Exam3 Speech Disorders Across the Lifespan
1/50
Earn XP
Description and Tags
Exam 3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
Dysarthria
a group of neuromuscular impairments that affect how muscles work to produce speech. This happens when there is damage to the central nervous system (CNS) or peripheral nervous system (PNS), both of which control the muscles responsible for speech.
What is in the central nervous system
the brain and spinal cord
Responsibilities of the CNS
speech planning, motor commands, and sensory processing happen.
Damage to the CNS (like stroke TBI, or degenerative disease) can
disrupt the brain’s ability to plan or send clear movement commands to the muscles used for speech.
PNS Peripheral Nervous System
Cranial nerves (which connect directly from the brain to the face, mouth, and throat) and spinal nerves (which connect from the spinal cord to muscles in the body, including those for breathing).
PNS responsibilities
carrying messages from the brain/spinal cord to the muscles. It also sends sensory information back up to the brain.
Damage to PNS can
can directly affect the muscles involved in speech — making them weak, uncoordinated, or unable to move correctly.
Dysarthria can impact
Respiration: Breathing needed for speech
Phonation: Producing sound with the vocal cords
Resonation: Shaping the sound in the throat, mouth, and nose
Articulation: Forming clear speech sounds with the tongue, lips, and jaw
Spastic Dysarthria vs Flaccid Dysarthria
Spastic: CNS (tightness, exaggerated reflexes)
Flaccid: PNS (weakness, low tone)
Why does Flaccid Dysarthria happen
when the lower motor neurons (the nerves connecting the spinal cord or brainstem to muscles) are damaged. It can also happen if the muscles themselves are affected.
Hypotonia
Weak, floppy muscles with low tone
what are aspects of Flaccid Dysarthria
Hypotonia: Weak, floppy muscles with low tone
Breathy voice
Reduced loudness and pitch control
Hypernasality (too much nasal sound)
Slurred articulation
Myasthenia Gravis
chronic autoimmune neuromuscular disorder. In MG, the body’s immune system attacks the communication point between nerves and muscles at the neuromuscular junction. This disrupts the ability of the nerve to successfully activate the muscle, leading to muscle weakness that gets worse with use (a hallmark symptom called fatigue).
What are aspects of myasthenia gravis
Reduced loudness — respiratory muscle weakness
Hypernasality — weak velum (soft palate) control
Imprecise articulation — tongue and lip weakness
Fatigue effect: Speech may sound relatively normal at the beginning of a conversation, but as the person keeps talking, their speech gets more slurred, weak, and difficult to understand.
When would a clinician/doctor suspect myasthenia gravis
when a client’s speech or voice deteriorates with use but temporarily improves after rest. This fatigue-recovery cycle is almost a giveaway that MG could be involved.
What does Spastic Dysarthria result from
bilateral upper motor neuron damage in the brain. Upper motor neurons send signals from the brain to the lower motor neurons. When these signals are damaged, muscles become overly stiff and tight (spastic). Spastic is typically a consequence of a stroke and often co-occurs with aphasia.
What are some aspects of Spastic Dysarthria
Hyperactive reflexes (exaggerated responses to touch)
Increased muscle tone at rest
Slowed, effortful speech
Strain-strangled voice quality
hypokinetic Dysarthria Hypo - Kinetic
hypo: too little
-kinetic: movement
Hypokinetic dysarthria is a ______________ caused by too little movement: movements are _____________________
Hypokinetic dysarthria is a MOTOR SPEECH DISORDER disorder caused by too little movement: movements are small, rigid, and hard to initiate or stop.
Common cause of hypokinetic dysarthria and other conditions that damage the basal ganglia
Parkinson’s disease
why does parkinson’s occur
less dopamine the brain has trouble starting and making movements big enough. At the same time, the brain over-suppresses movement, making everything smaller, stiffer, and slower.
