Surgery E2 random questions pt 1
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
what is a major determinant of capillary oncotic (suck) pressure?
albumin
what is used to insufflate the abdomen for laparoscopic procedures?**
CO2 through ports/trocars → 4L volume**
what are the clinical features of third-spacing?
- dec urine output despite hydration
- dec BP
- dec CV pressure
- inc. HR and body weight
- edema
what solutions are preferred for tx of third-spacing?
replace intravascular volume→ NS or LR (crystalloids preferred)
which IVF solution causes fluid to stay in intravascular space and doesn't move around?
isotonic
who is NS indicated for?
- pts at risk for fluid overload →CHF, HTN
- hemorrhage, severe vomiting/diarrhea, GI suctioning losses, wound drainage
which IVF solution causes osmotic movement of water OUT of cells and INTO intravascular space?
hypertonic → 3% NaCl
which IVF solution causes osmotic movement of water OUT of intravascular space and INTO intracellular space?
hypotonic →0.45% NaCl
who is hypertonic saline indicated for?
severe hyponatremia and cerebral edema
DONT use in HF, RF, or cellular dehydration
who is hypotonic saline indicated for?
- intracellular dehydration
- hypernatremia
- DKA
what is the minimum UOP for an adult on maintenance IV fluids?
30 mL/hr or 0.5-1 ml/kg/hr over 24 hrs
trauma pt = 50 ml/hr
post op hypotension or tachycardia is ______________ until proven otherwise
hemorrhage
what term describes UOP <400 ml/day or <20 cc/hr?
oliguria →represents impending ARF and earliest sign of inadequate organ perfusion
