1.03 Non-Medical Sciences
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
62 Terms
What is stigma?
A strong mark of disapproval many people in society will share in regards to a particular circumstance, quality or person. It usually results due to deviation from the social norm w/ different types found
What is discreditable stigma? Give an example
-not known by most of society, only those w/ the condition and few close relatives are aware of the stigmatised circumstance or quality
eg. scar on leg covered
What is discrediting stigma? Give an example
-cannot be hidden from others where the effects of illness may be obvious
e.g. cerebral palsy
What is enacted stigma? (2)
-discrimination by others on grounds of 'being imperfect'
-people experience this sort of stigma in real time and a particular condition will present as a disadvantage
What is felt stigma?
-when individuals feel shame or guilt as a result of experiencing or fear of enacted stigma
What is projected stigma? Give an example
-strategies or tactics used to combat or avoid enacted stigma
e.g. covering scar
Why might stigma cause problems in healthcare?
-people may not see health services at a time when they are most vulnerable
Outline the issues caused by stigma surrounding mental health (2)
-stigma + discrimination can worsen someone's mental health problems
-can delay or impede their getting health + their recovery
Outline the stigma surrounding obesity (2)
-obese people are blamed for their weight - some people think that this may motivate individuals to adopt healthier behaviours
-obesity stigma involves actions against people w/ obesity that can cause exclusion and marginalisation e.g. when people w/ obesity don't receive adequate healthcare or when they are discriminated against in the workplace or in educational settings
What is ethnography?
- the scientific description of people's cultures, customs, habits and mutual differences
What type of research is ethnography? What may be taken into account?
- a form of qualitative research whereby observational data is collated on human culture and society + allows different view points
-physical env., peoples' interactions + sequence of events may be taken into account
What is the most important part of ethnography?
-researcher explores subject from the point of view of the study subjects
What is an example of ethnographic research?
-group of medical students observed to see how they engaged with + learned from new curriculum in order to find the best balance of resources to teach
What is a major advantage of ethnography?
-immersive, real-life w/o disruptions
What is the transtheoretical model?
-used to model how people go through behaviour change and helps to understand decision making and apply relapse within behaviour change
What are the stages of the transtheoretical model?
PCPAM
-precontemplation: patient hasn't thought about the actions they may need to take or not aware they need to make health related change
-contemplation: people have identified a need to change within the next 6 months and weigh up the positives and negatives of making the change