Because parkinson’s is hypokinetic what does voice, prosody, speech rate, facial expression look like
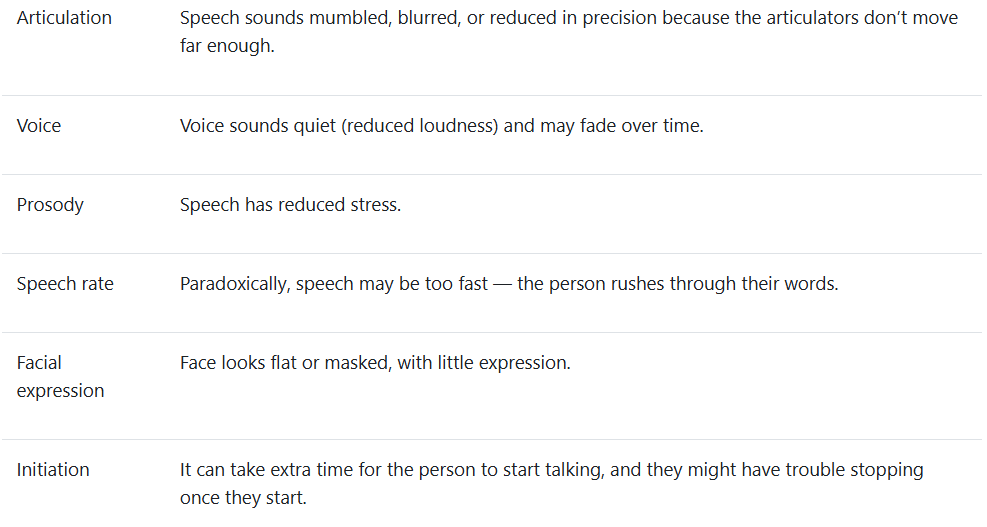
Hypokinetic dysarthria is only dysarthria where speech rate is typically ____________, Also is the only dysarthria where ___________ is dominant feature
too fast
reduced movement
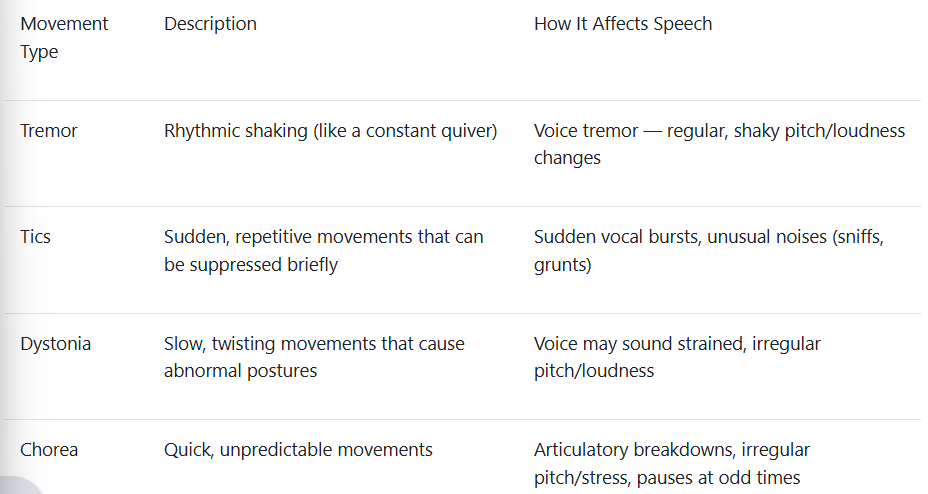
Hyperkinetic Dysarthria (too much movement) how does tremors, tics, dystonia, and chorea affect speech
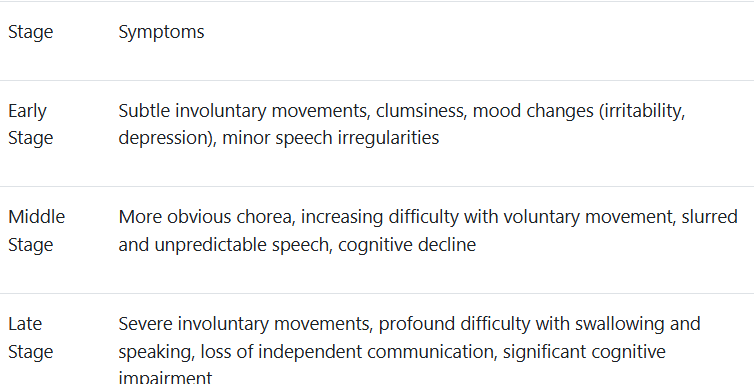
Huntingtons disease
genetic, progressive neurodegenerative disorder.
