Schizophrenia
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
what are the types of schizophrenia symptoms?
positive, negative, cognitive
symptom onset is usually in early adulthood
appear gradually over a period of 3-5 years
negative symptoms appear first, followed by cognitive then positive
positive symptoms
make themselves known by their presence (excess)
they include thought disorders, delusions and hallucinations
what are thought disorders?
disorganized, irrational thinking – probably the most important symptom of schizophrenia
great difficulty arranging thoughts logically, and sorting out plausible conclusions from absurd ones.
during conversation they jump from one topic to another as new associations come up.
sometimes utter meaningless words or choose words for rhyme rather than for meaning
what are delusions?
beliefs that are contrary to fact; there are many types:
persecution - false beliefs that others are plotting and conspiring against oneself
grandeur - false beliefs about one’s power and importance
control - related to persecution; the person believes that they are being controlled by others through radar or a radio receiver implanted in their brain
what are hallucinations?
perceptions of stimuli that are not actually present
most common are auditory but they can involve any of the other senses
olfactory hallucination are also fairly common and often contribute to the delusion that others are trying to kill them
negative symptoms
known by they absence or diminution of normal behaviours
cognitive symptoms
include:
difficulty in sustaining attention
low psychomotor speed
deficits in learning and memory
poor abstract thinking
poor problem solving
cognitive symptoms in the brain
all neurocognitive deficits are associated with frontal lobe hypofunction
Weinberger (1988) suggested that the negative symptoms of schizophrenia are caused primarily by hypofrontality, decreased activity of the frontal lobes, the dlPFC in particular
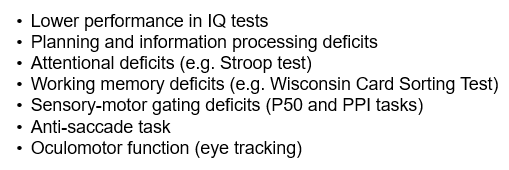
the stroop task
involves naming the colour of the ink in two conditions: congruent and incongruent
schizophrenia patients are slower and less accurate
the Wisconsin card sort test
normally during the task there is an increase in regional blood flow to the dlPFC
not seen in schizophrenia patients
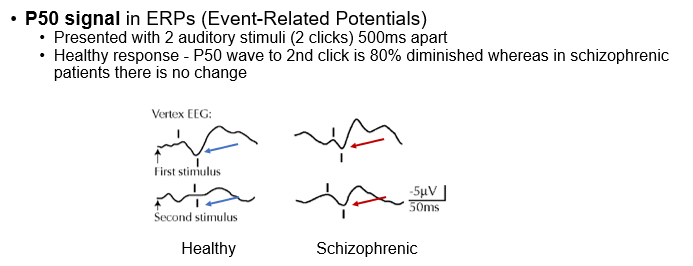
sensory-motor gating deficits
difficulties screening out irrelevant
pre-pulse inhibition (PPI)
when a weak stimulus precedes a startle stimulus by approx. 100ms, the normal response is to inhibit the startle
people with schizophrenia do not inhibit the startle
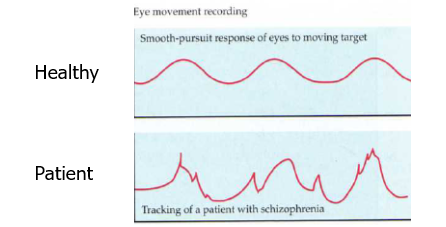
oculomotor function
smooth pursuit - tracking a moving stimulus
the eye movements of schizophrenia patients are not smooth compared to controls
