Pathophysiology II - Exam 4/CBL 3 - CNS Infections 🧫
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
describe the morbidity and mortality rates associated with meningitis
morbidity
- 15-40% experience neurologic complications after infection
- more frequent in post-pneumococcal meningitis
mortality
- overall fatality rate is 15% in the US
- dependent on the causative organism and related to delay (>3 hrs) in ABX therapy
what are some of the risk factors of meningitis (long list!)?
- chronic medical disorders (CKD, DM, CF, etc.)
- extremes of age (<1 or >65 yo)
- under-vaccination (specifically for meningococcal or HIB vax.)
- immunosuppressed states (steroids, chemo, HIV, transplant)
- malignancy
- asplenia and sickle cell disease (which can cause 'functional asplenia' due to blockage of blood flow)
- living in crowded conditions
- travel to endemic areas (SW or NE US, Sub-Saharan Africa)
- alcohol use disorder
- bacterial endocarditis and IV drug use
- presence of ventriculoperitoneal shunt
- neurotrauma
- dural defects
- close/lengthy contact with someone with meningococcal disease
what are the 3 meningeal layers of the brain?
- dura mater (attached to skull)
- arachnoid
CSF is housed in the subarachnoid space
- pia mater (direct contact with brain parenchyma)
what's the difference between meningitis, encephalitis, myelitis, and encephalomyelitis?
- meningitis: infection of the meninges; inflammation of the pia mater, arachnoid, and CSF-filled subarachnoid space
- encephalitis: infection of the brain parenchyma
- myelitis: infection of the spinal cord
- encephalomyelitis: infection of the brain AND spinal cord
what type of barrier is the blood brain barrier (BBB)? describe its function
structural AND biochemical barrier
- non-fenestrated capillaries prevent passive diffusion from the intravascular space into the brain parenchyma
- limit host defenses in the CNS → complement and Ig levels are lower in the CSF than in serum!
during inflammation, permeability of the BBB is _____________
increased
- but the host defenses are still too low to fight the infection
