Radiology Block 1 (Lectures 1-9)
1/152
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
153 Terms
Radiology 1: Introduction to Radiography
Radiology 1: Introduction to Radiography
What are the 2 Key Factors in Good Radiography (Taking the Radiographs)
1. Sedation (Most Important)
2. Positioning Aids

What are the 4 Key Factors in Good Radiology (Interpreting the Radiographs)
1. Good Quality Radiographs
2. 2 Large monitors, not the x-ray system monitor
3. Know Normal Anatomy
4. Systemic Approach
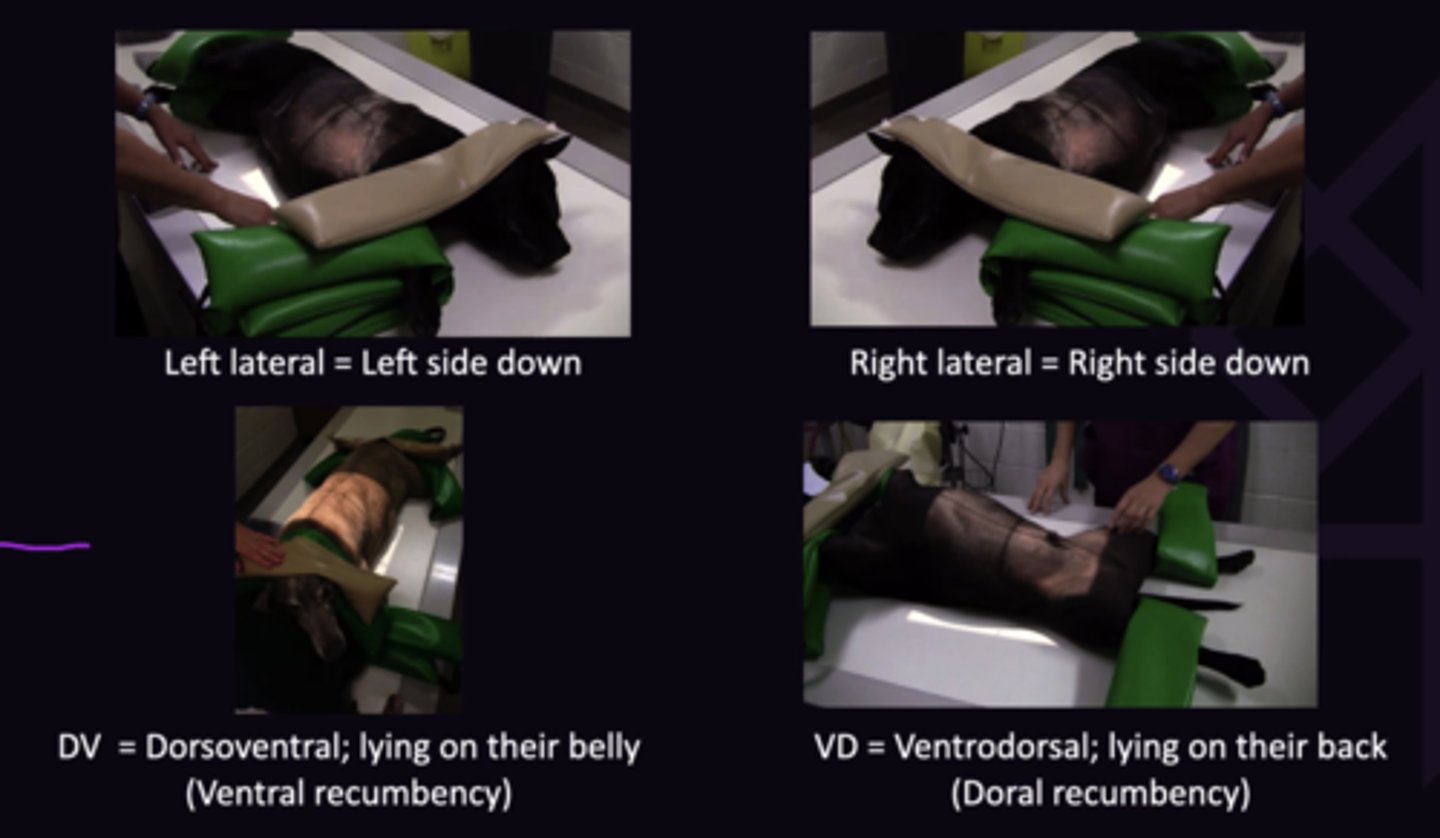
Describe the Following Thorax and Abdomen Radiograph Views:
1. Dorsoventral View
2. Ventrodorsal View
3. Right Lateral
4. Left Lateral
1. Lying on their Belly (Ventral Recumbency)
2. Lying on Their Back (Dorsal Recumbency)
3. Right Side Down
4. Left Side Down
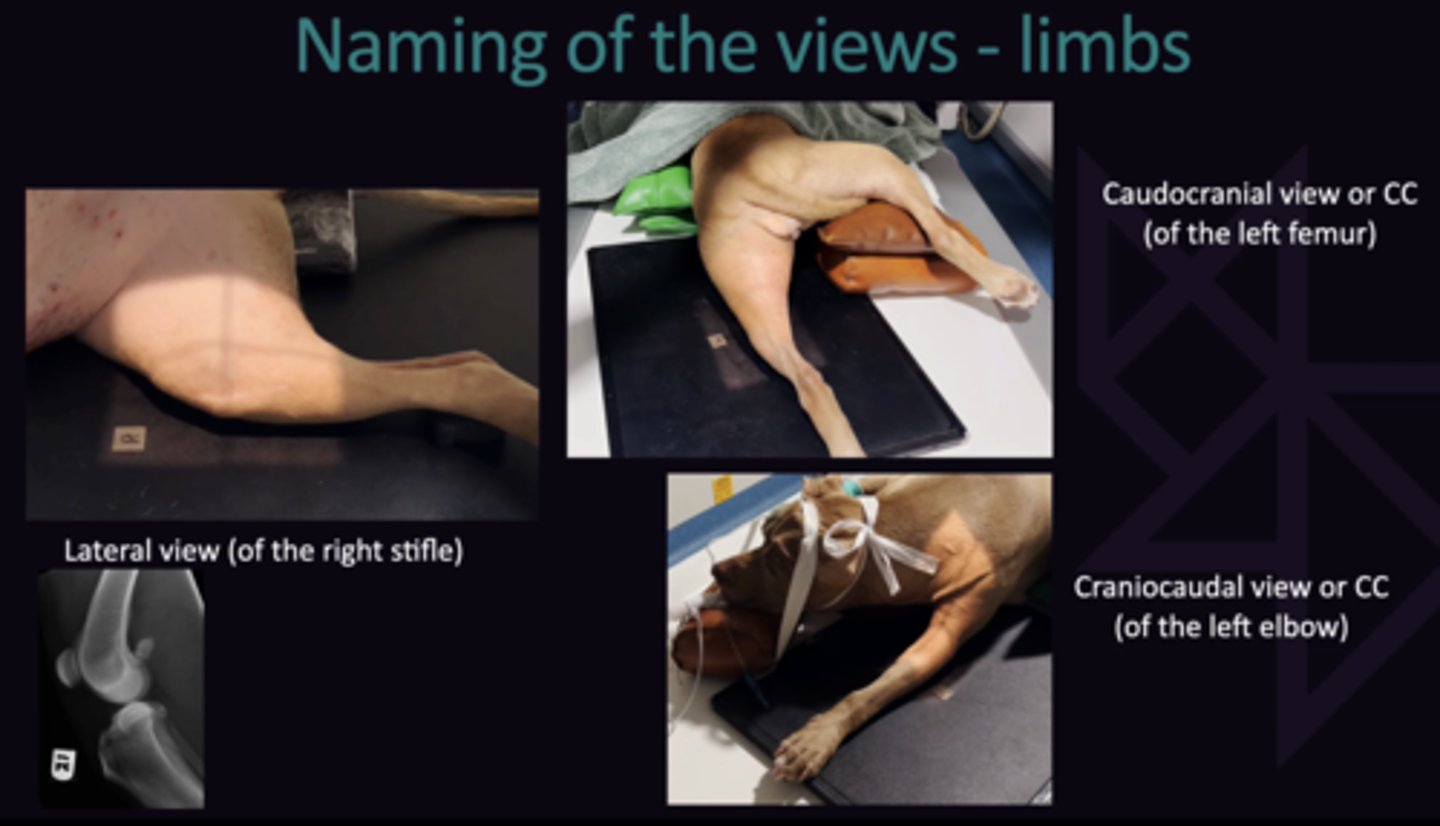
Describe the Following Limb Radiograph Views:
1. Lateral View
2. Caudocranial View (CC View)
3. Craniocaudal View (CC View)
1. In Theory "Mediolateral/Lateromedial View), However doesn't make a difference. Nomenclature relevant for whole limb
2. X-Ray hits caudal surface of leg first, then cranial surface
3. X-Ray hits cranial surface of leg first, then caudal surface
Describe the Difference Between a Dorsopalmar and CC Radiograph on the Thoracic Limb
Craniocaudal View: Proximal to the antebrachiocarpal joint
Dorsopalmar View: Distal to the antebrachiocarpal joint
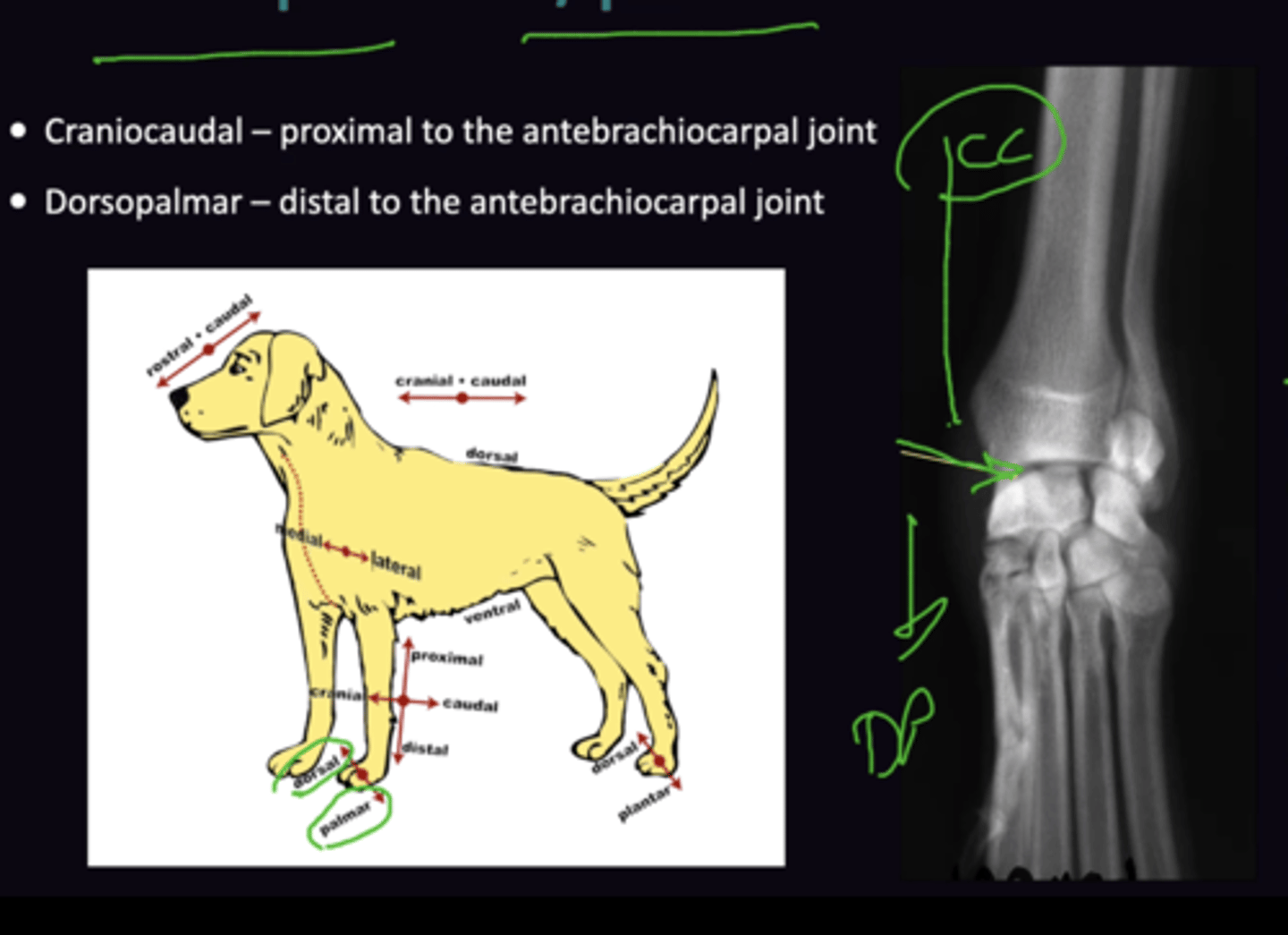
Describe the Difference Between a Dorsoplantar and CC Radiograph on the Pelvic Limb
Craniocaudal View: Proximal to tarsocrural joint
Dorsoplantar View: Distal to tarsocrural joint
List the 13 Steps in Taking a Radiograph
1. Patient Preparation for Abdomen
2. Plan the procedure
3. Sedate/anaesthetise
4. Position the patient
5. Collimate the beam
6. Place the left/right marker
7. Measure the thickness
8. Set the exposure factors
9. Check for safety
10. Take the exposure (press the button)
11. Finalise radiographs on the digital X-ray system
12. Interpret the radiographic study (Radiology)
13. Enter thee conclusions into the patient record
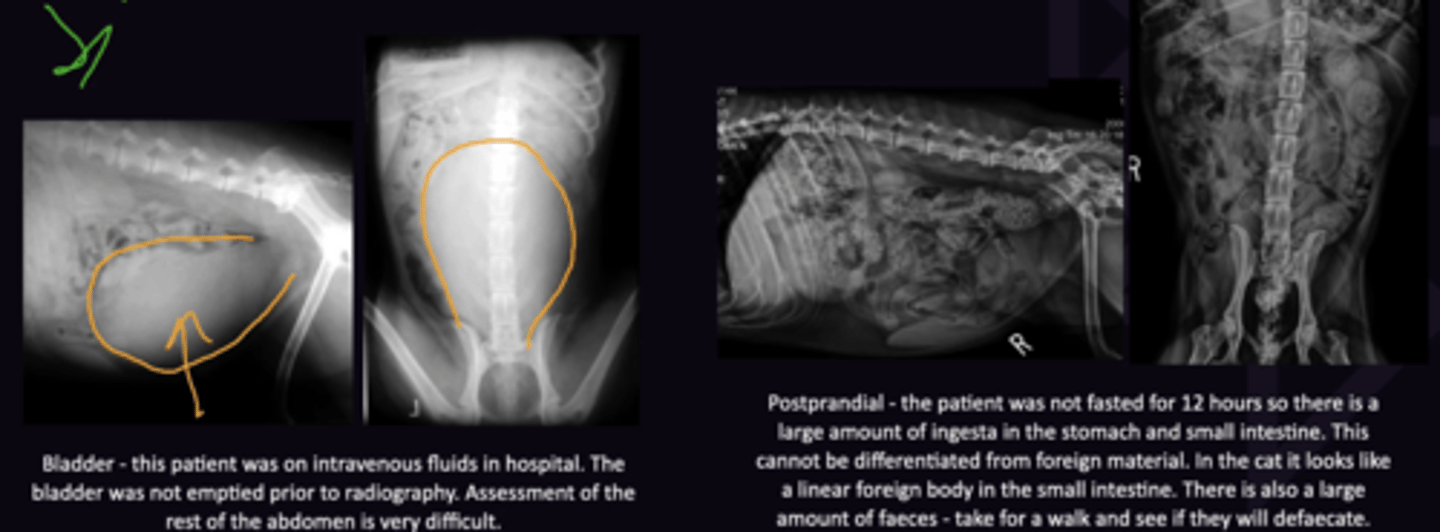
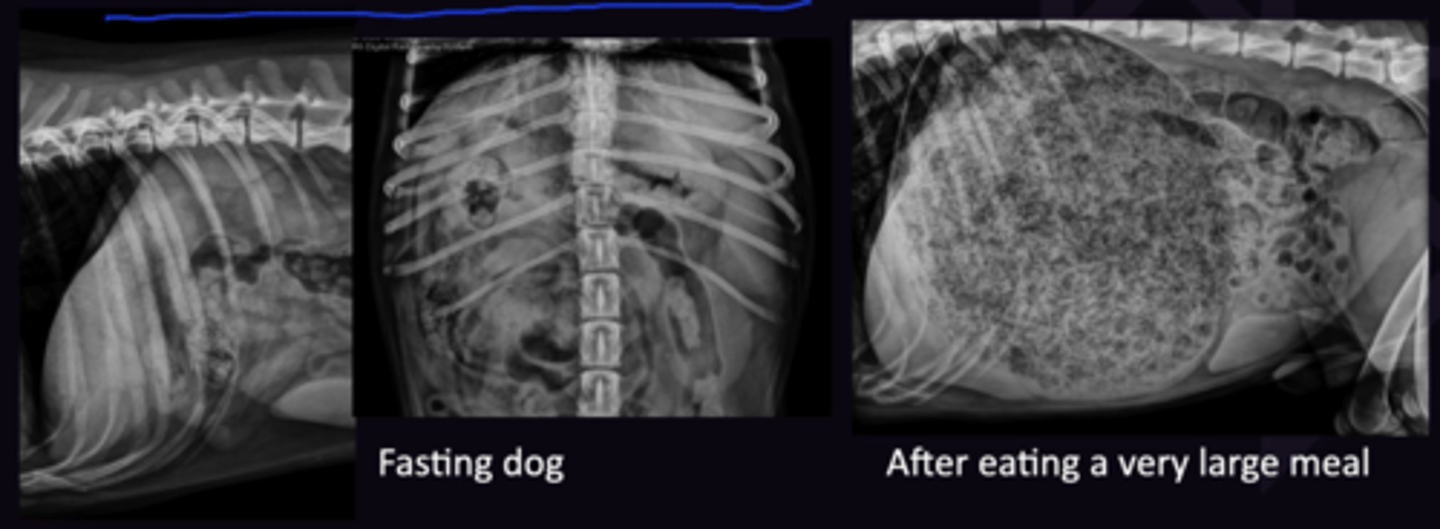
Describe the Patient Preparation for Abdomen Radiographs
Fast: At Least 12 Hours before radiograph (Faecal Material/Food Superimpose and form poor image)
Bladder: Empty just before radiography (Full Bladder Pushes/squishes) other Organs
Describe the Planning of Radiographic Procedures
Write a list of the order the radiographs will be taken
e.g. Left Laterals → Roll → Ventrodorsal → Roll → Right Laterals

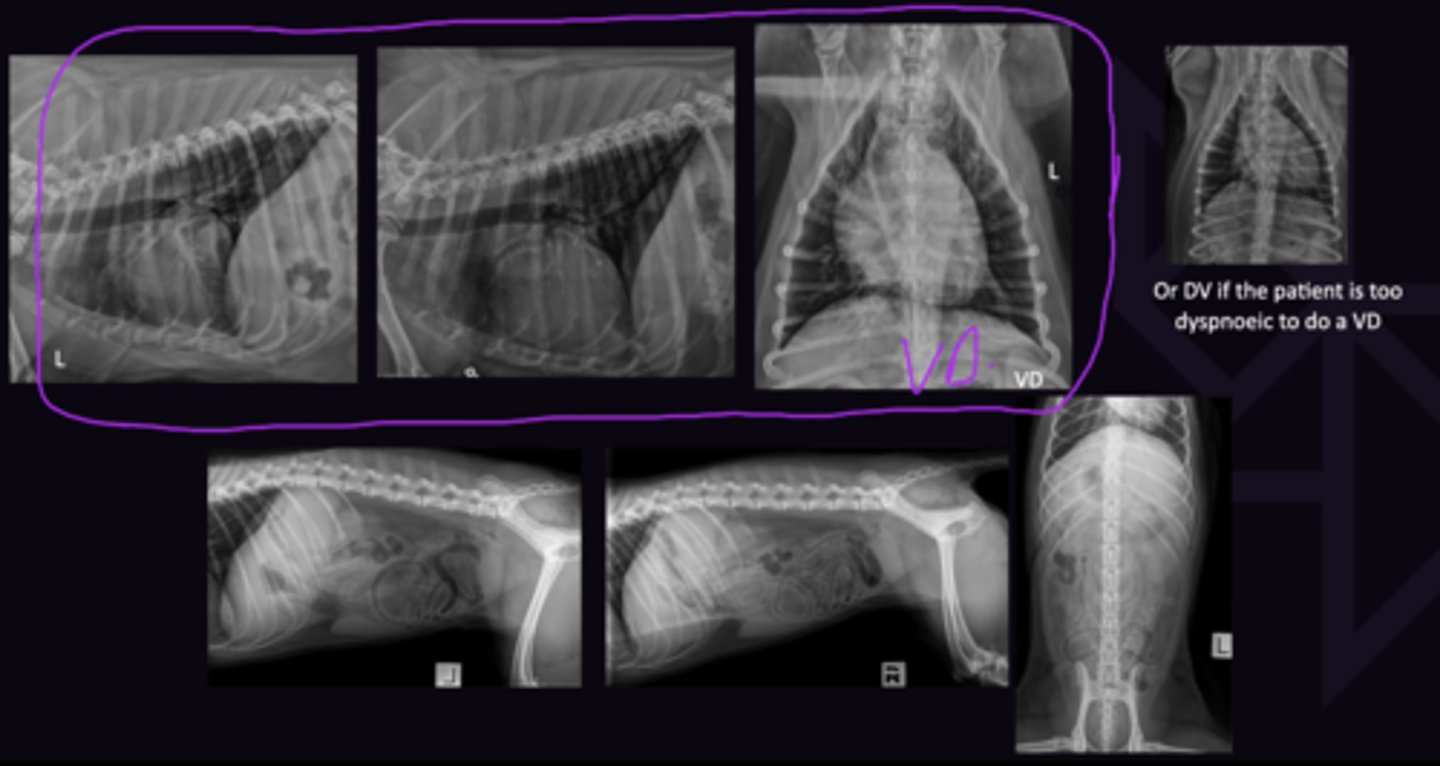
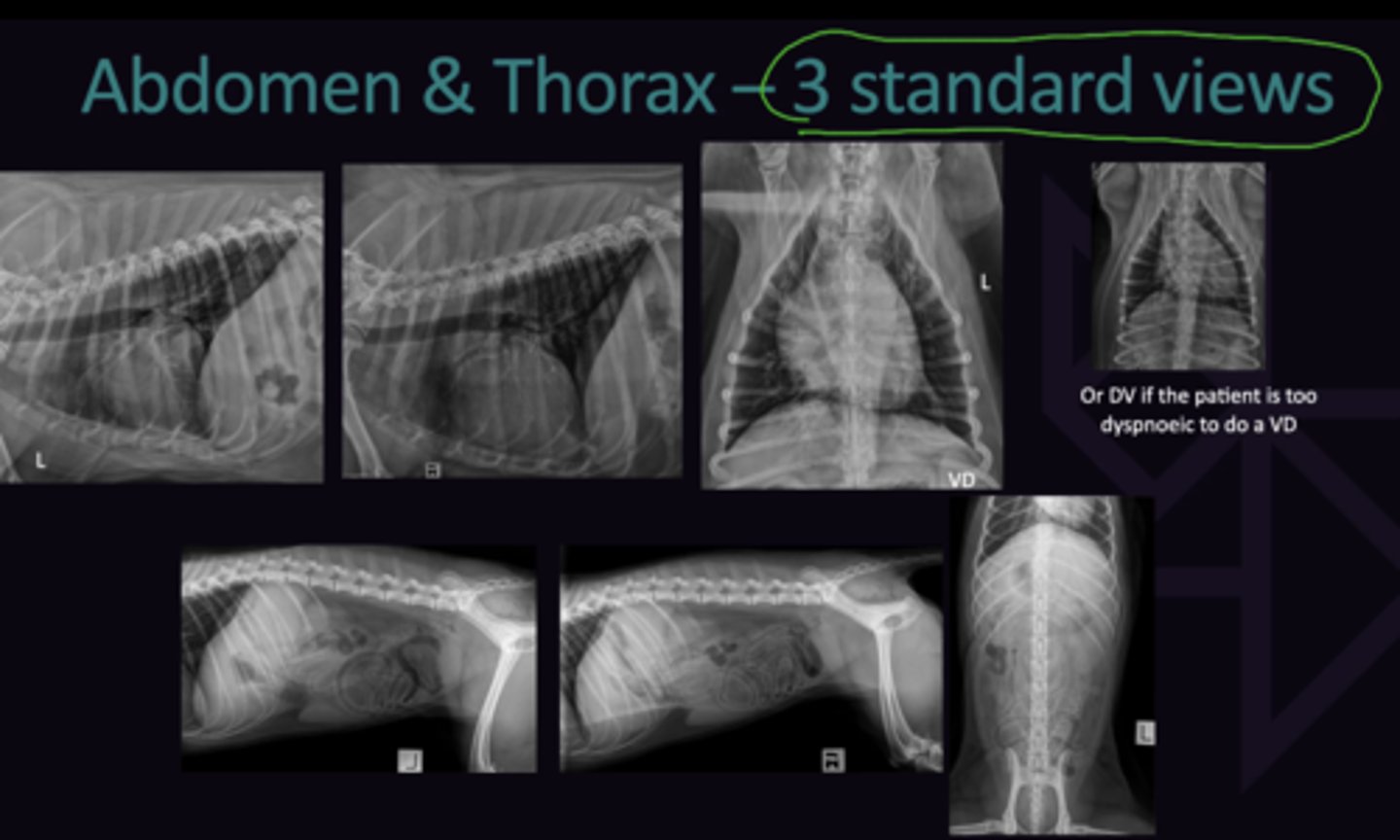
Describe the Standard Radiograph Views for the following
1. Abdomen
2. Thorax
3. Other Areas (Limbs)
1. Left Lateral, Right Lateral, Ventrodorsal Views
2. Left Lateral, right Lateral, Ventrodorsal Views
3. 2 Views of each limb. Always take radiographs of other limb for comparison.
