Gut Secretions
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
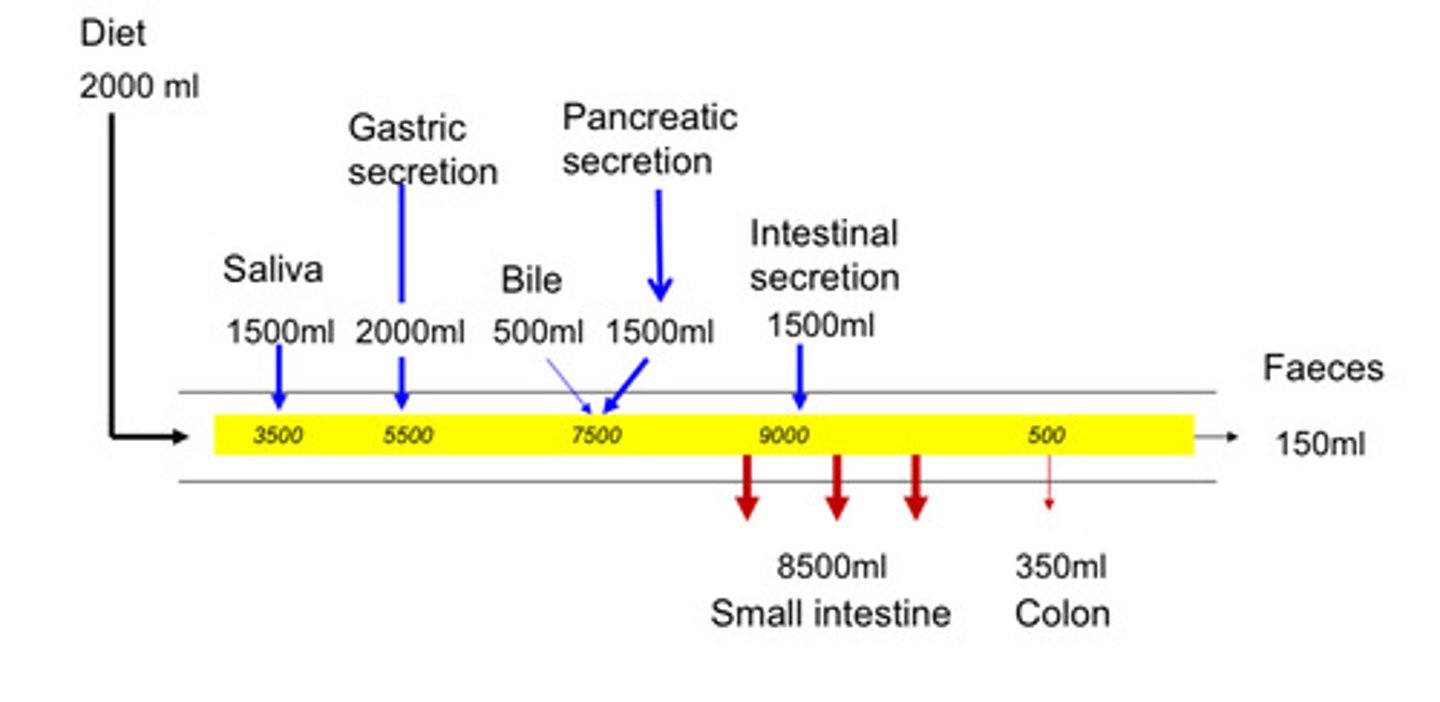
How much water flows into and out of the gut in 24 hours?
The gut handles a total of 9 liters of water daily (intake + secretions).
Intake: Approximately 2 liters of water consumed daily.
Secretions into the Gut:
Saliva: 1.5 liters
Gastric secretions: 2 liters
Bile: 0.5 liters (500 ml)
Pancreatic secretions: 1.5 liters
Intestinal secretions: 1.5 liters
Water Absorption:
Small Intestine: Absorbs 8.5 liters of water.
Colon: Absorbs 350 ml (0.35 liters).
Total Water Absorbed: 8.5 + 0.35 = 8.85 liters
Water Excreted:
Feces: Approximately 150 ml (0.15 liters) of water is excreted.
How is Saliva Secreted - MOA?
Saliva is produced by acinar cells at the base of salivary ducts, with the lumen inside and the basolateral side facing the bloodstream.
Primary Secretion by Acinar Cells:
Na+/K+ ATPase Pump: Located on the basolateral membrane of acinar cells, it drives the process by pumping Na+ out and K+ into the cell, creating a Na+ gradient.
Ion Movement: Na+ flows into the acinar cells via channels, followed by Cl- and HCO3- through co-transporters (e.g., Na+/K+/2Cl- co-transporter). K+ exits the cell, maintaining the gradient.
Water Movement: The movement of Na+ and Cl- into the acinar lumen (between cells) creates an osmotic gradient, pulling water into the lumen via osmosis.
Result: The primary secretion is a watery, isotonic fluid (same solute concentration as plasma).
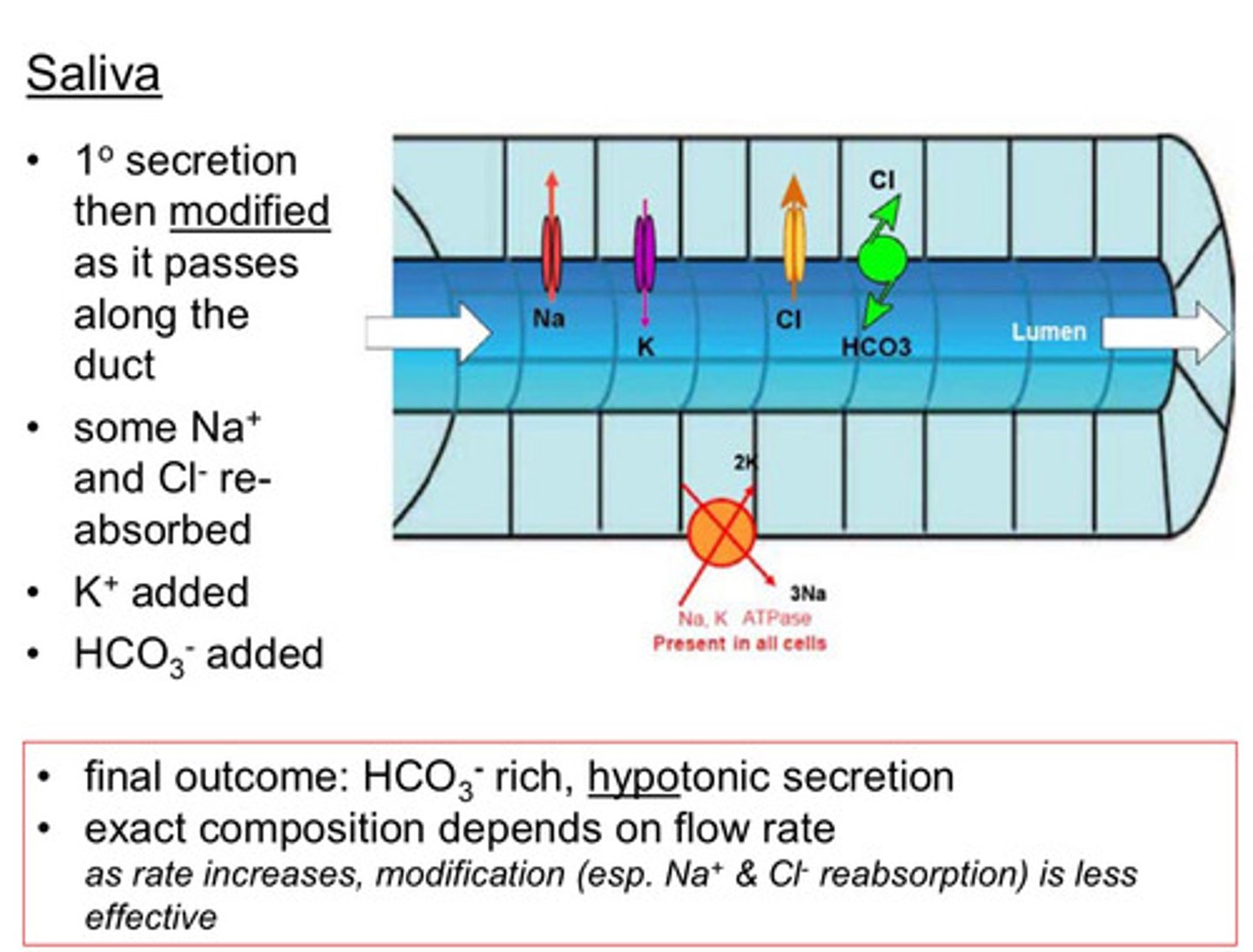
Modification in Salivary Duct:
As the primary secretion passes through the salivary duct, it is modified:
Na+ and Cl- Reabsorption: Some Na+ and Cl- are reabsorbed into the bloodstream.