What is the cause of Huntington’s disease
caused by a mutation in the HTT gene, which leads to the gradual breakdown of nerve cells in certain areas of the brain — especially the basal ganglia.
What does Huntington’s disease cause
Involuntary movements (chorea) that interrupt normal speech production.
Irregular breakdowns in articulation — sounds may get distorted or jumbled unpredictably.
Abnormal pitch and loudness — speech may suddenly get louder or softer without the person meaning to.
Unpredictable pauses — speech timing becomes erratic.
Early and late stages of huntingtins disease
How do SLPs help and how do devices help
Huntington’s patients often lose their ability to speak clearly — but they still want to communicate.
SLPs help with speech therapy in the early stages (focusing on compensatory strategies like slowing down or using communication partners).
In later stages, AAC (Augmentative and Alternative Communication) becomes critical — this could be low-tech (like communication boards) or high-tech (like eye-gaze communication devices).
Ataxic dysarthria is damage to _______. Issues with what?
cerebellar control circuit
Its characteristics are most evident in articulation and prosody
It reflects a breakdown in timing and coordination
What does the cerebellum do
Helps time the components of movement, scale the size of muscle actions, and coordinate sequences of muscle contractions for skilled motor behavior.
It monitors the adequacy of movement outcomes based on feedback from muscles, tendons, and joints.
When cerebellar lesions associated with ataxic dysarthria are unilateral, the lesion is more often on the right side. The right cerebellar hemisphere contributes to prearticulatory temporal organization of syllables (e.g., adjusting syllable length; implementing anticipatory coarticulation effects).
Severe ataxic dysarthria is most commonly associated with bilateral or diffuse cerebellar disease.
What features of ataxic dysarthria distinguish it from other dysarthrias?
Swallowing complaints are less frequent than in flaccid or spastic dysarthria.
Telescoping: An inconsistent breakdown of articulation in which a syllable or series of syllables are unpredictably run together, giving speech a transient accelerated character.
Friedreich ataxia is caused by _______-. Begins before _____. Evolves to __________.
a defect (mutation) in a gene labeled FXN, which carries the genetic code for the production of a protein called frataxin.
Usually begins before age 20
Evolves to incapacitation and death over a course of about 20 years
Mixed dysarthria
Amyotrophic Lateral Sclerosis (ALS) is a progressive neurodegenerative disease that affects both the upper motor neurons (UMNs) and lower motor neurons (LMNs). Because both types of motor neurons are damaged, ALS is known for causing mixed dysarthria — meaning a combination of spastic and flaccid characteristics.
The specific type of dysarthria a person with ALS experiences depends on which motor neurons are predominantly affected at the time.
Interviews should be how ? Ethnographic interview
Do not do a prescriptive approach. Look at behaviors and behavioral change. I am going to open up an opportunity to have a therapeutic relationship. Partnership! not have the clinical be the one with all the power. Having a conversation to understand the patient.
what is prosody
refers to the suprasegmental aspects of speech; it “describes properties of the speech signal that modulate and enhance its meaning
pitch/frequency
loudness/intensity
length/duration
What does prosody impact
social interactions (new versus given information, statements versus questions)
grammar (pauses before clauses)
prosody conveys emotion and is an individual style
PVSP
Phrasing
Rate
Stress
Loudness
Pitch
Laryngeal features
Resonance
Phrasing
Rate
Stress
Loudness
Pitch
Laryngeal features
Resonance
Phrasing
•repetitions: sound/syllable, word, multiple word
•revision and repetition with revision
Rate
•slow artic/pause time, slow/pause time, fast, or fast/acceleration
Stress
•equal stress, excessive stress, or misplaced stress
Loudness
•soft or loud
Pitch
•low pitch/glottal fry, low pitch, high pitch/falsetto, high pitch.
