Cardiac Muscle Function and Physiology Overview
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
What are the three major types of cardiac muscle?
Atrial muscle, Ventricular muscle, Specialized excitatory and conductive muscle fibers.
What occurs during Phase 0 of the cardiac muscle action potential?
Fast sodium channels open, causing depolarization and making the membrane potential more positive.
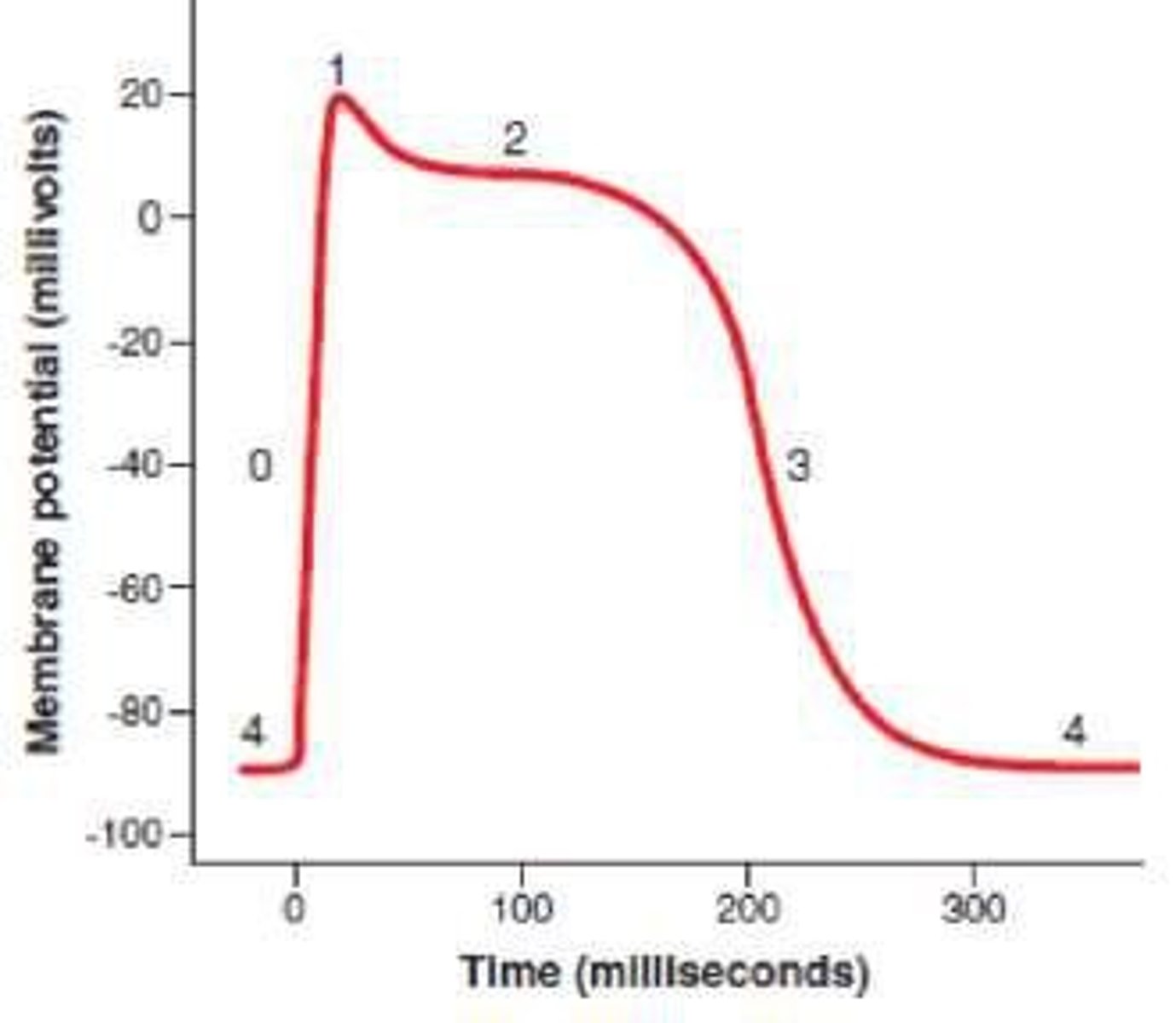
What happens during Phase 1 of the cardiac muscle action potential?
