unit 5 - skeletal muscle
1/46
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
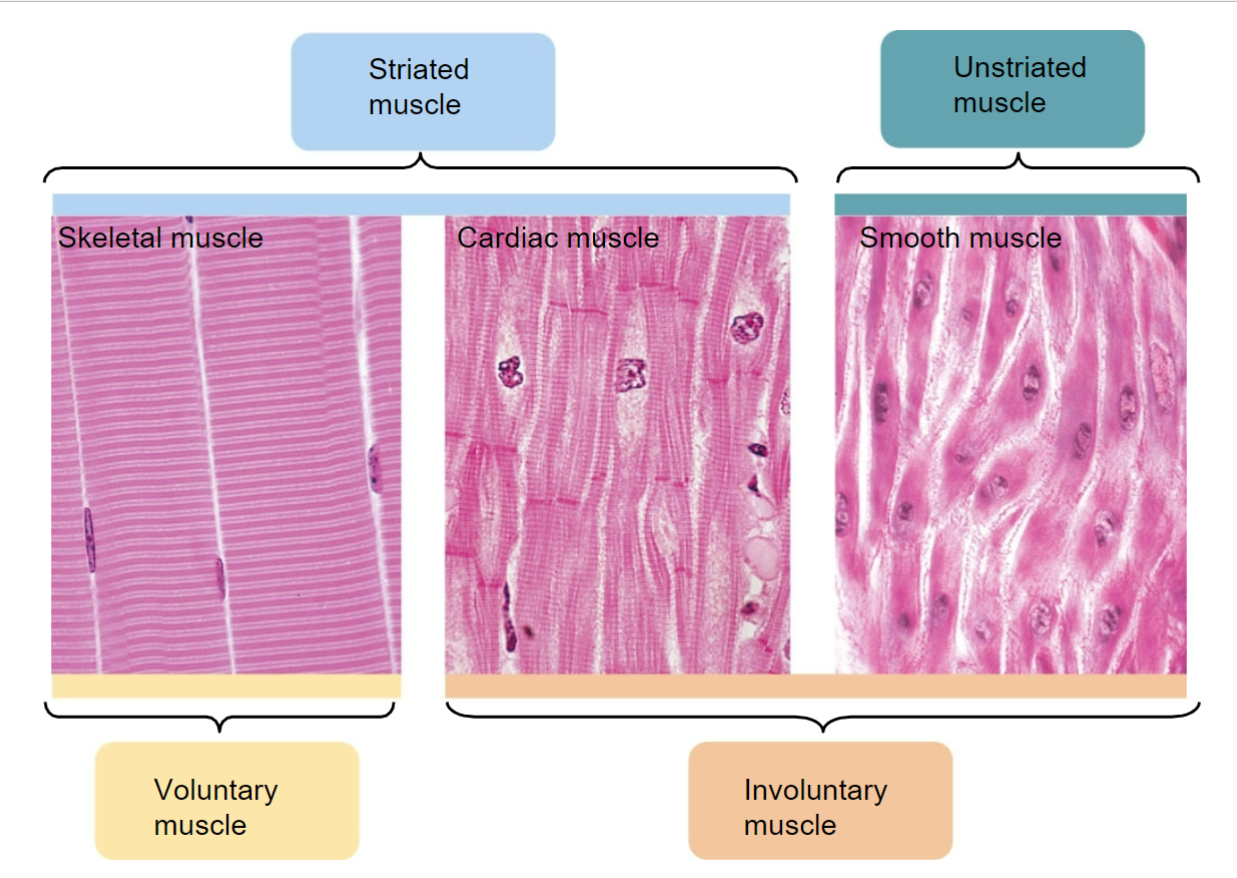
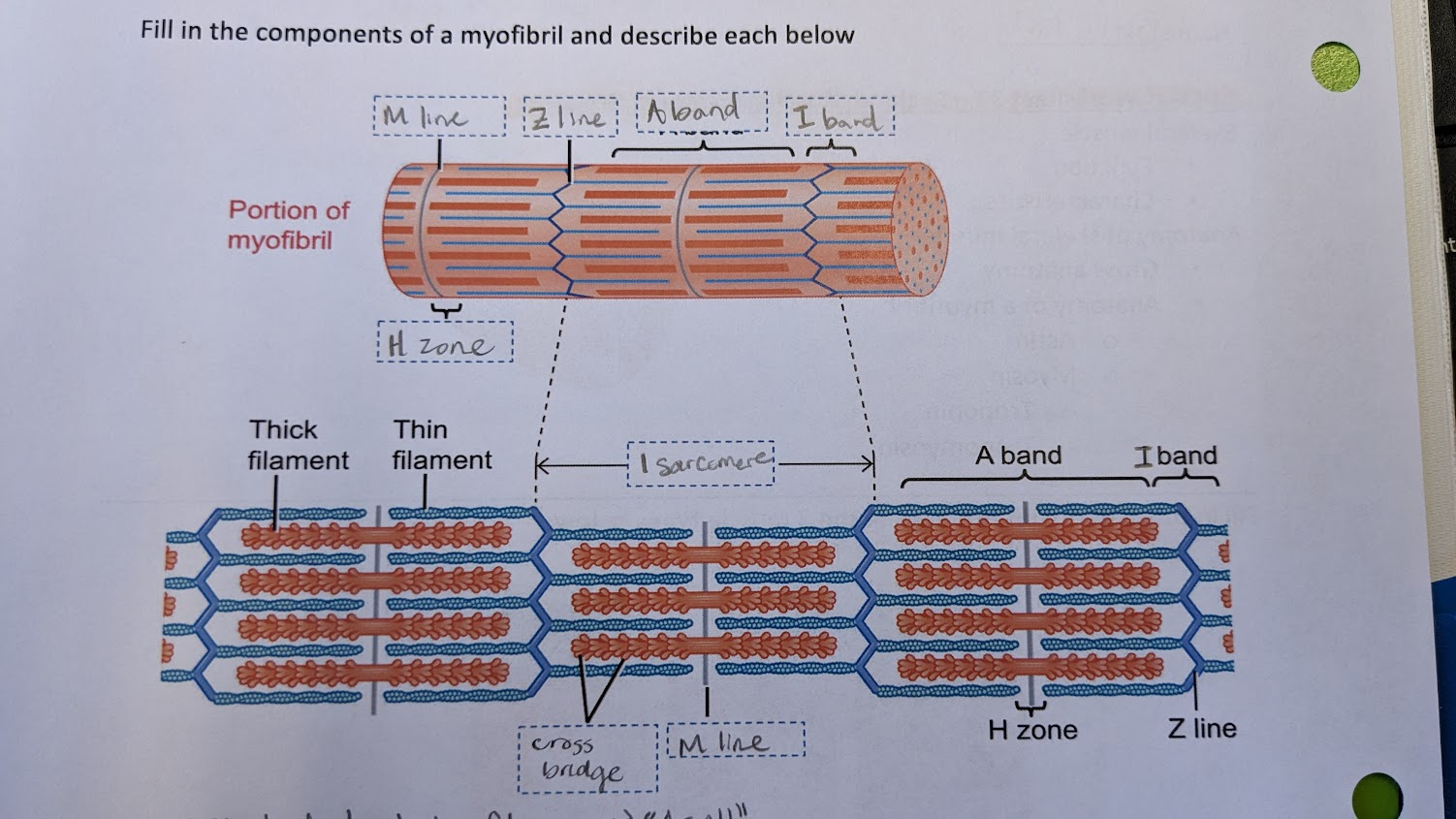
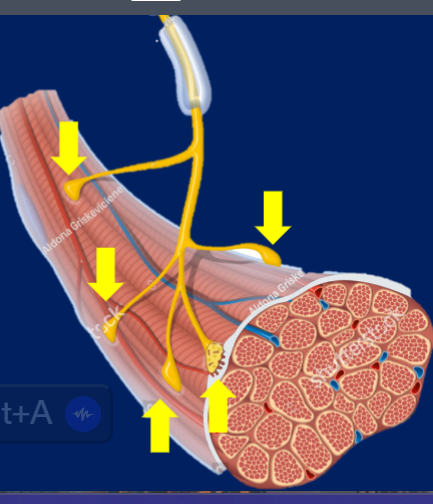
muscle picture diagram
(striated means there are light and dark lines alternating)
functions of skeletal muscle
-body movement
-maintain posture
-protect and support
-regulate elimination of materials
-heat production/maintain body temp
5 characteristics of skeletal muscle
1) excitability - respond to stimulus by change membrane potential
2) conductivity - send charge down cell
3) contractility
4) extensibility
5) elasticity - can return to normal shape after change
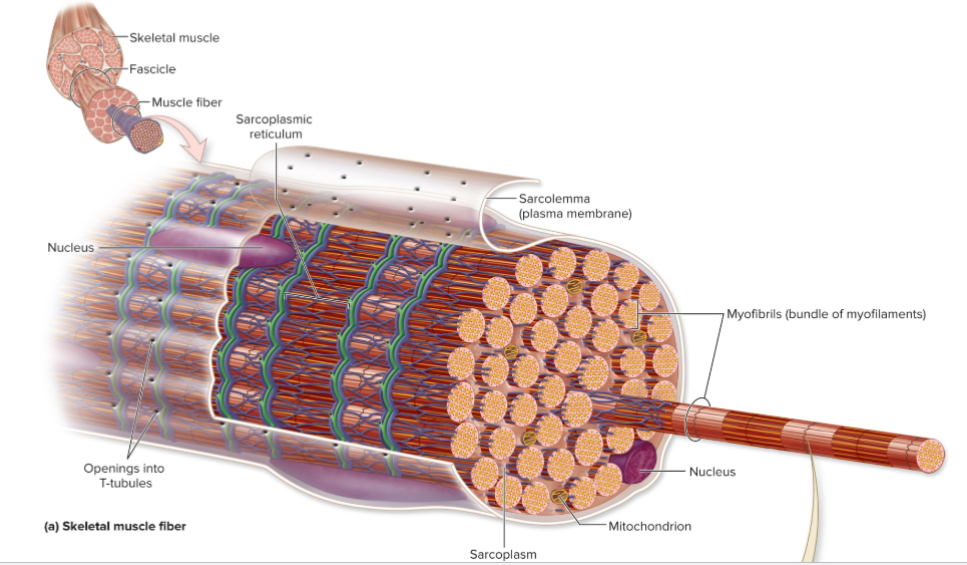
anatomy of skeletal muscle
-muscle cell is called muscle fiber
-SM consists of many fibers in parallel held by CT
-large, elongated, cylinder shaped
-fibers run length of muscle