FENa <1% indicates ____________ azotemia**
prerenal → HF, cirrhosis, intravascaular depletion
FENa >1% indicates _____________ azotemia**
intrinsic → ATN, glomerulonephritis
FENa >4% indicates ____________ azotemia**
postrenal →obstruction
which arteries supply 60% of breast blood?
anterior perforating intercostal arteries*** →arise from internal mammary artery or internal thoracic artery
where does majority of lymphatic drainage occur?
through the axilla (75%) and internal mammary nodes
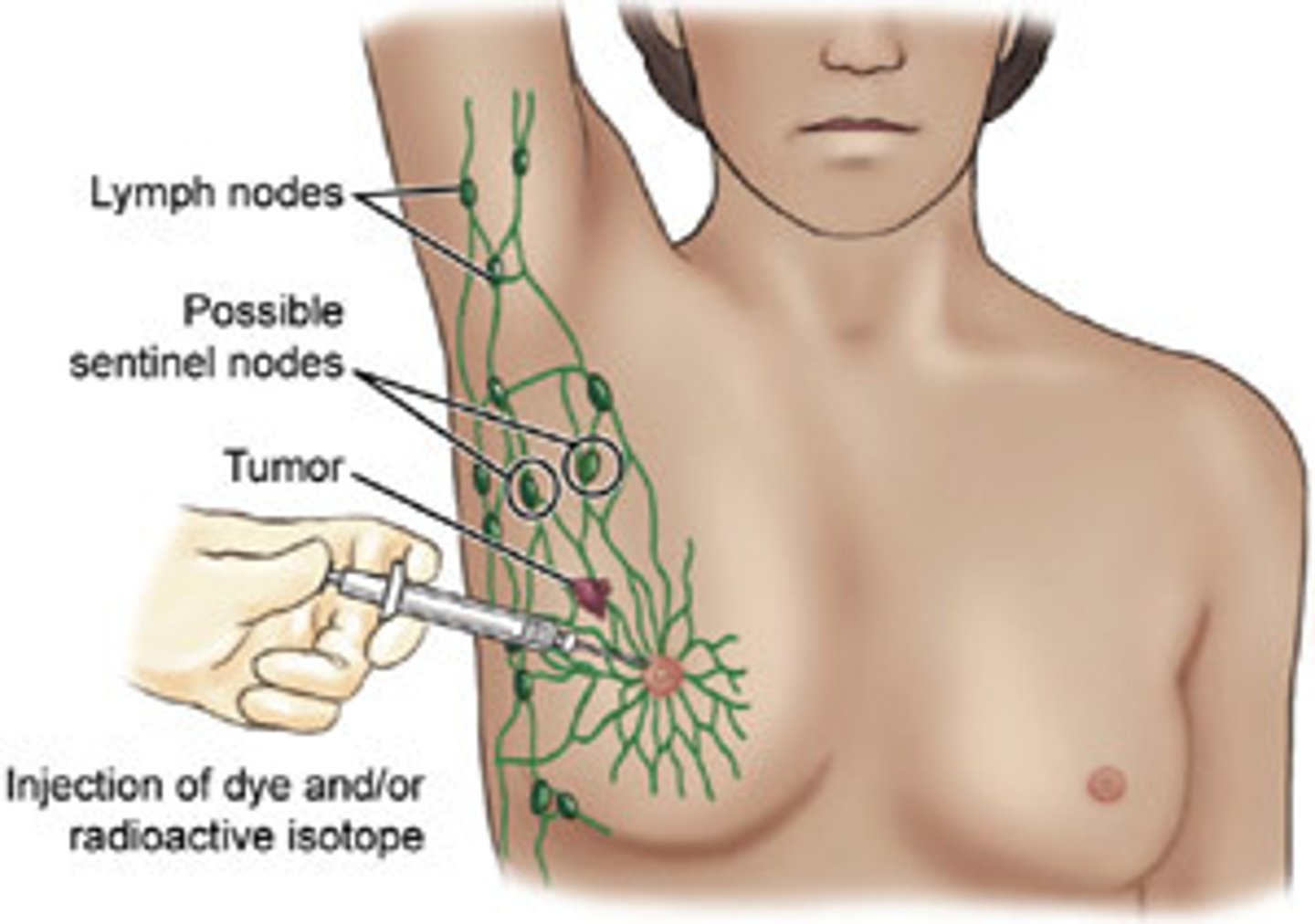
what is the rationale for sentinel node biopsy during rx of early breast cancer?***
- lowest node draining the cancer is biopsied
- if negative → axillary node dissection avoided
- usually an axillary node!
what are the 4 nerves to be aware of during axillary dissection?
long thoracic
thoracodorsal
medial pectoral
lateral pectoral
which pathology of cancer is involved in 90% of invasive breast cancers?
infiltrating ductal carcinoma (IDC) ***
which type of breast cancer tends to grow in a single file nature, making it difficult to detect?
infiltrating lobular carcinoma
what are the treatments for the different stages of hypoxia?
mild = nasal cannula
moderate = face mask, non-rebreather, HFNC
severe = mech vent
severe resp distress = intubation
after how many days on a mechanical ventilator is trach indicated?
> 10 days
which ligaments anchor breast tissue to the pectoralis muscle?
ligaments of cooper
Cooper's troopers!!

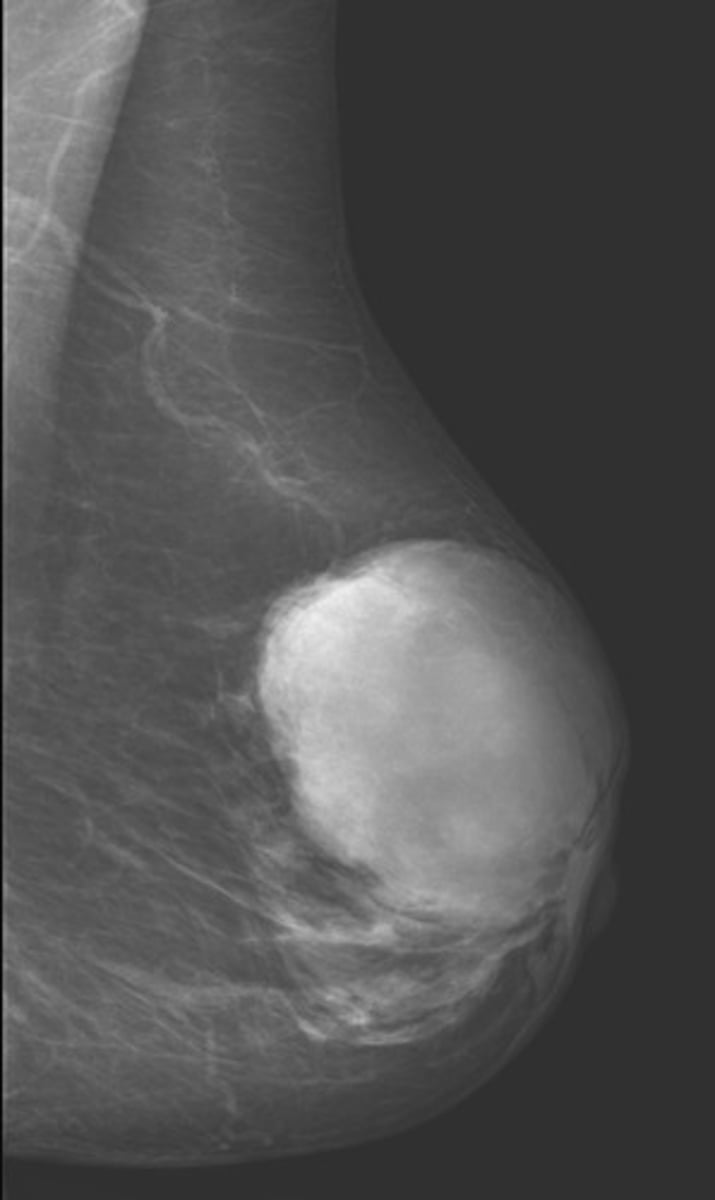
what is the MC screening modality for breast cancer?
