Vet Surgery Mega
1/741
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
742 Terms
LC - Stifle Disease I
Outside
Inside
Inside
Collateral ligaments are (inside/outside) of the joint
Cruciate ligaments are (inside/outside) of the joint
Menisci are (inside/outside) of the joint

Cranial cruciate ligament disease
What is the NUMBER ONE cause of pelvic limb lameness in dogs?
Orthopedic exam
What is the best way to diagnose cranial cruciate ligament disease (and the one it is done most frequently)?
A. Radiographs
B. CT scan
C. Orthopedic exam
D. Exploratory leg surgery
Limits cranial tibial translation, hyperextension, and internal rotation
What are the 3 roles of the cranial cruciate ligament?
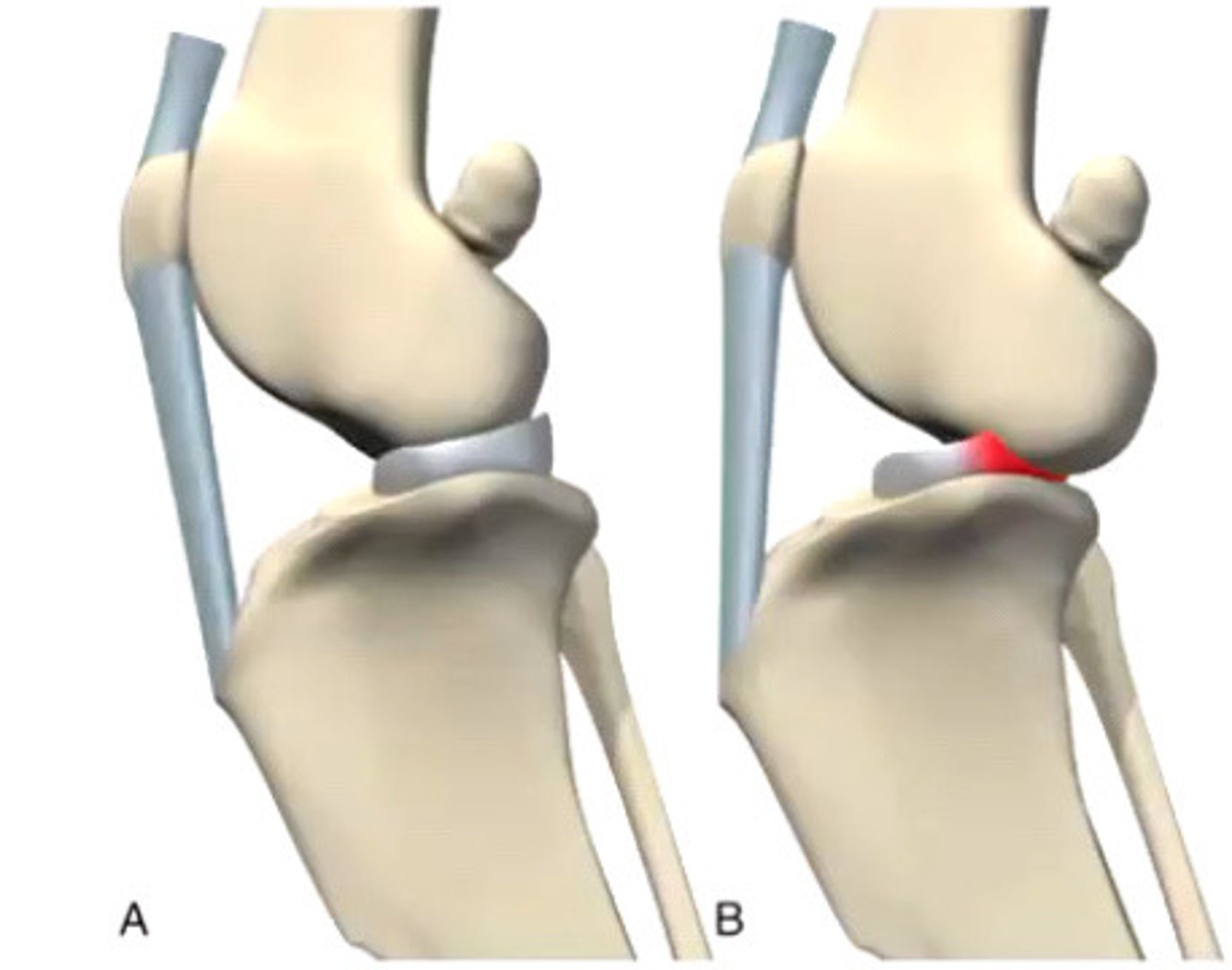
CCL disease; Positive sit test (doesn't want to flex stifle)
What disease is represented by this stance here? What is this test called?

Assess lameness and stance (see positive sit test)
Assess muscle mass
Feel for medial buttress and stifle joint effusion
Stifle manipulation/cranial drawer/tibial compression test
What are the 4 steps to an orthopedic exam for CCL disease?
Stand behind dog, cup hands on each side (as high as you can) and compare to the other side
How do we assess muscle mass for CCL disease?

Medial buttress
________________________ is a bump of bone along the medial aspect of the stifle that you feel in a very chronic CCL diseased dogs

Stifle joint effusion
_____________________ is one of the earliest signs and is very specific for CCL disease
Stand behind dog, try to grab patella tendons; if cannot feel tendon well, has effusion (feel with patella and tibial tuberosity is, between them should feel tendons)
How do you assess for stile joint effusion?

Behind dog
Where should you stand when assessing for muscle mass, medial buttress, and stifle joint effusion with CCL diseased dogs?
A. In front of dog
B. Behind dog
C. To the side of the dog
D. Underneath the dog
Hyperextension (+/- flexion and extension)
Crepitus (if OA), and click (indicative of meniscal injury)
Stifle manipulation is something we do on orthopedic exams to confirm CCL disease after getting positive tests for muscle mass, atrophy, positive medial buttress and stifle effusion.
Do we feel pain most on flexion/extension/hyperextension/hyperflexion?
What else are you feeling for?
Cranial drawer
Which test is most commonly used to diagnose CCL disease?
A. Ortolani
B. Cranial drawer
C. Campbell
D. Withdrawal reflex
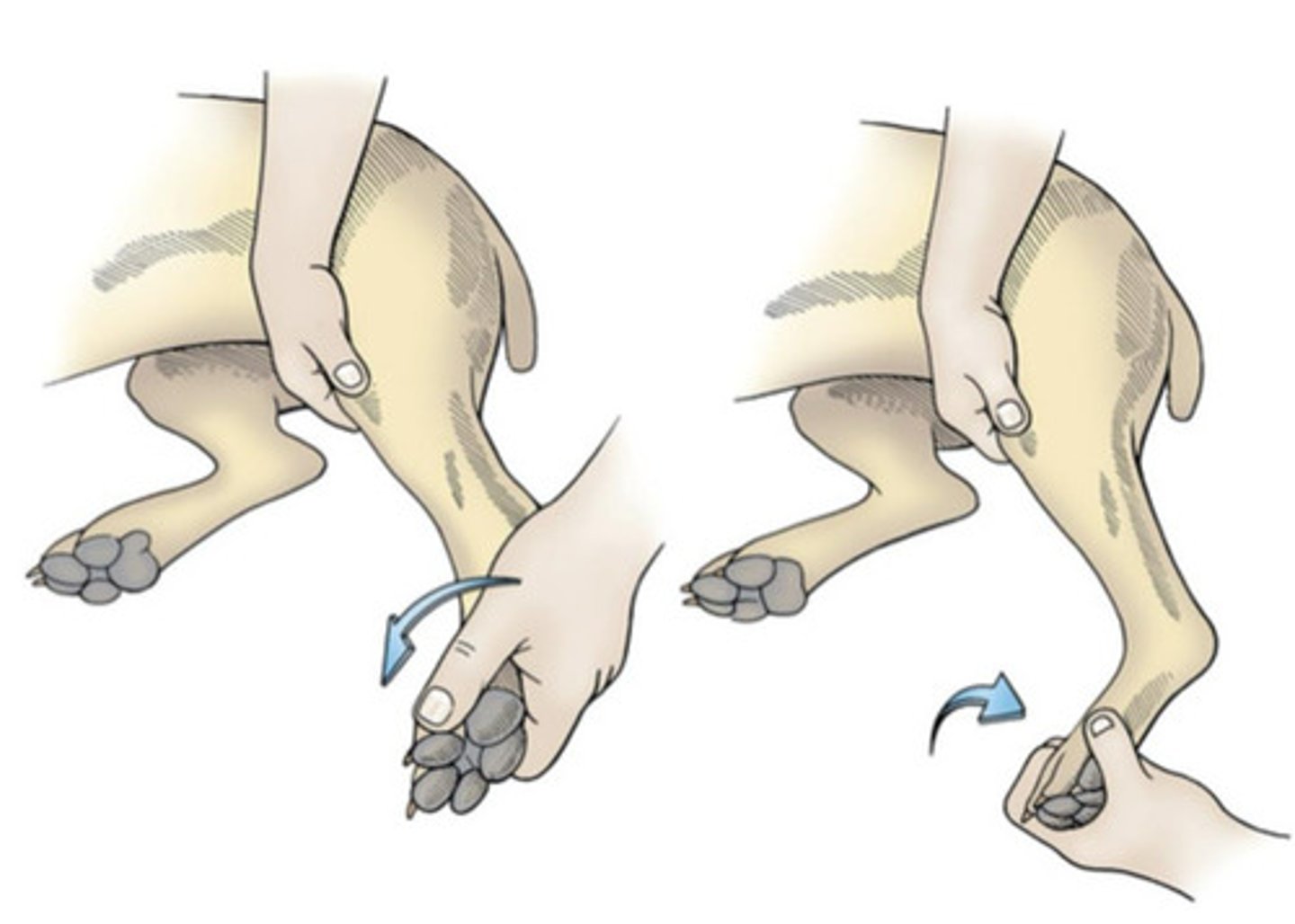
ON ADULTS, one hand on femur, one on patella, move bottom hand back and forth, will move if CCLR (if normal, should NOT move) (exception: up to 6mo will have some movement but not as much) may need sedation
Cranial drawer test is used for diagnosing CCL disease. How do you do it?