Describe the Importance of Sedation/Aestheticization in Radiography in terms of:
1. What Lack of Adequate Sedation Leads to
2. When Holding of Patient for Radiography is Warranted
1. a. Holding the Patient: Exposes personnel to radiation
b. Poor Quality Radiographs: Risks Misdiagnosis
2. The Patient is to sick (Should never be due to economic or social reasons)
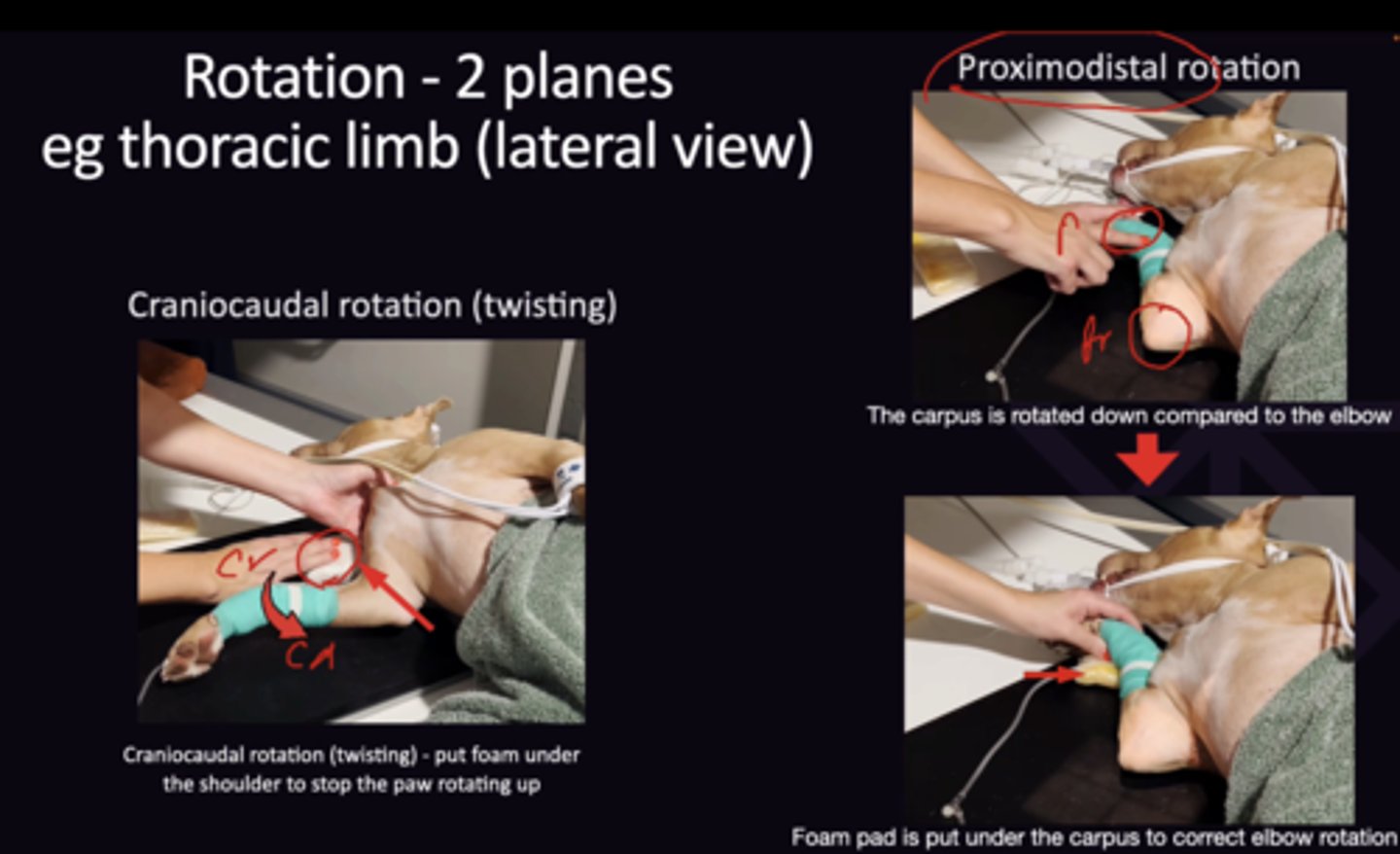
Describe Positioning of the Patient for Radiography in Terms of:
1. Positioning Aids
2. Craniocaudal Rotation Limb
3. Proximodistal Rotation Limb
4. Craniocaudal Rotation Thorax/Abdomen
5. Dorsoventral Rotation Thorax/Abdomen
1. Foam Wedges, Sand Bags, Tape
2. Put Foam under the shoulder to stop the paw rotating up
3. The carpus and elbow are rotated the same
4. Check that the spine is the same distance from the table all the way along
5. Check spine and sternum are the same distance from the table
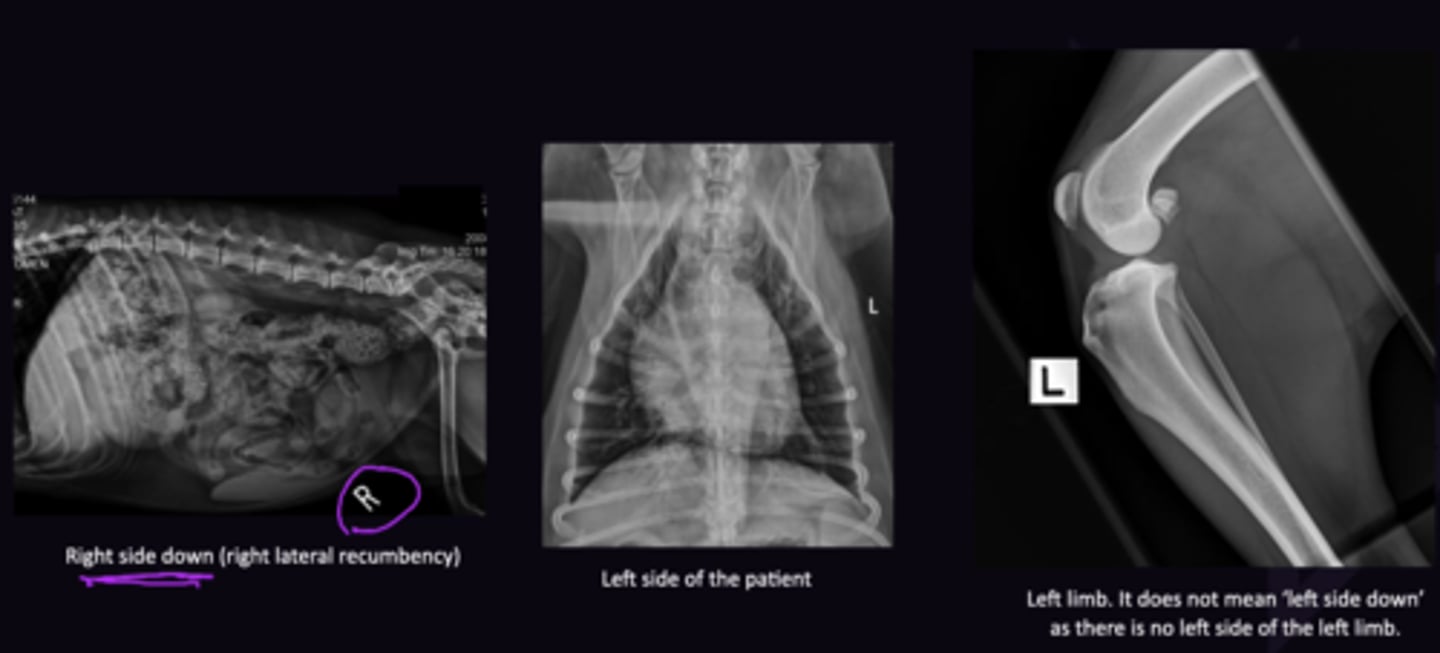
Describe What the Left + Right Markers on Radiographs Indicate in terms of:
1. "R" Marker on a Lateral Recumbency Radiograph of the Thorax + Abdomen
2. "L" Marker on a VD Radiograph
3. "L" Marker on a Limb
1. Right side down
2. Left side of patient
3. Left limb (Does NOT mean left side down)
On What Aspect is the Marker Placed for Limbs for:
1. Lateral Radiograph of Limb
2. CC View of Limb
1. Marker is put on the dorsal/cranial aspect of the limb
2. Marker is put on the lateral aspect of the limb

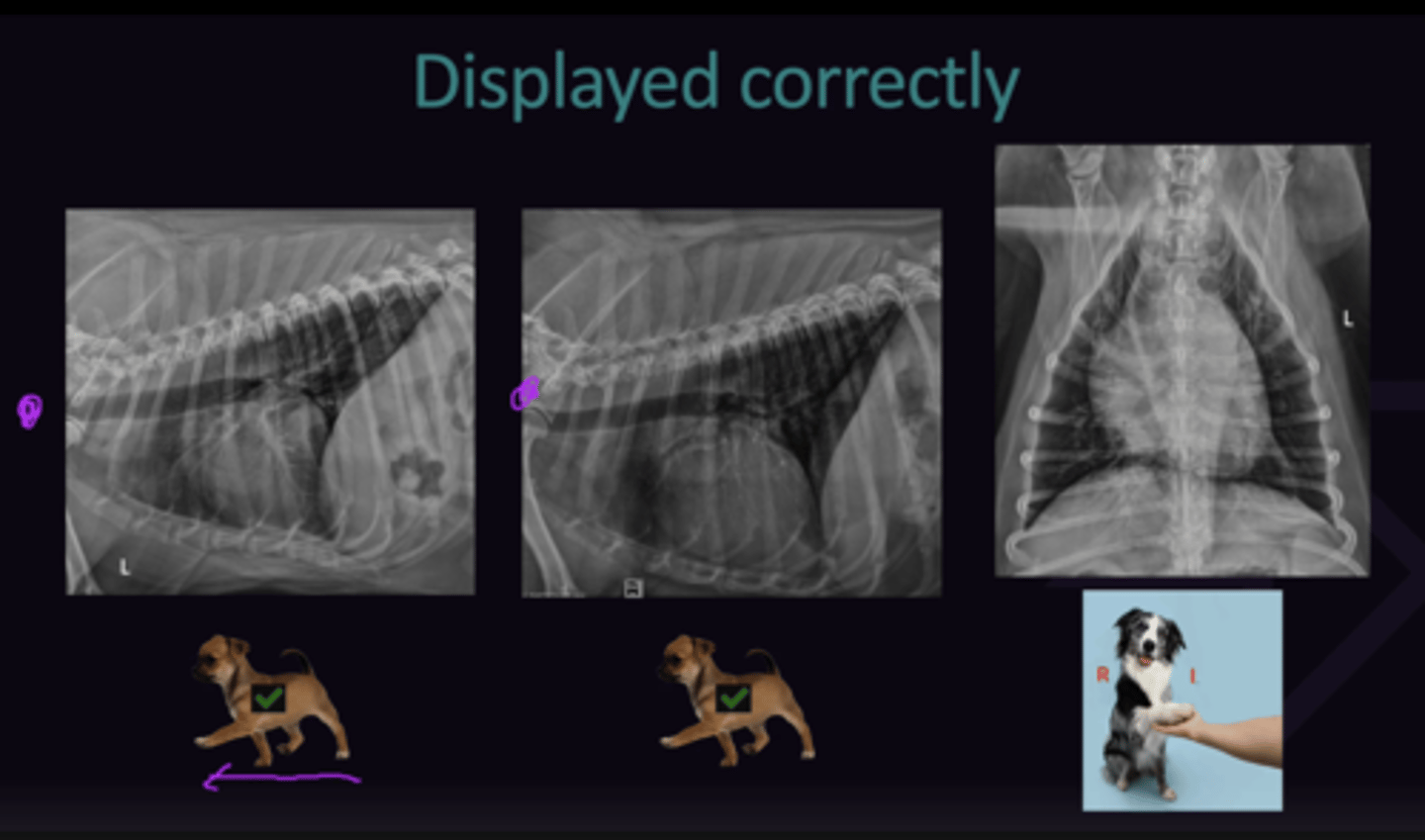
Describe the Correct Viewing of Radiographs in Terms of:
1. Left + Right Side Down (Left + Right Lateral Radiographs of Skull, Thorax, Abdomen, Limbs)
1. For both Images, Cranial Aspect of patient on Left of Monitor, Caudal Aspect of patient on Right of Monitor
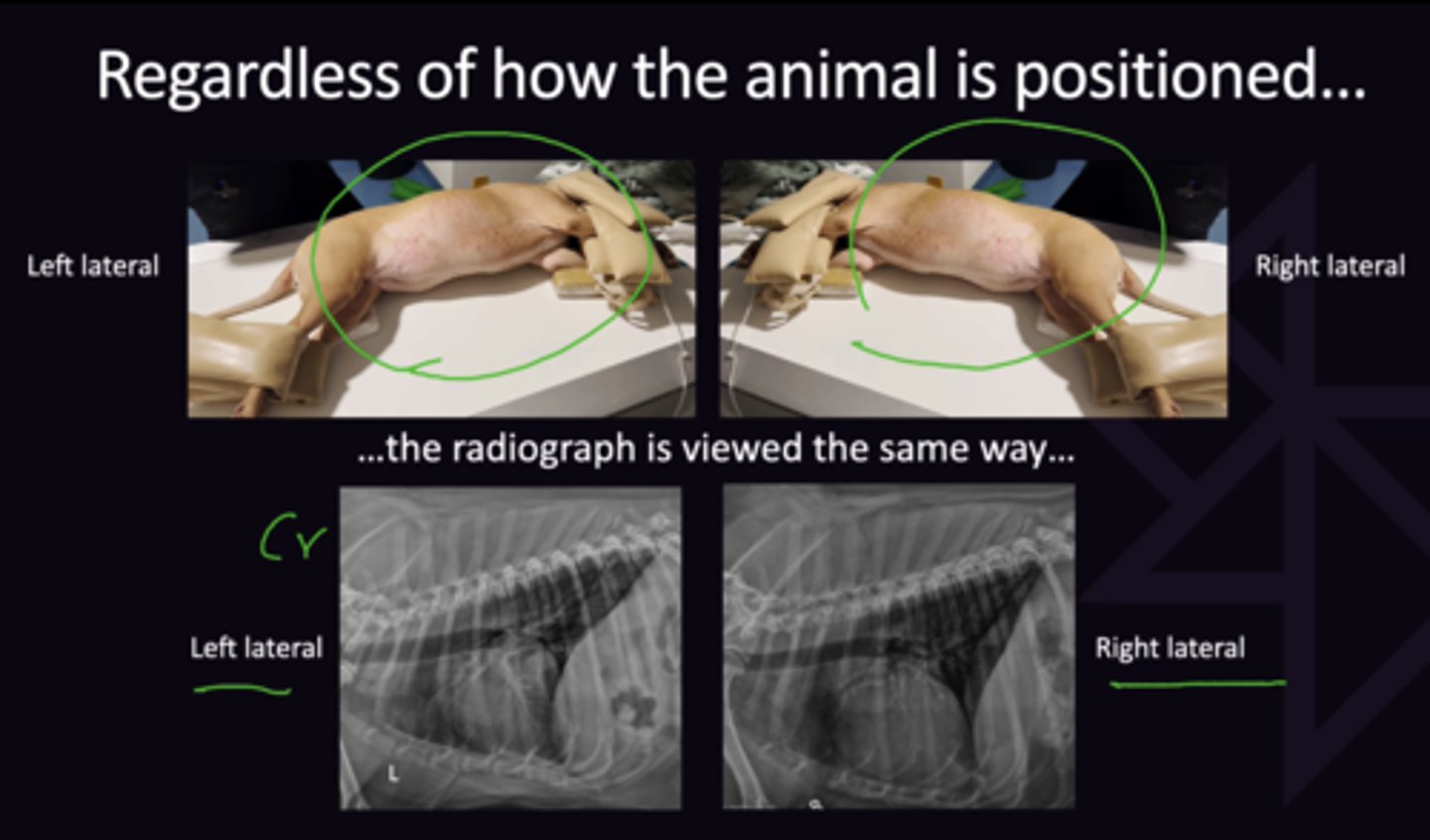
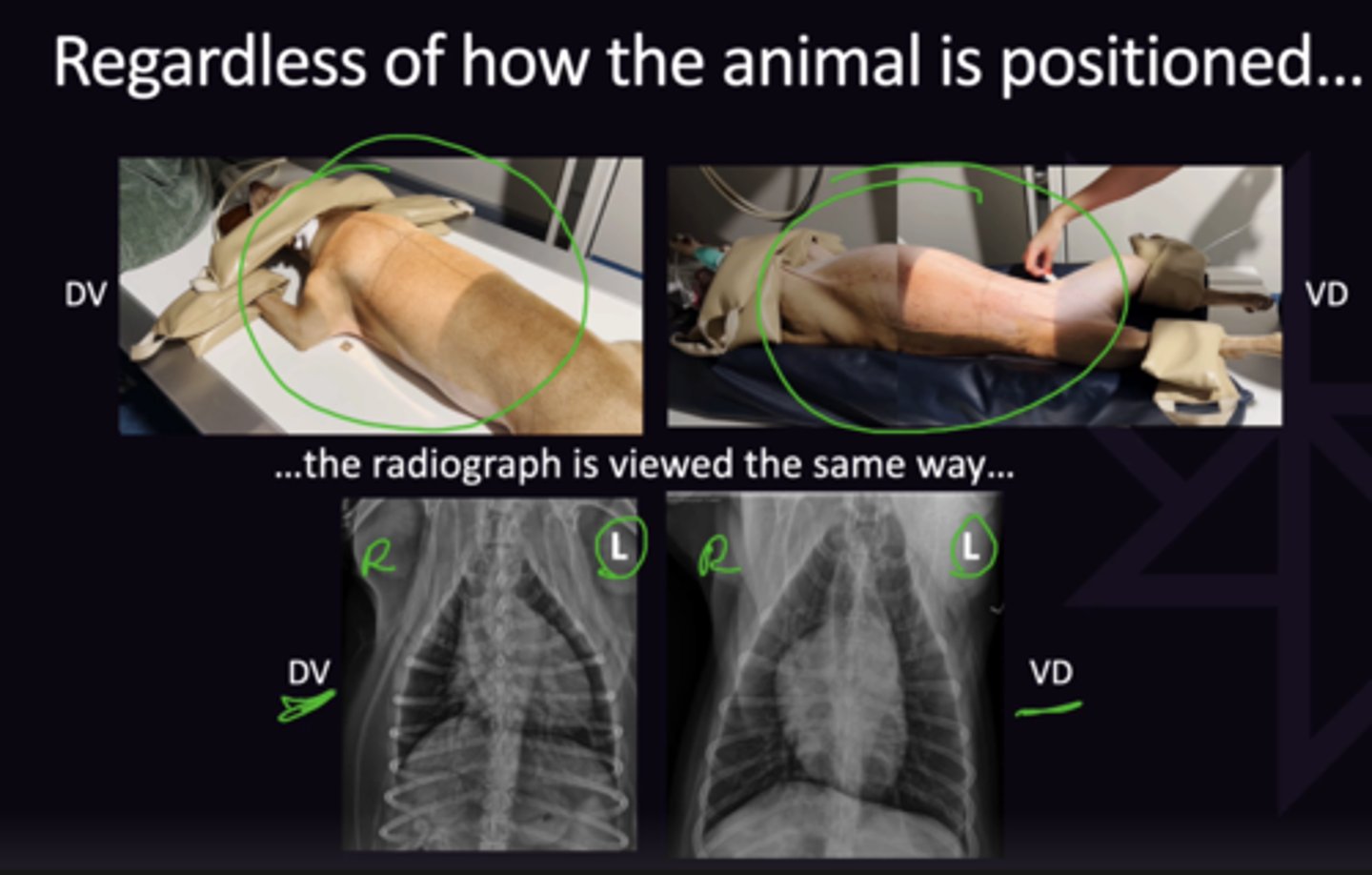
Describe the Correct Viewing of Radiographs in Terms of:
1. DV + VD Radiographs
1. for Both Images, View as if in VD (Left side of patient on right of monitor, right side of patient on left of monitor
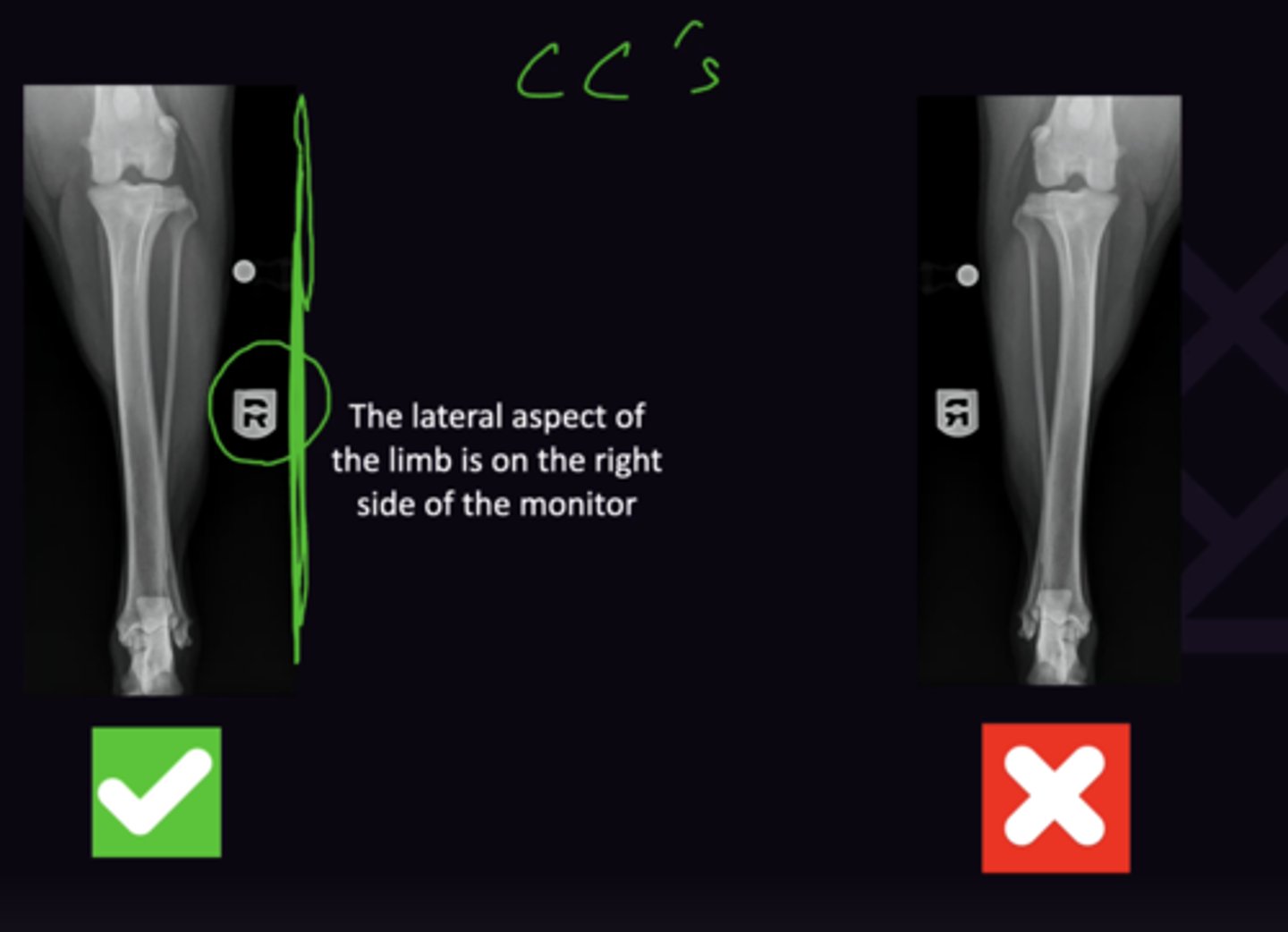
Describe the Correct Viewing of Radiographs in Terms of:
1. CC Radiographs
1. Lateral aspect of limb always on the right side of the monitor (marker should always be on the right hand side of the monitor)
Radiology 2: Introduction to Radiology
Radiology 2: Introduction to Radiology
What are the 3 Factors that Make a Good Radiographic Study
1. Good Algorithm (Digital X-ray system)
2. Good Radiography (Taking of radiographs)
3. Good Radiology (Interpreting the radiographs)
What are the 4 Factors of Good Radiology
1. Good Quality radiographs
2. 2 Large Monitors (Not x-ray system monitor)
3. Know normal anatomy
4. Systematic approach
For which Anatomical Structures are Radiographic Anatomy Resources needed for?
Limbs: It is not possible to know every bony prominence and physis for all species, breeds, and ages
Describe the Systematic Approach to Radiology in term of:
1. Definition
2. What Must be Done Before Moving to Next Organ
1. Checklist of things to look at so nothing is forgotten, done the same way every time. Different checklists for abdomen, thorax, limbs ect.
2. Look at the organ on all views before moving on
Describe the Following 3 Pitfalls of Interpretations that a Systematic Approach Avoids:
1. Satisfaction of Search
2. Distracted from a Systematic Approach
3. Didn't Intend to Use a Systematic Approach From the Start
1. Discovery of a lesion that answers the clinical question that prompted the radiographic examination, thereby distracting the evaluator
2. The presence of an obvious abnormality that distracts the evaluator from systematic evaluation of the rest of the radiograph
3. Tunnel vision, which is a preconception of what will be found, so that when the preconception is confirmed, viewing of the radiograph ends
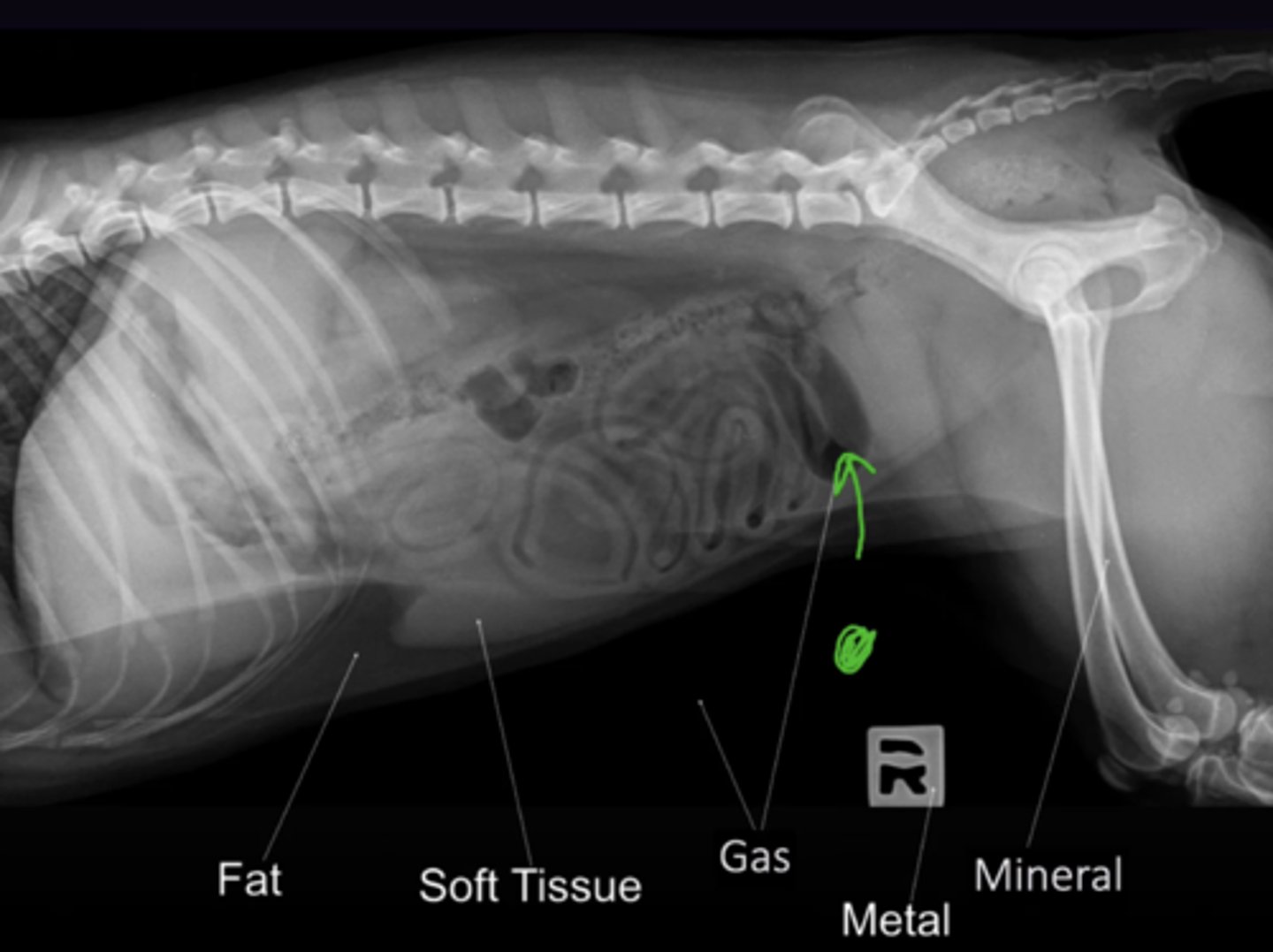
Describe the Following 5 Radiographic Opacities:
1. Gas
2. Fat
3. Soft Tissue
4. Mineral
5. Metal
Most Black → Most White:
Gas → Fat → Soft Tissue → Mineral → Metal
Describe the Appearance of Opacities as Relative
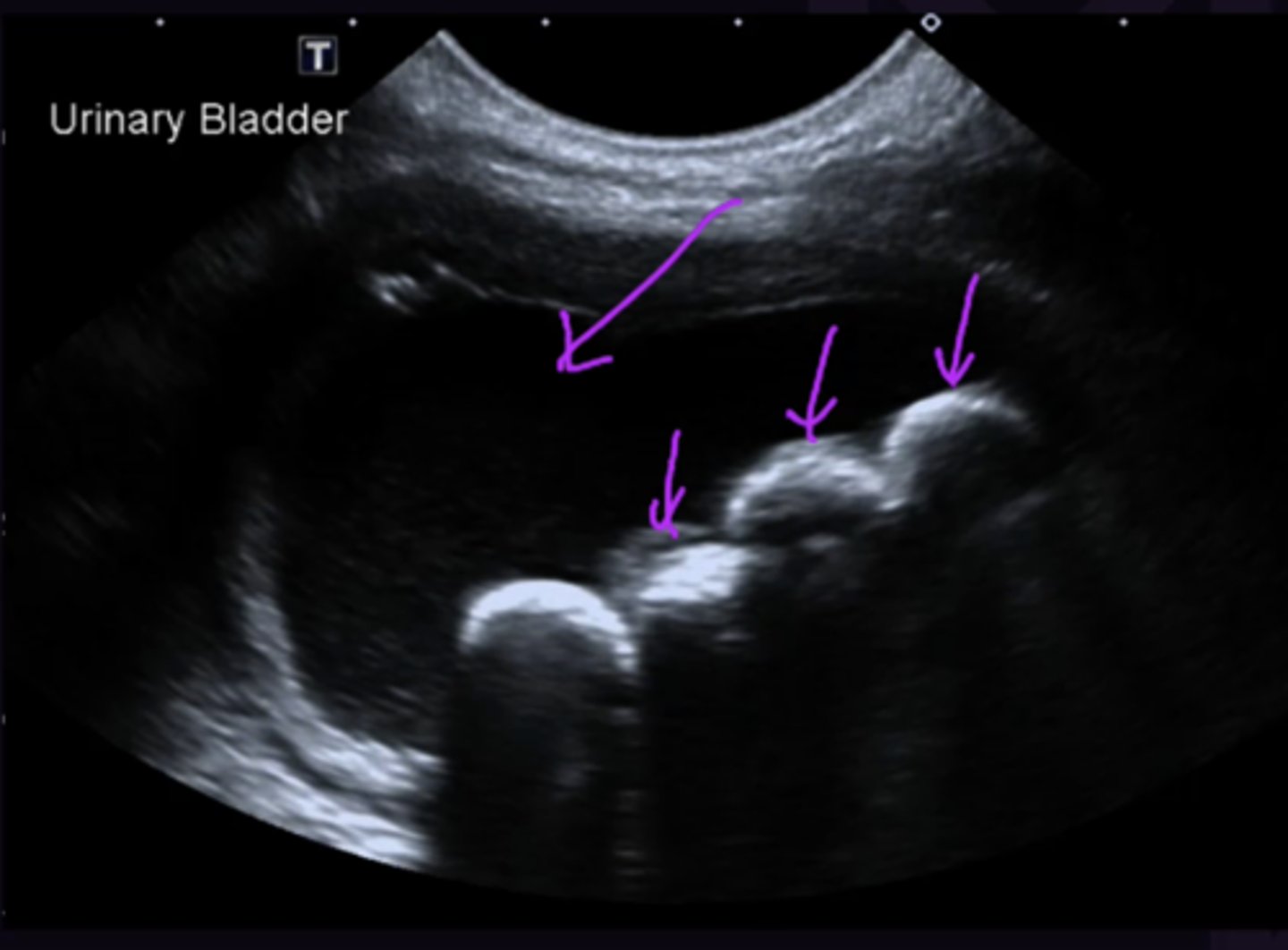