-preparation: where plans to make change are composed
-action: undertaking the changed behaviour
-maintenance: this is working to prevent relapse
important that can enter, exit and restart at any point
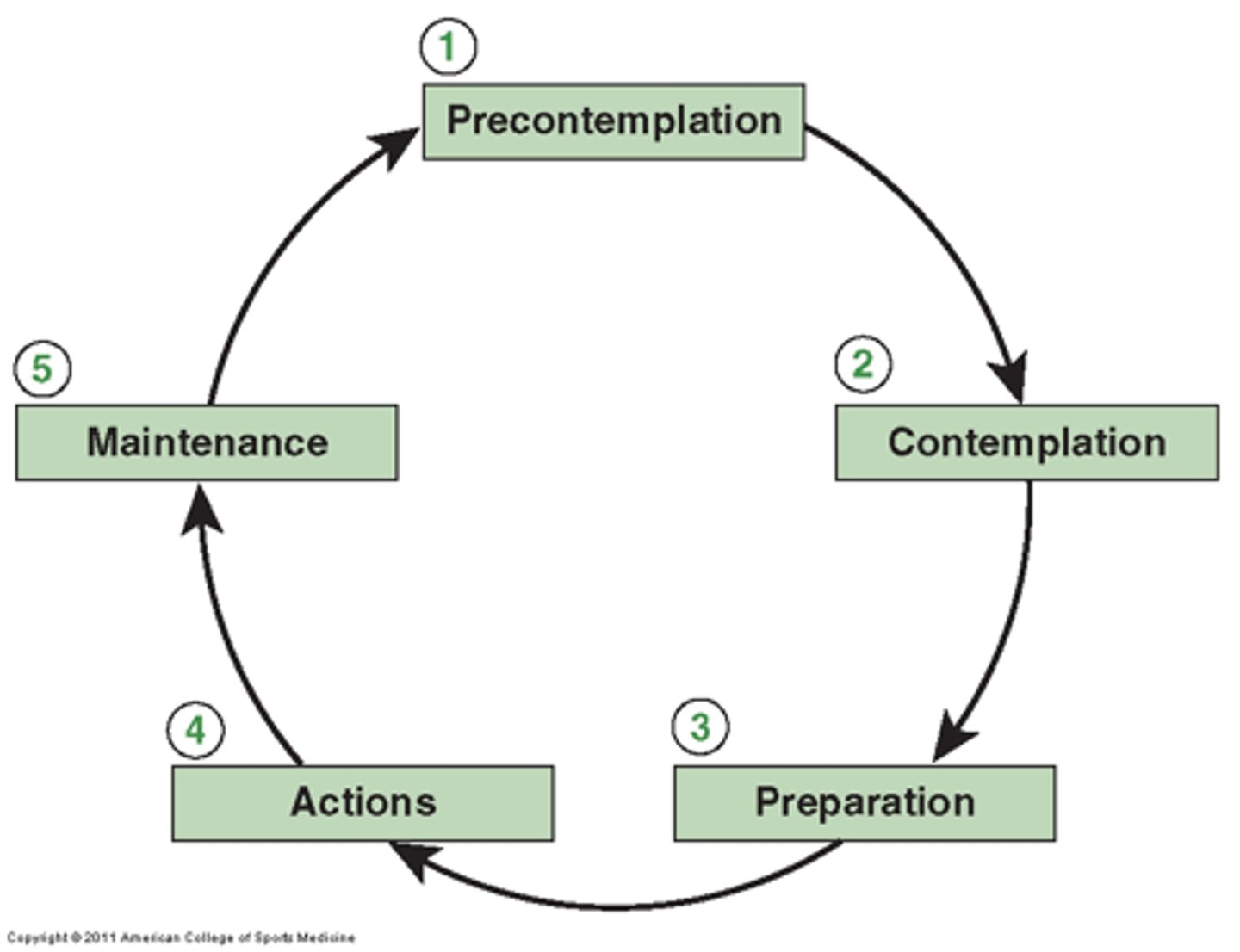
What varies among individuals going through the transtheoretical model?
-people will usually go through all of these stages however they make progress changes
How does relapse tie into the transtheoretical model? (3)
-individuals may relapse and have to go through the cycle a few times before they make the change permanently
-relapse is an important inclusion of the model as it normalises relapse and encourages not to see is as a failure but to keep trying to change their behaviour
-in clinical practice, a HCP could emphasise this and explore what a person has learned from a relapse and how this can be used to increase chances of success next time
What is the transtheoretical model useful for? (3)
-related to changing detrimental behaviours which are chronic and integrated into the patients lifestyle
-model to use when the behaviour is longstanding and addictive and needs to change
-useful in practice when dealing with smoking/alcohol/food/drug addictions etc, allows doctor to see if the patient is ready to change
What is the health belief model? (2)
-summarises peoples beliefs in relation to health and the threat ill health may have on them
-used to describe the factors that may influence the likelihood of a person changing their behaviour
Outline the health belief model (6)
1. Perceived susceptibility: opinion on how likely they are to get the condition
2.Perceived severity: how serious a condition may be seen
3.Perceived benefit: what gain from taking the action
4. Barriers: which may be influenced by demographics e.g. age/sex
5.Cue to action- e.g. mass media campaigns, advice from others, ilness of family member, physician's explanation
6.Self efficacy: confidence in ability to make a change
What is meant by Prima Facie duties? (3)
- " a principle is binding unless it conflicts w/ another moral principle- if it does, we have to choose between them"
-a principle is accepted as correct, until proven otherwise
-use discretion and judgement to decide which principle outweighs the other when they conflict
Give an example where Prima Facie duties come into action
-stealing a bike to reach a defibrillator for someone in cardiac arrest
-> harm prevention and beneficence for unwell stranger would override justice and reparation for the bike owner
List Ross' Prima Facie Duties (7)
-Fidelity: obligation to keep a promise
-Reparation: obligation to repair the harm
-Gratitude: obligation to recognise a granted benefit and express it
-Justice: obligation to fairly distribute the good
-Beneficence: obligation to do good to someone
-Self-improvement: obligation to make yourself a better person
-Non-maleficence: obligation not to harm anyone
Define autonomy
-right of patients to make meaningful decisions about their treatment w/o any controlling interference
How can a patient's autonomy be upheld? What are the potential challenges in doing this?
