Cardio & Respiratory Textbook Questions
1/87
Earn XP
Description and Tags
VET30420
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
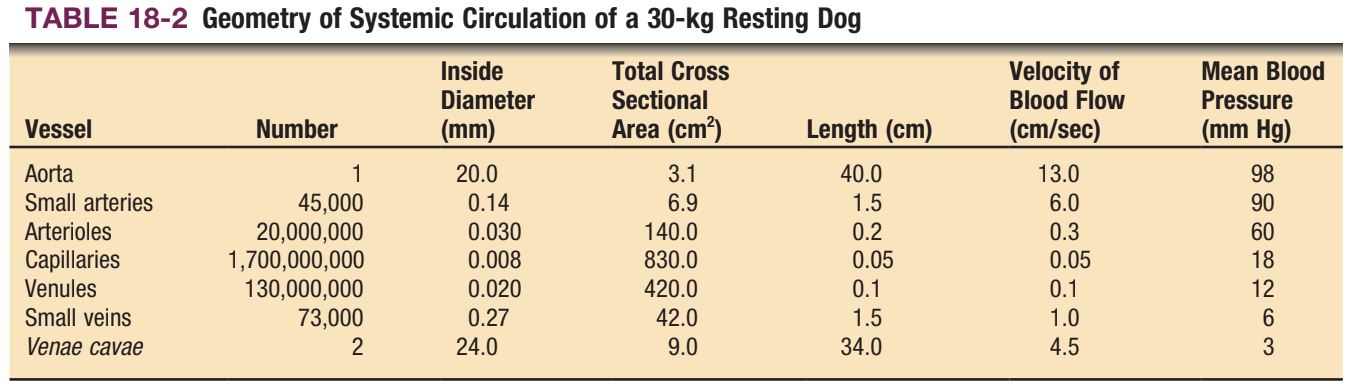
CH 18, Q1: according to Table 18-2, how long dies it take for blood to travel the length of a canine capillary?
a. 0.05 sec
b. 0.1 sec
c. 1 sec
d. 10 sec
e. 20 sec
c. 1 sec
CH 18, Q2: the amount of blood pumped by the left ventricle in 1 minute would equal:
a. the amount of blood that flowed through the coronary circulation (in the same minute)
b. one-half the cardiac output
c. two times the cardiac output
d. the amount of blood that flowed through all organs of the systemic circulation, except for coronary blood flow
e. the amount of blood that flowed through the lungs
e. the amount of blood that flowed through the lungs
CH 18, Q3: a transfusion of normal plasma into a normal dog would:
a. decrease the hematocrit of the recipient’s blood
b. increase the viscosity of the recipient’s blood
c. decrease the mean corpuscle hemoglobin concentration (MCHC) in the recipient’s plasma
d. increase the number of cells in the recipient’s blood
e. decrease the concentration of proteins in the recipient’s plasma
a. decrease the hematocrit of the recipient’s blood
CH 18, Q4: which of the following sequences of capillary beds might a red blood cell encounter in a normal circulation?
a. lungs, skin, lungs, brain
b. spleen, liver, mesentery, lungs
c. coronary, kidney (glomerular), kidney (tubular), lungs
d. lungs, coronary, stomach, liver
e. brain, lungs, liver, coronary
a. lungs, skin, lungs, brain
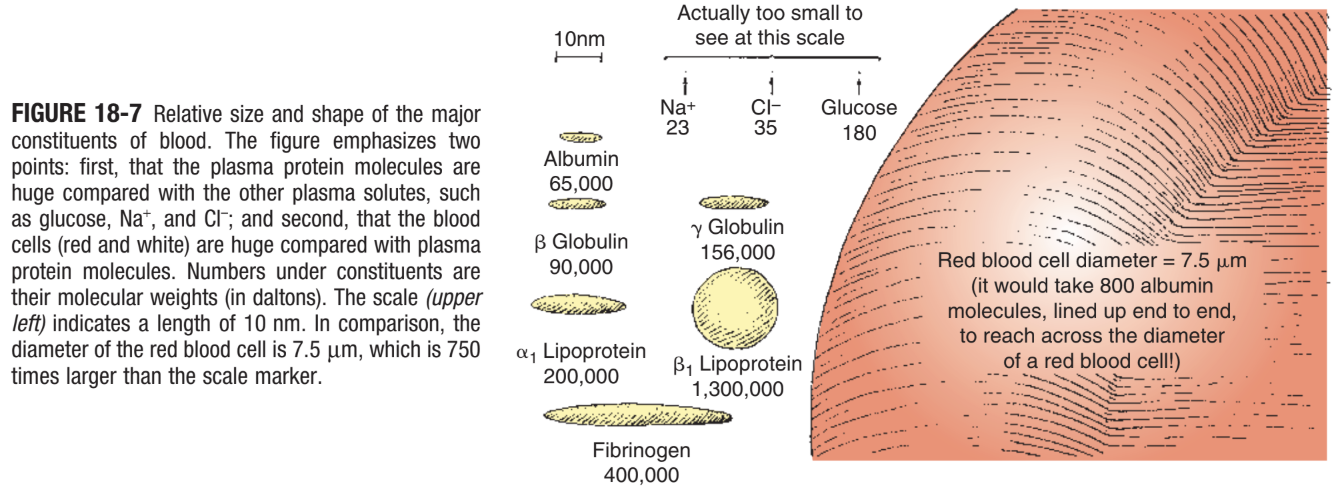
CH 18, Q5: the walls of most capillaries have pores or clefts in them, which are approximately 4 nm in diameter according to Figure 18-7:
a. a capillary pore is many times larger in diameter than a sodium ion
b. an albumin molecule is approximately 2.5 times longer than the diameter of a capillary pore
c. the diameter of a red blood cell is many times greater than the diameter of a capillary pore.
d. a molecule of β globulin or γ globulin could just about squeeze through a capillary pore if it were lined up exactly right
e. all of the above are correct
e. all of the above are correct
CH 18, Q6: suppose that the following conditions exist in a particular blood vessel:
blood pressure (BP) inside vessel at inlet = 60 mmHg
BP inside vessel at midpoint = 45 mmHg
BP inside vessel at outlet = 30 mmHg
BP outside vessel at midpoint = 5 mmHg.