K+ and HCO3- Addition: K+ and HCO3- are secreted into the saliva.
Purpose: Adjustments depend on the oral cavity's needs (e.g., pH buffering via HCO3-).
Final Outcome:
The final saliva is hypotonic (lower solute concentration than plasma) and HCO3--rich, aiding in buffering and digestion.
Flow Rate Impact: At higher flow rates, modification (especially Na+ and Cl- reabsorption) becomes less effective, reducing HCO3- concentration in the saliva.
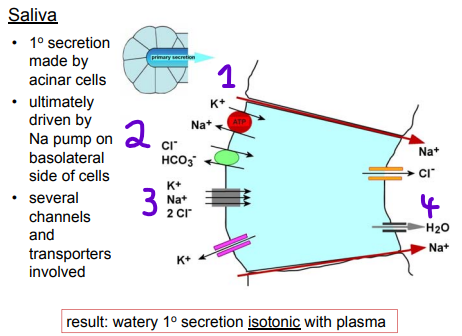
Diagram of Primary Secretion modification of Saliva
Modification Process:
As the primary secretion travels through the salivary duct, it is modified based on the mouth's needs (e.g., to neutralize pH or adjust ion balance):
Na+ and Cl- Reabsorption: Some sodium and chloride are reabsorbed to adjust adjust ion concentration balance.
K+ and HCO3- Addition: Potassium and bicarbonate are added to the secretion to neutralise pH
These changes help tailor saliva for functions like buffering (via HCO3-) or maintaining oral environment.
Final Outcome:
The final saliva is hypotonic (Lower solute concentration than plasma) and bicarbonate-rich, aiding in neutralizing acids in the mouth.
Flow Rate Impact:
Higher Flow Rates: At FASTER flow rates (e.g., before vomiting, when salivary glands are highly active), there’s LESS time for modification. Less Na+ and Cl- are reabsorbed, leading to a saltier taste (practical example: saliva tasting salty before being sick).
Lower Flow Rates: MORE time for modification results in greater Na+ and Cl- reabsorption and a higher HCO3- concentration.
What are the other components of Saliva and what is its function?
Saliva serves as a multifunctional fluid, providing lubrication, initiating digestion, offering antimicrobial protection, and safeguarding teeth.
Ions:
Includes Ca²⁺ (calcium) and phosphate, contributing to saliva's protective role.
Large Molecule Components:
Mucins (Glycoproteins): Released by acinar cells via exocytosis, making saliva slightly sticky and viscous, forming mucus to aid lubrication.
Lysozyme: An enzyme with antimicrobial properties, released by acinar cells via exocytosis.
Amylase: Initiates starch digestion, released by acinar cells via exocytosis.
Immunoglobulin A (IgA): Produced by nearby plasma cells (B lymphocytes), binds to receptors on the basolateral side of acinar cells, and is transported into the lumen for immune defense.
What are the functions of Saliva?
Lubrication: Mucins lubricate food, aiding chewing and swallowing, preventing discomfort as the bolus moves down the oesophagus.
Digestion: Amylase begins starch breakdown into sugars (e.g., glucose) for further digestion.
Antimicrobial Activity: Lysozyme and IgA protect against pathogens, critical due to the mouth’s exposure to the environment.
Tooth Protection: The pH and specific mix of Ca²⁺ and phosphate ions help prevent tooth demineralization, supporting dental health.
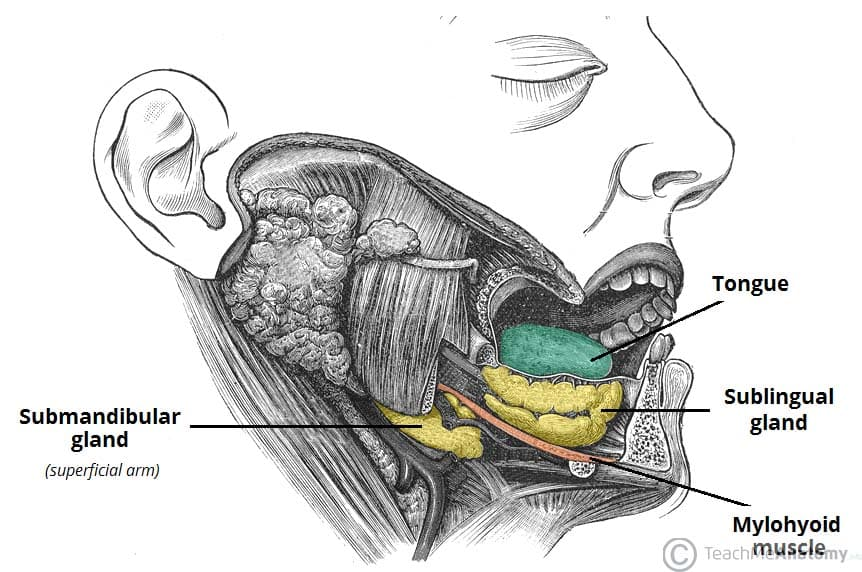
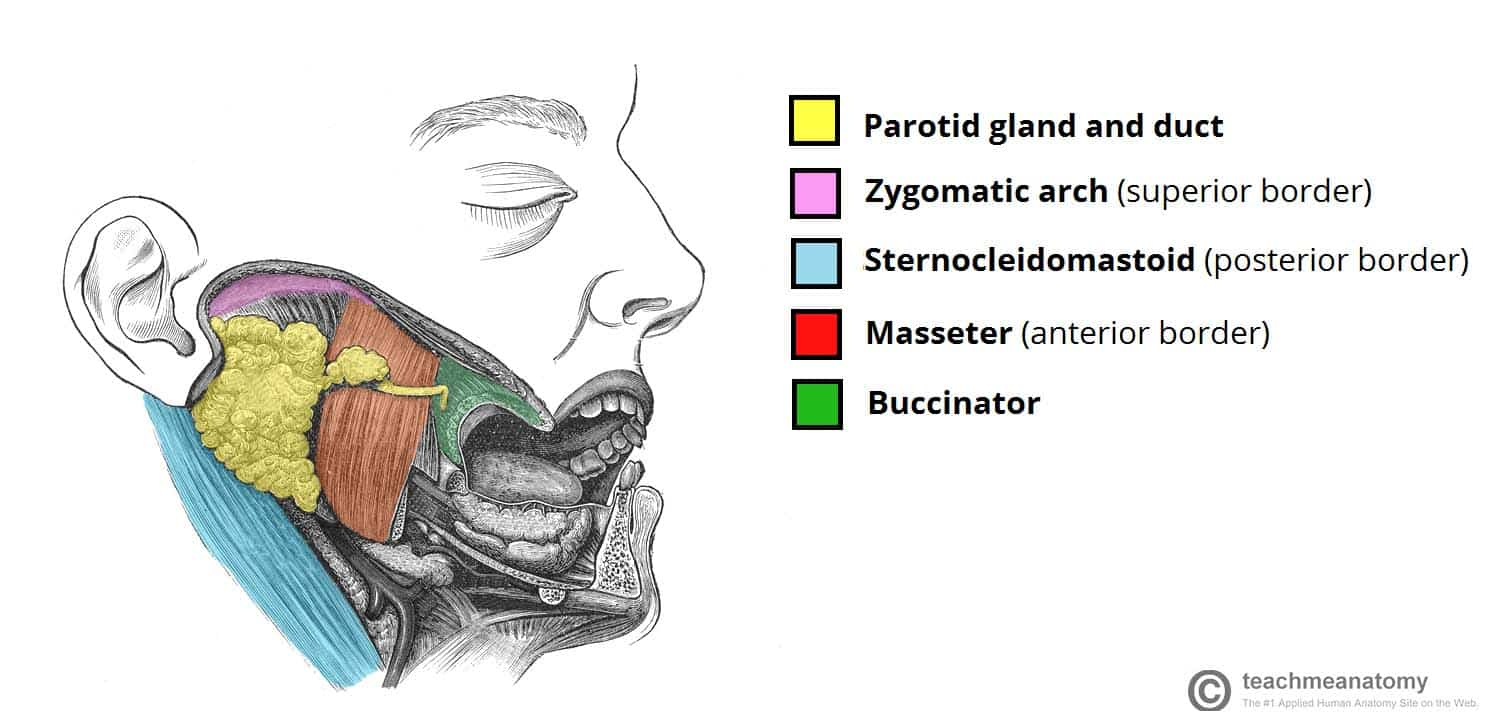
What are the different types of Salivary Glands?
Parotid Glands: Primarily produce amylase (for starch digestion) with less mucus.