Fast sodium channels close and potassium leaves the cell through open potassium channels, leading to initial repolarization.
Describe Phase 2 of the cardiac muscle action potential.
Calcium channels open while fast potassium channels close, resulting in a plateau due to decreased potassium efflux and increased calcium influx.
What occurs during Phase 3 of the cardiac muscle action potential?
Calcium channels close and slow potassium channels open, leading to rapid repolarization.
What is the resting membrane potential in Phase 4 of the cardiac muscle action potential?
Averages about -90 millivolts.
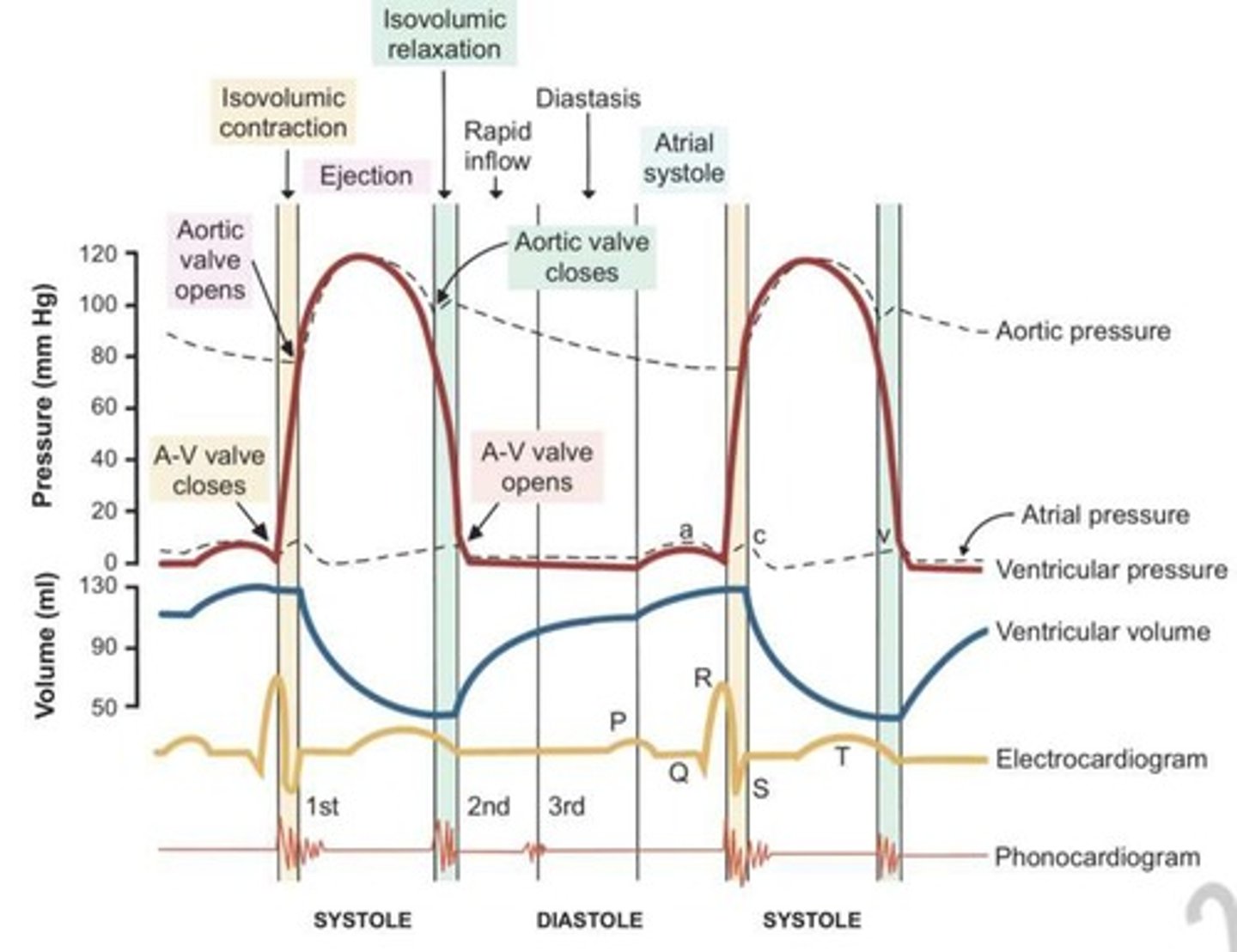
What is the cardiac cycle?