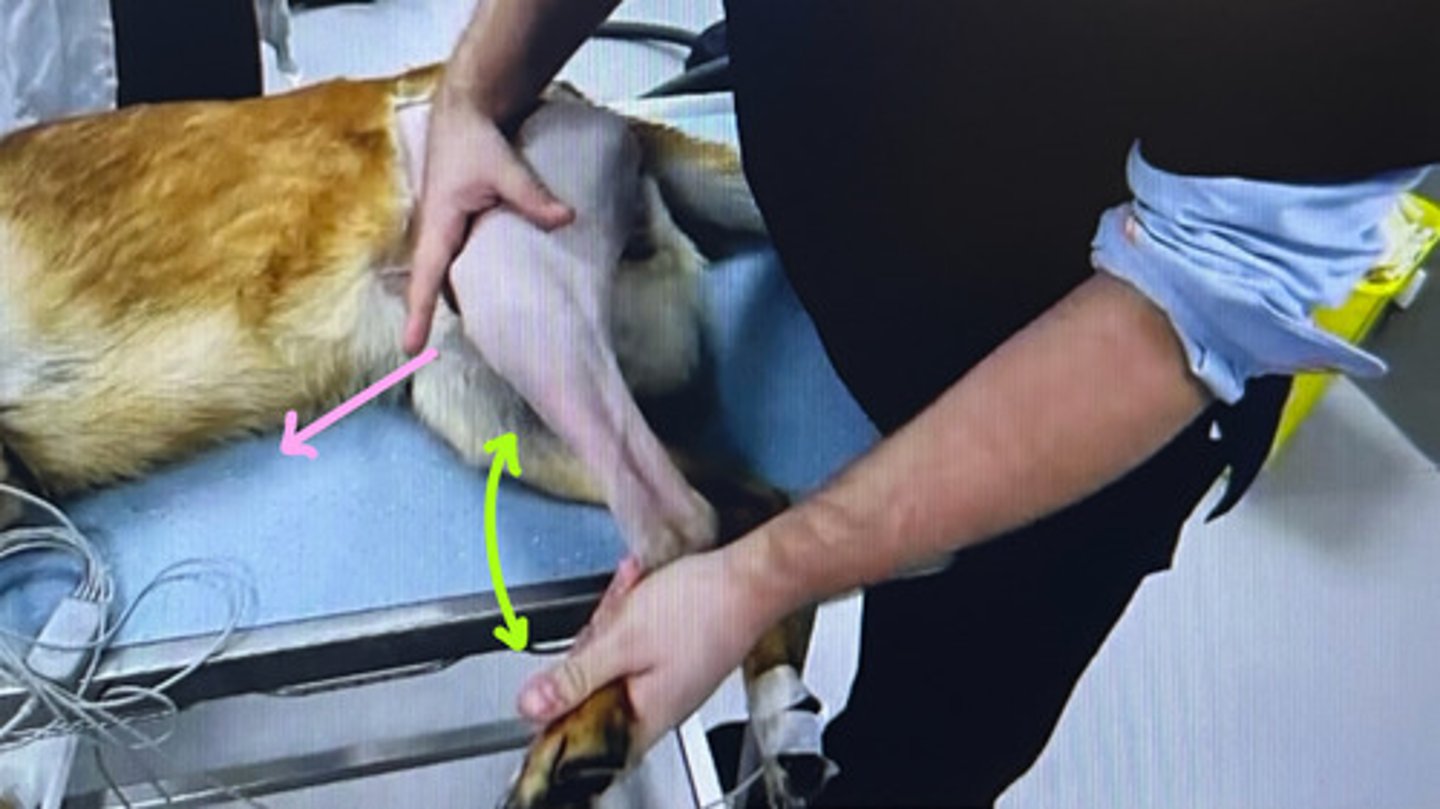
Hand on tibia, flex tarsus, tibia will move forward if CCLR (shouldn't move forward if normal) usually don't need sedation
Tibial compression test is used for diagnosing CCL disease. How do you do it?
Rad/CT/MRI
If you have a confusing cranial drawer test/tibial compression test, and you think there still could be a CCLR, what can you do for further diagnostics?
Loss of triangular fat pad or extension of caudal pouch (stifle effusion) or signs of OA, or see luxation (sesamoid moved down)
What are radiographic signs of CCL disease?

Trochlear groove, apex of patella, cr and cd aspects of tibia plateau, and around fabella
Most common places for OA with CCL disease?
Skeletally immature animals (bc fibers are stronger than bone)
Reattach if possible/early enough, if chronic proximal tibial epiphysiodesis (screw cranially to stop growth, will be unstable for a bit) or tibial osteotomies
Avulsion (not a full tear) of cranial cruciate ligament (dz of CCL) occurs in what kind of animals?
How do we treat it?

Cats
CCL overloaded
Pain, joint effusion, VERY acute (won't have ostephytes)
Acute traumatic rupture of CCL is rare but it happens!
Typical species/breed this occurs in?
Why does it occur?
Clinical signs?

