heat and hydration
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
as temperature increases
the temperature gradient between air and the body decreases
when Tbody>Tenvion
we lose heat via radiation
typical body temp
37c - 98.6F
temp over 26 C
the body absorbs heat, heat loss is from evaporation only
heat is generated by ____ sources
endogenous sources
muscle activity and metabolism
when an athlete exercises in a hot envionement
they sweat to dissipate heat
an increase in humidity
will decrease the vapour gradient, therefore there will be less evaporation
increased body temperature due to less evaporation of sweat
exertional heat stroke
occurs when the patient presents with exertion related hyperthermia and associated central nervous system disturbance or evidence of other end organ system damage
exertion related hyperthermia temp
core body temperature greater than 40c
individual and stopping sweating
during EHS they may stop sweating but this is unreliable
if they stop sweating this is bad because it means they’re trying to move blood around organs and cool off internally
experincing during ehs
dizziness, weakness nausea, fast pulse and resp , mental confusion
may collapse and become unconscious because body is shutting down
heat exhaustion is characterized by
an inability to continue functioning in the heat without evidence supporting the diagnosis of EHS
signs and symptoms are variable and may inc
heavy sweating w/ pale, moist, cool skin
headache wekaness, dizziness, nausea (with/w/0 vomiting)
heat exhaustion non severe primary signs
concious
alert
temp less than 40c
systolic >100mmHg
Secondary signs of non severe (heat exhaustion)
sweating
pale, moist, cool skin
cramping
nausea
primary signs — heat stroke (Severe)
unconsious or decreased mental status
temp greater than 40c
systolic < 100mmHg
secondary signs of severe heat stroke
no sweat
hot, dry skin
weakness/flaccid
nausea
management of heat injury - mild
patient: alert w appropriate behaviour, near-normal/stable vital signs and able to drink fluids
Care
on side line for up to one hour with up to 2 L fluid
rest in shade with reassessment every 5-10 min
does not improve? hospital
heat stroke management severe
patient: mental status changes, amnesia, syncope, seizure, unable to drink, unstable, high temp
Care
cool first transport second
agressive cooling within first ½ hour
remove gear, ice/water submersion (best) or on core starting w/ armpits and groin
rehydration
frequent vital signs and mental status assessment
evac to emergency
life threatening
intrinsic risk factors EHS *
lack of acclimatization
fever
overweight/obesity
dehydration
recent alcohol use
sunburn (can dehydrate ppl)
extrinsic risk factors EHS *
• Hot, humid environment
• Exercise intensity
• Inappropriate work-to-rest ratios
• Equipment/clothing
• Education
• athletes,
• Coaches and medical staff
• Lack of emergency plans to identify and treat EHS
• Lack of proper infrastructure (heat acclimatization)
• Access to fluids
• Access to preventative cooling strategies
combatting heat injuries concepts
get an accurate temp
get them cool
allow acclimatization
train coaches and players on signs
keep them hydrated
getting an accurate temperature
Know what we’re dealing with
devices to measure core body temperature via direct contact with the forehead or radiation from the ear canal may not be accurate and are potentially dangerous (devices typically underestimate the temp)
its ok to assume EHS if the patient is displaying signs even if the temp reading is slightly lower
keep them cool/get them cool
cold water and ice water immersion provide superior cooling rates (temp dec 5-14 times faster than packing with ice)
c100% effective in preventing death
amost ehs deaths
most ehs deaths occur among non-acclimatized players during the initial 3 days of summer
acclimatization improves cooling through
increased sweating (evaporation)
less effective in high humidity
may need to add electrolytes if sweating a lot because we’re losing salt
acclimatization occurs by
progressive and prolonged elevation of the body core temperature
conditioned athletes acclimatize
after 4-7 progressive exercise sessions of 1-4 hours total duration each over a period of 1-2 week
Four high-intensity intermittent acclimation sessions, in a 10-day period, is sufficient to improve games-type exercise capacity.
living in a hot environment
without exercising in the environment provides little acclimatization
bottom lime acclimatization
physiological adaptations will occur during 1-2 weeks of exercise heat exposure
these include
reduced rectal temp, cardiovascular strain, and perceived exertion as well as inc plasma volume
the medical team (heat and hydration)
must educate staff and players on signs and symptoms and ensure EAPs are completed, understood and followed
voice of reason
most ehs deaths in football
occur during practice
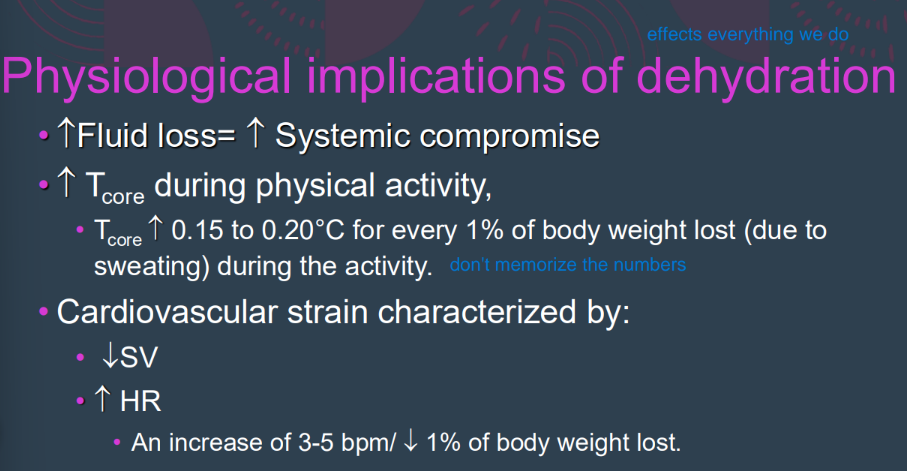
hypohydrated
more than 50% of athletes arrive at training sessions hypohydrated
and usually only replave 2/3 of sweat loss while training
excessive water deficit
The goal of drinking during exercise is to prevent excessive (>2% body weight loss from water deficit) dehydration and excessive changes in electrolyte balance to avert compromised performance
greater than 2% means we’re probably dehydrated
facctors that contribute to the risk of hypohydration (extrinsic)*
availability of fluids
exercise structure
sport specific factors
env conditions
risk of hypohydration (Intrinsic factors) *
sex
thirst drive
acclimatization status
body size and comp
tracking hydration changes
Acute hydration changes can be measured by taking nude body mass before and after exercise (go pee first)
Check urine concentration/colour in the morning
thirst: first morning thise is correlated w/ hypohydration
hydration status can be reliably estimated
using as few as three consecutive days of first morning euhydrated body weights, measured after voiding
if bm decreases more than 2% the individual is drinking too little, if it increases individual is drinking too much
thirsty at rest
means we’re already dehydrated
primary goal of rehydration
the primary goal is the immediate return of physiological function
rehydration points
compensate for urine losses by drinking (get what lost and then 50% over that)
when recovery time is greater than 12 hrs athlete can eat and drink
a balanced diet that provides 2500-3000 kcal will provide 1 litre of water per day from food alone so if they don’t wanna drink they can eat watery food (melons)
pre exercise hydration
start in a state of euhydration
hydration during exercise
try to maintain water levels
use CHO drink for periods greater than 1 hr
post exericse dluid
correct fluid loss ASAP
much of this through general nutrition and H20, may need to add CHO and electrolytes
Hyponatremia
An athlete who exercises for more than 4 hours and hydrates excessively (well beyond
sweat loss) only with water or low-solute beverages may be susceptible to a relatively rare
condition known as hyponatremia (also known as water intoxication)