NSG 212 - Exam 2 KW
1/187
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
188 Terms
factors influencing diffusion of gases (O2-CO2)
Factors Influencing Diffusion(Diffusion is gas exchange)
Change in surface area
-Removal of the lung
-Atelectasis
-Collapse of the alveoli… Prevents the exchange of gas by diffusion in the lungs…
Thickening of the membrane
-Pneumonia (lung infection)
-Pulmonary edema
Partial pressure change
-Decrease in environmental oxygen…high altitudes, lack of 02
Solubility and molecular weight of the gas
physiological factors that may increase or decrease respiration
Rate and depth of respirations
-Increase rate/depth in the presence of low 02 or high C02
-Respiratory center; in the medulla of the brain; stimulated by an increase of CO2 and by decreased 02 ( lesser degrees)
Chemoreceptors in the aortic arch and the carotid arteries are sensitive to change in blood gas levels and blood pressure and can activate the medulla to increase the rate/ depth of respirations.
chemoreceptors
sensitive to oxygen saturation
-aortic arch
-carotid arteries
-in response to low oxygen they will increae respirations
medulla (CNS)
triggered to control respirations
rate and depth of respirations
increase rate/depth in the presence of low O2 or high CO2
apnea
absence of breathing
=no respirations
orthopnea
difficulty breathing when lying down
=try to sleep sitting up

dyspnea
difficult or labored breathing
-change positions
-sit up first prior to putting oxygen on
-lowers the diaphragm and makes it easier to breath

main organs of respiration
-Lungs
-extend from the base of the diaphragm to the apex above the first rib.
-the right lung has 3 lobes and the left lung has 2.
contributing factors for alterations in the Cardiovascular system
Dysrhythmia or arrhythmia
-Something other than “lub-dub”…Problem with electrical signals; SA node
Myocardial ischemia
-Decreased oxygen supply to the heart…MAIN cause of a heart attack (MI)
Angina
-Coronary Artery Vasoconstriction; decreased oxygen= muscle pain=chest pain
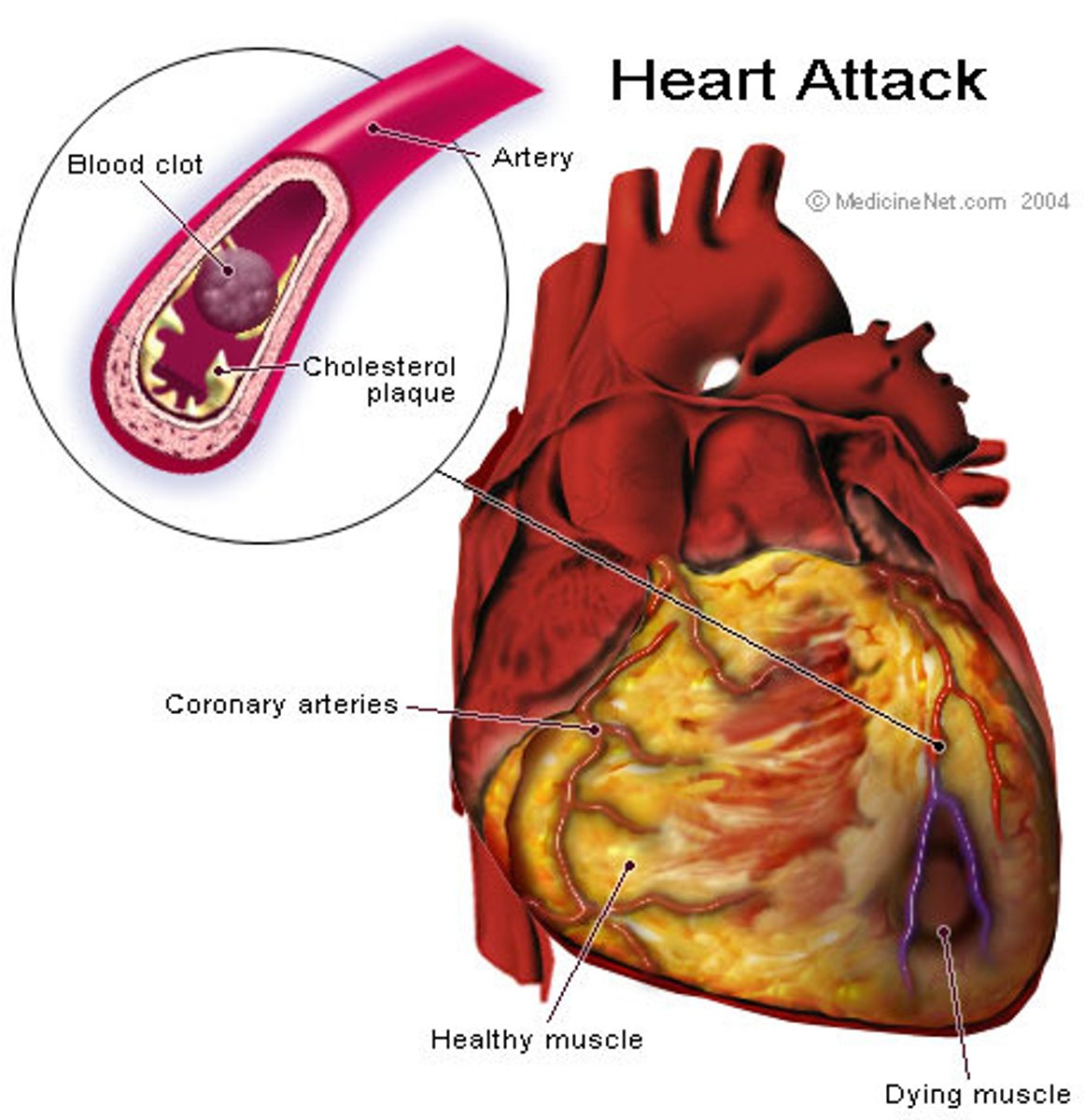
Myocardial Infarction (MI)
-Heart Attack…Caused by lack of oxygen to a part of the heart (blockage)
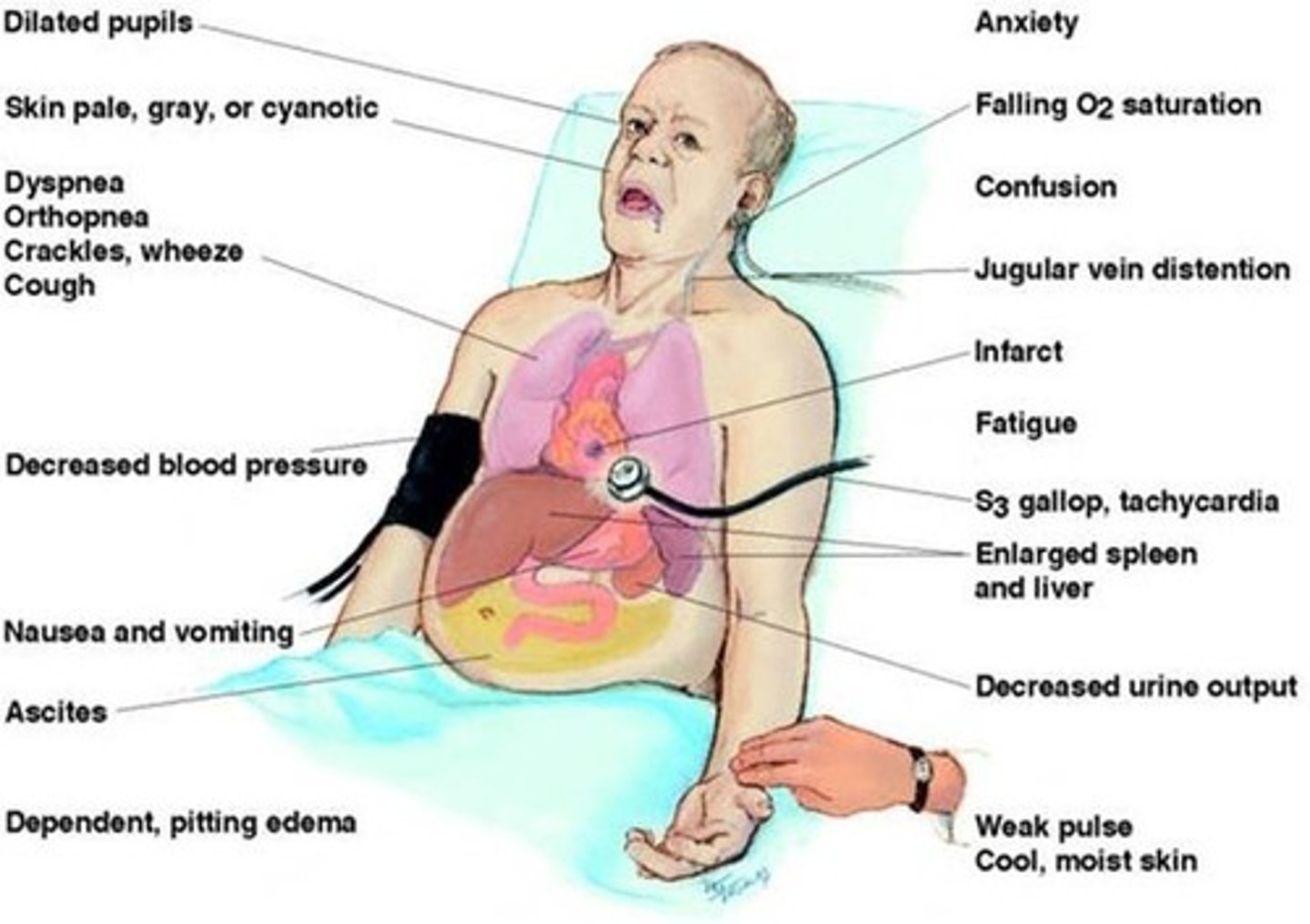
Heart Failure (Congestive Heart Failure [CHF])
-Failure of the Left Ventricle to pump…Back up of blood into the lungs…Heart AND Lung problem
Dysrhythmia or arrhythmia
disturbance of heart rhythm
-something other than "lub-dub"
-problem with electrical signals;SA node
myocardial ischemia
Lack of oxygen to the heart muscle
-decreased oxygen supply to the heart
=Main cause of a heart attack (MI)
angina
muscle pain=chest pain
-coronary artery vasoconstriction; decreased oxygen

myocardial infarction (MI)
heart attack
-caused by lack of oxygen to part of the heart(blockage)
heart failure
Congestive Heart Failure (CHF)
-failure of the left ventricle to pump
-back up of blood into the lungs
-heart and lung problem
cardiopulmonary developmental changes across the lifespan
?
factors affecting cardiopulmonary function and oxygenation
Level of health
-Other chronic illnesses
Developmental considerations
-Lifespan
Medication considerations
-Opioids decrease respiratory drive
Lifestyle considerations
-Occupation, smoking
Environmental considerations
-Pollution
Psychological health considerations
-Stress, hyperventilation
cillia
Tiny hairlike extensions that move together in a sweeping motion
alveoli
air sacs in the lungs
surfactant
a phospholipid that reduces the surface tension in the alveoli and prevents them from collapsing
parietal pleura
lines the thoracic cavity
visceral pleura
covers the lungs
pleural space
located between the parietal and visceral pleura-contains pleural fluid that acts as lubricant to assist in respirations
friction rub
a coarse, grating, adventitious lung sound heard when the pleurae are inflamed
inspiration
breathing in
-active phase of ventilation
expiration
breathing out
-passive phase of ventilation
how is oxygen carried?