Middle aged, large breed (esp if overweight)
Varied degree of lameness (slowly degenerating), osteophytes present
Progressive degeneration of CCL is the most common presentation of CCL disease
Typical signalment?
Signs?
55
With progressive degeneration of CCL, many are bilateral at presentation. If not bilateral yet, _____% WILL develop contralateral rupture within 2 years!
False, amputate!!
T/F: If owners cannot afford to fix the CCLR, euthanasia is usually indicated
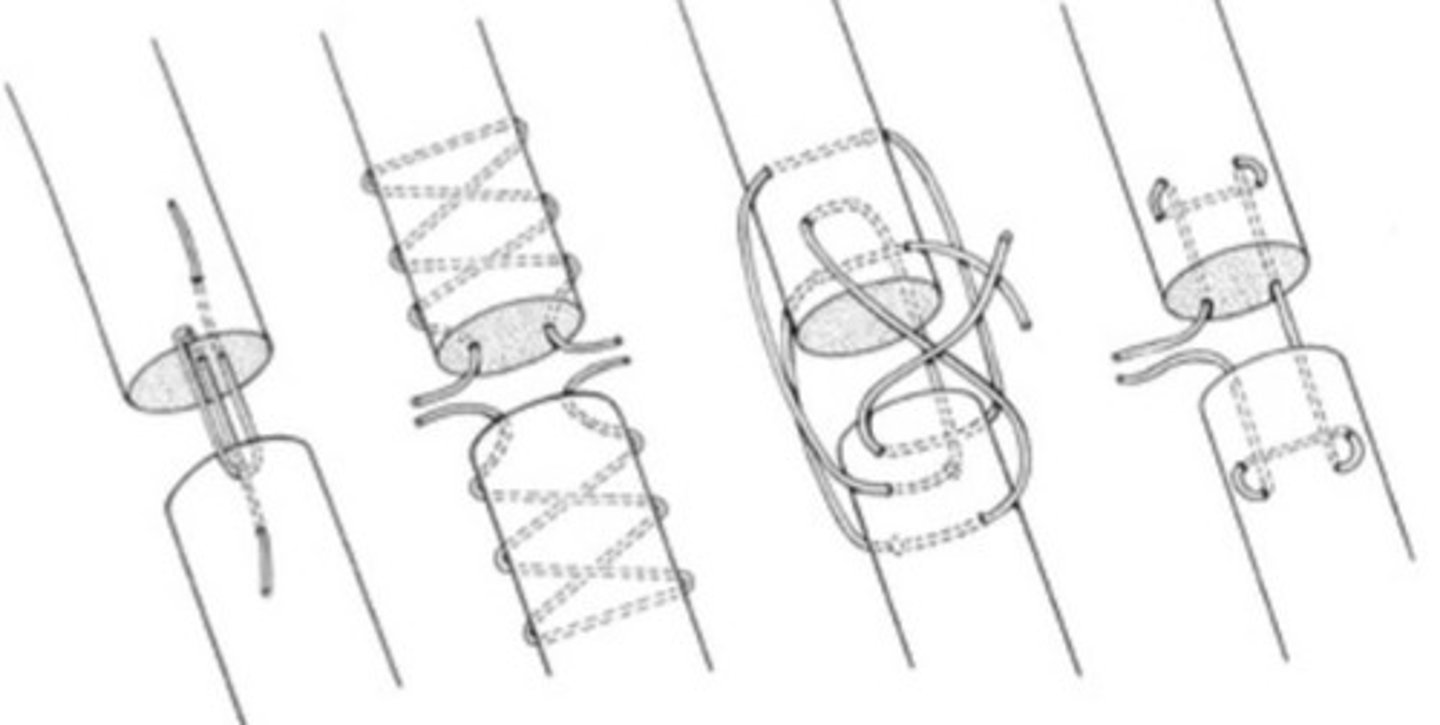
Tissue to mimic CCL (autogenous, allograft, synthetic); Never really (not really effective, outdated)
What is an INTRACAPSULAR procedure to treat acute CCL rupture and progressive degeneration of CCL? When would this be indicated?
Smaller breeds only
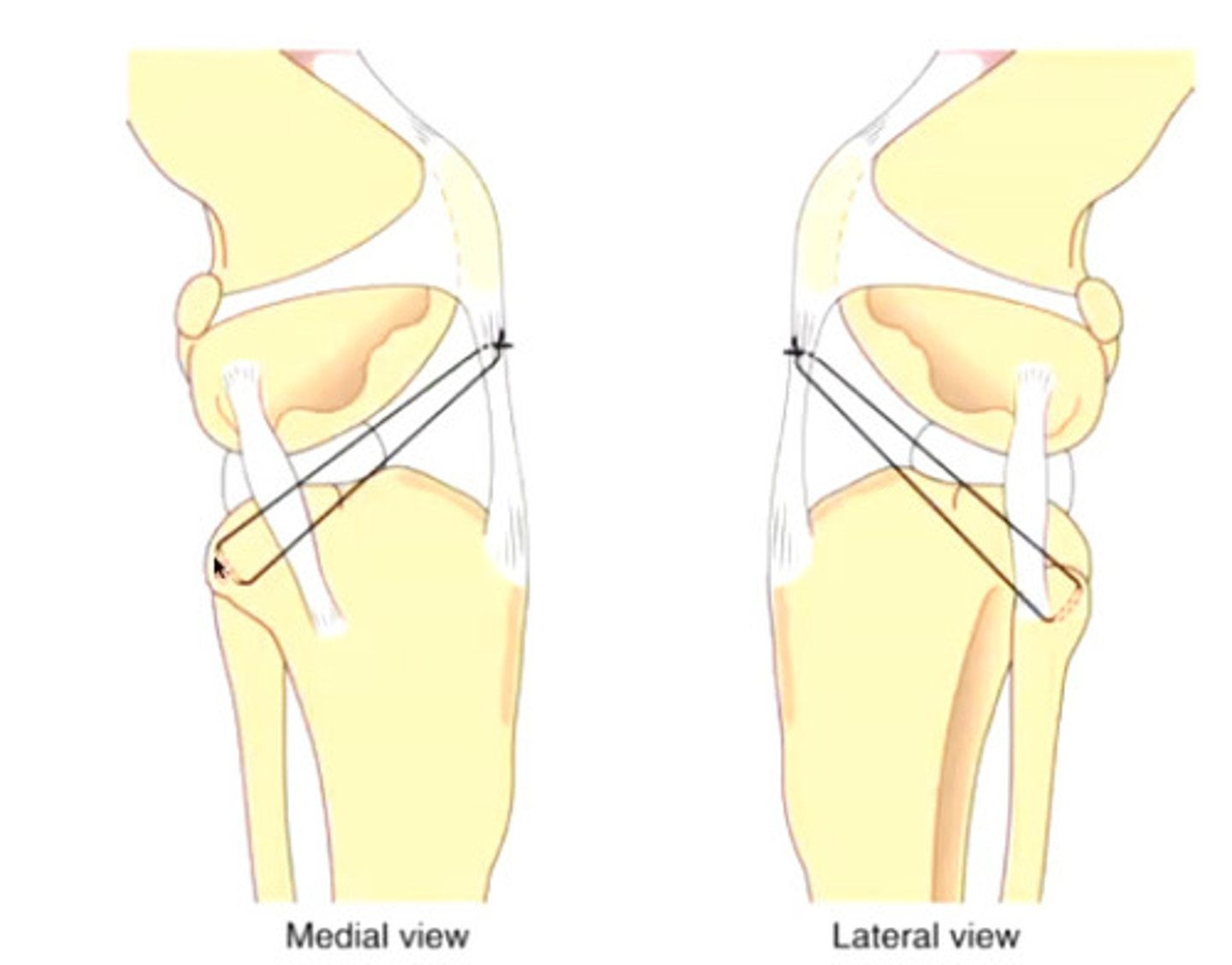
Use heavy non-absorbable suture to hold stifle stable long enough for fusion to occur (want stability, but not too tight that ROM is reduced)
80% satisfactory; long rehab and decreased function
Lateral fabellar suture technique (extracapsular procedure for CCL rupture/degen)
What signalment is this most successful in?
How is it done?
How successful is it? (%) How well do they do?