-be truthful -> deceit will infringe upon a patient's autonomy
-make sure patients are adequately informed to make healthcare decisions= informed consent -> but cannot be fully informed of all benefits and risks as even doctor may not be aware of these so UK law: doctor obliged to inform patient of main benefits and common/significant risks
-keeping confidentiality
What does autonomy require?
-the capacity for deliberation
What does autonomy include?
- the right to refuse treatment and the right to not know
Define beneficence
-an action of good towards another person/providing net benefit
Give an example of net benefit in practice
- two women have a mastectomy one has net benefit, other is distraught by the loss of her femenine identity and there is net harm
How can beneficence be implemented by practitioners? (3)
-promoting patients' health
-promoting autonomy
-up-to-date info from medical research to make patients aware of risks 7 benefits + skilled and competent enough to do so
What is non-maleficence?
-duty to do no harm or allow harm to occur though neglect
Describe the link between beneficence and non-maleficence (4)
-often considered together in order to maximise benefit and minimise harm
-any decision is made by balancing the potential benefit & the potential harm
-do positive good, make sure the good outweighs the harm, prevent harm, do not directly harm
- the two priniciples are kept separate because we always have an obligation to non-maleficence but not always an obligation of beneficence
What is meant by distributive justice? Example
-fair distribution of scarce resources i.e. don't waste -> if cheaper drug will work just as well as the expensive one, prescribe the cheaper one
What is meant by rights-based justice? Example
-rights-based justice: respect of patient's human rights i.e. don't discriminate against patients based on your own personal preferences (Human Rights Act 1998)
What is meant by legal justice? Example
-respect for morally acceptable laws
