Emergent Ultrasound Procedures
1/25
Earn XP
Description and Tags
Chapter 19
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
🧰 Sonography = Powerful & efficient
It's a super helpful tool for checking what's wrong with patients in the emergency room — fast and effectively!📦➡🩺 Smaller machines = more flexibility
Thanks to smaller ultrasound equipment and better technology, sonography isn’t just stuck in imaging departments anymore — it’s now common in the ED too!🎓📚 Better training = more use
Changes in medical training for emergency doctors and specialists have helped make ultrasound a key part of emergency care.⏱⚡ Quick decisions = better outcomes
In emergencies, the team has to act fast — sonography helps them figure out what’s wrong quickly and accurately.
🚨 Common Reasons People Visit the ED
🚗💥 Trauma (like car accidents)
❤🔥 Chest pain
Trouble breathing
🩸 Low blood pressure (hypotension)
🤢🤮 Bad nausea & vomiting
😵 Passing out (syncope)
😖 Belly or pelvic pain
🪓 Cuts/lacerations
🦴 Broken bones
🩻 Sonographer’s Role in Emergencies
📞 "Call-back" situations
You might get called in to perform an ultrasound after a quick check by the ED team.🩺 Formal or complete scans
If doctors need a more detailed look, that’s where you come in with your sonography skills!⚠ Critical conditions sonography can help with:
🤕 Internal bleeding from trauma
👶 Ectopic pregnancy
💓 Fluid around the heart (pericardial tamponade)
💥 A ruptured aortic aneurysm
🏥 Sonography in the Emergency Department (ED)
🚑 Blunt abdominal trauma is common
Doctors often have to check if a patient has internal injuries after a hit or blow to the belly (like from a car crash or fall).❓ Hard to tell just by looking
Physical signs (like bruising or pain) aren’t always reliable — especially if the patient:Is unconscious
🧠 Has brain or nerve issues
💊 Is on meds that hide symptoms
🤕 Has other serious injuries
So basically: doctors need extra help (like sonography!) to figure out what’s going on inside the belly because the outside doesn’t always show the full picture. 🧠🔍🩺
Assessment of Abdominal Trauma
🕵♀️ What is DPL?
It’s a test that checks for internal bleeding or organ damage in the belly after blunt trauma.🧍♂ Who gets it?
Used for patients when doctors weren’t sure if they needed surgery (exploratory laparotomy).
🛌 How the Procedure Works
😴 Patient lies flat (supine)
🚽 Bladder is emptied with a catheter
🤢 Stomach is emptied using a nasogastric (NG) tube to avoid pushing on the belly
💉 Skin is numbed (anesthetized)
✂ A small cut is made in the middle or near the belly button
🧵 Doctors go through several layers to reach the peritoneal cavity (inside the belly)
⚠ Risks of DPL
🕒 Takes about 10–15 minutes
⚔ Risk of:
Bowel injury
Bladder puncture
Blood vessel cuts
Wound problems
🚫 Why It’s Not Ideal Today
🙅♂ Too invasive for most patients (especially alert, stable ones)
💨💦 It can mess up future ultrasound or CT results by adding air or fluid into the belly
🧪 Diagnostic Peritoneal Lavage (DPL)
📏 CT = the go-to imaging test
It’s still the gold standard for checking injuries in the abdomen.
🛑 But there are some downsides:
🚚 Patient has to be moved — can’t do it at the bedside
⏳ Takes time, especially if bowel prep is needed
🚫 Not safe for unstable patients (they need faster, on-the-spot options)
When CT is used:
🤔 When doctors really suspect something’s wrong inside
🤷♀ When the exam isn’t clear but the patient seems stable
😣 If there’s ongoing belly pain
📉 When hematocrit drops (sign of internal bleeding)
✅ Why CT is helpful:
🔍 It’s very accurate (high sensitivity & specificity)
💧 Great at spotting fluid collections (like blood or other fluids)
💻 Computed Tomography (CT)
🌍 Started in Europe & Asia in the 1970s
🇺🇸 Came to North America & the UK in the 1990s
(Took a little longer to catch on!)
🔧 Why it became popular:
🧳 Ultrasound machines got smaller & better
= easier to use in emergency settings!
🚑 Why sonography is awesome in emergencies:
⚡ Fast — takes less than 4 minutes
🎯 Accurate
🏃♀ Portable — go anywhere the patient is
😌 Noninvasive — no needles, no surgery!