The period from the beginning of one heartbeat to the beginning of the next, including diastole (relaxation) and systole (contraction).
What is the normal refractory period of the ventricle?
0.25 to 0.30 seconds, approximately the duration of the prolonged plateau action potential.
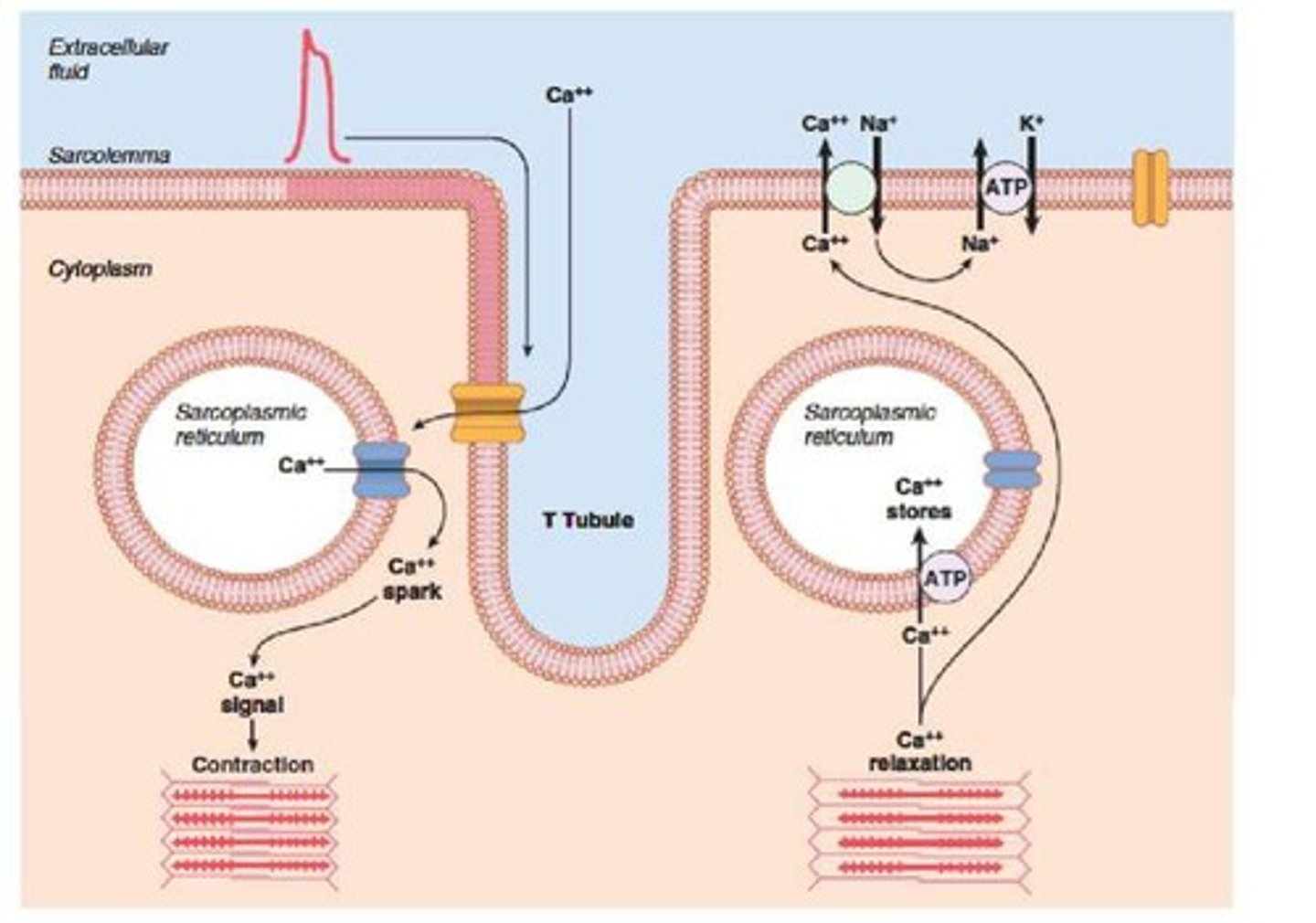
What is excitation-contraction coupling in cardiac muscle?