i.e. if patient has a notifiable disease e.g. measles you must notify the appropriate authorities even if you don't want to break patient confidentiality
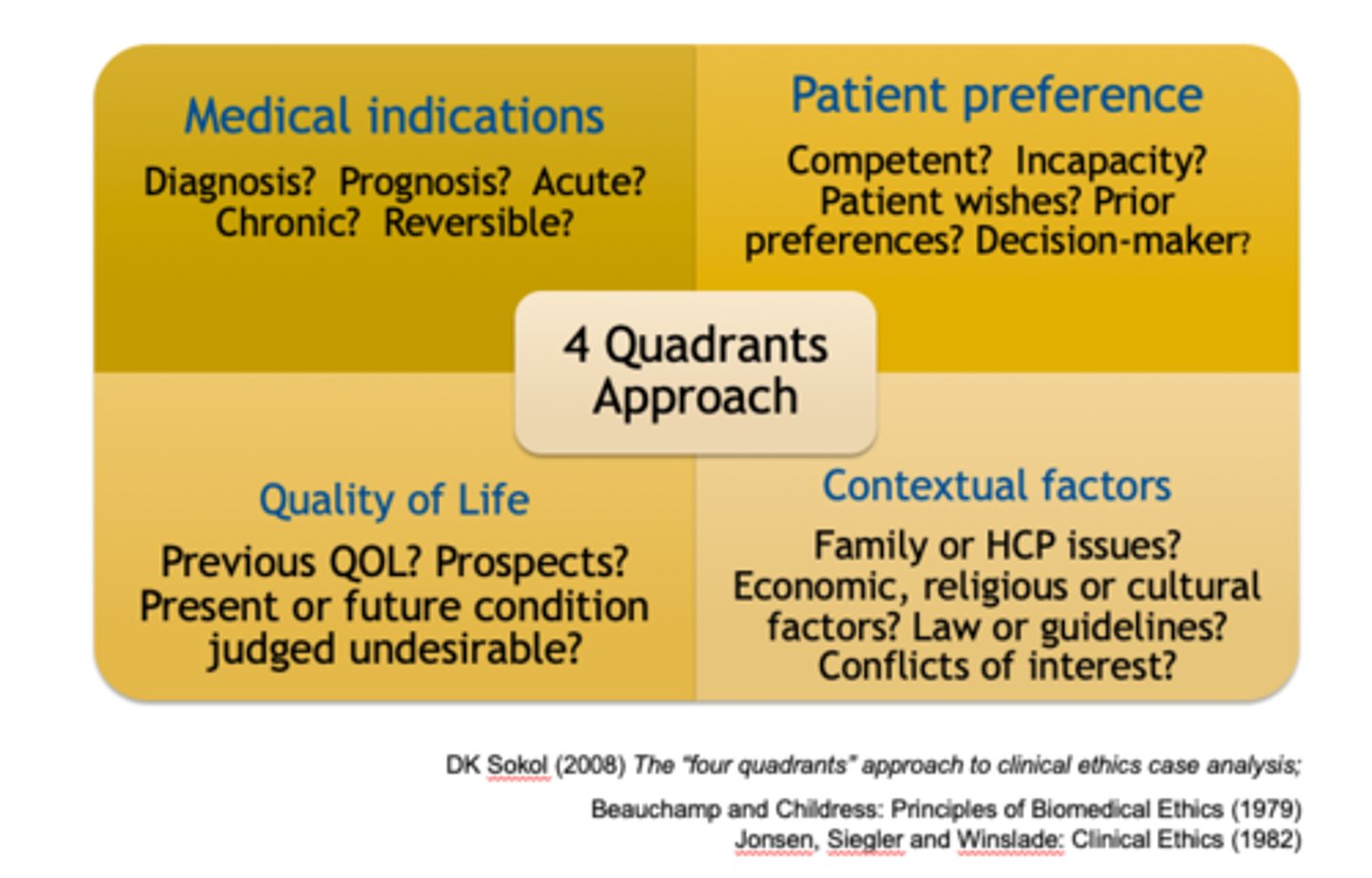
Describe the four quadrants approach
1. Medical indications- medical situation, treatment options, beneficence (if any) for that patient through treatment, prognosis, diagnosis, severity
2. Patient preference- patient's wishes if competent, and their presumed wishes if not
3. Quality of life- aiming to maintain/improve QoL, achieving goals of treatment, longevity vs QoL, how this treatment will affect them
4. Contextual features- economic, relgious, cultural factors, decision's impact on patient's family & medical team, doctor must reflect on personal bias
Consider these things w/ your case in mind -> not binding or absolute duties
What is meant by paternalism? (3)
- a doctor decides what is right and makes decisions with minimal consent
-do not impose your views on your patients, only support w/ expert advice
-it is assumed that the welfare or the best interest of the patient is primarily identified by the doctor
When can a paternalistic approach be useful?
-in emergencies, when patient can't consent
What is health promotion?
-process of enabling people to increase control over and improve their health
What does health promotion involve?
-involves population as a whole in the context of their everyday lives, rather than focusing on people at risk for specific diseases
What are the 3 main aspects to health promotion according to Tanahill's model?
-Health protection: use legal and fiscal (taxes) means, regulations and policies for the enhancement of positive health and prevention of ill-health e.g. high taxes on tobacco
-Health education: process by which individuals and groups of people leaern to behave in a manner conducive to the promotion, maintenance, or restoration of health -> via influencing the beliefs, attitudes and behaviour of those w/ power and of the community at large
-Disease prevention

What are the limits to the Tanahill model?