📉 Downsides:
💨 Air in the belly (subcutaneous or intra-abdominal) makes images harder to see
🍔 Obesity can reduce image quality
🏅 Still a top choice today!
🔁 Can be repeated easily if needed
🩻 Helps image many parts of the body — not just the belly!
🌀 Ultrasound for Blunt Abdominal Trauma (BAT)
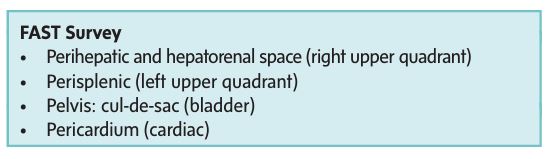
🔍 FAST = quick ultrasound exam
It’s a focused check of the belly, pelvis, and around the heart to look for free fluid (like blood).🏥 Who performs it?
Done in the ED by trained and certified staff (very important for accuracy!).
⚠ Why FAST is so important:
💔 Helps spot life-threatening bleeding (hemorrhage)
🏃♂ Timely diagnosis = fast decisions
Should the patient go to surgery?
Head to the CT scanner?
Go to the angiography suite?
✅ FAST Exam Key Areas:
Pericardium (around the heart)
Abdomen (look for blood or fluid)
🫃 Pelvis (check for internal bleeding)
🚑 FAST Ultrasound Surve:
🌍 FAST Ultrasound Area:
Pericardial sac (around the heart)
💧 Urinary bladder
🍗 Perihepatic area (liver and Morison’s pouch)
🍉 Perisplenic region (spleen area & splenorenal recess)
🍴 Paracolic gutters (sides of the intestines)
🏖 Cul-de-sac (area behind the uterus)
👀 What’s checked?
Visceral organs (organs inside the body) for any irregularities
🔴 Color Doppler may be used to check blood flow if needed
⏱ Why FAST is so Fast and Effective:
⚡ Quick to perform — so it’s perfect for trauma situations
👨⚕ Best when done by trained ultrasound techs who know what they’re doing
📍 Onsite testing = fast decision-making!
🚧 Limitations of FAST:
👨⚕ Operator skill matters — results depend on who’s doing the ultrasound
🏋♀️ Body size can affect image quality
If the patient is larger, it may be harder to see everything clearly
❌ CT is still better for some scans (intraperitoneal & retroperitoneal issues), but it’s not available bedside
🚑 Focused Assessment with Sonography for Trauma (FAST)
⏱ Fast exam!
Takes less than 4 minutes 🕓
Done simultaneously with physical check and patient stabilization
Looks for free fluid or hemoperitoneum (blood in the abdomen)
🩺 What’s Checked During the Ultrasound:
Four quadrants of the abdomen
Check the pericardial sac (around the heart) ❤
Check the cul-de-sac (pelvic area) 🍑
Right and left upper abdomen 🏃♀
Epigastrium (top part of abdomen) 🥞
Retroperitoneal space (behind abdominal organs) 🏙
📋 How the Ultrasound Is Done:
Patient position: Usually supine (lying down) 🛏
Transducer use: Different size transducers based on patient size 🎛
Bladder check: Filled with 200-300 mL sterile saline to help with pelvic scan 💦
Goal: Check for free fluid, organ texture, and heart sac ❤
🔍 What the Ultrasound Looks For:
Free Fluid:
Usually hemoperitoneum (blood) 🩸
Could also be bowel, urine, bile, or ascitic fluid (fluid build-up) 💧
Hypoechoic or Hyperechoic Fluid:
Fluid may look dark or bright with scattered echoes, showing blood inside 🩸
Where Fluid Collects:
Most common area: Subhepatic space (Morison’s pouch) 🧠
Next common area: Pelvic cavity 🍑
⚠ What Happens If Fluid Is Found:
Small fluid collection:
The surgeon might not do immediate surgery 🛑
Instead, they’ll monitor with ultrasound or CT 🩻
Massive fluid collection:
Organs float in the fluid 🌊
🏥 Why It Matters:
Quick and non-invasive — super helpful in emergencies!
Helps doctors decide if surgery is needed 🔪
Gives immediate info on internal bleeding or injury!
🚑 Blunt Trauma Ultrasound Assessment
🩸 Hepatic and Splenic Injury Detection with Ultrasound:
Liver Injuries:
Lacerations or contusions are easily detected with ultrasound.
