6.2 Theme 1 - Bacteria & Antimicrobial Agents
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
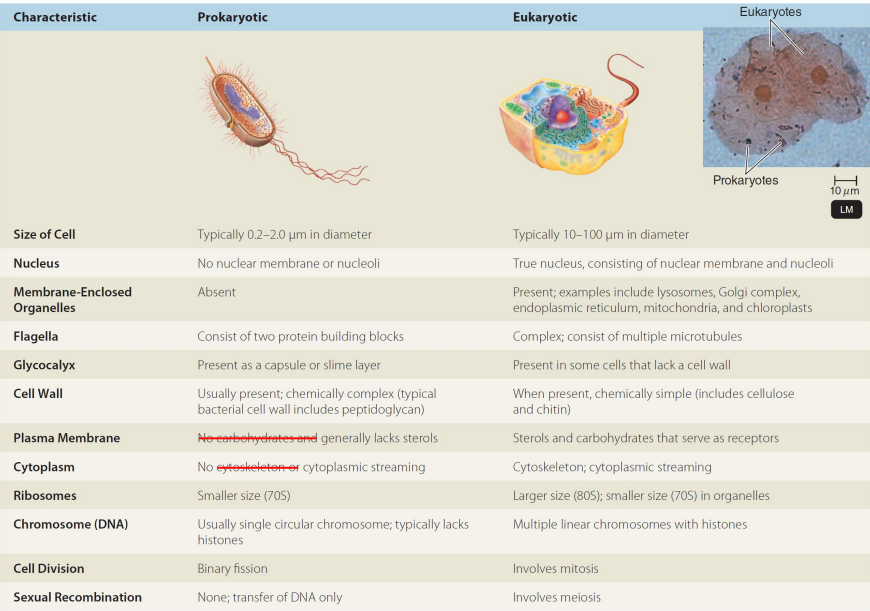
Outline the main differences between prokaryotes & eukaryotes.
Prokaryotes are unicellular organisms that lack a defined nucleus and membrane-bound organelles, while eukaryotes are multicellular (or unicellular) organisms that possess a true nucleus and are more complex in structure.
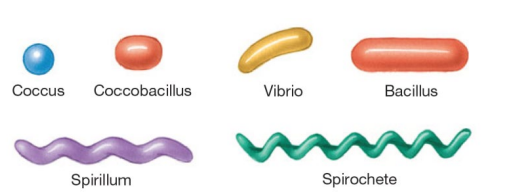
Outline the diff shapes of bacteria.
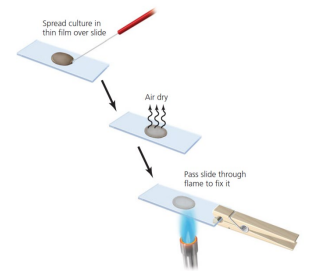
How do you fix a bacterial sample to a slide before staining?
Spread culture thinly over the slide
Air dry
Pass slide through flame to fix it
What is the Gram stain procedure?
Apply crystal violet for 1 min
Add iodine for 1 min (purple = Gram +)
Rinse and decolourise with acetone for 5 s
Wash immediately with water (if stained still, it’s Gram +; if not, it’s Gram –)
Apply safranin for 30 s to stain Gram –
Wash, blot, and air dry (Gram – will appear red)
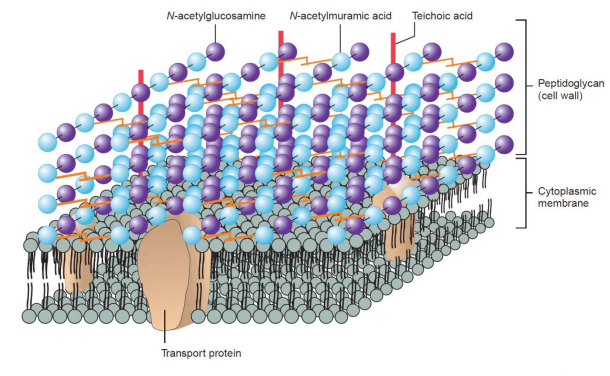
Why do Gram-positive bacteria stain purple and how does their cell wall structure affect permeability?