mammogram
which imaging study is used for local staging for DCIS and lobular cancer?
MRI →BIRADS score
1 = negative
2 = benign
3 = low sus
4 = sus
5 = super sus
6 = confirmed cancer
how is breast cancer diagnosed? how is it staged?
FNA bx
TNM staging
which hormonal therapies are used for ER+ breast cancer?
tamoxifen → use for 5 yrs
aromatase inhibitors → post-menopausal women
which breast surgery involves removal of the lesion only?
lumpectomy
central lump → periareolar incision
peripheral lump → curvilinear incision
who is nipple-sparing mastectomy possible in?
pts with cancer >2 cm away from nipple
what is the difference between a total mastectomy, radical mastectomy, and modified radical mastectomy?
total = removal of affected breast only
radical = removal of affected breast, ALL lymph axillary drainage, pectoral muscle
modified radical = removal of affected breast and PART of the axillary lymph drainage, preserves underlying muscles
damage to which nerve during breast surgery can cause winged scapula?
long thoracic nerve

what is known as swelling d/t obstructed lymph flow?
lymphedema → thick rough skin, pigment changes (usually dark), fibrosis
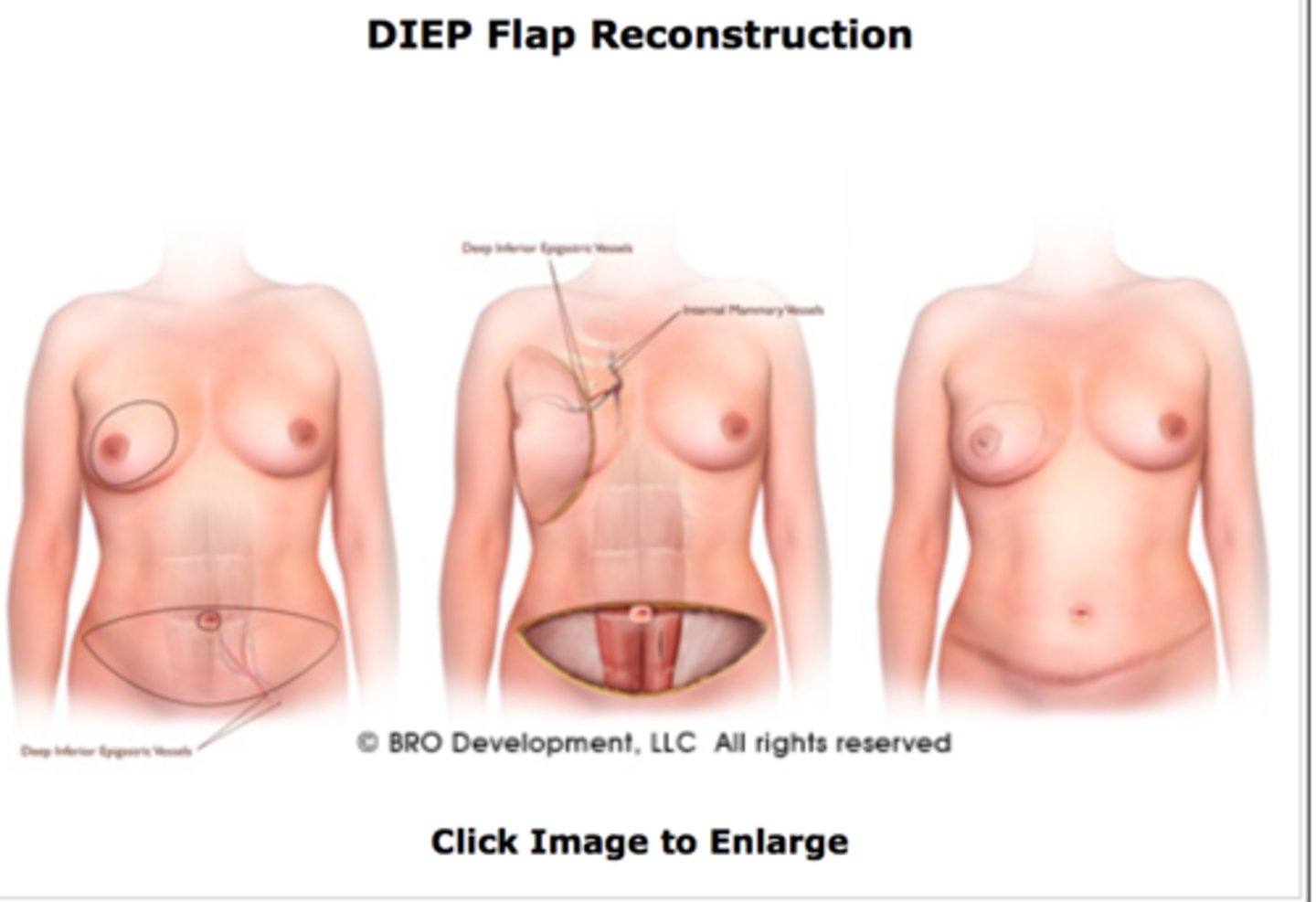
what is a DIEP flap?