-multinucliated - many nuclei in 1 cell
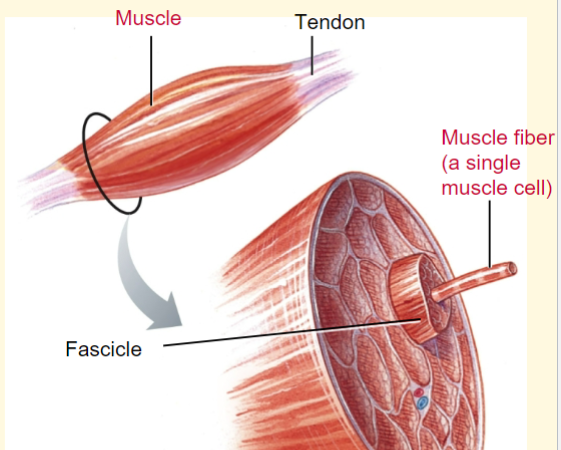
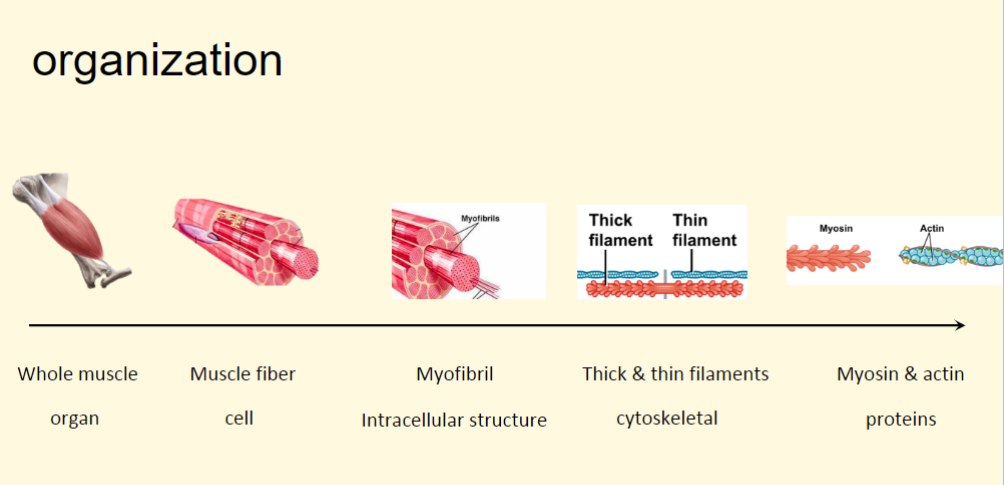
skeletal muscle organization overview
know fascicle, muscle fiber, myofibril
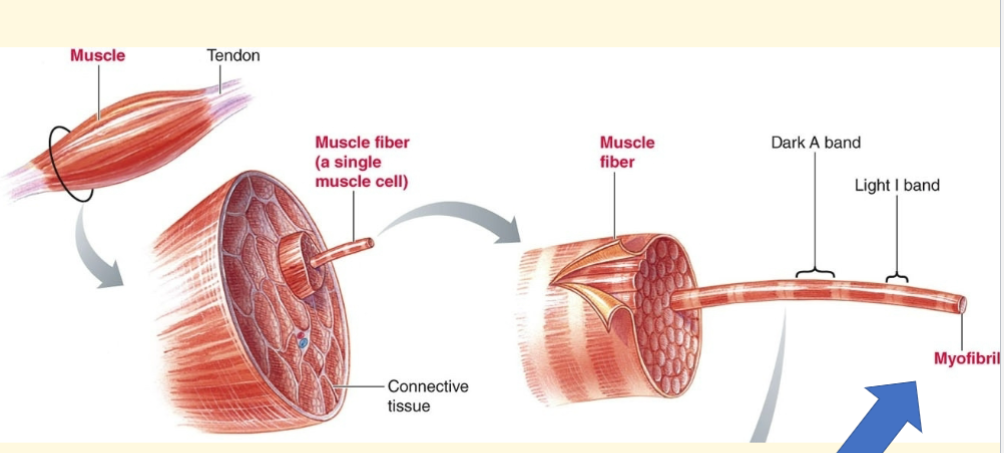
skeletal muscle fiber and fascicle
-many fibers into 1 fascicle
3 layers of muscle wrapping
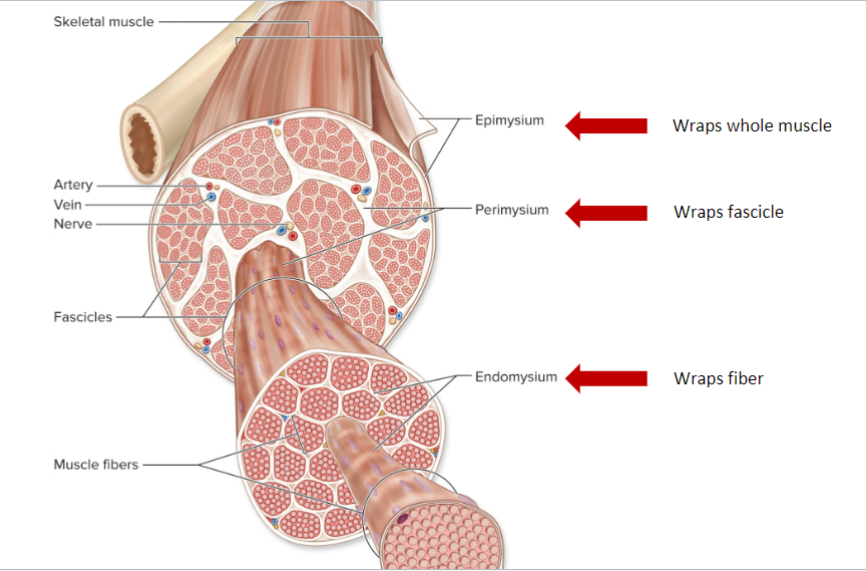
skeletal muscle - BV and nerves
-SM is vascularized → deliver O2 and nutrients, remove waste products
-SM is innervated by somatic neurons → allow voluntary control (where we release ACh)
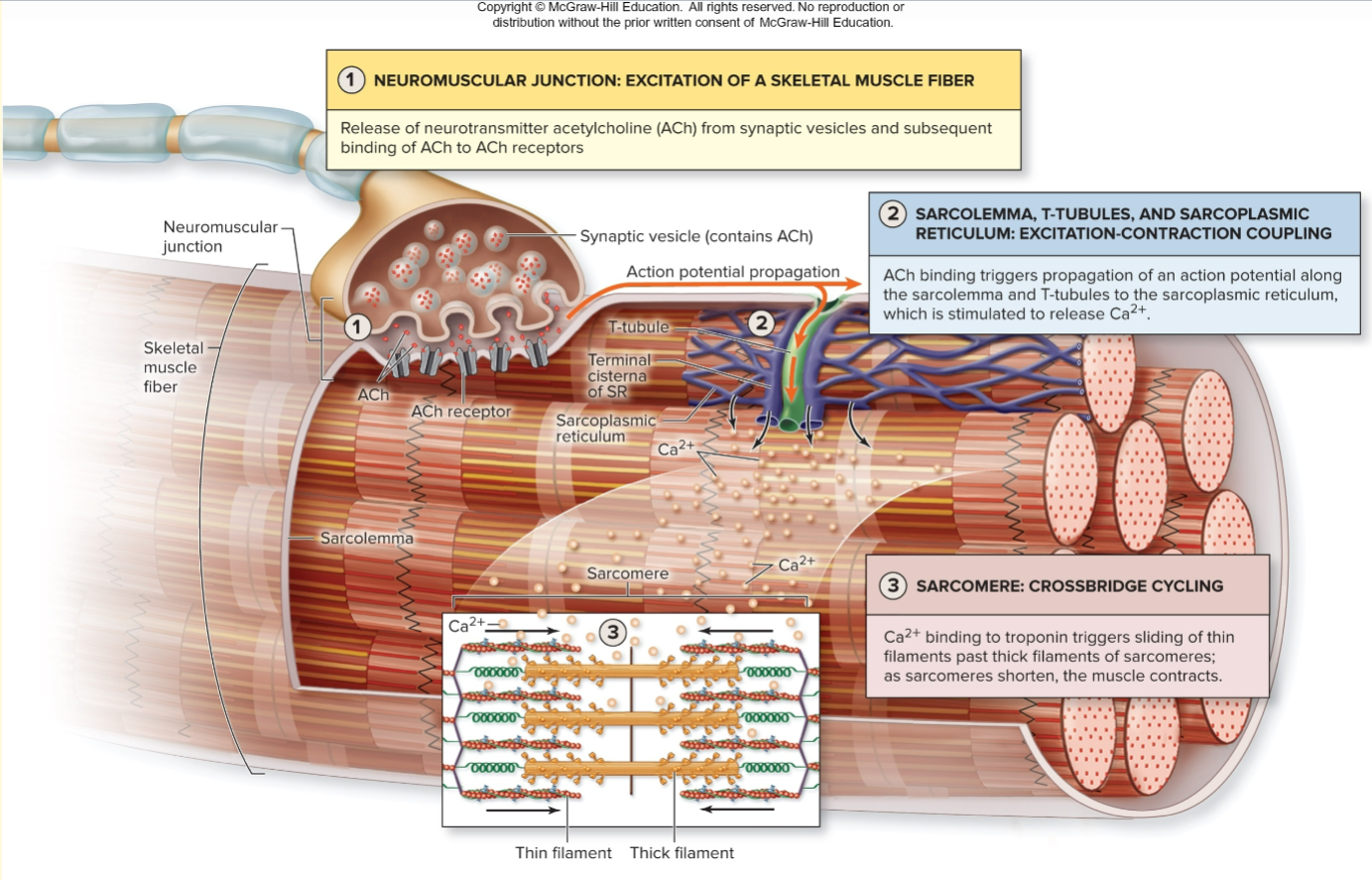
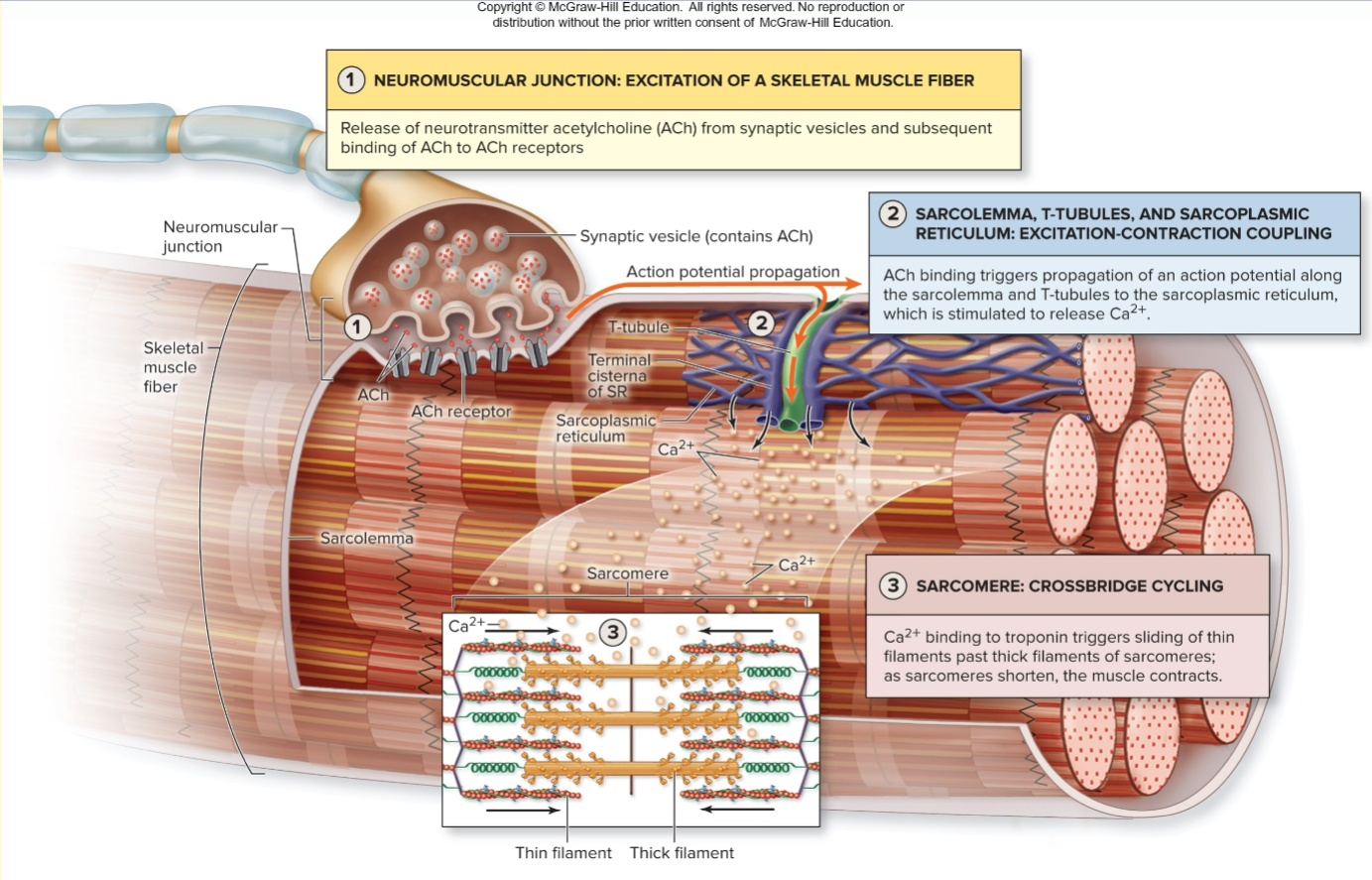
skeletal muscle depolarization overview (image)
inside one 1 fiber image
-sarcolemma = outside membrane of fiber → holes go into T-tubules
-T-tubules = shown as the teal lines
-sarcoplasmic reticulum = shown as blue net. stores Ca.