structural differences
Weinberg and Wyatt (1982) - CT scans of schizophrenics and healthy controls of the lateral ventricles
the relative ventricle size of the schizophrenic patients was more than twice as big as that of normal control subjects
reduced brain volume (less grey matter) in temporal, frontal lobes and hippocampus
faulty cellular arrangement in the cortex and hippocampus
heritability and genetics
adoption and twin studies indicate that schizophrenia is a heritable trait but is not due to a single dominant or recessive gene
having a “schizophrenia gene” causes a susceptibility to develop schizophrenia which may be triggered by environmental factors
genetics of schizophrenia
one rare mutation involves a gene called DISC1 (disrupted in schizophrenia 1)
involved in the regulation of neurogenesis, neuronal migration, postsynaptic density in excitatory neurons, and mitochondria function
appears to increase the chance of schizophrenia by a factor of 50
paternal age
the children of older fathers are more likely to develop schizophrenia
most likely due to mutations in the spermatocytes
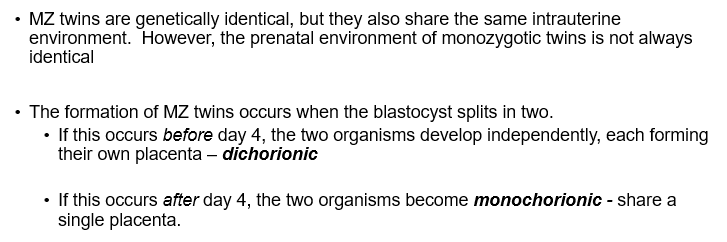
twins studies
the concordance rate for monochorionic MZ twins was found to be 60% vs 32% in dichorionic MZ twins
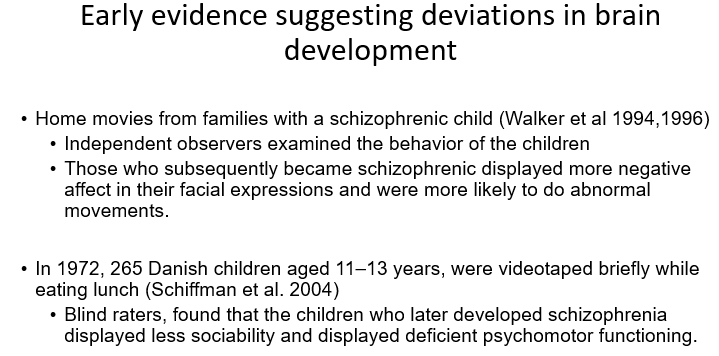
the ‘early’ neurodevelopmental model
Events in early life (prenatally) cause deviations from normal neurodevelopment and these lie dormant until the brain matures sufficiently to call into operation the affected systems (Murray & Lewis, 1987)
Early events such as infections, obstetric complications, nutritional deficiencies etc. provide evidence in support of this theory
the ‘late’ neurodevelopmental model
schizophrenia may result from an abnormality or deviation in adolescence when synaptic pruning takes place
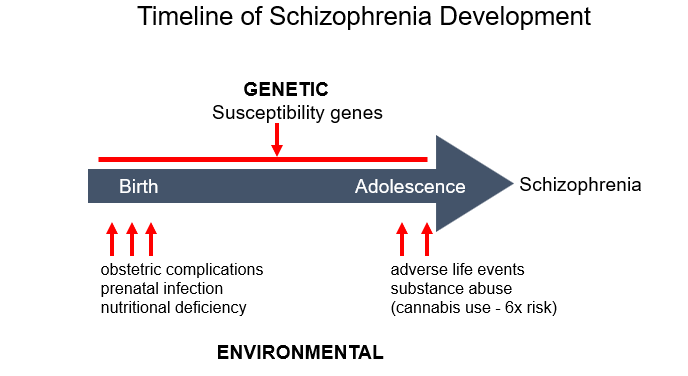
‘two-hit’ model
atypical development in schizophrenia takes place during 2 critical time points: early brain development and adolescence
early developmental insults may lead to dysfunction of specific neuronal networks that would account for premorbid signs
during adolescence, excessive synaptic pruning and loss of plasticity may account for the emergence of symptoms
the dopamine (DA) hypothesis
Proposes the schizophrenia is caused by abnormalities in DA functioning in the brain
Overactivity of DA in the mesolimbic system results in the positive symptoms of schizophrenia
Underactivity of DA in the mesocortical system results in the negative and cognitive symptoms of schizophrenia
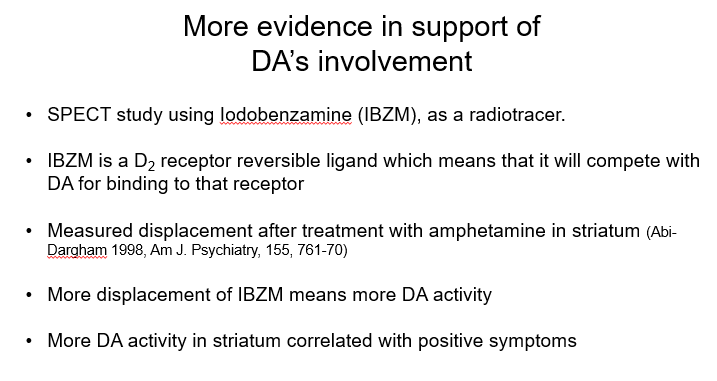
DA agonists induce psychosis (evidence for DA hypothesis)
DA agonists produce symptoms that resemble the positive symptoms of schizophrenia.
