GI system - unit 3
1/212
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
213 Terms
What s the role of the GI tract/alimentary canal?
route of intake for nourishment, digest and absorb nutrients, eliminates waste products
What are the accessory organs of the GI system?
salivary glands, pancreas, liver, gallblader
What are the indications for a salivary gland imaging procedure?
eval of dry mouth (xerostomia)
rule out blockage of one or several glands/ducts
evaluate palpable mass
What is the patient prep for a salivary gland procedure?
none
What type of collimator is used for a salivary gland procedure?
low energy, parallel hole collimator
How is the patient positioned for a Salviary gland procedure?
seated, facing the camera
head tilted backward with neck extended
chin resting on camera
Why do we position the patient with their head tilted back in a salivary gland imaging procedure?
to prevent the thyroid from obscuring the salivary glands
why do we give the patient lemon juice during a salivary gland imaging procedure? What types of images are we taking after this?
gustatory stimulation
20-minute flow images of tracer clearance from the salivary gland
What is a general normal finding on a salivary gland imaging procedure?
simultaneous, rapid, and symmetrical uptake of all three glands
What are some abnormal findings on a salivary gland image, and what is the cause of each?
hot spots/area of increased uptake = Warthin tumors
cold areas = metastatic lesions
poor response to gustatory stimulation = blockage
Where is the esophagus located?
posterior to the trachea
What are the three parts of the esophagus? What type of muscle is in each?
upper third = striated
middle = combination of striated and smooth
lower third = smooth
What is the dosage for a salivary gland imaging procedure? How is it given?
1-5 mCi Tc-99m pertechnetate via IV
What is the method of uptake of Tc-99m pertechnetate into the salivary glands?
ions are excreted by glands into saliva
What images are taken in a salivary gland imaging procedure? How long are we taking these images for?
dynamic images of the anterior face and neck
1-2 second intervals for 15-20 seconds
what are we looking for in salivary gland initial dynamic imaging?
simultaneous and symmetrical uptake
What additional images are we taking for a salivary gland imaging procedure? And why are we taking these photos?
anterior and lateral views of the head and neck
confirming the normal presence of tracer in the saliva in the oral cavity
What are normal findings for a salivary gland imaging procedure after the first swallow?
rapid decrease in esophageal activity within 5-10 seconds after first swallow
What are normal findings for a salivary gland imaging procedure after 2 minutes?
at 2 min 10% of peak activity remains
What are normal findings for a salivary gland imaging procedure after 10 minutes?
less than 5% of peak activity remains
What are abnormal findings on a salivary gland imaging procedure?
any sort of delay - anything in esophageal track after 2 and 10 min
activity present in esophagus
Achalasia - absence of relaxation of the lower esophageal sphincter
What are the indications for a Esophageal transit procedure?
esophageal motor disorder
efficacy of surgical or mechanical interventions on the lower esophagus
What is an esophageal motor disorder?
difficulty or pain associated with swallowing
What is the patient prep for a Esophageal transit procedure?
NPO for 2 hours
What does NPO mean?
nothing per oral - aka no eating or drinking
What is the dose for an Esophageal transit procedure?
300uCi of Tc-99m sulphur colloid
How is the dose for an Esophageal transit procedure given?
in 15ml of tap water (orally)
What type of collimator is used for a Esophageal transit procedure?
low energy, all purpose
How is the camera positioned over the patient during an Esophageal transit procedure?
entire esophagus with the stomach at the bottom of the FOV
What types of images are we taking for an Esophageal transit procedure? How long is each image taken?
flow/dynamic for total of 10 min
0.25 sec for first 2 min
15 sec intervals for 8 min
How should the patient be instructed during an Esophageal transit procedure?
Pt should take entire dose/water in mouth but not swallow until instructed
have Pt swallow every 15 sec for 10 min
What is gastroesophageal reflux?
complex symptoms including regurgitation of food/liquid, heartburn, and chest pain
gastric or duodenal contents enter the esophagus
What can cause gastroesophageal reflux?
anatomic abnormalities, incompetence of the lower sphincter
fat, alcohol, chocolate, cigarettes
What is the patient prep for a gastroesophageal reflux imaging procedure?
NPO for 8 hrs
If an esophageal transit study is planned on the same day as a gastroesophageal reflux, which should be performed first?
esophageal transit study first
What is the dose for a gastroesophageal reflux imaging study?