via plasma and red blood cells
hypoxia
-Low oxygen saturation of the body, not enough oxygen in the blood
-can be caused by hypovolemia, hypoventilation, and interruption of arterial flow
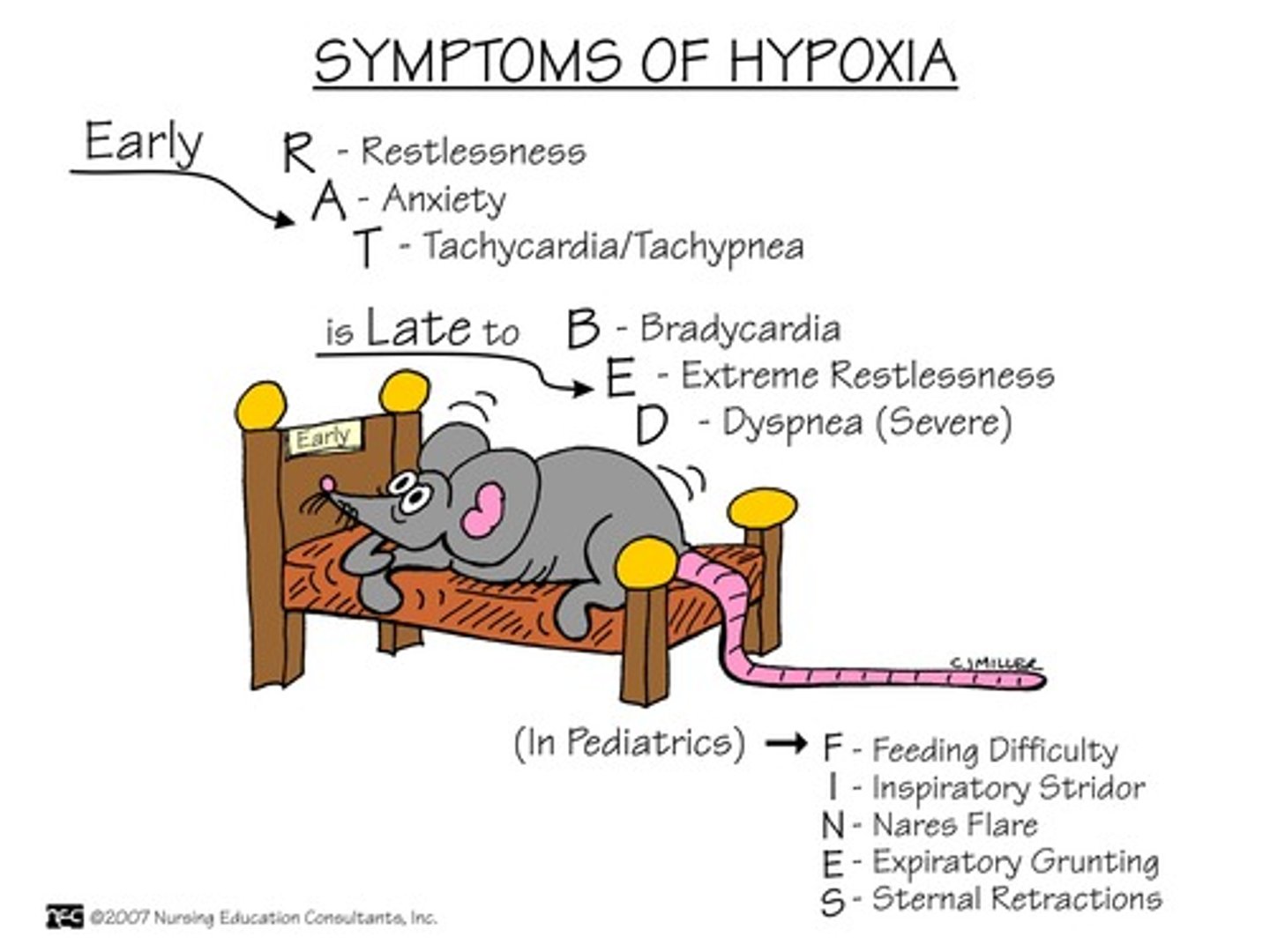
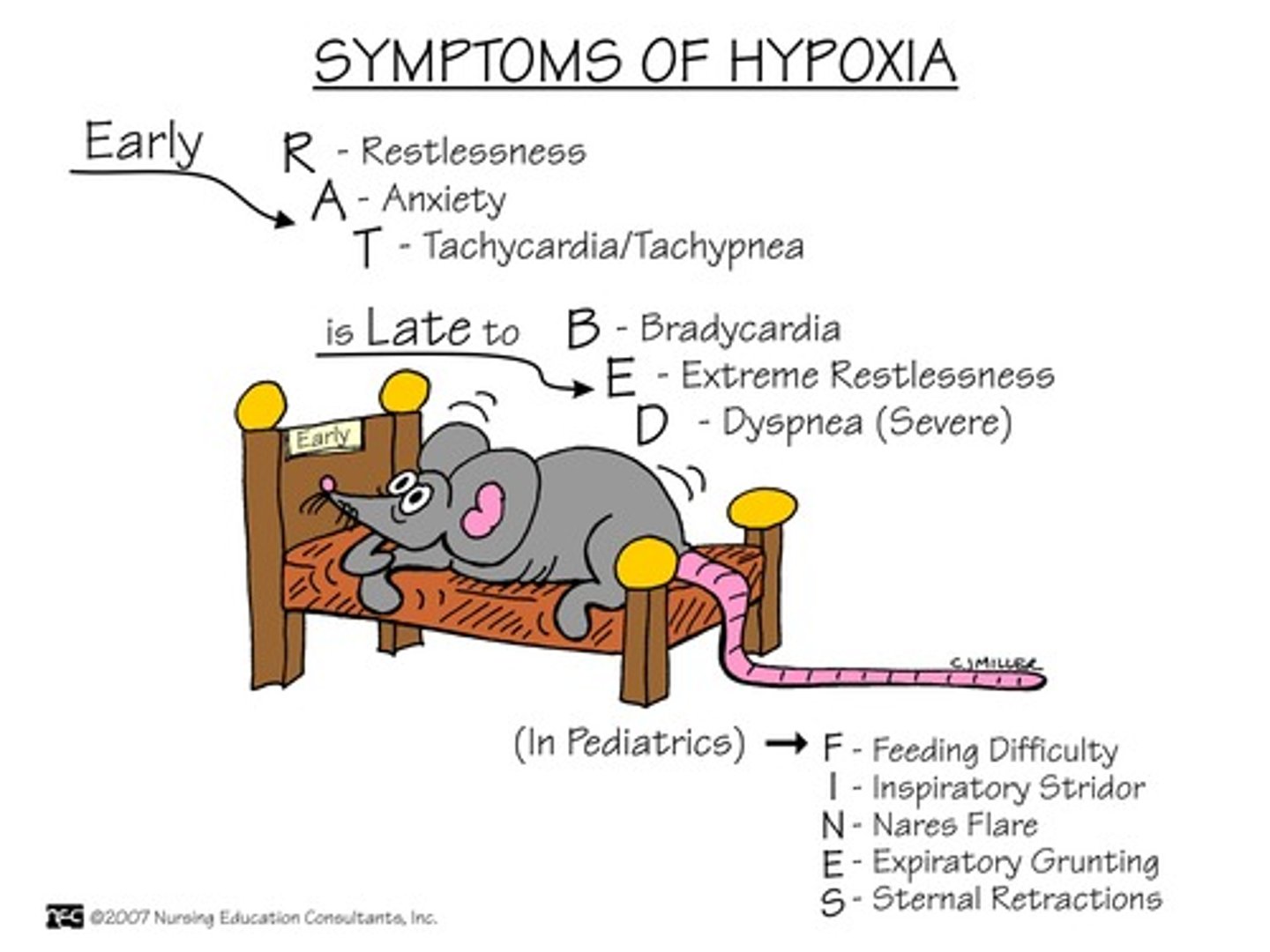
early hypoxia s/s
S/S of Early:
-Tachypnea
-Tachycardia
-Restlessness (ENGAGE)
-Pallor
-Increased BP