These drugs include amphetamine, cocaine, methylphenidate and L-DOPA.
The symptoms that they produce can be alleviated with antipsychotic drugs
strengthens the argument that the antipsychotic drugs exert their therapeutic effects by blocking DA receptors
DA antagonists (evidence for the DA hypothesis)
Henri Laborit (mid 20thce): French surgeon who discovered that a drug used to prevent surgical shock also reduced anxiety
A related compound called chlorpromazine (CPZ) was developed in 1952 which had dramatic effects on schizophrenia.
CPZ is a DA antagonist – first antipsychotic
antipsychotic drugs (evidence for the DA hypothesis)
Since the discovery of CPZ, many drugs have been developed for the treatment of schizophrenia – typical antipsychotics
Two major families of DA receptors:
D1-type family (Gs coupled): D1 & D5
D2-type family (Gi coupled): D2, D3, D4
These drugs have one property in common: They block D2 receptors
treatment with typical antipsychotics
these drugs eliminate/diminish the positive symptoms in most of the patients (about 20-30%) do not respond to these drugs
long-term treatment leads to at least some symptoms resembling those in Parkinson’s disease - slowness in movement, lack of facial expression and general weakness
a more serious side effect develops in approx. 1/3 of all patients who took the drugs for an extended period - tardive dyskinesia (unable to stop moving)
newer drugs - treatment with atypical antipsychotics
they work in treatment-resistant patients
atypical do not have the Parkinsonian side-effects due to their lower affinity for the D2 receptors
improve both positive and negative symptoms of schizophrenia
also improve the performance in neurotypical tests which is not the case with typical antipsychotics
clozapine
first of the atypical antipsychotic drugs
Has lower affinity for D2 and higher affinity for other DA receptors (D3, D4 and even 5HT)
Although it is highly effective it is still not widely used – despite international consensus to use it when other drugs have failed
The only antipsychotic to reduce suicide rates in schizophrenics
Still considered to be tricky due to its side effects: weight gain, sedation, hypersalivation, tachycardia, hypotension, neutropenia etc
problems with the dopamine hypothesis
It explains only a part of schizophrenia (positive symptoms not negative symptoms)
Atypical antipsychotic drugs e.g. Clozapine (with weaker anti-dopaminergic activity) are better antipsychotics
Negative symptoms are caused by under-activity in the mesocortical dopamine pathway
So, dopamine underactivity is the problem rather than dopamine overactivity
the glutamate hypothesis of schizophrenia
glutamate is the major excitatory neurotransmitter in the central nervous system and the most prevalent one
many neurons in the brain use glutamate as their neurotransmitter
In mammalian brains, glutamate is balanced with GABA (main inhibitory chemical transmitter)
Both neurotransmitters influence almost every other chemical and brain area
Evidence implicates NMDA receptors in schizophrenia
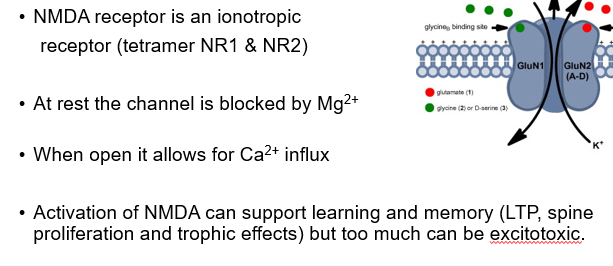
NMDA and schizophrenia
NMDA receptors comprise a critical component of development processes which include:
•Development of neural pathways
•Neural migration
•Neural survival
•Neural plasticity
•Neural pruning of cortical connections
•Apoptosis
glutamate hypo-functioning hypothesis (Olney and Farber, 1995)
Schizophrenia is due to NMDA receptor hypofunction which may explain:
Why there are so many treatment-resistant negative symptoms
Why the onset is in early adulthood
Why the disorder is associated with structural changes and cognitive deficits.