Submandibular Glands: Produce a mix of amylase and mucus, with mucus being more prominent than amylase.
Sublingual and Minor Mucous Glands: Mainly produce mucus, with minimal amylase.
—
-Parotid: amylase > mucus
-Submandibular: amylase < mucus
-Sublingual & minor mucous: mucus
Differences between glands: in exact composition: Parotid: amylase > mucus; Submandibular: amylase < mucus; Sublingual & minor mucous: mucus in highest flow rates: basal condition: submandibular; stimulated: parotid
Under Basal conditions what salivary gland has the highest flow rate?
Submandibular
—
Basal conditions describe the baseline secretion rate of saliva when there is no significant stimulation (e.g., from chewing or tasting food). This represents the minimal, continuous flow of saliva to maintain oral health and lubrication under normal circumstances.
Under stimulated conditions what salivary gland has the highest flow rate?
Parotid
—
Under the influence of external stimuli (chewing or tasting food)
How are salivary glands controlled
Autonomic Nervous System (ANS):
Parasympathetic Stimulation: Increases the formation of fluid and electrolyte components of saliva, resulting in a more watery secretion to maintain oral hydration and support digestion.
Sympathetic Stimulation: Enhances the release of macromolecular components, such as amylase (for starch digestion) and mucus (for lubrication and protection), making saliva more viscous.
What is secreted in the oesophagus and why is this secreted?
The oesophagus secretes MUCUS using widespread minor glands that secrete only mucus.
Control of Secretion:
Secretion is neurally controlled, primarily by the autonomic nervous system.
Purpose of Secretion:
Lubrication: Mucus lubricates the oesophageal tube, facilitating the rapid passage of food to the stomach.
Protection: Mucus protects the lower oesophagus from acidic damage due to reflux, especially if the sphincter (e.g., lower oesophageal sphincter) is faulty.
What are the 3 phases of Digestion
1) Cephalic Phase (All Neural Control):
Triggers: Thinking about food or presence of food in the mouth (e.g., Pavlov’s dogs experiment).
Mechanisms:
Promotes salivary and gastric secretions via neural (extrinsic) control.
Amylase in saliva initiates starch digestion.
Chewing breaks food into smaller particles.
2) Gastric Phase (Neural - Brain, Enteric Nervous System, Hormones):
Triggers: Presence of food in the stomach.
Mechanisms:
Stomach secretes hydrochloric acid and pepsinogen in response to food.
Gastric motility and secretions are controlled by the brain, enteric nervous system (ENS), and hormones, facilitating mechanical breakdown and protein digestion.
3) Intestinal Phase (Neural - Brain, Enteric Nervous System, Hormones):
Triggers: Food entering the small intestine.
Mechanisms:
Controlled by neural (brain and ENS) and hormonal signals.
Hormones inhibit gastric secretion and motility [enterogastrone] while promoting biliary and pancreatic secretions into the duodenum [CCK / Gastrin].
Most digestion and nutrient absorption occur during this phase.