**when you get an AP, it flows along the sarcolemma until it goes into one of the holes into the T-tubules → lead to depolarization, Ca release, muscle contraction
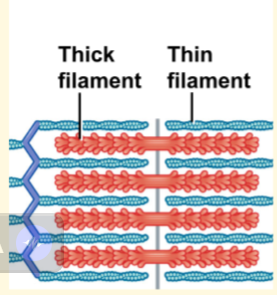
thick and thin filaments
-contractile proteins
-inside each myofibril
-thick = myosin. thin = actin
-together form “contractile unit” = sarcomere
SM organization overview (image)
sarcomere
-contractile unit
-made of thick and thin proteins
*image shows 3 sarcomeres
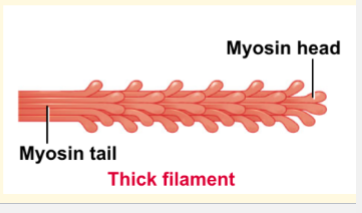
myosin
-component of thick filament
-globular head grabs onto actin in thin filaments → form cross-bridge
2 sites - actin-binding site, and myosin ATPase site (split ATP)
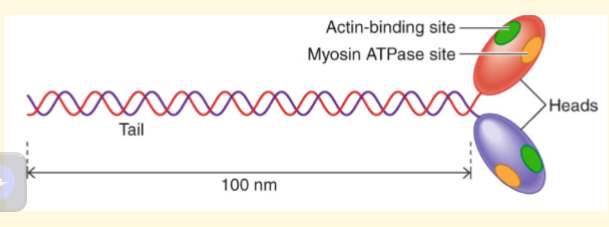
thin filament - actin, tropomyosin, troponin
-actin = component of thin filaments, binds myosin
tropomyosin = rope covering binding site
troponin = has 3 units, one binds to Ca, which moves tropomyosin and allows myosin to bind to actin → allows muscle contraction
A band
-stacked thick & thin filaments
-thick filaments can only be found in A band → appears dark
-A band defined by each end of a thick filament
”A = all”
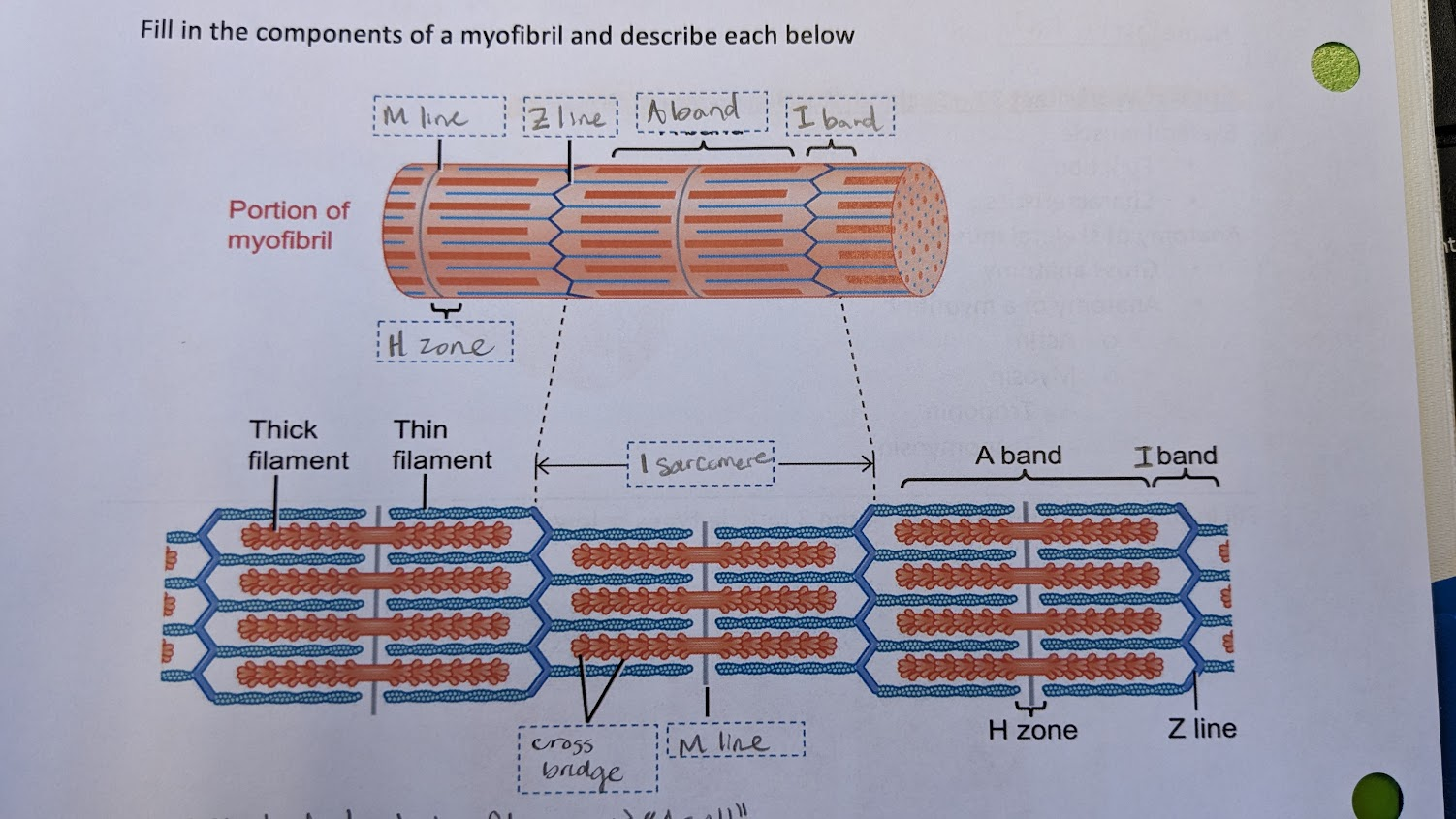
H zone
-area with thick filament only, has no thin fil.