300uCi of Tc-99m Sulphur colloid
How is the patient given the dose for a gastroesophageal reflux procedure?
300uCi of Tc-99m sulphur colloid, mixed with 150ml of orange juice and 150ml of 0.1 M hydrochloric acid
Why is the dose for a gastroesophageal reflux procedure mixed with orange juice and hydrochloric acid?
acidity stimulates gastric reflux
What is the estimated amount of fluid we give patients for a gastroesophageal reflux scan?
300ml or 10oz
What are the four factors required to induce gastroesophageal reflux?
oral administration of acidified solution
successive, increased pressure applied to the abdomen
maintenance of supine position
at least 300ml volume in the stomach to oppose the applied pressure
Describe the imaging procedure for a gastroesophageal reflux scan?
give patient dose
fit patient with an abdominal binder
10min after tracer administration begin imaging
position patient supine, w/ stomach at bottom of FOV (including entire stomach
if esophagus visualized during positioning give patient water to flush esophagus
acquire images for 30 seconds at the pressure points 0,20,40, 60, 80, 100mHg, without deflating between points
take post deflation image
What are normal and abnormal findings for a gastroesophageal reflux study for adults?
normal = <4% reflux
abnormal = > 4% reflux and can be visualized in the images
Why would 24 hr delayed images be performed on a gastroesophageal reflux study?
detection of pulmonary aspiration
What types of findings might you see in a child/infant gastroesophageal reflux study? What dosage do we give to pediatric patients?
shows aspiration, or GER caused by delayed emptying
1mCi of Tc-99m Sulfur colloid in infant formula orally via NG or g-tube
What is the role of the stomach in the digestive system?
food reservoir
breaks down solid food into chyme
controls rate of emptying gastric content into the duodenum
Where does the stomach empty into?
duodenum into small intestine
What is the top portion of the stomach?
fundus
What is the lower region of the stomach before it empties into the small intestine? What is the valve that controls the rate of emptying?
pylorus
pyloric sphincter
What is the patient prep for a gastric emptying procedure?
NPO 4-12 hrs before
What are the indications for a gastric emptying procedure?
confirm gastroparesis as a cause of persistant nausea and vomiting
monitor effects of therapy in patients with abnormal motility - diabetics
What are some factors that affect a gastric emptying procedure?
sex, time of day, composition of meal (volume, caloric content, amount, protein)
What is gastroparesis?
delayed gastric emptying, food staying in stomach and not emptying
What is the dose for a gastric emptying procedure? What are we giving to the patient? How fast should the meal be eaten?
1mCi of Tc-99m Sulfur colloid in eggs (scrambled, liquid), oatmeal
2 slices of white toast, 2 containers of jelly, 200ml of water
should be eaten in 10 min
What are the pediatric tracer(s) used for a gastric emptying study? How is it given?
Tc-99m DTPA in formula, can also do In-111 DTPA in OJ
What is the procedure for a gastric emptying study?
have patient eat breakfast within 10 min, immediately lay down under the camera(sometimes upright)
tape C0-57 marker right of xiphoid process
initial 45min dynamic study, then by 1 min static at 2, 3, and 4 hours post meal
How long are we imaging/taking images in the initial dynamic image phase for a gastric emptying study? and when do we begin imaging?
1 min dynamic images for 45 minutes after patients meal
If we graph the behavior of solids in a gastric emptying study, what type of behavior should we expect to see? What is the normal half-time for solids and why?
linear, 90min half time
3 textures all processed differently in body
If we graph the behavior of liquids in a gastric emptying study, what type of behavior should we expect to see? What is the normal half-time for liquids?
exponential
half time = 30min
What is the gastric emptying half time? What is it used for?