Under these conditions:
a. perfusion pressure for blood flow through this vessel = 30 mmHg
b. perfusion pressure for blood flow through this vessel = 15 mmHg
c. distending pressure at the vessel midpoint = 45 mmHg
d. distending pressure at the vessel midpoint = 40 mmHg
e. both a and d are correct
e. both a and d are correct
CH 18, Q7: compared with the systemic circulation, the pulmonary circulation:
a. carries more blood flow per minute
b. has a lower perfusion pressure
c. has a higher resistance to blood flow
d. carries blood that has a lower hematocrit
e. contains a higher blood volume
b. has a lower perfusion pressure
CH 19, Q1: an increase in heart rate could result from:
a. an increase in sympathetic nerve activity to the heart
b. an abnormally rapid decrease in permeability of SA node cells to K+ during diastole
c. an abnormally rapid increase in permeability of SA node cells to Na+ during diastole
d. a decrease in parasympathetic nerve activity to the heart
e. all the above
e. all the above
CH 19, Q2: in which of the following arrhythmias will there be more atrial beats per minute than ventricular beats?
a. complete (third-degree) AV block
b. frequent premature ventricular contractions
c. sick sinus syndrome (sinus bradycardia)
d. first-degree AV block
e. ventricular tachycardia
a. complete (third-degree) AV block
CH 19, Q3: the normal pathway followed by a cardiac action potential is to begin in the SA node and then propagate:
a. across the atria in the bundle of His
b. through the connective tissue layers that separate the atria and ventricles
c. across the atria and to the AV node
d. from the left atrium to the right atrium
e. from the left atrium to the left ventricle and from the right atrium to the right ventricle
c. across the atria to the AV node
CH 19, Q4: which statement is true?
a. the refractory period of cardiac muscle cells is much shorter than their mechanical contraction
b. the cardiac action potential propagates from one cardiac cell to another through gap junctions
c. purkinje fibers are special nerves that spread the cardiac action potential rapidly through ventricles
d. ventricular muscle cells characteristically depolarize spontaneously to threshold
e. the permeability of ventricular muscle cells to Ca2+ is lower during the plateau of an action potential than it is at rest
b. the cardiac action potential propagates from one cardiac cell to another through gap junctions
CH 19, Q5: which of the following types of drugs would be the best choice to treat a patient with both supraventricular tachycardia and inadequate cardiac contractility?
a. local anesthetic (fast Na+ channel blocker)
b. muscarinic cholinergic antagonist
c. beta-adrenergic agonist
d. cardiac glycoside (inhibits Na+/K+ pump)
e. calcium channel blocker
d. cardiac glycoside (inhibits Na+/K+ pump)