Appear as heterogeneous (uneven) or hyperechoic (brighter) areas 🩻
Hematomas (blood clots) and localized lacerations:
Initially hypoechoic (darker) due to red blood cells 🩸
Then echogenic as blood clots or coagulates 💥
Eventually, they become anechoic (no echo) as blood breaks down over time
Splenic Injury:
Appears as diffusely heterogeneous parenchyma (liver or spleen tissue).
Both hyperechoic and hypoechoic regions are seen.
🚨 Pitfalls of Abdominal Ultrasound:
Limitations include:
Missed injuries to organs like:
Diaphragm, pancreas, adrenal glands, and some bowel injuries.
Negative ultrasound doesn’t rule out injury; clinical observation or CT is still needed.
🔍 Types of Parenchymal Injuries in Ultrasound:
Intraparenchymal Hemorrhage (Bleeding inside the organ):
Appears as anechoic (dark) regions within the parenchyma (tissue of the liver or spleen) 🩸
Global Parenchymal Injury:
The normal vascular pattern in the liver is absent and shows widespread disruption of liver tissue.
🏥 Impact of Early Diagnosis:
Splenic Injury:
If hemoperitoneum (fluid in the abdomen) is seen and there’s a clear splenic injury, surgery may be performed directly.
Hepatic Injury:
Extensive liver injury may need further investigation (like CT or angiography) before surgery 🔬
🍑 Free Pelvic Fluid in Women:
Women of reproductive age:
Fluid in the cul-de-sac (space in the pelvis) is likely normal (physiologic) and just needs follow-up.
Fluid elsewhere in the abdomen might indicate important injury that requires further evaluation.
🚫 Limitations of Ultrasound in Trauma Assessment:
Obesity can block proper viewing of internal structures.
Subcutaneous emphysema (air under the skin from injuries like pneumothorax) may affect imaging.
Intraperitoneal clots may appear hyperechoic (bright) but sometimes may be isoechoic (same brightness), making it harder to detect.
Contained parenchymal injuries (like liver or spleen) and bowel injuries may not have visible free fluid and could be missed if only ultrasound is used.
🔍 Summary:
Ultrasound is excellent for detecting liver and spleen injuries, but has limitations for identifying injuries to other organs (pancreas, diaphragm, bowel).
Close monitoring or CT is needed in many cases for better clarity and diagnosis.
Parenchymal Injury Overview with Ultrasound 📉
Common complaint in the ER: sharp pain in the right upper abdomen 💥
Can be due to various causes, such as:
Diabetes or peptic ulcer disease 🏥
Heart attack (MI) 💔
Important to consider the patient’s history and do a thorough physical exam 👩⚕
Right Upper Quadrant Pain
Female patients with right upper quadrant pain 😖, fever, tenderness, and elevated white blood cells 🦠: likely acute cholecystitis
Most common cause: Cholelithiasis (gallstones) blocking the cystic duct
Acute Cholecystitis vs. Cholelithiasis
Irregular, thickened gallbladder wall 🏰 (gallbladder looks inflamed)
Positive Murphy sign (pain when pressing on the gallbladder area) ⚠
Sludge (thick, gooey bile) 🛢
Pericholecystic fluid (fluid around the gallbladder) 💦
Dilated gallbladder > 5 cm (bigger than usual) 📏
Sonographic Findings of Acute Cholecystitis
Echogenic foci (bright spots) inside the inflamed gallbladder ✨
Acoustic shadowing (dark shadow behind the stones) 🌑
Make sure the shadow is from the stones, not nearby bowel gas 🍽
If the stones are small, they can get stuck at the gallbladder neck 😵
Cholesterol stones:
Smaller and less echogenic (don’t show up as bright)
Can cause a comet tail artifact (a tail-like appearance) 🚀
Gallstones on Ultrasound
Common Bile Duct (CBD) is easy to spot on ultrasound 🏞
Find the portal vein: The CBD is to the right and anterior (in front) of it 👀
Hepatic artery is in front and slightly to the left of the portal vein 🩸
Normal CBD size: Up to 6 mm 📏
Can increase to 10 mm with age 🧓
Looking for Stones in the CBD:
Check for echogenic foci (bright spots) inside the duct ✨
These stones will cause acoustic shadowing (a dark spot behind them) 🌑
Adjust gain on ultrasound to get a clear view 🔧
Change the patient’s position to avoid interference from bowel gas 🏃♀💨
Biliary Dilation
Pain Location:
Midepigastric pain that radiates to the back 🏥💥
Classic sign of acute pancreatitis 🔥
What Happens in Pancreatitis?