”H = heavy”
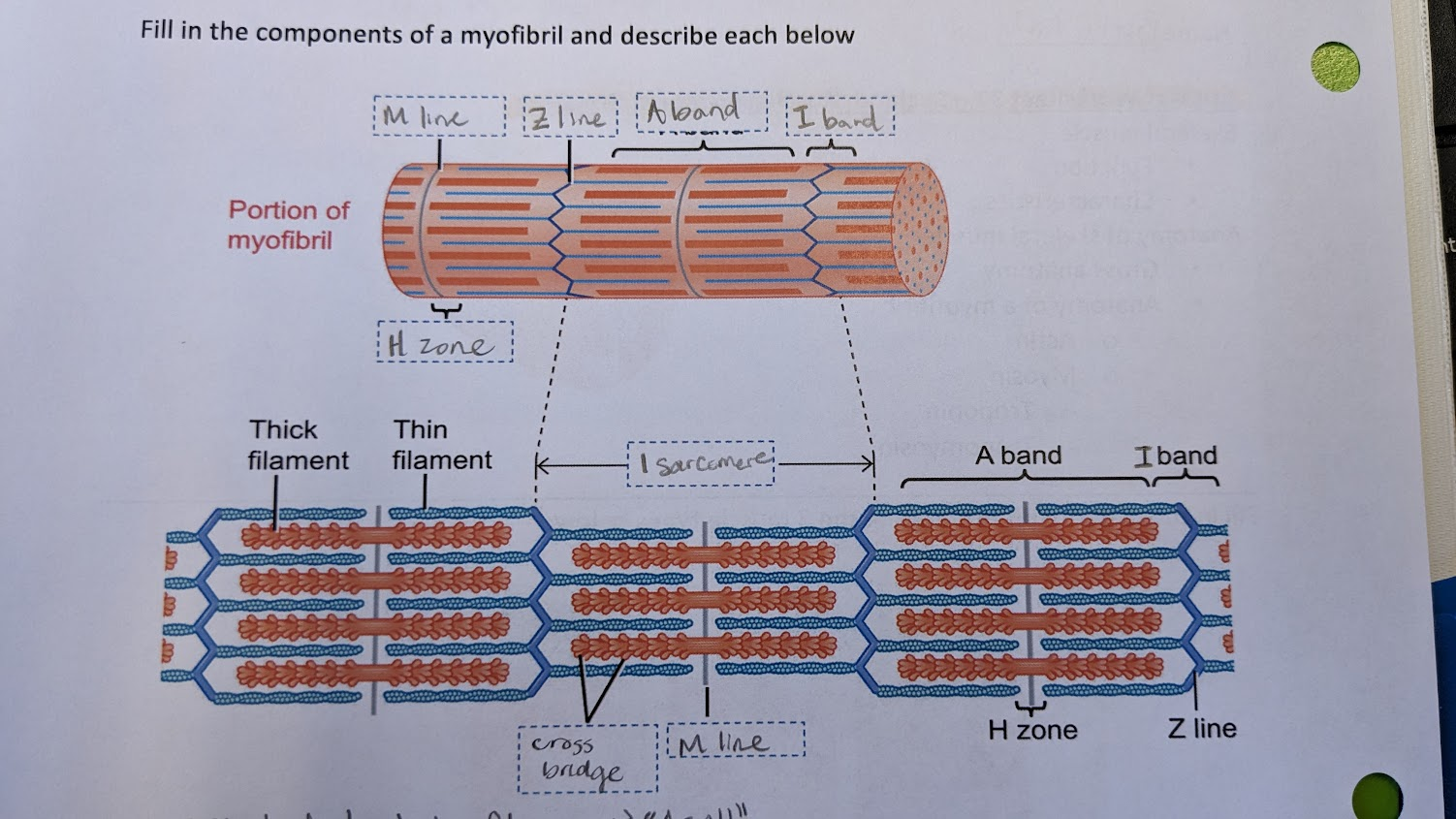
M line
-protein strand holds thick fil. together
-protein in a vertical line
“M = middle” since it’s in the middle of the sarcomere
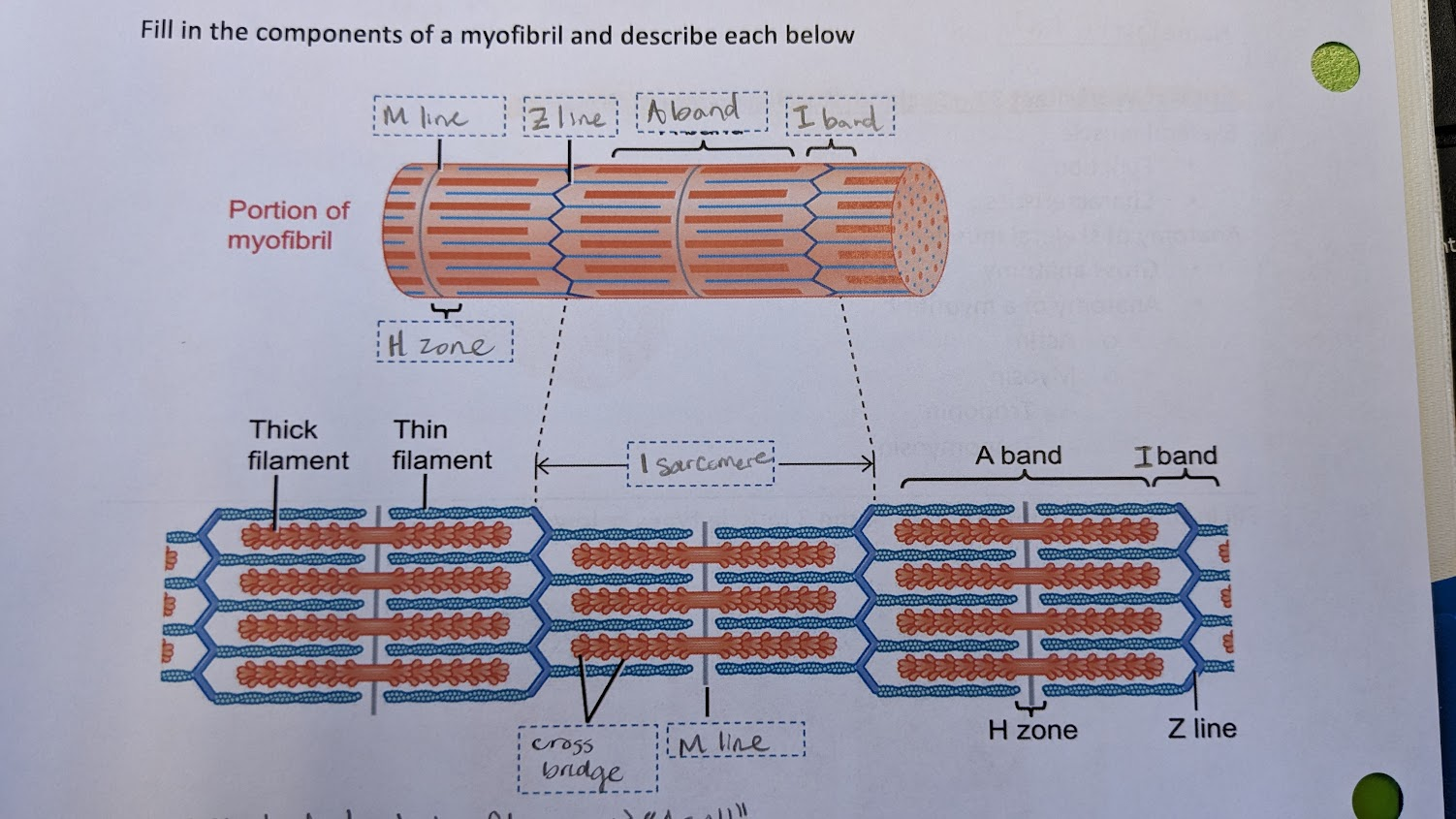
i band
-part of thin fil. sticking out of A band on either side
“thin”
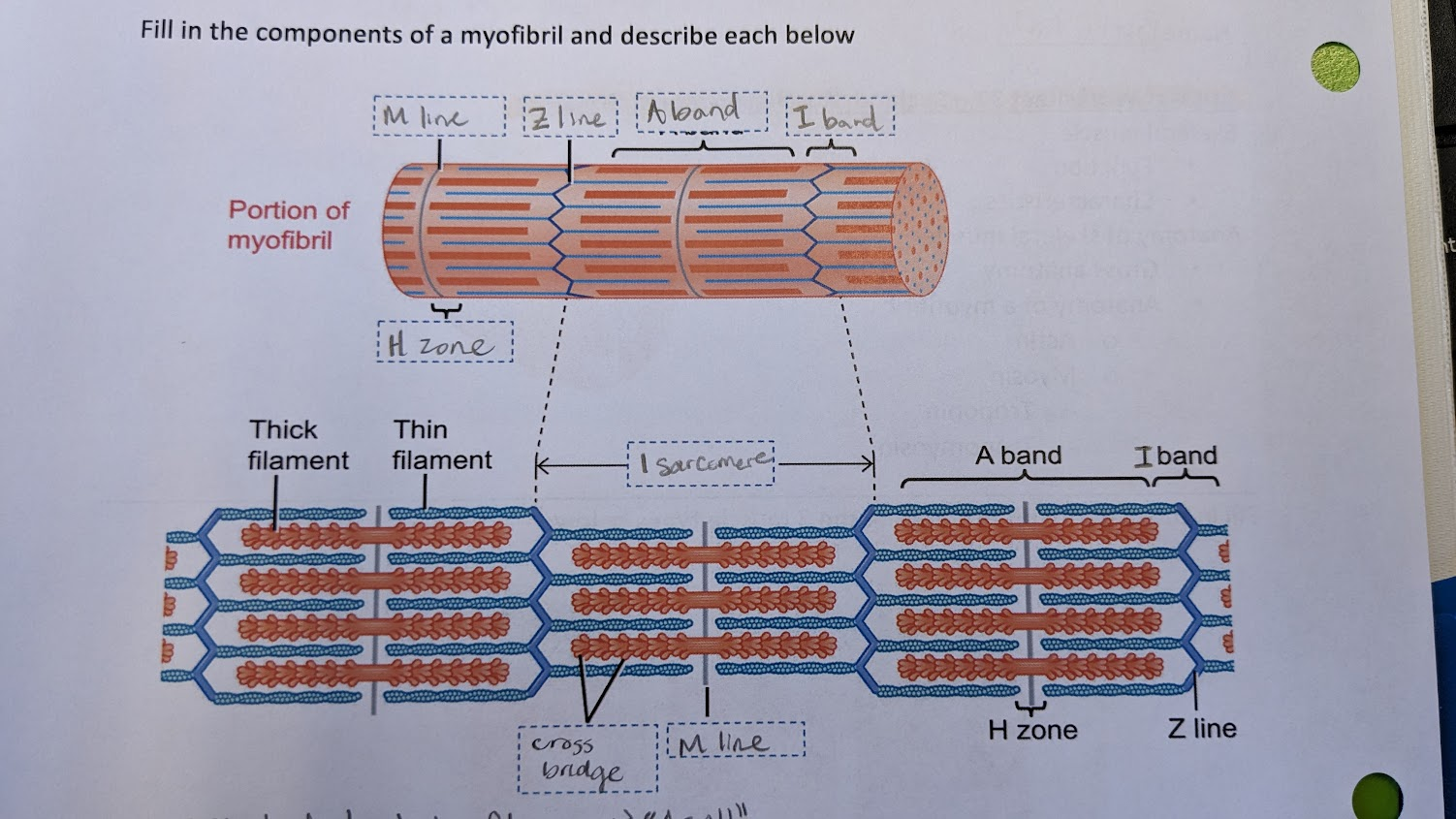
Z line
-middle of i band
-Z line to Z line defines sarcomere
Z shaped
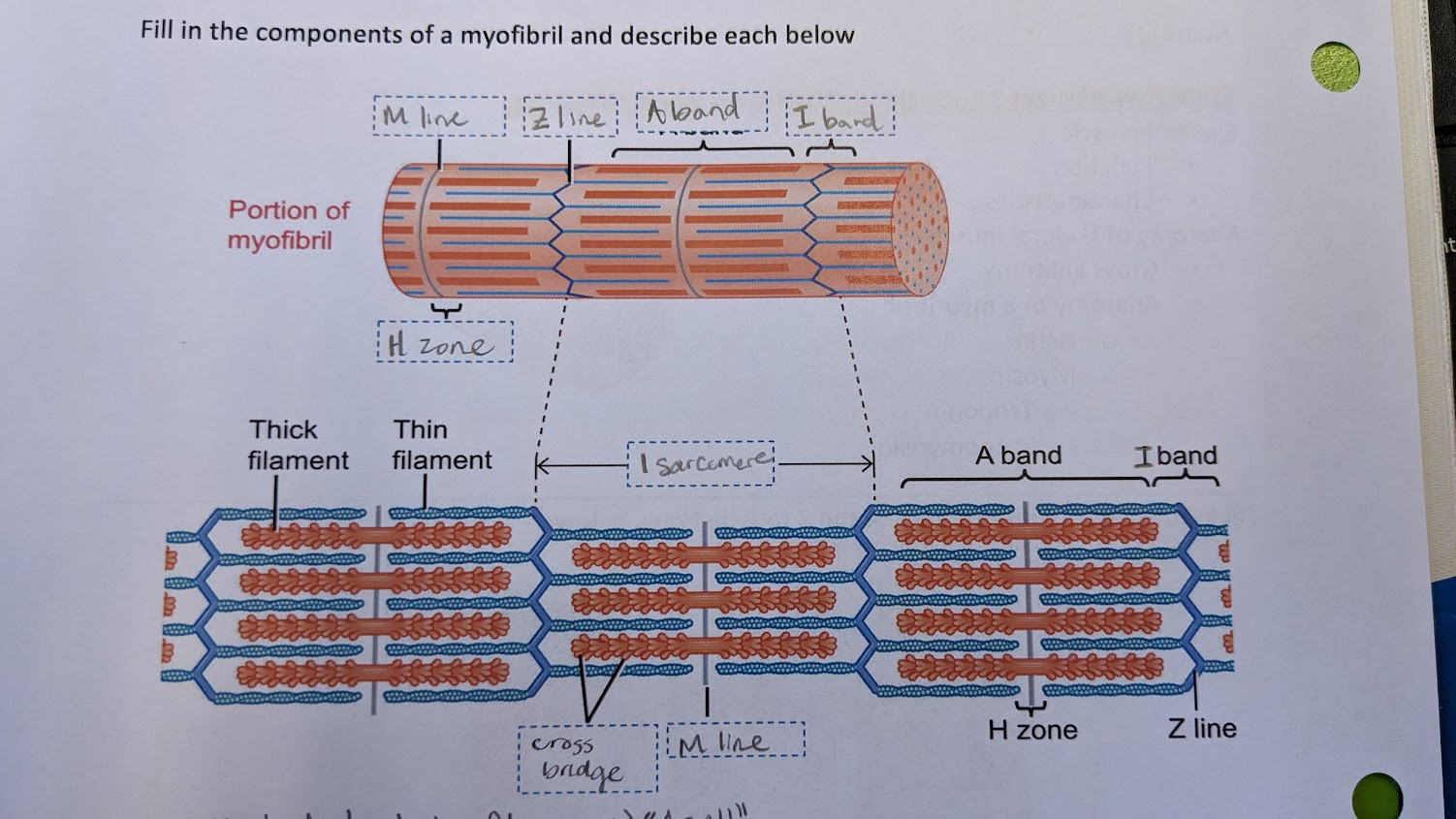
cross bridges
-formed by myosin heads grabbing onto thin filaments
-fils. become ‘connected’ when muscle contracts
-this only happens during AP → when troponin binds to Ca and moves tropomyosin out of the way → allows myosin to bind to actin
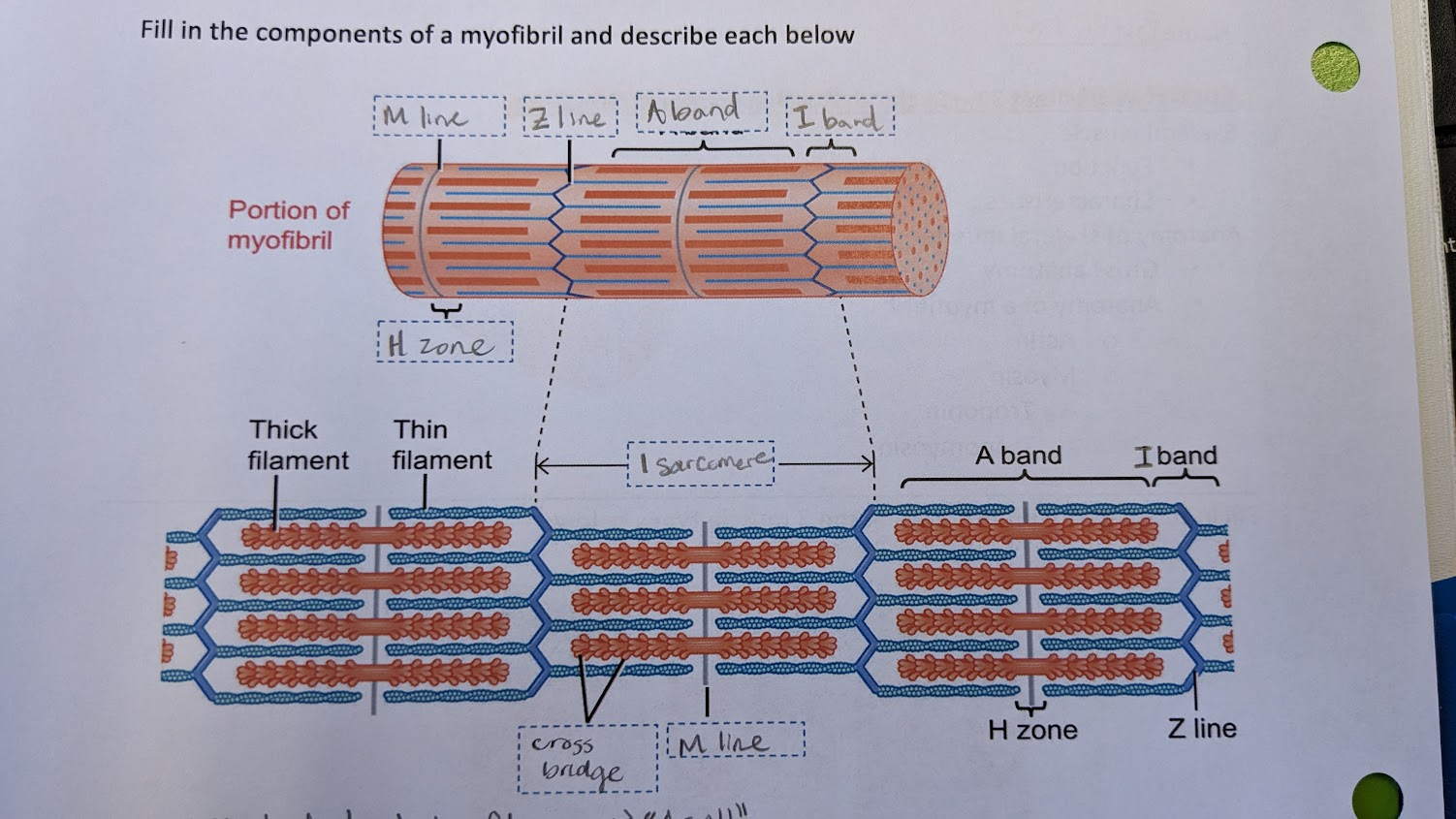
how do the sarcomere subunits change during a muscle contraction?
-filaments do not change length
-A band stays the same, i band gets shorter
-filaments slide over each other to contract sarcomere
-H zone also shorter
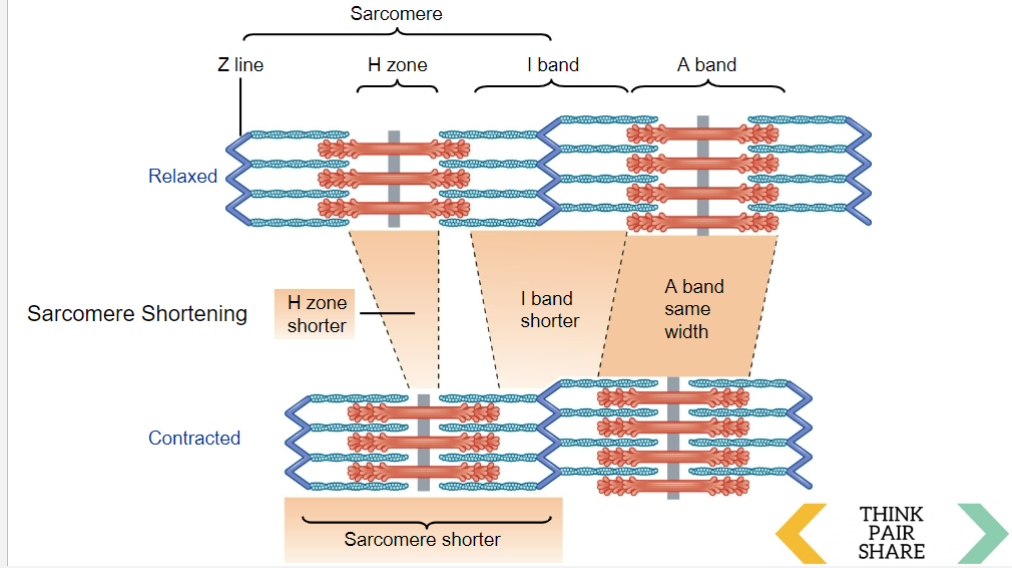
power stroke - myosin & actin binding (image)
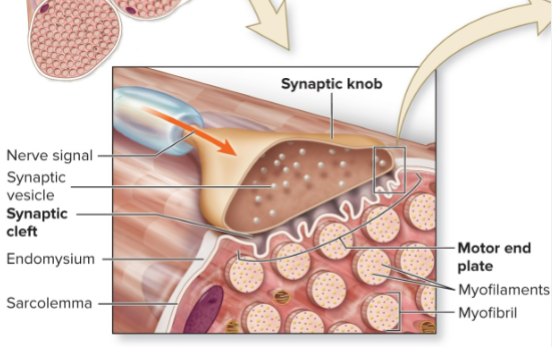
neuromuscular junction (NMJ)
the location (mid-region) where fiber innervated by motor neuron
-only one per muscle fiber. each dendrite goes to diff muscle fiber
-one motor neuron can innervate many muscle cells
components of NMJ
-junctional folds = area below cleft is ruffled → more SA for more receptors
-nAChR = nicotinic receptors on the junctional fold (cation channel)
-VGC Na+ → for EPSPs
how to stop muscle activation
1 - stop release of ACh (ACh only released during AP’s. no AP = no ACh)