-not much about wellbeing or salutogenesis (medical approach focusing on factors that support health & well-being rather than on factors that cause disease)
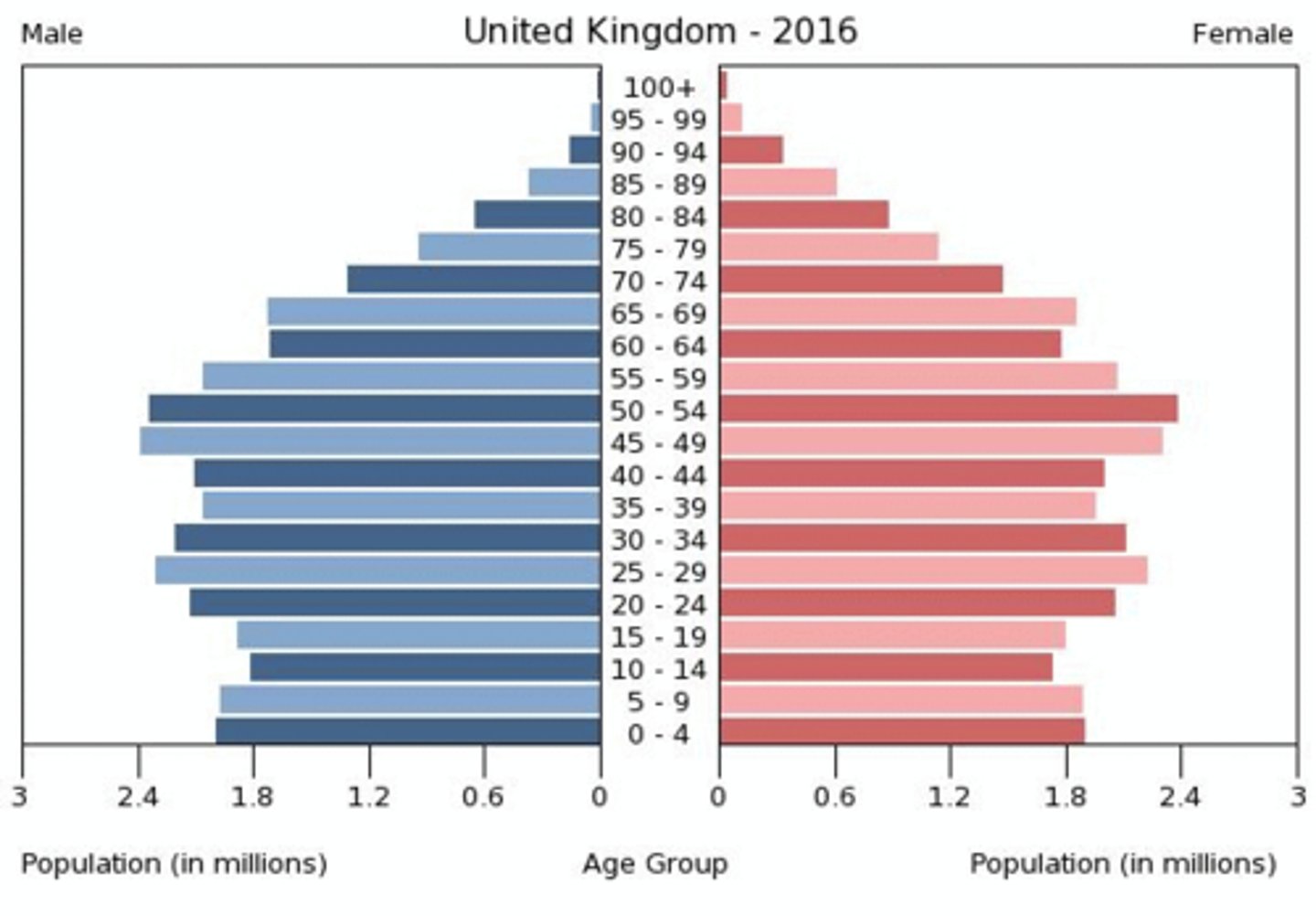
What is demography?