Occurs when Structure is Surrounded by Positive Contrast
e.g calculi are mineral opaque in the bladder as they are in urine (Soft tissue opacity). In a double contrast cystogram, the calculi (mineral opacity) appear relatively lucent compared to the contrast agent (Metal Opacity).
e.g. Nipple surrounded by gas so appears opaque
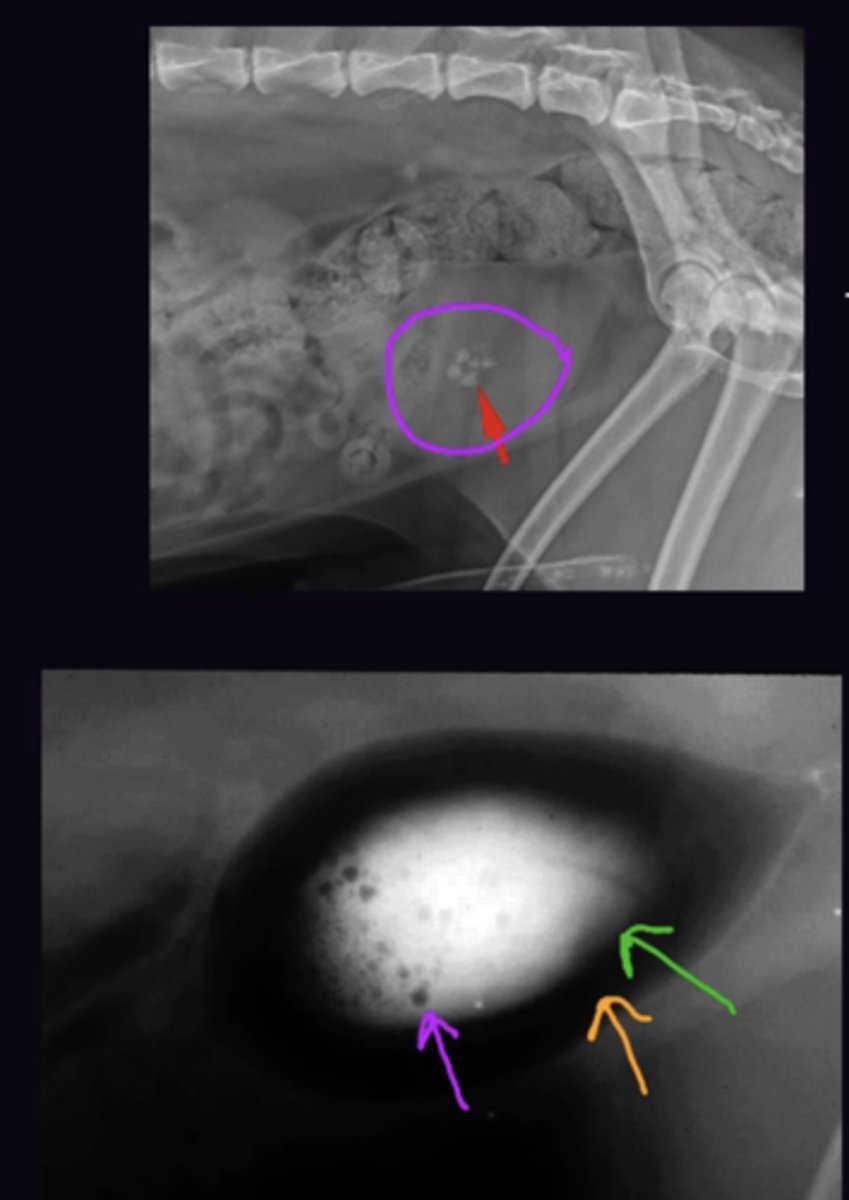
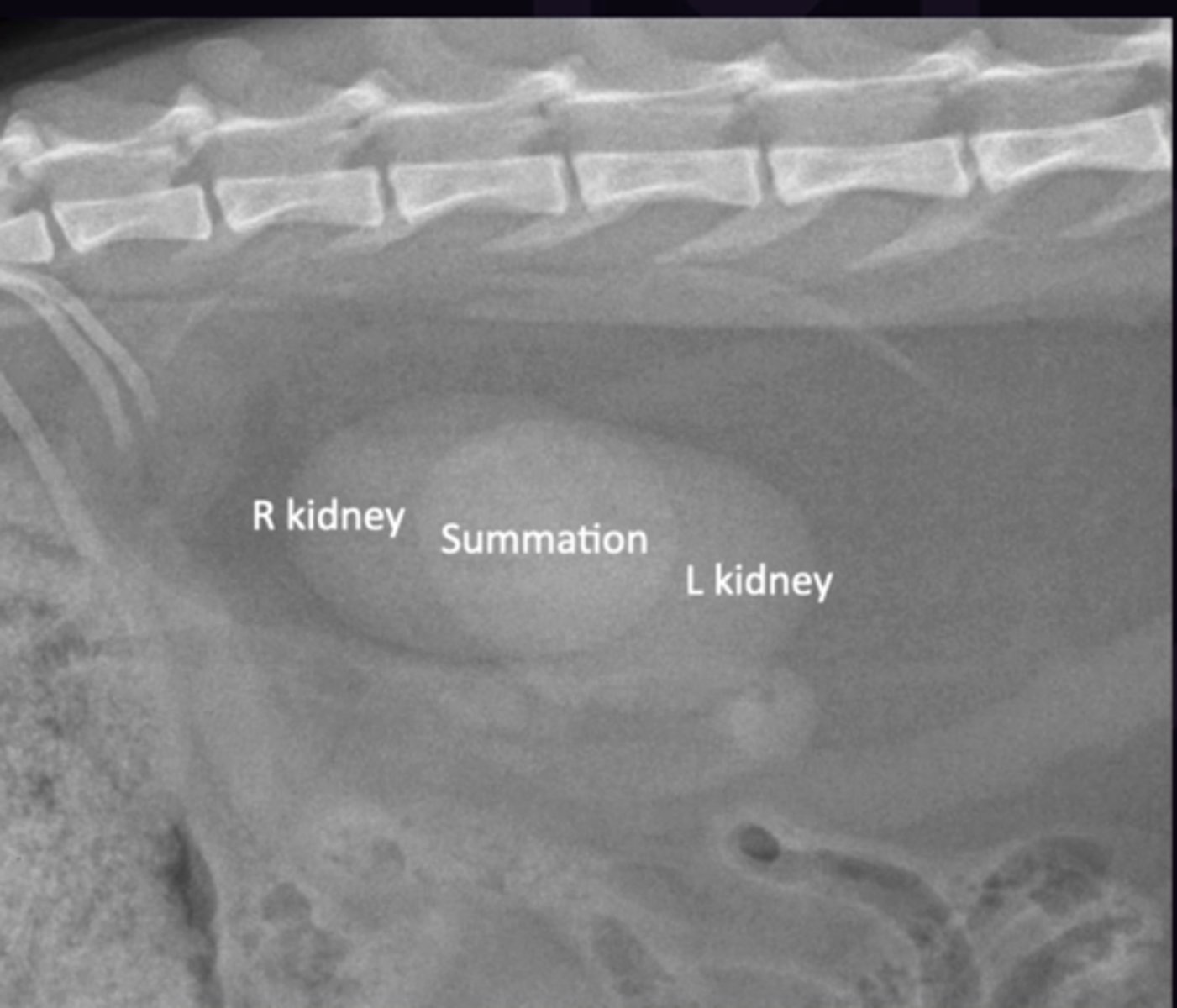
Describe Summation in terms of:
1. Definition
2. Common Examples
1. Superimposed opacities adding together (Can be tissue or gas). Differs from effacement as separate margins of each kidney can be seen
2. Superimposition of left + right kidneys, where they are superimposed it is more opaque
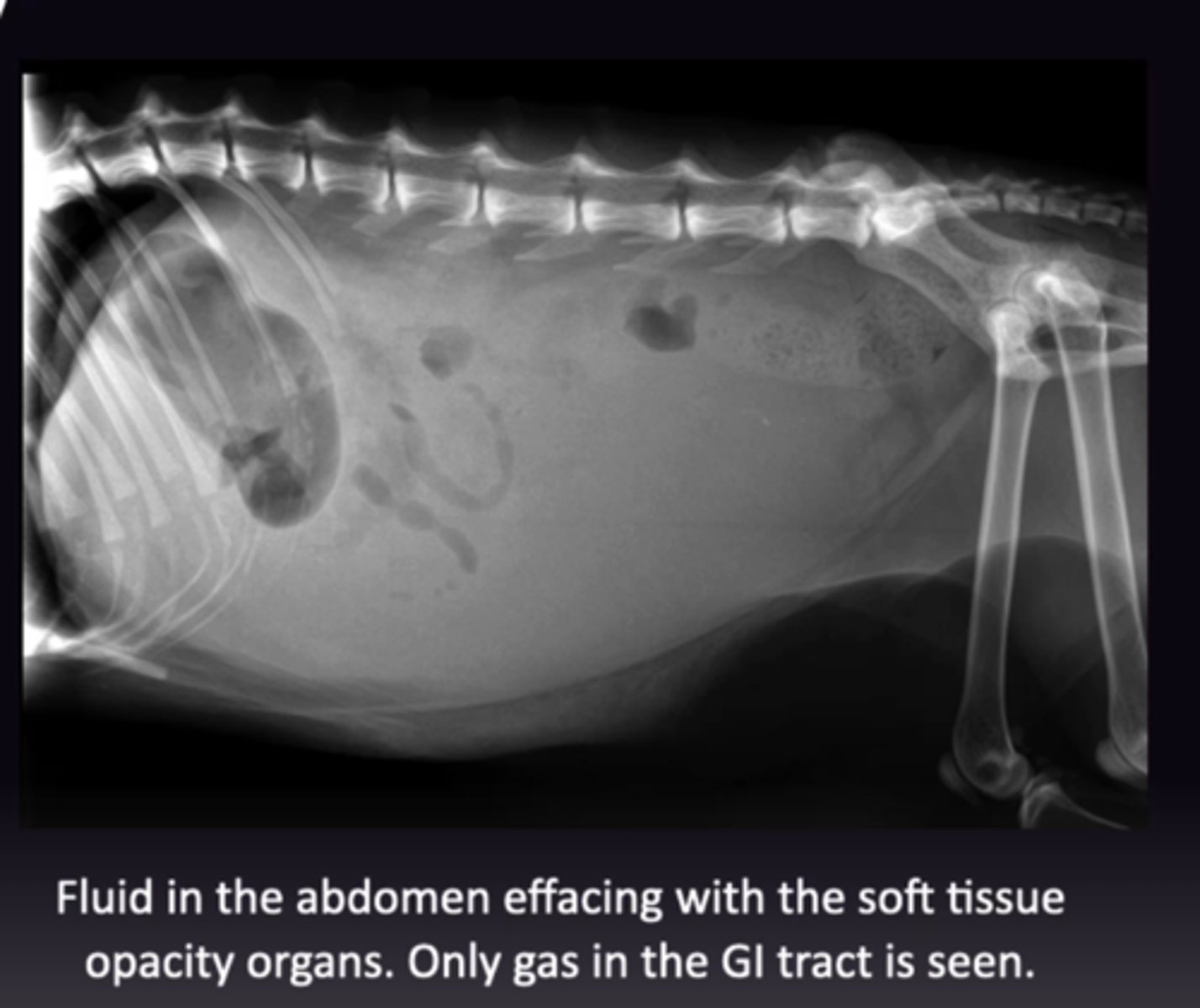
Describe Effacement (Border Effacement/Silhouette Sign) in terms of:
1. Definition
2. Rules of Effacement
1. When 2 structures of the same opacity are in contact, their individual margin at the point if contact cannot be distinguished
2. Same Opacity + In contact
Describe the Use of Effacement to Locate Structures (Masses ect.) using the following examples concerning a Thoracic Radiograph:
1. Where Does X-Ray Beam Pass Through
2. What Opacity is it
3. Could it be in the Liver
4. Could it be in the Lung
5. Could it be on the Skin
1. Skin-Lung-Liver
2. Soft tissue opacity
3. No, because it would efface with it and not be seen (as the mass and the liver are the same opacity and if the mass was in the liver it would be in contact with it)
4. Yes, because it is surrounded by gas opacity lung
5. Yes, Because it is surrounded by gas opacity (air outside the dog) if it protrudes up from the skin
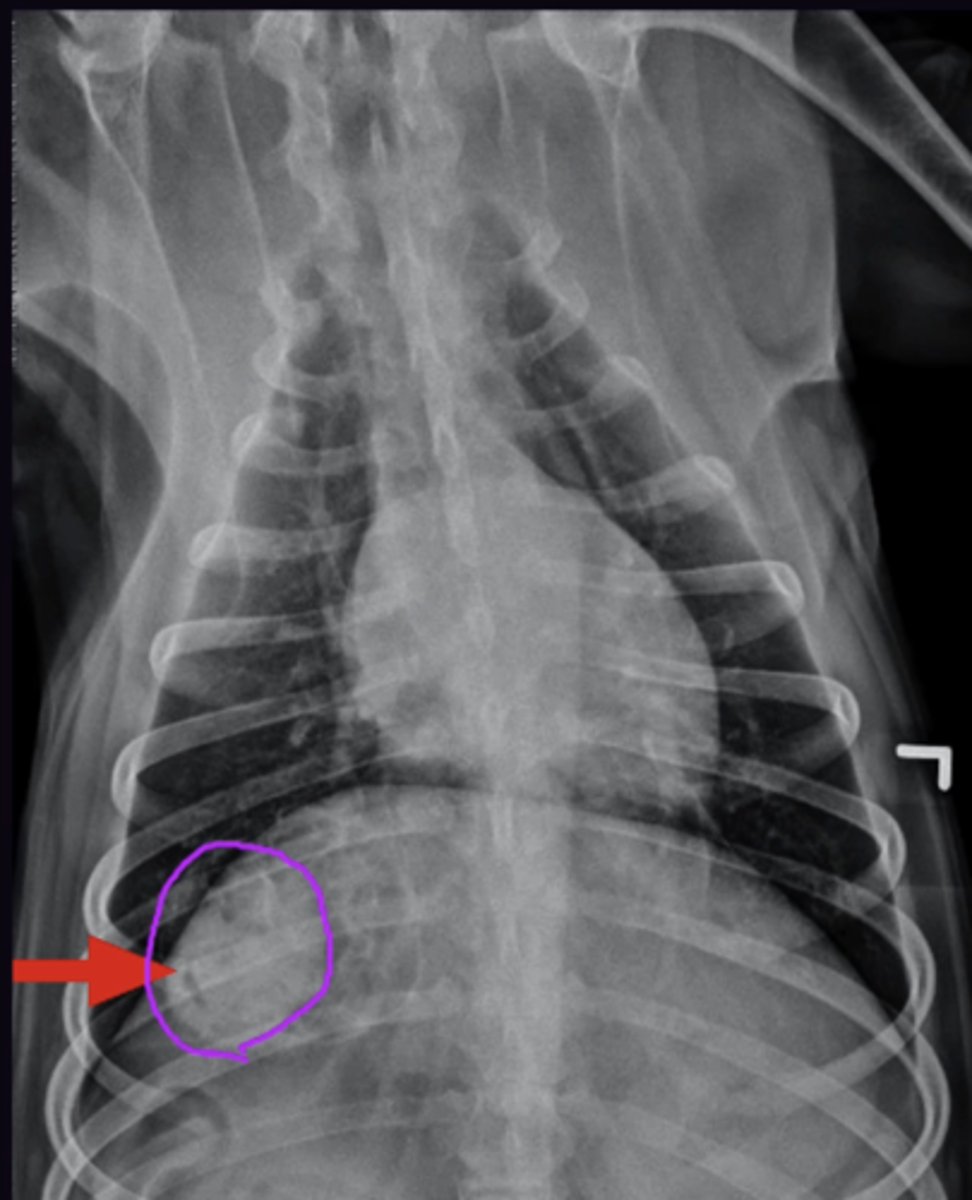
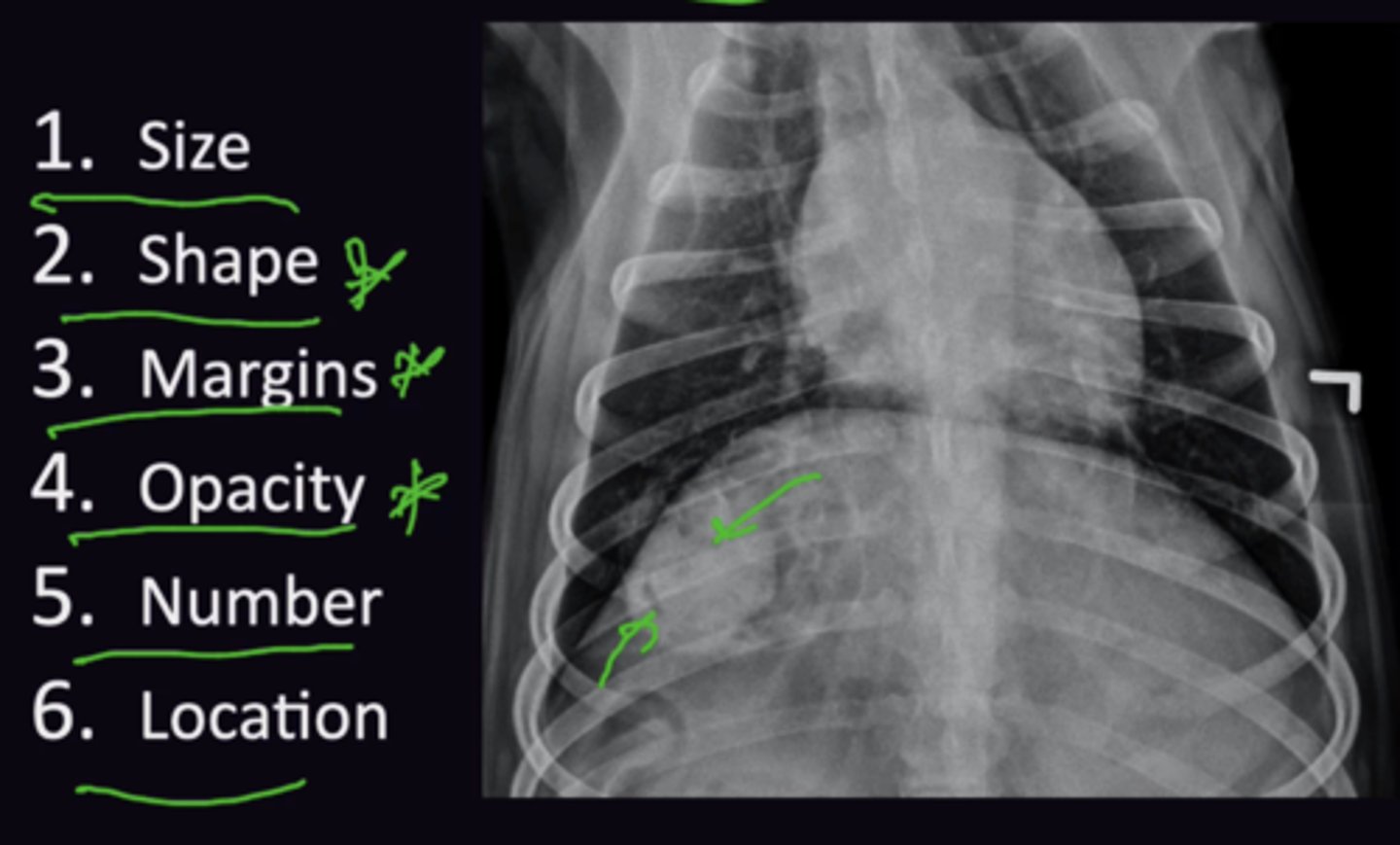
Describe Roentgen Signs in terms of:
1. Definition
2. What are the 6 Roentgen Signs
3. When to Use Roentgen Signs
1. A list of adjectives to describe abnormalities, they are prompts for how to describe the appearance of the radiographic abnormality
2. Size, Shape, Margins, Opacity, Number, Location
3. For each structure ask if it is normal or abnormal
→ Normal → Move on
OR
→ Abnormal → Evaluate using Roentgen Signs
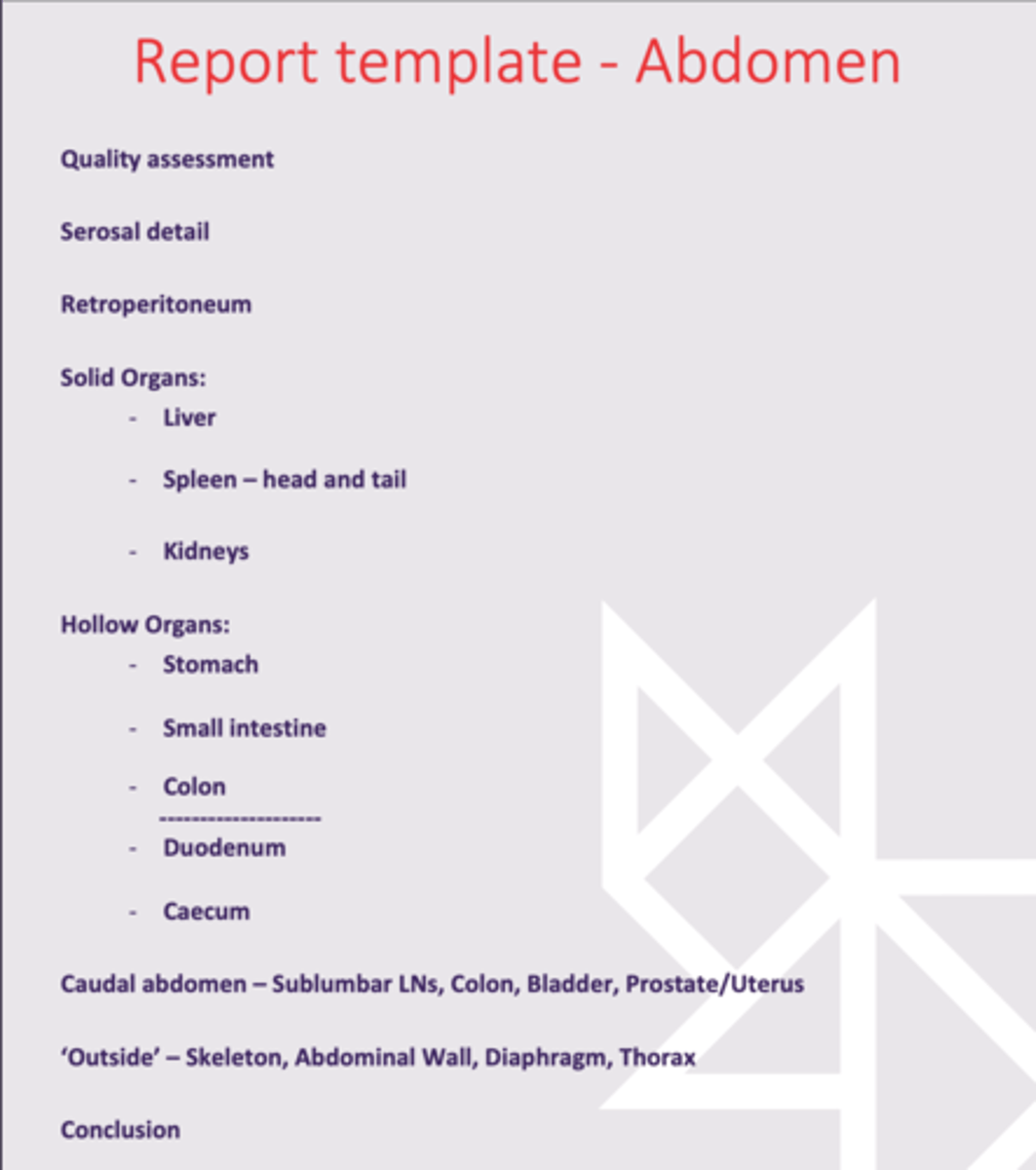
Radiology 3: Abdomen Quality Assessment
Radiology 3: Abdomen Quality Assessment
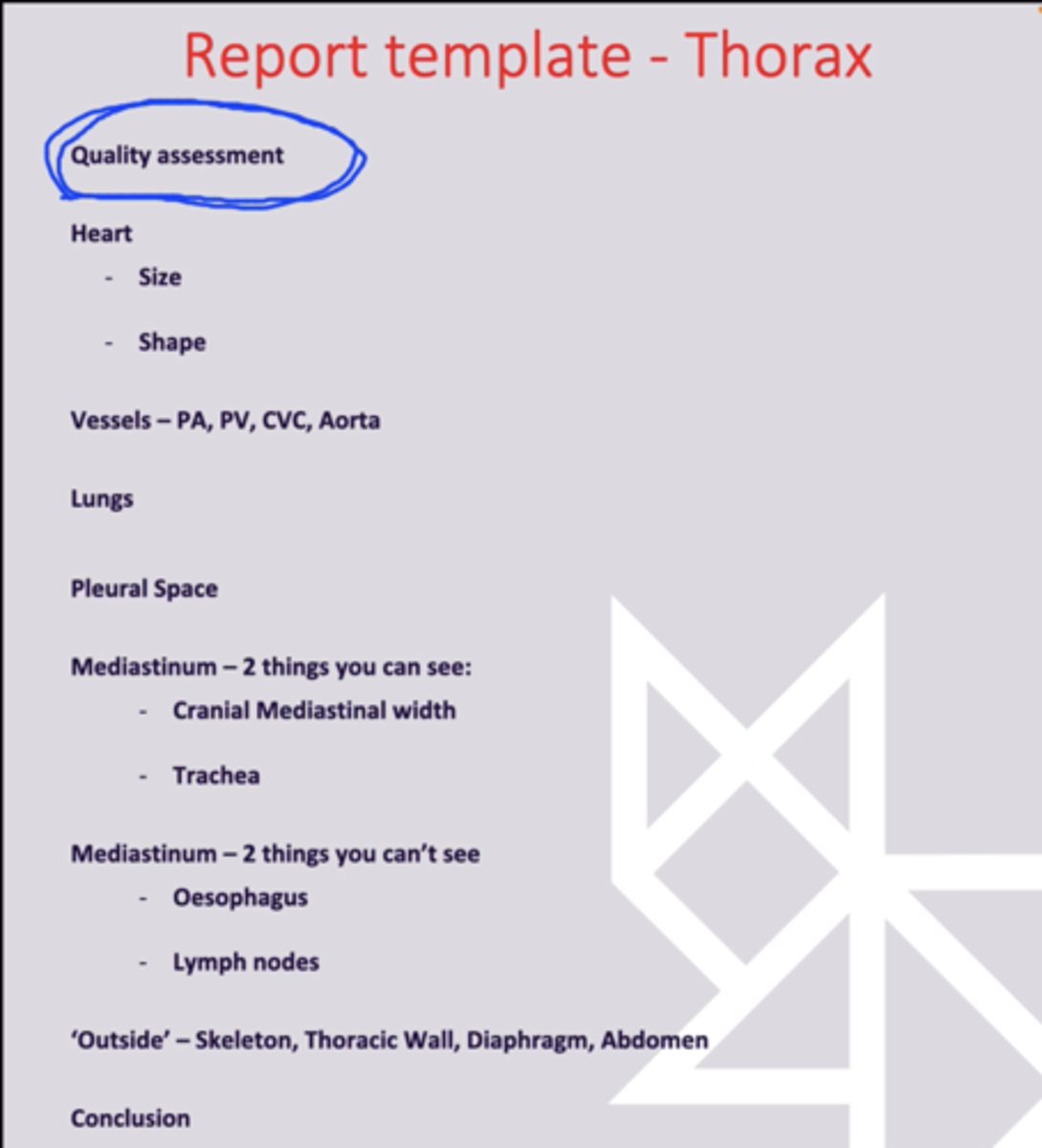
When is the Quality Assessment of a Radiograph in terms of the Systematic Apporach?
First
Describe how to Identify a Full Bladder on Radiography and its Implications
Makes assessment of the rest of the abdomen difficult. Always Empty Bladder prior to radiography
Describe how to Identify a Fasted/Post-Prandial Stomach+Intestines on Radiography and its Implications
Postprandial: Patient was not faster for 12 hours so there is ingesta in stomach + small intestine. Cannot be differentiated from normal material
Describe Radiography of the Abdomen in terms of:
1. Views Taken
2. Why The Dorso-Ventral View is Not Taken
1. Left Lateral, Right Lateral, Ventro-Dorsal
2. Makes Abdomen very hard to interpret
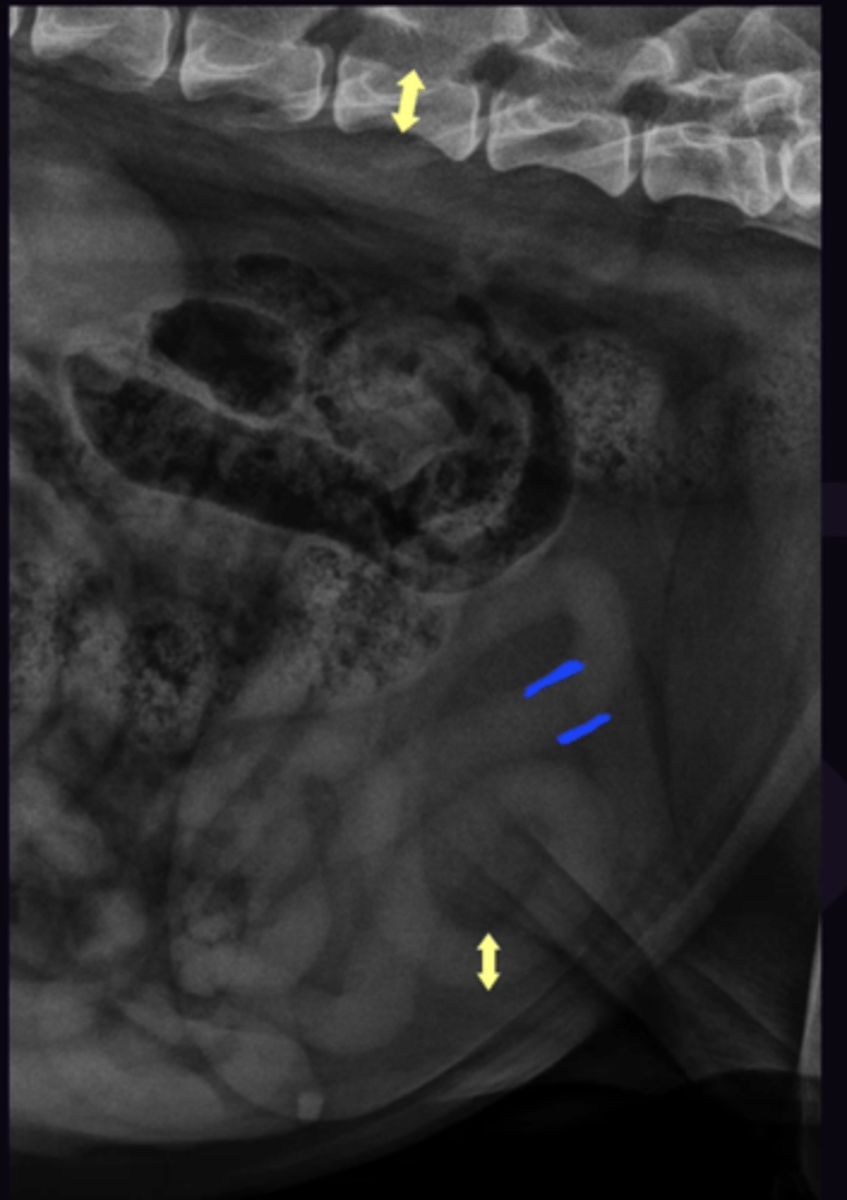
Describe how to Differentiate a Right vs. Left Lateral View of the Abdomen
If both lateral views are available then they can be compared. The left lateral view will have the most gas in the pylorus
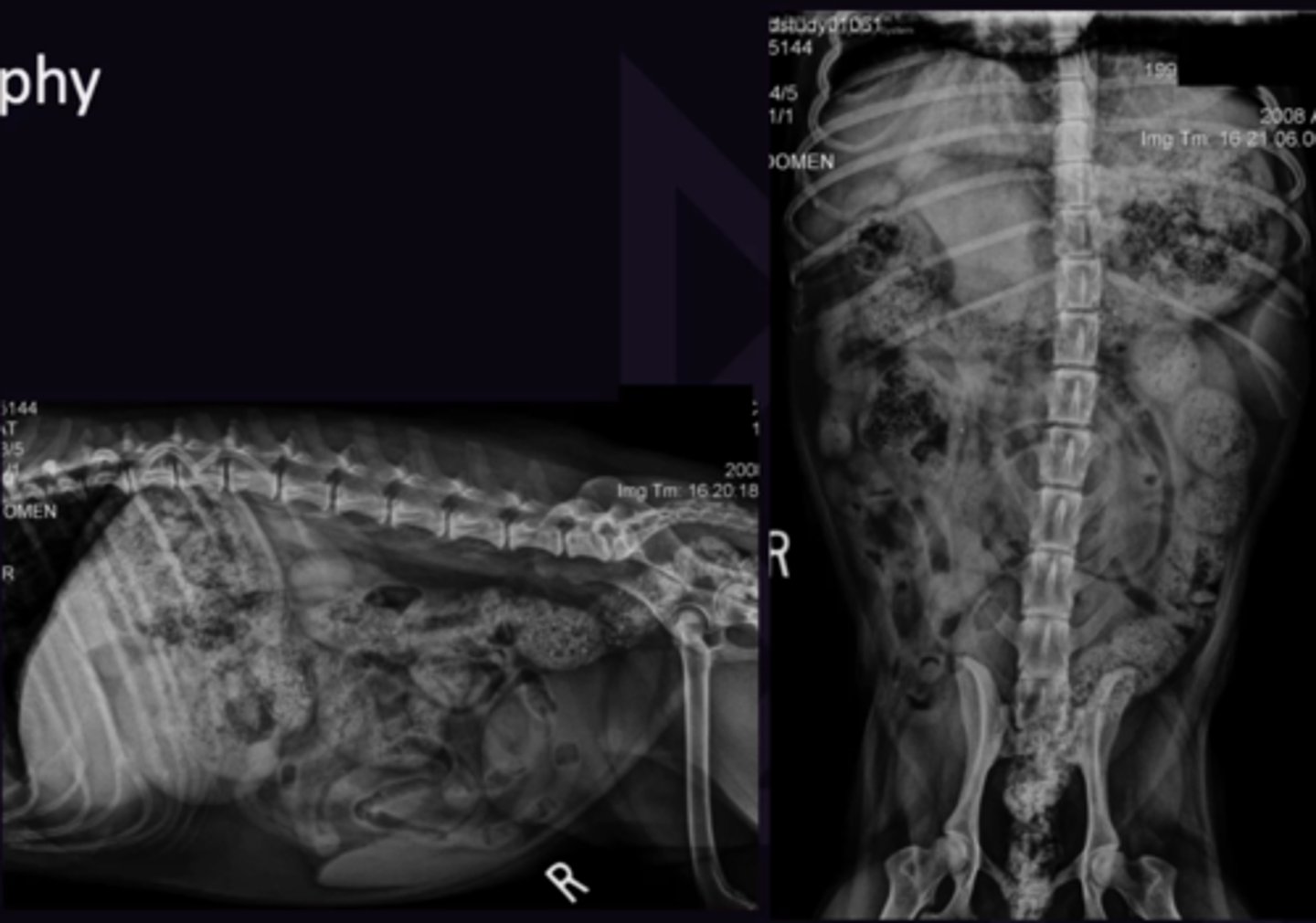
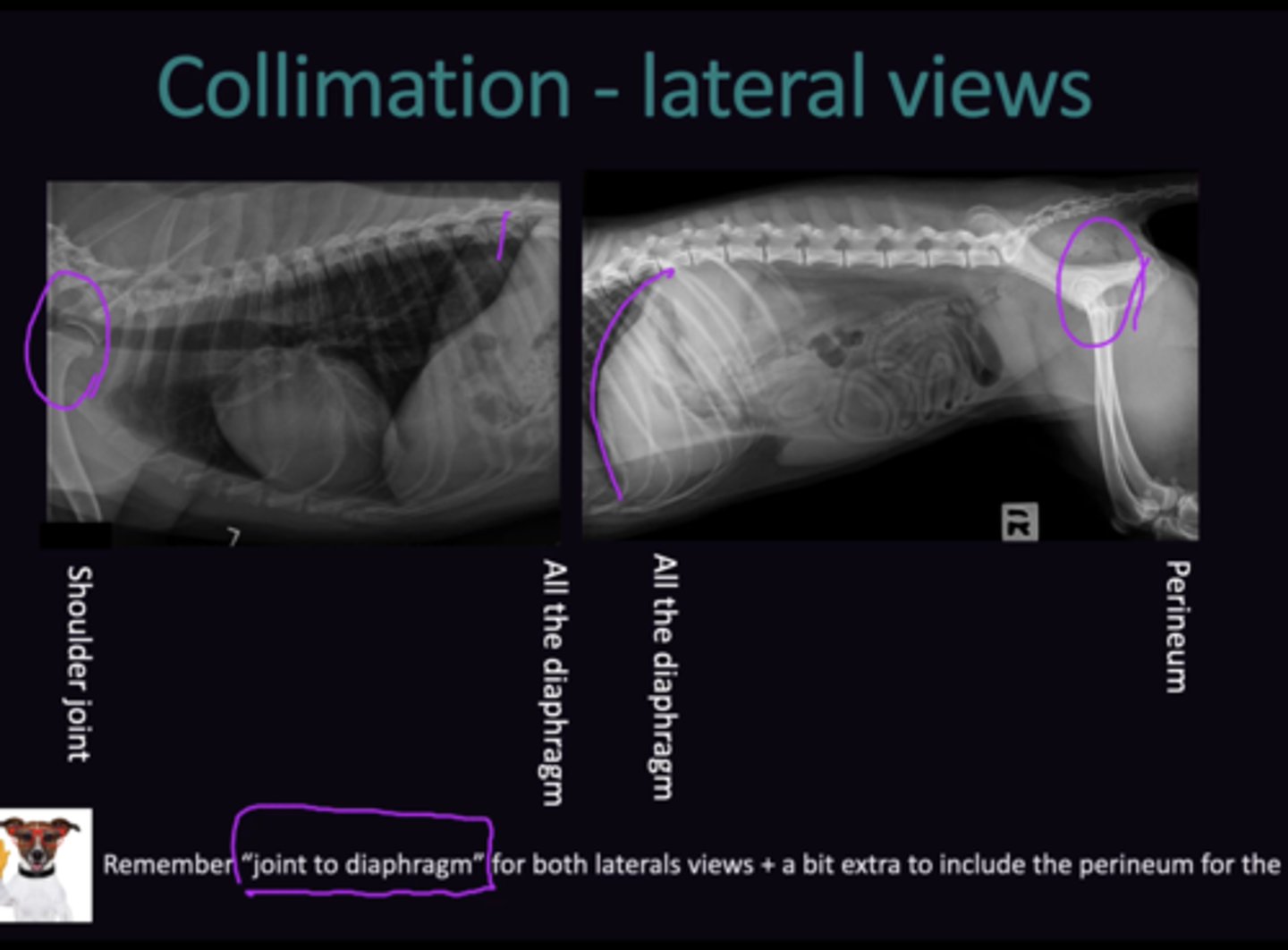
Describe how to Assess the Quality of Collimation Distance on Radiographs in terms of:
1. Thoracic View
2. Abdominal View
3. Ventro-Dorsal View
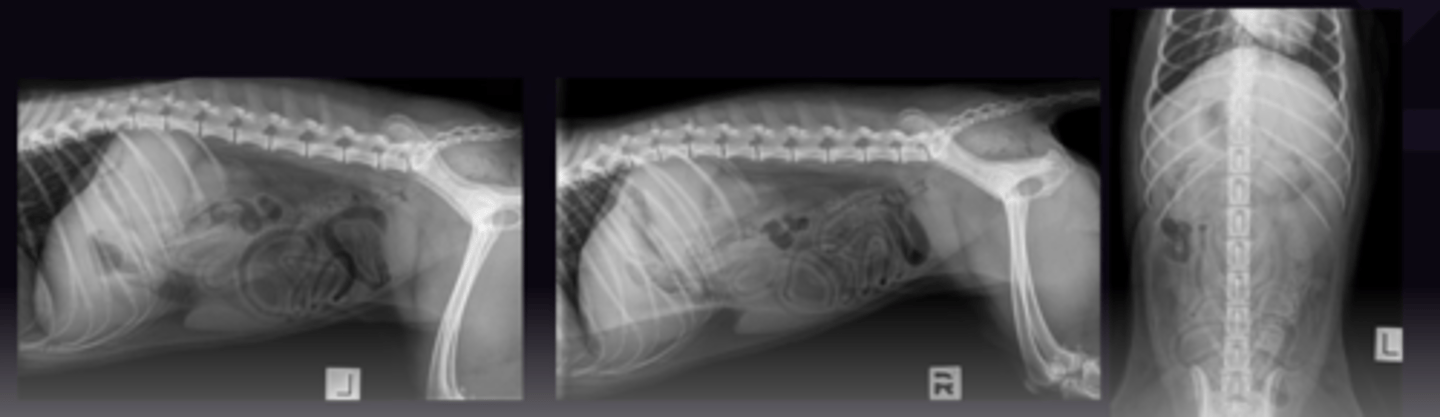
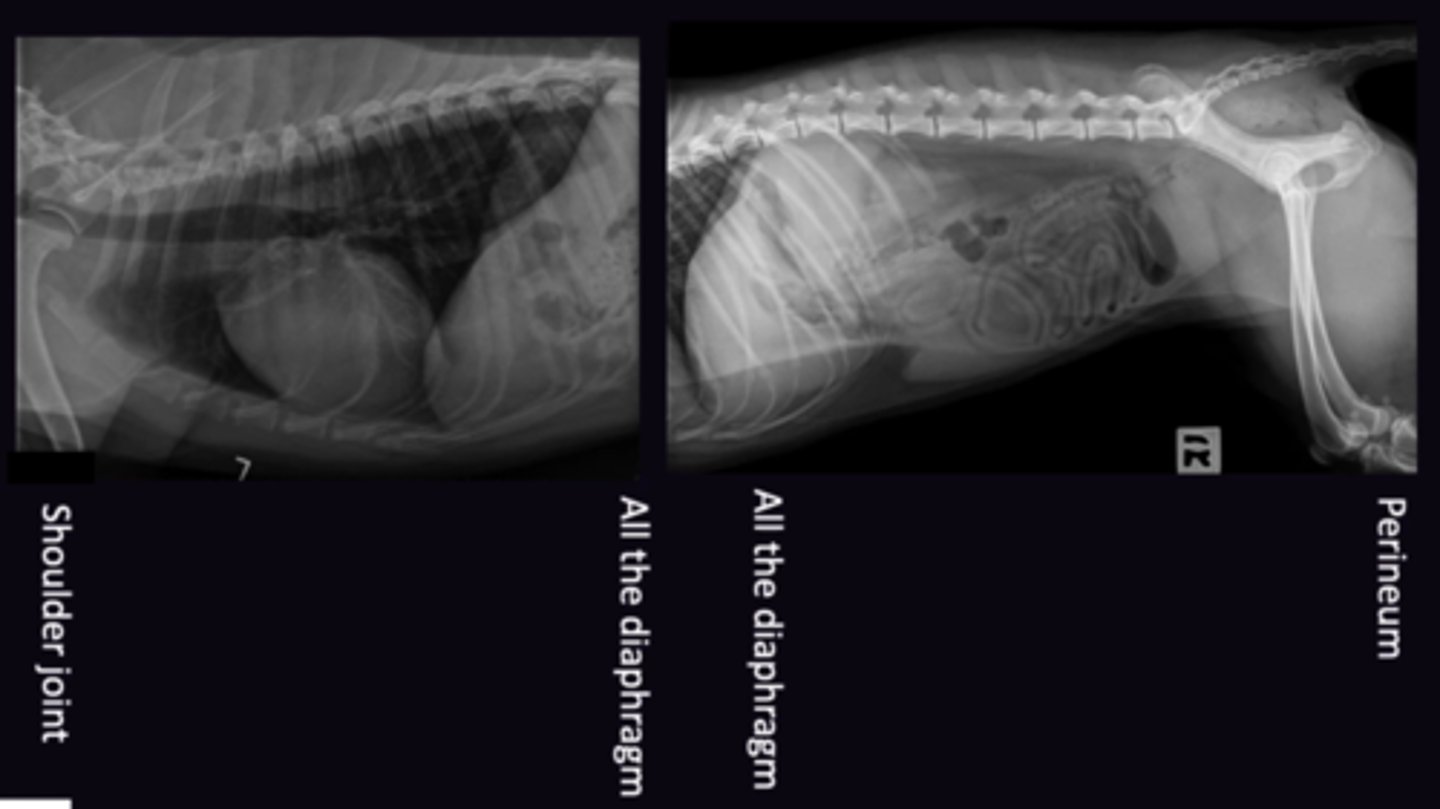
4. Large Breed Dog Considerations
"Joint to Diaphragm"
1. Shoulder Joint → All of Diaphragm Visible
2. All of Diaphragm → Hip Joint (+Perineum) Visible
3. Joint to Diaphragm
4. Will not fit on Imiging plate. 2 radiographs need to be made for each view (6 Total). Ensure caudal and cranial collimation rules are respcted
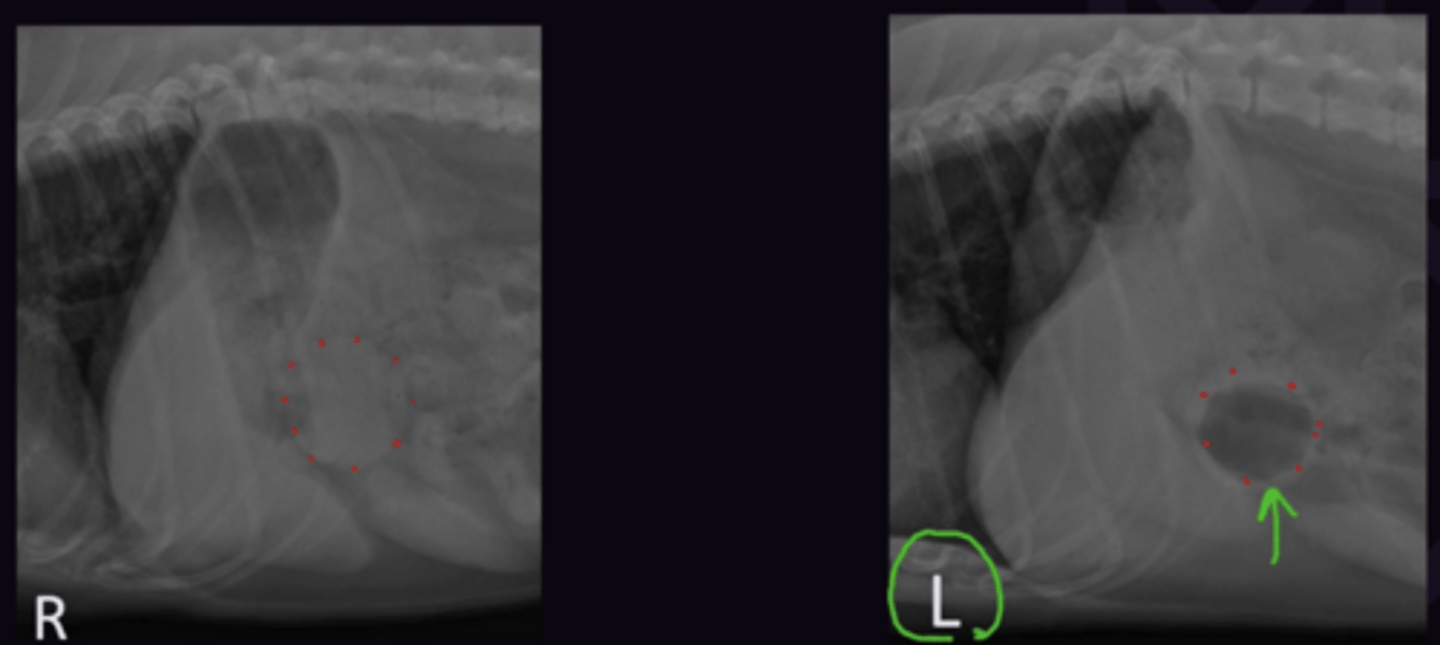
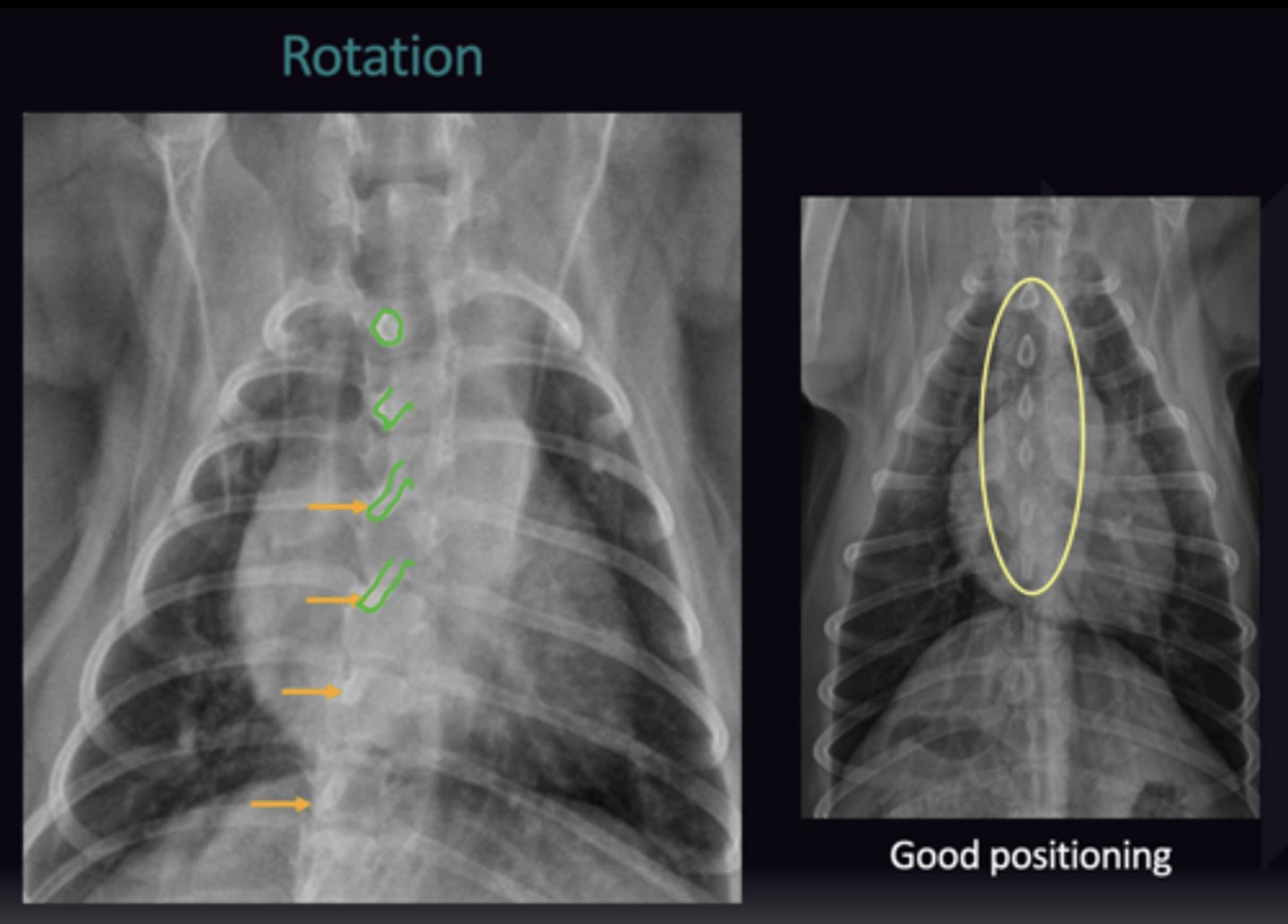
Describe how to Evaluate Rotation on Abdominal Radiographs in terms of:
1. Pelvic Limb Evaluation
2. 3 Locations for Lateral Rotation Evaluation
3. Ventro-Dorsal Evaluation
1. Ensure Pelvic Limbs are pulled caudally
2.
