Pathophysiology II - Exam 4 - Anxiety Disorders 😓
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
what is anxiety?
emotional state typically caused by the perception of real or perceived danger that threatens personal security
- natural adaptive response to threats
- allows for preparation of reaction to environmental changes
if anxiety is a natural state, when do disorders arise?
when the anxiety response becomes excessive, is triggered too frequently, or is a result of irrational fears
- leads to impairment in normal social or occupational functioning
what are the criteria for generalized anxiety disorder (GAD)?
- excessive anxiety/worry (apprehensive expectation) occurring for the majority of days of 6+ months about several events
- difficulty controlling the worry
- anxiety/worry are associated with 3+/6 common Sx (see next card)
- anxiety/worry or physical Sx cause significant distress or impairment in social or occupational functioning
- disturbance is NOT attributed to a substance or medical condition
- disturbance is NOT better explained by another mental disorder
for an anxiety disturbance to meet GAD criteria, the anxiety/worry must be associated with 3+ of what 6 Sx?
- restlessness or feeling keyed up/on edge
- easily fatigued
- difficulty concentrating or mind goes blank
- irritability
- muscle tension
- sleep disturbance
what demographics experience the highest incidence of GAD?
- females
- middle-ages (average age is 35 and declines with age)
- most common in developed countries vs. non-developed countries
how is GAD distributed across ages?
bimodal distribution
- earlier onset when GAD is the primary presentation
- later onset when GAD is the secondary presentation
- waxing and waning course is common
what are the rates of psychiatric comorbidity with GAD?
- comorbidity with MDD is ~50%
- lifetime comorbidity with another psychiatric disease is estimated at 90%
noradrenergic model - fear and anxiety are associated with an increase in ______________ release; what center of the brain modulates this response?
NE
- NS is hypersensitive and overreacts to stimuli
- majority of NE cell bodies in the brain is the locus coeruleus (LC), which mediates the fear response
- meds. that directly inhibit LC firing have demonstrated anxiolytic effects
noradrenergic model - how does chronic noradrenergic overactivity affect receptors in GAD?
chronic overactivity of central NE leads to downregulation of α2 adrenoreceptors in patients with GAD
GABA R model - what is GABA's role in the body with respect to GAD?
major inhibitory NT in the CNS
- regulates 5-HT, NE, and DA
- the specific role of GABA Rs in GAD is not fully understood
GABA R model - what are the 2 major subfamilies of GABA Rs?
GABA-A and GABA-B
- when GABA binds to GABA-A R, neuronal excitability is reduced
- GABA-B is G-protein-coupled and is thought to be involved in the presynaptic inhibition of GABA release
5-HT model - describe how 5-HT may contribute to GAD
5-HT is an inhibitory NT used by neurons in the raphe nuclei of the brainstem
- meds. that inhibit presynaptic 5-HT reuptake have demonstrated anxiolysis
- least-defined pathophysiologic hypothesis
5-HT model - what abnormalities are associated with this hypothesis?
abnormalities may occur...
- through release and uptake at presynaptic autoreceptors (alpha 2)
- at the 5-HT reuptake transport site (SERT)
- at postsynaptic Rs
what is a panic attack?
an abrupt surge of intense fear/discomfort that reaches a peak within minutes
what are the 4 primary criteria for panic disorder (PD)?
- recurrent unexpected panic attacks, during which 4+ characteristic Sx occur (see next card)
- 1+ attacks have been followed by 1 month of 1 or both of the following:
■ constant concern about next attack and its consequences
■ maladaptive change in behavior to avoid next attack
- disturbance is NOT attributed to a substance or medical condition
- disturbance is NOT better explained by another mental disorder
what are the 13 key Sx that meet criteria for PD?
- palpitations, pounding heart, or accelerated heart rate
- sweating
- trembling or shaking
- sensations of SOB or smothering
- feelings of choking
- Chest pain or discomfort
- nausea or abdominal distress
- feeling dizzy, unsteady, light-headed or faint
- chills or heat sensations
- paresthesias (numbness or tingling sensations)
- derealization or depersonalization
- fear of losing control or "going crazy"
- fear of dying
T/F: women are twice as likely to be diagnosed with PD than men
TRUE
- possible hormonal and/or social influences
what are some potential environmental and psychological causes of PD?
- specific environmental triggers (ex: fear of driving over bridges)
- unpredictable or uncontrollable life stressors
- smoking
- temperament/personality type
- learned behaviors
how many PD patients achieve remission with treatment?