removes tissue from lower abdomen with perforators and blood vessels
no muscle removed, but cut into to retrieve deep perforators!
what is a SIEA flap?
similar to DIEP but removes superficial perforators (doesn't cut into muscle)
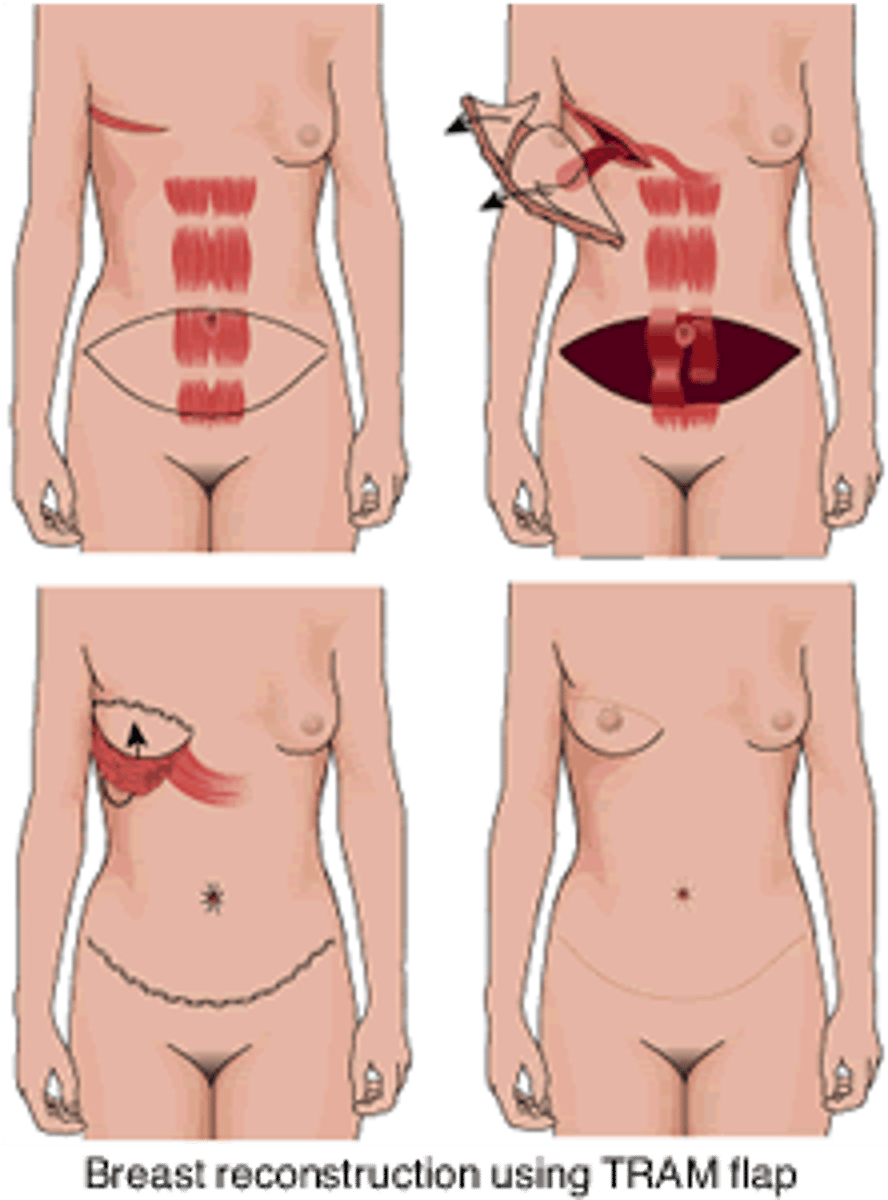
what is a TRAM flap?