Toxic enzymes leak into the pancreas tissue 🧪💣
This causes inflammation and blockage in the ducts, blood vessels, and fat 🛑
Peripancreatic tissue (around the pancreas) can also become inflamed 💔
Clinical Findings 👩⚕
Fever 🌡
Leukocytosis (high white blood cell count) ⚪
Elevated enzymes in the blood 🩸
Amylase spikes within 24 hours ⏳
Lipase spikes after 72 hours and stays higher longer 🕒
Ultrasound Findings (What We See on the Screen!) 👀
Pancreas looks normal to swollen (edematous) 📏➡📈
It may be hypoechoic (darker) compared to normal tissue 🌑
Irregular borders due to inflammation 🌀
Increased blood flow around the pancreas (shows as more color on Doppler) 💉
Pancreatitis (Epigastric Pain)
Symptoms:
Abdominal pain that radiates to the back 💥➡🦵
Hypotension (low blood pressure) ⬇
Pulsatile abdominal mass (can feel a heartbeat-like pulse in the belly) 💓
What to Look for in the ED? 👩⚕🏥
Sonography helps separate:
Aortic dissection (tear in the aorta) 🚨
Vague abdominal complaints 🩻
Symptoms that might look like kidney stones 💎
If dissection is suspected, CT with contrast is more specific because it shows the whole aorta clearly 💻
Ultrasound Findings 📊🔍
Locate aneurysm near the renal vessels (kidney arteries) 🔄
Aneurysms can extend into these vessels if a dissection happens 🚨
Measure the aorta:
Measure the outside wall-to-wall diameter in two planes:
Transverse (side-to-side) ↔
Longitudinal (top-to-bottom) ⬆⬇
Most aneurysms occur near the umbilicus (belly button) 🌍
Aneurysms can grow in:
Transverse diameter (side-to-side) ↔
Anterior-posterior diameter (front-to-back) ↕
Challenges & Pitfalls 🧐💥
Obesity or bowel gas can block a clear view 🏋♀️💨
Try imaging from lateral abdominal wall (using the liver or spleen as a "window" 🌟)
Positioning: If needed, the patient can be rolled to a decubitus position (on their side) for a better view 🔄
Measurement tip: The transducer should be perpendicular to the vessel to avoid inaccurate sizing 📏
Important Things to Know! ⚠💡
A small aneurysm can still rupture — it’s important to assess carefully ⚡
Free fluid in the belly (intraperitoneal fluid) should be checked for, especially in acute cases 💧
Paraaortic nodes may look like aneurysms but they don’t have blood flow 🚫
Abdominal Aortic Aneurysm (AAA) 🩸💥
What is it?
Fluid builds up in the pericardial sac (the lining around the heart) 🫣💦
How to Detect?
Cardiac ultrasound is used to rule out pericardial effusion or check heart function during emergencies 🚑
Who’s Affected?
Body habitus (how someone’s body is built) and other health conditions can make it harder to see the heart on ultrasound 🏋♂️
Types of Fluid & Appearance 👀
Normal Fluid:
Appears anechoic (black on ultrasound) or hypoechoic (gray) 🖤⚫
Abnormal Fluid:
Fluid with inflammation, cancer, or bleeding can have more complex textures 🩸🦠
Where does the fluid collect?
Fluid usually starts in the lowest part of the heart (depends on gravity) ⬇
Measuring the Effusion 📏
Small effusion (<1 cm):
Can only be seen posteriorly (back side of the heart) 🔙
Moderate effusion (1-2 cm):
Fluid is circumferential (around the heart) 🌍
Large effusion (>2 cm):
Fluid is extensive and may affect heart function 🚨
Check in multiple views:
Parasternal long axis, short axis, apical four chamber, and subcostal views 🔄
Distinguishing from Pleural Effusion 🩺
Pleural effusion (fluid around the lungs) can look similar to pericardial effusion! 🤔
Pericardial effusion is anterior (in front of the aorta) 🫣
Pleural effusion is posterior (behind the aorta) 🫨
Cardiac Tamponade & Other Emergencies ⚠
Cardiac Tamponade:
A severe fluid buildup that compresses the heart and can be life-threatening 💔🚨
Right heart chamber collapse during diastole (when the heart relaxes) is a key sign 😱
What to do?