CH 19, Q6: during which phase of a normal ventricular action potential is it most likely that fast Na+ channels are in an inactivated state, slow Ca2+ channels are open, and most K+ channels are closed?
a. phase 0 (rapid depolarization)
b. phase 1 (partial repolarization)
c. phase 2 (plateau)
d. phase 3 (repolarization)
e. phase 4 (rest)
c. phase 2 (plateau)
CH 19, Q7: which of the following is true for both cardiac muscle and skeletal muscle?
a. the muscle forms a functional syncytium
b. an action potential in the muscle cell membrane is required to initiate contraction
c. pacemaker cells spontaneously depolarize to threshold and initiate action potentials
d. frequent action potentials in motor neurons can cause a sustained (tetanic) muscle contraction
e. extracellular Ca2+ that enters the muscle cell during an action potential triggers the release of additional Ca2+ from the sarcoplasmic reticulum
b. an action potential in the muscle cell membrane is required to initiate contraction
CH 20, Q1: in which of the following arrhythmias will the ECG characteristically show the same number of P waves and QRS complexes?
a. complete (third-degree) AV block
b. first-degree AV block
c. ventricular tachycardia
d. atrial flutter
e. all the above
b. first-degree AV block
CH 20, Q2: the time required for the conduction of the cardiac action potential through the AV node would be approximately equal to the:
a. RR interval
b. PR interval
c. ST interval
d. PP interval
e. QT interval
b. PR interval
CH 20, Q3: the T wave in a normal ECG is:
a. always negative
b. always positive if the R wave is positive
c. also known as the pacemaker potential
d. caused by the delay between atrial and ventricular depolarization
e. caused by ventricular repolarization
e. caused by ventricular repolarization
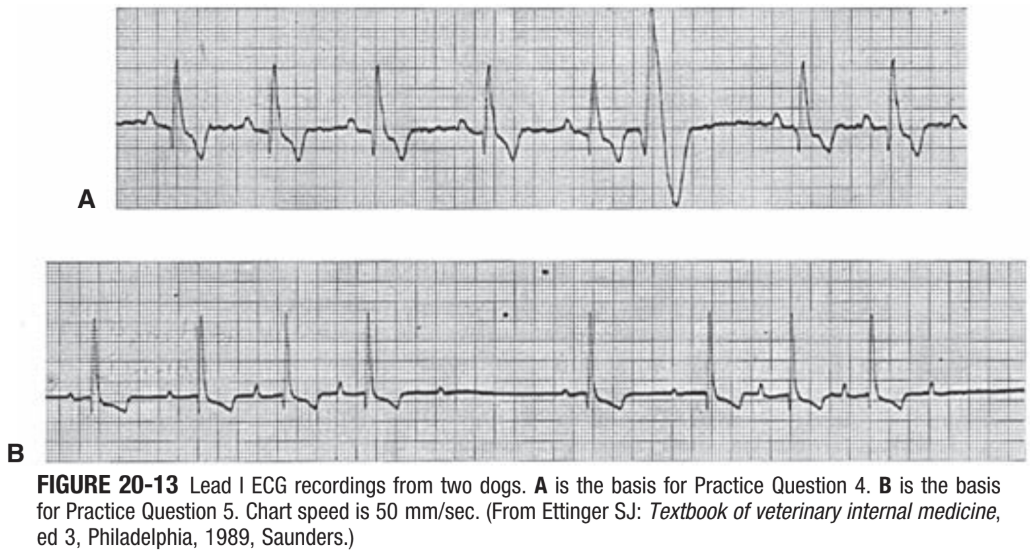
CH 20, Q4: the ECG in Figure 20-13, A indicates:
a. sinus arrhythmia
b. right ventricular hypertrophy
c. ST segment elevation
d. premature ventricular contraction
e. atrial fibrillation
d. premature ventricular contraction
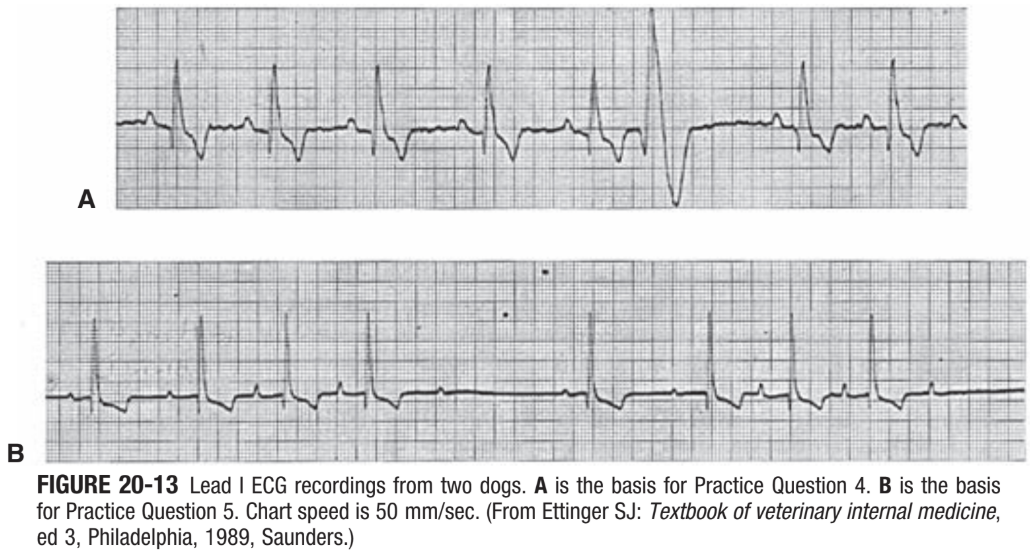
CH 20, Q5: the ECG in Figure 20-13, B, indicates:
a. second-degree AV block
b. third-degree AV block
c. sinus bradycardia
d. ventricular tachycardia
e. ST segment elevation
a. second-degree AV block
CH 21, Q1: in the normal cardiac cycle:
a. ventricular systole and ventricular ejection begin at the same time
b. the second heart sound coincides with the beginning of isovolumetric relaxation
c. the highest left ventricular pressure is reached just as the aortic valve closes
d. aortic pressure is highest at the beginning of ventricular systole
e. atrial systole occurs during rapid ventricular ejection
b. the second heart sound coincides with the beginning of isovolumetric relaxation
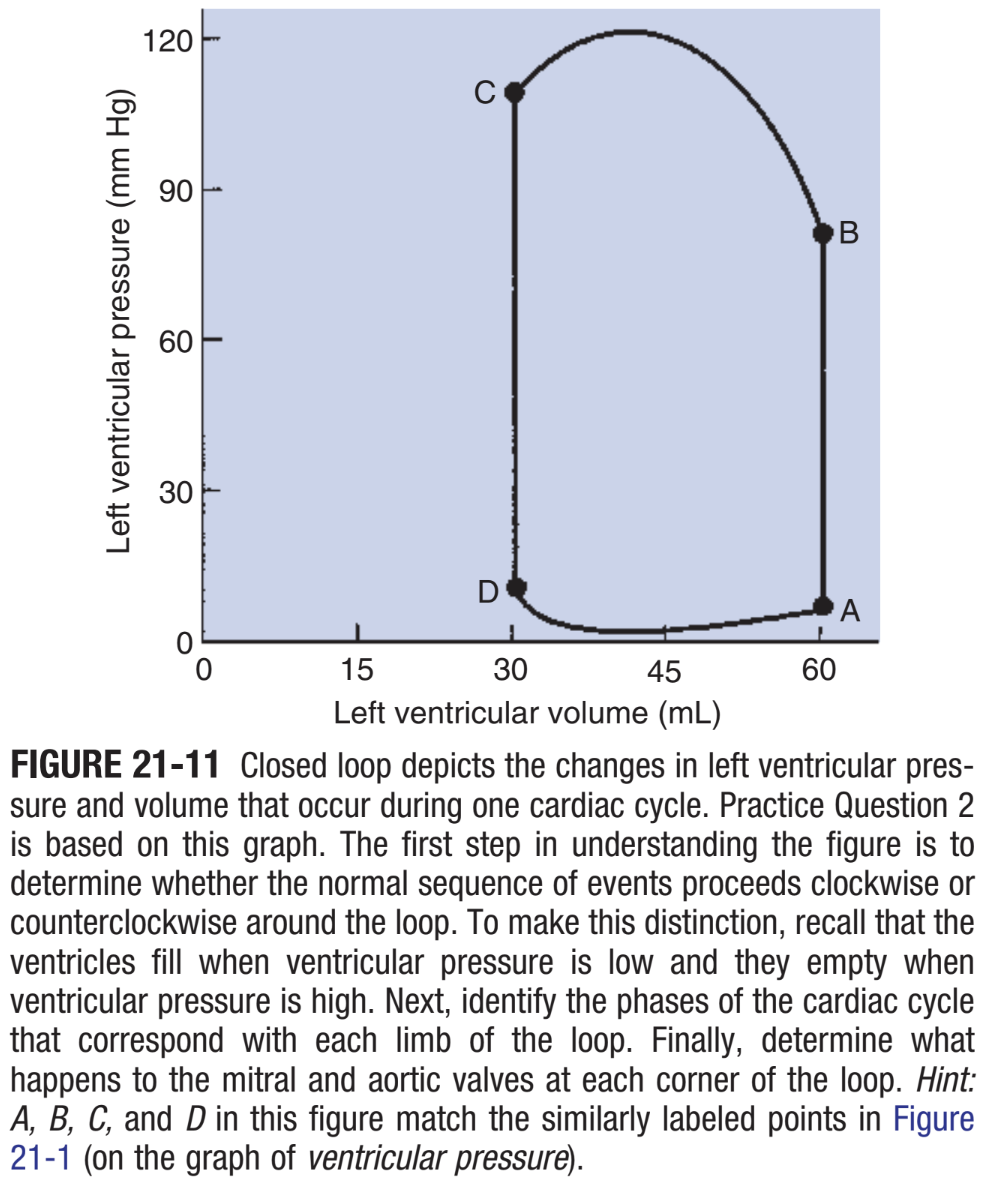
CH 21, Q2: Figure 21-11 shows a plot of the changes in pressure and volume that occur in the left ventricle during one cardiac cycle. Which of the following is true?