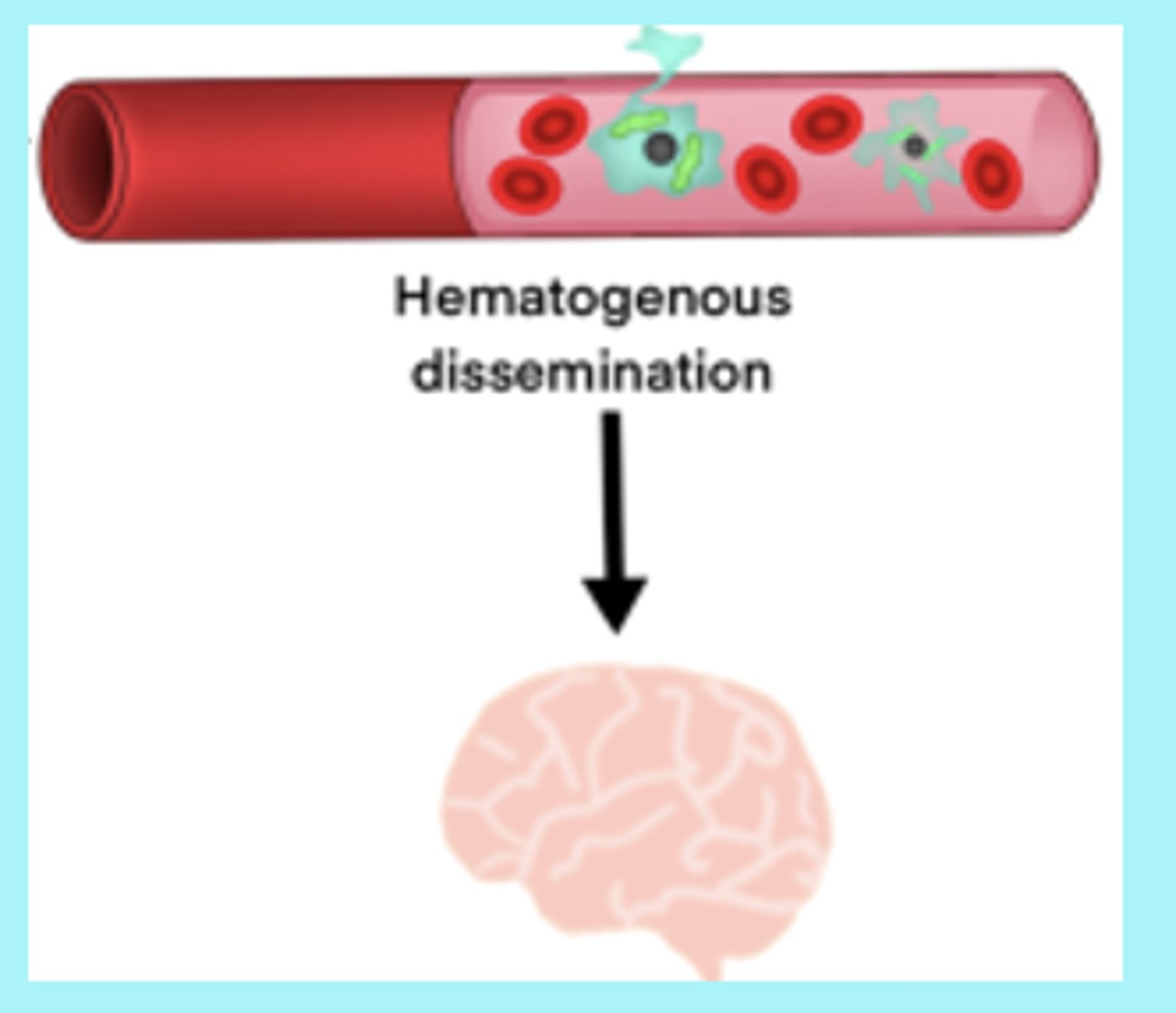
what are the 3 methods of bacterial spread into the CNS?
hematogenous, contiguous, and nosocomial
what is hematogenous spread?
spreading via the bloodstream
- bacteria attach to the nasopharyngeal epithelium, breach the mucosal barrier, and gain access to the bloodstream
what is contiguous spread?
spread from local infections
- secondary to infections such as otitis media, sinusitis, or mastoiditis
- secondary to direct invasion through trauma
what is nosocomial spread?
caused by contamination during surgery or LP
what are the common infectious viral and fungal causes of meningitis?
- viral: enterovirus, herpes virus, HIV
- fungi: cryptococcus
what are the common non-infectious causes of meningitis?
rare!
- drugs: NSAIDs, methotrexate
- systemic disease: sarcoidosis, lupus
- neoplastic disease
what are the most common bacterial causes of meningitis in a patient <1 month old?
- Streptococcus agalactiae
- gram-(-) enteric organisms (E. coli, Klebsiella, Enterobacter)
- Listeria monocytogenes
what are the most common bacterial causes of meningitis in a patient 3-23 months old?
- Streptococcus agalactiae
- Streptococcus pneumoniae
- Neisseria meningitidis
- Haemophilus influenzae
- E. coli
what are the most common bacterial causes of meningitis in a patient 2-50 years old?
- Streptococcus pneumoniae
- Neisseria meningitidis
what are the most common bacterial causes of meningitis in a patient >50 years old?
- Streptococcus pneumoniae
- Neisseria meningitidis
- gram-(-) enteric organisms (E. coli, Klebsiella, Enterobacter)
- Listeria monocytogenes
what are the most common bacterial causes of meningitis in a patient with risk factors present (alcoholism, immunocompromised)?
- Streptococcus pneumoniae
- Listeria monocytogenes
- Haemophilus influenzae
what are the most common bacterial causes of meningitis in a patient post-neurosurgery (any age)?
- aerobic gram-(-) bacilli (Pseudomonas)
- Staphylococcus aureus
- coagulase-(-) staphylococci
what are the most likely pathogens, onset of Sx, and presentation of acute meningitis?