Transverse Rectus Abdominis Muscle (TRAM) is rotated on its pedicle or transferred as a free flap to reconstruct the breast mound
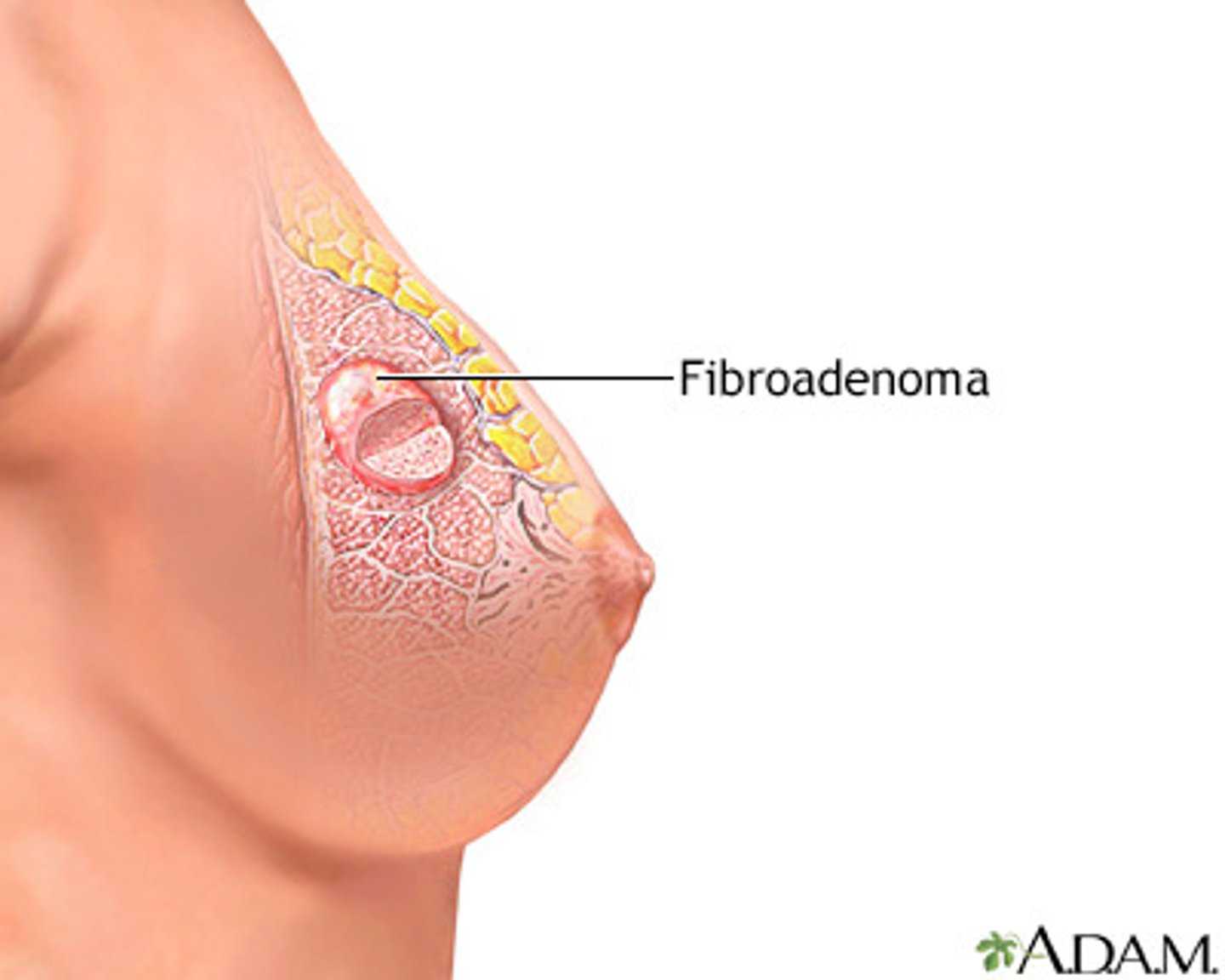
what is a painless, unilateral, firm rubbery breast mass with irregular borders?
fibroadenoma
what is the genetic cause of phyllodes tumors?
li-fraumeni syndrome
what is a unilateral, firm, enlarging painless breast mass?