a. point D marks the beginning of isovolumetric relaxation
b. point B marks the closure of the aortic valve
c. point C marks the opening of the mitral valve
d. point A marks the beginning of isovolumetric contraction
e. point D marks the beginning of ventricular systole
d. point A marks the beginning of isovolumetric contraction
CH 21, Q3: which statement is true for a normal heart?
a. sympathetic activation causes end-systolic ventricular volume to increase
b. an increase in ventricular preload causes end-diastolic ventricular volume to decrease
c. an increase in ventricular contractility causes systolic duration to increase
d. an increase in ventricular contractility causes the external work of the heart to decrease
e. pacing the heart at a high rate causes stroke volume to decrease
e. pacing the heart at a high rate causes stroke volume to decrease
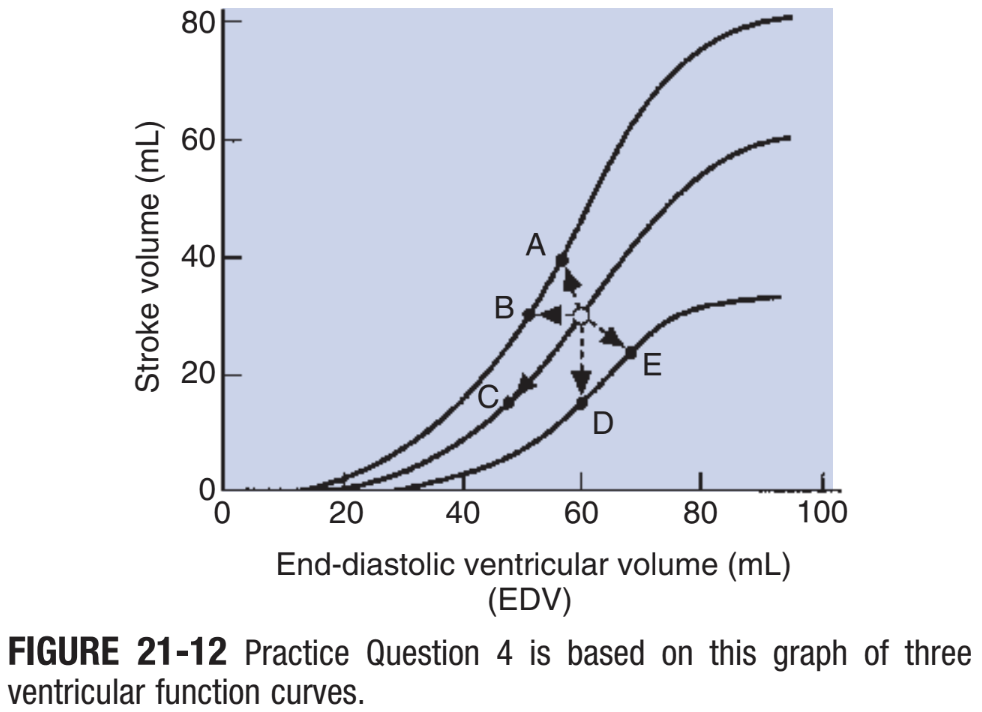
CH 21, Q4: starting at the open circle in Figure 21-12, which point would be reached after the contractility decreased and the preload increased?
a. point A
b. point B
c. pont C
d. point D
e. point E
e. point E
CH 21, Q5: you examine a 7-year-old poodle and find evidence of a systolic murmur (no diastolic murmur), pulmonary edema (indicated by rapid, noisy respiration and cough), left ventricular hypertrophy (no right ventricular hypertrophy), and exercise intolerance. the most likely explanation for the symptoms is:
a. mitral regurgitation
b. mitral stenosis
c. aortic regurgitation
d. pulmonic stenosis
e. ventricular septal defect
a. mitral regurgitation
CH 22, Q1: which of the following is a correct comparison between segments of the systemic circulation?
a. the aorta and large arteries have a higher compliance than the veins
b. the aorta and large arteries have a higher resistance to blood flow than the capillaries
c. the veins have a higher resistance to blood flow than the capillaries
d. the arterioles have a higher resistance to blood flow than the capillaries
e. if the heart is stopped, the pressure in the veins will become higher than the pressure on the aorta and large arteries
d. the arterioles have a higher resistance to blood flow than the capillaries
CH 22, Q2: if aortic compliance decreases while heart rate, cardiac output, and total peripheral (TPR) remain unchanged:
a. pulse pressure will be unchanged
b. pulse pressure will increase
c. pulse pressure will decrease
d. one cannot know the effect on pulse pressure because stroke volume may have changed
e. one cannot know the effect on pulse pressure because mean aortic pressure may have changed
b. pulse pressure will increase
CH 22, Q3: which of the following would cause mean aortic pressure to increase?
a. stroke volume increases from 30 to 40 mL, and heart rate decreases from 100 to 60 beats/min
b. arterial compliance decreases
c. cardiac output decreases
d. arterioles throughout the body dilate
e. TPR increases
e. TPR increases
CH 22, Q4: the following measurements are made on a dog:
heart rate, 80 beats/min
stroke volume, 30 mL
mean aortic pressure, 96 mmHg
mean pulmonary artery pressure, 30 mmHg
left atrial pressure, 5 mmHg
right atrial pressure, 12 mmHg
The TPR of this dog (taking into account both arterial and atrial pressure) is exactly:
a. 10.42 mmHg/L/min
b. 12.50 mmHg/L/min
c. 35.00 mmHg/L/min
d. 37.92 mmHg/L/min
e. 40.00 mmHg/L/min
c. 35.00 mmHg/L/min
TPR= perfusion pressure/ cardiac output (84/2.4= 35)
perfusion pressure = mean aortic pressure - right arterial pressure (96-12= 84)
cardiac output = heart rate x stroke volume (80×0.03= 2.4)
CH 22, Q5: which of the following would cause the largest decrease in coronary blood flow?
a. coronary arterioles constrict to ½ their normal diameter
b. coronary arteries develop atherosclerosis, and lipid plaques plug up ½ their normal cross-sectional area
c. mean aortic pressure decreases to ½ its normal level
d. the resistance to coronary blood flow doubles
e. the resistance to coronary blood flow decreases to ¼ its normal value
a. coronary arterioles constrict to ½ their normal diameter
CH 22, Q6: a change from breathing normal air (21% O2) to breathing a gas mixture with only 10% O2 would cause pulmonary blood vessels to ___ and pulmonary vascular resistance to ___ .