Doppler to check blood flow changes 🩸
Inferior vena cava (big vein) checked for dilation 🧠
Pulsus tardus:
A slow pulse seen in tamponade cases (heart’s having trouble pumping) 🕒
Trauma & Hemopericardium 🩸🚑
Hemopericardium (blood in the pericardial space) can occur after trauma 🚗💥
Blood will look echogenic (brighter) compared to the heart muscle 🩸🖤
Fatty tissue around the heart might look like effusion, but it’s just fat 🐮🍔
Fast-Forming vs. Slow-Forming Effusions ⏳⚡
Rapidly forming effusion (small) can cause tamponade quickly 🏃♀💨
Large, slow-forming effusion might be tolerated with minimal symptoms 😌
Pericardial Effusion Overview 💧
Definition:
A tear in the aorta's lining (intima) causes blood to flow between the layers of the vessel, creating a false lumen (a blood-filled space) 🩸💔Where does it happen?
70% in the ascending aorta (part closest to the heart) 💓
10-20% in the aortic arch 🌉
20% in the abdominal aorta (lower part of the aorta) 🌾
How it spreads?
Most dissections spread downward to iliac vessels (lower body), but they can also extend upward ⬆⬇
Clinical Symptoms (How It Feels) 🚨
Pain:
Sudden, severe chest pain that feels like tearing 💥
Pain radiates to the arms, neck, or back 💪🦸♀
Other Signs:
Syncope (fainting) in some cases
If the carotid artery is involved, it can cause hemiplegia (paralysis on one side) 🧠🚶♀
Decreased pulses if subclavian or iliac arteries are affected (weak arms/legs) 🙌🦵
Pain Location Clues:
Anterior thorax pain = proximal dissection (close to the heart) 💔
Interscapular (between the shoulder blades) pain = distal dissection (farther from the heart) 💥
Back pain = distal dissection 🦋
Abdominal pain = could indicate visceral artery occlusion (blockage of arteries to organs) 🤕
Sonographic Findings (What We See on Ultrasound) 👀💻
Most common area to see it:
The ascending aorta is where most dissections happen 🚀What do we look for?
Flap: A moving echogenic intimal membrane (the flap) visible in the aorta or iliac arteries 🌊
False lumen: The blood in the false lumen may move freely if both lumens (true and false) are open 💧
What happens if the flap is thick?
The membrane might not move, and the lumen can become thrombosed (clotted) 🩸🛑
Using Color Doppler:
Flow in the false lumen is usually slow or reversed (blood moving in the opposite direction) 🩸🔴
What is Aortic Dissection? ⚡
What’s a pseudodissection?
A blood flow pattern that looks like a dissection but doesn’t have a flap 🙅♂❌
Hypoechoic thrombus (dark clot) forms near the aorta's outer layer 🖤
No intimal flap is seen 👀
Pseudodissection (Fake Dissection!) 😳
A fancy name for kidney or urinary tract stones 💎.
Causes flank pain (side of your body, between ribs and hip) 😣.
🩻 How Doctors Check for Stones
CT scan (noncontrast helical) = best at finding stones 🔍📸.
IVU (Intravenous Urography) also good, but uses dye 🧪.
Ultrasound is used if CT or IVU aren’t safe (like pregnancy 🤰 or allergies 🚫).
💥 Symptoms to Watch For
Renal colic = sharp, wave-like spasms of pain 🌀.
Pain often starts suddenly in the flank 😵.
May spread to lower abdomen, groin, scrotum, or labia 🧭.
Needs strong pain meds sometimes 💊💤.
🧪 Lab Tests
Urinalysis shows blood in urine (85% of the time) 🩸.
No blood? It might be a fully blocked ureter 🚫💧.
Fever, high white blood cells (WBCs) = possible infection 🦠.
🧿 Ultrasound Findings
Stones look like bright (echogenic) spots with dark shadows behind them ⚫✨.
Can see tiny stones, even as small as 0.5 mm!
If the ureter is blocked → shows hydronephrosis (kidney swelling) 🚰🔄.
Gas in the bowels can hide the lower ureter 😑💨.
🎨 Doppler Ultrasound Tricks
Look for "ureteral jets" – tiny spurts of urine into the bladder 🚿.
Use color Doppler: Wait 2–3 mins and jets should appear 💦🌈.