Phyllodes tumor → high recurrence rate and/or metastatic potential
may stretch skin and show superficial veins
what is the mainstay of treatment for phyllodes tumors?
surgery →wide local excision with >1cm margins
large tumors may require mastectomy!
what is the MC congenital defect of male genitalia?
cryptorchidism → confirm with US and tx with orchiopexy
what is the tx for testicular torsion?
bilateral orchiopexy to scrotum
what imaging study diagnoses torsion?***
stat scrotal US + doppler
what is the gold standard for dx of urethral injury?
retrograde urethrogram
how would you treat a urethral injury?
cystoscopy with urethral repair
how long should a post-op foley be left in after urethral repair?
1-3 months
what are the s/sx of urethral injury?
blood at meatus
dysuria/retention
palpable bladder
usually follows trauma!
what are the surgical indications for BPH?
- PVR >100 ml
- retention
- gross hematuria
- recurrent UTIs
what is the MC prostate cancer?
adenocarcinomas → stimulated by testosterone
what are the surgical complications of prostatectomy?
- hematuria
- painful/difficulty urinating
- incontinence
- infection
- retrograde ejaculation
how is prostate cancer diagnosed?***
DRE and PSA is abnormal → get a biopsy (gold standard) to confirm
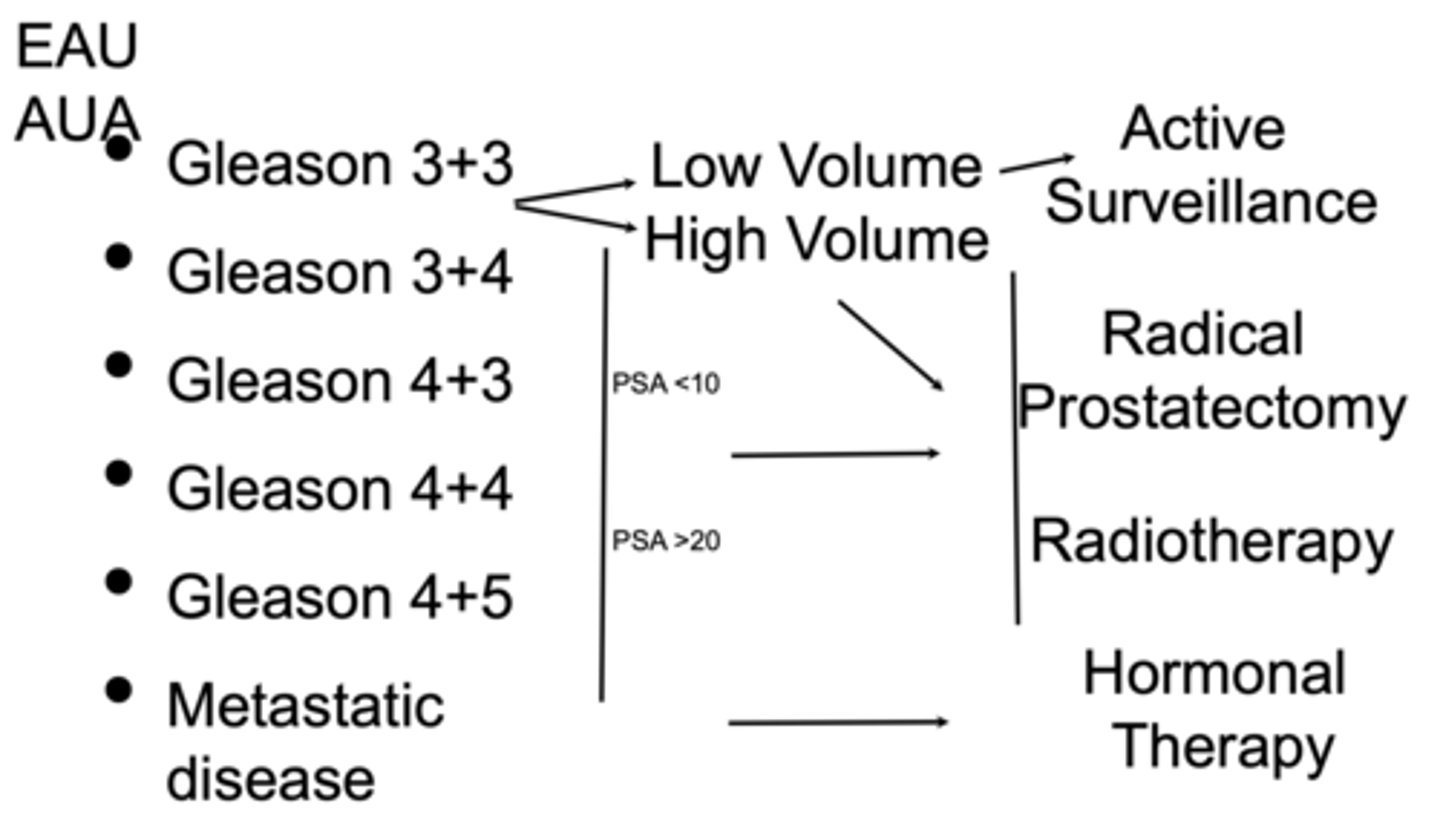
what are the prostate cancer gleason scores?