a. constrict; increase
b. constrict; decrease
c. dilate; increase
d. dilate; decrease
e. remain unchanged; remain unchanged
a. constrict; increase
CH 23, Q1: which of the following will not cause pulmonary edema?
a. an increase in pulmonary capillary permeability to protein
b. a blockage of pulmonary lymph vessels
c. an increase in left atrial pressure
d. a constriction of pulmonary arterioles
e. left-sided heart failure
d. a constriction of pulmonary arterioles
CH 23, Q2: a patient with a form of protein-losing kidney disease has a plasma colloid osmotic pressure of 10 mmHg. The patient has edema but is not getting any worse. blood pressure and heart rate are normal. which of the following is probably preventing further edema?
a. increased interstitial fluid hydrostatic pressure
b. increased capillary hydrostatic pressure
c. decreased lymph flow
d. increased plasma sodium ion concentration
e. increased interstitial fluid oncotic pressure
a. increased interstitial fluid hydrostatic pressure
CH 23, Q3: the following parameters were measured in the microcirculation of a skeletal muscle during a period of vigorous exercise:
Pc (capillary hydrostatic pressure)= 34 mmHg
Pi (interstitial fluid hydrostatic pressure)= 10 mmHg
πc (capillary plasma oncotic pressure)= 24 mmHg
πi (interstitial fluid oncotic pressure)= 3 mmHg
which of the following is true?
a. these conditions would favor filtration
b. these conditions would favor reabsorption
c. these conditions would favor neither filtration nor reabsorption
d. it it not clear what these conditions favor because the concentration of plasma proteiin is not specified
a. these conditions would favor filtration
CH 23, Q4: the rate of diffusion of glucose molecules from capillary blood to interstitial fluid is most directly affected by the:
a. voltage difference between capillary blood and interstitial fluid
b. interstitial fluid hydrostatic pressure
c. size and number of capillary pores
d. amount of oxygen in the blood
e. hematocrit
c. size and number of capillary pores
CH 23, Q5: during a 30-minute hemorrhage, a horse loses a substantial volume of blood. The horse’s mean arterial pressure decreases from 90 to 75 mmHg, and the heart rate increases from 40 to 90 beats/min. The skin becomes cold and the mucous membranes become pale, suggesting marked vasoconstriction. Because hemorrhage involves the loss of whole blood (both plasma and cells) you might expect that, soon after such a hemorrhage, the horse’s remaining blood would still have a normal composition. however, you take a blood sample and discover that the hematocrit is abnormally low (only 28%). which of the following would most likely account for the decrease in hematocrit observed after the hemorrhage?
a. arteriolar constriction has caused capillary hydrostatic pressure to increase above normal
b. low capillary hydrostatic pressure has caused interstitial fluid to be reabsorbed into the bloodstream
c. many blood cells have been filtered out of capillaries and into the interstitial fluid
d. excess capillary filtration has caused interstitial fluid pressure to increase above normal
e. excess capillary filtration has caused capillary colloid osmotic pressure to increase above normal
b. low capillary hydrostatic pressure has caused interstitial fluid to be reabsorbed into the bloodstream
CH 24, Q1: the increase in coronary blood flow during exercise is:
a. called starling’s law of the heart
b. caused by activation of parasympathetic nerves to the heart
c. caused by compression of the coronary blood vessels during systole
d. closely matched to the metabolic requirements of the heart
e. called reactive hyperemia
d. closely matched to the metabolic requirements of the heart
CH 24, Q2: a dog with an arterial blood pressure of 120/80 mmHg has a cerebral blood flow of 100 mL/min. when blood pressure is increased to 130/100 mmHg, the cerebral blood flow increases to 105 mL/min. this is an example of:
a. active hyperemia
b. auto regulation
c. reactive hyperemia
d. the blood-brain barrier
e. hypoxic vasoconstriction
b. auto regulation
CH 24, Q3: local metabolic control of blood flow through skeletal muscle:
a. characteristically dominates over neurohumoral control
b. characteristically is subservient to neurohumoral control
c. can either dominate or be subservient to neurohumoral control, depending on whether the muscle is exercising or resting
d. depends primarily on changes in the resistance of the veins within the muscle
e. depends on the release of histamine from mast cells within the skeletal muscle
c. can either dominate or be subservient to neurohumoral control, depending on whether the muscle is exercising or resting
CH 24, Q4: in response to an increase in perfusion pressure, the arterioles of an auto-regulating organ ___, and the vascular resistance of the organ ___.
a. constrict; increases
b. constrict; decreases
c. dilate; increases
d. dilate; decreases
a. constrict; increases
CH 24, Q5: when a young dog with PDA attempts vigorous exercise:
a. arterioles in the exercising muscle constrict
b. oxygen concentration in the skeletal muscle interstitial fluid decreases
c. left ventricular output decreases
d. right ventricular output decreases
e. mean arterial pressure increases to very high levels
b. oxygen concentration in the skeletal muscle interstitial fluid decreases
CH 24, Q6: which of the following characteristically acts as a paracrine to cause vasoconstriction in systemic arterioles?