-Use of accessory muscles
-Nasal flaring
-Tracheal tugging
-Adventitious lung sounds
-Dyspnea
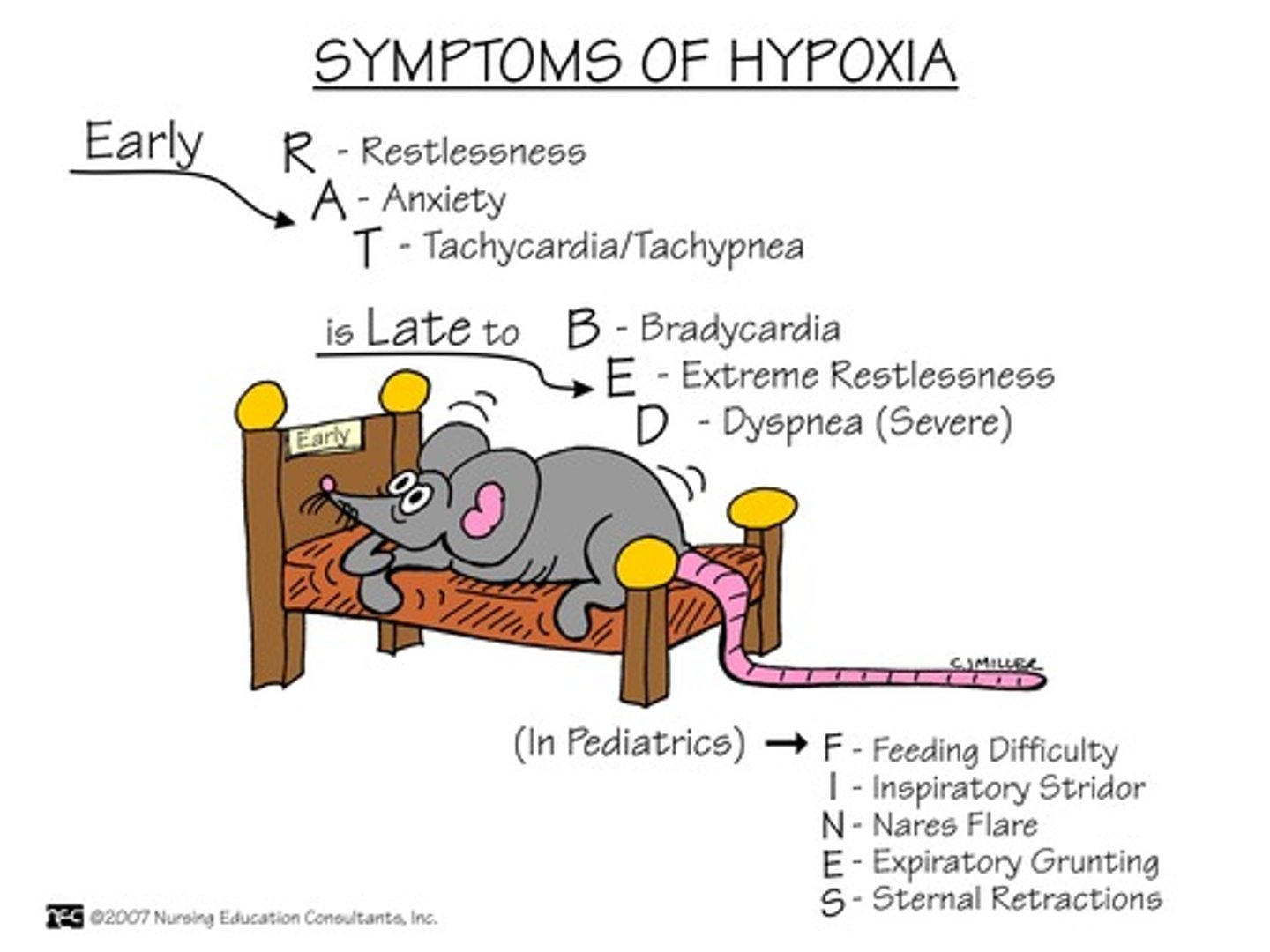
late hypoxia s/s
S/S of LATE:
-Bradypnea
-Bradycardia
-Confusion and stupor,
-Cyanosis
-Hypotension
-Cardiac arrhythmias
-Metabolic acidosis
hypoventilation
decreased rate or depth of air movement into the lungs
-acute disease