The mechanism by which an action potential causes myofibrils to contract, involving transverse T tubules and calcium release.
How does increasing heart rate affect the duration of the cardiac cycle?
It decreases the duration of each cardiac cycle, including contraction and relaxation phases.
What does the P wave represent in an ECG?
The spread of depolarization through the atria.
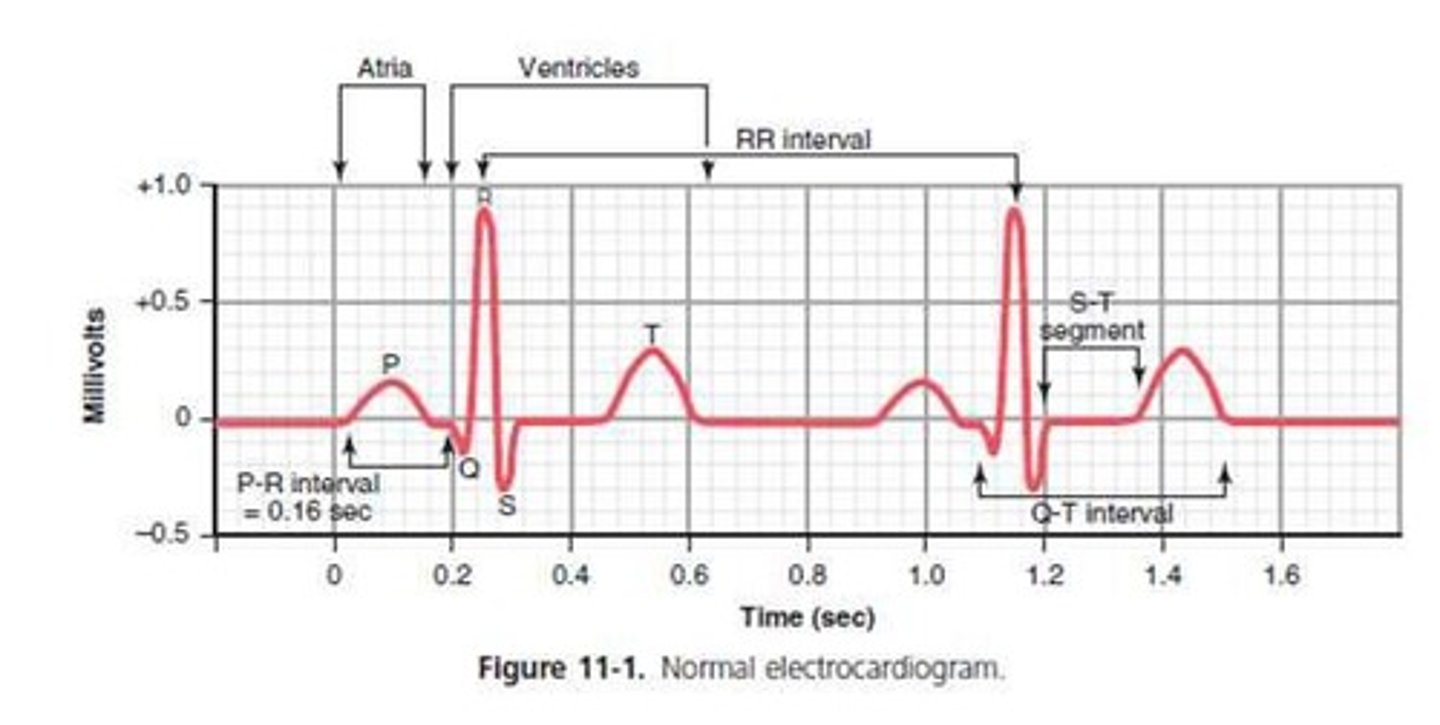
What do the QRS waves indicate in an ECG?