-scientific study of human populations
Why is demography important?
-it is important to understand the structure of a population in order to plan health and public health interventions; population health structures can be represented as age pyramids
What are population pyramids?
-population pyramids provide a simple way to compare population structures across countries and can provide an indication of the state of development of each country
What do population pyramids look like in developing countries?
-broad base, tapering at the top e.g. India
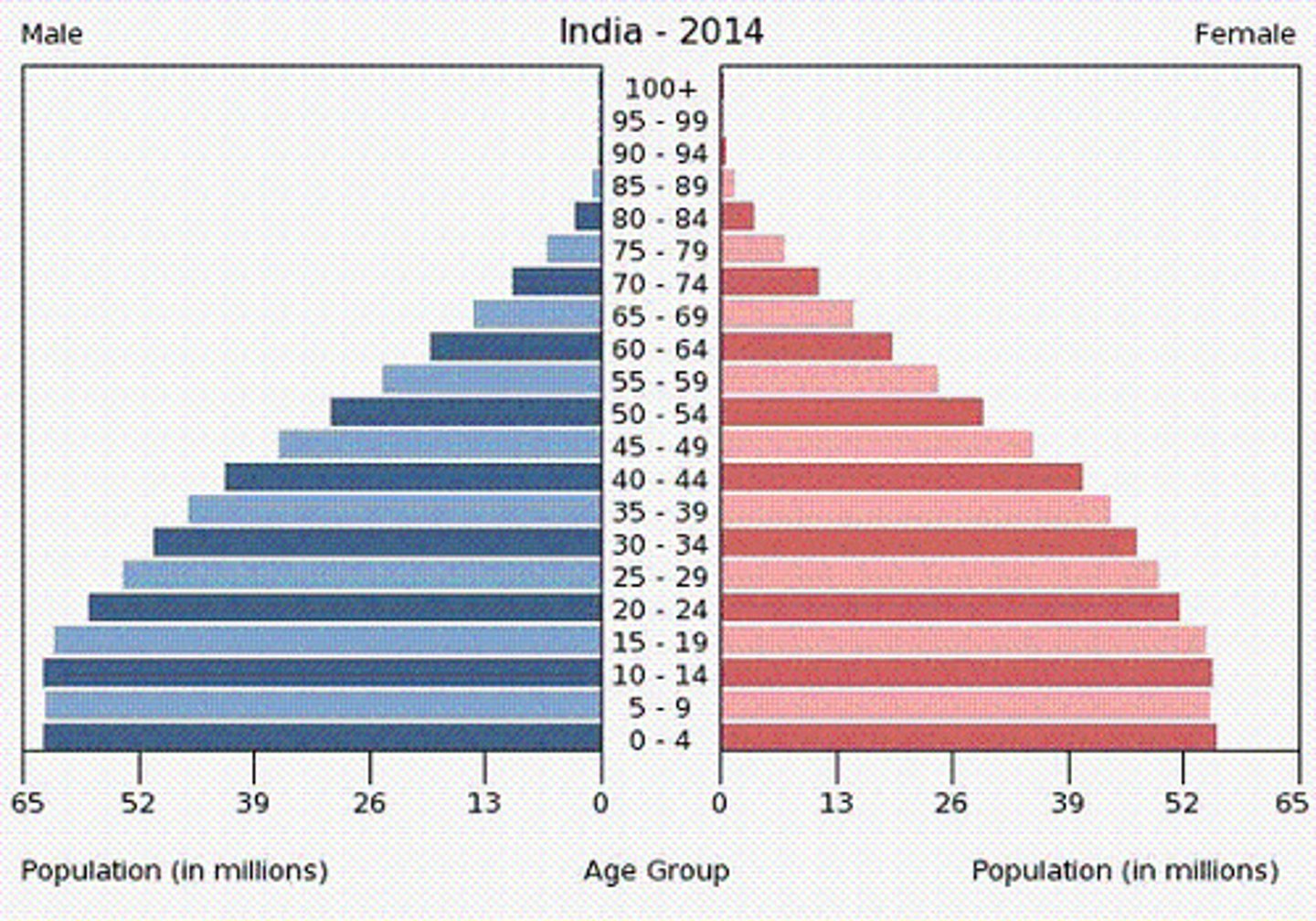
What do population pyramids look like in developed countries?