a. carbon dioxide
b. nitric oxide
c. prostacyclin (PGI2)
d. endothelin-1 (ET1)
e. bradykinin
d.endothelin-1
CH 25, Q1: vasovagal syncope:
a. involves decreased blood pressure and heart rate
b. involves increased sympathetic activity
c. involves decreased cardiac parasympathetic activity
d. prepares an animal for “fight or flight”
e. involves constriction of splanchnic arterioles
a. involves decreased blood pressure and heart rate
CH 25, Q2: the dilation of arterioles that occurs during steady-state exercise in active skeletal muscles could be eliminated by:
a. pharmacological blockade of action potentials in all autonomic nerves innervating the muscles
b. complete surgical removal of sympathetic innervation of the skeletal muscles
c. administration of a muscarinic cholinergic blocking agent
d. administration of a beta-adrenergic blocking agent
e. none of the above
e. none of the above
CH 25, Q3: a drug is injected intravenously into a dog and causes a transient increase in mean arterial pressure and a transient decrease in heart rate. the baroreceptor nerves are cut; the drug is re-injected and now causes a greater increase in blood pressure but no change in heart rate. these results are most consistent with the primary action of the drug being to:
a. activate the muscarinic cholinergic (M3) receptors of arterioles
b. activate the alpha-adrenergic receptors of arterioles
c. activate beta 1-adrenergic receptors of the pacemaker cells of the SA node
d. increase the synthesis of nitric oxide in arterioles
e. decrease the activity of arterial baroreceptors
b. activate the alpha-adrenergic receptors of arterioles
CH 25, Q4: a dog has had a hemorrhage. the heart rate is increased above normal, and the skin is cold. the mucous membranes are pale. in this situation (compared with normal):
a. the baroreceptor nerves are firing at a higher rate
b. the sympathetic nerves to the heart are firing at a decreased rate
c. the sympathetic nerves to the blood vessels of the skin and mucous membranes are firing at an increased rate
d. the parasympathetic fibers to the blood vessels are firing at an increased rate
e. the release of renin by the kidney is decreased
c. the sympathetic nerves to the blood vessels of the skin and mucous membranes are firing at an increased rate
CH 25, Q5: blood (250 mL) is taken from a vein of a dog. mean arterial pressure does not decrease measurably. nevertheless, it is likely that:
a. stimulation of atrial stretch receptors has decreased
b. stroke volume has increased
c. stimulation of aortic arch baroreceptors has increased
d. TPR has decreased
e. secretion of ADH by the pituitary has decreased
a. stimulation of atrial stretch receptors has decreased
CH 26, Q1: during experimental trials on a new artificial aortic valve, a dog is anesthetized and placed on cardiac bypass for 1 hour. after successful installation of the artificial valve, the dog is taken off bypass, and the normal circulation is restored. ten minutes later, the dog’s central venous pressure is 20 mmHg, mean arterial pressure is 90 mmHg, and heart rate is 130 beats/min. the cardiac output is not measured. but the surgeon suspects that it is too low and therefore the patient’s tissues are not being adequately supplied with blood. which of the following measures would be most likely to improve the delivery of blood to the patient’s tissues?
a. transfusion with 500 mL of whole blood
b. administration of isoproterenol (selective beta-adrenergic agonist)
c. increasing the heart rate by electrical pacing
d. administration of norepinephrine (non-selective alpha/beta adrenergic agonist)
e. administration of a beta-adrenergic antagonist, such as propranolol
b. administration of isoproterenol (selective beta-adrenergic agonist)
CH 26, Q2: one of the nerves leading to a dog’s heart is stimulated for 1 minute while left atrial pressure, heart rate, and left ventricular output are measured (Figure 26-10). during this stimulation:
a. venous return to the left atrium transiently exceeds left ventricular output
b. the increase in left ventricular output at the beginning of stimulation can be explained by Starling’s law of the heart
c. stroke volume is lower after 15 seconds of stimulation than before stimulation
d. the effects of the nerve stimulation are similar to those caused by sympathetic activation of the heart
e. the progressive decline in left ventricular output during the stimulation is probably caused by a progressive increase in ventricular end-diastolic volume
d. the effects of the nerve stimulation are similiar to those caused by sympathetic activation of the heart
CH 26, Q3: one hour after a severe hemorrhage, a dog’s arterial pule pressure, mean pressure, and hematocrit are all below nomrla. which of the following statements is true?
a. the diminished pulse pressure reflects decreased aortic compliance
b. the diminished mean pressure probably results from decreased TPR
c. the diminished hematocrit probably results from reabsorption of interstitial fluid into the bloodstream
d. under these conditions, the action potential frequency of the arterial baroreceptor is greater than normal
e. under these conditions, sympathetic activity is probably less than normal
c. under these conditions, the action potential frequency of the arterial baroreceptor is greater than normal
CH 26, Q4: when a sheep is held in a vertical, head-up position, arterial pressure decreases because:
a. the baroreceptor reflex causes an increase in TPR
b. valves in the leg veins promote the return of blood to the heart
c. the respiratory pump promotes movement of abdominal venous blood into the thorax
d. central blood volume is increased
e. right atrial pressure is decreased
e. right atrial pressure is decreased
CH 26, Q5: during exercise in a normal animal:
a. TPR is decreased
b. cardiac output is increased
c. stroke volume is increased
d. blood pressure is nearly normal
e. all the above are true
e. all the above are true
CH 45, Q1: which of the following is true?
a. oxygen consumption per kilogram body weight is greater in a 50-g mammal than in a 50-kg animal
b. maximal oxygen consumption in mammals is directly related to the volume of mitochondria in the skeletal muscles
c. oxygen consumption increases when metabolic rate increases
d. oxygen consumption can increase up to thirtyfold during intense exercise
e. all of the above are true
e. all of the above are true
CH 45, Q2: functional residual capacity is:
a. the volume of air remaining in the lung at the end of a maximal forced expiration
b. the mechanical equilibrium of the respiratory system
c. less than residual volume
d. greater than total lung capacity
e. determined by metabolic rate
b. the mechanical equilibrium of the respiratory system
CH 45, Q3: which of the following lists includes only structures that compose the anatomic dead-space?
a. respiratory bronchioles, alveoli, trachea, nasal cavity
b. pharynx, bronchi, alveolar ducts, larynx
c. capillaries, respiratory bronchioles, trachea, bronchi
d. pharynx, nasal cavity, trachea, bronchi
e. capillaries, respiratory bronchioles, alveolar ducts, alveoli
d. pharynx, nasal cavity, trachea, bronchi
CH 45, Q4: a horse has a
tidal volume (VT) of 5 L
respiratory rate of 12 breaths/min
VD/VT ratio of 0.5
calculate minute ventilation (Ve) and alveolar ventilation (Va):
a. Ve= 60 L/min; Va= 2.5 L/min
b. Ve= 30 L/min; Va= 30 L/min
c. Ve= 60 L/min; Va= 30 L/min
d. Ve= 2.5 L/min; Va= 1.25 L/min
e. Ve= 5.0 L/min; Va= 2.5 L/min
c. Ve= 60 L/min; Va= 30 L/min
Ve= total volume of air breathed per minute (5 × 12 = 60)
Va= Ve - physiologic dead space (60 - (60 × 0.5) = 30)
CH 45, Q5: which of the following occur during inhalation?