![<p><strong><u>1) </u><mark data-color="purple" style="background-color: purple; color: inherit"><u>Cephalic Phase</u></mark><u> (All Neural Control):</u></strong></p><p>Triggers: Thinking about food or presence of food in the mouth (e.g., Pavlov’s dogs experiment).</p><p><strong>Mechanisms:</strong></p><ul><li><p>Promotes <mark data-color="red" style="background-color: red; color: inherit">salivary and gastric secretions via neural (extrinsic) control.</mark></p></li><li><p><mark data-color="red" style="background-color: red; color: inherit">Amylase in saliva initiates starch digestion.</mark></p></li><li><p><strong><mark data-color="blue" style="background-color: blue; color: inherit">Chewing breaks food into smaller particles.</mark></strong></p></li></ul><p></p><p><strong><u>2) </u><mark data-color="purple" style="background-color: purple; color: inherit"><u>Gastric Phase (Neural - Brain, Enteric Nervous System, Hormones)</u></mark><u>:</u></strong></p><p>Triggers: Presence of food in the stomach.</p><p><strong>Mechanisms:</strong></p><ul><li><p>Stomach secretes<strong><mark data-color="red" style="background-color: red; color: inherit"> hydrochloric acid and pepsinogen</mark></strong> in response to food.</p></li><li><p>Gastric motility and secretions are controlled by the brain, enteric nervous system (ENS), and hormones, facilitating <strong><mark data-color="blue" style="background-color: blue; color: inherit">mechanical breakdown and protein digestion.</mark></strong></p></li></ul><p></p><p><strong><u>3) </u><mark data-color="purple" style="background-color: purple; color: inherit"><u>Intestinal Phase (Neural - Brain, Enteric Nervous System, Hormones)</u></mark><u>:</u></strong></p><p>Triggers: Food entering the small intestine.</p><p><strong>Mechanisms:</strong></p><ul><li><p>Controlled by neural (brain and ENS) and hormonal signals.</p></li><li><p><mark data-color="red" style="background-color: red; color: inherit">Hormones inhibit gastric secretion and motility </mark><strong><mark data-color="red" style="background-color: red; color: inherit">[enterogastrone] </mark></strong><mark data-color="red" style="background-color: red; color: inherit">while promoting biliary and pancreatic secretions into the duodenum </mark><strong><mark data-color="red" style="background-color: red; color: inherit">[CCK / Gastrin]</mark></strong><mark data-color="red" style="background-color: red; color: inherit">.</mark></p></li><li><p><strong><mark data-color="blue" style="background-color: blue; color: inherit">Most digestion and nutrient absorption occur during this phase.</mark></strong></p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/423e0f39-95dc-4bbf-a3ba-35781fadfa7c.png)
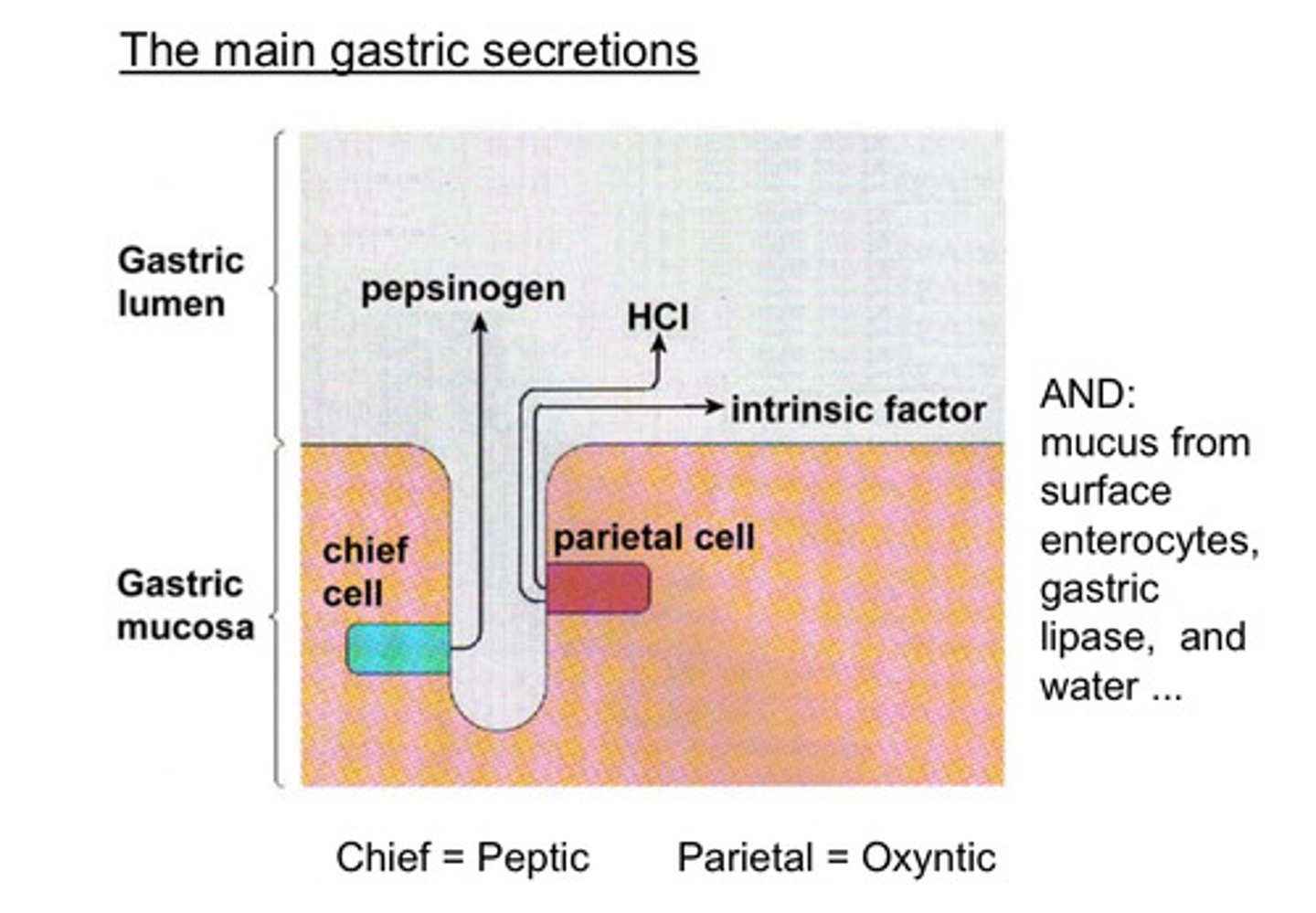
What are the main gastric secretions in the stomach?
Pepsinogen → Pepsin / Hydrochloric acid (HCl) for pepsin activation / Intrinsic factor, crucial for Vitamin B12 / Mucus / Gastric Lipase / Water
—
Chief Cells (located in gastric pits):
Secrete Pepsinogen, which activates to pepsin to begin protein digestion.
Parietal Cells (located in gastric pits):
Secrete hydrochloric acid (HCl) to create an acidic environment for pepsin activation and pathogen control.
Secrete intrinsic factor, crucial for vitamin B12 absorption in the ileum.
Surface Enterocytes:
Secrete mucus to protect the stomach lining from acid and enzymes.
Other Secretions:
Gastric lipase, which starts breaking down fats.
Water, contributing to the luminal fluid environment.
What is the Mechanism of acid secretion in the stomach?
Hydrochloric acid secretion is critical for creating an acidic environment in the stomach lumen to break down food and activate digestive enzymes like pepsin.
H⁺ secretion results in a net movement of HCO₃⁻ into the blood, maintaining cellular balance while the stomach lumen becomes highly acidic.
Mechanism:
H⁺ Production:
CO₂ and H₂O react, catalyzed by carbonic anhydrase, to form H₂CO₃ (carbonic acid).
H₂CO₃ dissociates → HCO₃⁻ (bicarbonate) + H⁺, with H⁺ used for acid secretion.
Cl⁻ Uptake:
Cl⁻ is obtained from the blood via a HCO₃⁻/Cl⁻ exchanger on the basolateral membrane, moving Cl⁻ into the cell while HCO₃⁻ exits into the blood.
Proton Pump (H+/K+-ATPase):
Requires ATP to pump H⁺ ions into the lumen against their concentration gradient.
Acid Formation:
H⁺ (via the proton pump) and Cl⁻ (via channels) enter the lumen, forming HCl.
The liberation of H⁺, proton pump activity, and Cl⁻ movement create the acidic environment.
Water Movement:
Net ion movement (H⁺ and Cl⁻) into the lumen drives water movement via osmosis, contributing to the fluid in the stomach.
—
Clinical Relevance:
Proton Pump Inhibitors (PPIs): Block the H+/K+-ATPase pump to inhibit acid secretion, used to treat reflux and related conditions by reducing stomach acidity.
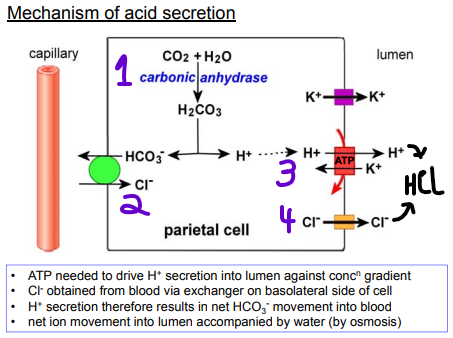
Why do parietal cells have lots of mitochondria?