Both right and left ureters should show jets (check both sides!) 👀➡⬅.
Power Doppler is also great for detecting the jets ⚡🔍.
🧍♂ What is Urolithiasis?
During late pregnancy, it’s common for kidneys to look slightly swollen (hydronephrotic) 🫣.
This happens because the growing uterus presses on the ureters 🚼➡🧵.
Right kidney is affected more often because:
It sits lower than the left 👇🏽.
So it gets more pressure from the uterus .
🧪✨ How to Tell If It’s a Problem
Since mild hydronephrosis is normal in pregnancy, how do you check for a stone (obstruction)? 🧐
Use color Doppler to look for ureteral jets (urine flow into the bladder) 🚿🌈.
Seeing the jets = ureters are working ✅ = No blockage!
No jets = possible stone or obstruction 🚫💧.
🤰💧 Hydronephrosis in Pregnancy
Acute appendicitis = inflamed appendix 😖🔥
Caused by blockage in the appendix (often poop, infection, or lymph tissue) 🚫🧻
Leads to swelling, reduced blood flow, and possible bursting (perforation) 💣😬
👧👦 Who Gets It?
Most common surgical emergency in kids age 2+ 🧒👦🧑
Can happen to anyone, any age
🩹💢 Classic Symptoms
Pain in the lower right belly ➡⚡️
Nausea & vomiting 🤢🤮
Fever 🌡
High white blood cells (leukocytosis) 🧪
Rebound tenderness (McBurney's sign) = hurts more when you let go than when pressing 😣👆
🔍💻 Ultrasound Tips
Use a high-frequency linear probe 📡🔎
Be gentle—the area is very tender 👐😖
Apply gradual pressure to move bowel out of the way and see the appendix
🧽🌀 What You’ll See on Ultrasound
Appendix wall > 2 mm thick = likely inflamed 🧱🔥
Target sign on cross-section 🎯 (hypoechoic center = fluid, bright ring = mucosa, dark outer ring = muscle)
No peristalsis and non-compressible (unlike normal bowel) 🚫🌀
If asymmetric wall or fluid nearby → could mean rupture and need to check for abscesses 💧🦠
⚠📍 What is Appendicitis?
Happens when abdominal wall is weak ➡ organs (viscera) push through
Paraumbilical hernia = near the belly button 🎯
More common in women
Inguinal hernia = in the groin area ⚽
More common in men 🧔
🔁 TYPES OF HERNIAS
Reducible ➡ contents can go back in ✅
Incarcerated ➡ contents are stuck 🚫
Strangulated ➡ stuck + blood flow blocked ❌🩸 = emergency!
🧬 CAUSES OF HERNIA
Congenital (born with it) 👶
Weak muscles 🏋♂️❌
High belly pressure (from obesity, pregnancy, ascites, masses) 🧸🤰⚖
Repeated pregnancies or surgeries 🔁🔪
⚠ COMPLICATIONS
Strangulation ➡ cut-off blood flow 🚫🩸
Rupture in severe ascites 💧💥
📸 SONOGRAPHIC FINDINGS
See bowel moving inside the hernia 🌀🩻
Check during Valsalva maneuver (bear down like pushing 💨) 😤
Look for:
Anterior wall defect 💢
Bowel loops inside sac 🔄
Sac gets bigger with Valsalva ➕
Contents can return with gentle push 🤲✅
🔬 WHAT YOU'LL SEE ON SCREEN
Colon = fluid + gas + movement 🌊💨🌀
Omentum and fat = very bright (echogenic) ✨
Use high-frequency linear probe 🎯🔎
Lower gain to see the layers clearly 📉🔍
Use color Doppler to check blood flow in sac 🌈🩸
⚔ INGUINAL HERNIAS
Indirect (🚶♂ follows path of spermatic cord)
Goes through inguinal canal
Enters at deep inguinal ring
Found lateral to inferior epigastric vessels
Usually congenital or injury-related 👶⚠
Direct (📍bulges directly out)
Pushes through weak fascia
Found medial to inferior epigastric vessels
Rarely goes into scrotum ❌🍒
Common in older men 👴
💥 WHAT IS A HERNIA?