- Costochondral Junctions are same level (Not necessarily superimposed)
- Transverse processes of the lumbar spine are superimposed
- Hips are superimposed
3. Spinous processes are in the centre of the vertebrae
Describe the Image Quality Assessment of Abdominal Radiographs in terms of:
1. Algorithm
2. Radiography
3. Windowing
1. Quality of Digital System, can't be changed
2. Correct Exposure Settings
3. Post processing to change the density + contrast so the image is the best it can be
Radiology 4: Thorax Quality Assessment
Radiology 4: Thorax Quality Assesment
When is the Quality Assessment of a Radiograph in terms of the Systematic Approach?
First
Describe the Radiography of the Thorax in terms of:
1. Views taken
2. When the Dorso-Ventral view is taken
1. Left Lateral, Right Lateral, Ventro-Dorsal (Total 3 Views)
2.
- If patient is to Dyspnoeic to do a VD (Harder to breath lying on their back)
- Caudal Lung lobe pathology + Normal structures
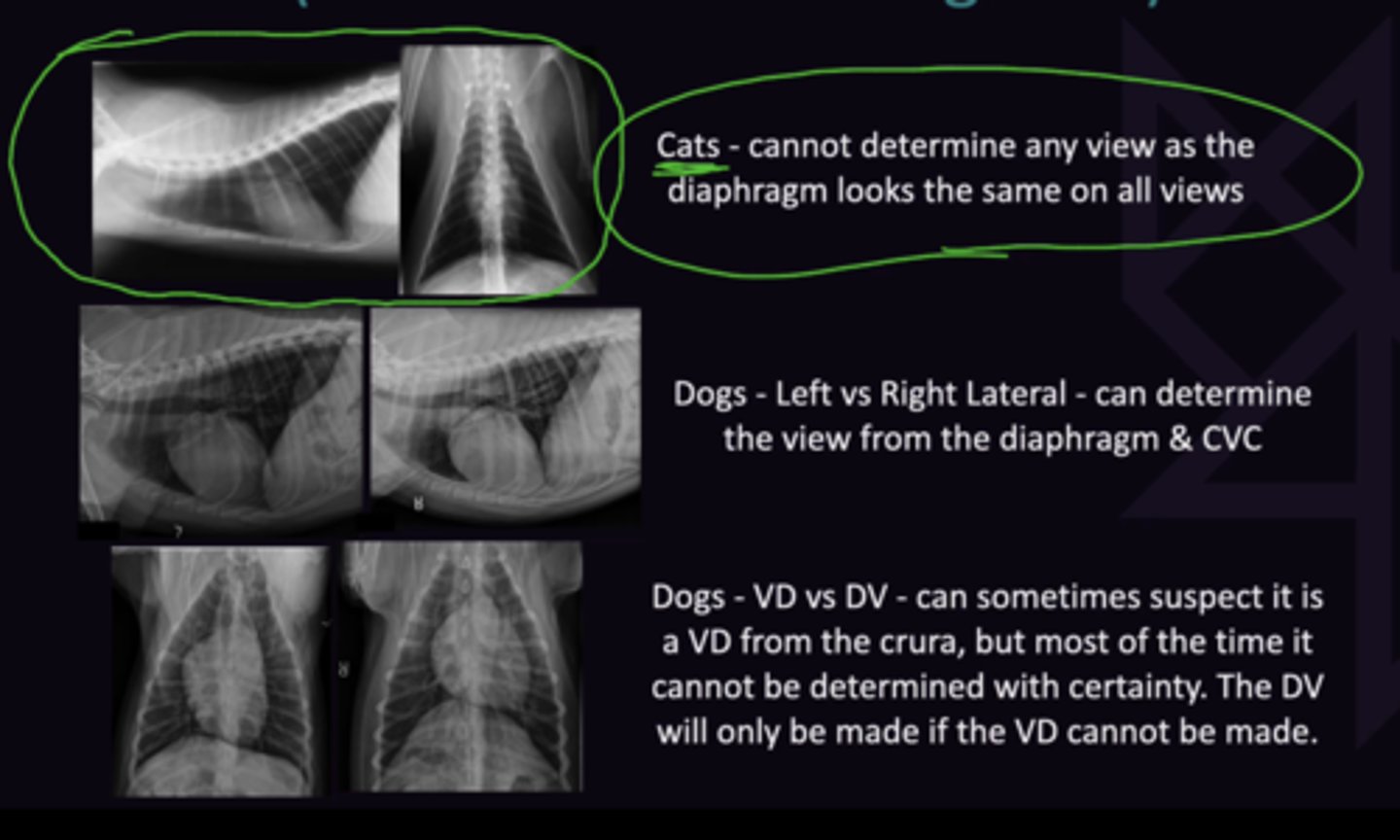
Describe how to Differentiate the Different Views of the Thorax Without Markers in terms of:
1. Cats Thorax
2. Dogs Left vs. Right Lateral
3. Dogs VD vs. DV
1. Cannot determine any views as the diaphram looks the same on all views
2. Can determine the view from the Diaphragm + CVC
3. Can sometimes suspect it is VD from crura, but cannot be certain. DV will only be made if VD cannot be made
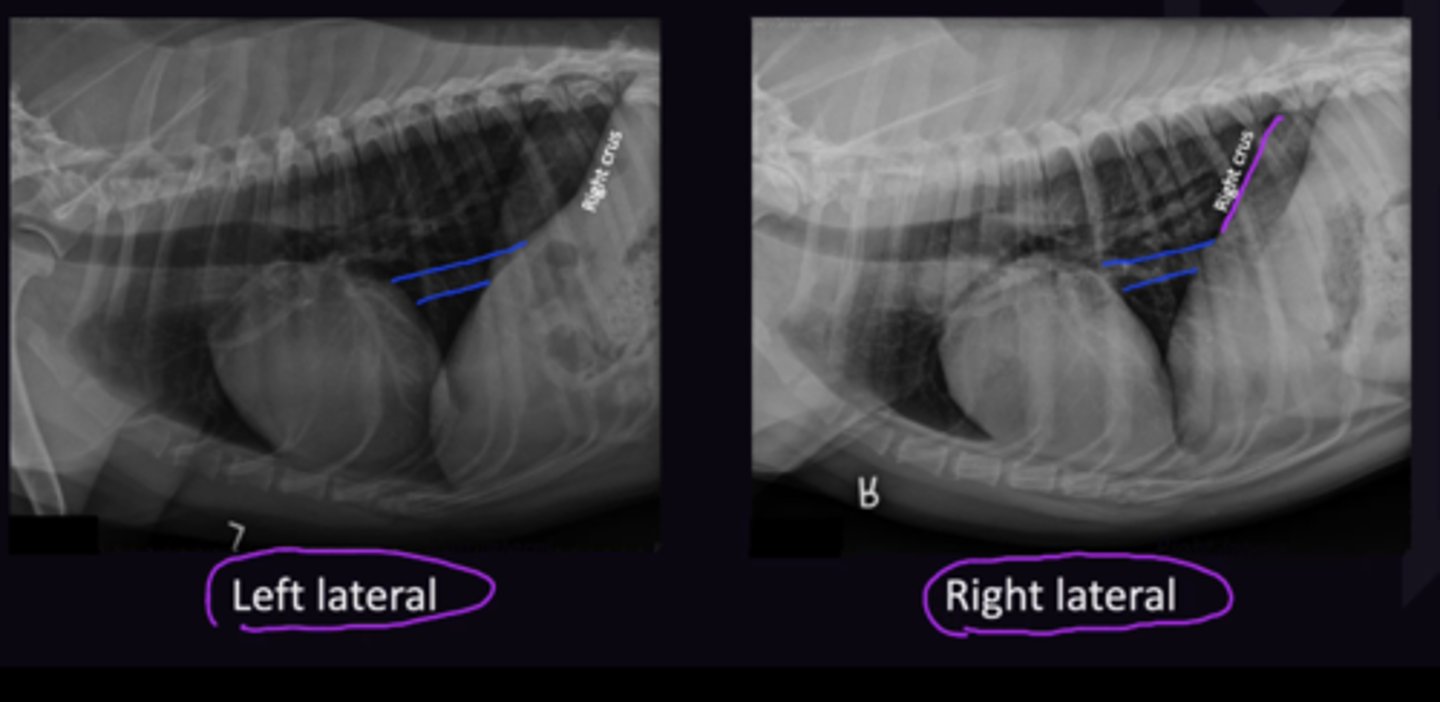
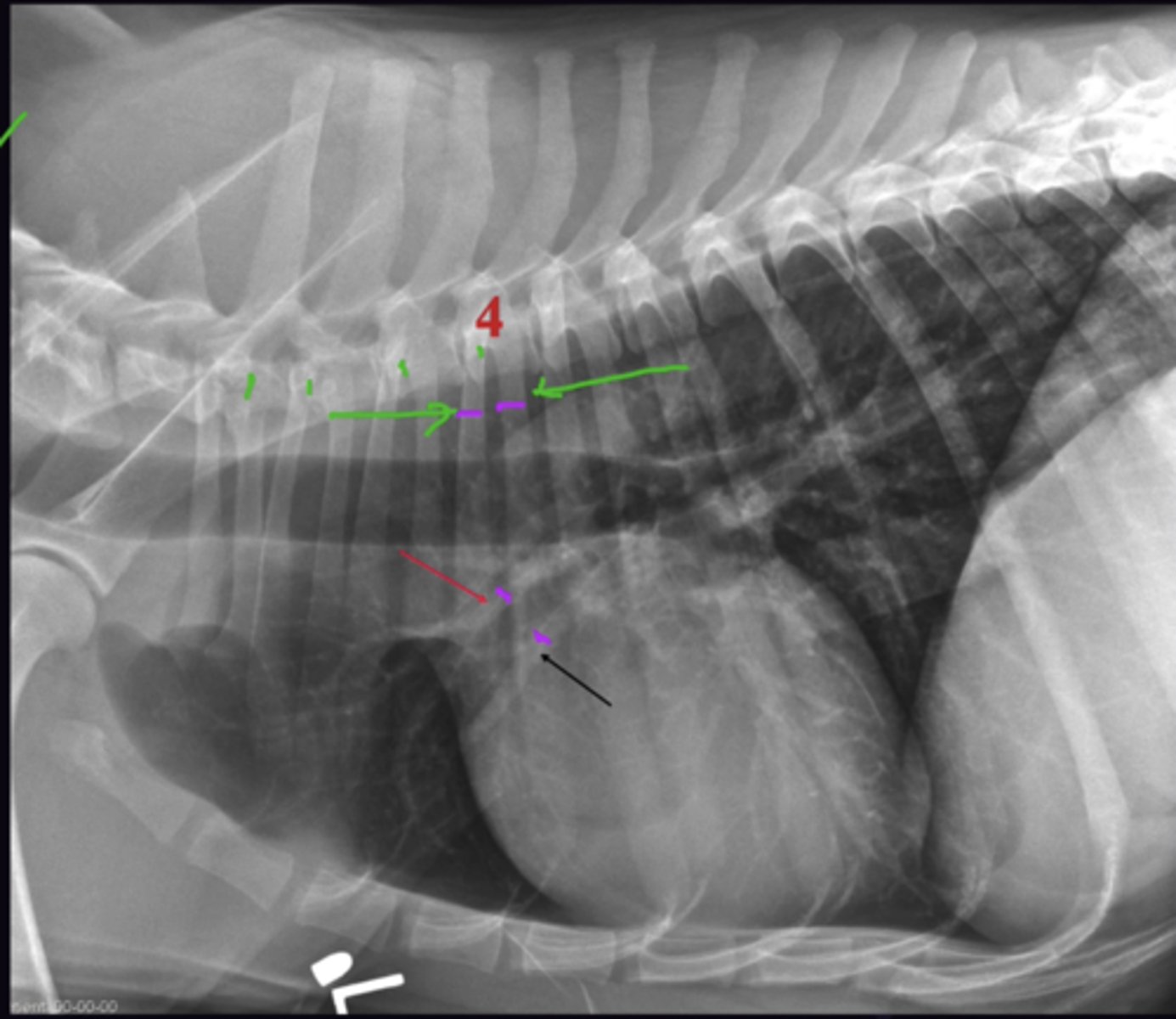
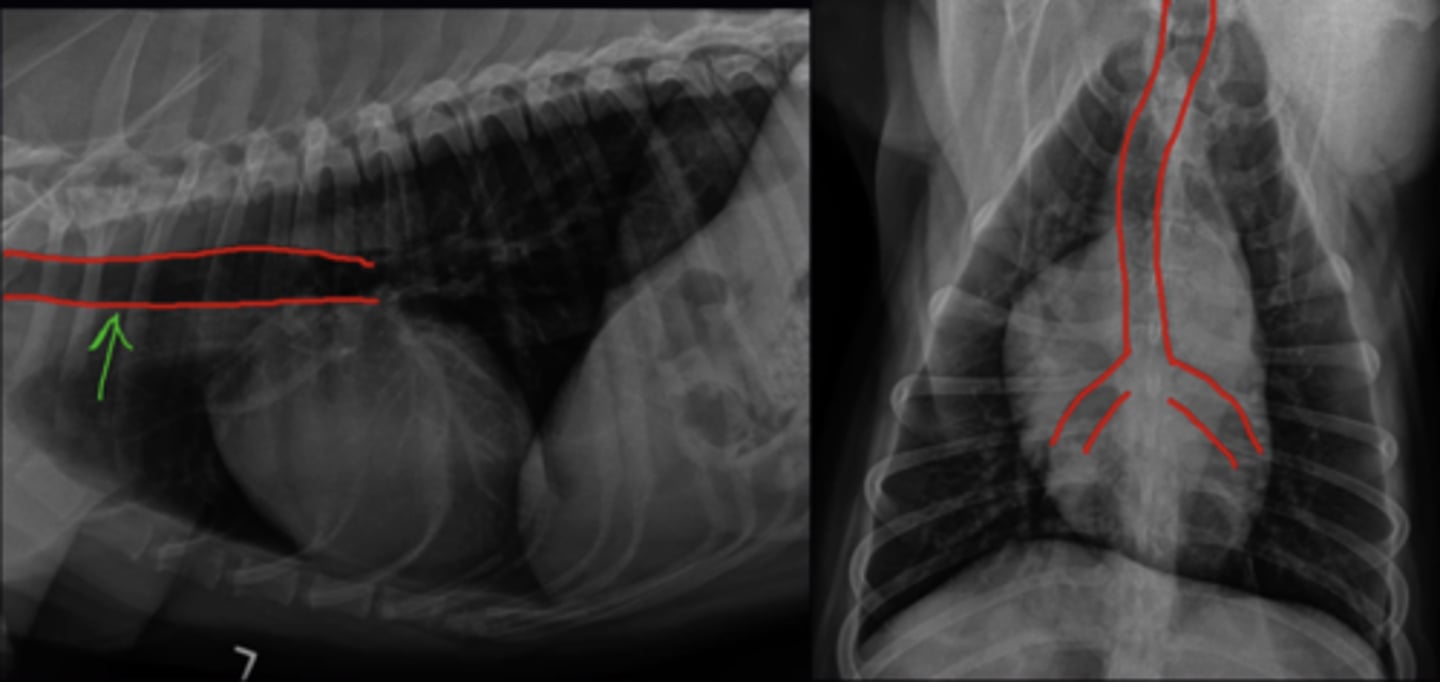
Describe how to Determine the Left vs. Right Lateral View of the Thorax in terms of:
1. Left Lateral View Differentiation
2. Right Lateral View Differentiation
1. Left Side down → Left lung cannot inflate as much as right → Left Crus more cranial
2. Right Side down → right lung cannot inflate as much as left → right Crus more cranial
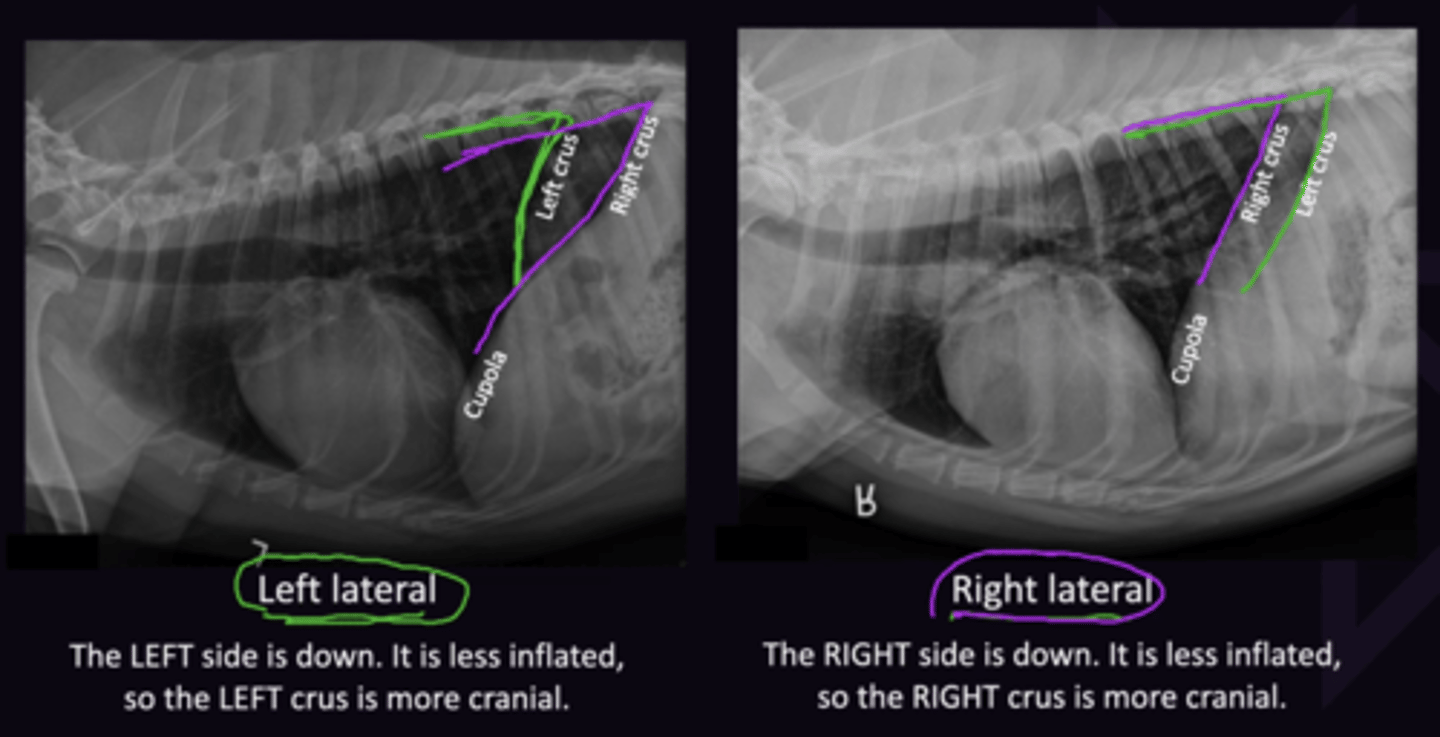
Describe how to Determine the Left vs. Right Lateral View of the Thorax in terms of the Caudal Vena Cava
Enters diaphragm on Right side (Goes through Right Crus).