Parietal cells have lots of mitochondria because they need LARGE AMOUNTS OF ATP to power the H⁺/K⁺-ATPase pump, which secretes HCl into the stomach.
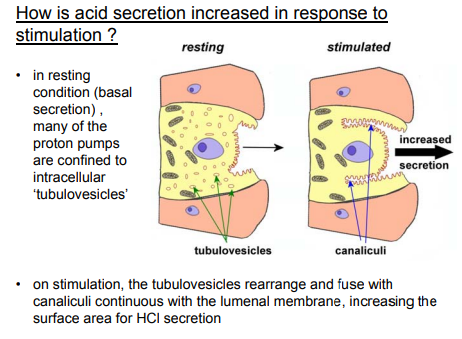
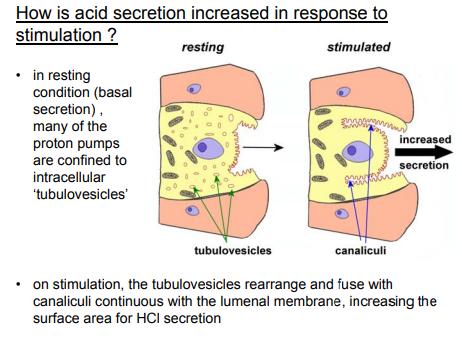
Why do Parietal cells have tubulovesicles?
Tubulovesicles act as a reservoir for proton pumps:
Tubulovesicles are little bits of epithelium which store proton pumps (H⁺/K⁺-ATPase) when inactive
This rapidly mobilizes to the cell membrane when acid secretion is needed (e.g., by food or gastrin).
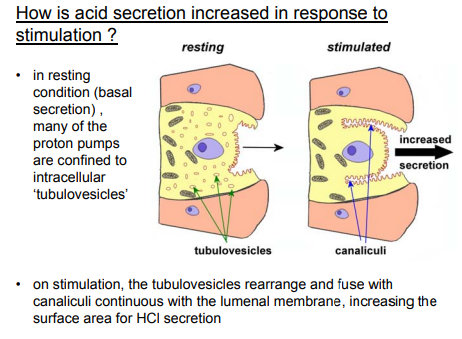
How is acid secretion from the parietal cell increased in response to stimulation?
Resting State (Basal secretion):
Proton pumps (H⁺/K⁺-ATPase) are stored in tubulovesicles (inactive).
The luminal membrane has minimal surface area.
Upon Stimulation (By Gastrin / Histamine / Acetylcholine - ACh):
Tubulovesicles rearrange, fusing with the canaliculi (invaginations of the epithelium).
This dramatically increases surface area, inserting more proton pumps into the membrane.
Results in Rapid, high-volume HCl secretion into the stomach.
Allows a fast, powerful response to digestive demands.
Without this mechanism, acid secretion would be too slow/weak.
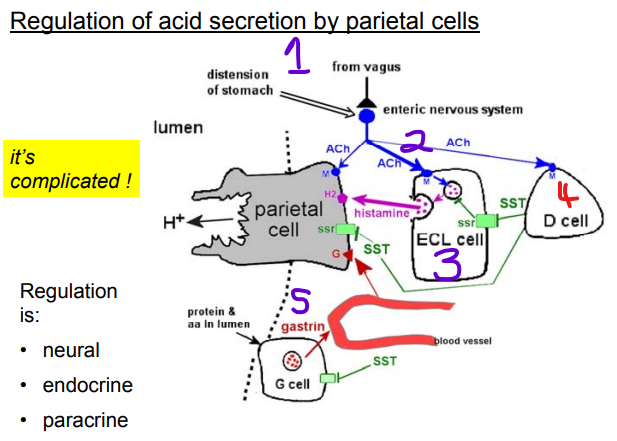
How is acid secretion regulated by parietal cells? Hint 3 ways
Neural Regulation:
Enteric Nervous System (ENS) + Vagus Nerve (CNS): → Responds to distension from your stomach to secrete acids
Mechanism:
Vagus/ENS releases acetylcholine (ACh).
ACh binds muscarinic (M₃) receptors on parietal cells → directly stimulates acid secretion.
Also acts on ECL cells (indirectly via histamine) and D cells (inhibitory).
Paracrine Regulation:
Acetylcholine (ACh): acts via the muscarinic receptor, causing direct stimulation onto the Parietal cells and ECL cells and D cells
ECL cells → releases histamine → binds H₂ receptors on parietal cells → potent acid secretion.
~~
D cells → releases somatostatin (inhibitory).
Inhibition: Somatostatin (from D cells) is the brake on BOTH pathways (blocks ECL/parietal cells).
Binds to SST2 receptors.
Endocrine Regulation:
Gastrin (from G cells in stomach antrum): Responds to Protein/amino acids presence in stomach lumen.
Mechanism:
Gastrin circulates in blood → binds TO CCK₂ receptors on BOTH:
Parietal cells (minor direct effect).
ECL cells → releases histamine → amplifies acid secretion.
Note: Due to Paracrine regulation, muscarine and histamine agonists help secrete gastrin
But all controlled by proton pump
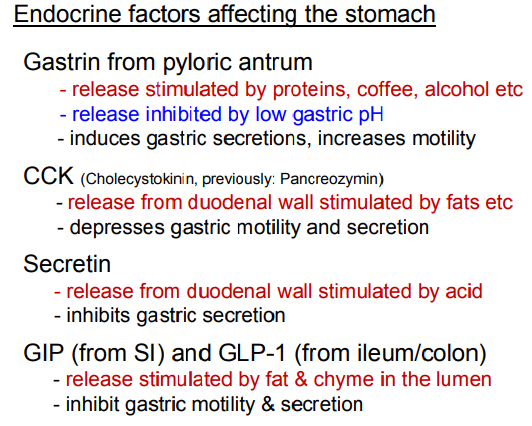
What 4 endocrine factors effect the stomach?
Regulation of Stomach Function:
Gastrin:
From G cells in the pyloric antrum (near the duodenum).
Activators: Release stimulated by Proteins, coffee, alcohol.
Inhibitor: Low gastric pH (<3) ("stop if the stomach is empty/acidic").
Induces gastric secretions, increases motility (via parietal + ECL cells → histamine).
Cholecystokinin (CCK):
From I cells in the duodenal wall.
Release stimulated by Fats
Slows gastric motility and acid secretion to stop stomach releasing load into the duodenum if at full capacity.
Secretin:
From S cells in the duodenal wall.
Release stimulated by Acidic chyme
Inhibits gastric secretion (protecting the duodenum).
GIP & GLP-1:
GIP from the Small intestine (K cells) & GLP-1 from the Ileum/colon (L cells) respectively.
Release stimulated by arrival of fats & glucose
Incretin effect: Boost insulin (GLP-1 > GIP).
Inhibits gastric motility/secretion (protecting the duodenum).
Feedback Loops:
Acid turns off gastrin (via somatostatin).
Nutrients trigger incretins (GLP-1/GIP) to optimize absorption.
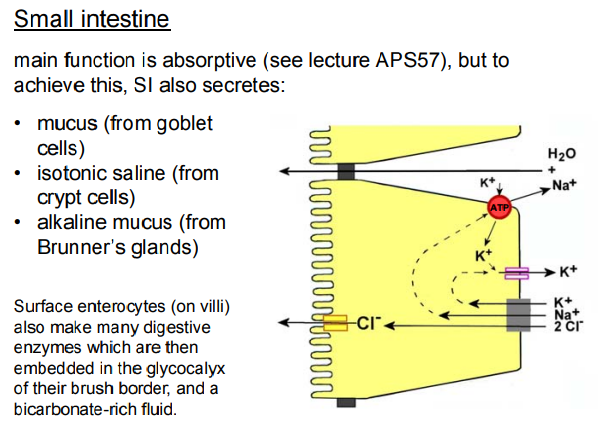
What is the main function of small intestine (SI) and and what else does it secrete to aid it carrying out this function?