3 - acetylcholinesterase breaks down Ach into Choline + acetate
excitation contraction coupling (ECC)
link skeletal muscle AP to physical muscle contraction
1) AP arrives, VGC Ca channels open and allow for ACh exocytosis
2) binds to nAChR. this opens a chem gated channel for Na
3) Na depolarizes, opens VGC Na. more Na rush in, AP
4) AP travels down T-tubule
5) conformational change. activates DHPR receptor to bind with RyR receptor on sarcoplasmic reticulum
6) Sarcoplasmic reticulum releases Ca
7) Ca goes to thin filament, binds to tropomyosin to reveal actin binding site. Thick & thin bind = muscle shortens
8) SERCA pump recycles Ca, puts back in sarcoplasmic retic
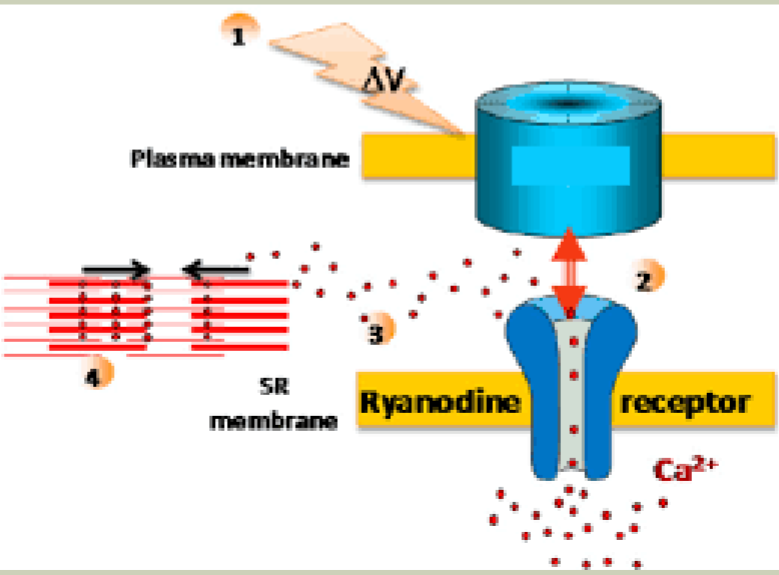
RyR and DHPR receptors
Ryaninodine binds to RyR receptors (DHPR)
→ conformational change of protein, trigger Ca release from SR as AP travels down T-Tubles
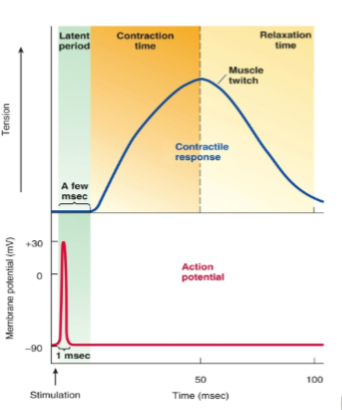
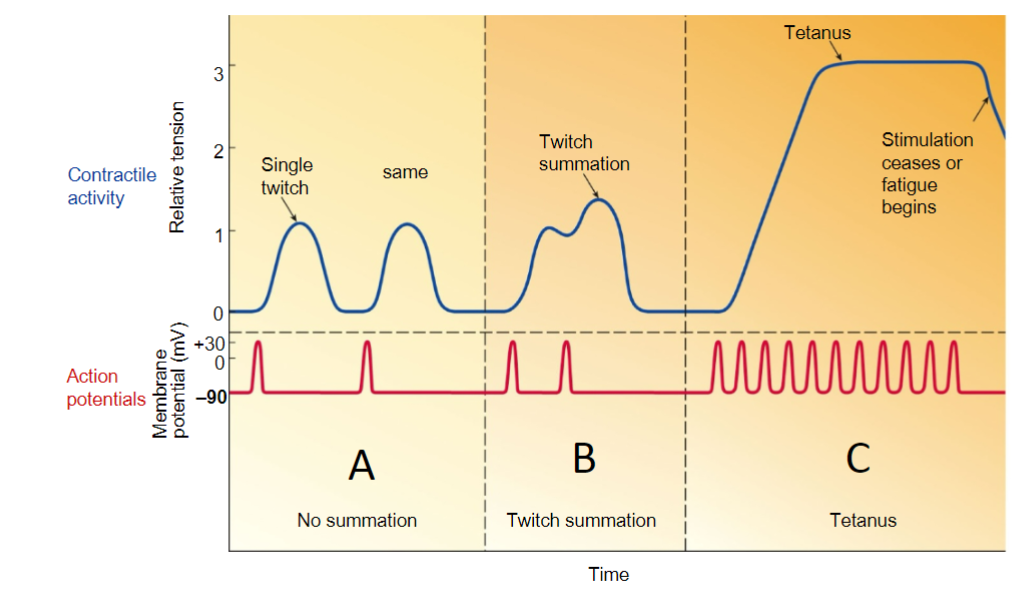
different periods of a muscle twitch.
latent period, contraction time, relaxation time
latent period = where ECC takes place
contraction time = form cross bridge. Ca binds to troponin
relaxation time = when cross bridge stops. Ca unbinds
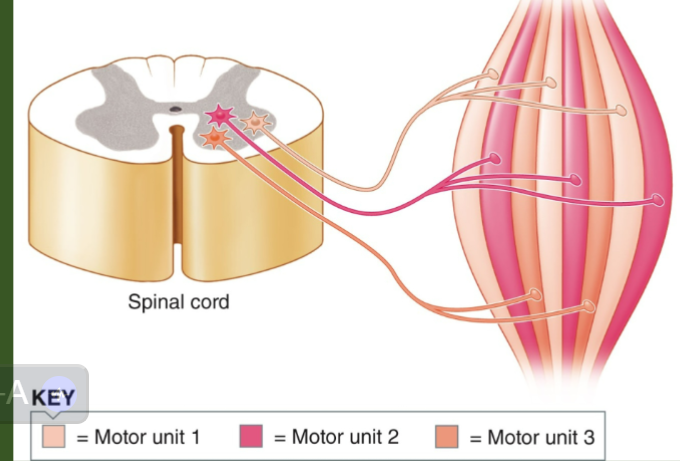
motor unit
a motor neuron and ALL the muscle fibers that it controls
-they are spread out thru a muscle, not all in one area (shown in pic)
-depending on force, you can activate 1 fiber to all fibers
-more fibers = larger muscle = more muscle tension/power, but less precise control
-less fibers = more fine control, but less force
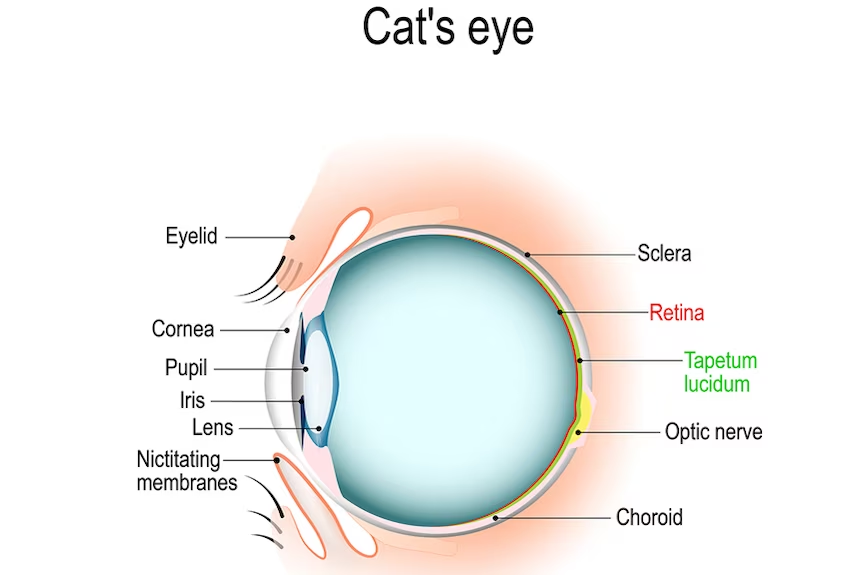