~1/3 achieve remission with treatment
- ~1/5 follow an unremitting, chronic course
- remaining ~1/2 experience a waxing/waning course
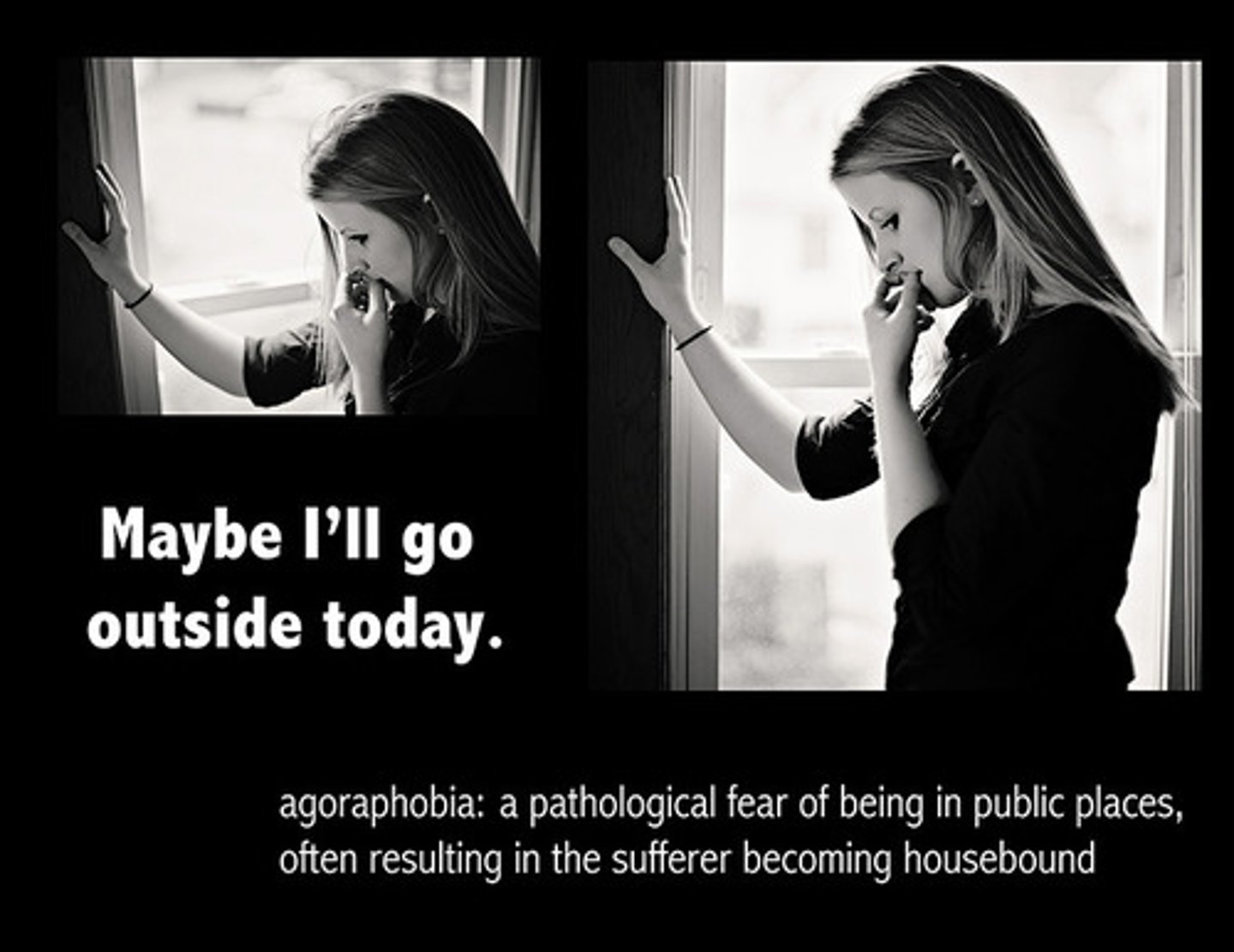
what are some predictors of a more chronic course of PD?
- longer duration of illness
- severe agoraphobia (fear of situations where escape might be difficult)
- excessive sensitivity to physical Sx of anxiety
- comorbid personality, mood, or other anxiety disorder
neurobiological pathophysiology - what changes in brain structure and function are observed in PD patients?