Main Function: Absorption
The SI is where 90% of nutrient absorption occurs, enabled by:
Villi / Microvilli: Massive surface area expansion.
Brush Border Enzymes: Final digestion at the site of absorption.
Secretions Supporting Absorption:
• Mucus (from Goblet Cells) - Protective, Defensive barrier (Forms the unstirred layer atop villi) and a lubricant (Enabling smooth chyme movement)
• Isotonic Saline (from Crypt Cells) (base of villi) - Maintains osmotic balance for nutrient transport. Prevents dehydration of the epithelial surface.
• Alkaline Mucus (from Brunner’s Glands) (Duodenum (submucosa)) - Neutralizes stomach acid ("stops the duodenum from being burned"). Rich in HCO₃⁻ (bicarbonate) to raise pH for enzyme function.
Note:
Surface enterocytes (on villi) - Make many digestive enzymes which are then embedded in the glycocalyx of their brush border, and a bicarbonate-rich fluid - to neutralise the acidic chyme (a semi-fluid mixture of partially digested food, stomach acid, digestive enzymes, and fluid) coming through the stomach.
Brush Border Enzymes (on Enterocytes) (Embedded in the glycocalyx) - Final digestion just before absorption. Eg. Lactase, sucrase (carbs), peptidases (proteins), enterokinase (activates trypsin).
What is the difference between endocrine and exocrine secretions?
Endocrine glands:
Release hormones directly into the bloodstream, where they travel to cells throughout the body. Endocrine glands are also known as ductless glands. e.g. pituitary, thyroid, and adrenal glands
Exocrine glands:
Release substances through ducts onto the body's surfaces, such as the skin or oral cavity. e.g. salivary, sweat, and sebaceous glands
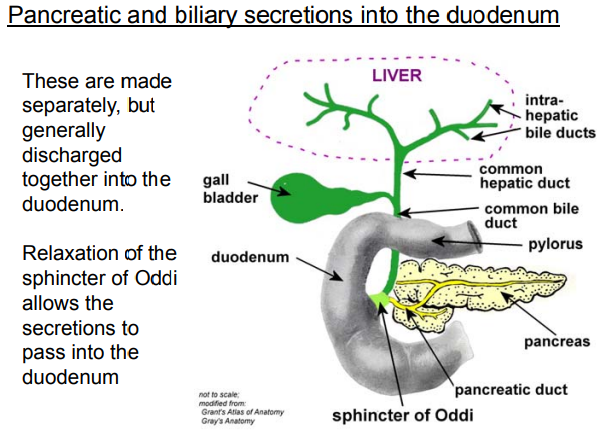
What secretions get released into the duodenum and how does this occur
The duodenum receives pancreatic juice and bile, which are produced separately & essential for digestion, acid neutralization, and fat processing.
Discharged together into the duodenum via hepatopancreatic ampulla through a coordinated mechanism.
Biliary Secretions (Bile):
Continuously synthesized by the liver → stored and concentrated in the gallbladder.
Travels via the common bile duct.
Bile salts (critical for fat emulsification).
Bilirubin (waste product).
Cholesterol/phospholipids.
Bile breaks fats into droplets → pancreatic lipase can efficiently digest them.
Pancreatic Secretions:
Exocrine pancreas releases:
Digestive enzymes (acinar cells) (Proteases (e.g., trypsin), lipase, amylase.)
Bicarbonate-rich fluid (duct cells): Neutralizes stomach acid via the pancreatic duct.
How They Reach the Duodenum:
Pathway Convergence:
The common bile duct (carrying bile) and pancreatic duct merge at the hepatopancreatic ampulla (Ampulla of Vater).
Sphincter of Oddi:
A muscular valve that normally remains closed to prevent leakage.
Relaxation triggered by:
CCK (released in response to fats in the duodenum).
Secretin (stimulated by acidic chyme).
Allows simultaneous release of bile and pancreatic juice.
Important for digestion, lipid digestion, and neutralisation of the chyme
What are the 2 main components of Pancreas exocrine secretions
1) Alkaline fluid rich in HCO3-
• Produced largely by the cells of the pancreatic duct
• Role is to neutralize the acidic chyme entering the small intestine from the stomach.
2) Digestive enzymes
• Includes endopeptidases, carboxypeptidase, amylase, lipase, etc
• Produced largely by the acinar cells, and stored intracellularly as inactive precursor forms in ‘zymogen’ granules
• Released by exocytosis
• Role is to break down most macromolecules found in food
What hormones affect pancreatic exocrine secretion
• CCK:
- Released from duodenal wall by fats etc
- Induces release of enzyme-rich secretions
• Secretin:
- Released from duodenal wall by acidic chyme
- Induces release of bicarbonate-rich secretions
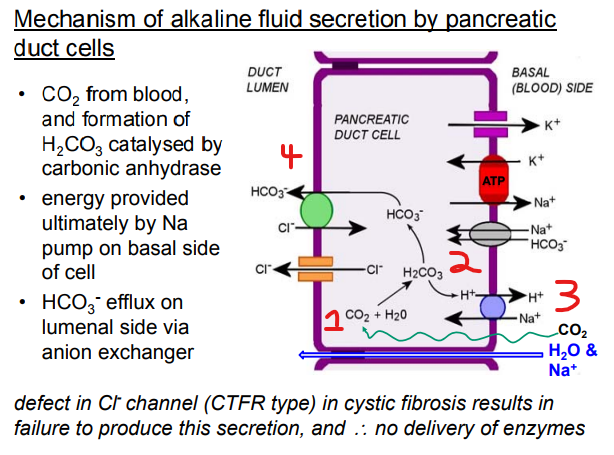
What is the Mechanism of fluid secretion by pancreatic duct cells?
HCO₃⁻ Production:
CO₂ and H₂O react, catalyzed by carbonic anhydrase, to form H₂CO₃ (carbonic acid).
H₂CO₃ dissociates → HCO₃⁻ (bicarbonate) + H⁺, with HCO₃⁻ used for neutralisation → (Very important as it alkali and will neutralise any acid)
Energy provided ultimately by Na pump on basal (blood) side of cell
—
• HCO₃⁻ efflux on luminal side via anion exchanger
• CFTR ion channel takes the Cl- out of the cell
Note:
Defect in Cl- channel (CTFR type) in cystic fibrosis results in failure to produce this secretion, and therefore no delivery of enzymes = can't produce the right pancreatic digestive juices or neutralise the acidic chyme
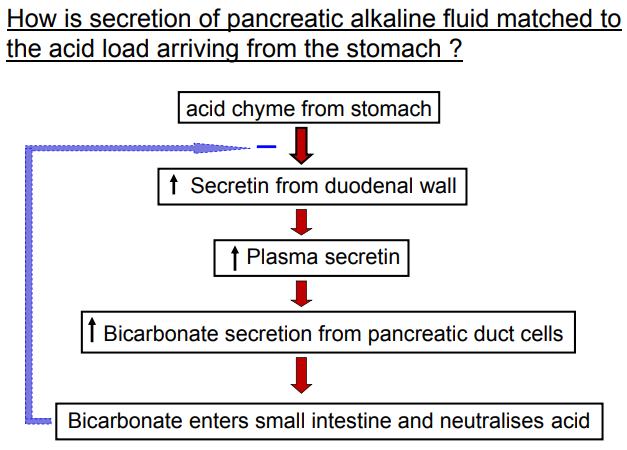
How is secretion of pancreatic alkaline fluid matched to the acid load arriving from the stomach ?