evidence for the glutamate hypo-functioning hypothesis
The drugs Phencyclidine (PCP, also known as “angel dust”) and ketamine (“Special K”), can cause positive, negative, and cognitive symptoms of schizophrenia
Both of them are NMDA receptor antagonists
Glutamate agonists seem to improve both positive and negative symptoms of schizophrenia
Evidence in support from animal genetic studies with NMDA receptor subunits as well as GWAS
positive and negative symptoms: role of the PFC
The negative and cognitive symptoms produced by ketamine and PCP are caused by a decrease in the metabolic activity of the frontal lobes.
Jentsch et al. (1997) administered PCP to monkeys twice a day for two weeks.
A week later, tested the animals on a task that involved reaching around a barrier for a piece of food
Performance depends on the function of the PFC (animals with lesions of the PFC perform poorly).
Control monkeys performed well, but those treated with PCP showed a severe deficit
hypo-functioning NMDA receptors theory
This theory is more comprehensive - it can explain the positive, negative & cognitive symptoms of schizophrenia
It accounts for the lack of effectiveness of DA antagonists in treating schizophrenia
Hypo-functioning NMDA receptors can account for both the excessive DA release in the mesolimbic DA system as well as the reduced release of DA in the prefrontal cortex
microglial activation and schizophrenia (neuroinflammatory hypothesis of schizophrenia)
The brain’s immune cells are hyperactive in people who are at risk of developing schizophrenia
Many animals studies show a link between pro-inflammatory agents and schizophrenia symptoms
The symptoms are reversed upon treatment with antipsychotics or treatment with antibiotics that reduce microglial activation
Support the evidence for prenatal or perinatal infection and the increased risk for schizophrenia
recent genome-wide association studies of schizophrenia
Identified 100+ genetic loci that contribute to schizophrenia risk.
The dopamine-receptor gene, DRD2, GLU receptor subunits etc are associated with risk of schizophrenia
Most significant association is on chromosome 6 which includes a region of genes involved in acquired immunity (major histocompatibility complex - MHC)
microglia
In healthy conditions they are in a ramified state and survey the brain for pathogens or debris
Upon identification of a threat they become activated (amoeboid morphology)
Their function goes beyond the immune system – involved in a range of homeostatic functions in a healthy brain such as:
•Neuronal cell death and survival
•Synaptogenesis
•Synaptic pruning etc
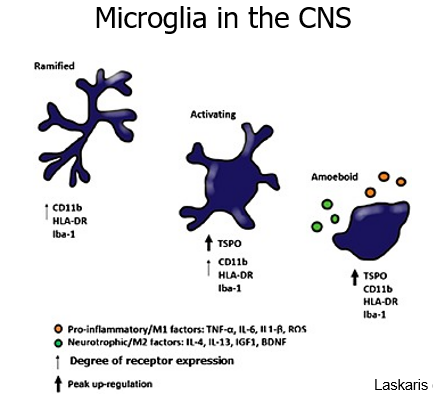
microglial activation and schizophrenia in animal studies
microglial activation is not instantaneous in response to infectious agents
a pre- or perinatal infection primes microglia and this priming may interact with cells in the developing nervous system
may lead to subtle rearrangement of synaptic circuitry resulting in behavioural impairment in adolescence
oestrogen hypothesis of schizophrenia
Estrogen is the primary “female” sex hormone with 17β-estradiol being the most potent form
17β-estradiol is secreted mainly by the ovaries, fat, breasts and the brain (neuroprotective effect)
In women there is a 2nd peak onset of schizophrenia at age 45-50y (menopause)
Estrogen seems to play a protective role against the development of schizophrenia (buffer)