Modify stifle so joint is stable without action of CCL
Tibial osteotomies like TPLO, TTA, CCWO, TTO, MMT, PTWO (and many more different names) ALL share one objective:
Pros: faster recovery, greater efficacy (esp for big dogs), reduced OA
Cons: complex surgery, more severe complications, expensive
Pros and cons to tibial osteotomies (like TPLO) for CCL rupture/degen?
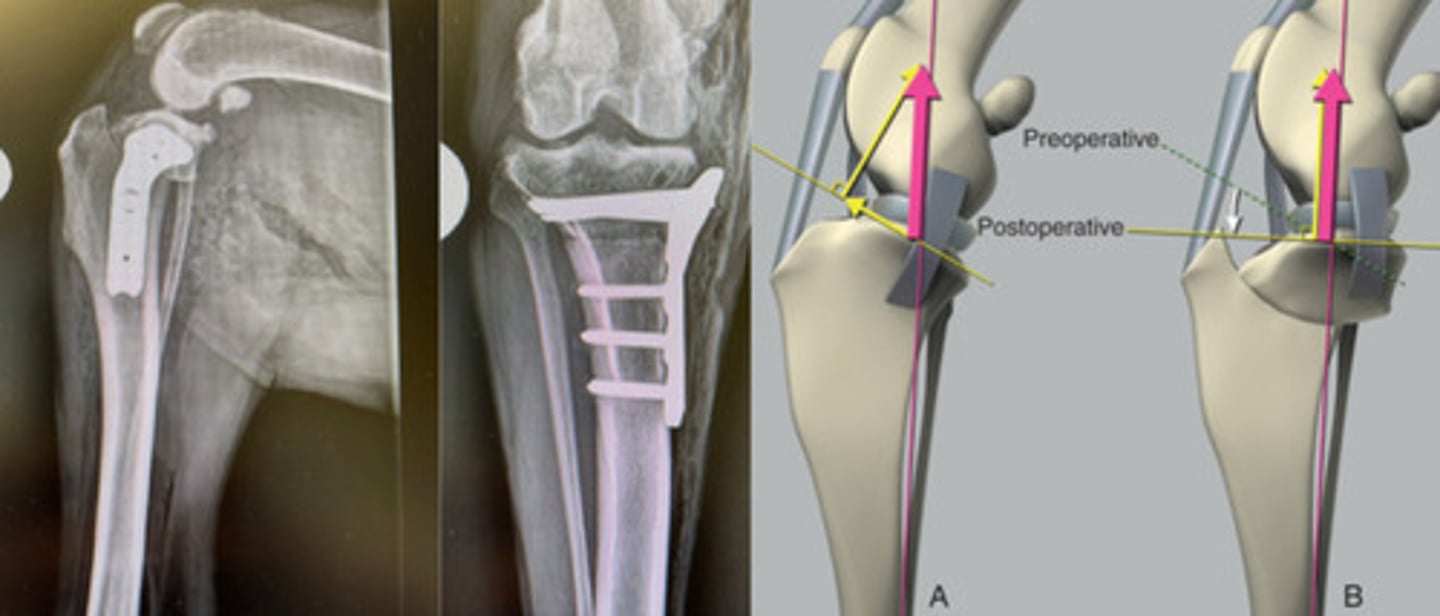
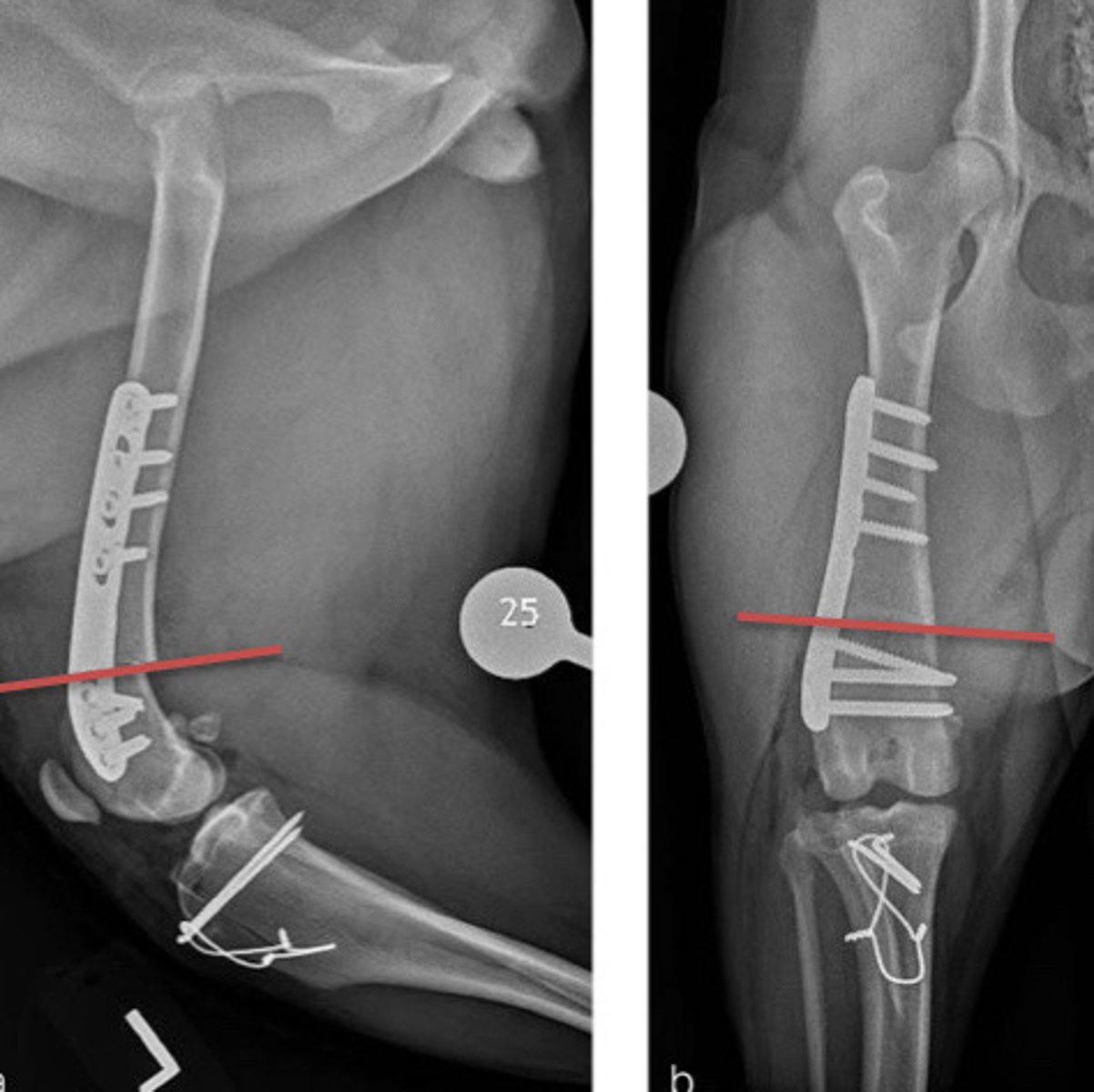
To get rid of cranial tibial crest to stabilize (semicircular osteotomy with 5 degree rotation of fragment)
What is the goal of a TPLO?
Extra; small; 80
Extra; large; 95
Lateral fabellar suture techniques are (intra/extra)capsular procedures more indicated in (small/large) breed dogs and have ______% positive outcomes
Tibial osteotomies are are (intra/extra)capsular procedures more indicated in (small/large) breed dogs and have ______% positive outcomess
LC - Stifle Disease II
Caudal drawal sign (hard to assess)
None in small/inactive dogs; Suture patella ligament to head of fibula for large/performance dogs (backwards lateral fabella suture)
Caudal cruciate ligament ruptures are not frequently seen
Dx?
Tx?
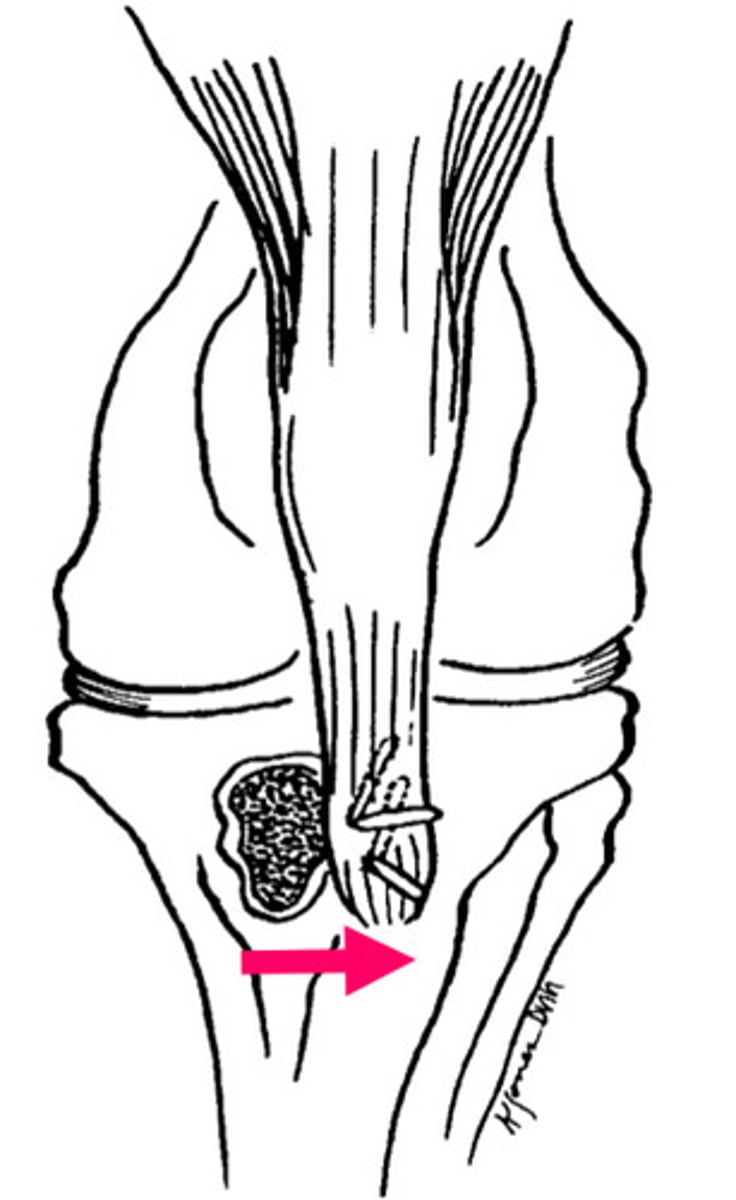
Caudal body of medial meniscus (bucket handle tear)
CCL disease (medial femoral condyle presses on meniscus)
#1 location for meniscal injuries?
Between 20-75% of meniscal injuries are associated with what other injury?
Make patella tendon perpendicular to level of tibial plateau (gets rid of thrust)
What is the goal of a TTA?