a. diaphragm contracts, plural pressure increases, alveolar pressure decreases
b. diaphragm relaxes, external intercostal muscles contract, pleural pressure increases
c. diaphragm relaxes, pleural pressure decreases, internal intercostal muscles relax
d. external and internal intercostal muscles contract, pleural and alveolar pressures increase
e. diaphragm and external intercostal muscles contract, pleural and alveolar pressures decrease
e. diaphragm and external intercostal muscles contract, pleural and alveolar pressures decrease
CH 45, Q6: lung compliance
a. has the units of pressure per volume (cm H2O/L)
b. is greater at functional residual capacity (FRC) than at total lung capacity (TLC)
c. is less when the lung is inflated with saline than when the lung is filled with air
d. is greater in small mammals than in large mammals, even when adjusted for differences in lung sizes
e. is the only determinant of the change in pleural pressure during breathing
b. is greater at functional residual capacity (FRC) than at total lung capacity (TLC)
CH 45, Q7: pulmonary surfactant:
a. can be deficient in premature newborns
b. is produced in type 2 alveolar cells
c. is in part composed of dipalmitoyl phosphatidylcholine
d. decreases surface tension of the fluid lining the alveoli
e. all the above
e. all the above
CH 45, Q8: which of the following increases the frictional resistance to breathing?
a. intravenous administration of a beta2-adrenergic agonist
b. contraction of the abductor muscles of the larynx
c. a decrease in lung volume from FRC to residual volume
d. relaxation of the trachealis muscle
e. inhibition of the release of histamine from mast cells
c. a decrease in lung volume from FRC to residual volume
CH 45, Q9: the distribution of ventilation within the lung is influenced by:
a. regional variations in lung inflation
b. regional variations in airway resistance
c. regional variations in lung compliance
d. collateral ventilation
e. all the above
e. all the above
CH 46, Q1: which of the following statements accurately describes the pulmonary circulation?
a. it receives the total output of the right ventricle, except under conditions of alveolar hypoxia, when vasoconstriction reduces pulmonary blood flow
b. the medial layer of the main pulmonary arteries is composed of a thick layer of smooth muscle
c. the pulmonary veins return blood to the right atrium
d. unlike systemic capillaries, the pulmonary capillaries provide a large percentage of the total resistance to blood flow
e. all the above
d. unlike systemic capillaries, the pulmonary capillaries provide a large percentage of the total resistance to blood flow
CH 46, Q2: during exercise, cardiac output can increase fivefold, but pulmonary arterial pressure may not even double. this occurs because:
a. pulmonary vascular resistance decreases during exercise
b. unperfused capillaries are recruited during exercise
c. previously perfused vessels are distended during exercise
d. factors that dilate the pulmonary arteries are released by the endothelium during exercise
e. all the above
e. all the above
CH 46, Q3: which of the following will cause the greatest increase in pulmonary arterial pressure?
a. exposure of a cow to the hypoxia of high altitude
b. a twofold increase in pulmonary blood flow
c. stimulation of the vagus nerve (parasympathetic system) in a sheep
d. inhalation of a tidal volume in a horse
e. none of the above
a. exposure of a cow to the hypoxia of high altitude
CH 46, Q4: the bronchial circulation:
a. receives the total output of the right ventricle
b. drains into the pulmonary circulation and azygos vein
c. vasoconstricts in response to hypoxia
d. supplies nutrient blood flow only to bronchi and no other structures
e. has bronchial arterial pressure of the same magnitude as pulmonary arterial pressure
b. drains into the pulmonary circulation and azygos vein
CH 46, Q5: in quadrupeds, pulmonary blood flow is distributed:
a. within the lung, as would be predicted by the action of gravity
b. primarily to the ventral part of the lung during exercise
c. so that the dorsal-caudal regions of the lung receive the most blood flow
d. uniformly among the alveoli
e. uniformly when the animal is anesthetized
c. so that the dorsal-caudal regions of the lung receive the most blood flow
CH 47, Q1: calculate the alveolar oxygen tension (PAO2) of an anesthetized cow when the
barometric pressure = 750 mmHg
PH2O at body temperature = 50 mmHg
PaCO2 = 80 mmHg
the cow is breathing a mixture of 50% oxygen and 50% nitrogen. assume the respiratory exchange ratio is 1.
a. 270 mmHg
b. 620 mmHg
c. 275 mmHg
d. 195 mmHg
e. 670 mmHg
a. 270 mmHg
[fraction of inspired oxygen x (barometric pressure - water pressure) - (arterial CO2 pressure / respiratory exchange ratio)]
[0.5 x (750 - 50) - (80 / 1)] = 270
CH 47, Q2: which of the following will decrease the rate of oxygen transfer between the alveolar air and the pulmonary capillary blood?
a. increasing PaO2 from 100 to 500 mmHg
b. perfusing previously unperfused pulmonary capillaries
c. decreasing the mixed venous oxygen tension from 40 to 10 mmHg
d. destruction of alveolar septa and pulmonary capillaries by a disease known as alveolar emphysema
e. none of the above
d. destruction of alveolar septa and pulmonary capillaries by a disease known as alveolar emphysema
CH 47, Q3: during exercise, recruitment of muscle capillaries that are unperfused in the resting animal results in all the following except:
a. an increase in the velocity of capillary blood flow
b. an increase in the surface area for gas diffusion between tissues and blood
c. a decrease in distance between tissue capillaries
d. maintenance of tissue PO2 in the presence of increased demand for oxygen
e. a shorter distance for gas diffusion
a. an increase in the velocity of capillary blood flow
CH 47, Q4: which of the following could potentially result in more low Va/Q regions within the lung?
a. atelectasis (collapse) of one lobe of a dog lung
b. obstruction of both pulmonary arteries
c. doubling the ventilation to the right cranial lobe while its blood flow remains constant
d. vasoconstriction of the pulmonary arteries of the left lung in a cow
e. none of the above
a. atelectasis (collapse) of one lobe of a dog lung
CH 47, Q5: which of the following statements is correct?
a. right-to-left shunts represent an extremely high Va/Q ratio
b. right-to-left shunts are not a cause of elevated alveolar arterial oxygen difference
c. an increase in the alveolar dead-space can result from an increase in the number of high Va/Q units in the lung
d. the shape of the oxyhemoglobin dissociation curve means that low Va/Q units in the lung are not a cause of hypoxemia (low PaO2)
e. totally occluding (obstructing) the right pulmonary artery increases the right-to-left shunt fraction by 50%
c. an increase in the alveolar dead-space can result from an increase in the number of high Va/Q units in the lung
CH 47, Q6: a horse has difficulty inhaling, especially during exercise. arterial blood gas tensions at rest are
PaO2= 55 mmHg
PaCO2= 70 mmHg
after you give the horse oxygen to breathe, PaO2 increases to 550 mmHg, and PaCO2 remains unchanged. the cause of these gas tensions is:
a. right-to-left shunt through a complex cardiac defect
b. alevolar hyperventilation
c. a large number of alveoli with high Va/Q ratios
d. alveolar hypoventilation
e. none of the above
d. alveolar hypoventilation
CH 48, Q1: if 1 g of hemoglobin has an oxygen capacity of 1.36 mL of oxygen, what is the oxygen content of blood containing 10 g of hemoglobin when the blood Po2 is 70 mmHg?