- likely pathogens: bacterial, viral
- onset of Sx: hours-days
- presentation: fever, chills, severe HA, nuchal rigidity (neck stiffness), AMS, photophobia, vomiting
what are the most likely pathogens, onset of Sx, and presentation of subacute or chronic meningitis?
- likely pathogens: TB, crytococcus, non-infectious
- onset of Sx: weeks-years (gradual)
- presentation: low fever, HA, lethargy, disability
what are the 4 primary signs of acute meningitis is adults?
- fever
- nuchal rigidity
- AMS
- severe HA
other than the 4 key signs of acute meningitis in adults, what are some other signs/Sx that you may observe?
- chills
- vomiting
- photophobia
- purpuric and petechial rash (meningococcal or H. influenzae)

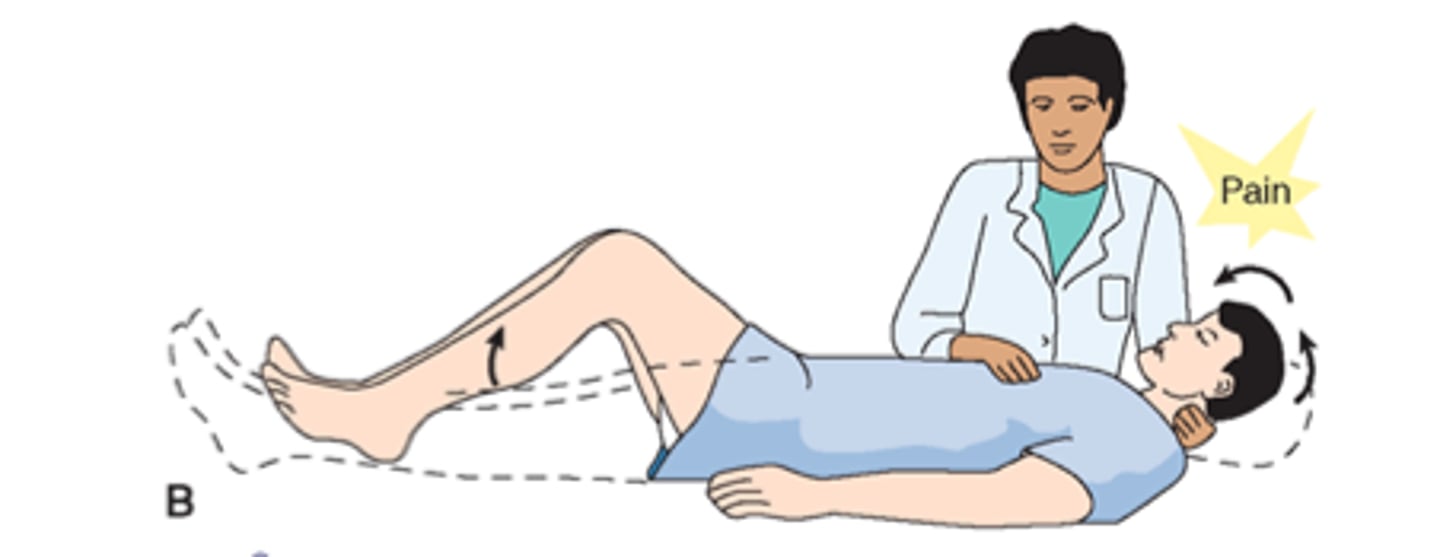
what are the 2 physical assessments that may suggest acute meningitis in adults?