Laryngeal features
•breathy, rough, strained, tremulous, register break
Resonance
•nasal, denasal, or nasopharyngeal.
Intervention
focuses on
Speech-oriented approaches
Improving speech intelligibility
Improving efficiency and naturalness of spoken communication
Prosody
Communication-oriented approaches
Improve - communication even when speech itself does not change
AAC
Sensory cueing techniques utilize ____ input to guide speech movement sequences
sensory
Integral Stimulation (IS)
Approach:
Focus:
Mechanism:
Evidence:
Outcome:
Approach: Step-by-step practice of speech movements using phonemic word lists.
Focus: Improves motor planning and coordination for speech production.
Mechanism: Breaks down complex movements into smaller components, gradually building towards more challenging speech targets.
Evidence: Studies demonstrate effectiveness in improving motor learning and speech production in adults with AOS.
Outcome: Enhances speech intelligibility and communication skills by decomposing speech and progressing systematically.
PROMPT Therapy:
Approach:
Focus:
Mechanism:
Cues:
Evidence:
Outcome:
Approach: Tactile-sensory method using touch pressure, kinesthetic signals, and proprioceptive cues.
Focus: Restructuring oral muscular movements for improved sound production, rate, and prosody.
Mechanism: Provides physical, tactile prompts to guide articulator movement.
Cues: Touch pressure, kinesthetic cues, and proprioceptive cues.
Evidence: Demonstrated effectiveness in treating AOS by addressing specific motor planning challenges.
Outcome: Develops accurate and fluent speech production skills by targeting precise articulation.
What is the difference between the type of neuron and type of damage associated with flaccid versus spastic dysarthria?
Why is it important to interview both patient and primary communication partner?What is ethnographic interviewing and what are its benefits? How are questions designed in ethnographic interviewing?
What is the purpose of ASHA NOMS?
What is the purpose of the PVSP? Why would this be included in a diagnostic protocol?
What is the purpose of obtaining maximal phonation times?
What is the purpose of the Frenchay Intelligibility Test?
What is the purpose of the PACE Rating Scale?
If groping is present in the oral mechanism exam, an SLP would test nonverbal oral apraxia and verbal apraxia. How are these two tasks different?
Define factors that may influence decision making and treatment.
Define the 5 categories of management.
How are the goals of speech-oriented approaches different from communication-oriented approaches?
Provide one example of a strategy/approach that would address each subsystem for individuals with dysarthria.
How are goals of apraxia therapy different from dysarthria therapy?
Subsystem- back it up
What are key speech characteristics of hypokinetic dysarthria?
What are movement types associated with hyperkinetic dysarthria and how do they affect speech?
What features distinguish ataxic dysarthria from other dysarthrias?
What is an example of mixed dysarthria? Why is it considered mixed?
What distinguishes AOS from aphasia?
What distinguishes AOS from dysarthria?
Why is it important to interview both patient and primary communication partner?What is ethnographic interviewing and what are its benefits? How are questions designed in ethnographic interviewing?
What is the purpose of ASHA NOMS?
What is the purpose of the PVSP? Why would this be included in a diagnostic protocol?
What is the purpose of obtaining maximal phonation times?
What is the purpose of the Frenchay Intelligibility Test?
What is the purpose of the PACE Rating Scale?
If groping is present in the oral mechanism exam, an SLP would test nonverbal oral apraxia and verbal apraxia. How are these two tasks different?