Electrical depolarization of the ventricles.
What does the T wave represent in an ECG?
The stage of repolarization of the ventricles.
What occurs during the period of rapid filling of the ventricles?
Blood flows into the ventricles during the first third of diastole, aided by atrial contraction in the last third.
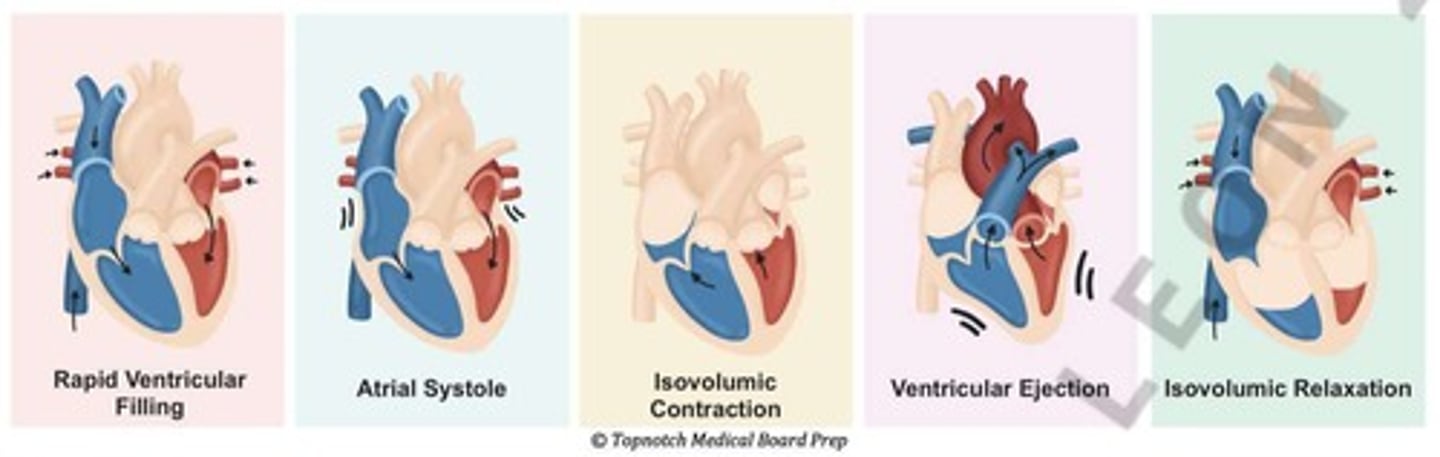
What is isovolumic contraction in the cardiac cycle?
A period where cardiac muscle tension increases without shortening of muscle fibers.
What happens during the period of ejection in the cardiac cycle?
Left ventricular pressure rises above 80 mm Hg and right ventricular pressure rises above 8 mm Hg, ejecting 70% of blood in the first third and 30% in the last two-thirds.
What is isovolumic relaxation?
A phase allowing both right and left intraventricular pressures to decrease rapidly.
What is preload in cardiac function?
The degree of tension on the muscle when it begins to contract.
What is afterload in cardiac function?
The load against which the muscle exerts its contractile force.
