrhage vs. a bloody spinal tap?
With the traumatic tap, the maximum amount of blood in the first sample tube progressively decreases as the sample tubes fill up.
With a CNS hemorrhage, the blood is consistently mixed in all the collection tubes.
expected glucose value for bacterial meningitis
decreased
viral meningitis glucose level
N
MS glucose level
N
subarachnoid hemorrhage glucose
D
neoplasm/tumor glucose
D
bacterial meningitis protein
I
viral meningitis protein
I
MS protein
N/sl I
neoplasm/tumor protein
I
subarachnoid hemorrhage protein
I
severe head trauma protein
D
How can synovial fluid be differentiated from other fluid types?
The high molecular weight mucopolysaccharide hyaluronic acid or hyaluronate
functions with a specific viscosity to lubricate the joints.
inflammatory vs infectious (fill out on mon)
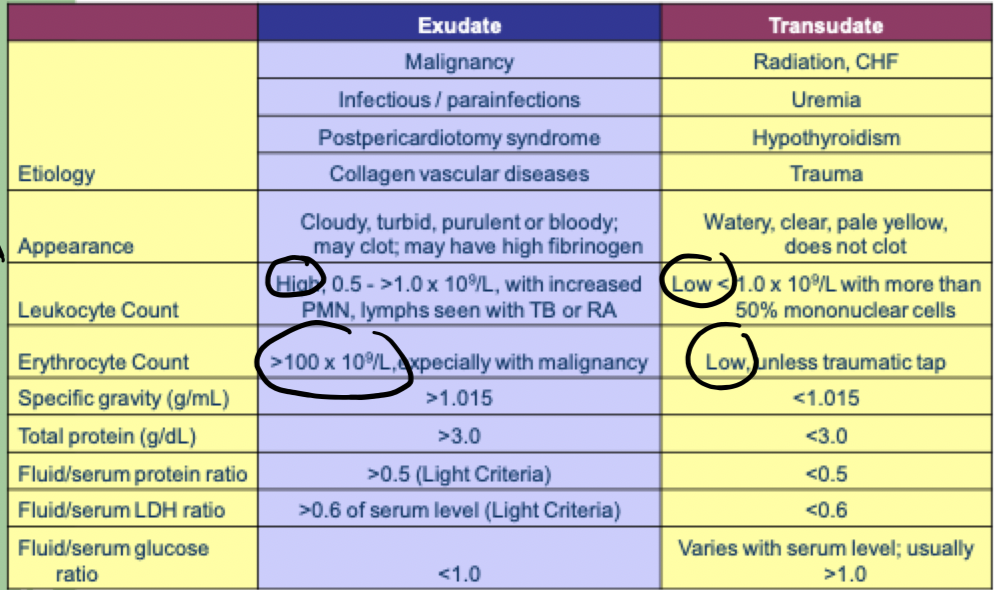
A pericardial fluid that is clear and pale yellow which has a protein value of 2.5 g/dl and a specific gravity of 1.010 is probably due to which of the following conditions?
CHF
Analysis of a seminal fluid specimen - a tech diluted 20 uL of semen with 180 uL of diluent. She observed 100 sperm on each side, using the 5 RBC squares in the center square on an Improved Neubauer hemacytometer.
dilution?
sperm count / uL
sperm count /mL
1/10
50,000
50,000,000
At what value(s) are the baby’s lungs considered mature for L/S
>3.0
At what value(s) are the baby’s lungs considered mature for L/S - safe to deliver
>2.0
At what value(s) are the baby’s lungs considered mature for phosphatidyl glycerol
>0.3
At what value(s) are the baby’s lungs considered mature for foam stability
>0.48
At what value(s) are the baby’s lungs considered mature for lamellar body count
50,000/uL
purpose of delta A450 test
assesses hemolytic disease of the newborn by measuring bilirubin concentration (the breakdown product of hemolyzed RBCs) in amniotic fluid.