Total or partial* meniscectomy (remove damaged part) or Meniscal release (transect meniscotibial ligament OR midbody) (but sometimes just resting is best)
OA
Although overall controversial and we don't know what is best, what are the two treatments for meniscal injuries? Both of these treatments can lead to what?

Small breeds
Intermittent skipping
CCLR
Patellar luxation
Typical signalment?
Signs?
If a dog gets acutely a lot worse, what do you think is going on?

True
T/F: Regardless of CCL disease repair technique, DJD will advance
True (most associated with CCL disease)
T/F: Isolated meniscal injuries are really rare in dogs
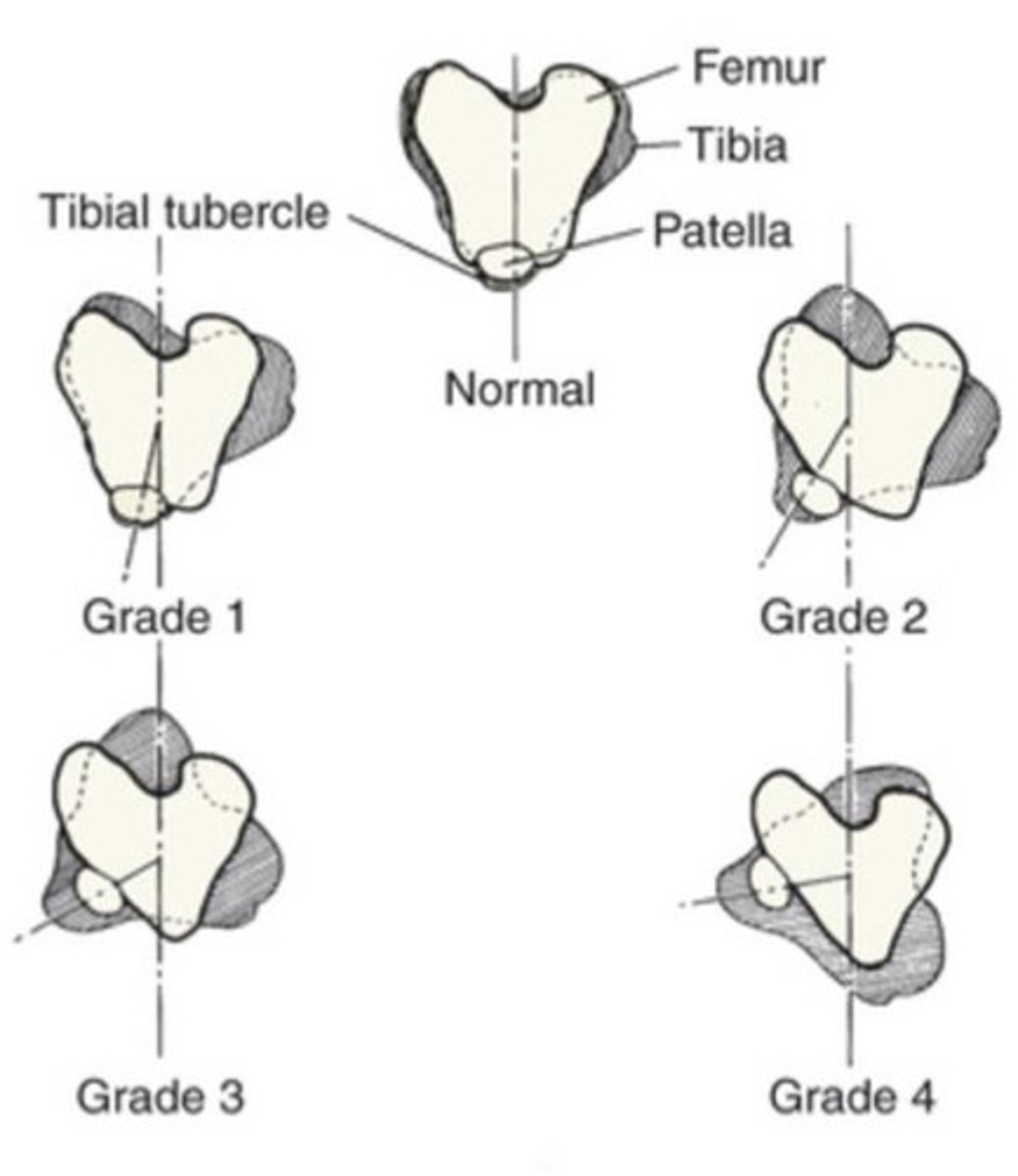
I: usually in, pops back in when luxated
II: usually in, stays out when luxated
III: usually out, pops back out quickly
IV: always out, can't be reduced
DESCRIBE GRADES I-IV OF PATELLAR LUXATION
Medial (larger dogs can get lateral, but medial still most common)
CCLR
With patellar luxation, is medial or lateral luxation more common?
Can predispose to what issue?
Manipulation (flex/extend/rotate to try and illicit a luxation)
Feel for depth of groove
Quadriceps mechanism
What things on physical exam can be done to assess for a patellar luxation?
Patellar luxation
What's going on with this patient?