tapetum lucidum in walleye - extra credit question
a layer in the back of the eye that reflects light back so more can be absorbed → allows for high acuity in the dark, but blurry image
-eye looks like a mirror when you shine light on it
(picture is cat’s eye but walleye is the same)
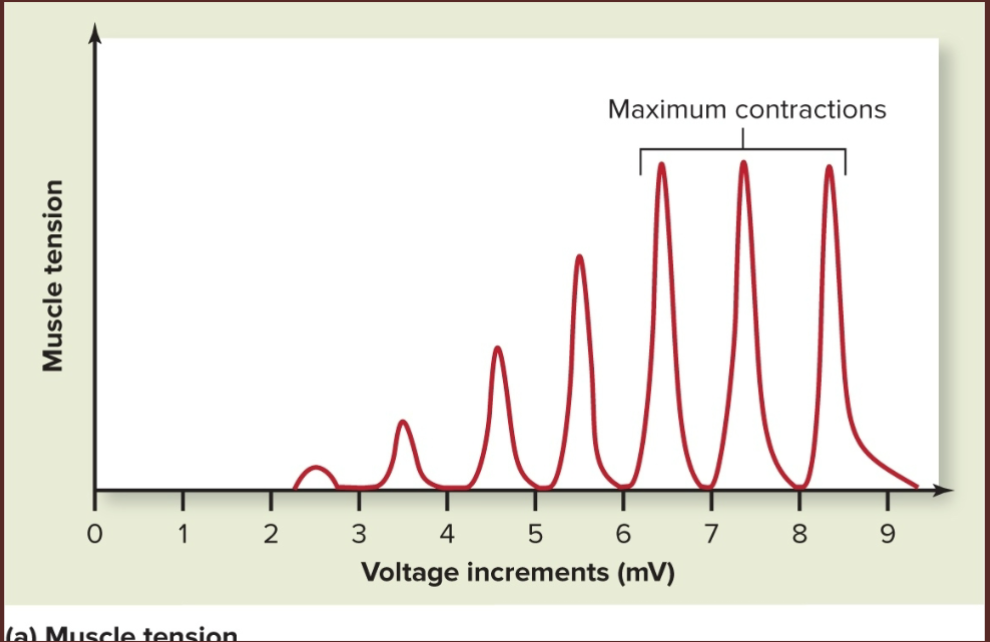
muscle tension
the force generated when a muscle is stimulated to contract
-tension is produced within sarcomeres
-must be transmitted to bone via CT & tendons before bone can be moved → CT/tendons = series-elastic component
muscle twitch characteristics
-brief, weak contraction
-produced by one single AP
-too short and weak to be powerful
**but muscle tension depends on many muscle fibers contracting, not just one twitch
→ increase muscle tension = recruit more fibers to contract
muscle tension maximum contraction
-as voltage increases, more motor units are recruited to generate more contractile force
-smaller, slow-oxidative units recruited first, larger, fast glycolytic units recruited last
-eventually all motor units recruited, so muscles can’t contract any more = maximum contraction
asynchronous recruitment
-motor units alternate which ones are contracting to prevent fatigue
-cannot occur if max contraction since there will be no left over units
muscle twitch summation, and tetanus/tetany diagram
*this type of tetanus is good because it allows us to have sustained muscle contraction, is VOLUNTARY. it is not referring to the tetanus toxin from bacteria
→ in this way tetanus/tetany is just referring to a sustained contraction
why might muscle fatigue happen?