time it takes for the stomach to empty 50% of ingested meal
used to assess gastric transit
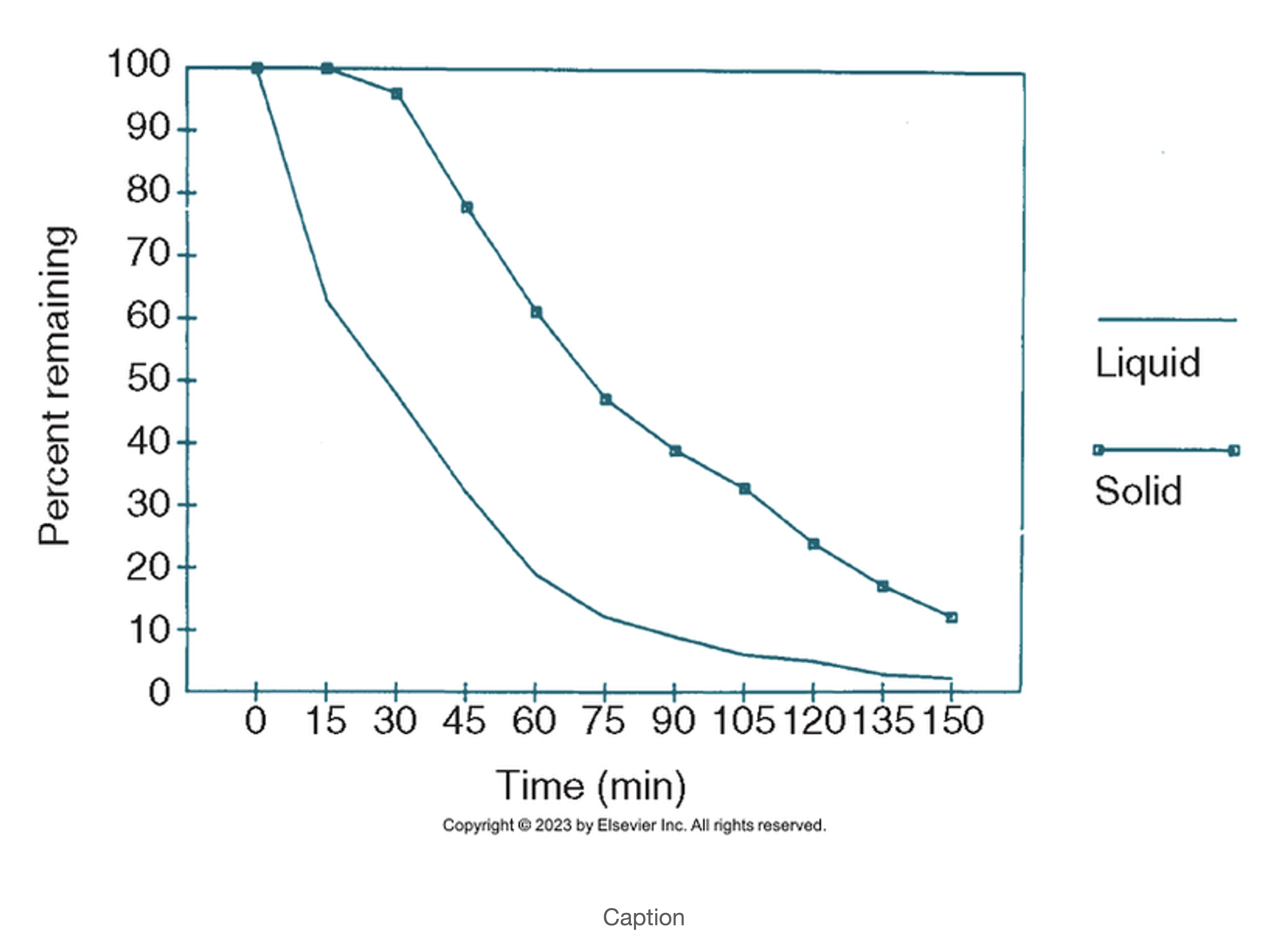
This gastric emptying graph demonstrates:
normal liquid emptying
normal/slightly delayed solid emptying
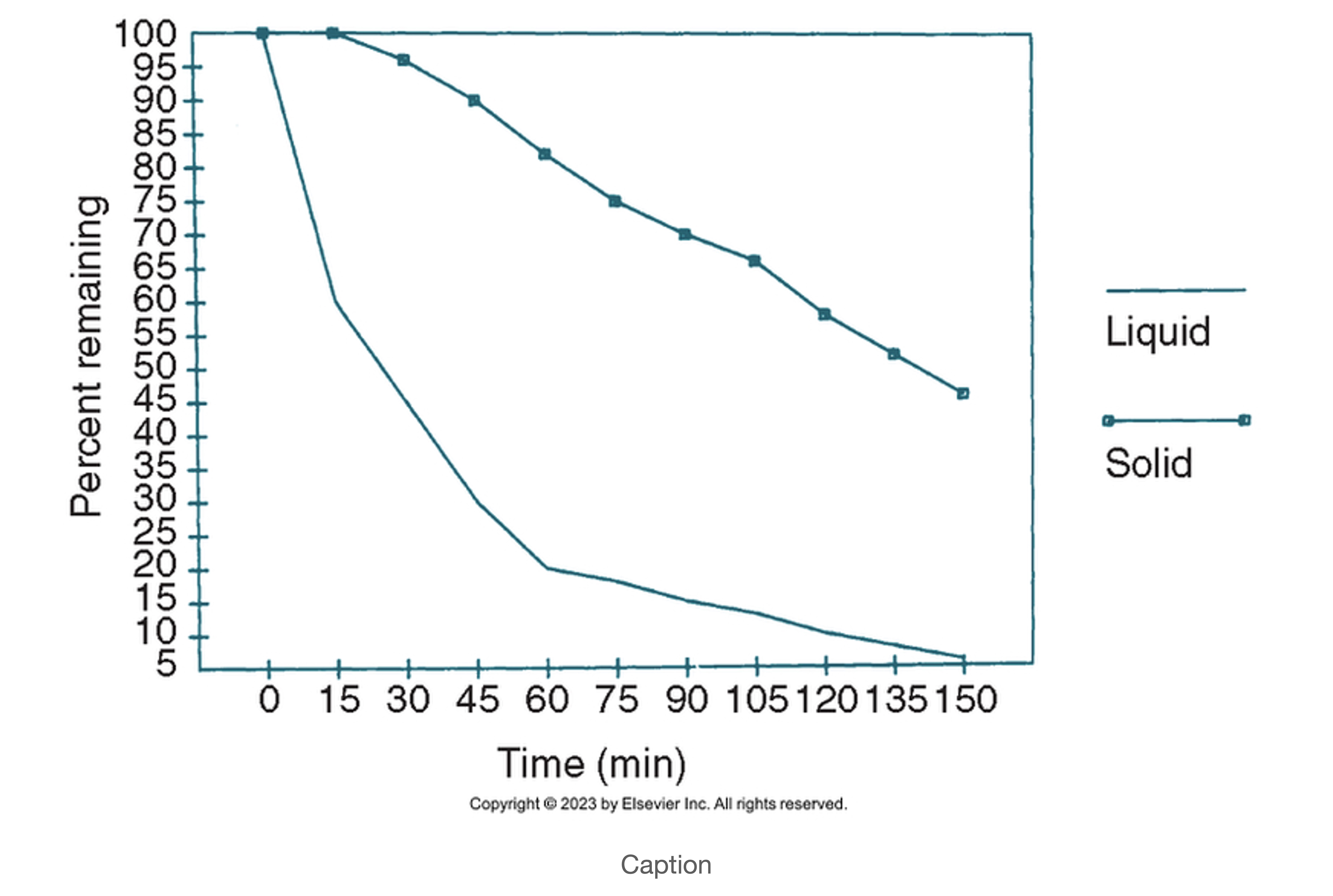
This gastric emptying graph demonstrates:
normal liquid emptying
delayed solid emptying
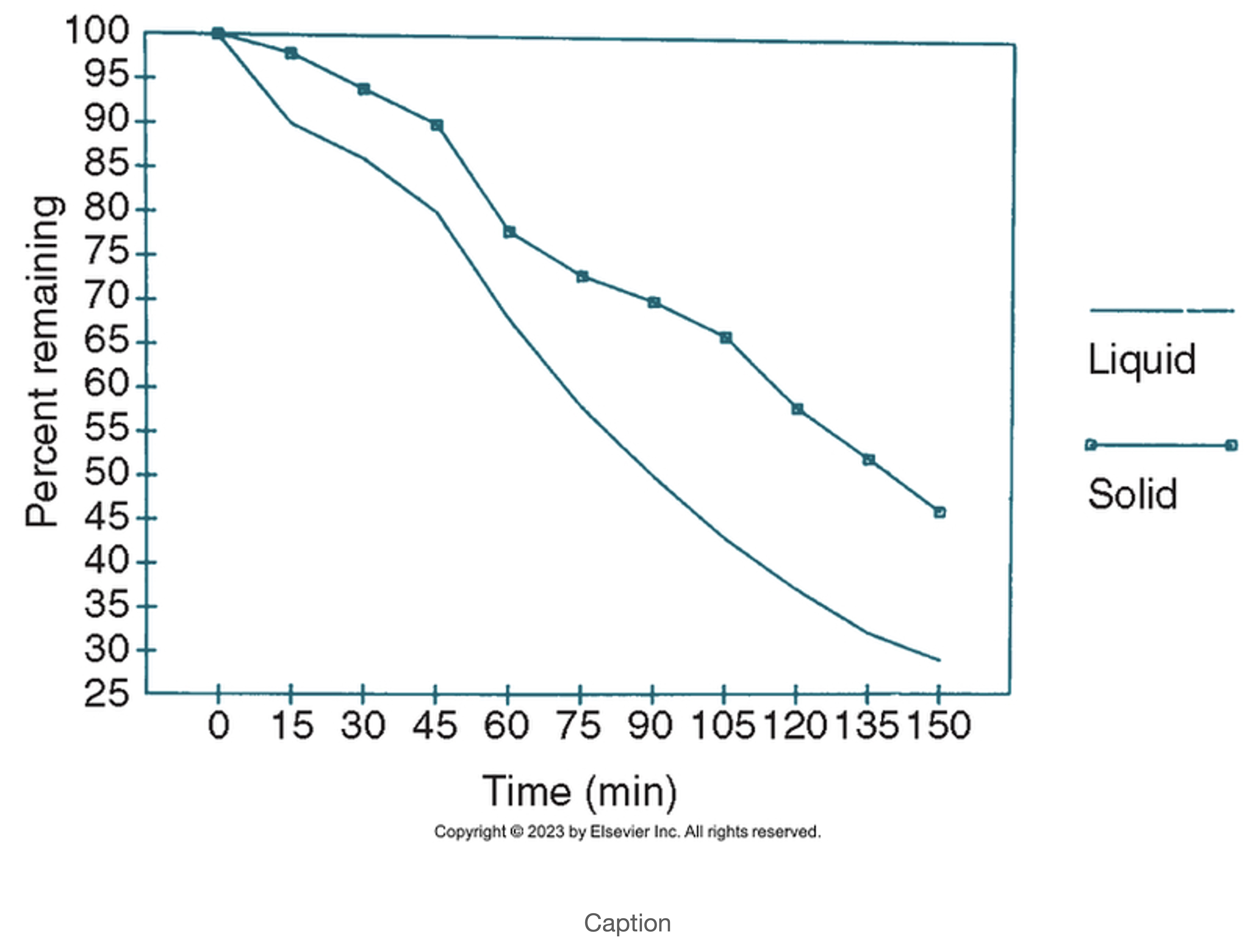
This gastric emptying graph demonstrates:
delayed liquid emptying
delayed solid emptying
what is a GI bleed?
blood loss from any organ in the GI tract (mouth to anus)
Where does an upper GI bleed ordinate from? What can be a telltale indicator that it’s an upper GI bleed?
esophagus, stomach, duodenum (first part of small intestine)
dark, tarry stools
Where does a small bowel bleed orignate from?
jejunum, ileum
Where does a lower GI bleed originate from? What can be a telltale indicator that it’s a lower GI bleed?
colon, rectum, anus
bright red blood
What are the indications for a GI bleed?
localization of the site of bleeding -active or intermittent
detecting and localization of hemorrhage including retroperitoneal and peripheral locations
Is a GI bleed study usually an emergency procedure? why or why not?
prompt therapy depends on exact localization
usually substantial bleeding in stool
patient can bleed out - find cause to fix in surgery
Is there any patient prep for a GI bleed scan?
no
Are we performing static or dynamic images for a GI bleed?
dynamic to catch the bleed and localize the source of it
What type of radiopharmaceuticals are we using for a GI bleed?
Tc-99m Sulfur colloid
Tc-99m labeled red blood cells
What are the pros and cons of using tc 99m sulfur colloid for a GI bleed?
pros: minimizes background activity, promotes high contrast ratio
cons - rapid clearance, requires pt to be actively bleeding
List the three ways we can label red blood cells for a GI bleed using Tc-99m.
in Vivo
in Vivi/in vitro
in vitro
How are RBCs labeled in vivo for a GI bleed?