-pyramid generally shows a bulge in the middle and has a narrower base e.g. UK
What does population growth/decline depend upon? (3)
-fertility
-mortality
-migration
What is meant by an ageing population?
-when the median age of a country/region rises due to rising life expectancy and or declining fertility rates
What has led to an ageing population?
-modern medical advances have meant that we are able to keep people alive for longer than before
What are the implications of an ageing population (3)
-more people to treat- doctors/nurses/health care professionals have more people to treat per head -> can't train more people to match increased demand
-elderly have comorbidities e.g. heart disease, COPD, diabetes, cancer, kidney disease, high cholesterol, obesity, hypertension -> more difficult to treat than patients w/ single problems and more vulnerable to side effects of treatment
-living longer means more conditions are going to arise by chance -> more expensive to deal with
Explain what QALYs are
-while we are living longer, the proportion of our lives we can expect to live in good health is decreasing
-QALYs -> quality adjusted life years aim to measure both the quality and length of life
1 year of perfect health = 1 QALYs
Death= 0 QALYs
1 year of being bedridden= 1/2 QALY
-ve QALYs -> health state thought to be worse than death
What is dementia? What challenges does it bring for healthcare?
-A group of neurological conditions and symptoms that impair cognitive and social function which includes Alzheimer's disease
-patients require a massive increase in care -> lack capacity to make choices/ consent, family members may have to decide for them
What is bed-blocking? (3)
-even if elderly person is mentally sharp + well, they may require assistance w/ ADLs (acitivites of daily living) e.g. eating, getting dressed or using the toilet w/o assistance i.e. require social care
-must remain in hospital until suitable social care is available so 'block' hospital beds as a result for weeks/months
-particularly common during winter as A&E attendance increases due to increased risk of falls and high infection rates
What are the possible solutions to tackling an ageing population? (3)
-our tax contributions will need to increase as cost of running NHS continues to increase
-beed to train more geriatricians to cope w/ more complex needs of these patients-> not hugely popular post so incentives required
-need public health campaingns and patient education to prevent later development of serious diseases
What is health protection? Give an example
-to protect the public from being exposed to hazards which damage their health and to limit any impact on health when such exposures can't be avoided, includes legal or fiscal controls, regulations & policies and voluntary codes of practice
e.g. levying of tax on tobacco products + legal restrictions on advertising
Describe what Public Health England is and what their responisbilities are (1) + (5)
-exists to protect and improve nation's health & wellbeing, and decrease health inequalities - sponsered by the Department of Health and Social Care
Responsibilities:
-protect nation from public health hazards
-prepare & respond to public health emergencies
-share information + expertise, identify + prepare for future public health challenges
-support local authorities & NHS to plan + provide health and social care services e.g. immunisation & screening programmes
-researching, collecting, analysing data to improve our understanding of public health challenges + come up w/ answers to public health questions
What is the Food Standards Agency (FSA)?
-independent government department working to protect public health and consumers' wider interests in relation to food in England, Wales and Northern Ireland
When and why was the FSA established?
-established in 2000 after several high-profile of food borne illnesses
What does the FSA cover?
-food supply, price, availability and some aspects of food production e.g. environmental concerns and animal welfare
What are the main goals of the FSA? (6)
-protect people
-decrease economic burden of foodborne illness
-supports UK economy by ensuring our food has a strong reputation for safety & authenticity in the UK & abroad
-food is safe
-food is what it says it is
-consumers can make informed decisions about what to eat