muscle fatigue = when muscle can no longer contract the same level as it used to
-main cause: glycogen stores depleted
-also caused by decreased Ca and decreased synaptic vesicles
muscle tone
muscle tone = resting tension in a muscle
-muscles always a little bit contracted → to stabilize positions of bone and joints (ex. posture muscles in back)
-involuntary skeletal muscle contraction → from nervous system stimulation
-decreased during sleep
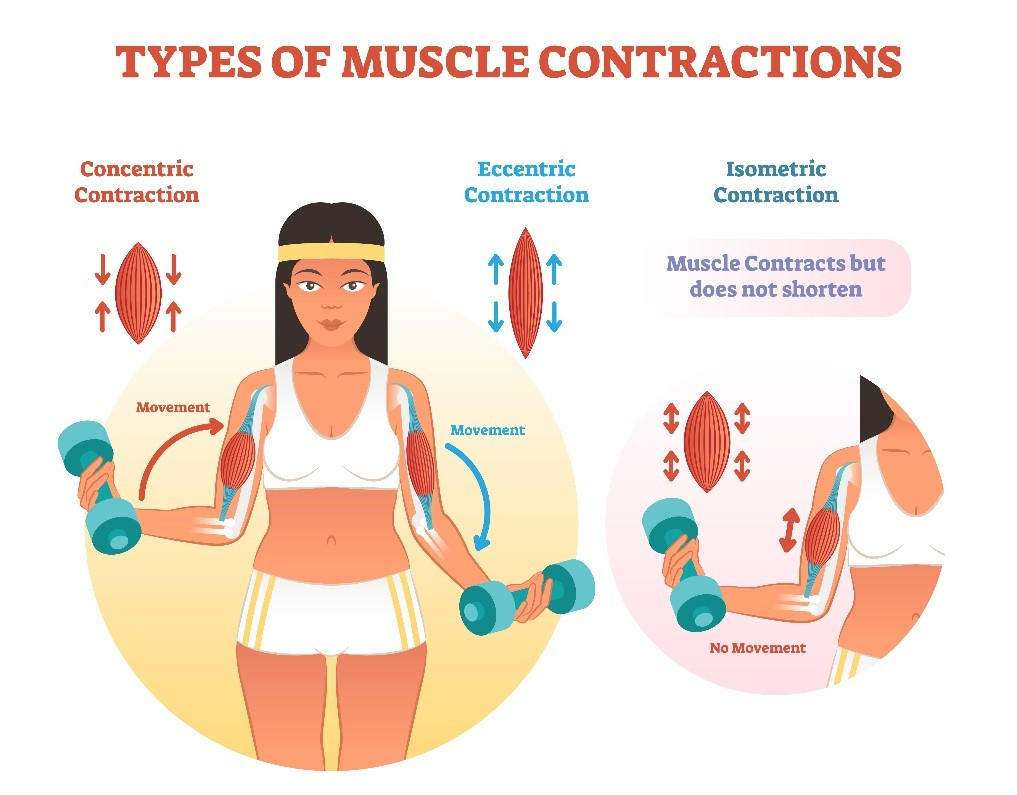
isotonic contraction
“same tone” → tension is constant, but muscle changes length
-2 types:
→ concentric = shorten muscle
→ eccentric = lengthen muscle
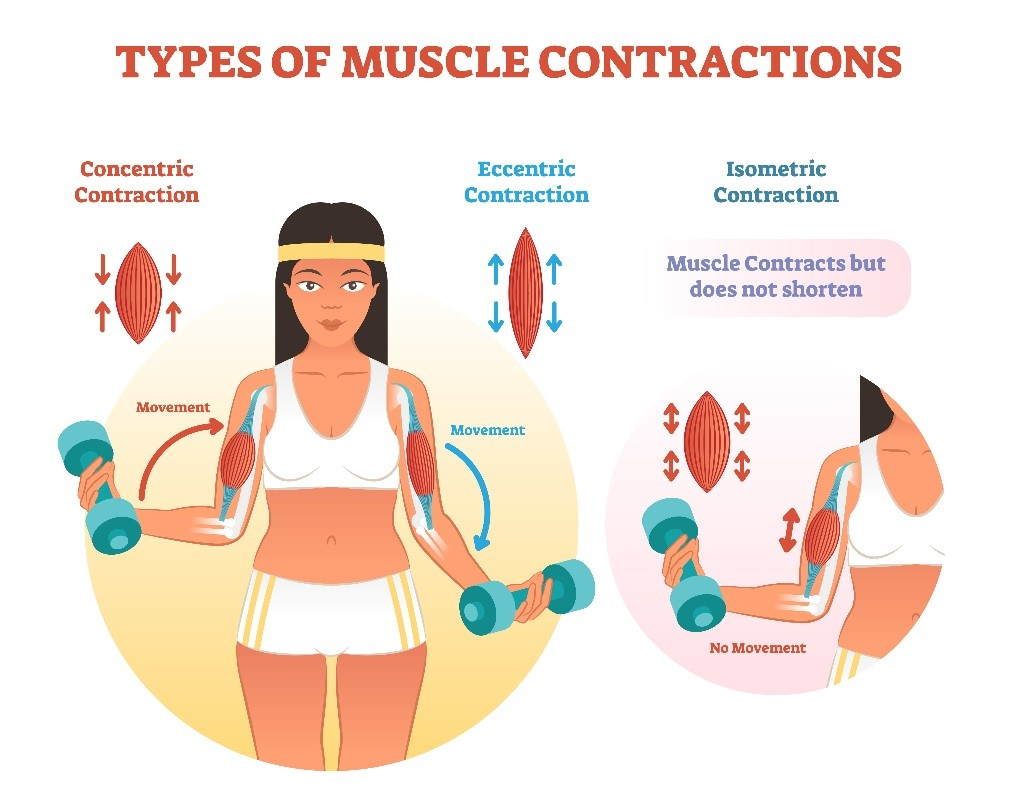
isometric contraction
“same length” → muscle does not change length, but tension changes
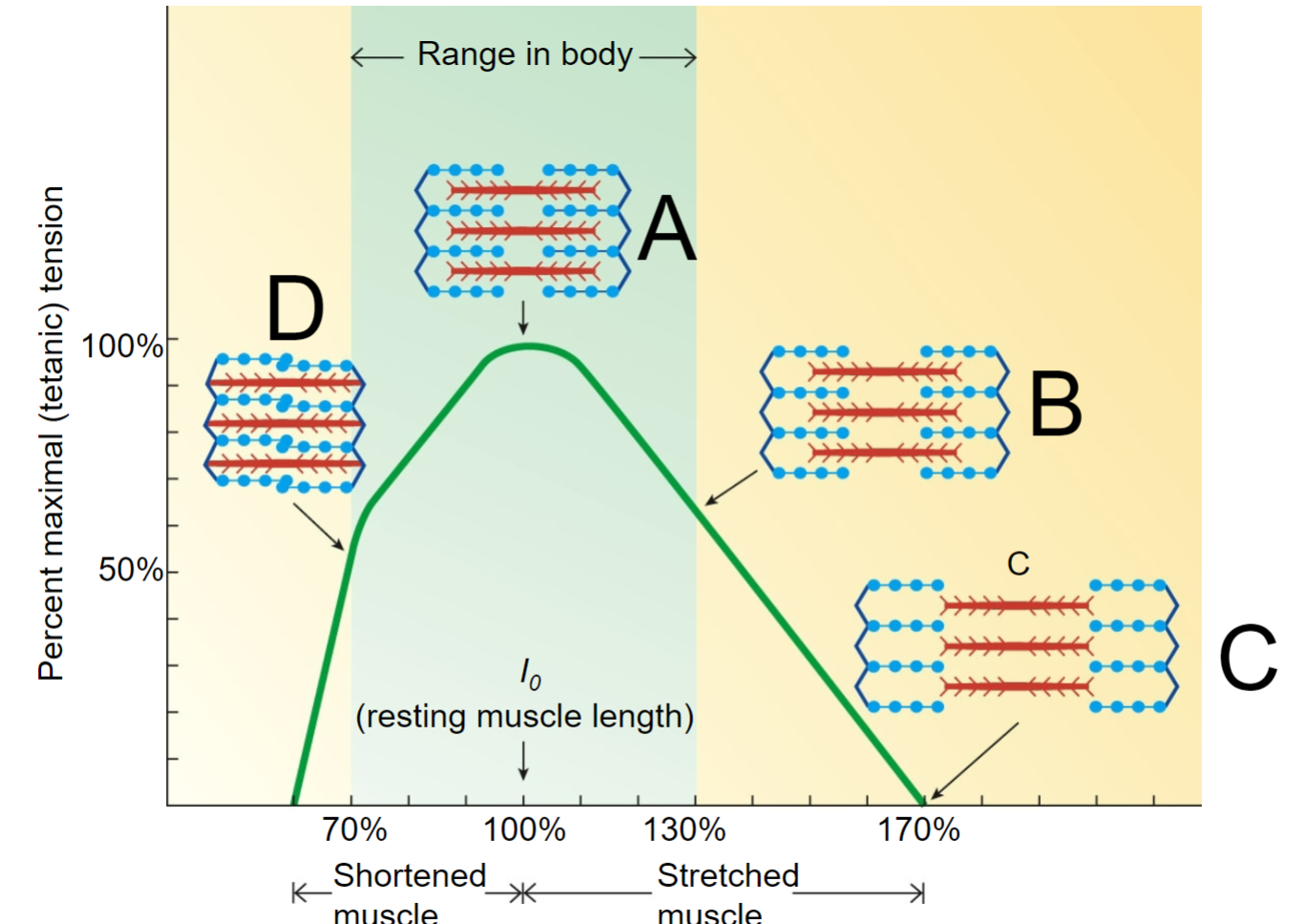
length-tension relationship - A
optimal contraction
-fiber at resting length generates maximum contractile force
-optimal overlap btwn thick and thin filaments
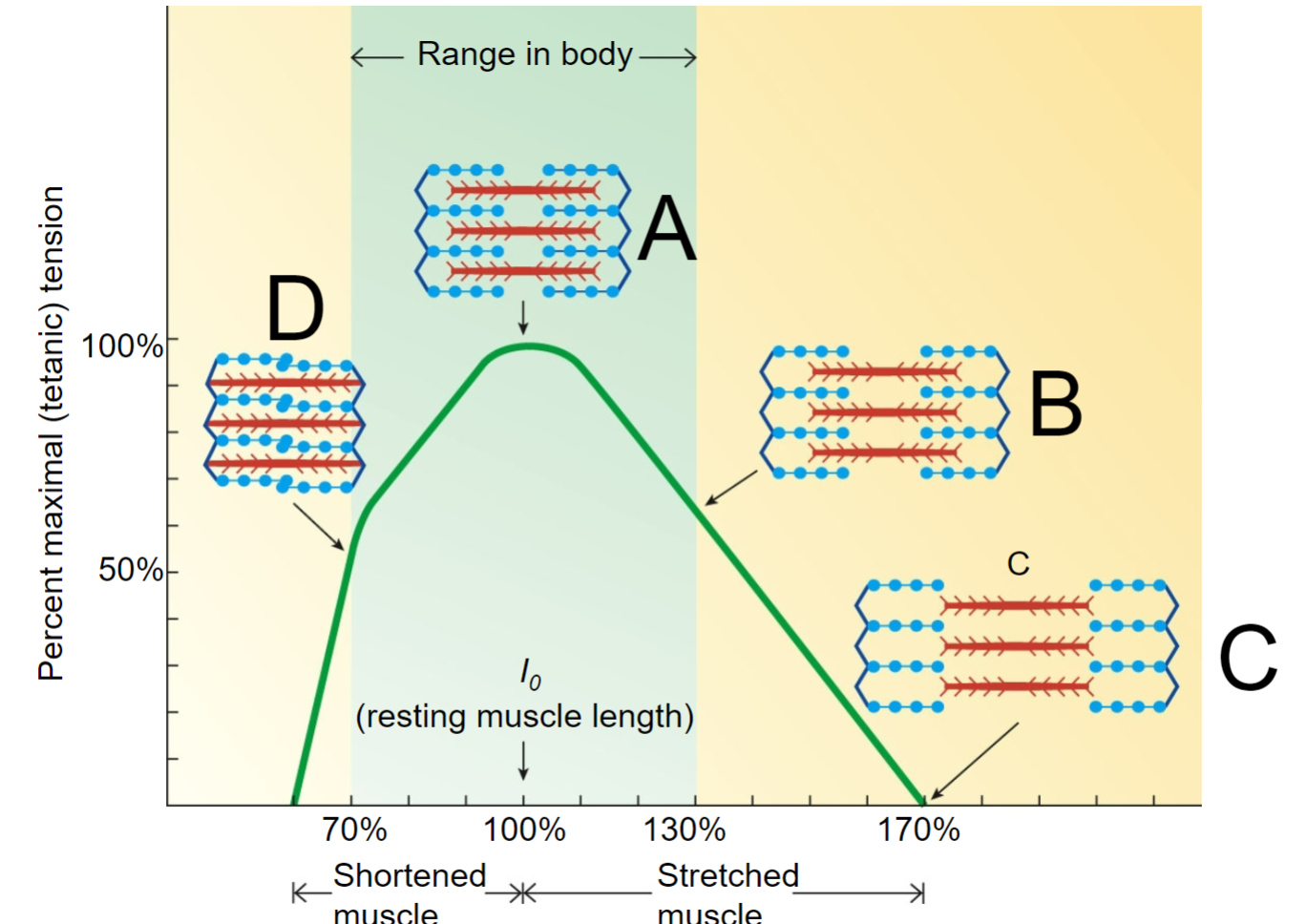
length-tension relationship - B
partial contraction
-fiber at extended length generates weaker force
-minimal overlap btwn thick and thin filaments