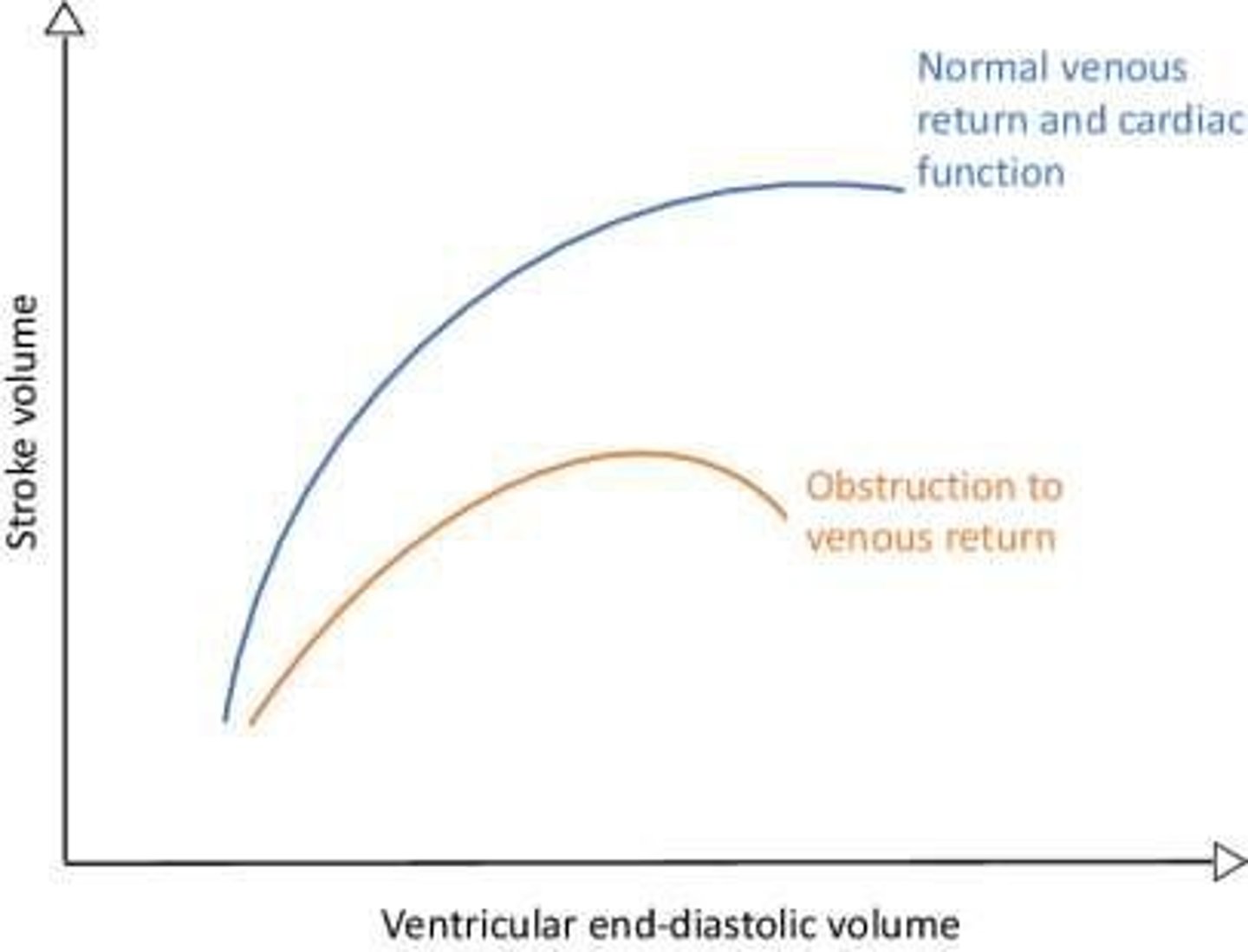
What is the Frank-Starling mechanism?
The greater the heart muscle is stretched during filling, the greater the force of contraction and the quantity of blood pumped into the aorta.
What effect do potassium ions have on the heart?
They can cause dilation, flaccidity, slow heart rate, weakness, abnormal rhythm, and potentially death.
What effect do calcium ions have on cardiac muscle?
They can cause spastic contraction and cardiac weakness.
How does temperature affect heart rate?
Increased temperature, such as during fever, increases heart rate.
What does S1 represent in heart sounds?
Closure of AV valves, characterized as longer, louder, and lower in pitch.
What does S2 represent in heart sounds?
Closure of SL valves, shorter and not louder than S1.
What does S3 indicate in heart sounds?
Rapid filling of ventricles, associated with pathological conditions like congenital heart failure.
What does S4 indicate in heart sounds?
Atrial systole, associated with conditions like myocardial infarction and hypertension.
Where is the sinoatrial node located?
In the superior posterolateral wall of the right atrium, near the opening of the superior vena cava.