- lower volumes in the amygdala and temporal lobes
- decreased cerebral glucose metabolism in the amygdala, hippocampus, thalamus, and brainstem
neurobiological pathophysiology - what Rs demonstrate reduced activity in Panic Disorder (PD) patients?
reduced BZD R activity
- less sensitive to the effects of BZDs
- lower concentrations of cortical GABA at baseline
- smaller decrease in cortical GABA in response to BZD administration
reduced 5-HT R concentration
- results in pathological anxiety and changes in GABA
psychopathological pathophysiology - what is anxiety sensitivity?
belief that anxiety can cause serious physical, social, or psychological consequences
- predicts the onset of panic attacks, and panic attacks increase anxiety sensitivity
psychopathological pathophysiology - how is panic maintained in patients with PD?
- acute fear develops after the initial panic attack
- conditioned fear towards internal cues of anxiety
- slight changes in bodily function that elicit conditioned exaggerated fear and panic
what are the 10 major criteria for social anxiety disorder (SAD)?
- marked fear/anxiety about 1+ social situations in which the individual is exposed to possible scrutiny by others
- the individual fears that he/she will act in a way or show anxiety symptoms that will be negatively evaluated
- the social situations almost always provoke fear or anxiety
- the social situations are avoided or endured with intense fear or anxiety
- the fear or anxiety is out of proportion to the actual threat posed by the situation and to the sociocultural context
- the fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more
- the fear, anxiety, or avoidance cause clinically significant distress or impairment in social or occupational functioning
- the disturbance is not attributable to the physiological effects of a drug/substance or another medical condition
- the disturbance is not better explained by another psychiatric diagnosis
- if another medical condition is present, the disturbance is clearly unrelated or excessive
what gender and age range has the highest prevalence of SAD?
- females
- more pronounced in adolescence and young adults (mean age of onset is 14-16 yo)
describe the psychiatric comorbidities associated with SAD
~80% of cases have Hx of concurrent anxiety, depression, or substance abuse disorder
- ~20% of patients with SAD also have substance use disorder
T/F: SAD is often caught and treated very early on
FALSE
- a delay in treatment of up to 10 years is common
- without treatment, the course becomes chronic, unremitting, and life-long
- higher levels of depression may predict a greater severity of SAD
what regions of the brain are thought to be affected by SAD?
- amygdala
- orbital frontal regions
- hippocampus
how do DA, 5-HT, and NE play a role in SAD?
NT dysfunction hypothesis
- DA: decreased D2 binding, low levels of DA metabolites
- 5-HT: increased synthesis, overactive signaling
- NE: anxious temperament
what CV, endocrine, and GI disease states are associated with anxiety Sx?
- CV: angina, arrhythmia, CHF, HTN, IHD, MI
- endocrine: Cushing's, DM, hyper-/hypo-thyroidism, hyponatremia, hyper-K+, vitamin B12/folate deficiency
- GI: Chron's IBS, UC, PUD
what neurologic, respiratory, and any other disease states are associated with anxiety Sx?
- neurologic: migraines, seizures, strokes, chronic pain
- respiratory: asthma, COPD, PE, PNA
- other: anemia, CA, lupus, vestibular dysfunction
what meds. are associated with anxiety Sx?
- anticonvulsants: carbamazepine, phenytoin
- antidepressants
- antihypertensives: clonidine, felodipine
- antibiotics: quinolones, isoniazid
- bronchodilators: albuterol, theophylline
- corticosteroids
- dopamine agonists: amantadine, levodopa
- herbals: ginseng, ephedra
- drugs of abuse: ecstasy, cannabis, cocaine
- NSAIDs
- stimulants: amphetamines, methylphenidate, caffeine, nicotine
- levothyroxine
one of the criteria of PTSD is exposure to actual or threatened death, serious injury, or sexual violence in 1 of what 4 ways?
- directly experiencing the traumatic event
- witnessing, in person, the event as it occurs
- learning that the traumatic event occurred to a close family member or friend (in this case, the even must have been accidental OR violent)
- experiencing repeated or extreme exposure to aversive details of traumatic event(s)
one of the criteria of PTSD is the presence of 1+ intrusion Sx associated with the traumatic event after it has occurred; what are these Sx?
- recurrent, involuntary, and intrusive distressing memories
- recurrent distressing dreams related to the event
- dissociative reactions (flashbacks) in which the individual feels or acts as if the event is recurring
- intense or prolonged psychological distress at exposure to internal or external cues associated with the event
- marked physiological reactions to internal or external cues associated with the event
one of the criteria of PTSD is the persistent avoidance of stimuli associated with the event, as evidenced by 1 or both of...?
- avoidance or efforts to avoid distressing memories, thoughts, or feelings closely associated with the traumatic event
- avoidance or efforts to avoid external reminders that arouse distressing memories, thoughts, or feelings closely associated with the event
one of the criteria of PTSD is negative alterations in cognition or mood associated with the event, as evidenced by 2+ of...?