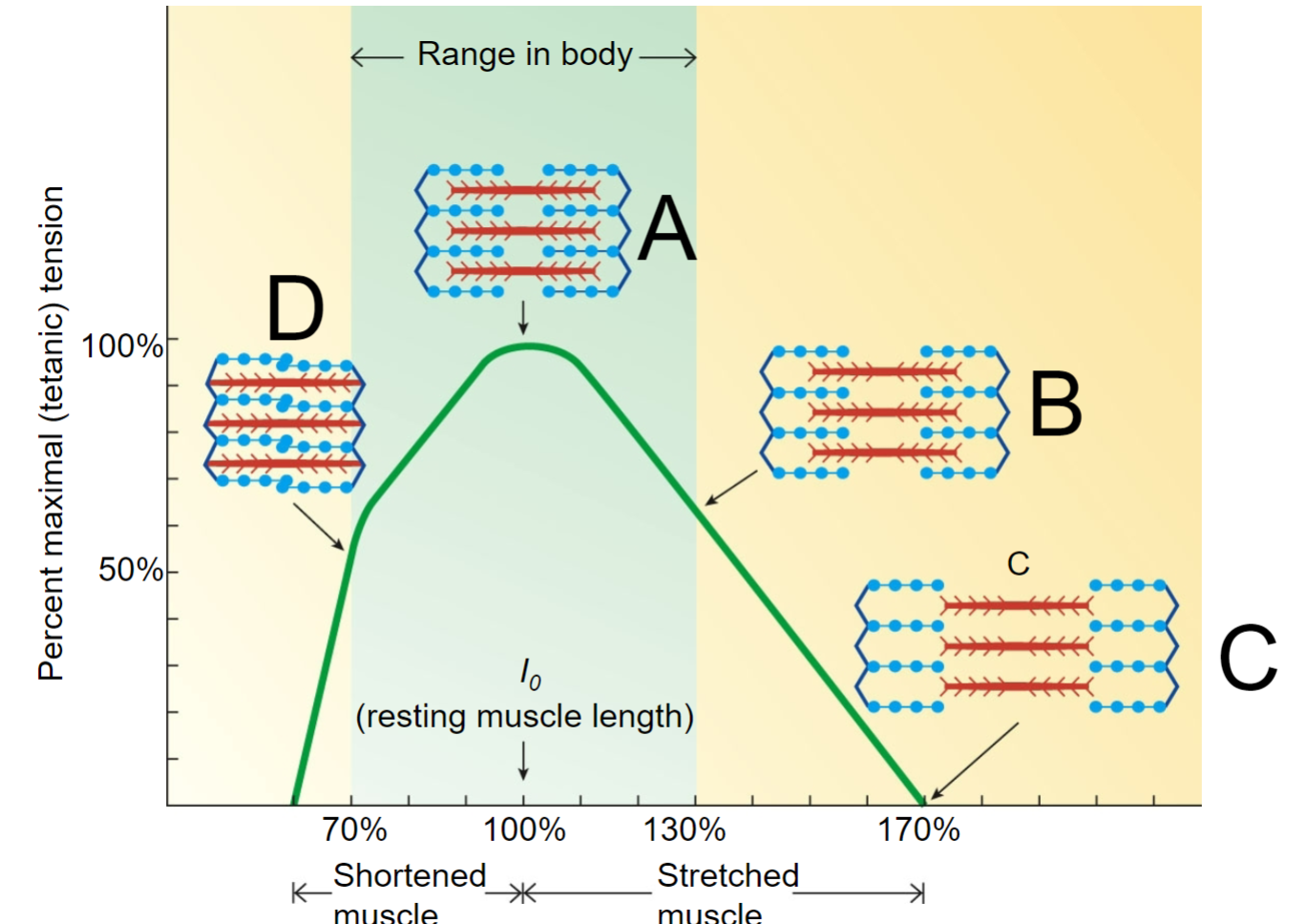
length-tension relationship - C
no contraction
-overextended, not possible in human body
-no overlap between thick and thin filaments
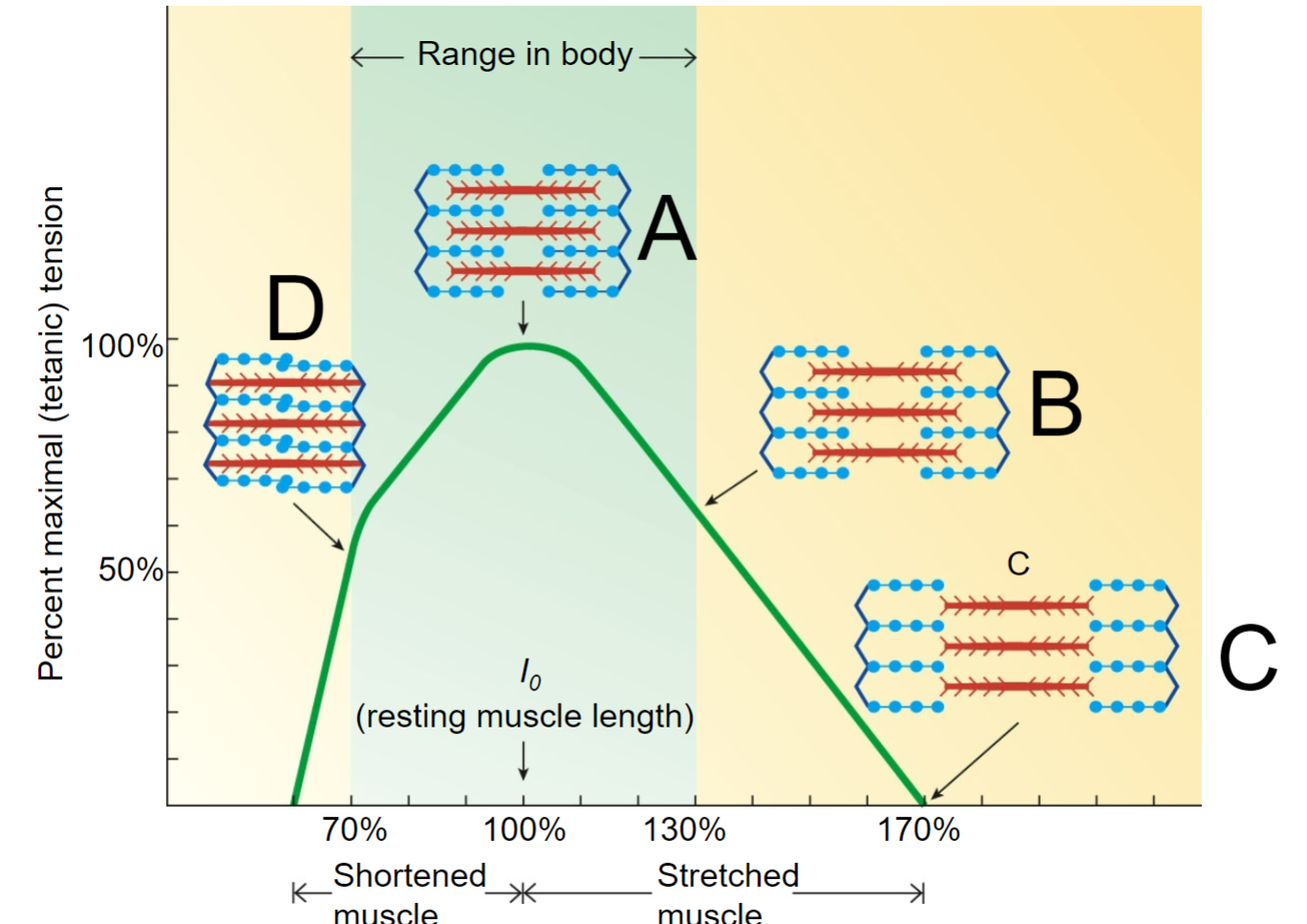
length-tension relationship D
partial contraction
-fiber at shorter length generates weaker force
-filament too close to Z disk, overlap is limited
case study: what is malignant hyperthermia (MH)
a genetic mutation that causes increased body temp when exposed to certain chemicals like anesthesia
**genetic mutation on the RyR1 receptor
case study: how does MH cause muscle rigidity?
it leads to increased Ca release from the SR → Ca always available to bind to troponin, create cross-bridge and make muscles contract
**it does this by acting on the person’s RyR receptor (which releases Ca)
case study: MH symptoms steps
1) anesthetic binds to the RyR receptor
2) Ca release initiated from SR → muscle contraction
3) ATP consumption increases due to constant contraction. once aerobic runs out, glycolysis happens
4) increase CO2 and lactic acid in body as result of glycolysis → pH decreases in body
5) body temp increases as byproduct of ATP rxns since they produce heat