False, most all are developmental, traumatic rare (if dog doesn't present til years later with issue, likely had it since birth. Investigate why it is an isue now. CLLR? Gained weight?)
T/F: Patellar luxation's that present after 1-2yo are not developmental disorders
Medial displacement of tibial tuberosity, shallow trochlear groove, medial displacement of quadriceps, deformities of femur
What are some deformities associated with patellar luxation?
Grade I: conservative, if lame reevaluate
Grade II: depends on lameness
Grade III-IV: surgical, early management
How do we treat grades I-IV patellar luxation (in adults, juveniles are different and on a different flashcard)
2 stages: Do soft tissue reconstruction techniques first (i.e. trochlear chondroplasty), then once skeletally mature if still having issues do bone reconstruction techniques (DON'T WAIT, manage early!)
How do we treat patellar luxation in juvenile patients? (It's different than adults!)
Long digital extensor tendon
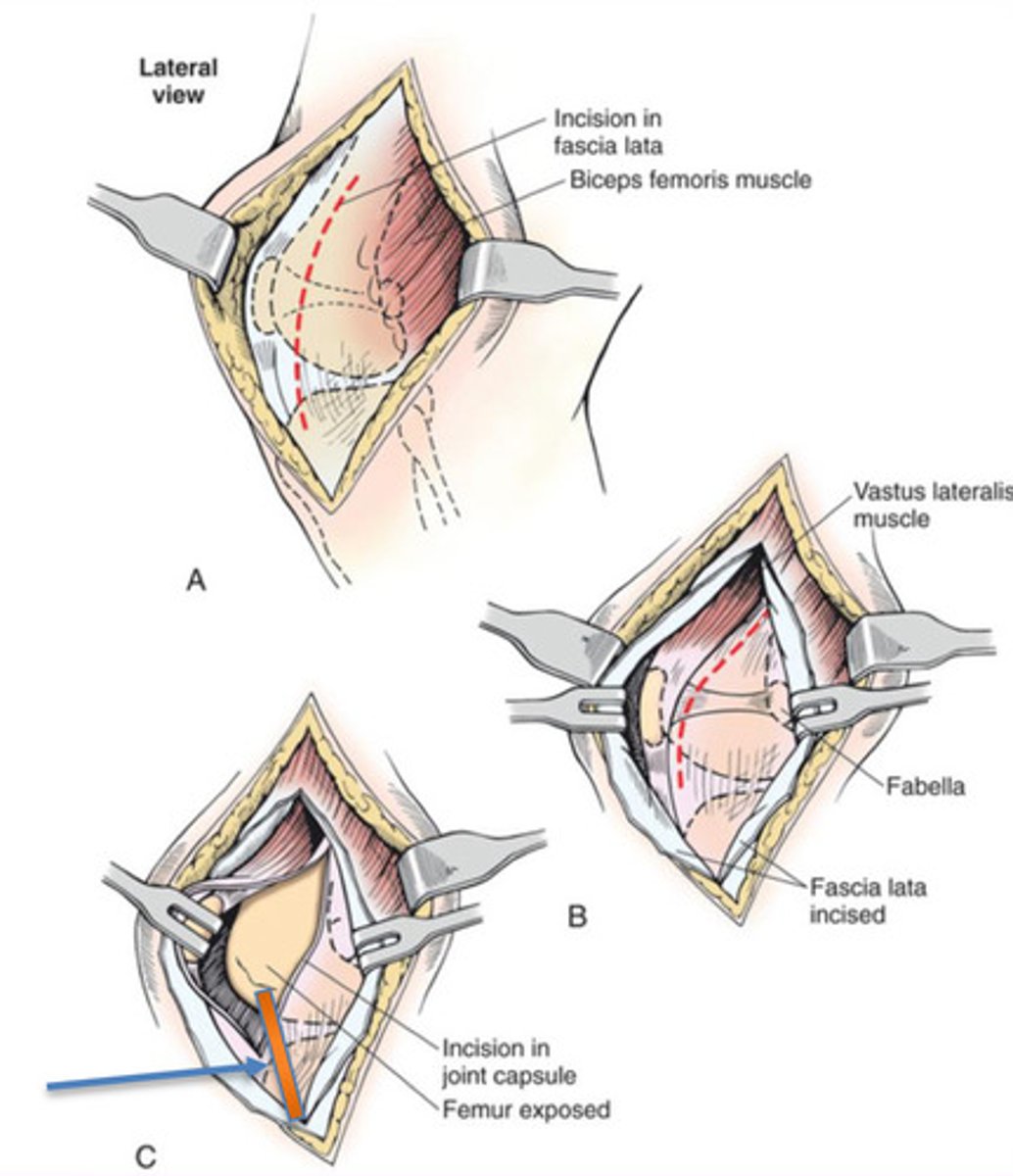
When doing a lateral approach to the stifle when repairing patellar luxations, what structure do we need to be aware of in order to avoid damaging it?
Align extensor mechanism, stabilize the patellar in trochlea (but treatment is individualized, everyone different)
What are our goals with patellar luxation management?
Remove wedge or bloc (bloc better), deepen groove, place fragment back to accomodate patella
Wedge and bloc recession trochleoplasty for patellar luxation treatment - How do you do it?

Lateral approach to the stifle
Trochlear groove, extensor mechanism, ST balance
Stifle joint exploration
What approach do you use?
What are the 3 steps/things you evaluate? (List them in order)
For first step in dogs less than 6mo (can't do in older dogs bc cartilage won't separate from bone); Make cartilage flap, deepen subchondral bone
Trochlear chondroplasty for patellar luxation treatment - When do you do it? How do you do it?

To deepen trochlear groove so 50% of patella protrudes above trochlear ridges
Wedge/block, abrasion, trochlear
Trochleoplasty is a treatment option for patellar luxation
What is the goal of it?
What are the 3 techniques?
Abrasion trochleoplasty (removes all the articular cartilage, bad! We want to preserve the cartilage)
All of these are treatments for patellar luxation. Which is NOT a good option?
A. Wedge recession trochleoplasty
B. Bloc recession trochleoplasty
C. Abrasion trochleoplasty
D. Trochlear condroplasty
Osteotomy, leave distal periosteal attachment (don't cut all the way if possible), transposition enough, fixation with pins in proximal tibia (+/- tension band wire if traction/large breeds)
Tibial tuberosity transposition for patellar luxation treatment - How do you do it?
Tibial tuberosity transposition; Dorsal
____________________________________ is the most important part of fixing a patellar luxation. Do in all adults!! It is easiest to do in (dorsal/lateral) recumbency.
To relieve tension
Corrective osteotomies
What is the purpose of doing soft tissue repairs with patellar luxations?
What is an example of something we can do?
False, never a primary repair
T/F: Soft tissue reconstruction is the primary repair for patellar luxation
True
T/F: Soft tissue repairs with patellar luxations are needed for release of tension
I-III good, IV fair (60% of time patella will stay in); DJD will progress with all of these though
Prognosis for patellar luxations grades I-IV?
Long digital extensor tendon avulsion/luxation
Avulsion of origin of gastrocnemius
Patellar fracture
Patellar tendon injury
OCD
Collateral ligament injuries
Name 6 other things that can damage the patella that are not patellar luxations?
Patella doesn't fit, have to do a parial parasagittal patellctomy (remove abaxial sides of patella)
We can do just a bloc recession by itself in dogs, why can't we in cats? What else do we need to do?

LC - Muscles and Tendons
False, often misses muscles and tendon lesions
T/F: No radiographic lesion means there is no lesion
Muscle injury with variable degree of hemorrhage and fiber rupture
External trauma
What is a contusion?
What are they always caused by?
Longitudinal stretching or tearing of muscle fibers (graded I-IV)
By overstretching or overuse
What is strain/elongation?
What are they caused by?
Depends on severity, severe ones associated with fracture
Rads (to look for fracture/FB), US is the best, MRI
High CK will tell you muscle is damaged (don't know how much tho), myoglobinuria means SEVERE damage
Contusions and strains
Clinical signs?
Dx?
Is bloodwork helpful?
Sarcolemmal cells survive and endomysial sheath is not destroyed
Will get fibrous interposition (scarring)
In mild cases of contusions and strains, myofibrils can regenerate if these 2 conditions are met:
What if they are not met?
Rest most important! (3+ weeks)
NSAIDs (for 3-4d for inflam)
Hot compress if within first 24hr of injury for 10min 3x daily, switch to cold compress after 24hr
How do we treat contusions and strains?
Damage to msucle/nerves due to compression
Increased pressure causes bleeding into muscle compartment
Incision into epimysium (either while in surgery or after or if emergent setting can aspirate out with needle/syringe)
What is compartment syndrome?
Why does it occur?
How can you fix it?

Blunt penetration
Near carpus/tarsus (lower and less coverage)
Once stable, rads to exclude FB or fracture
Lacerations
Causes?
Can affect any muscle-tendon unit, but where commonly?
Dx?

Apposition and deep long-lasting absorbable sutures
Immobilize for 5d an activity restrict for 6w
If muscle is lacerated, how do we fix it?
Post-op care?