- gleason 6 = low grade
- gleason 7 (3+4) = intermediate with some poorly formed glands
- gleason 7 (4+3) = mostly poorly formed glands
- gleason 8 = only poorly formed glands, high risk dz
- gleason 9 or 10 = rly bad
which type of hysterectomy leaves the cervix?
partial
what is removed in a radical hysterectomy?
uterus
cervix
upper part of vag
which hysterectomy surgical approach involves resecting the uterus into small pieces?
laparoscopic
which hysterectomy surgical approach involves laparoscopic incisions to separate the uterus and pulling it out through the vagina?
robot-assisted vaginal
which hysterectomy surgical approach is done through the vaginal introitus and dissection starts around the cervix?
transvaginal
which hysterectomy surgical approach is an open procedure through a transverse or midline vertical incision in the lower abdomen?
abdominal
review organ prolapses!
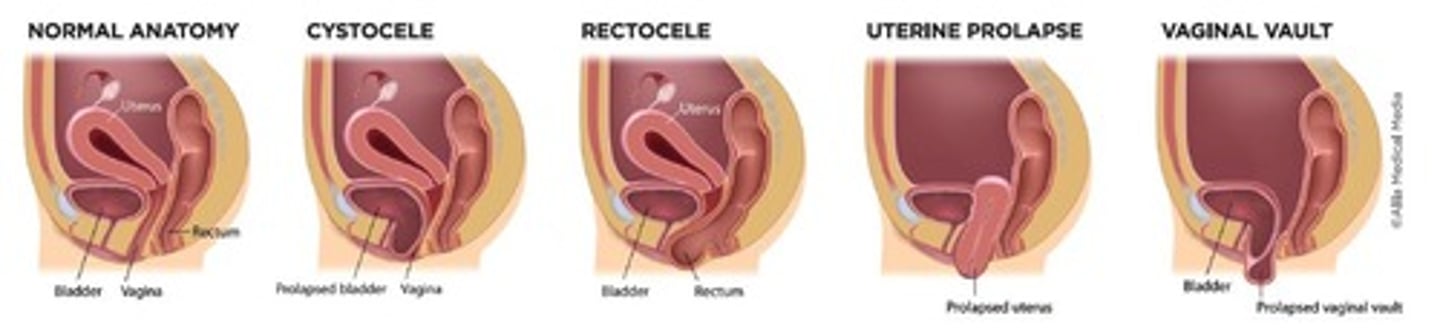
what procedure is used to repair pelvic organ prolapse?
sacrocolpopexy → synthetic mesh attaches pelvic organs to pelvic bones
what is the gold standard for CAD diagnosis?
cardiac catheter
what is the surgical management for ASCVD?
PCI and CABG
what is the diff between AAA and aortic dissection presentation?***
AAA = nontender, pulsatile abd mass
AD = sudden severe tearing chest pain, pulsatile abd mass
at what size does AAA require surgery?**
>5.5 cm
enlarging >0.5 cm in 6 months
enlarging 1 cm in 12 months
symptomatic
what is Leriche syndrome?
claudication of thigh and butt + impotence with decreased femoral pulse
where is the MC location of a DVT?
left iliac→ dx with duplex US
what is the tx for acute ischemic stroke?
IV tPA within 4.5 hrs
what should you do to prevent hypertensive crisis when performing an adrenalectomy for pheochromocytomas?
treat with alpha blockade THEN beta blockade
what is the management for DVTs?
- intermittent sequential compression devices (SCDs)
- early ambulation
- pharm → LMWH, faxtor Xa inhibitors, unfractionated hep
how would you manage chronic venous insufficiency?
- leg elevation, regular exercise, elastic compression stockings
- surgery (not 1st line) → valvuloplasty, sclerotherapy, endovenous thermal ablation
what is the tx for peripheral artery disease?
