Other virus notes
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
What are common viral targets for molecular detection
Common viral targets for molecular detection:
- Herpes viruses (family Herpesviridae)
o Herpes simplex virus (HSV)
o Epstein-Barr virus (EBV)
o Cytomehalovirus (CMV)
o Varicella-zoster virus (VZV)
- Human papilomavirus (HPV)
- Hepatitis C virus (HCV)
- BK/JC viruses
name the organisms that are common targets for molecular-based laboratory tests, and describe basic characteristics such as the pathophysiology of infection of the following
Virus | Family | Pathophysiology | PCR/NAAT Target(s) |
Cytomegalovirus (CMV) | Herpesviridae | Latent, reactivating infection; severe in immunocompromised | Polymerase (UL54), glycoprotein B (gB) |
Herpes Simplex Virus 1 & 2 (HSV) | Herpesviridae | Latent in nerves; mucocutaneous lesions | Thymidine kinase, DNA polymerase, glycoproteins gb–gg |
Epstein–Barr Virus (EBV) | Herpesviridae | Infectious mononucleosis, latent B-cell infection | EBNA1, LMP-1 genes |
Varicella-Zoster Virus (VZV) | Herpesviridae | Chickenpox & shingles; latent in nerve cells | ORFs in VZV genome (by PCR) |
Hepatitis C Virus (HCV) | Flaviviridae | Chronic hepatitis → cirrhosis, carcinoma | 5′ UTR, core gene (quant/qual PCR) |
Human Papillomavirus (HPV) | Papillomaviridae | Latent infection; some types oncogenic | L1/E1 genes (detection); E6/E7 mRNA (oncogenic activity) |
BK & JC Viruses | Polyomaviridae | Latent renal/CNS infections; BK nephritis | Large T protein gene |
What is herpes simplex virus
Herpes simplex virus (HSV)
- Herpes viruses as a whole are frequent sources of human infection
- There are two types of HSV: HSV type 1 (HSV-1) and HSV type 2 (HSV-2)
- HSV-1 mainly causes cold sores or fever blisters
o Also accounts for 5-10% of encephalitis cases
- HSV-2 mainly causes genital sores but can cause mouth sores
o Can cause encephalitis in neonates and aseptic meningitis in older individuals
- In the more serious infections, these are typically due to reactivation of disease or exist in immunocompromised individuals
- Transmitted via saliva, unprotected sex, or skin-to-skin contact
How is HSV detected
Detection
- Originally detected by viral culture, antigen, and antibody tests
o Viral culture was not sensitive enough
o Some antibodies are not detectable until up to 3 months after the initial infection
- PCR and qPCR tests target the dsDNA virus
o Type-specific testing is preferred
- Sample types can include genital swabs, blood, urine, tears, amniotic fluid, lavages, and CSF
What is the Epstein-Barr virus
Epstein-Barr virus
- EBV is one of the most common human viruses
o Most people have been infected with EBV at some point during their lifetime by the age of 35-40 years; if/when infected as a child you can be asymptomatic or have a very brief infection
- Causes mononucleosis and remains dormant in your body after the infection
o Lives in its inactive state in the throat, blood, and immune system
o Can be reactivated
- Symptoms of an active infection include fatigue, fever, inflamed throat, swollen lymph nodes, enlarged spleen and liver, and rash
- Transmitted via saliva, blood, and semen
How is the Epstein-Barr virus detected
Detection
- Traditionally, EBV detection was performed using antigen tests
- In the mid 80s, EBV DNA repeat sequences became a good target for in situ hybridization and southern blot analysis
o Each genome can contain up to 20 terminal repeat sequences
- PCR is now used for detecting EBV, including qPCR
o qPCR allows for measuring the viral load in a sample
- Blood, body fluid, or even tissue samples can be used
What is the Cytomegalovirus?