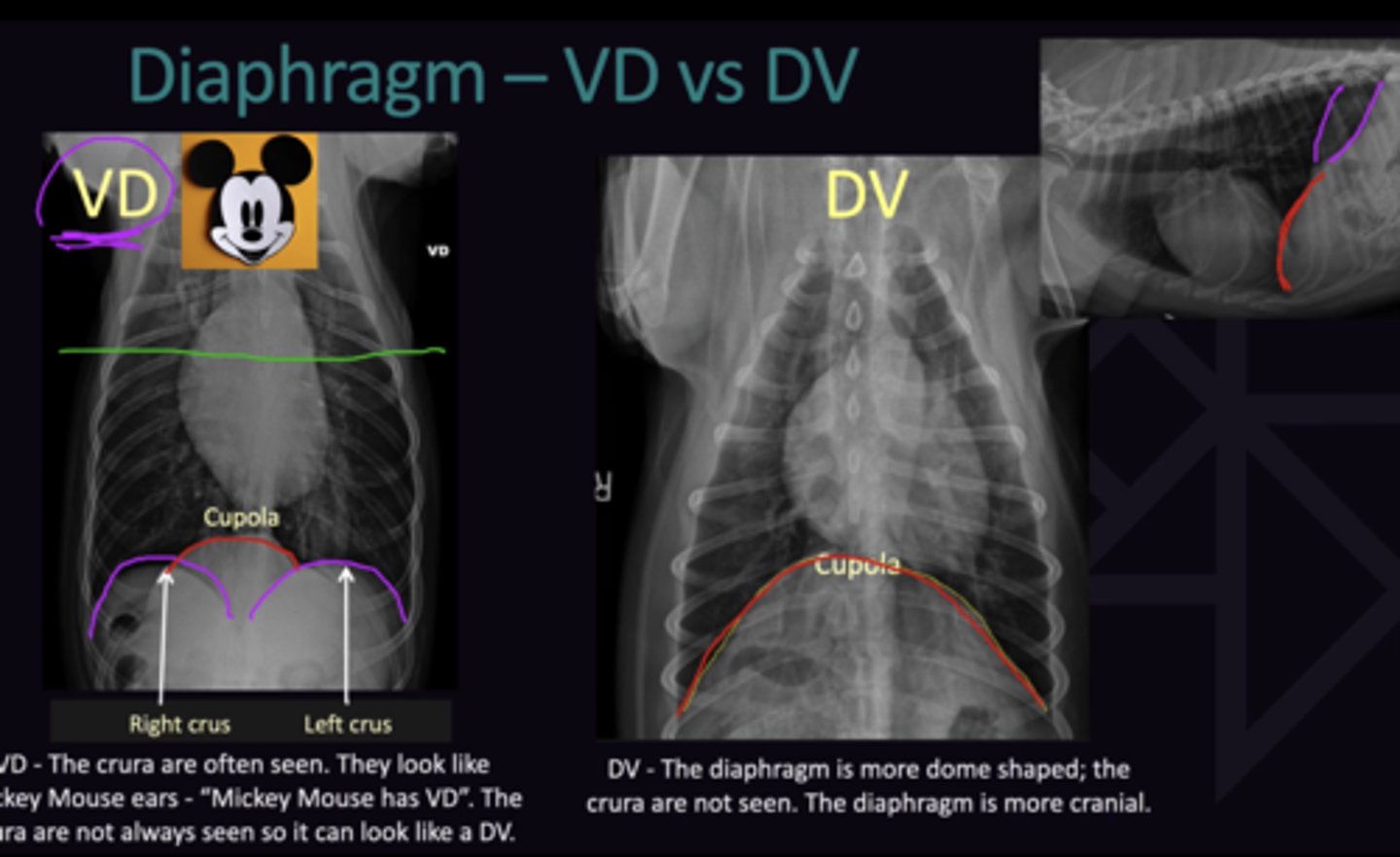
Describe how to Determine the VD vs. DV View of the Thorax in terms of:
1. Ventro-Dorsal View
2. Dorso-Ventral View
Cannot Determine for Certain
1. Crura are often seen, and look like "Micky Mouse" ears. However not always seen
2. Diaphragm is more dome shaped; crura are not seen, diaphragm is more cranial
Describe the Correct Way to Display Thorax Radiographs in terms of:
1. Left + Right Lateral Views
2. Ventro-Dorsal View
1. Cranial to left of screen, caudal to right of screen
2. Left Side on right of screen
Describe how to Assess the Quality of Collimation Distance on Radiographs in terms of:
1. Thoracic View
2. Abdominal View
3. Ventro-Dorsal View
4. Large Breed Dog Considerations
"Joint to Diaphragm"
1. Shoulder Joint → All of Diaphragm Visible
2. All of Diaphragm → Hip Joint (+Perineum) Visible
3. Joint to Diaphragm
4. Will not fit on Imaging plate. 2 radiographs need to be made for each view (6 Total). Ensure caudal and cranial collimation rules are respected
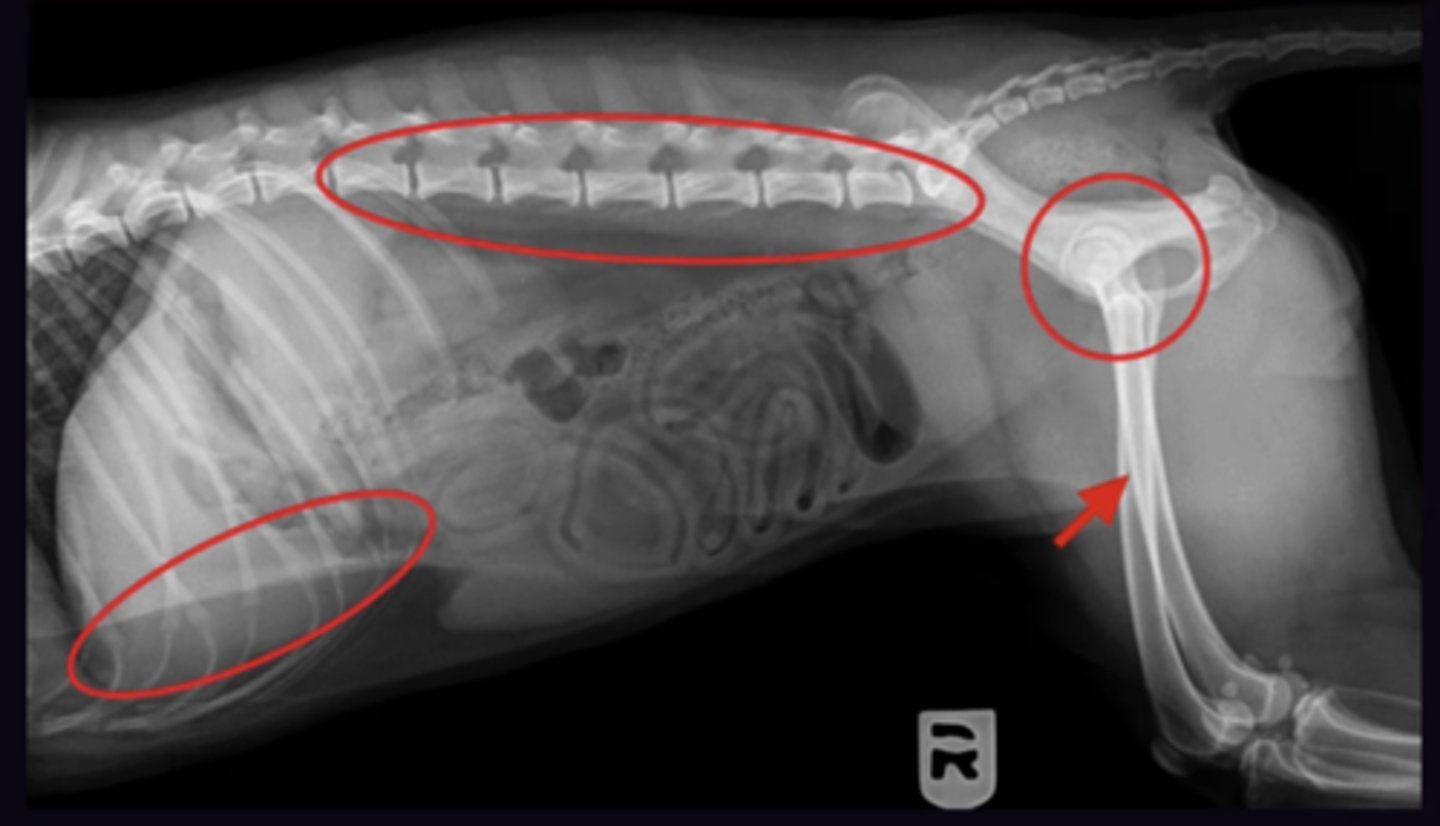
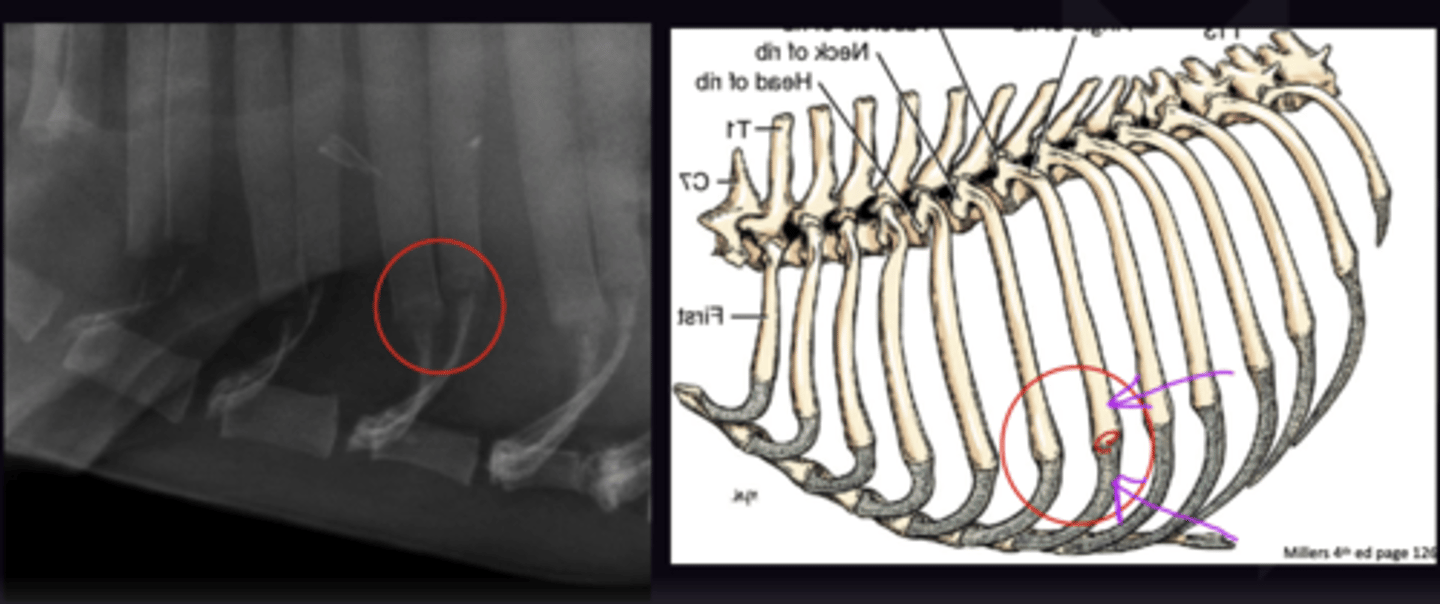
Describe how to Evaluate Rotation on Thoracic Radiographs in terms of:
1. Thoracic Limb Evaluation
2. 2 Locations for Lateral Rotation Evaluation
3. Ventro-Dorsal Evaluation
1. Legs are pulled Cranially, not superimposed on thorax
2. - Level Sternum
- Costochondral Junctions are same level (Not necessarily superimposed)
Describe how to Evaluate Rotation on Thoracic Radiographs in terms of DV/VD Views
Spinous processes Are in the centre of the vertebrae
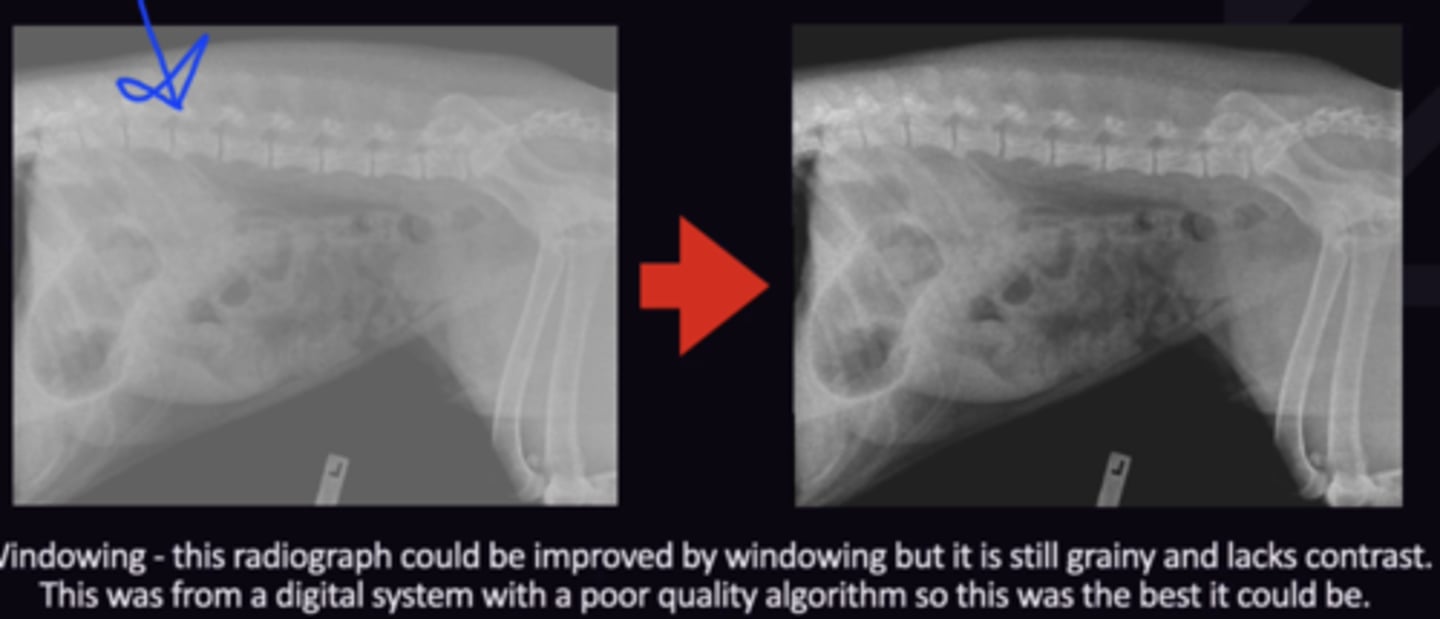
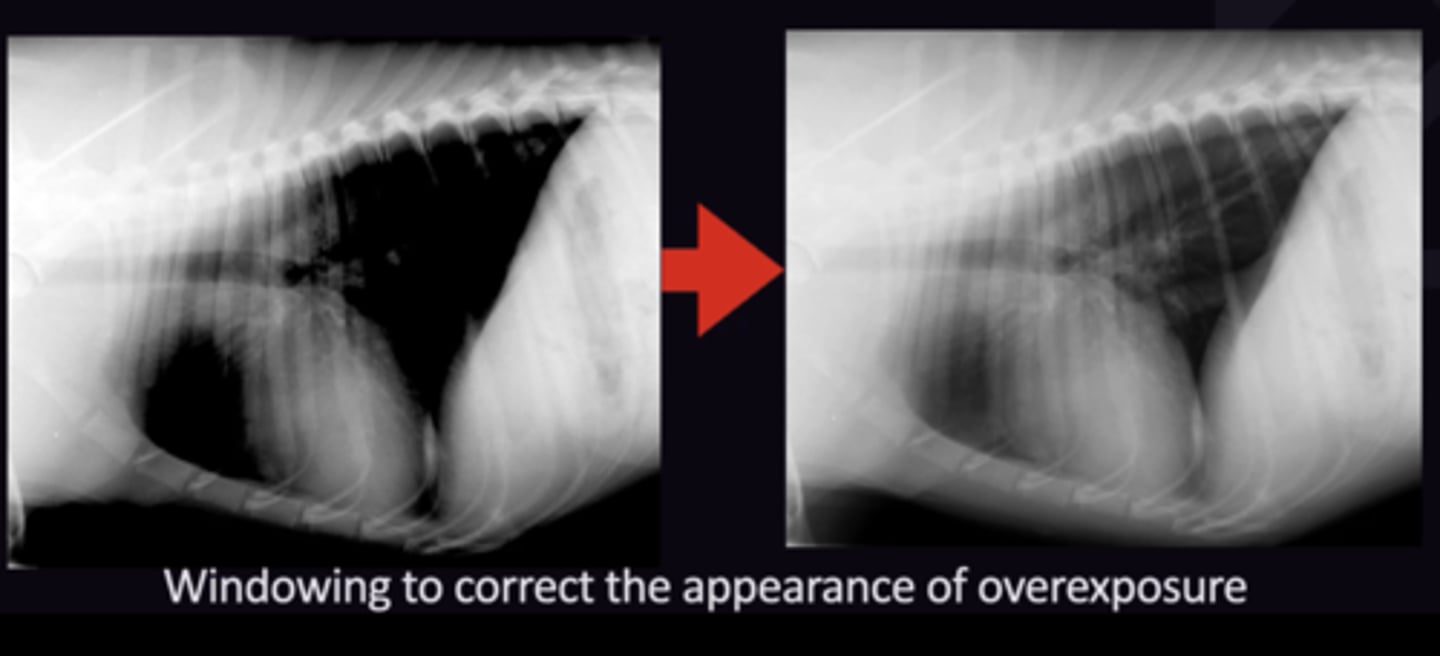
Describe the Image Quality Assessment of Thoracic Radiographs in terms of:
1. Algorithm
2. Radiography
3. Windowing
1. Quality of Digital System, can't be changed
2. Correct Exposure Settings
3. Post processing to change the density + contrast so the image is the best it can be
Radiology 5: Normal Thorax
Radiology 5: Normal Thorax
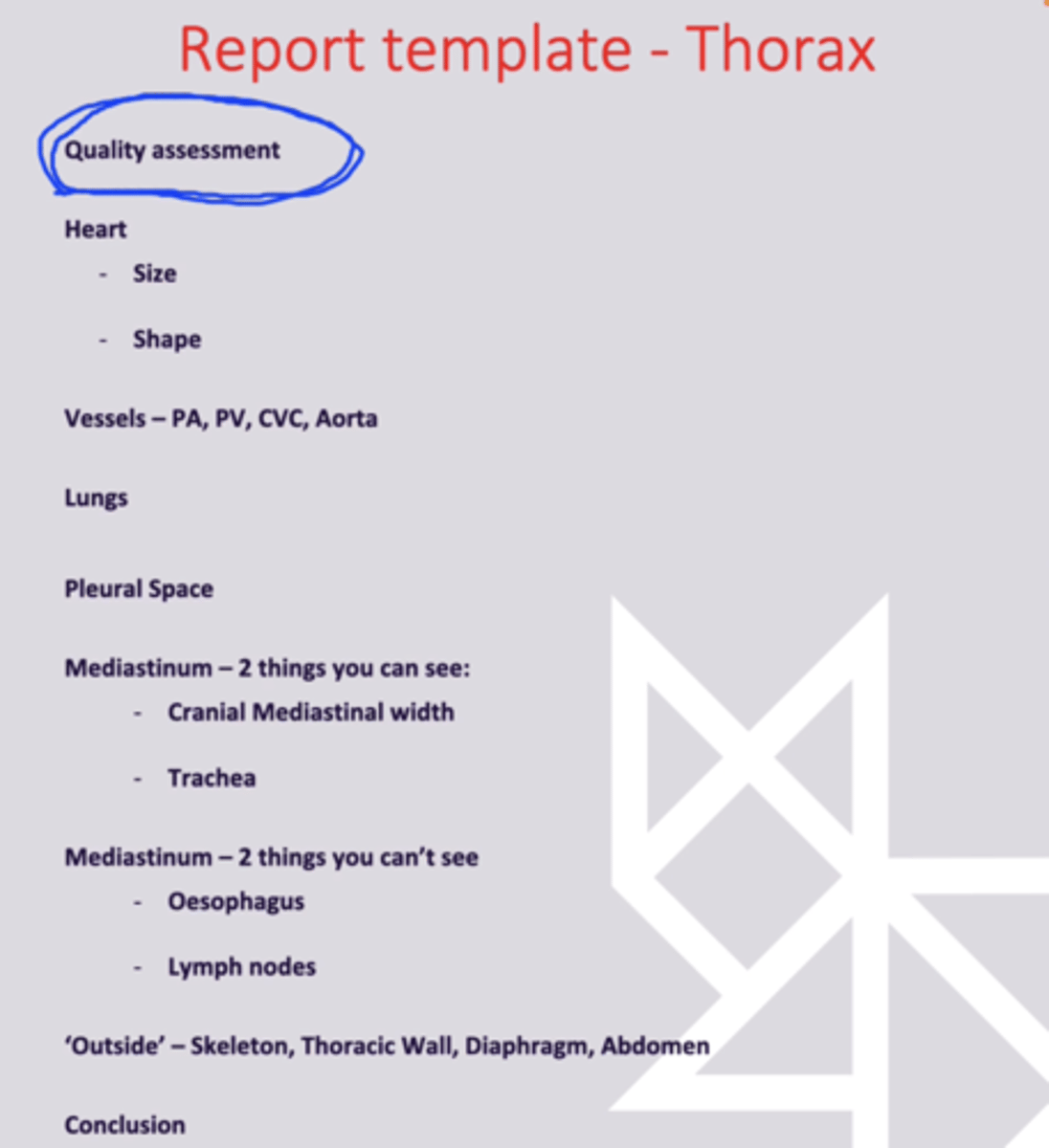
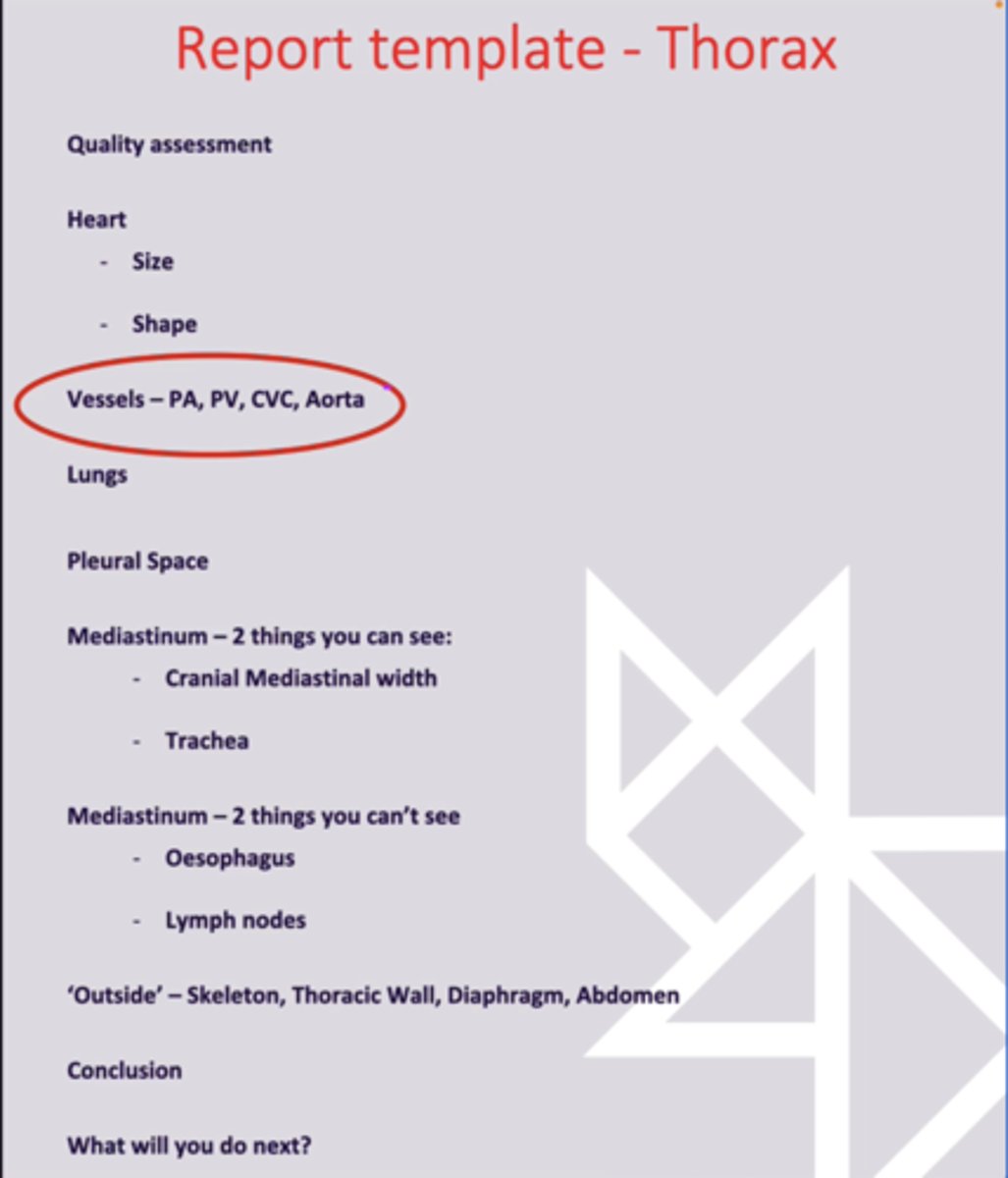
When are the Following Assessments of Radiographs in terms of the Systematic Approach of The Thorax:
1. Heart
2. Vessels
3. Lungs
4. Pleural Space
5. Mediastinum
6. Outside Structures
1. 2nd (Behind Quality Assesment)
2. 3rd
3. 4th
4. 5th
5. 6th
6. 7th
Describe the Normal Heart in terms of:
1. Size
2. Shape
1. Height + Width
2. Chamber Enlargement (bulges in heart)
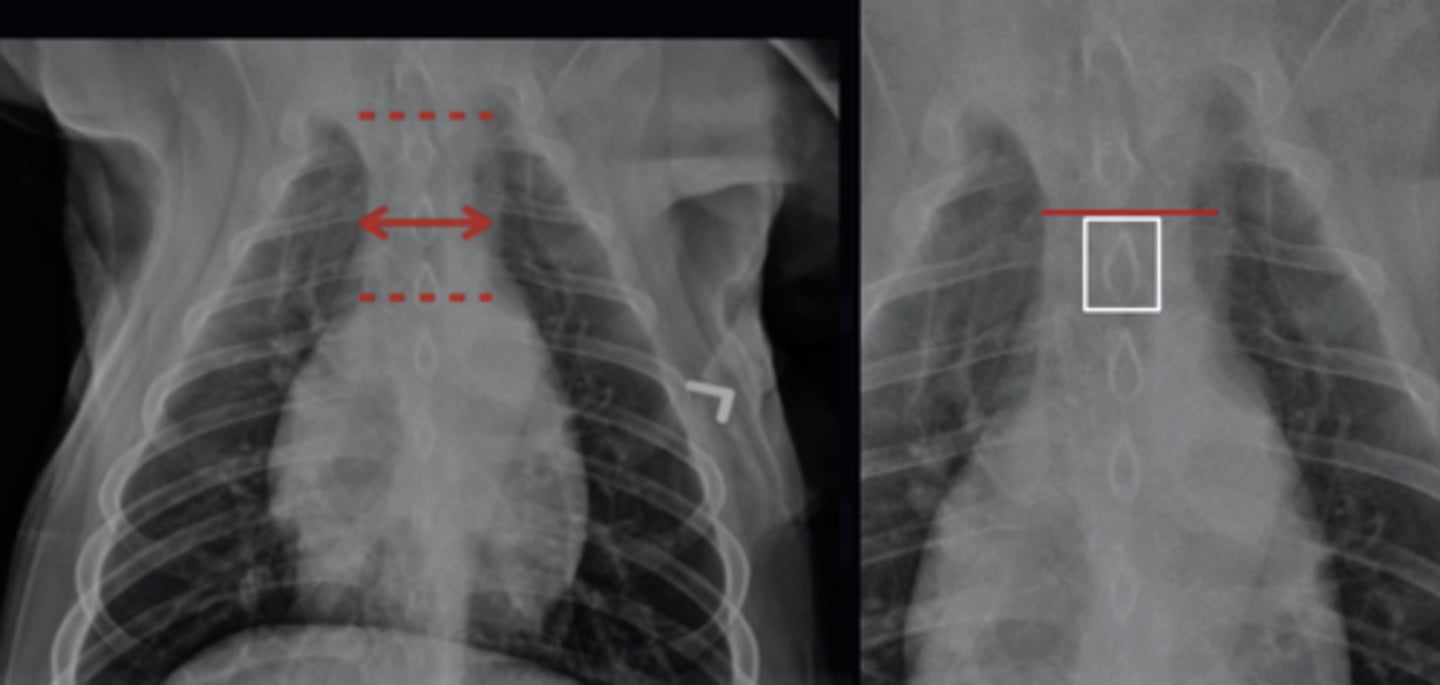
Describe the Size of The Heart in terms of:
1. 2/3's Assessment
2. Intercostal Width in Dogs
3. Intercostal Width in cats
4. How to Count Ribs
1. On the Lateral + VD Views, Heart is 2/3's width/height of the thorax (cat is 50% of thorax on VD)
2. Lateral Views. 2.5-3.5 intercostal spaces wide
3. Lateral Views. 2 Intercostal spaces wide
4. Ribs not superimposed. Follow ribs up from sternum → Find cranial rib of pair → count from cranial rib to cranial rib
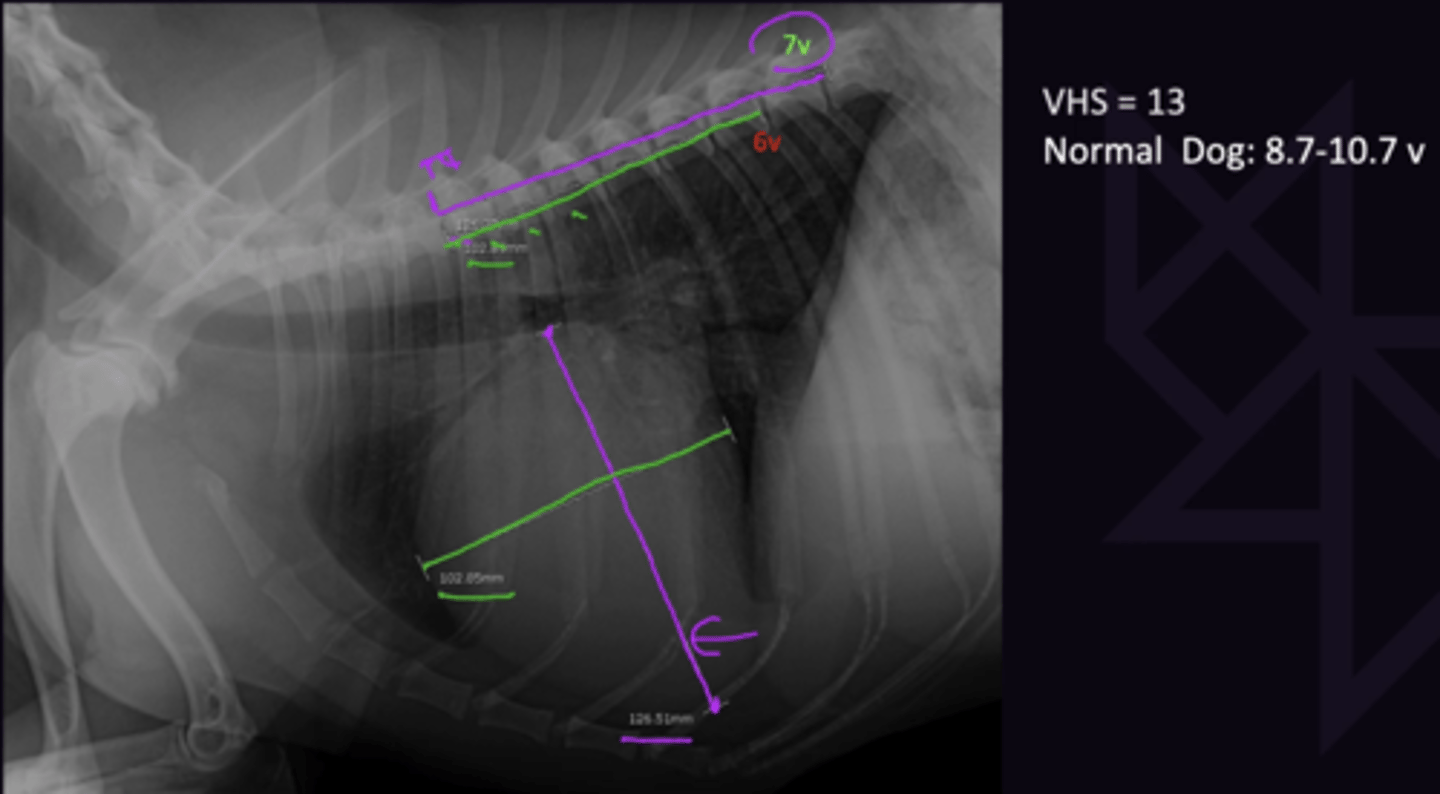
Describe Vertebral Heart Score (VHS) in terms of:
1. Definition
2. Normal VHS in Dogs
3. Normal VHS in Cats
1. Objective way of assessing heart. Does not replace subjective assessment
2. 8.7 - 10.7 v
3. Not Reliable. 6.9 - 8.1 v
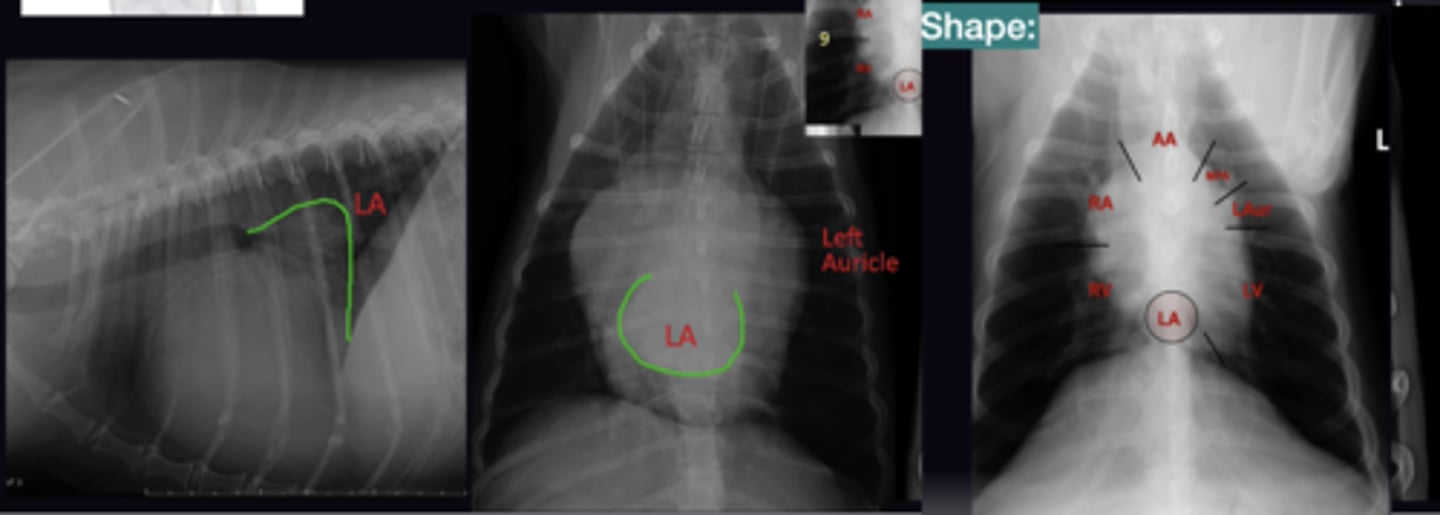
Describe Vertebral Left Atrial Size (VLAS) in terms of:
1. Definition
2. Normal VLAS
1. Measurement from the ventral aspect of the carina to the junction between the CVC + HEart
2. Up to 2.3 Vertebrae
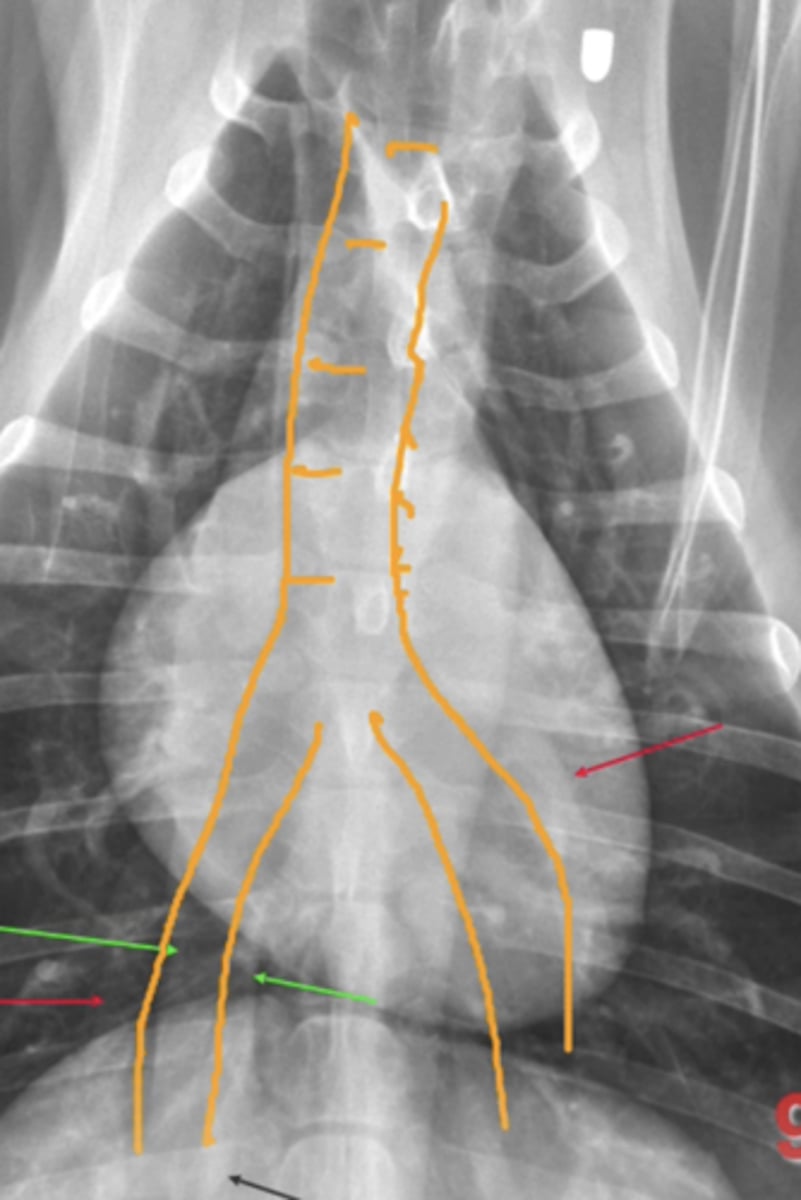
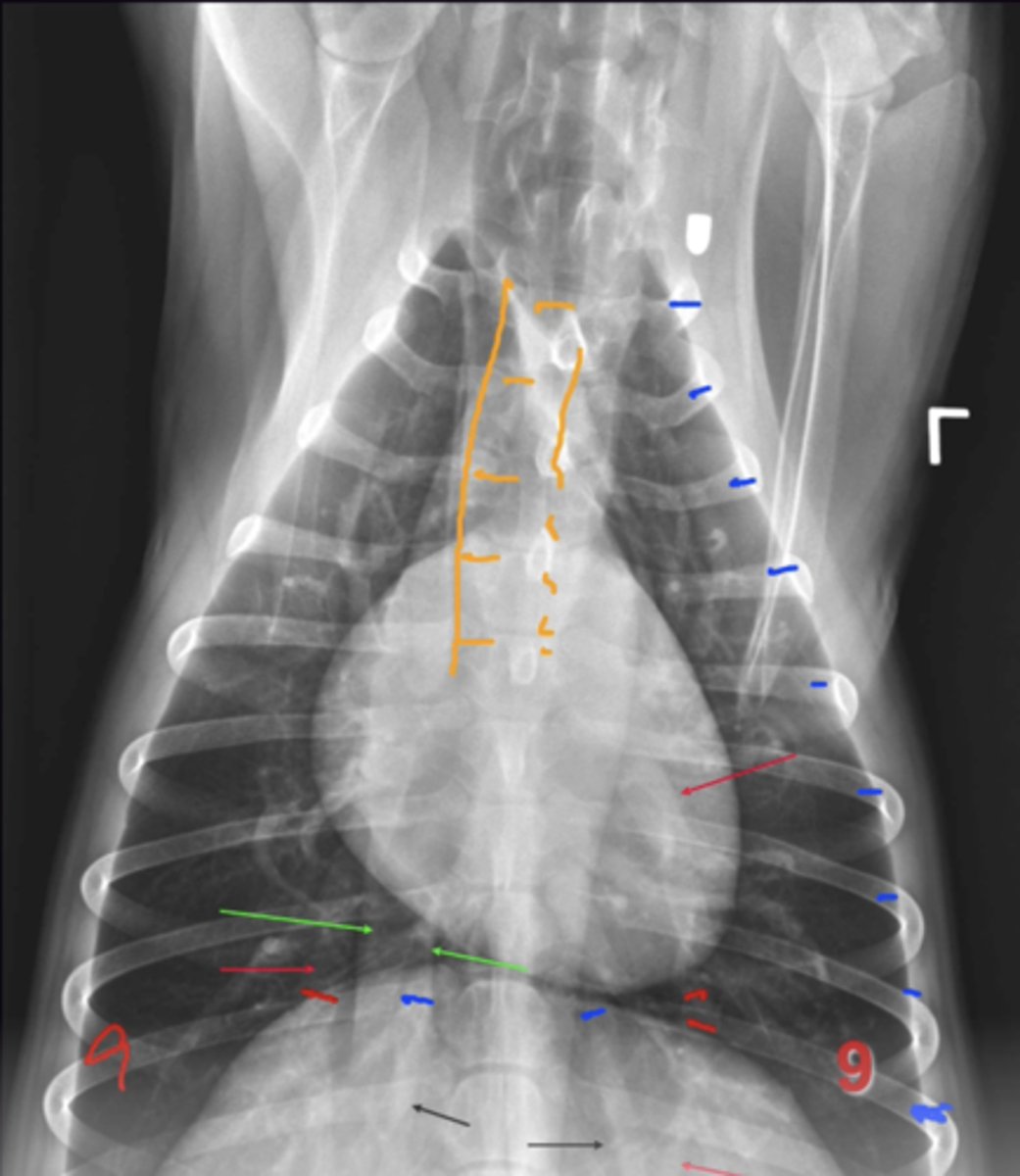
Describe Where to Find the Following on a VD View of the Dog:
1. Left Atrium
2. Left Auricle
3. MAin Pulmonary Artery (MPA)
"Clock Face Analogy"
1. On Spine (6 O'Clock) Opacity over spine indicates pathology
2. 2-3 O'Clock
3. 1-2 O'Clock
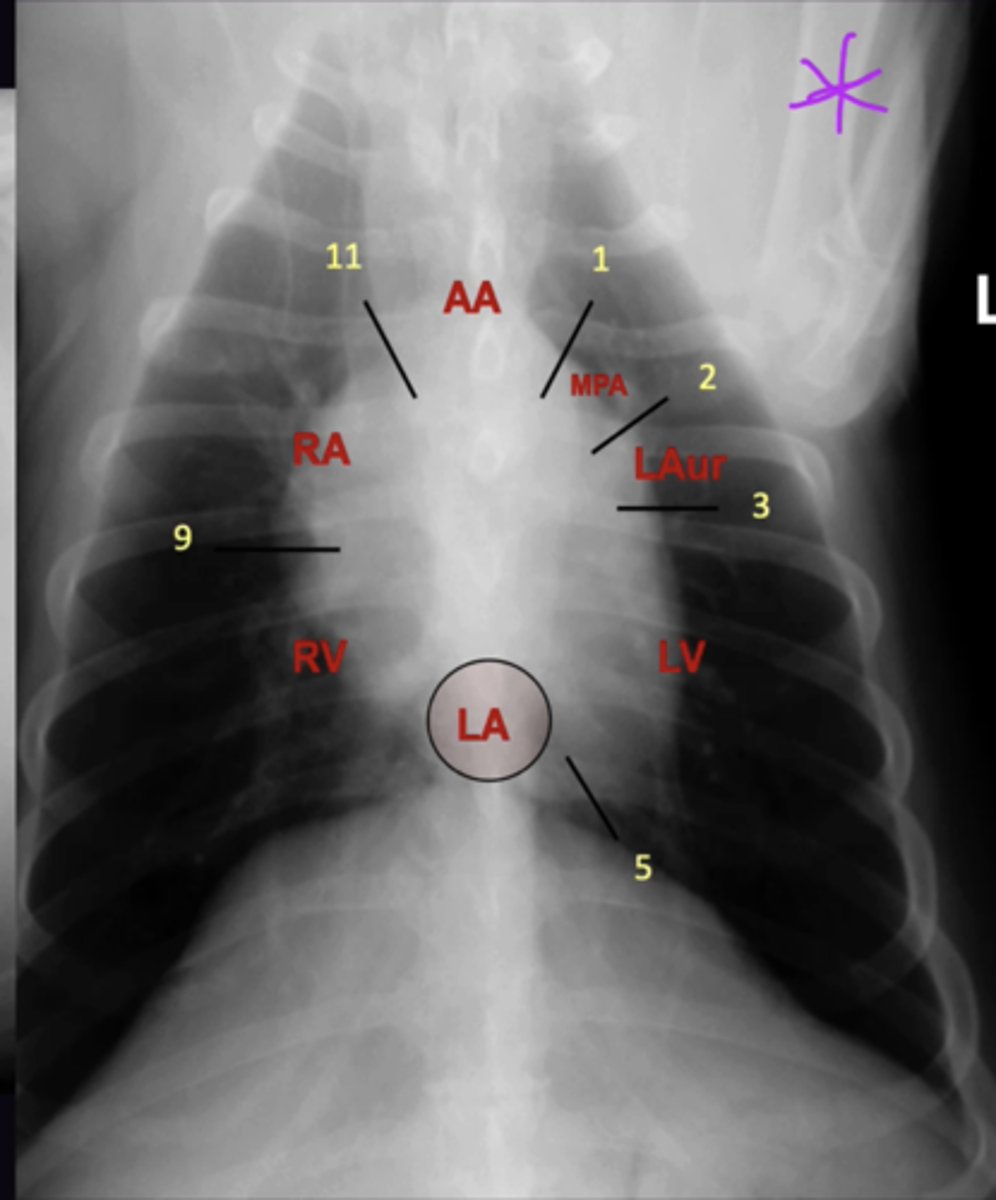
Describe the Shape of the Heart in terms of:
1. Main "Bulges" That Can be Assessed
2. Ride Side Heart Enlargement
1. Left Atrium, Left Auricle, main Pulmonary Artery (VD)
2. Radiography is not accurate for right side enlargement
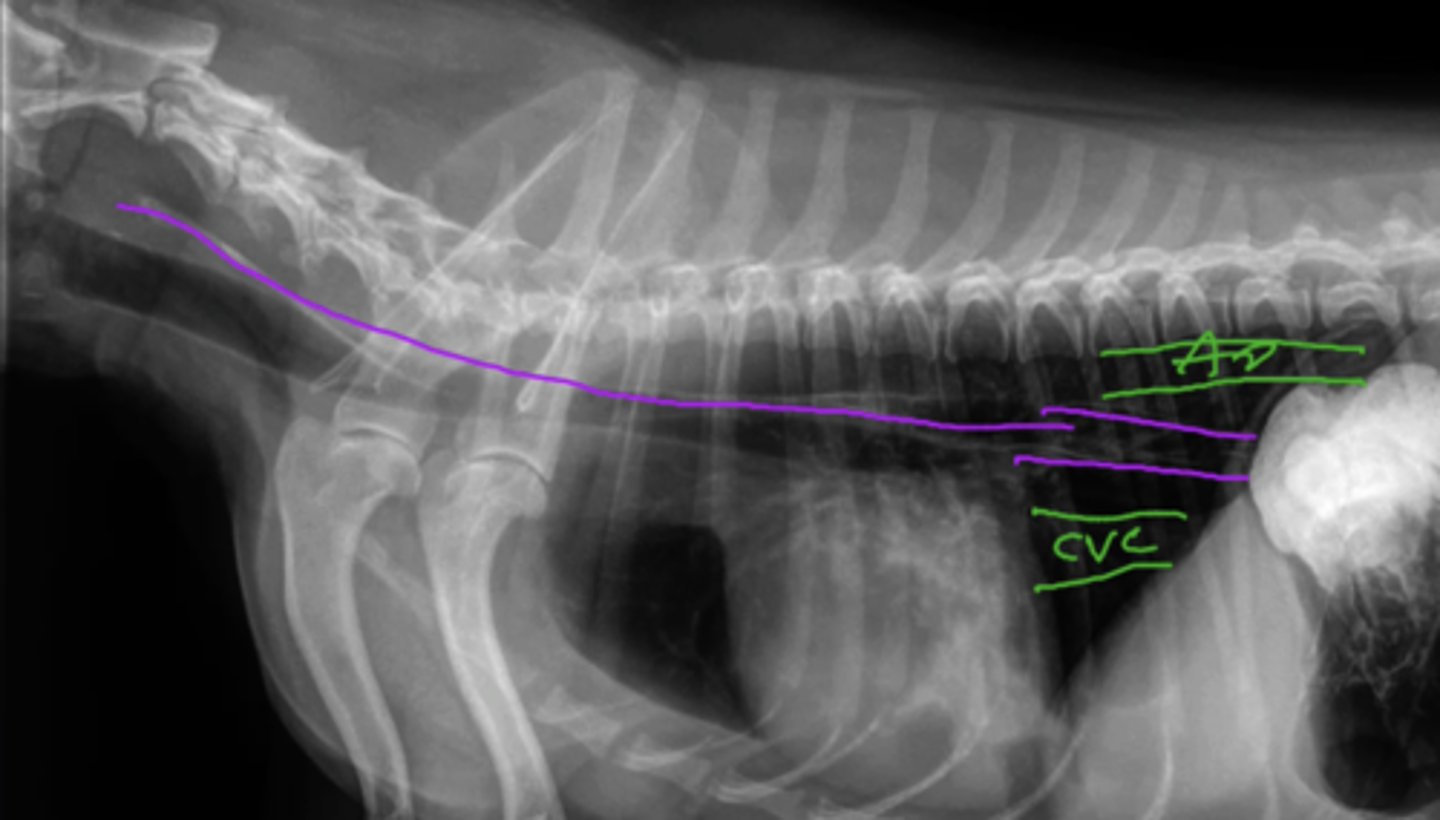
Describe the Normal Appearance of the Following in the Thorax:
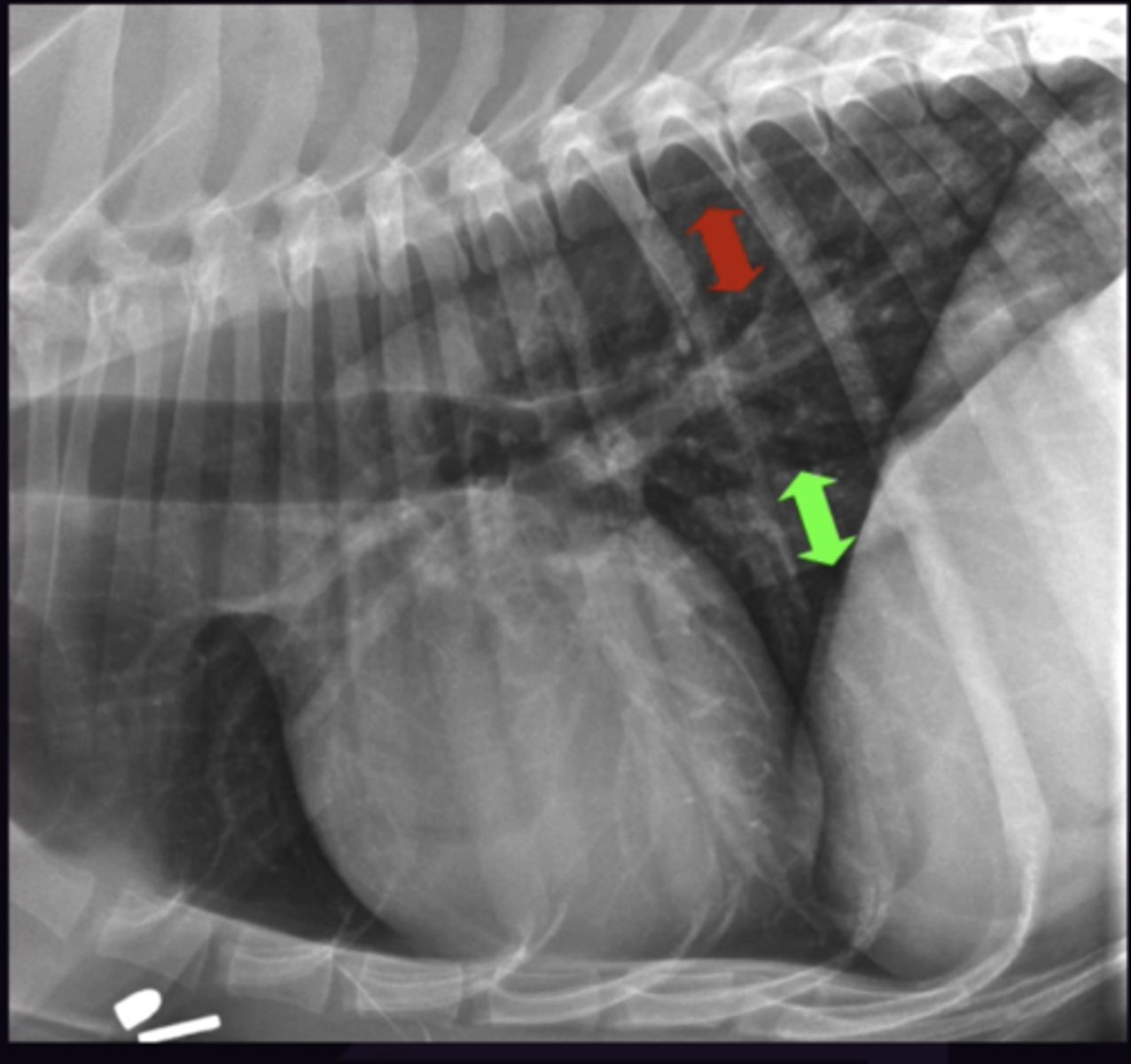
1. Caudal Vena Cava (CVC)
2. Aorta (Ao)
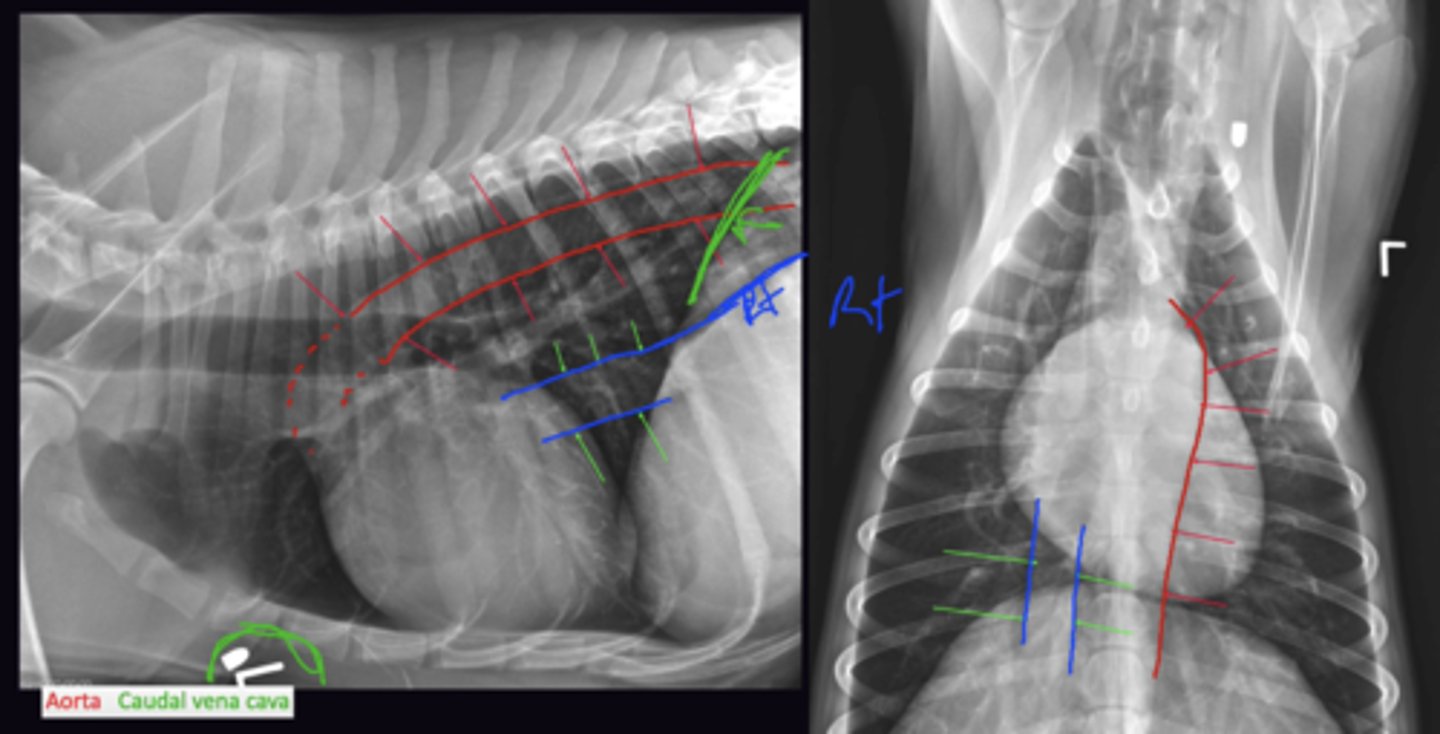
Describe the Size of the Caudal Vena Cava (CVC) in terms of:
1. Considerations
2. When To classify CVC as Dilated
1. Varies with cardiac cycle so care when calling it small/dilated
2. Dilated if 1.5x the width of the Aorta on the lateral view
Describe the Normal Appearance of the Following in the Thorax:
1. Pulmonary Arteries
2. Pulmonary Veins
3. Bronchus
1. "Dorsal + Lateral (Lateral + VD View)