GENTLY appose with thin but strong, long-lasting suture (tendon heals slowly and has delicate blood supply)
PROTECT IT! Immobilize for 3w (via rigid external fixation) and PT*
If tendon is lacerated, how do we fix it?
Post-op care?
Acute (secondary to trauma) or chronic (in very active/police dogs, usually degeneration at level of calcaneus)
What are the two presentations for achilles tendon rupture?
All of the above
Which one describes an achilles tendon rupture?
A. Proximal origin of achilles tendon complex
B. Rupture at myotendinous junction
C. Laceration thorugh tendon only
D. Avusion at calcaneous
E. All of the above

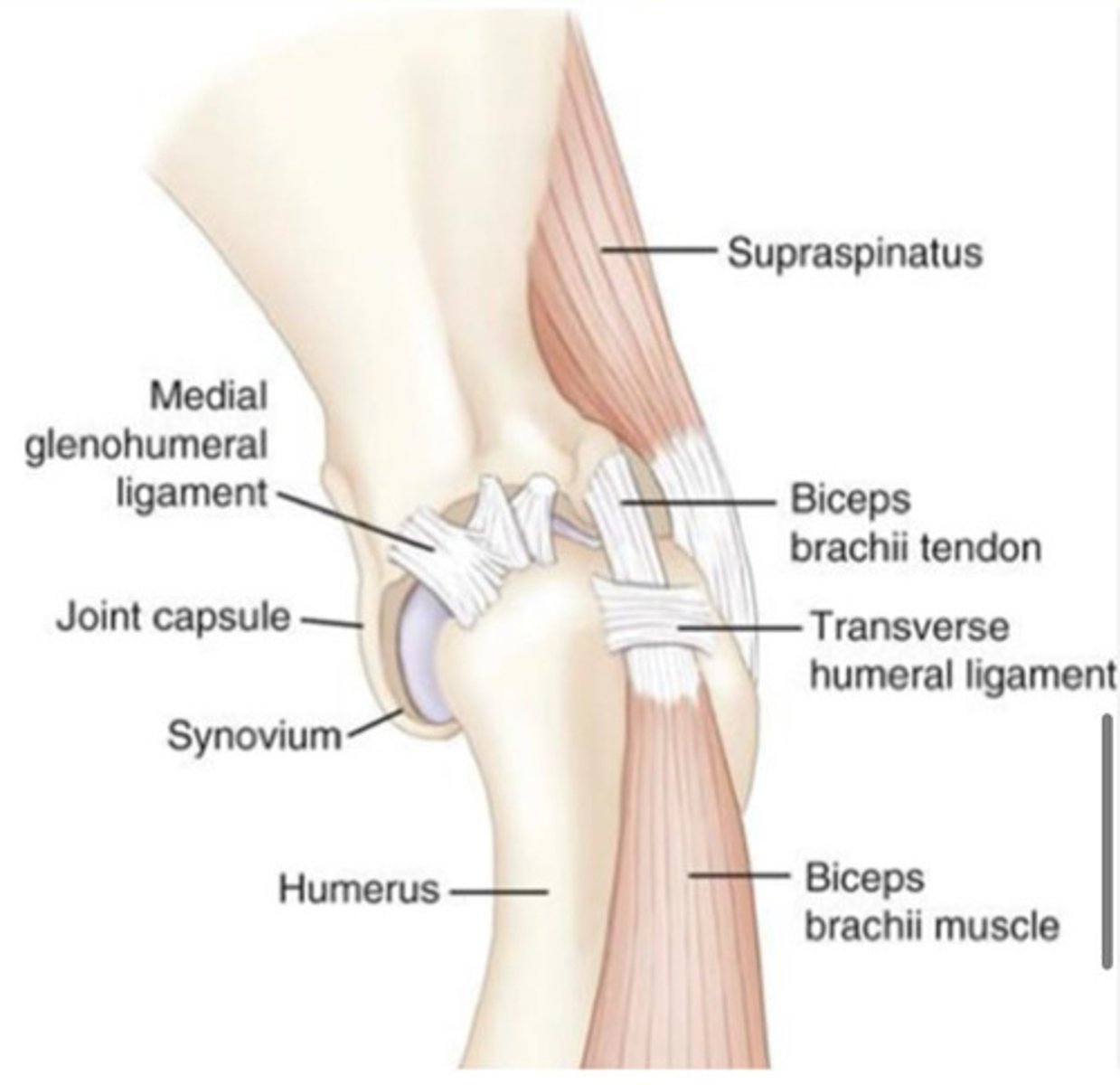
Tendon tearing, inflammation of tendon AND synovial sheath around it
Trauma or various tissue lesions (repetitive injury or overuse) causing hyperplasia/mineralization
Biceps tenosynovitis is an umbrella term for...?
Cause?
See plantigrade (if chronic) or gripper (if acute) stance, palpate large bulge, US for location of it, rads to look for bone avulsion
Achilles tendon rupture are very common. How do we diagnose it?

If acute, suture 3 parts (gastrocnemius tendon, SDF tendon, and common tendon of biceps femoris, semitendinosis and gracilis)
If chronic, suture whole complex
Protect the repair! Immobilize for 3-6w
Achilles tendon rupture are very common. How do we treat it acute vs chronic? Post-op care?

Superficial
Patellar
We need to repair most tendons, especially (superficial/deep) ones.
Between the digital flexor tendon and patellar tendon, which do you think is more important to fix?

Working/active dogs
Chronic/progressive/intermittent lameness, worse after exercise
Biceps test, rads/US*/MRI, arthroscopy
Biceps tenosynovitis
Can affect anyonre, but typical signalment?
Signs?
Dx?
Steroids or platelet enriched plasma within tendon and REST, slowly reintroduce activity
Want to prevent biceps tendon from gliding into shealth, so cut it! (Tenotomy or tenodesis) (do tenodesis if really active, consists of cutting and attaching to proximal humerous so recover faster; tenotomy will eventually reattach itself)
First we try to treat biceps tenosynovitis with medical management, what does this consist of?
If this doesn't work, what do we do next?

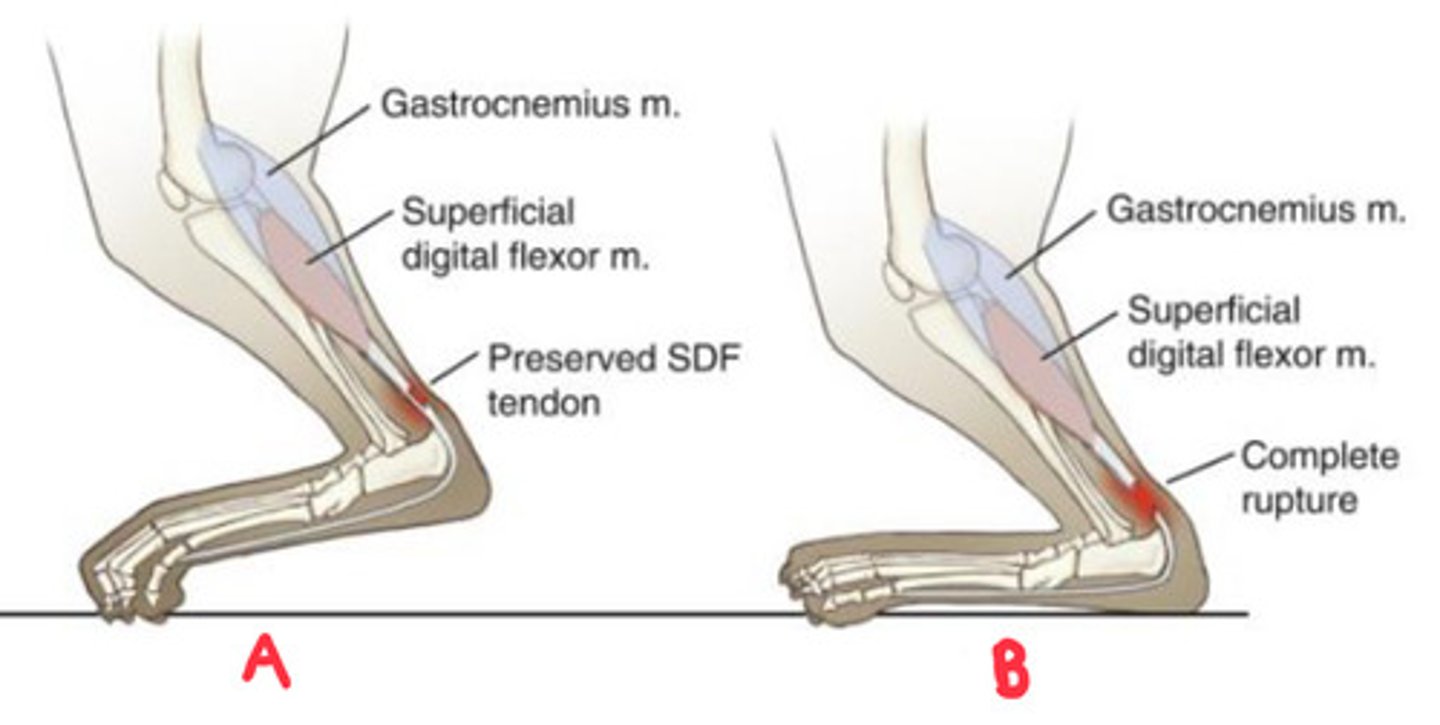
Partial (A): hyperflexion of digits (gripper stance)
Complete (B): hyperflexion of tarsus and hyperextension of digits (platigrade stance)
Clinical presentation of partial vs complete achilles tendon rupture?
Feel for scapular spine, atrophy if really prominent
How can you assess for muscle atrophy with biceps tenosynovitis?
Usually a hunting dog with trauma ~3w ago
Hold elbows up (specific stance)
Resect myotenounus junction, excellent! (fast recovery)
Infraspinous fibrous contracture
Typical signalment and history?
Signs?
Tx/prognosis?