Acid Detection: The acid chyme from the stomach enters the duodenum, acting as the trigger based on the acid load's intensity.
Secretin Release: The duodenal wall responds to the acid by releasing secretin into the bloodstream. The amount of secretin released is PROPORTIONAL to the acid level—more acid leads to more secretin.
Pancreatic Response: Secretin stimulates the pancreatic duct cells to secrete bicarbonate, an alkaline fluid. Higher secretin levels (from more acid) result in greater bicarbonate secretion.
Neutralization: The bicarbonate enters the small intestine and neutralizes the acid, with the quantity of alkaline fluid matched to the acid load to achieve a balanced pH.
This ensures the pancreas secretes just enough alkaline fluid to neutralize the incoming acid, protecting the small intestine and optimizing digestion.
Note: The bicarbonate can feedback to inhibit gut motility (Negative Feedback Loop)
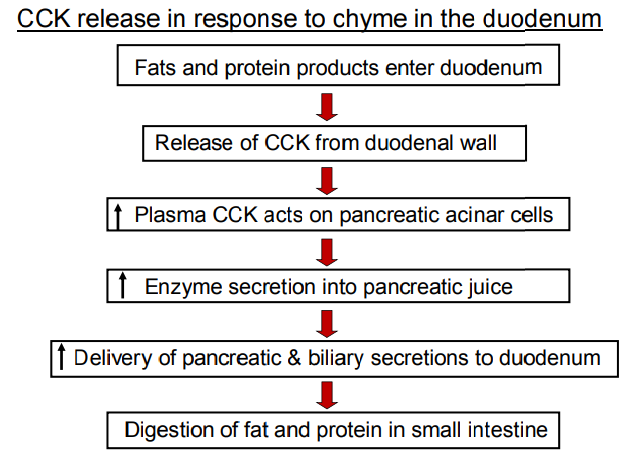
How is CCK released in response to chyme in the duodenum?
1) Fats and protein products enter duodenum
2) Release of CCK from duodenal wall
3) Increase in Plasma CCK acts on pancreatic acinar cells
4) Increase in Enzyme secretion into pancreatic juice
5) Increase in Delivery of pancreatic & biliary secretions to duodenum
6) Digestion of fat and protein in small intestine
Bile Secretion - How is it primarily secreted, Secondarily modified and Released from the Gall bladder?
Primary secretion made in the Liver:
• solutes made or extracted from the blood by hepatocytes, and discharged into bile canaliculi containing extracellular fluid
• bile salt/acid component important for the emulsification of fats in the SI
• bile pigments (e.g. bilirubin) = breakdown product of Hb (porphyrin ring), for excretion
• other components include cholesterol, lecithin
Secondary modification of the fluid as it passes along Bile Ducts:
• water and HCO3- added
• mechanism similar to that for pancreatic alkaline secretion
• stimulated by secretin
Release from gall bladder (where stored):
• CCK causes gallbladder to contract & sphincter of Oddi to relax
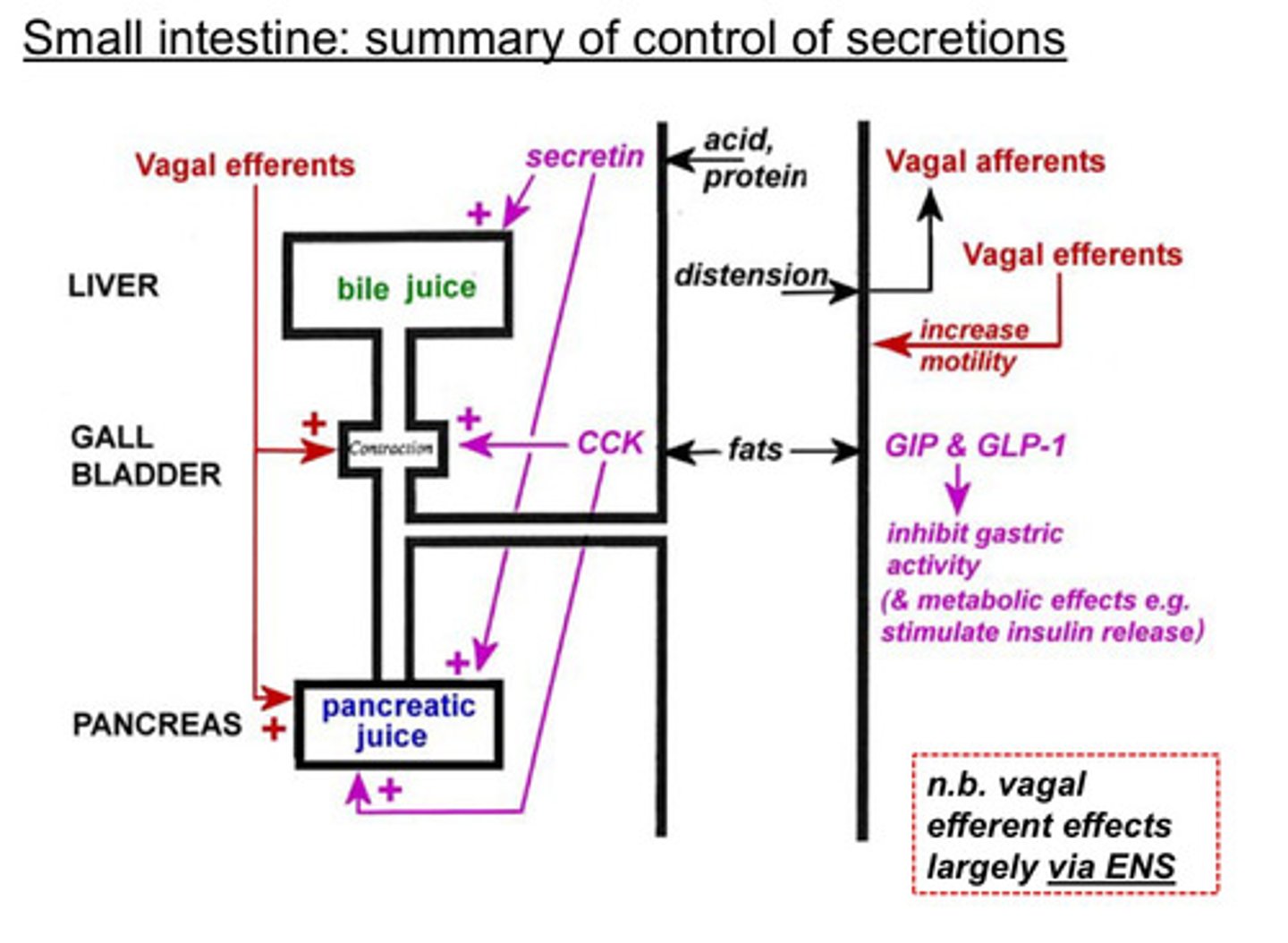
Small intestine: Summary of control of secretions
In summary, the presence of food (acid, proteins, fats) and distension in the duodenum triggers a coordinated response via hormones (secretin, CCK, GIP, GLP-1) and vagal efferents to secrete bile and pancreatic juice, aiding digestion and glucose metabolism.