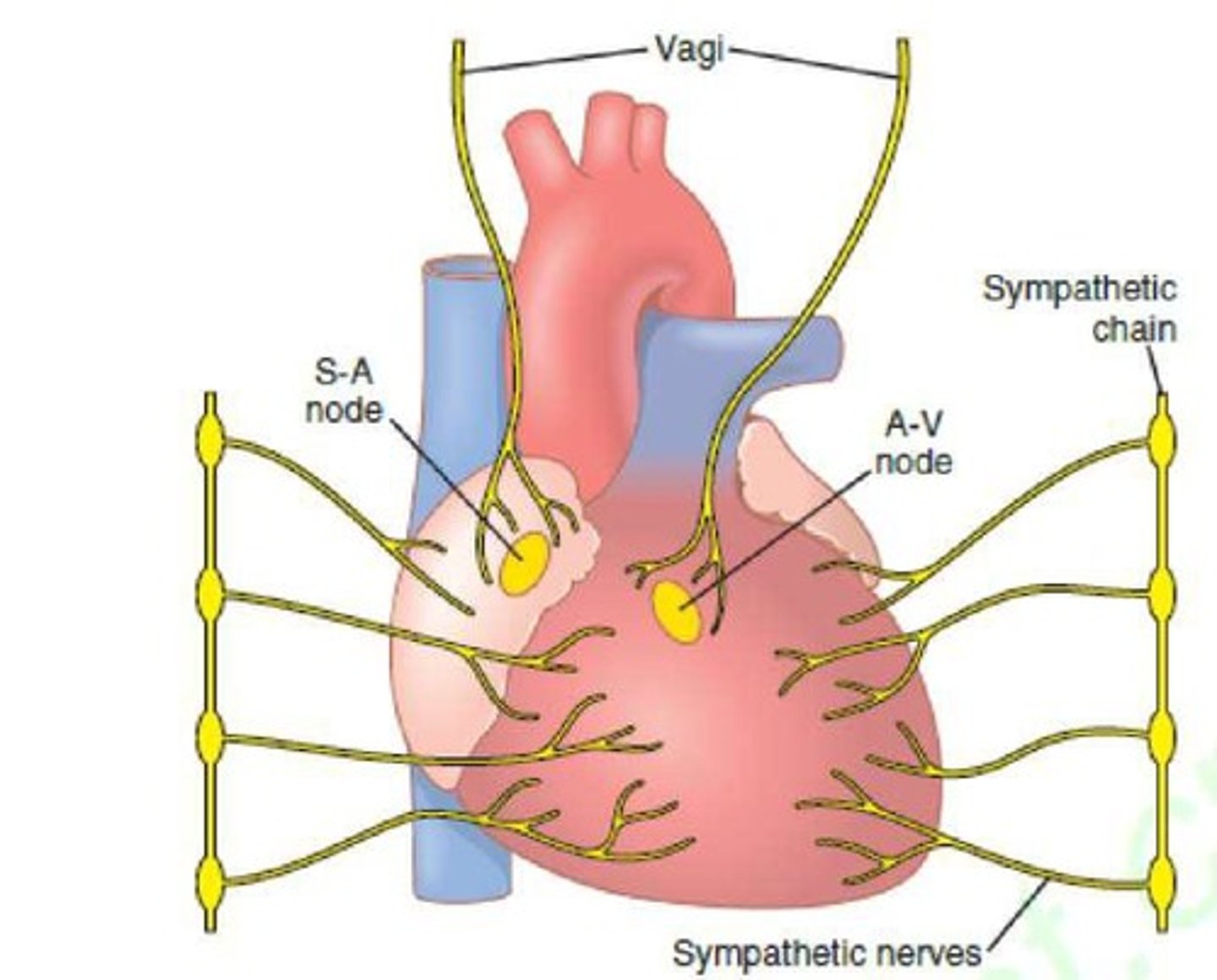
What is the role of the AV node?
It delays the cardiac impulse to allow atria to empty blood into the ventricles before ventricular contraction.
What is the function of Purkinje fibers?
They provide rapid transmission of electrical impulses compared to AV nodal fibers.
What is the effect of sympathetic stimulation on the heart?
It increases the rate of sinus nodal discharge, conduction rate, excitability, and force of contraction.
What is the role of the lymphatic system in circulation?
It provides an accessory route for fluid to flow from interstitial spaces into the blood and carries proteins and large particles away from tissues.
What are the two phases of local blood flow control?
Acute control (rapid changes in vasodilation or vasoconstriction) and long-term control (slow changes over days or weeks).