During normal RBC destruction in the fetus, unconjugated bilirubin is made and rapidly removed into maternal circulation by the placenta, but with HDN, the destroyed RBCs enter the amniotic fluid. The level of bilirubin present in amniotic fluid directly correlates to the severity of hemolysis.
substances that interfere with delta A450 test
blood contamination, meconium contamination, and any exposure to light
transudates vs exudates
infectious vs inflammatory fluid pathological
infectious: bacterial infection S. aureus and N. gonorrhoeae, Haemophilus, mycobacterium, fungi, anaerobic bacteria
inflammatory: immunological diseases RA, lupus
infectious vs inflammatory fluid appearance
infectious: cloudy, low viscosity, yellow, green, milky
inflammatory: cloudy, yellow, low viscosity
infectious vs inflammatory fluid WBC count
infectious: >50 × 10^9/L
inflammatory: 3-50 × 10^9/L
infectious gluose and neutrophil
low glucose content
>90% neutrophils
acute glomerulonephritis caused by
renal glomeruli damage, triggering inflammation and proliferation of glomerular tissue-damage to the basement membrane
(but tubular function is normal)
acute glomerulonephritis symptoms
RBC casts, Na and H2O retention, elevated BUN/creatinine, losing blood in urine anemia, decreased GFR, hematuria and proteinuria, glomerular lesions
acute glomerulonephritis related to what infection
recent strep infection
chronic glomerulonephritis
>6 months, lengthy inflammation with scarring and loss of functioning nephrons
chronic glomerulonephritis symptoms
slight decrease in renal function and proteinuria and hematuria at first, gradual development of uremia, azotemia (nitrogenous waste)
nephrotic syndrome cause
glomerular basement membrane injury and increased permeability
nephrotic syndrome symptoms
massive proteinuria
hypoalbuminemia
hyperlipidemia
lipiduria (losing proteins transporting lipids) OVAL FAT BODIES
cystinosis can lead to what?
fanconi syndrome
fanconi syndrome causes
heavy metal poisoning, cystinosis (hereditary)
fanconi syndrome results
aminoaciduria, proteinuria, glycosuria, phosphaturia
tubular diseases or defects include what?
renal tubular acidosis type I (distal tubules), II (proximal tubules), acute tubular inflammation
where do tubular diseases/defects happen?
in most renal diseases after the glomerular filtration rate declines. the ability to excrete/reabsorb substances decreases
what causes renal tubular acidosis?
kidneys can’t excrete enough acid
T/F renal tubular acidosis is the most clinically significant tubular disease
true
what happens during renal tubular acidosis type I: distal tubules?
decreased H+ secretion into distal tubules
H+ are retained and K is excreted instead
how to diagnose renal tubular acidosis type I: distal tubules
urine pH >5.3
usually the pH is lower to eliminate acid
what happens during renal tubular acidosis type II: proximal tubules?
proximal tubules can’t reabsorb bicarbonate (the base for the body), bicarb gets excreted in the urine
the patient excretes excessive bicarb ion and gets hyperchloremic acidosis, chloride is retained and elevated levels are in the plasma
SYMPTOMS of renal tubular acidosis type I: distal tubules
low serum phosphate and uric acid
glucose and amino acids in the urine
<2g protein/day in urine
urine pH isn’t low enough
acute tubular inflammation caused by
bacterial-viral-fungal infection, pain-relief drug toxicity, radiation toxicity, methicillin hypersensitivity, and renal transplant rejection
acute tubular inflammation symptoms
decreased GFR, decreased ability to concentrate urine (low SG), excreted acid in urine, WBC casts, problems with sodium balance
mechanism of acute renal failure
direct damage to renal tubules causes sudden, sharp decline in renal function over hours/days
toxic/hypotoxic occurrence in the kidney
acute renal failure symptoms
oliguria, anuria (<200mL), increased BUN and creatinine, metabolic acidosis, decreased ability to excrete electrolytes and water (edema), GFR <10mL/min
pre-renal failure problem
blood flow/supply problem
CHF, cardiovascular system failure, hypovolemia
renal failure problem
acute tubular necrosis, vascular obstruction, inflammation, glomerulonephritis
post-renal problem
urinary tract post-kidney
lower urinary tract obstruction
blasser rupture
what causes chronic renal failure?
chronic kidney disease,
increased with: diabetes, obesity, aging, metabolic syndrome, diabetic nephropathy
what causes diabetic nephropathy
glomerular problems: diabetic urine is hyperosmolar (glucosuria, ketosuria, polyuria, nocturia)
increased basement membrane permeability exacerbating renal damage
chronic insufficiency/nephrotic syndrome
end-stage renal disease caused by
kidney failure to function usually after chronic kidney disease (up to 20 yrs before)
<10% kidney function, needing dialysis/kidney transplant
ESRD symptoms
low urine volume, increased BUN to 70-80 mg/dL
creatinine increased to 7 mg/dL
eGFR <15
what does this cause?
renal hypertension
2 UTI infections
pyelonephritis and acute cystitis
pyelonephritis caused by
infections in the kidney
WBCs are diagnostic for it!
acute cystitis caused by
infection in the urinary bladder