😖
Happens often in the middle of the night 🌙🛌
Patients show up at the ER in serious pain 🚑😩
Sonographer's job = find the cause fast! ⚡🔍
🔥 POSSIBLE EMERGENCIES TO LOOK FOR:
Tubo-ovarian abscess (infection-filled sac) 🦠💥
Ruptured ovarian cyst 💧💔
Ectopic pregnancy 👶❌
Ovarian torsion (twisted ovary) 🔄🛑
🩻 SONOGRAPHY MODES
Transabdominal (TA) – bladder full 💦, gives a big picture 🖼
Transvaginal (TV) – bladder empty 🚽, gives close-up detail 🔬
🏰 UTERUS CHECK
Should look smooth and even 🎯
Center line = endometrial canal ➖
Check from fundus to cervix 🔄
Look for:
Fibroids = pain & bleeding 😖🩸
Interstitial pregnancy = near edge of uterus wall 🧱👶 (danger zone!)
Normal pregnancy = sac high in cavity 🎈👶
Fetal heartbeat = use TV ultrasound ❤👶
🌊 CUL-DE-SAC (a fluid trap!)
Small fluid = normal, varies with cycle 🩸📆
Too much fluid = 😱 Could be:
Ruptured ectopic 💥👶
Pelvic inflammatory disease (PID) 🦠🔥
Ascites or trauma 💧⚠
🥚 OVARIES
Best seen with TV ultrasound 🔬
Look for:
Cysts 🎈
Ectopic pregnancy 🚫👶
Masses or enlargement 🔍
Torsion signs = big swollen ovary + low/no blood flow 🩸❌
🧪 FALLOPIAN TUBES
Also best with TV ultrasound 🎯
Originate from the cornua of the uterus 🌱
Watch for:
Hydrosalpinx (fluid-filled tube) 💧🧪
Tubo-ovarian abscess (infected mess) 🦠💥🔥
ACUTE PELVIC PAIN
🥴
Ouch! 😖 Painful and swollen scrotum!
Causes:
Car accident 🚗💥
Sports injury ⚽🏈
Direct hit 🥊
Straddle injury 🚲🚫
🎯 MAIN GOAL OF ULTRASOUND:
Check for rupture! ⚠🩸
If caught early (within 72 hours) 🕒➡ 90% can be saved! 🙌
After 72 hours ➡ only 45% chance 😟
🩸 TRAUMA COMPLICATIONS:
Hydrocele = fluid around testicle 💧
Hematocele = blood around testicle 🩸💥
(can also show up with bad infections like epididymitis or orchitis) 🦠🔥
🔍 SONOGRAPHY FINDINGS FOR RUPTURE:
Weird tissue pattern in the testis 🎨❌
Broken tunica albuginea (protective layer) 🧱
Bumpy or irregular testis shape 🤯
Thickened scrotal wall 📏
Hematocele present 🩸
🧠 These might look like a tumor or abscess, but with trauma history = likely rupture ⚠
🔄 TESTICULAR TORSION – Twisted Emergency!
Caused by abnormal mobility of testis 🕺🌀
Emergency 🚨—needs FAST diagnosis!
Common in teens and young adults 👦
Symptoms = sudden pain + swelling on one side 🌪⚡
🩻 SONOGRAPHY STAGES OF TORSION:
Early (0–6 hrs) ⏰
Testis looks normal at first 😇
After 4–6 hours 🕓
Testis gets swollen + hypoechoic 🥚⬛
Lobes become clear due to swelling 🌀
After 24 hours ⏳
Testis looks heterogeneous (mixed pattern) 🎨
Due to bleeding, infarction, necrosis 😵🩸💀
Epididymal head = enlarged, dull or patchy 🧠
🌈 COLOR DOPPLER MAGIC:
Shows blood flow! 🩸
⚠ No flow on painful side + normal flow on other side = TORSION confirmed! ✅🚨
SCROTAL TRAUMA
🦵–
Common reason: Deep Venous Thrombosis (DVT) 🩸❌
Other possible causes:
Baker's cyst = bulge behind knee that can go down to the calf 🎈🦵
Cellulitis = skin infection 🔥
Abscess = pus pocket 💥
Muscle hematoma = internal bruise 🟣
Fasciitis = inflamed connective tissue ⚠
🧪 2 TYPES OF DVT EVALUATIONS:
Compression Test 🤏
Gently squeeze veins to see if they collapse
Full Ultrasound 💻
Uses gray scale, color Doppler, and spectral Doppler to check flow 🟥⬛🔵
🔍 DVT TYPES:
Acute = recent clot 🆕
Chronic = old clot 🧓
Distal = lower down the leg 👣
Superficial = close to skin (less dangerous) 🧼
😣 PATIENT SYMPTOMS:
Swollen leg 🦵💨
Tender & painful to touch 😖
Use gentle compression during scan to avoid hurting them 🧸
🧠 SONOGRAPHY TIPS:
Use Color Doppler = sees blood flow 🟥🔵
Helps tell veins (slow flow) from arteries (fast flow) 🔄
Avoid false results ❌ by checking flow and compressibility
⚠ CAUTION IN OBESE PATIENTS:
Fat may hide deep veins under big superficial ones 🍔🧻
May lead to missed DVT (false negative!) 👀🙅
🧫 CLOTS – How Do They Look?