Stimuli in the Duodenum:
Acid, protein, and fats from the stomach enter the duodenum.
Distension of the duodenum activates mechanoreceptors.
Hormonal Responses:
Secretin: Triggered by acid, it stimulates the pancreas to release pancreatic juice (rich in bicarbonate to neutralize acid) and the liver to produce bile juice.
CCK (Cholecystokinin): Stimulated by fats and proteins, it prompts the gallbladder to release bile for fat digestion and the pancreas to secrete pancreatic juice with digestive enzymes.
GIP (Glucose-dependent Insulinotropic Peptide) and GLP-1 (Glucagon-like Peptide-1): Released in response to nutrients, they inhibit gastric activity (slowing digestion) and have metabolic effects like stimulating insulin release for glucose utilization.
Vagal Efferents:
Vagal nerve stimulation (largely via the enteric nervous system, ENS) enhances motility and secretion of bile and pancreatic juice. It amplifies the effects of secretin and CCK.
Organs Involved:
Liver: Produces bile juice.
Gallbladder: Stores and releases bile (triggered by CCK).
Pancreas: Secretes pancreatic juice (enzymes and bicarbonate) for digestion.
How do gut hormones contribute to regulation of metabolism?
Released in response to digestion of food:
• GIP (from SI): → Stimulates insulin release (feedforward function to ensure prompt rise in circulating insulin when glucose, amino acids, etc are absorbed)
• GLP-1 (from ileum/colon) → Stimulates insulin release (feedforward function again) & inhibits glucagon release; promotes satiety
• CCK (from SI) promotes satiety: → release inhibited by digestion of food:
Release inhibited by digestion of food:
• Ghrelin (from stomach, and other parts of GI tract) → the ‘hunger hormone’ which promotes appetite and feeding behaviour
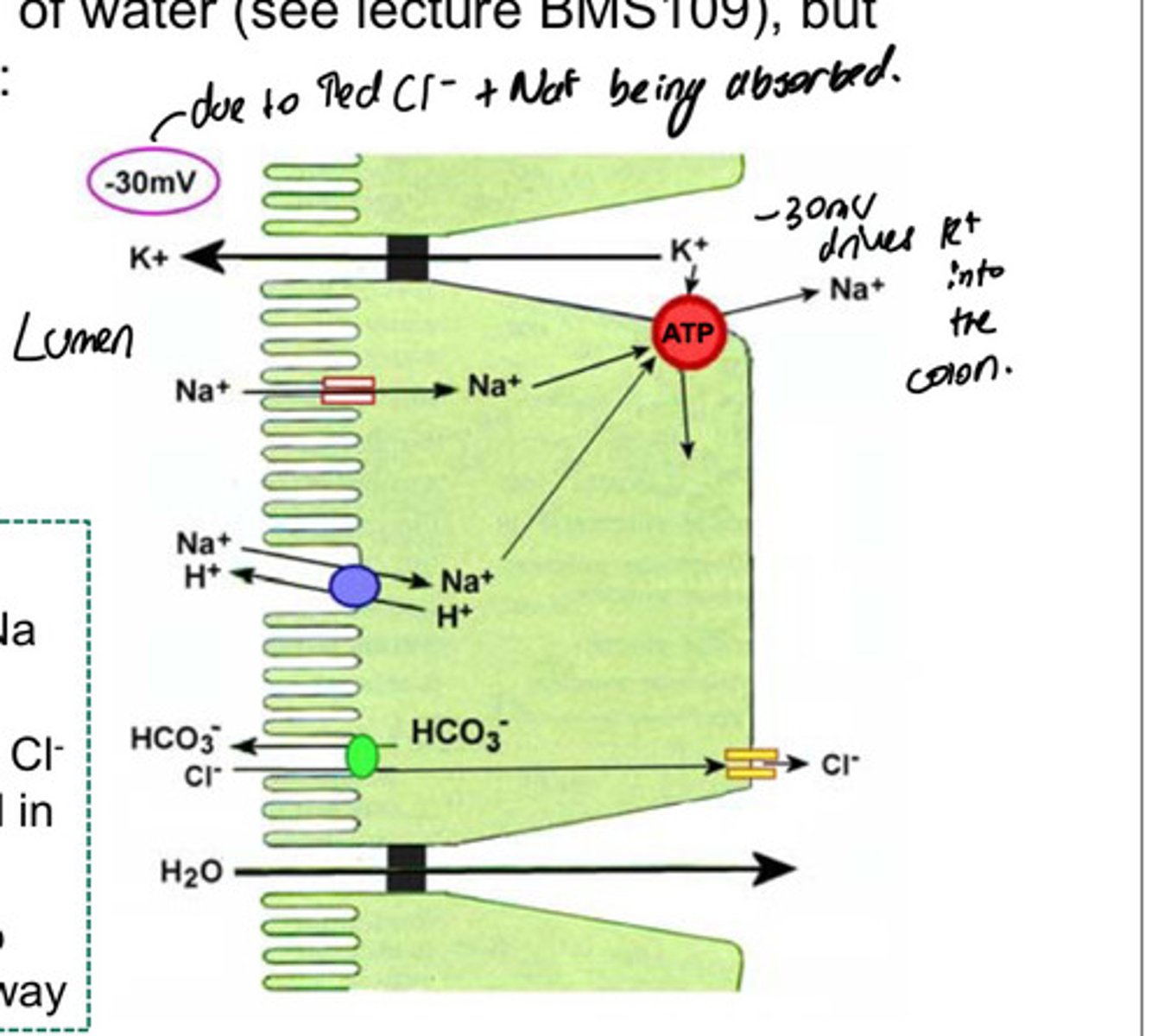
What is the main function of the colon and what secretions are made up at the colon and how does this work:
Colon: Absorption of water / Secretes key substances to maintain mucosal health and electrolyte balance.
Secretions that are made up of:
• Mucus (for lubrication) (Shields epithelium from mechanical damage and bacterial toxins.) ← Goblet cells (abundant in the colon).
• Secretion of HCO3- into the lumen (in exchange for Cl-) ← Cl⁻/HCO₃⁻ exchanger on luminal membrane.
• some secretion of K+
How does this work?
• These cells have a luminal Na channel
• Absorption of more Na+ than Cl leaves net negative potential in lumen
• This drives K+ movement into lumen, via paracellular pathway
What are some consequences of dysfunction of GI secretions: Saliva, Gastric Secretions, Pancreatic secretions, Biliary Secretions
Saliva:
• Inadequate salivary production (‘dry mouth’) leading to difficulties in swallowing, enamel damage, and reduced microbiological protection
Gastric secretions:
• Gastric atrophy – lack of intrinsic factor, leading to pernicious anaemia
• gastritis (e.g. due to H. pylori infection) - failure of mucosal barrier, and exposure to acid (not neutralisng the chyme properly) & proteases leads to gastric & duodenal ulcers
• excess acid production – leading to duodenal ulcers, Small Intestine malabsorption, diarrhoea (as water isn't be absorbed) etc
Pancreatic secretions:
• pancreatitis – leading to malabsorption because of inadequate production of digestive enzymes
• cystic fibrosis – reduced Cl- conductance reduces formation of pancreatic alkaline juice, and therefore reduces delivery of enzymes to duodenum
Biliary secretion:
• failure to make enough and/or to deliver it to duodenum – leads to malabsorption because of inadequate fat digestion