Cytomegalovirus
- CMV is another common herpes virus that can infect individuals at any age
o Healthy individuals usually prevent the virus from causing infection
o CMV can go dormant and reactivate later
- Mild symptoms can include fever, sore throat, fatigue, and swollen glands
o Occasionally CMV can cause mononucleosis or hepatitis
- Congenital CMV is seen in babies that are bore with the infection and can affect the brain, liver, spleen, lung, and cause hearing loss
- Virus is transmitted via body fluids, including breast milk
How is the Cytomegalovirus detected
Detection
- CMV is a dsDNA virus
- DNA can be targeted via PCR or qPCR
- The key to CMV detection is to detect CMV levels above the “normal amount” found in individuals that have been previously exposed to CMV
o This means no PCR amplification for normal amounts present in plasma
- Gene targets = CMV polymerase (UL54) or glycoprotein B (gB) gene
- Sample types for molecular detection include cell-free plasma or other body fluids such as blood, saliva, or urine (preferred in newborns)
What is the Varicella zoster virus
Varicella zoster virus
- VZV is the causative agent of chickenpox and shingles
o Chickenpox (Varicella) usually infects children, with the rash being the first sign of infection
o Shingles (herpes zoster) is a painful rash that usually presents as a single stripe
- Varicella is very contagious and can be spread by direct contact or by inhalation of aerosols from vesicular fluid of skin lesions
- The average incubation period for VZV is 14 to 16 days after exposure
- A mild fever and malaise may occur 1 to 2 days before the rash presents, particularly in adults
- VZV is neurotropic and remains latent in nerve cells
o Can be reactivated years after primary infection to result in shingles
How is the Varicella zoster virus detected
Detection
- Enzyme-linked immunosorbent assays (ELISA) and PCR tests have been used for detecting VZV
- VZV is a dsDNA virus
- Sample types include swabs of vesicular fluid, maculopapular lesions, crusts from lesions, or plasma
- Molecular tests can include both qualitative and quantitative PCR test
o Most quantitative PCR kits include internal controls to rule out false-negatives due to the presence of inhibitors
What is the Human papillomavirus (HPV)
Human papillomavirus (HPV)
- HPV is a dsDNA virus that is recognized as oncogenic
- There are over 200 HPV types that can be further broken down into five HPV genotype groups
- 40 types are transmitted sexually; 12-15 of these have strong association with cervical cancer and are considered high-risk HPV types
- High-risk HPV types are 16,18, 31, 33, 35, 39, 45, 51, 56, 58, 59, 68, 73, & 82*
- HPV 16 and 18 are responsible for most HPV-related cancers
- HPV 6 and 11 cause genital warts and are not carcinogenic
How is Human papillomavirus (HPV) detected
Detection
- HPV is difficult to culture in the laboratory, so molecular testing is often preferred
- Molecular tests include hybridization or amplification methods
- HPV expresses E1 through E8 genes shortly after host infection
o E6 and E7 are overexpressed in oncogenic genotypes and are involved in cellular transformation to cervical cancer
o Measurement of E6 and E7 mRNA expression in cells can be used to identify cells that are precancerous
- Panels are usually designed to detect common HPV types, especially high-risk HPVs
- What group includes these high-risk HPVs? alpha
What cancers are caused by HPV
Cancers caused by HPV
- According to the CDC, 9 out of 10 cervical cancers are caused by HPV
- HPV cervical screening is routinely performed in asymptomatic patients
- Ex: back of throat, cervical, anus, vulva, penis, and vagina cancer
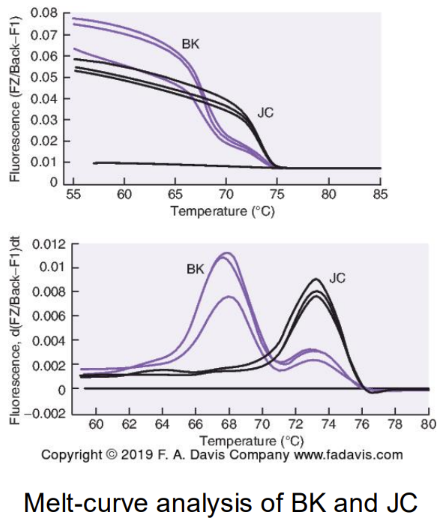
What is the BK/JC virus
BK/JC viruses
- BK and JC are dsDNA viruses that fall under human polyomaviruses