What is the general efficiency of using this method?
labeled inside body
inject stannous ion (Sn+2), wait 20-30 min, inject Tc-99m Pertechnetate
variable, 60-90% labeling efficiency
What are the pros of performing a GI bleed scan in Vivo? What are the cons and why?
convenient and easy
can’t see bleeding in the stomach, small bowel, and/or colon because they’re natural areas of uptake of free Tc99m in body
What is the procedure for an in VIvo/In vitro Gi bleed procedure? What is the efficiency rate of labeling?
IV injection of stannous ion
blood sample collected in syringe containig Tc-99m-pertechnetate and anticoagulant (heparin)
reinject labeled sample
~95% efficiency
What are the pros of doing a Tc99m RBC labeled GI bleed procedure in vivo/In vitro?
absence of blood manipulation -less risk of mix ups
low risk of contamination
What is the procedure for an In Vitro GI bleed procedure?
labeling done outside of body, small sample of blood (1-3ml) withdrawn into syringe containing anticoagulant heparin
let sit for 5 min
add sodium hypochlorite and ACD and. Tc-99m pertechnetate
wait 20 min, then inject into patient
Why is in vitro the preferred labeling method for a GI bleed labeled RBC procedure?
high labeling efficiency, superior imaging quality
What type of collimator are we using for a Tc-99m pertechnetate labeled RBC GI bleed procedure?
low energy, parallel hole collimator
how is the patient positioned under the camera for a labeled RBC GI bleed procedure?
supine, often on a stretcher
What anatomy should be included on a GI bleed labeled RBC procedure?
inferior margin of the liver at the top of the FOV
aka Xiphoid process to bladder should be in view
Tc-99m Sulpfur colloid is better for what type of GI bleed?
an active bleed
Which is the preferred tracer for a GI bleed procedure, Tc-999m sulfur colloid or Tc-99m labeled RBCs?
Tc-99m labeled RBCs
What is the dose for Tc-99m Sulfur colloid for a GI bleed?
7-10 mCI
What types of images are being taken for a Tc-99m sulfur colloid GI bleed procedure? What should be done if the GI bleed is not visualized during these initial images
dynamic for 2-3 min
static images ever 1-2 min for 30 min
should take specified count image of upper abdomen
What are the downsides of using Tc-99m Sulfur colloid for a GI bleed procedure?
has rapid clearance, and only good for active bleed
What is the dose for Tc-99m labled RBCs in a GI bleed?
10-15 mCi
up to 30 mCi
What types of images are we taking for a tc99m sulfur colloid GI bleed procedure? Based on what parameter do we use when determining how long to image a patient?
initial flow images for 32 frames
dynamic images 1/min if bleed not visualized
basically keep imaging until you see something`
Why is Tc99m labled RBCs the prefered method?
allows for imaging up to 36 hrs, possible delayed images
lower radiation dose to liver and spleen
preferred for intermittent bleeding
What are the normal areas of uptake using Tc-99m Labled RBCs in a GI bleed procedure?
great vessels of the abdomen, liver, sometimes spleen depending on how well tagged
general outline of kidneys, bladder, small and large intestines, and genital organs
What are the findings using Tc-99m sulfur colloid GI bleed procedure?
positive bleed within 5 min
focal areas
false positives in renal transplant pt due to accumulated tracer
What are the findings using Tc-99m labled RBCs in a GI bleed procedure?
focal areas gradually become more intense
if first pictures are negative use delayed images
What are some general things to be aware of in a GI bleed procedure?
patient in critical condition, keep an eye on them
smell = likely positive
catheter needs to be moved out of FOV
start imaging THEN inject patient
What is a Meckel Diverticulum? What age is it most commonly found in?
pouch on wall of intestines that is present at birth (congenital) often contains gastric mucosa
children
What are some symptoms of a Meckel Diverticulum?
abdominal pain
bloody stools
What are some complications of Meckel Diverticulum?
peptic ulceration
hemorrhage from acid excretion (rupture/tearing)
What is the patient prep for a Meckel Diverticulum imaging procedure?
NPO for 12 hrs
What is the dose for Meckel Diverticulum?
10-15 mCi of tc-99m pertechnetate
How is the camera positioned over the patient for a Meckel Diverticulum imaging procedure?
xiphoid to bladder