Fresh clots = isoechoic or slightly dark (hypoechoic) 🔘
Hard to see on low-end machines 😓💻
💣 HIGH-RISK VEINS for DANGEROUS CLOTS (can travel to lungs 😬):
Common femoral vein 🦵
Superficial femoral vein (yes, it’s deep!) 🚫🌊
Popliteal vein (behind the knee) 🎯
❗The deep femoral vein = usually safe from emboli = not always checked ❌
🩻 HOW TO DO THE EXAM:
Use a high-frequency linear probe 📡
Apply pressure right over the vein
Normal = walls touch completely 🤝
Abnormal = vein won’t compress 😵🛑
❗LOOK OUT: LYMPH NODES
Sometimes confused with clots 😬
Enlarged nodes = dark with a bright center 🌓
Do not compress — different from vein clots 🚷
🧭 CHECK BEYOND THE LEG:
Look at IVC and iliac veins too! 🛣
These may be the source of clots causing pain/swelling ⚠🩸
EXTREMITY SWELLING & PAIN
🩺 Emergency Ultrasound Basics (FAST & More)
🧪 DPL (Diagnostic Peritoneal Lavage) used to be the go-to method for checking abdominal trauma — now it's mostly replaced.
🧍♂➡🧍♀ FAST scan is the new superhero! It's a quick ultrasound used right in the ER to check for internal bleeding.
FAST scan checks the:
❤ Pericardium (around the heart)
🍔 Perihepatic space (near the liver, like Morison’s pouch)
🍇 Perisplenic space (near the spleen)
🚽 Bladder
🌊 Paracolic gutters & cul-de-sac (fluid check zones!)
💥 Trauma & Pain Detection with Ultrasound
💔 Liver injuries (lacerations or bruises) are easier to find than injuries to other organs.
⚠ BUT, ultrasound might miss injuries to:
🫃 Diaphragm
🥞 Pancreas
☄ Adrenal glands
🥣 Some bowel issues
⚡ Pain Locations & What They Might Mean
🔥 RUQ (Right Upper Quadrant) pain = possible gallbladder issues
🔙 Midepigastric pain radiating to the back = classic acute pancreatitis
💣 Aneurysms & Dissections
💥 Aneurysms often show up at the belly button level (🩻 where the aorta splits into iliac arteries)
They can grow both sideways and front to back!
🪓 Aortic Dissection = layers of the aorta split apart = emergency!
Happens in 3 spots:
At the root of the aorta 🌱 (can spread everywhere!)
Near the left subclavian artery 💪
Just the ascending aorta ⬆
😖 Feels like sharp, tearing chest pain that can go to the arms, neck, or back.
😬 Other Common Emergencies
💦 Flank pain = could be kidney stones (urolithiasis)
🍽 Appendicitis = blocked appendix → inflammation → pain → often surgery
Most common emergency surgery in kids over 2⃣!
🧱 Other Causes of Abdominal Pain
🧷 Hernias = rare but can cause blockage and pain
💃 Pelvic pain in women could mean:
🦠 Tubo-ovarian abscess
💣 Ruptured cyst
🚨 Ectopic pregnancy
🔄 Ovarian torsion (twisting — urgent!)
🩳 Scrotal trauma = may lead to:
💧 Hydrocele (fluid)
🩸 Hematocele (blood)
⚠ Testicular torsion = spermatic cord twist = emergency surgery needed ASAP!
🦵 Swelling & Pain in the Limbs
🩻 Can be due to venous issues (acute, chronic, distal, or superficial)
Other possible causes:
🥣 Baker cyst (behind the knee)
🔥 Cellulitis
💥 Abscess
🩹 Muscle hematoma
🧱 Fasciitis (infection of connective tissue)
KEY PEARLS