- Most human polyoma disease is acquired during childhood with minor symptoms
o Symptoms in children include respiratory problems and sometimes cystitis (bladder infection)
- Infection in adults is typically subclinical i.e. not severe enough to present obvious symptoms of infection
- The viruses can remain latent until the immune system is suppressed enough for the virus to reactivate and become dangerous
- BK is urotheliotropic and reactivation causes a form of interstitial nephritis
- JC is neurotropic and has been known to cross the blood brain barrier
How is the BK/JC virus detected
Detection
- Transmission of these viruses is not well known; studies suggest the feco-oral and respiratory routes, as well as through other body fluids, including blood and semen
- Molecular detection of BK can be done using urine or blood
- JC molecular detection includes analysis of CSF and less frequently, brain biopsies
- Gene target for both BK and JC is the large T protein, although needs to be very specific
o BK, JC, and SV40 (primate counterpart) share sequence homology
- qPCR and multiplex PCR assays have been developed for successful amplification and detection
Classify organisms by their common viral families relevant to molecular diagnostics, including Herpesviridae, Papillomaviridae, and Polyomaviridae
Family | Examples | Genome Type |
Herpesviridae | HSV, VZV, CMV, EBV | dsDNA |
Papillomaviridae | HPV | dsDNA |
Polyomaviridae | BK, JC | dsDNA |
Flaviviridae | HCV | ssRNA |
Explain the necessity of HCV genotyping and recall which genotypes respond to treatment
HCV Genotyping & Treatment Relevance
Six genotypes (1–6) and > 50 subtypes exist【5 p. 321–322】.
Genotypes 2 & 3 respond best to antiviral therapy; Genotype 1 is more resistant.
Genotyping guides drug choice and duration by PCR RFLP, reverse hybridization, or sequencing.
What are the HPV genotype groups
HPV Genotype Groups
Five evolutionary groups: α, β, γ, μ, ν【5 p. 322】
α-HPVs infect mucosa and include high-risk oncogenic types (16, 18, 31, 33, 35, 39, 45, 51, 56, 58, 59, 68, 73, 82).
β-HPVs infect skin; linked to nonmelanoma skin cancer.
γ, μ, ν groups usually cause benign lesions.
What is viral hepatitis
Viral hepatitis
- Hepatitis is an inflammation of the liver most often cause by hepatitis A, B, or C virus
- Each viral infection can produce similar symptoms, but each have different routes of transmission and infection
- Hepatitis A and B both have vaccines and infections have continuously decreased over the yrs
- There is no vaccine for HCV and the incidence of hepatitis C infection has doubled since 2013
- HCV is an enveloped, ssRNA virus that is transmitted parenterally i.e. introduced into the body through piercing or puncturing the skin
o Considered a bloodborne pathogen
How is viral hepatitis detected
Detection
- Acute HCV infection is often asymptomatic and can go undetected
- It is not usually until the chronic phases of hepatitis that patients get tested
- Several NAATs have been developed for the detection and quantification of HCV, most based on RT-PCR
o Qualitative tests can help determine active infection (Presence/absence)
o Quantitative tests determine viral load and monitor response to antiviral therapy
- HCV genotypes can be determined by analyzing the 5’ UTR or the core of the genome
- Genotyping is important to determine treatment
Interpret molecular microbiology results, including identification of gene target and evaluation of control validity
Interpretation & Control Evaluation
HPV L1 assays may miss integrated virus (genomic loss) → false negative.
Multiplex PCRs can show uneven amplification of mixed HPV types【5 p. 323】.
Include internal controls to monitor for amplification inhibition and assay integrity.
Quantitative PCR (viral load) used for CMV, EBV, HCV monitoring; interpret values in clinical context.