- manage CV risk factors → stop smoking, control HLD/HTN/DM, weight loss
- exercise rehab
- foot care
- pharm → asa, clopidogrel
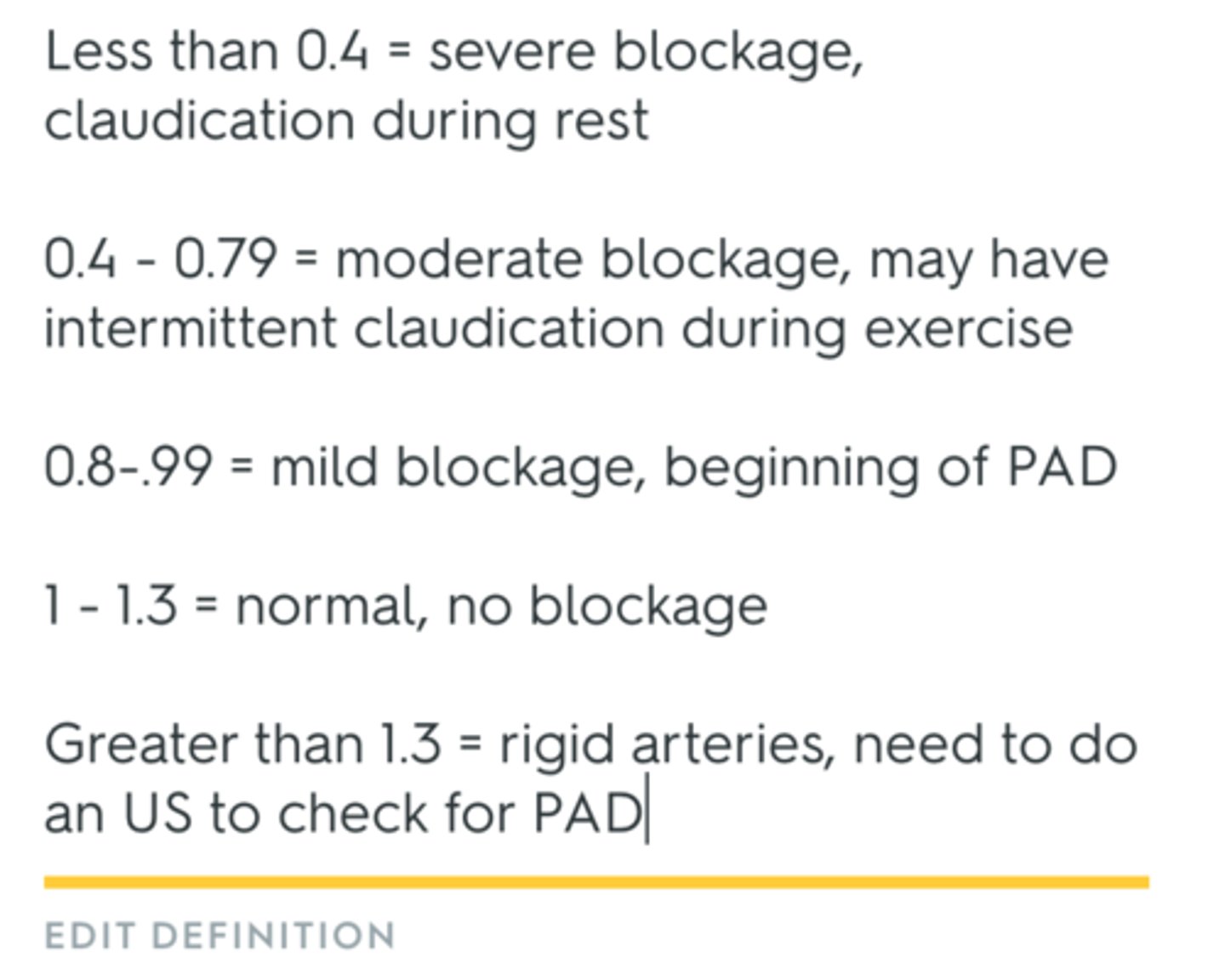
what is the ABI score?***
1-1.4 is normal
< 0.9 abnormal
0.5 is severe
what conditions are RF for PAD?***
- Inc. LDL
- HTN
- smoking
- DM
what meds are used for tx of intermittent claudication?
pentoxifylline
cilosatzol
which type of CABG procedure stops the heart to allow for a "bloodless field"?
on-pump → requires systemic anticoag, and systemic hypothermia
which type of CABG is known as beating heart surgery?
off-pump → sternotomy approach