Thick peptidoglycan layer retains crystal violet/iodine after acetone → stains purple
Cell wall allows chemicals and enzymes to pass through (porous)
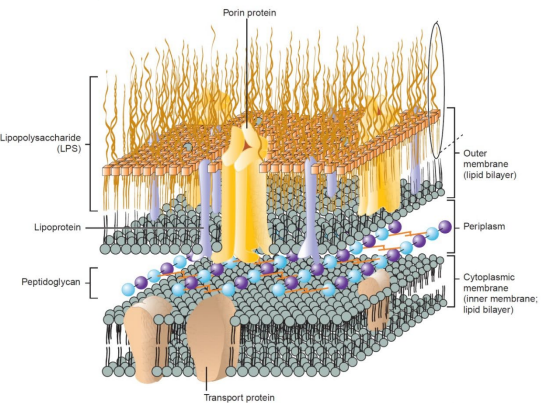
Acetone removes outer membrane; thin peptidoglycan cannot retain crystal violet/iodine = decolourised
Counterstaining with safranin = cells appear red
Thin peptidoglycan with porin channels allow diffusion of nutrients
Why do acid-fast bacteria like Mycobacterium tuberculosis grow slowly?
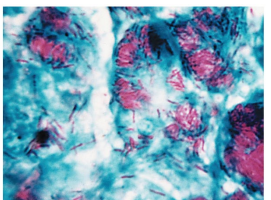
Mycobacteria have a thick cell wall (~60% lipid, less peptidoglycan than Gram +)
Lipid-rich wall slows nutrient and agent flow → slow growth and high energy demand for wall synthesis
Example: Mycobacterium tuberculosis stains red with carbolfuchsin
How does oxygen affect the growth of different types of bacteria?
Obligate aerobes – need O₂ to grow
Facultative anaerobes – grow with or without O₂, better growth with O₂
Obligate anaerobes – cannot grow in presence of O₂
Aerotolerant anaerobes – grow anaerobically, tolerate O₂
Microaerophiles – need low O₂ concentration to grow
What is a pathogen?
A pathogen is an organism capable of causing disease; true pathogens cause disease in healthy, immunocompetent subjects.
What is pathogenicity?
Pathogenicity is the ability to cause disease
E.g. Neisseria gonorrhoeae requires pili to attach to urethral epithelium, and strains without pili are non-pathogenic
What is virulence?
Virulence is an organism’s relative power to cause disease; illness can be asymptomatic, mild, or severe, and may depend on host factors or microbial virulence factors
How does the capsule of Streptococcus pneumoniae affect pathogenicity and virulence?
The presence of a capsule determines if Streptococcus pneumoniae (pneumococcus) is pathogenic, and the type of capsule determines its virulence—type 3 causes severe disease, while type 30 rarely causes severe disease.
Outline Koch’s method for identifying a bacterial pathogen
Observe the same bacterium in all individuals with the disease
Isolate the bacterium and grow it in a pure culture
Introduce the pure culture into a healthy host
Observe if the host develops the same disease
Re-isolate the same bacterium from the newly diseased host
What are the limitations of Koch’s postulates?
They don’t apply to all infectious diseases
Mycobacterium leprae (causes leprosy) cannot be cultured in the lab
Ethics prohibit deliberately transmitting diseases between humans, so animal models are used instead
Some diseases have a polymicrobial origin
Immunosuppression may lessen the antibody response and render the host very susceptible to the disease
Genetic predisposition of individuals
Some infections arise from the host’s own normal flora (e.g., E. coli, Candida spp.)
What are the characteristics of a successful pathogen?
1. Survival and transmission in the environment
2. Attachment to the surface of the host
3. Overcoming the body defences against infection
4. Ability to damage the host, either directly or indirectly
5. Ability to replicate in the host, producing progeny able to infect others
What is required of an antimicrobial drug for it to be effective in vivo?
It must be toxic to the microbe but not toxic to the host.
How are antibacterial agents classified and how do they work?
Bactericidal drugs – kill bacteria
Bacteriostatic drugs – inhibit bacterial growth; reversible and rely on host defences
Cidal or static activity may depend on bacterial species (e.g., chloramphenicol inhibits E. coli but kills Haemophilus influenzae)
Classification by target site – drugs inhibit specific bacterial processes
Classification by chemical structure – drugs grouped into families
Cell wall inhibitors
Cell membrane
DNA/RNA
Ribosomes
Folic acid
Why do antibiotics affect bacteria but not human cells?
They target processes specific to microbes, such as peptidoglycan synthesis so they can kill or inhibit bacteria without harming human cells.
Why is activity at several body sites important for an antibacterial agent?
Some microorganisms can infect multiple body sites. After a local infection, they may enter the bloodstream and spread (focal infection), so the drug needs to reach all relevant sites to be effective.
How else are antibiotics different from other drugs?
They are often given to large numbers of patients for short periods, and can be used therapeutically (to treat infection) or prophylactically (to prevent infection).
How can antibiotic resistance spread between bacteria?
Resistance can be transferred to other bacteria and spread clonally or via gene transfer
Plasmids – extra-chromosomal DNA loops – can carry resistance genes
Conjugative plasmids can pass between different bacterial species or genera, promoting the spread of resistance