2. "Ventral + Central" (Lateral + VD View)
3. Between Arteries and Veins
Describe the Systematic Approach to Locating the Bronchus, PA, and PV
Find Bronchus First → Look for vessels on each side:
On VD/DV, the bifurcation of the trachea is at the 5th rib, follow caudal lobar bronchi out from here
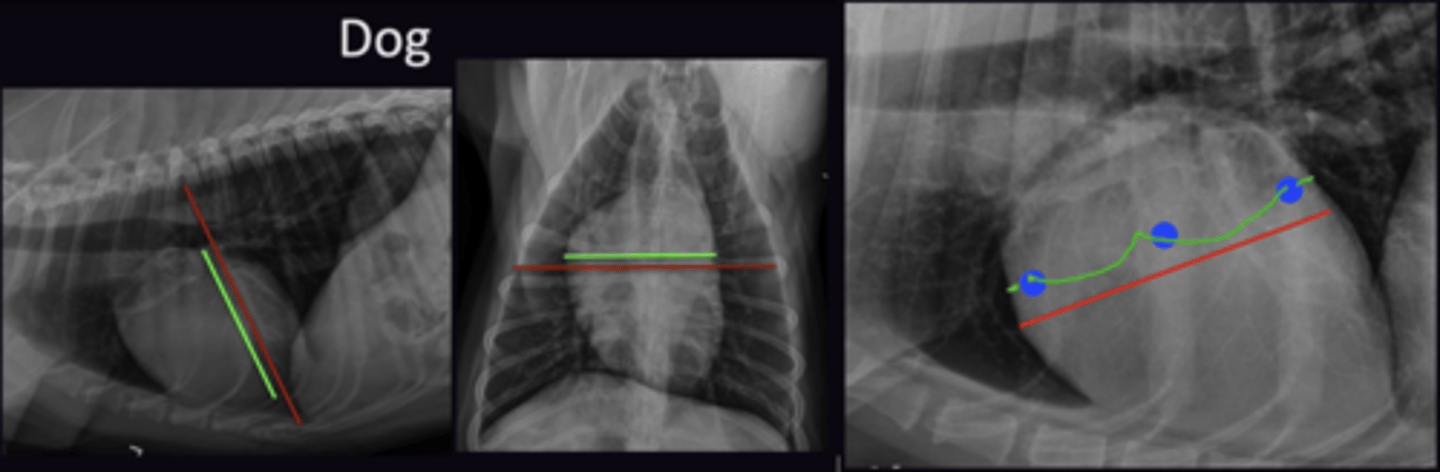
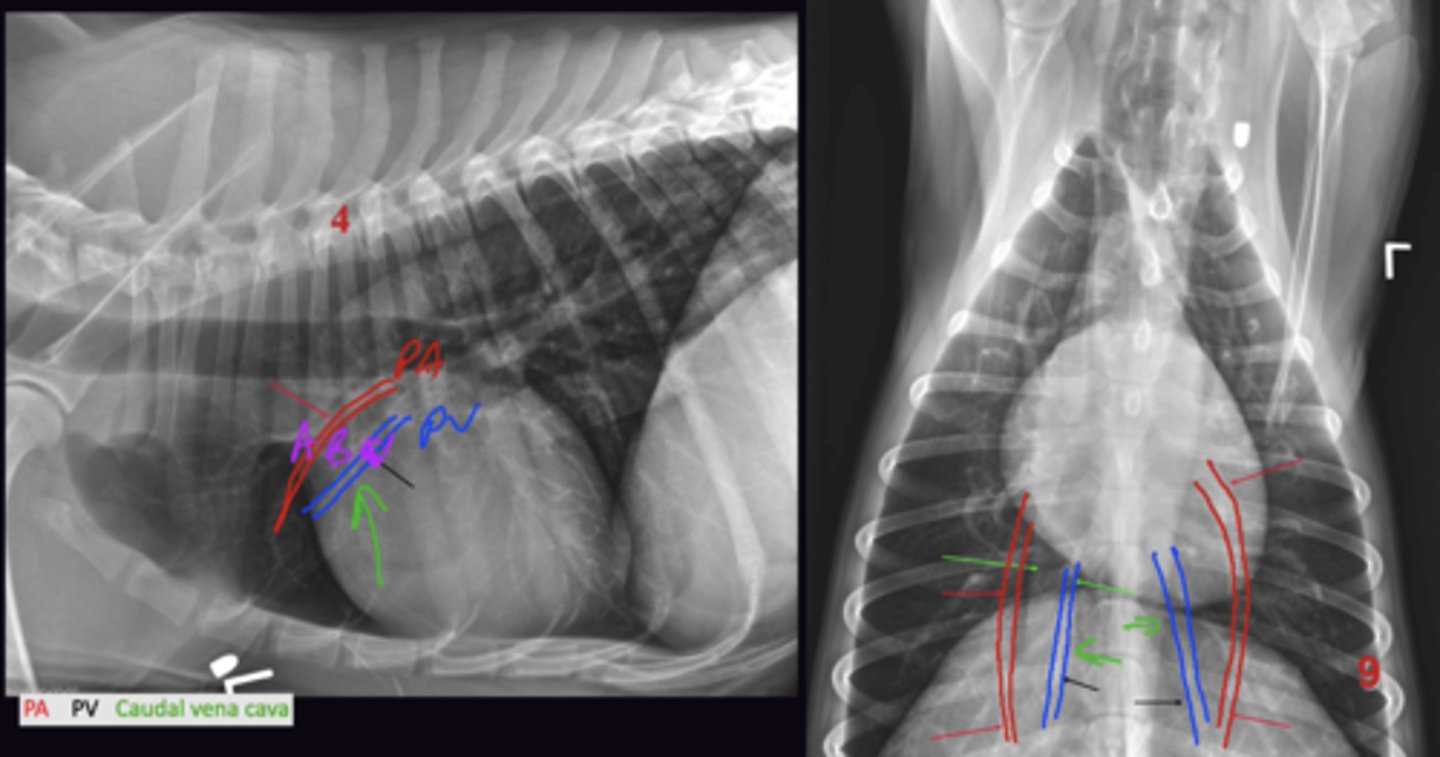
Describe the 2 Tests of the PA + PV
Must Pass both Tests
Test 1: Are the PA + PV the same width
Test 2: Are they normal compared to the ribs
Describe the Tests of the PA +PV on the Lateral View in terms of:
1. What can be Assessed
2. Test 1
3. Test 2
4. Choice of Left/Right Lateral View Assessment
1. Cranial lobar vessels
2. Are they the same width
3. Taken on the 4th Rib. Look at the width of the PA + PV where they cross the 4th ribs. Compare this to the width of the 4th rib near the spine (Normal PA + PV is approx. 3/4 the width of the rib)
4. Check both the left and right lateral as one will be better than the other (Usually left lateral)
Describe the Tests of the PA +PV on the DV/VD View in terms of:
1. What can be Assessed
2. Test 1
3. Test 2
4. Choice of Left/Right Lateral View Assessment
1. Caudal Lobar Vessels
2. Are they the same Width
3. Taken on the 9th rib,. Look at the width of the PA + PV where the 9th rib crosses them. Width of the Vessels should be less than width of the rib (Normal PA + PV is approx. 3/4 the width of the rib)
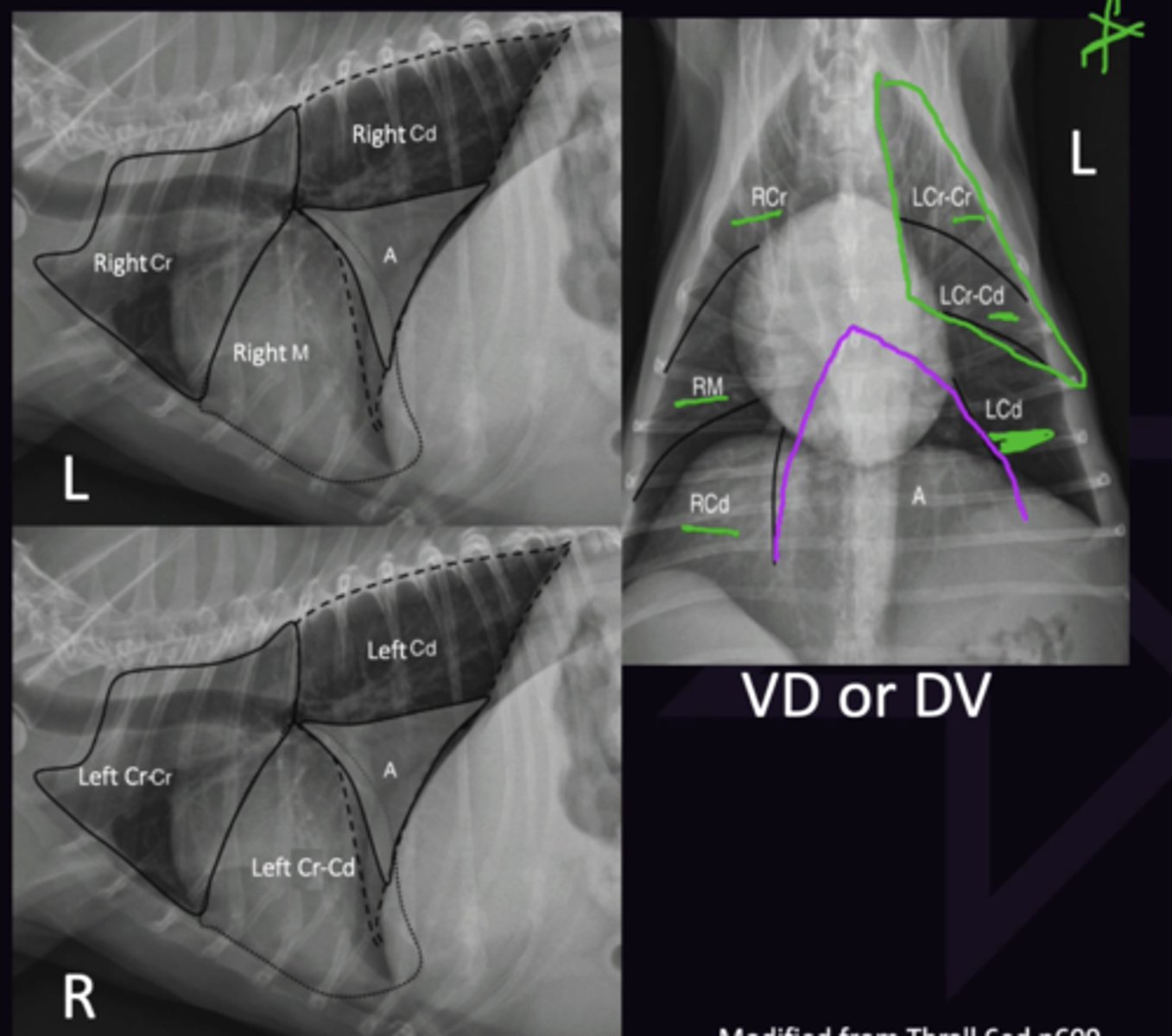
Describe the Lung Lobe Anatomy of the Following Lungs:
1. Right Lung
2. Left Lung
3. What Should be seen on Normal lung radiography
Borders not seen as they are same opacity and share a border so they efface
1. Cranial, Middle, Caudal, Accessory (On both sides but considered right lobe). Observed on a Left Lateral View
2. Cranial (Cranial Part), Cranial (Caudal Part), Caudal. Observed on a Right Lateral View
3. Only Blood Vessels
Describe why Pathology is Better Seen in an Aerated (Upper Lung)
Lung pathology is best seen in the non-dependant (uppermost) lobes as these contain more air to contrast against the soft tissue opacity pathology

Describe Pleura Assessment Using Radiography in terms of:
1. Parietal + Visceral Pleura + Pleural Space Locations
2. Pleural Effusion
3. Pneumothorax
4. If Gas + Fluid are not evident on radiograph
1. Parietal pleura lines thoracic wall, Visceral pleura lines lungs. Space inbetween is Pleural Space (Usually empty)
2. Fluid in the pleural space
3. Gas in the pleural space
4. Pleura deemed normal
Describe the Assessment of the Mediastinum Using Radiography in terms of:
1. 2 Things You Can See
2. 2 Things You Can't See
1. Cranial Mediastinal Width + Trachea
2. Lymph Nodes + Oesophagus
Describe the Assessment of the Cranial Mediastinum in terms of:
1. Where the Cranial mediastinum runs from
2. Structures
3. How to Measure the Width of the Cranial Mediastinum
1. First ribs to the cranial aspect of the Heart. Measure in the middle of these locations
2. Trachea, Oesophagus, Vessels, Lymph nodes. All structures are soft tissue opacity (except trachea) so they efface.
3. Measure on VD View. Locate first ribs and cranial heart border. Measure the Width halfway between these structures. Normal width is <2x the width of the vertebra (Wider in brachiocephalic/obese dogs
Describe the Assessment of the Trachea in terms of:
1. Where the Trachea Runs From
2. Breed Differences
3. Cat vs Dogs Differences
1. Neck to 5th Rib, curves to the right side but usually returns to middle.
2. Angle of trachea with spine can vary between breeds / Brachycephalic animals
3. Cates have natural lordosis of the thoracic spine. Cranially trachea is parallel to spine, caudally rachia is at an angle to the spine
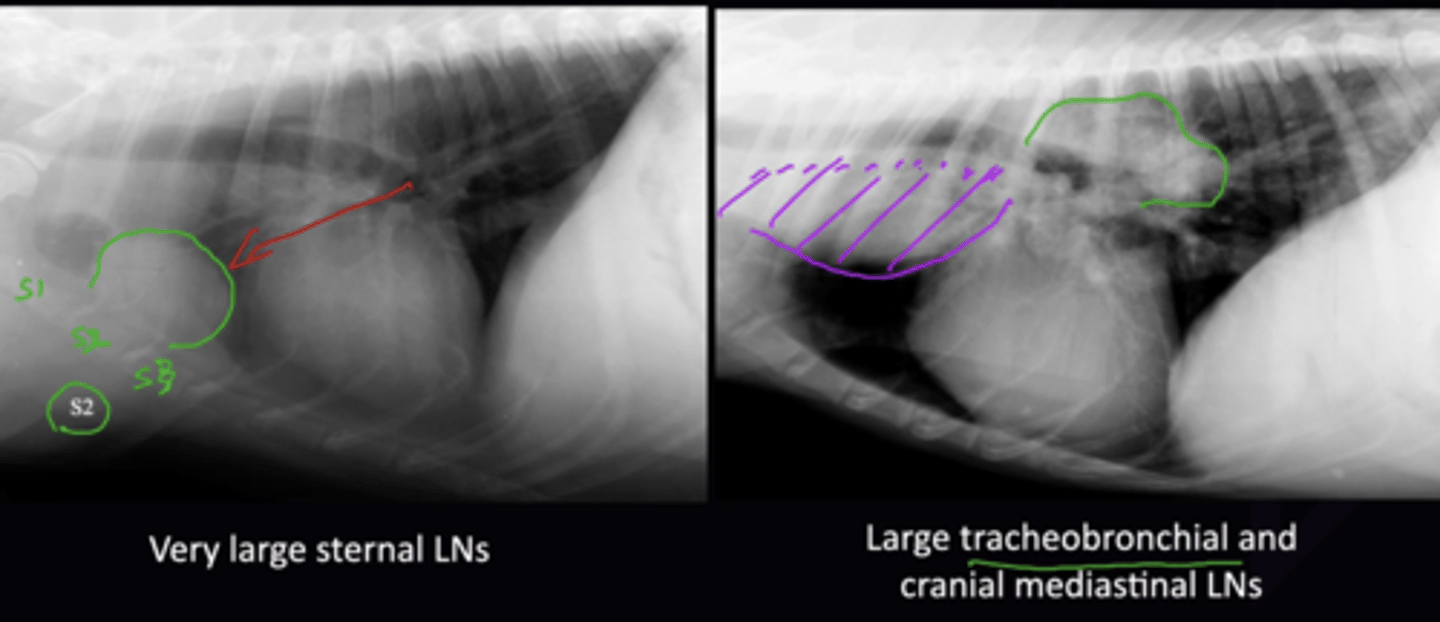
Describe the Assessment of the Lymph Nodes in terms of:
1. Sternal LN Location
2. Cranial Mediastinal LN Location
3. Tracheobronchial LN Location
Lymph Nodes are Normally Not Seen
1. At the Level of S2 (Sternal 2) in dogs, and S3 in Cats
2. Multiple LNs along the cranial mediastinum ventral to the trachea. Efface so cannot be seen until they cause cranial mediastinal mass
3. LNs at the carina. Displace the caudal aspect of the trachea ventrally
Describe the Assessment of the Oesophagus in terms of:
1. Where Oesophagus is seen on Lateral View
2. Where Oesophagus is Seen on VD/DV View
Normally Not Seen
1. Sits between Aorta and CVC
2. Superimposed on mediastinum/midline and often not seen (even when enlarged)
Radiology 6: Normal Abdomen
Radiology 6: Normal Abdomen
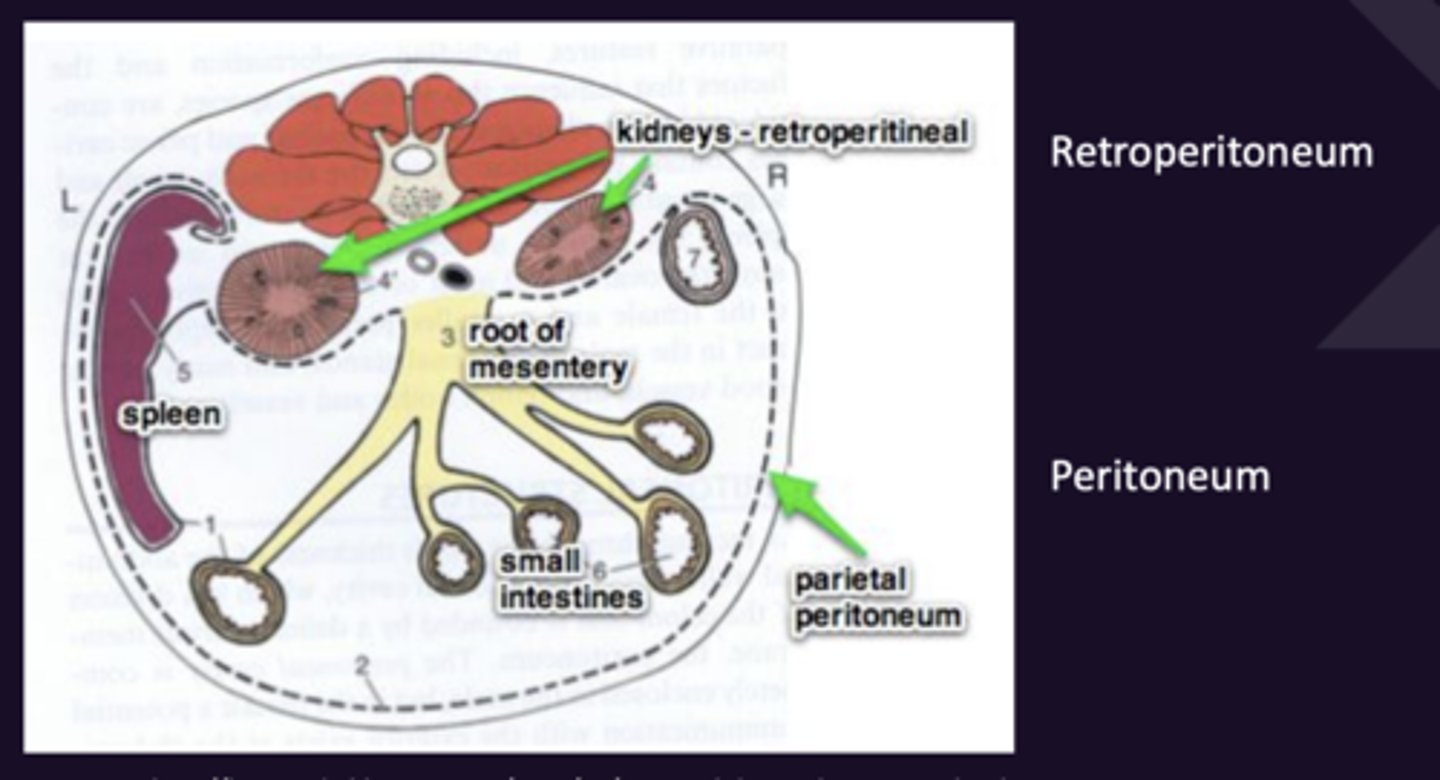
Describe the Following Anatomy of the Abdomen:
1. Peritoneum
2. Retroperitoneum
Do Not Communicate With Each Other
1. The serous membrane lining the abdominal cavity. Most abdominal organs are inside the peritoneum.
2. The space in the dorsal abdomen, outside the peritoneum, between the peritoneum and the dorsal abdomen (Contains Kidneys)
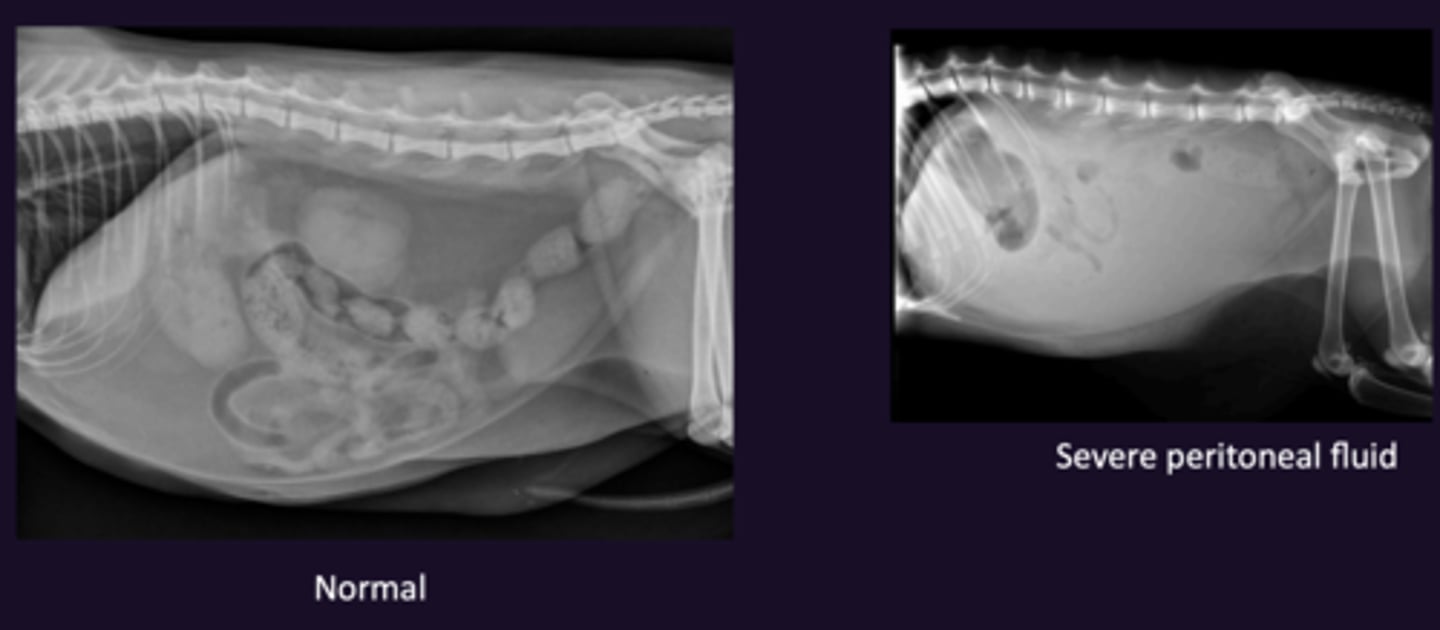
Describe Serosal Detail in terms of:
1. Definition
2. What ↓ Serosal Detail Usually Indicates
3. What Else Can Cause ↓ Serosal Detail
1. How well the organs can be seen in the peritoneum
2. Indicates abdominal fluid
3. Mass, Fluid, Skinny, Young, Radiograph Technique
Describe the Assessment of the Retroperitoneum in terms of:
1. Views Assessed
2. Muscle Assessment
3. Fat Assessment
4. Kidney Assessment
1. Lateral Views
2. How Well muscles are seen (Ventral to spine)
3. Is normal fat opacity seen
4. Are the Kidneys seen well
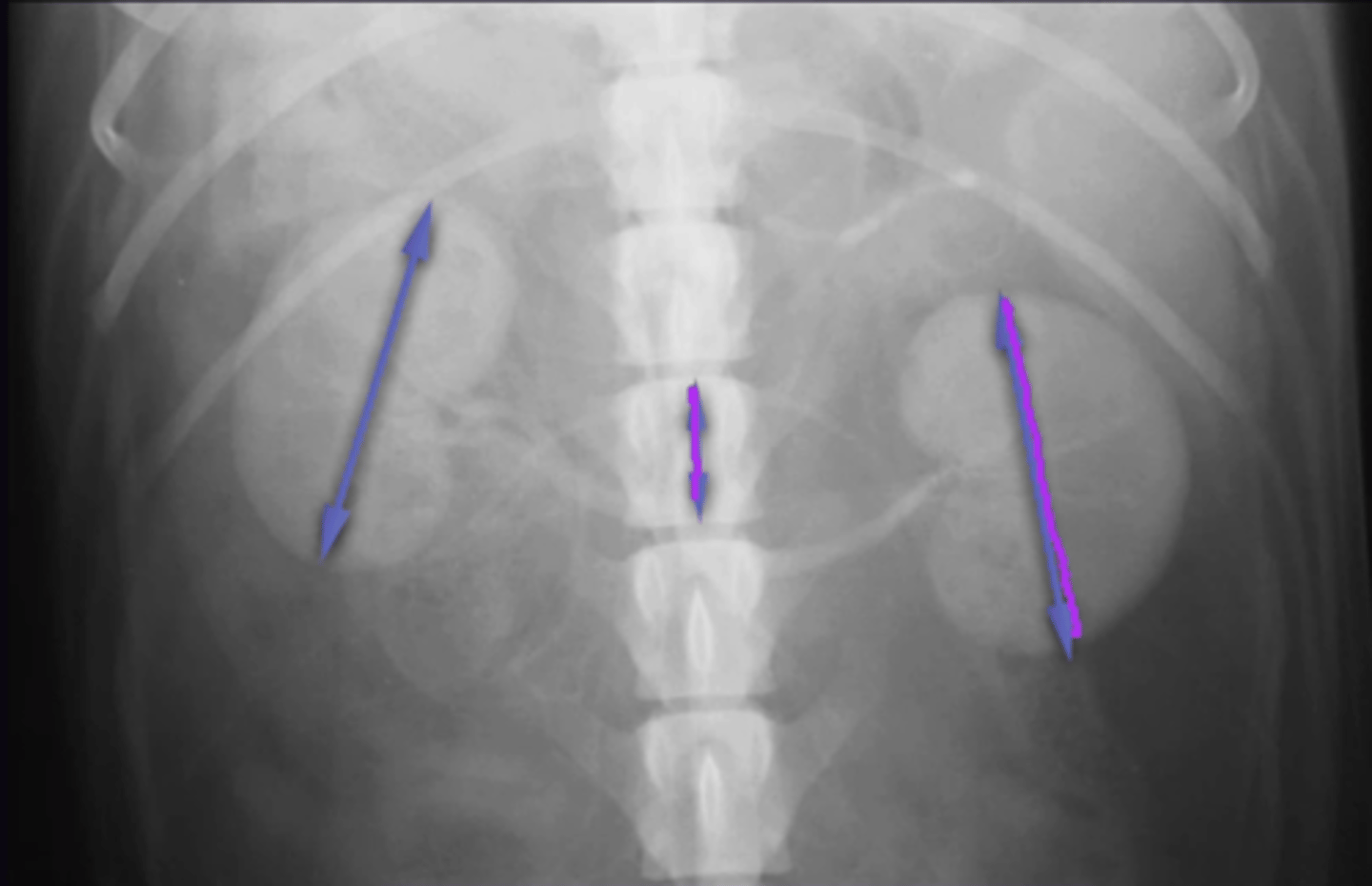
Describe Assessment of the Kidneys on Radiographs in terms of:
1. Left vs Right Kidney Anatomy
2. Dog Right Kidney Visibility on Lateral Radiograph
3. Dog Right Kidney Visibility on VD Radiograph
4. Cat Kidney Visibility on Radiograph
1. Right Kidney more cranial, Caudal pole of Right kidney should be in line with middle of left kidney
2. Can only see caudal pole as cranial pole is effacing with liver
3. Not seen on VD in most dogs as cranial pole is effacing the liver (Seen on cats as kidney doesn"t efface)
4. Both seen on both views (More parallel + more mobile)
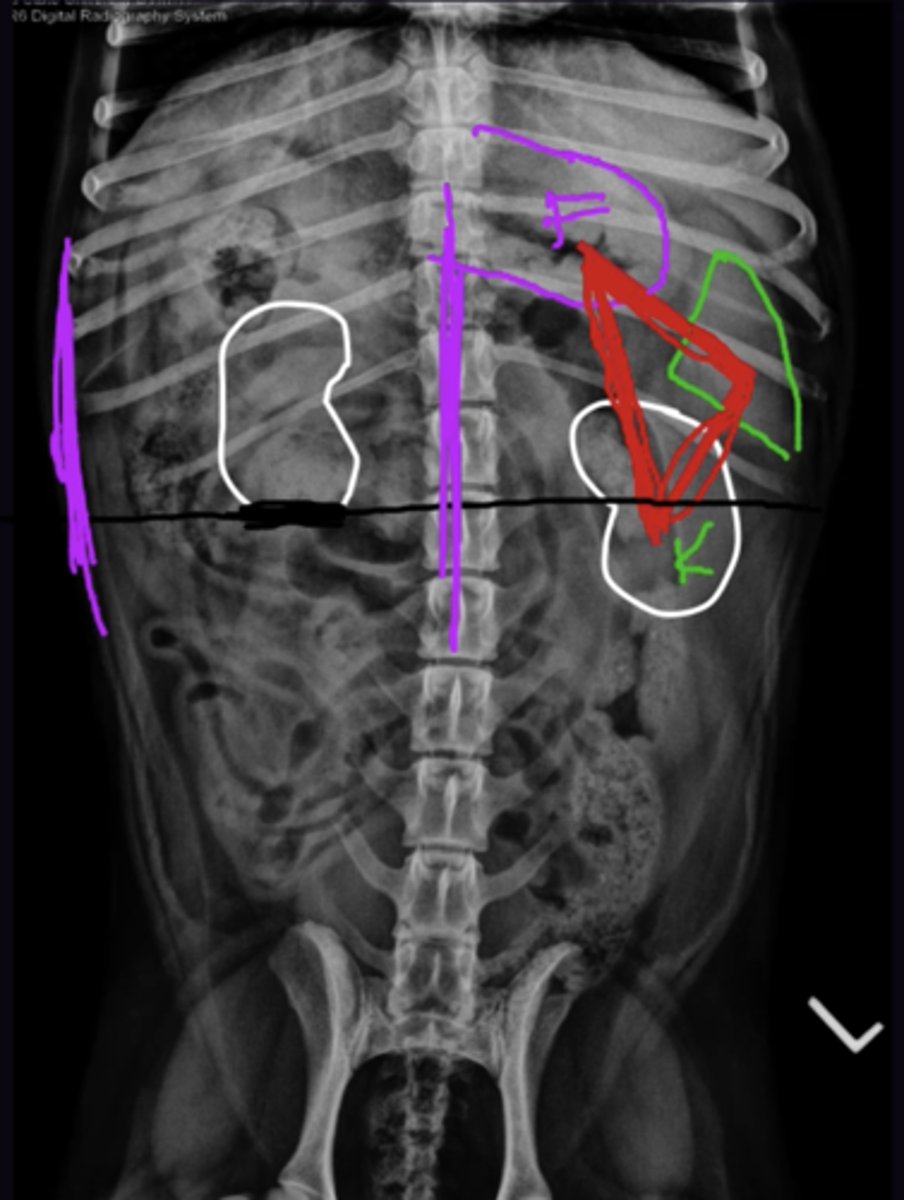
Describe Assessment of the Kidneys on Radiographs in terms of:
1. 2 Things That are Assessed
2. What View is Assessed
3. How to Assess Kidney Length
4. Normal Kidney Size in Dogs
5. Normal Kidney Size in Cats
1. Are they the same size, are they normal size compared to L2
2. Only VD
3. Length Kidney : Length L2
4. 2.5-3.5
5. 1.9-2.6
Describe Assessment of the Liver on Radiographs in terms of:
1. Cranial Margin
2. Caudal Margin
3. Liver Size on Lateral View
4. Liver Size on VD View
1. Diaphragm
2. Stomach (Follow the liver caudally from the diaphragm until some gas is seen, which is gas in the stomach)
3. Asses Gastric Axis + caudoventral margin (rounded margin indicates hepatomegaly)
4. Subjective. Asses if liver is normal size + that liver extends from diaphragm to stomach (Stomach is "U" shaped if liver is large)
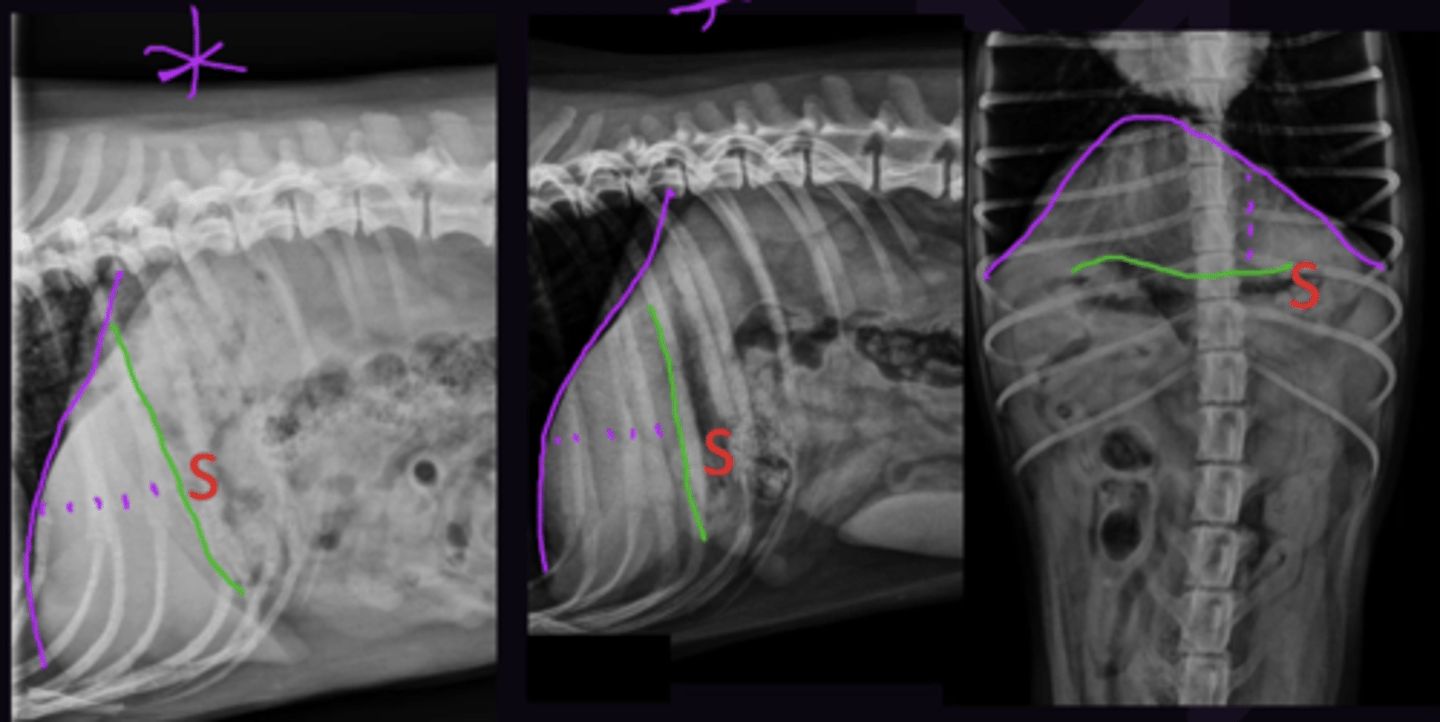
Describe the Gastric Axis as an Estimate of Liver Size in terms of:
1. Definition
2. Pylorus
3. Fundus
4. Normal Axis
1. Line Between the Fundus and Pylorus (Only Assessed on lateral view)
2. Needs to be seen to make gastric axis; always seen on lateral views
3. Can be assumed (In cranial dorsal abdomen next to diaphragm)
4. Axis should be between perpendicular to spine and parallel to ribs
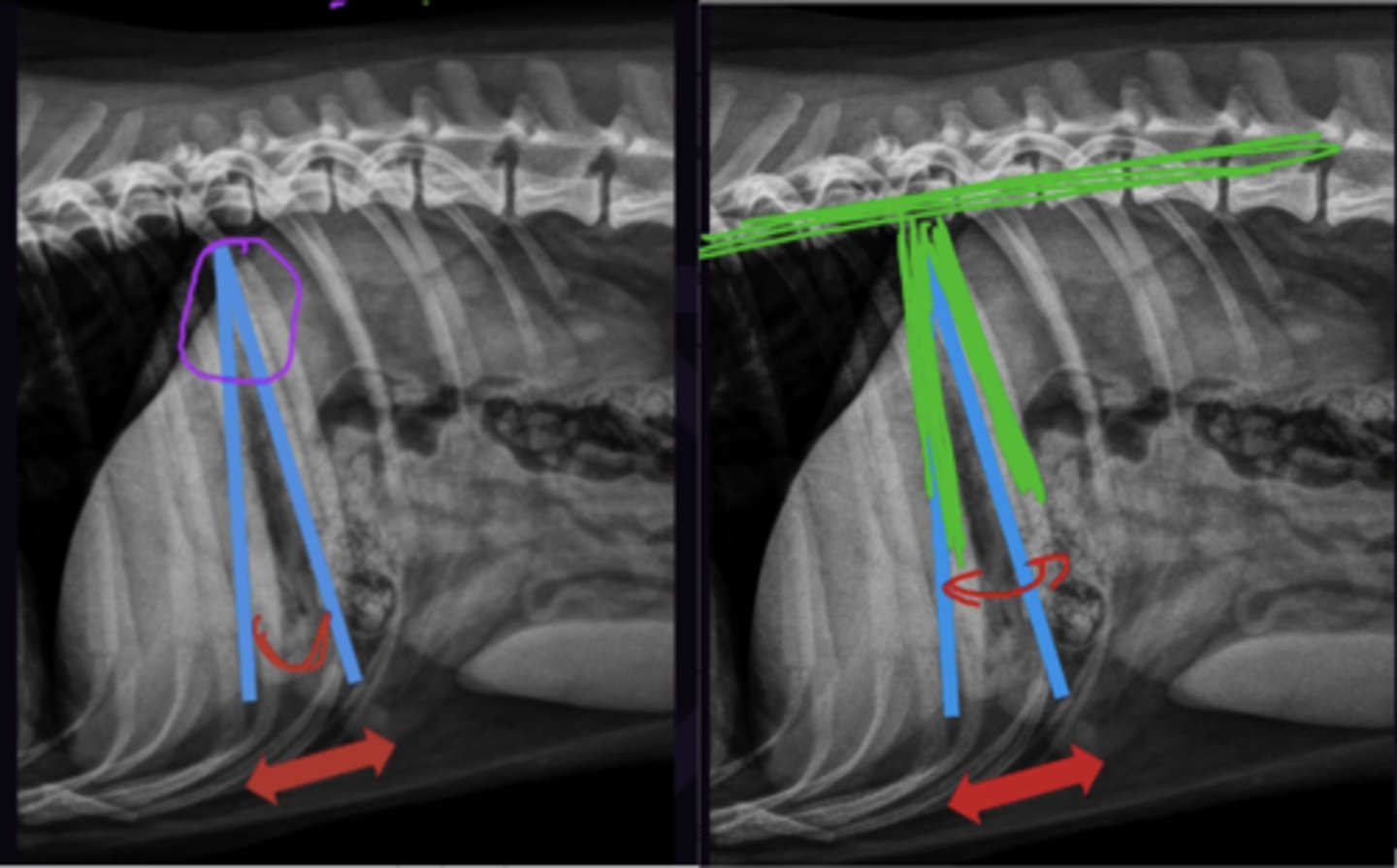
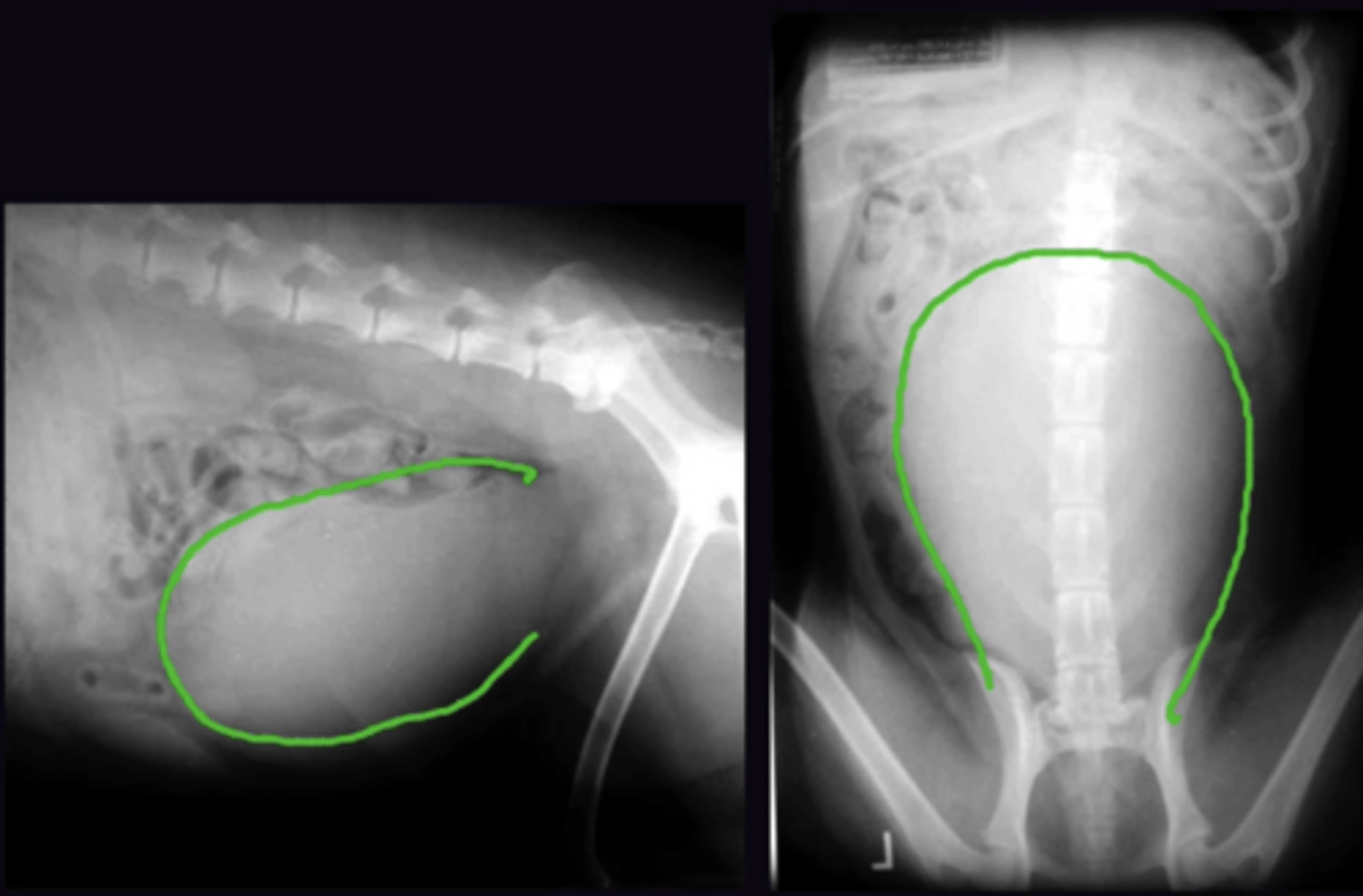
Describe Assessment of the Spleen on Radiographs in terms of:
1. Head of Spleen
2. Tail of Spleen
3. What Can be Seen in Dogs
4. What Can be Seen in Cats
1. Seen only on VD View. Always seen in Cats + dogs
2. Seen only on Lateral View. seen anywhere between liver + bladder
3. Head of Spleen, Normal for tail to be seen/not seen in dogs
4. Head of Spleen, Tail should not be seen in cats
What are the Hollow Organs Assessed on Radiographs
1. Stomach
2. Small Intestine
3. Colon
4. Duodenum (Superimposed on Ascending Colon)
5. Caecum (Dog Only, superimposed on small intestine)
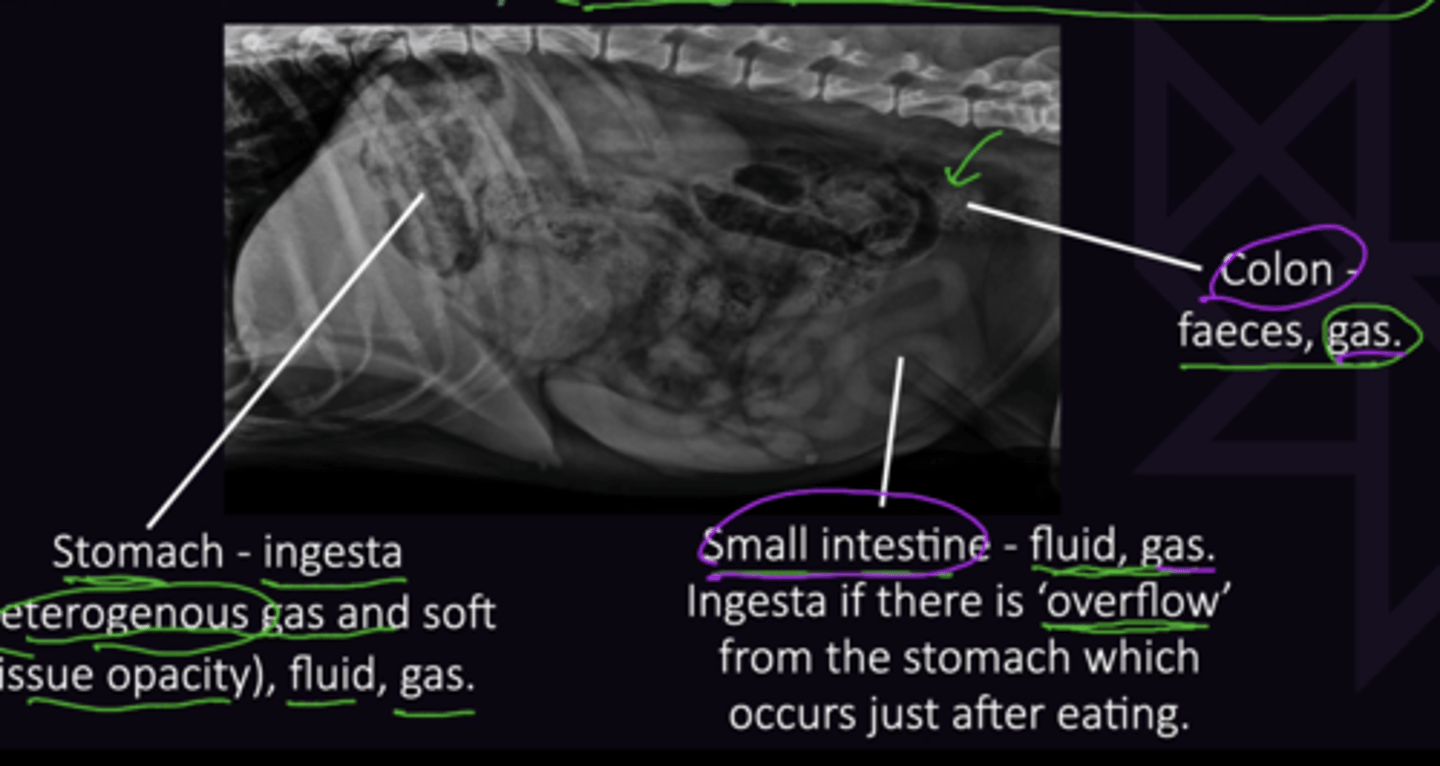
Describe what is Normal Content for the Following:
1. Stomach
2. Small Intestine
3. Colon
1. Ingesta (Heterogenous gas + soft tissue opacity) fluid, gas
2. Fluid, gas (Ingesti if there is "overflow" just after eating)
3. Faeces, Gas
Describe the Assessment of The Stomach on Radiograph in terms of:
1. Stomach Location
2. Fundus Location
3. Pylorus Location
1. Lateral + VD: First gas seen caudal to the liver. Use Triad on VD
2. Dogs Like Fun (Dorsal, Left, Fundus) Dorsal and Left (Gas Opacity on Right Lateral View)
3. Ventral and Right (Gas Opacity on Left Lateral View)
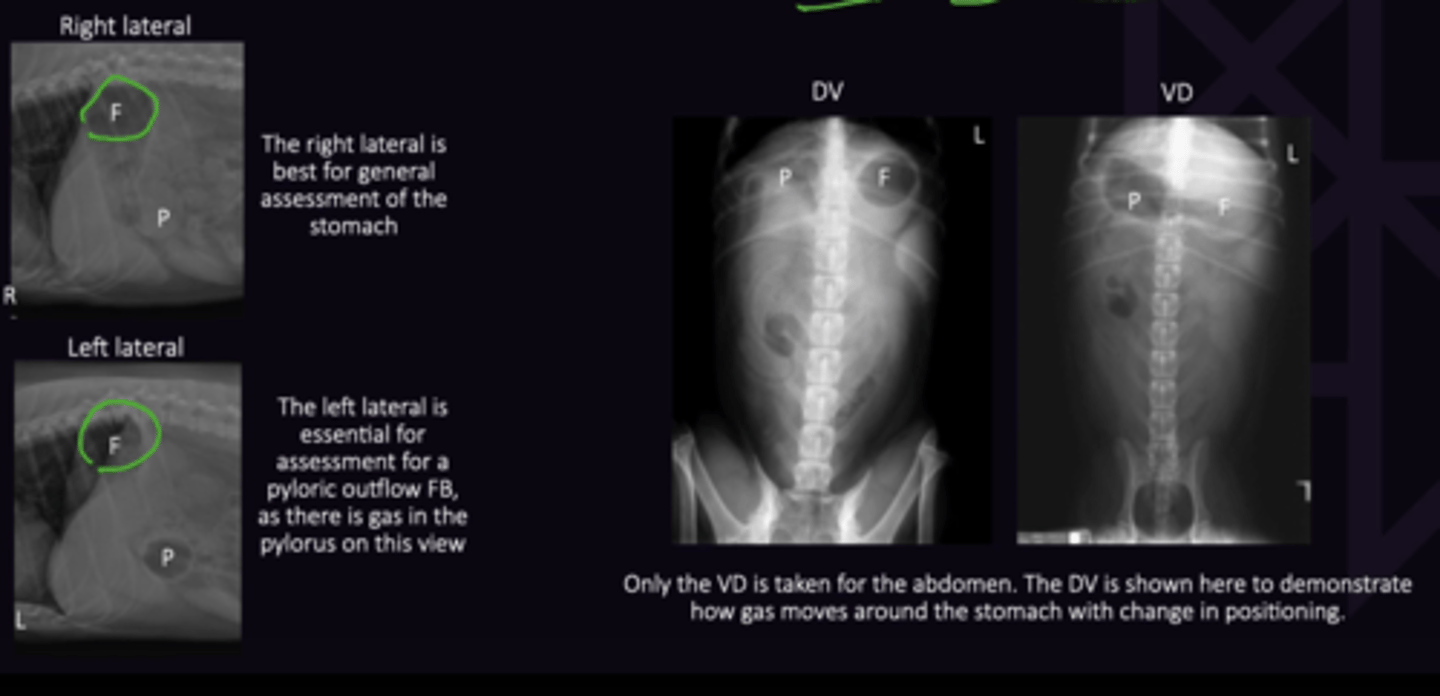
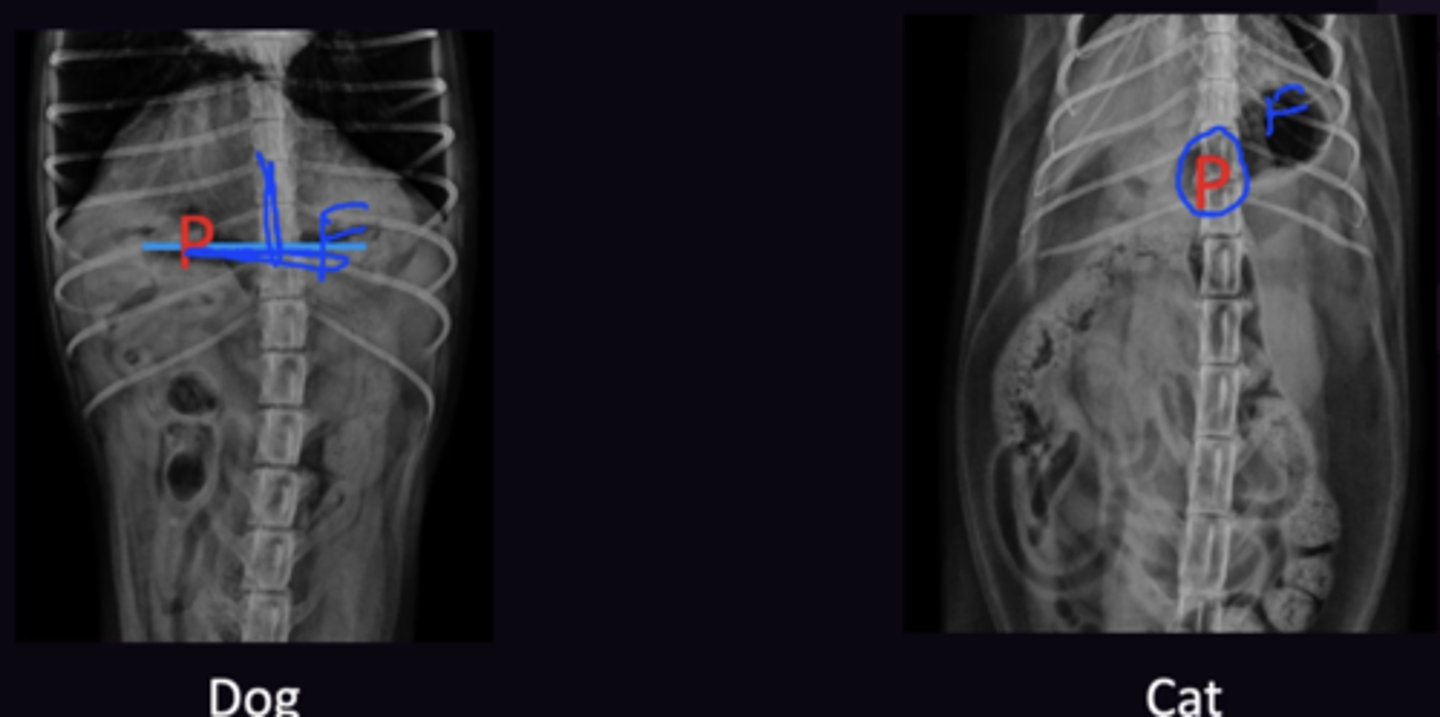
Describe the Location of the Pylorus in the Dog vs. Cat in terms of:
1. Lateral View
2. Cat Differences in VD Views
1. Same in Dog and Cat
2. Pylorus is on midline, not on the right side as it is in dogs
Describe the Content + Size of the Stomach on Radiographs in terms of:
1. What it depends on
2. When Dog Stomach will be Empty after Meal
3. When Cat Stomach will be Empty after Meal
4. General Rule of Thumb for fasting Before Radiography
1. When Animal last ate
2. 24h
3. 8h
4. Fast 12 Hours Before Radiography, Time of last meal needs to be known before accessing GIT
Describe the Assessment of the Small Intestine on Radiograph in terms of:
1. Normal Appearance
2. How Small Intestine Width is Measured
3. Normal Width of Small Intestine In Dogs
4. Normal Width of Small Intestine In Cats
5. Normal Small Intestine Size Compared to Each Other
1. Smooth, Sweeping, continuously curving tubes, solid circles/rings in transverse
2. Measure Serosa → Serosa.
3. <1.6 x L5 height at narrowest part (Middle)
4. <2 x L5 height at endplate
5. Similar Width. If greater than 1.5x the size of other small intestine = indicates Ileus, obstruction, or recent meal
Describe the Assessment of the Duodenum on Radiograph in terms of:
1. Superimposition
2. Size
3. Considerations in The Cat
1. Superimposed on ascending colon on all views → often not seen. Best Seen on left lateral (Gas floats into Duodenum)
2. Normally slightly larger than other parts of the small intestine → Hard to tell a ileus/obstruction → follow up 12 hours late if concerned
3. Also superimposed, but small piece of proximal duodenum seperate from ascending colon may be seen
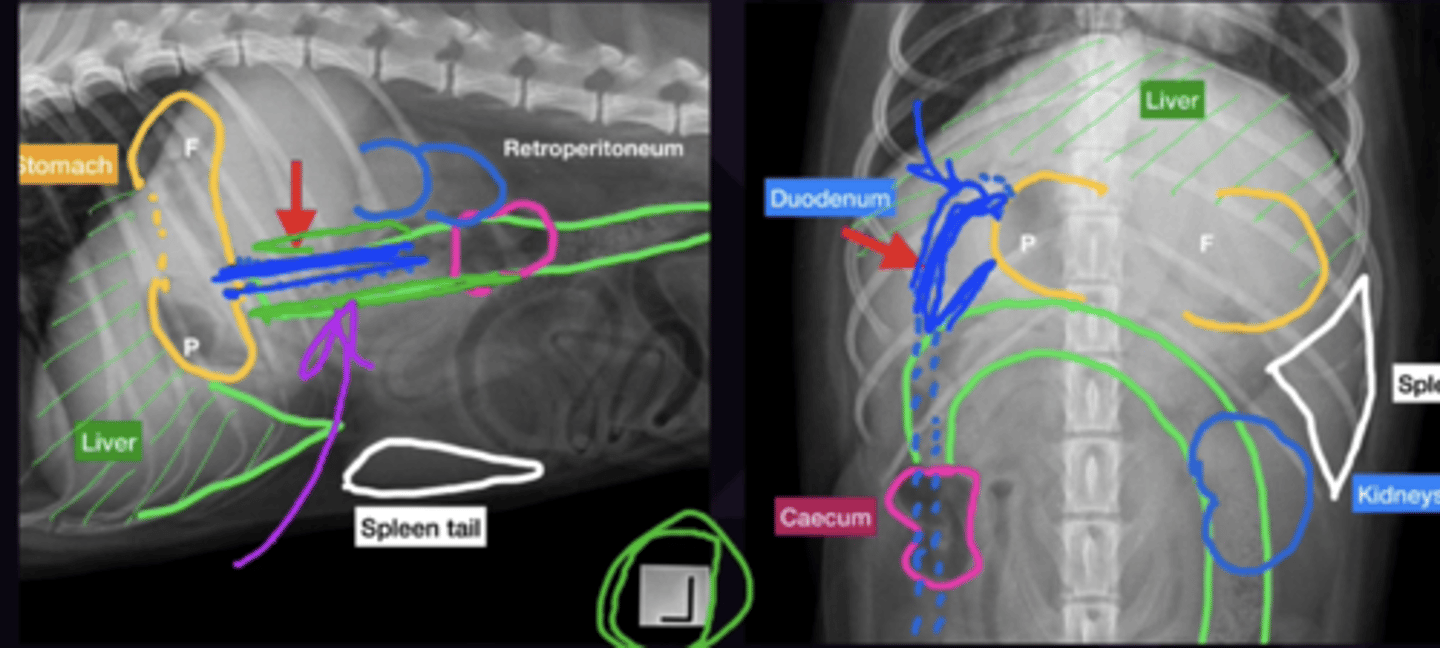
Describe the Assessment of the Ceacum (Dog Only) on Radiograph in terms of:
1. Location
2. Size
1. Approx. level of L3 on both views
2. Large - not significant (Do not mistake for a segment of dilated small intestine)
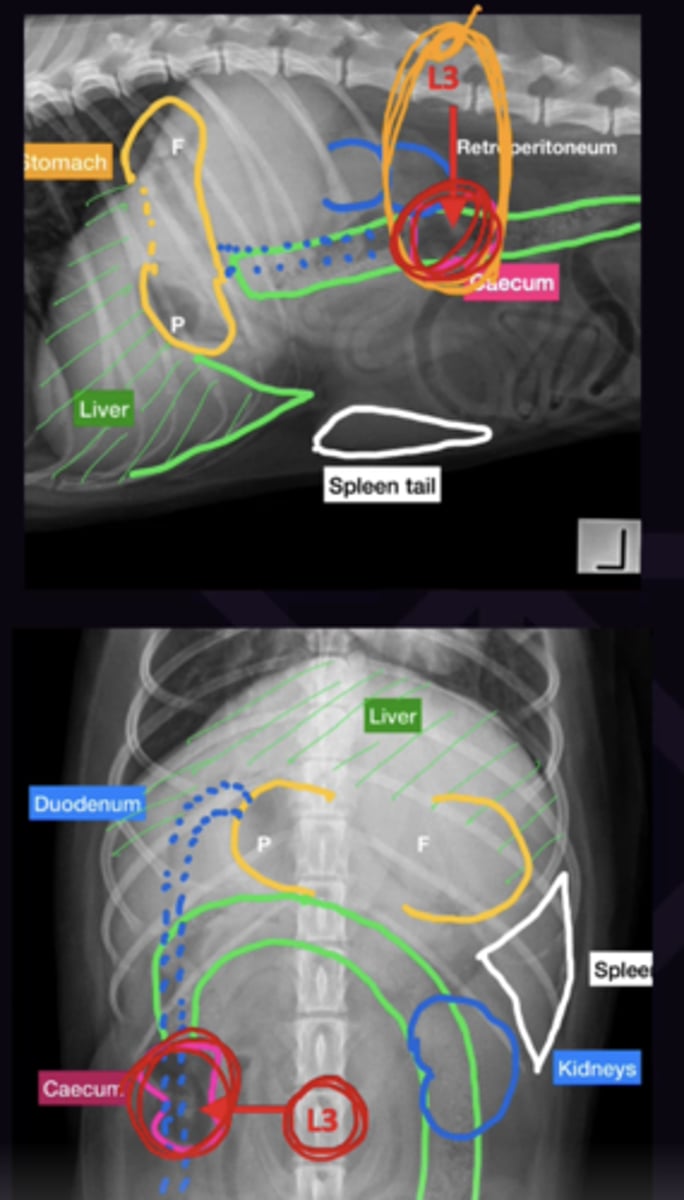
Describe the Assessment of the Colon on Radiograph in terms of:
1. Location
2. Superimposition
3. How to Find Colon Easily
1. Divides the abdomen in half Dorsoventrally
2. the Ascending, transverse, and proximal descending colon are superimposed (Need VD to assess)
3. Pelvic Inlet. Follow cranially
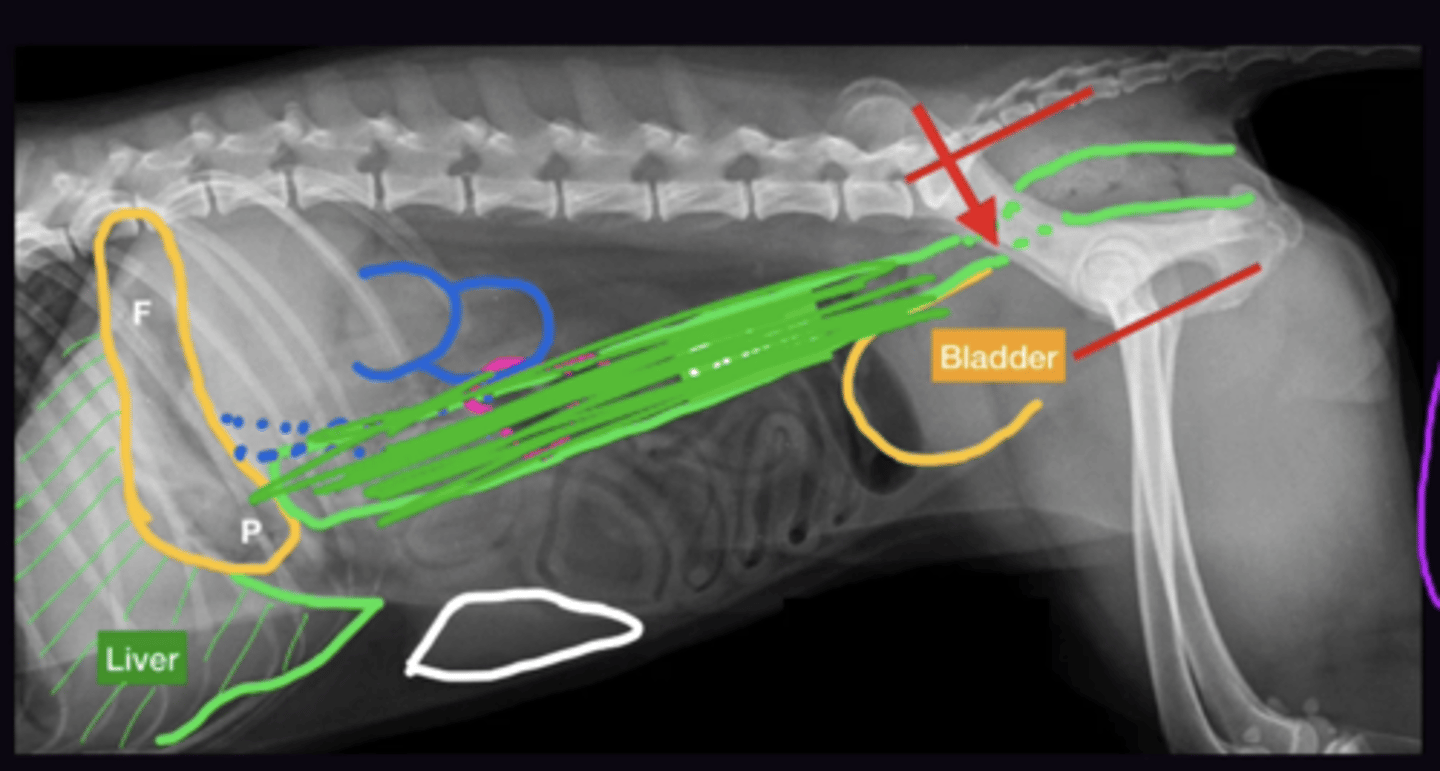
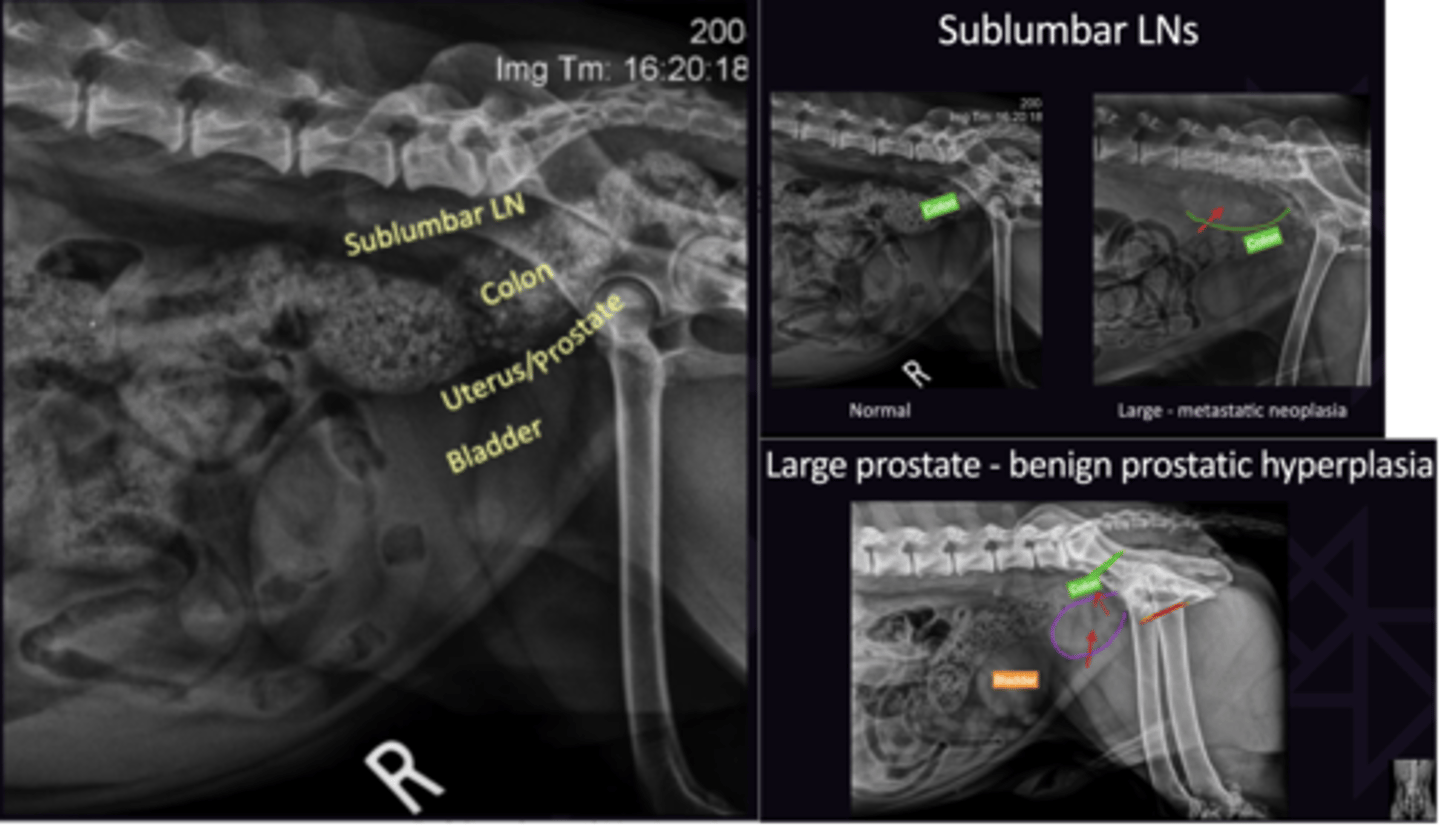
Describe the Location/Visibility of the Following Caudal Abdomen Structures:
1. Sublumbar Lymph nodes
2. Colon
3. Uterus/Uterine Stump
4. Bladder
5. Prostate
Use lateral View to Assess
1. Not Seen
2. Assess for Displacement (Should be half way between spine/pubis
3. Not Seen
4. Size/Opacity
5. Often Seen if Neutered
Describe the Cat Abdominal Radiography Differences in terms of:
1. Fat
2. Stomach/Pylorus on VD
3. Kidneys on VD
4. Spleen on Lateral View
5. Fat Cats on Lateral View
6. Fat Cats on VD View
1. More fat in cats
2. Stomach is J shaped, pylorus is on the midline (on the right in dogs)
3. Kidneys are closer to parallel (Right more caudal) and easier to see
4. Should not be seen
5. Have fat ventral to liver making liver look small . USe gastric axis for liver size
6. May have all intestines on 1 side. If displacement is being caused my a tumour and not fat it will be obvious

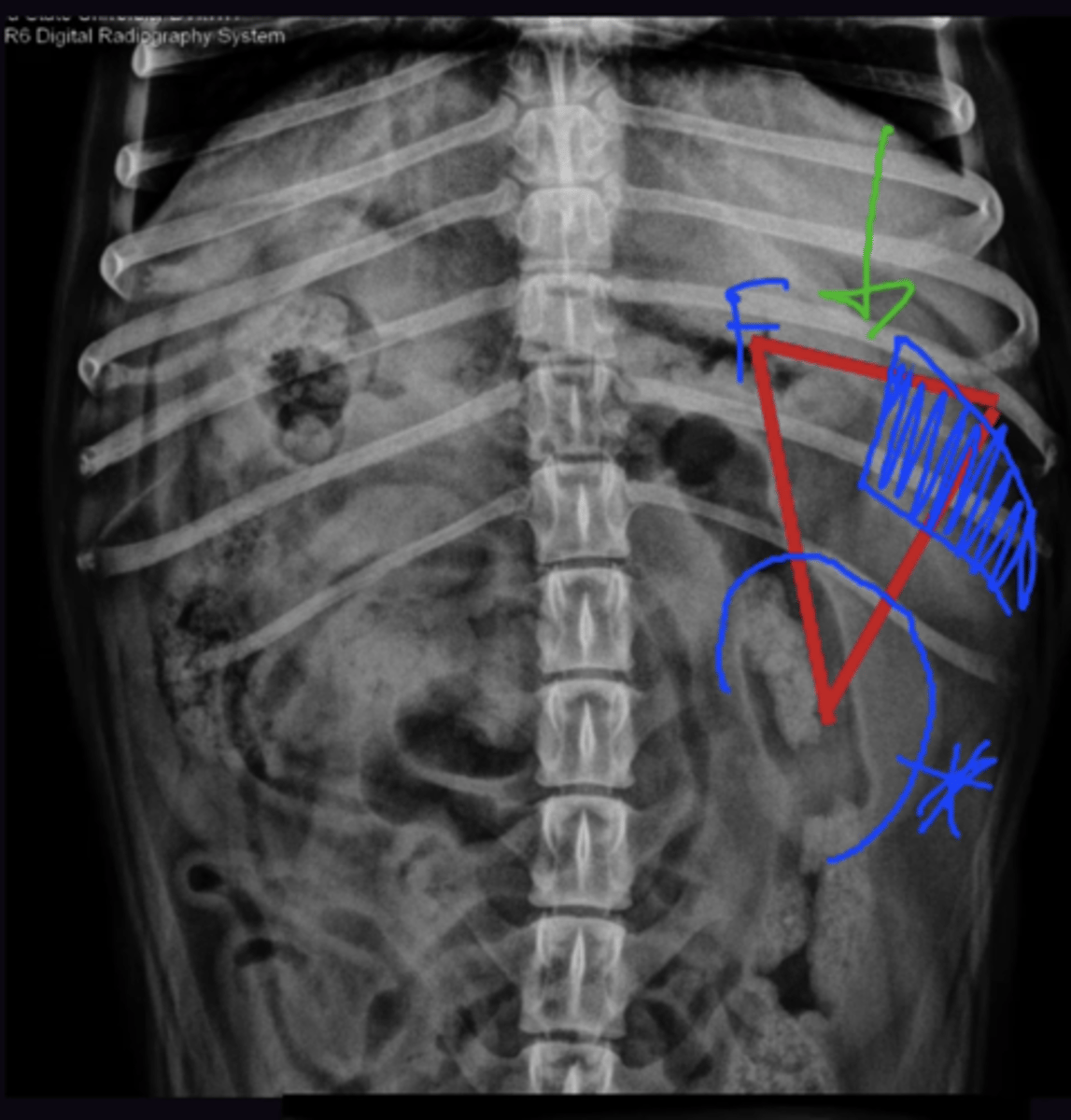
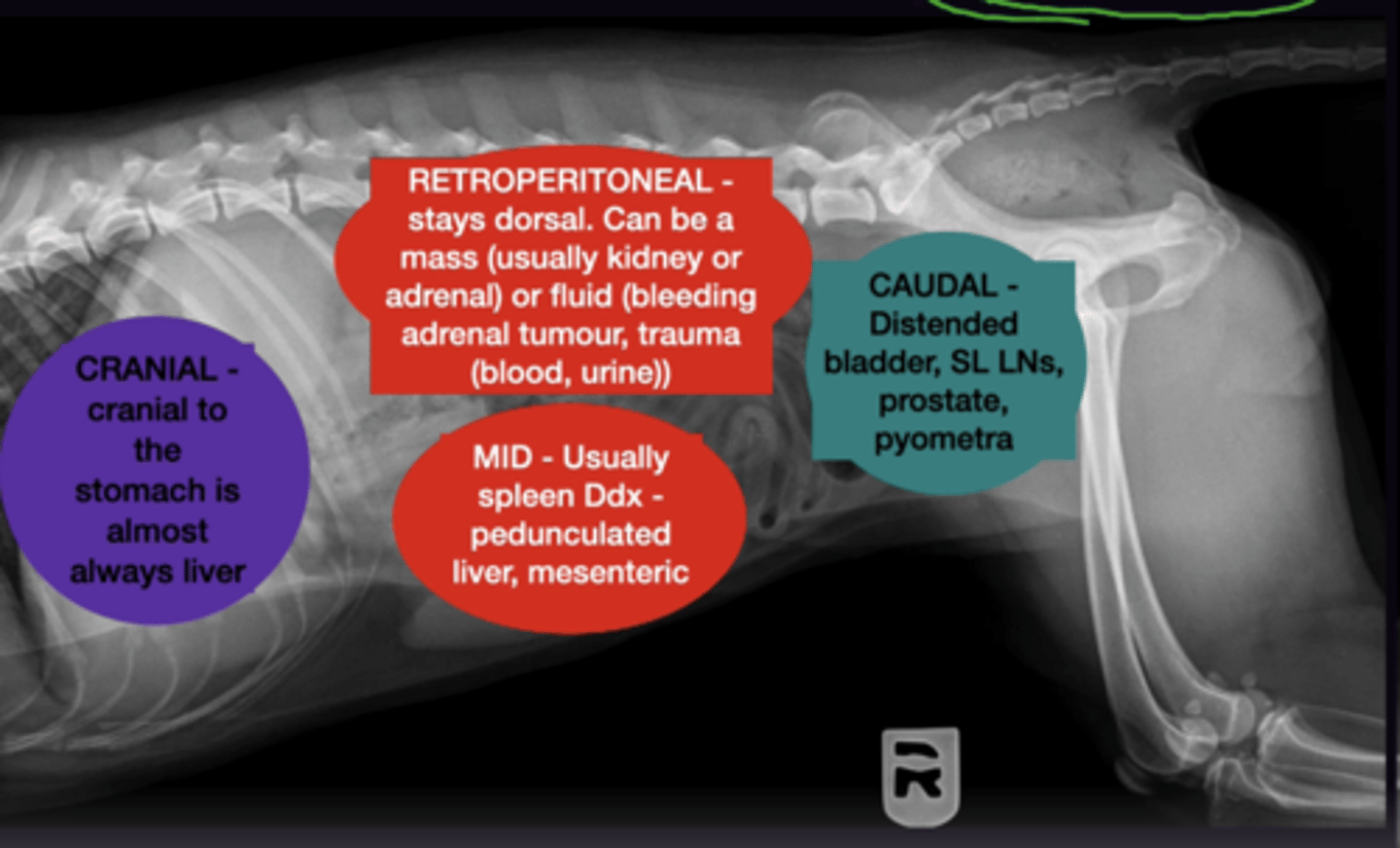
Describe Abdominal Masses in terms of:
1. Cranial Abdominal Masses
2. Retroperitoneal Abdominal Masses
3. Mid Abdominal Masses
4. Caudal Abdominal Masses
1. Almost Always Liver Masses - Displaces Stomach
2. Retroperitoneal stay dorsal and colon is displaced ventrally.
3. Organs displaced dorsally usually indicates splenic mass
4. Distended Bladder, SL LNs, Prostate Pyometra - Displaces Small Intestines Cranially + Colon Dorsally/Ventrally
Radiology 7: Ultrasound
Radiology 7: Ultrasound
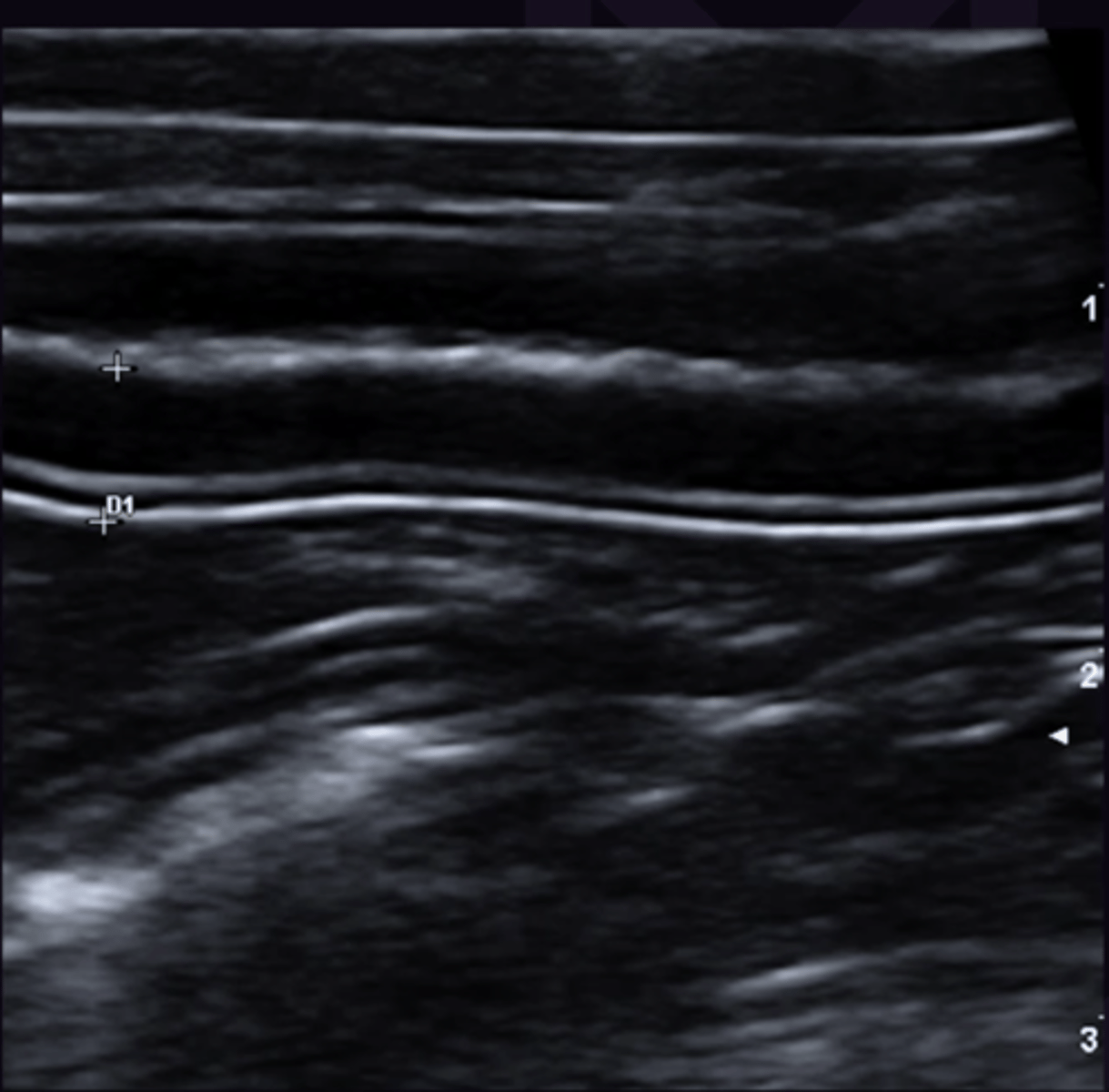
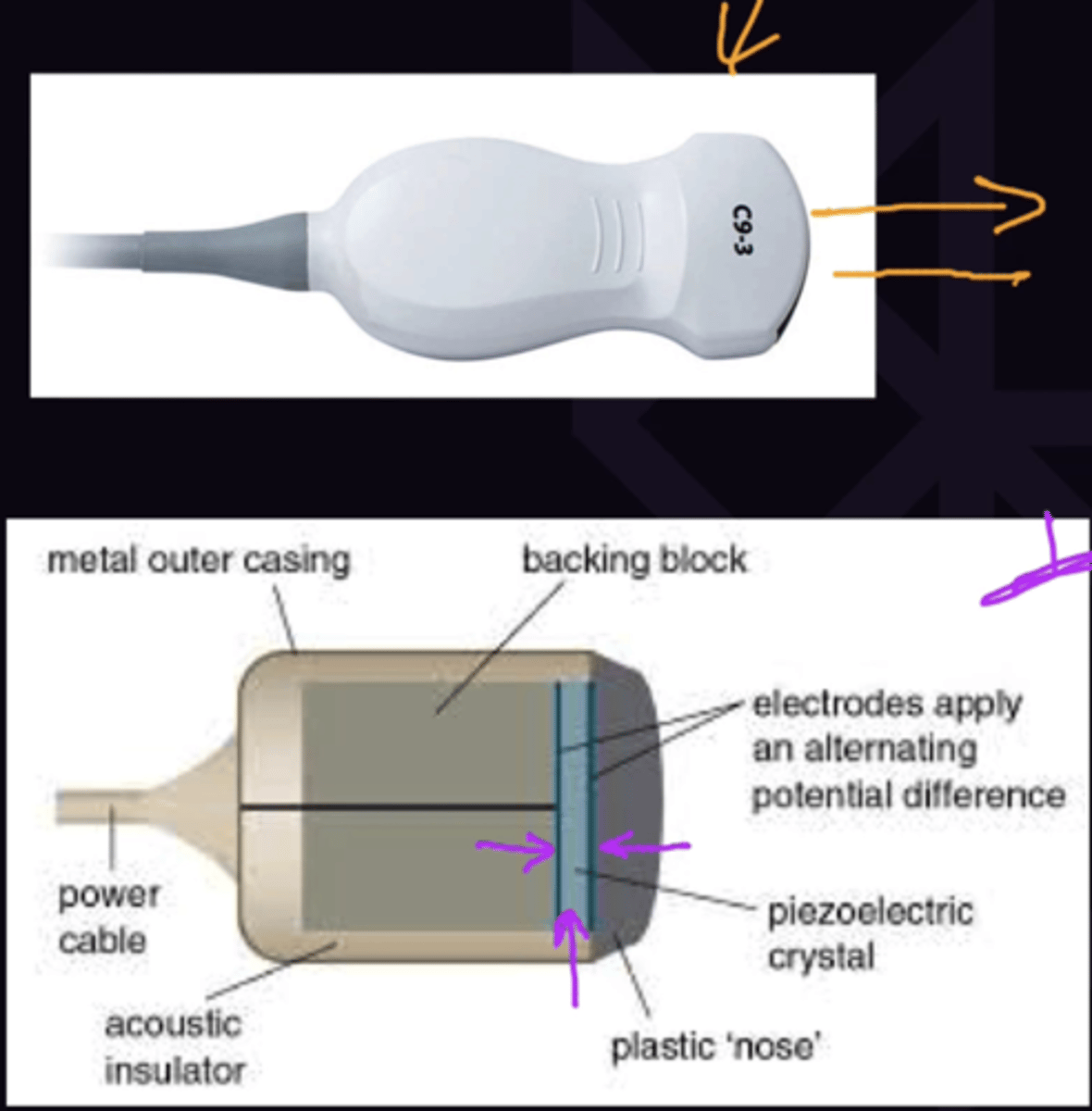
Describe How an Ultrasound Image is Made in terms of:
1. General Concept
2. Piezoelectric Principle
3. "Echo" Amplitude
1. Transducer sends sound into tissue → Tissue reflects sound back → Image Formed
2. An electric current applied to the crustal makes it vibrate and emit sound → reflected sound vibrates crystal and makes electric current → Image Made
3. At each tissue plane some sound is reflected back (Echo), Each echo is displayed as a white dot on the ultrasound image. Each echo has its own amplitude → the greater the amplitude the brighter the dot. the longer the echo takes to return the deeper it is displayed
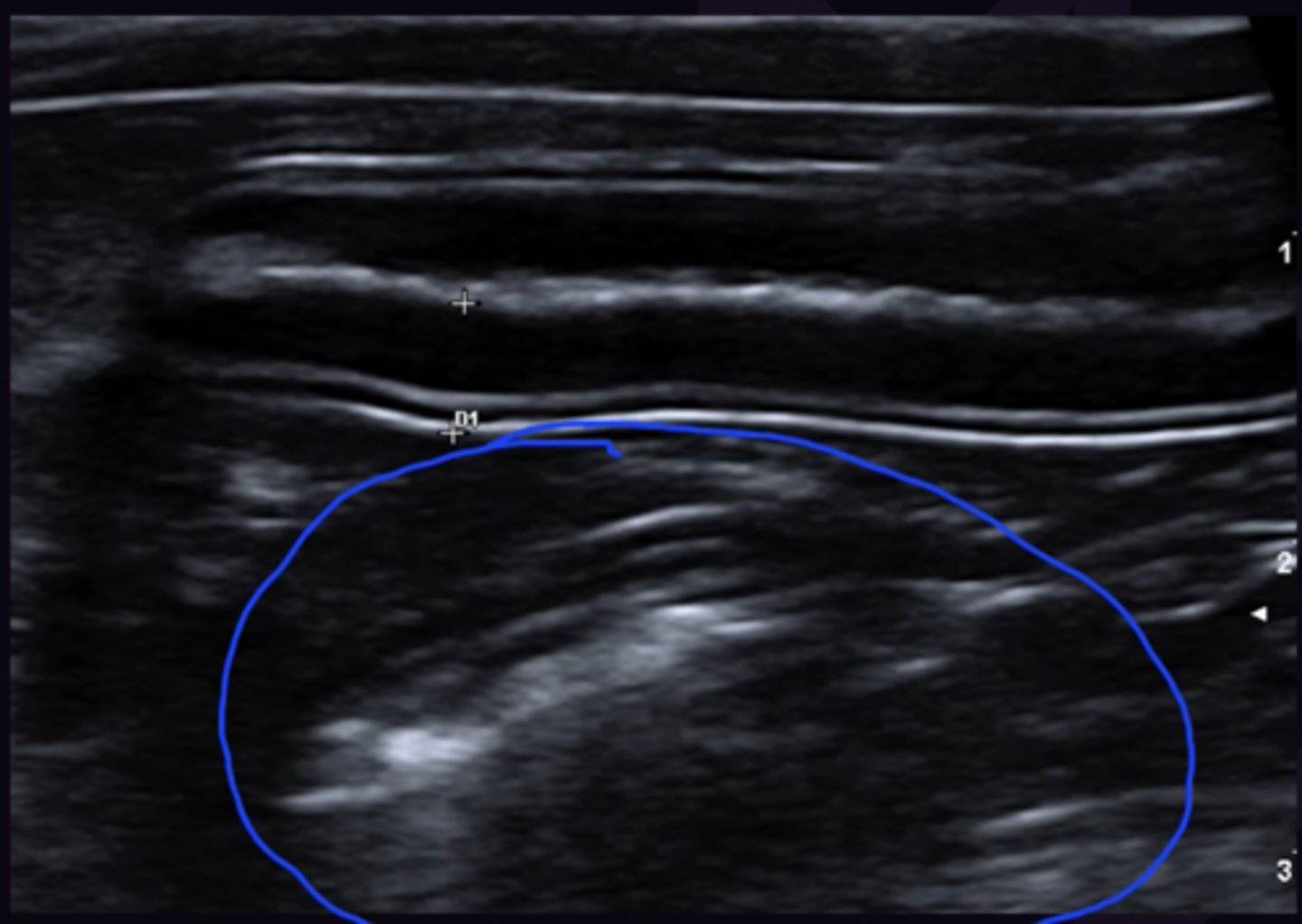
Describe What Determines if Sound is Reflected in Ultrasounds in terms of:
1. Acoustic Impedance
2. What determines Acoustic Impedance
3. What Creates Darker/Brighter Dots on Ultrasound
4. What Causes White Structures on Ultrasound
5. What Causes Black Structures on Ultrasound
1. The resistance the sound wave encounters through a tissue
2. Depends on the density + speed of sound in tissue
3. Sound is reflected at an interface between tissues of different acoustic impedance. Large difference = bright dot
4. Tissues that are heterogenous with many different acoustic impedance so there are lots of reflective interfaces
5. Tissues/Fluid that are homogenous with no internal differences in acoustic impedance so sound passes through without reflection
Describe the Following Absolute Terms:
1. Echogenic
2. Anechoic
1. White
2. Black
Describe the Following Relative Terms:
1. Hypoechoic
2. Hyperechoic
3. Isoechoic
1. Blacker than nearby tissue
2. Whiter than nearby tissue
3. The same as nearby tissue