- inability to remember important aspects of the event
- persistent and exaggerated negative beliefs about oneself, others, or the world
- persistent, disoriented cognitions about the cause or consequences of the event leading to inappropriate blame
- persistent negative emotional state
- marked diminished participation in significant activities
- feelings of detachment or estrangement from others
- persistent inability to experience positive emotions
one of the criteria of PTSD is marked alterations in arousal and reactivity associated with the event, as evidenced by 2+ of...?
- irritable behavior and angry outbursts
- reckless or self-destructive behavior
- hyper-vigilance
- exaggerated startled response
- problems with concentration
- sleep disturbance
outside of the mentioned emotional or behavioral criteria for PTSD, what 3 other criteria must be met in terms of duration and disturbance?
- duration of disturbance is >1 month
- disturbance causes clinically significant distress or impairment in social or occupational functioning
- disturbance is NOT attributed to a substance or another medical condition
what are the risk factors for pre-, peri-, and post-traumatic stress disorder?
- pre-traumatic: female, race, FHx, socioeconomic status, preexisting psychological disorder, Hx of SUD
- peri-traumatic: severity of trauma, emotional response, perceived threat to life, dissociation
- post-traumatic: perceived lack of support, dysfunctional social interactions, subsequent life stresses
how soon after trauma can PTSD manifest? what is the typical age of onset and duration of illness?
Sx tend to peak in days-weeks after trauma and can gradually decrease over time
- can onset at any age
- average duration of illness is 3 years in those who receive treatment, but 5 years in those who do not
- 1/3 of patients will develop non-remitting, chronic Sx!
T/F: men are more likely to recover from PTSD than women
TRUE
- likely an evolutionary basis
what are the comorbidities associated with PTSD?
- depression (80%)
- SUD (50%)
- suicide attempts (20%)
describe the neuroendocrine model of PTSD; how do cortisol levels change?
abnormal HPA axis activity and cortisol patterns
- ambient levels of cortisol are LOWER in PTSD patients ("chronic adrenaline exhaustion")
- lower increases of cortisol in immediate aftermath of traumatic events
- lower plasma cortisol levels are associated with greater severity of PTSD Sx
in the neurochemical model of PTSD, the ANS is thought to be hypersensitive and overreactive to stimuli; how do catecholamines, glutamate, and GABA play into this theory?
- uncontrolled catecholamine release affects the formation of memories during the trauma and exacerbates Sx when the patient is exposed to cues
- glutamate signaling dysfunction is linked to poor emotional processing under stress
- abnormalities of GABA inhibition may lead to increased awareness or response to stress, as seen in PTSD
how are α1 and α2 adrenergic postsynaptic Rs linked to PTSD?
involved in startle and sleep responses
- theorized that excessive activation of these Rs leads to sleep related disturbances and nightmares associated with PTSD
- REM sleep (when dreams occur) is altered with the stimulation of α1 Rs
what are obsessions?
intrusive, unwanted, recurrent thoughts, urges, or images that often cause anxiety or distress
- the individual tries to ignore, suppress, or neutralize them with another thought or action
what are compulsions?
repetitive behaviors or mental acts performed in response to an obsession with rigid rules
- done to reduce anxiety or prevent a feared event, though the actions are unrealistic or excessive
what are the 4 main criteria for OCD?
- presence of obsessions, compulsions, or both
- obsessions/compulsions are time-consuming (take >1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
- the obsessive/compulsive Sx are NOT attributable to the physiological effects or a substance or medical condition
- the disturbance is NOT better explained by another mental disorder
what are the risk factors of OCD? what is PANDAS?
- female (adulthood), male (adolescence)
- pediatric autoimmune neuropsychiatric disorder associated with Streptococcal infections (PANDAS) → Abs are produced in response to Strep. infection and can cause onset or exacerbation of OCD
- pregnancy
T/F: patients often present to psychiatrists first with OCD Sx
FALSE
- often present to providers OTHER than psychiatrists first
describe the clinical course of OCD; is onset sudden or gradual?
variable course, but is often life-long
- >50% of patients have sudden onset of Sx, often after a stressful event
- ~50% of treated patients have an incomplete response
- treatment delays of several years are common due to patients masking/hiding Sx
what are the common comorbidities/risks associated with OCD?
- depression (~1/3)
- increased risk of suicide
while the exact pathophysiology of OCD is not completely understood, what are the current beliefs about etiology?
- NTs are thought to be involved (5-HT, DA, glutamate)
- immunological causes may contribute (PANDAS)
- genetic risks (high coincidence rates in twins!)