a. 13.6 mL/dL (vol%)
b. 9.5 mL/dL (vol%)
c. 6.8 mL/dL (vol%)
d. 21 mL/dL (vol%)
e. cannot be calculated from the information provided
e. cannot be calculated from the information provided
must know the percent hemoglobin saturation when pO2 is 70 mmHg to calculate
(O2 content= [Hb] x Hb saturation x O2 capacity per g)
CH 48, Q2: an increase in pH of blood will:
a. shift the oxyhemoglobin dissociation curve to the right
b. decrease P50
c. decrease the affinity of hemoglobin for oxygen
d. decrease the oxygen capacity of the blood
e. do all the above
b. decrease P50
CH 48, Q3: which of the following decreases oxygen content but does not alter PaO2 or percentage saturation of hemoglobin?
a. ascent to an altitude of 3500 m
b. polycythemia
c. breathing 50% oxygen
d. anemia
e. development of a large right-to-left shunt
d. anemia
CH 48, Q4: all the following shift the oxyhemoglobin dissociation curve to the right except:
a. an increase in pH
b. an increase in PCO2
c. an increase in 2,3-DPG
d. an increase in temperature
a. an increase in pH
CH 48, Q5: quantitatively, the most important form of carbon dioxide (CO2) in blood is:
a. HCO3- produced in plasma
b. CO2 dissolved in plasma
c. HCO3- produced in the erythrocyte
d. CO2 dissolved in the erythrocyte
e. CO2 combined with plasma proteins
c. HCO3- produced in the erythrocyte
CH 48, Q6: oxygenation of hemoglobin in the lungs assists with the release of CO2 from the blood because:
a. oxygen combines with the -NH groups on hemoglobin and displaces CO2 from carbamino compounds
b. oxygen combines with HCO3- and produces CO2
c. oxygen facilitates the movement of chloride ions out of the erythrocyte
d. oxygen combines with hemoglobin, making it a better buffer, which retains H+
e. none of the above
e. none of the above
CH 49, Q1: the rhythmicity of breathing is thought to originate in:
a. the carotid body
b. the central pattern generator
c. the central chemoreceptor
d. rapidly adapting pulmonary stretch receptors
e. none of the above
b. the central pattern generator
CH 49, Q2: which of the following receptors have afferent nerve fibers in the glossopharyngeal nerve?
a. carotid bodies
b. slowly adapting pulmonary stretch receptors
c. aortic bodies
d. intercostal stretch receptors
e. rapidly adapting pulmonary stretch receptors
a. carotid bodies
CH 49, Q3:which of the following statements correctly describes the carotid bodies?
a. carotid bodies can increase ventilation in response to low PaO2, but not in response to an increase in PaCO2
b. carotid bodies have a low blood flow/metabolism ratio
c. chemoreception is thought to occur in the sustenacular cells
d. carotid bodies are located near the bifurcation of the internal and external carotid arteries
e. all the above
d. carotid bodies are located near the bifurcation of the internal and external carotid arteries
CH 49, Q4: the retrotrapezoidal neurons:
a. are highly sensitive to increases in hydrogen ion concentration
b. receive inputs from the carotid body via the nucleus tractus solitarius
c. provide input to the central pattern generator
d. receive inputs from higher centers such as the hypothalamus
e. are described by all the above
a. are highly sensitive to increases in hydrogen ion concentration
CH 49, Q5: which of the following is correct concerning the role of PaCO2 in breathing?
a. PaCO2 exerts its effects on ventilation by changing the pH of brain interstitial fluid
b. PaCO2 has no effect on the carotid body
c. PaCO2 remains constant when hypoxia increases ventilation during the ascent to altitude
d. PaCO2 is much less important than PaO2 in the regulation of breathing
e. none of the above
a. PaCO2 exerts its effects on ventilation by changing the pH of brain interstitial fluid
CH 49, Q6: which of the following receptors are thought to initiate a cough in response to mechanical deformation of the airway?
a. juxtacapillary receptors
b. rapidly adapting stretch receptors
c. slowly adapting stretch receptors
d. intercostal tendon organs
e. none of the above
b. rapidly adapting stretch receptors
CH 50, Q1: particles greater than 5 μm in diameter are deposited in the respiratory tract by:
a. inertial deposition in small airways
b. sedimentation in airways
c. diffusion in the alveoli
d. inertial deposition in large airways
e. sedimentation in the alveoli
d. inertial deposition in large airways
CH 50, Q2: the mucociliary system:
a. consists of a gel layer in which cilia beat, overlaid by a sol layer that entraps particles
b. is restricted to the nasal cavity and trachea and does not extend into the bronchi
c. consists in part of mucus produced by goblet cells in the respiratory bronchioles and by Clara cells in the trachea
d. has a more rapid transport rate in the trachea than in the bronchioles
e. lacks ciliated cells in the bronchioles, so mucus must be pulled into the larger airways by viscous drag
d. has a more rapid transport rate in the trachea than in the bronchioles
CH 50, Q3: phagocytosis of inhaled particles:
a. is generally by type 2 aleovlar cells
b. can always be accomplished by alveolar macrophages
c. sometimes requires both macrophages and neutrophils
d. is accentuated by alveolar hypoxia
e. none of the above
c. sometimes requires both macrophages and neutrophils
CH 50, Q4: movement of fluid between pulmonary capillaries and lung lymphatic vessels:
a. does not occur in a normal animal
b. is accentuated by an increase in capillary hydrostatic pressure
c. is accentuated by an increase in capillary oncotic pressure
d. occurs by way of the alveolar surface
e. is facilitated by a positive pressure in the peribronchial spaces of the bronchovascular bundle
b. is accentuated by an increase in capillary hydrostatic pressure
CH 50, Q5: which of the following occurs as a result of enzymes localized on the pulmonary endothelium?
a. conversion of angiotensin 1 to angiotensin 2
b. conversion of angiotensin to angiotensin 1
c. release of renin
d. conversion of renin to angiotensin 2
e. none of the above
a. conversion of angiotensin 1 to angiotensin 2