Infraspinous fibrous contracture and elbow luxation; Elbow luxation will be SUPER painful and lots of swelling, contracture is non-painful and no swelling
You have a dog that has this stance shown here, holding his elbow up. Without any other information what are your top 2 differentials? How can you tell the difference?

Biceps tenosynovitis
Flex shoulder (distal insertion of biceps is on radius), extend elbow, and push with finger on biceps tendon - if painful will get reaction
What does the "biceps test" look for?
How do you do it?

German and belgian shepards
Non-painful lameness with a "jerk" (circumduction like gait, short steps), feel thick spot in caudal thigh by gracilis
50%
No treatment (ppl have tried resecting it but recurs in 2-4m), guarded prognosis - will eventually not be able to walk
Gracilis semitendinosus fibrotic myopathy
Only seen in what two breeds?
Signs?
What % are bilateral?
Tx/prognosis?

LC - Assimilation
All of the above (that's why we need multimodal treatment, lots of different pain pathways!)
OA is an issue with the...
A. Cartilage
B. Bone
C. Joint capsule
D. All of the above
The 3 A's: Anticipate (if don't, will get flares of pain), Assess (know what to look for), Alleviate
What is the best way to understand and best manage OA?
OA
______________ is the best model for chronic pain
Weight management (want 4/9 BCS)
Diet (omega 3's)
Exercise triad (regular)
Anti-inflammatory agents (carprofen, firocoxib, meloxicam)
PT
OA management needs a multimodal approach. What are the 5 most important steps?
Secondary; Primary
Most OA cases in dogs are (primary/secondary)
Most OA cases in cats are (primary/secondary)
Puppies with history of distal femoral fracture
Muscular trauma, osseous callus, and immobilization (occurs within 5d after not using leg)
MAKE SURE to practice ROM post fracture
No quad muscles, can't flex, feels like a tight cord
If acute, PT to break adhesions but if it's been a few days will need surgery to break adhesions (or shorten femur, salvage procedure)
Femoral quadricepts contracture
Typical signalment and history?
Predisposing factors?
How can you prevent it?
Signs?
Tx/prognosis?

True :(
T/F: Scottish folds are predisposed to OA so knowing how to manage it is crucial knowledge (not on the test at all but related and extremely important 2 me)

A small walk everyday
For OA management, which is the best choice?
A. A small walk everyday
B. Big, long walks only on the weekend
C. No exercise at all
D. Take them to pilates and cycling classes
Omega 3 fatty acids
What diet-related thing(s) have research to prove it helps with OA management?
A. Soybean and avocado unsaponifiables
B. Glucosamine
C. Omega 3 fatty acids
D. All of the above
E. None of the above
All of the above E
What anti inflammatory-related thing(s) have research to prove it helps with OA management?
A. Carprofen
B. Firocoxib
C. Meloxicam
D. All of the above
False, don't over-interpret rads (look at how dog is doing!)
T/F: This dog presents with no clinical signs but has severe evidence of OA on rads therefore we should start treatment to manage this

Long term treatment (over 28d)
For OA, with all NSAIDs combined, which has been proven to have better success?
A. Long term treatment (over 28d)
B. Short term treatment (under 28d)
Done
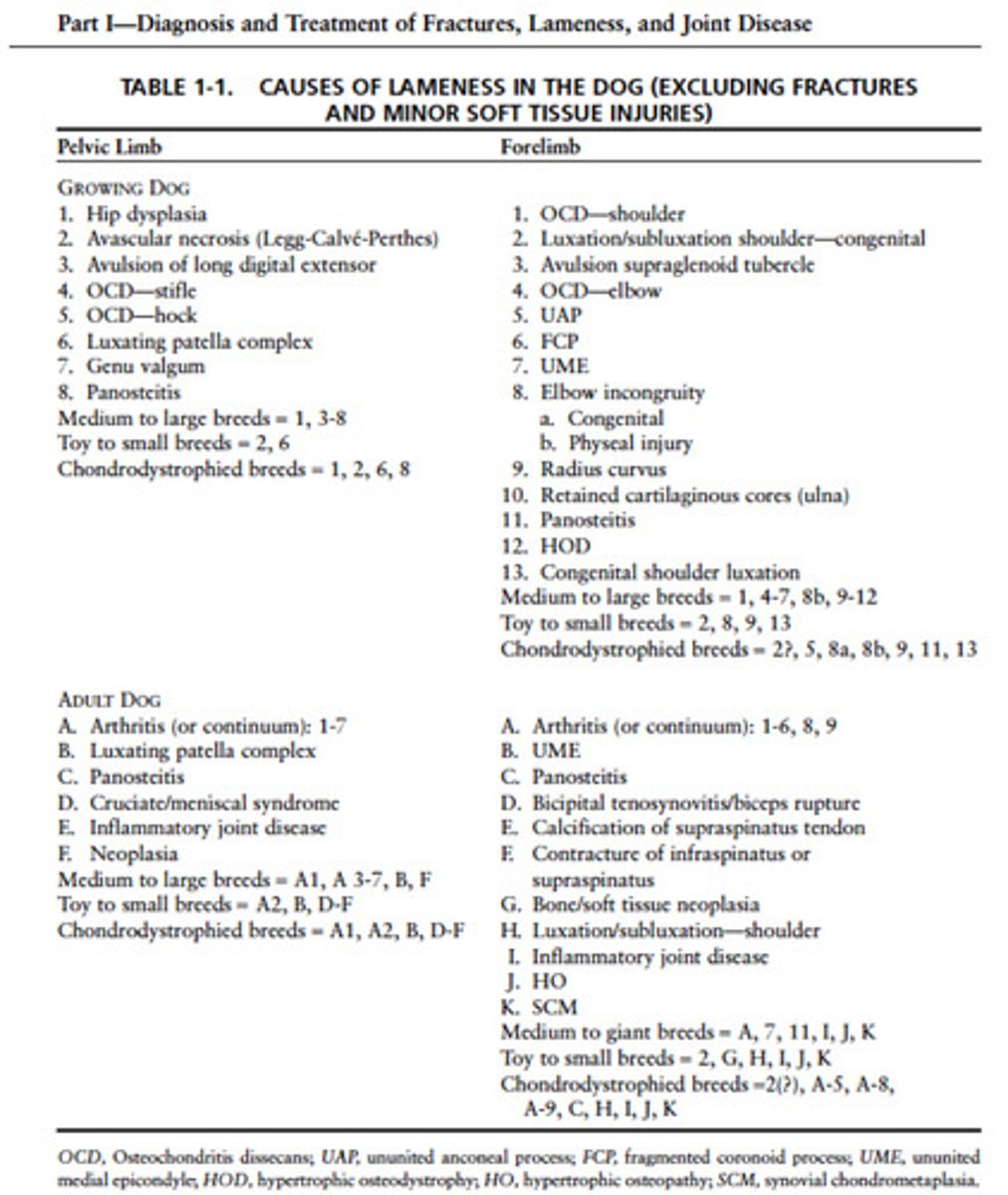
Review this list of lameness differential diagnoses