- Brudzinski's sign: flexion of the neck induces flexion of the knees
- Kernig's sign: stiffness of the hamstrings causes an inability to straighten the leg when the hip is flexed to 90 degrees
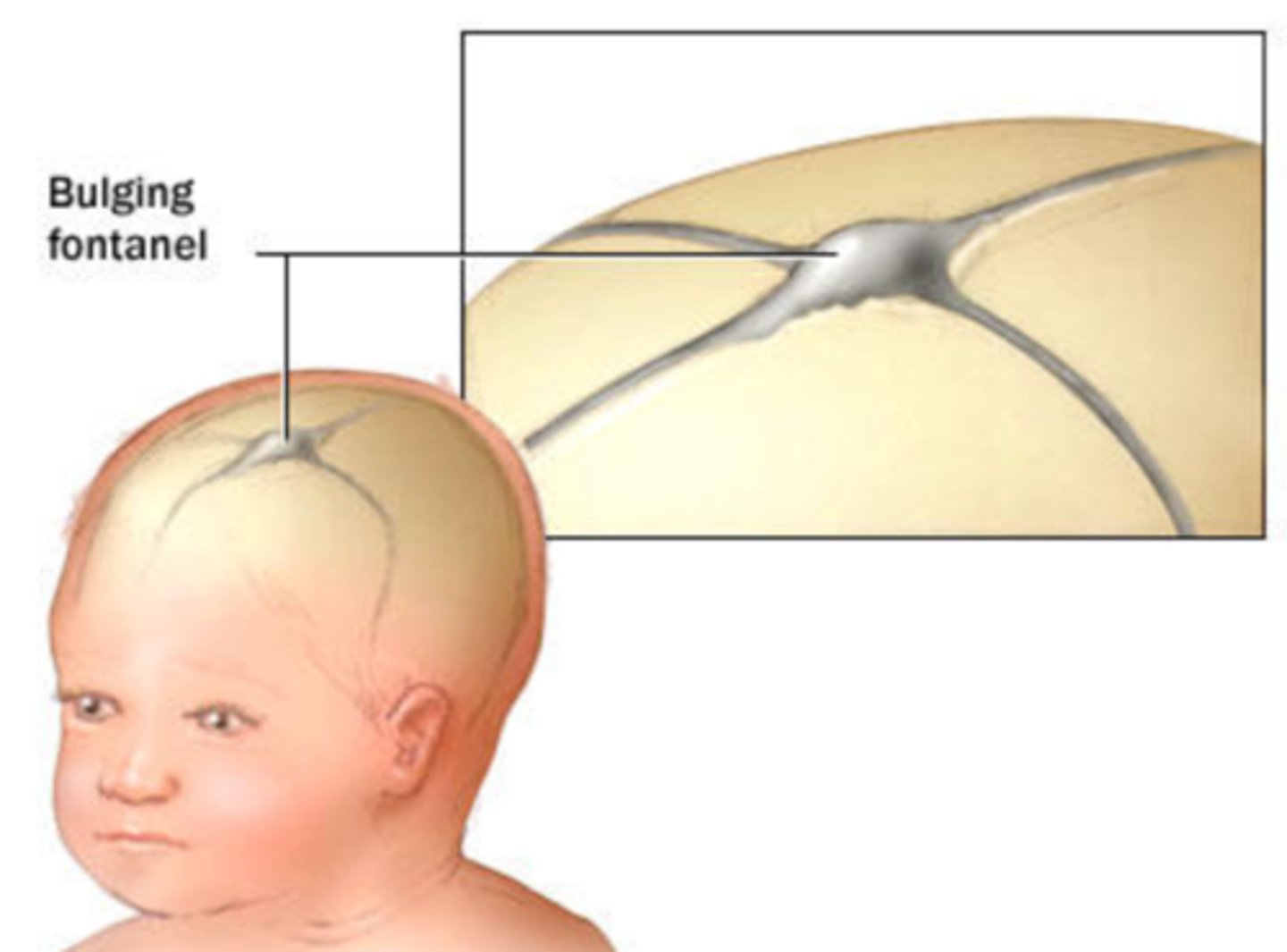
what are signs of acute meningitis in young children?
- bulging fontanelle (if not yet fused)
- apnea
- purpuric rash
- irritability
- refusal to eat
- convulsions
FYI - signs of a brain abscess depend on...?
size and location
- similar to other space-occupying lesions
FYI - what are the specific and non-specific signs of a brain abscess?
specific
- focal neurological deficits
- motor speech disorder
- ataxia
- seizures
non-specific
- HA
- fever
- nystagmus
- vomiting
what are the specific and non-specific signs of infective encephalitis?
specific
- AMS
- severe HA
- seizures
non-specific
- fever
- N/V
what are the primary physical assessment techniques used to identify meningitis?
determine the presence of meningeal irritation; reflect resistance to painful stretching of inflamed meninges from the lumbar level to the head
- Brudzinski's sign
- Kernig's sign

when would you seek cranial imaging to support a diagnosis of meningitis?
- moderately or severely impaired LOC
- new-onset seizures
- signs/Sx of brain abscess
- age >60 yo
- immunocompromised
what 3 tests should be performed to diagnose bacterial meningitis?
- CBC (leukocytosis)
- blood cultures
- lumbar puncture (spinal tap)
if a patient has bacterial meningitis, what would be observed upon visual inspection and lab testing of their CSF?
- CSF is cloudy, purulent (healthy CSF is clear!)
- increased WBC and PMNs (1000-5000 WBC/mm³, 80-95% PMNs)
- increased protein (100-500mg/dl)
- decreased glucose (<40 mg/dl, CSF to serum glucose ratio is ≤ 0.4)
- bacterial gram stain and culture positive (70-85% of the time)
- perform PCR for certain organisms!
what are the potential complications of a LP?
HA, local bleeding ("traumatic tap"), and brain herniation
how common are HAs as a complication of LPs?
10-25%
- likely due to low CSF pressure when the patient stands, caused by continued leakage of CSF at the lumbar site
how common is local bleeding as a complication of LPs?
20%
- rarely harms patient
- caused by hitting the venous plexus
describe brain herniation as a complication of LPs
- may occur in patients with increased ICP that transiently drops after LP
- patients are at risk for having CNS mass predisposed
- perform a CT/MRI for at-risk patients!
list the color, WBC count, differential, glucose levels, and protein levels in a patient with a normal CSF result
- color: clear, colorless
- WBC count (cells/mm³): <5
- differential: monocytes predominate
- glucose (mg/dl): 45-80
- protein (mg/dl): <50
list the color, WBC count, differential, glucose levels, and protein levels in a patient with bacterial meningitis
- color: cloudy
- WBC count (cells/mm³): elevated (1000-5000)
- differential: PMNs predominate
- glucose (mg/dl): decreased
- protein (mg/dl): elevated
list the color, WBC count, differential, glucose levels, and protein levels in a patient with viral meningitis
- color: cloudy
- WBC count (cells/mm³): elevated (50-1000)
- differential: lymphocytes predominate
- glucose (mg/dl): normal
- protein (mg/dl): slightly elevated
list the color, WBC count, differential, glucose levels, and protein levels in a patient with fungal meningitis
- color: cloudy
- WBC count (cells/mm³): normal to elevated (20-500)
- differential: lymphocytes predominate
- glucose (mg/dl): normal to decreased
- protein (mg/dl): elevated
list the color, WBC count, differential, glucose levels, and protein levels in a patient with TB meningitis
- color: cloudy
- WBC count (cells/mm³): normal to elevated (25-500)
- differential: lymphocytes predominate
- glucose (mg/dl): decreased
- protein (mg/dl): elevated
what are the common community-acquired organisms that cause meningitis?
- S. pneumoniae (gram-(+) cocci in pair/chains)
- H. influenzae (gram-(-) coccobacilli)
- N. meningitidis (gram-(-) diplococci)
- S. agalactiae (gram-(+) cocci in pair/chains)
- L. monocytogenes (gram-(+) bacilli)
- Enterobacterales (gram-(-) bacilli)
what are the common nosocomial or HC-acquired organisms that cause meningitis?
- P. aeruginosa (gram-(-) bacilli)
- S. aureus (gram-(+) cocci in clusters)