-can cause hypercarbia(high CO2)
s/s
-restlessness
-HT
-headache
chronic hypoxia
-live in a state of low oxygen due to disease process
s/s
-Headaches
-Chest pain
-Enlarged heart
-Clubbing the of fingers/toes
-Anorexia
-Constipation
-Decreased urine output
-Weakness
-Muscle pain
-Right sided heart failure
-Respiratory acidosis
safe oxygen administration
Delivered via nasal cannula:
-1 liter 24 %
-2 liters 25 %
-3 liters 32 %
-4 liters 36 %
-5 liters 40 %
-6 liters 44 %
-Humidification 3-4 Liters
Oximizer
high flow nasal cannula

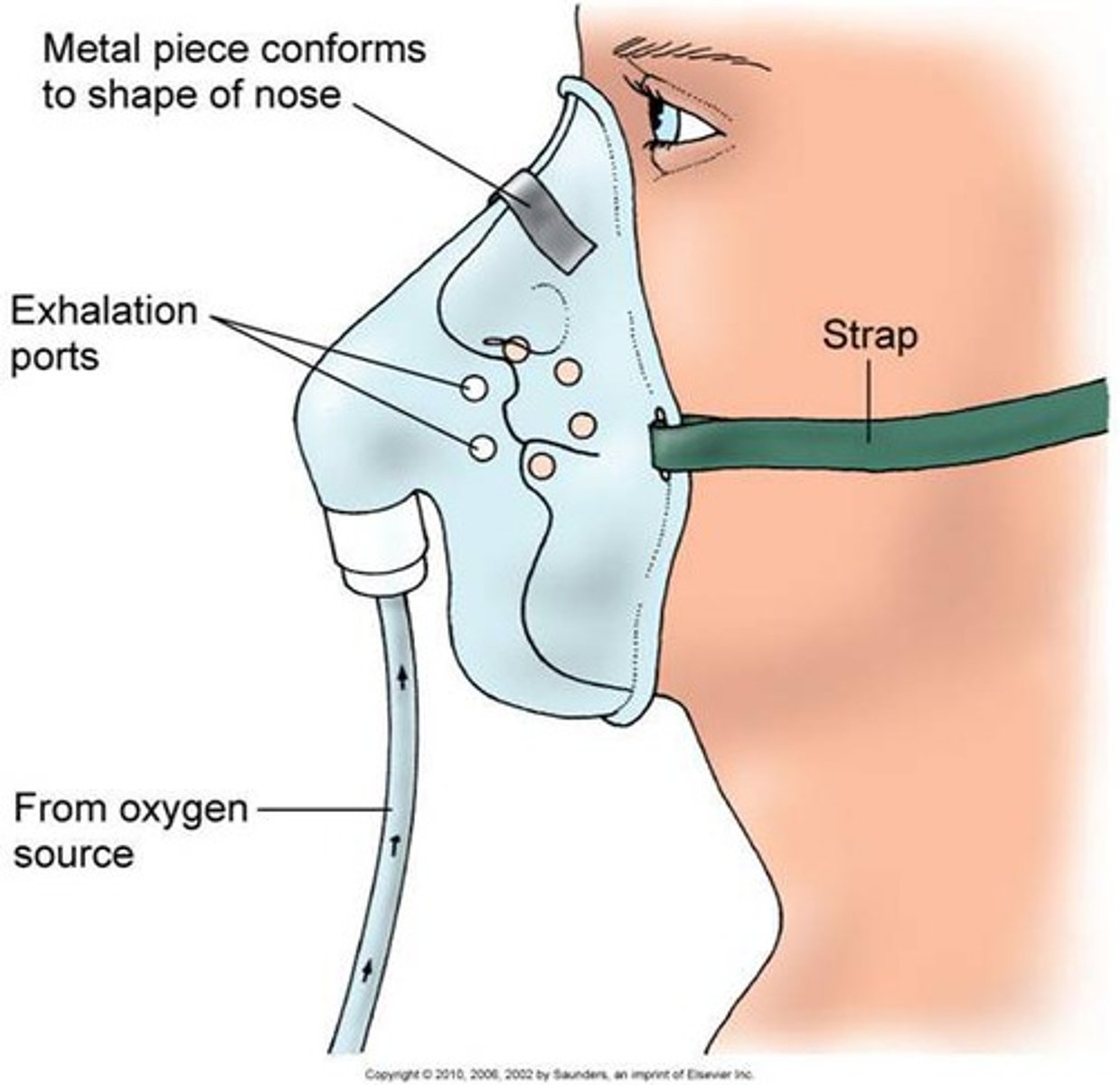
simple mask
40-60% of oxy, 5-8 liters/min
-never less than 5 L or CO2 build up can occur
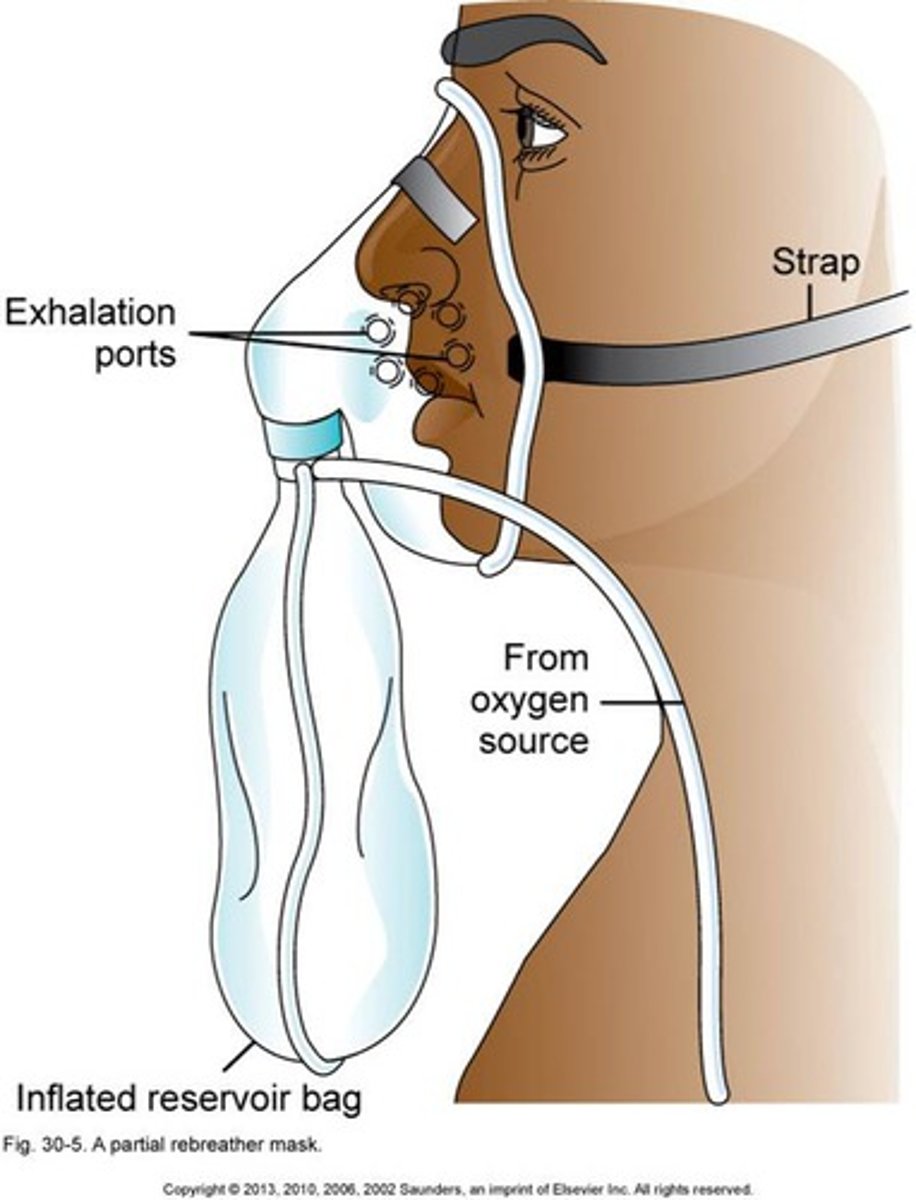
partial rebreather
60-75% at a flow of 6-11 liters/min
-1/3 of expired air from exhaled breath
-bag should stay 2/3 full, complete deflation of the bag during inspiration can cause CO2 build up

non rebreather
80-95% except for intubation; flow of 10-15 liters/min
-Non-rebreather means they are NOT REBREATHING any of their CO2.
-That means that what they ARE breathing in is almost 100% oxygen.
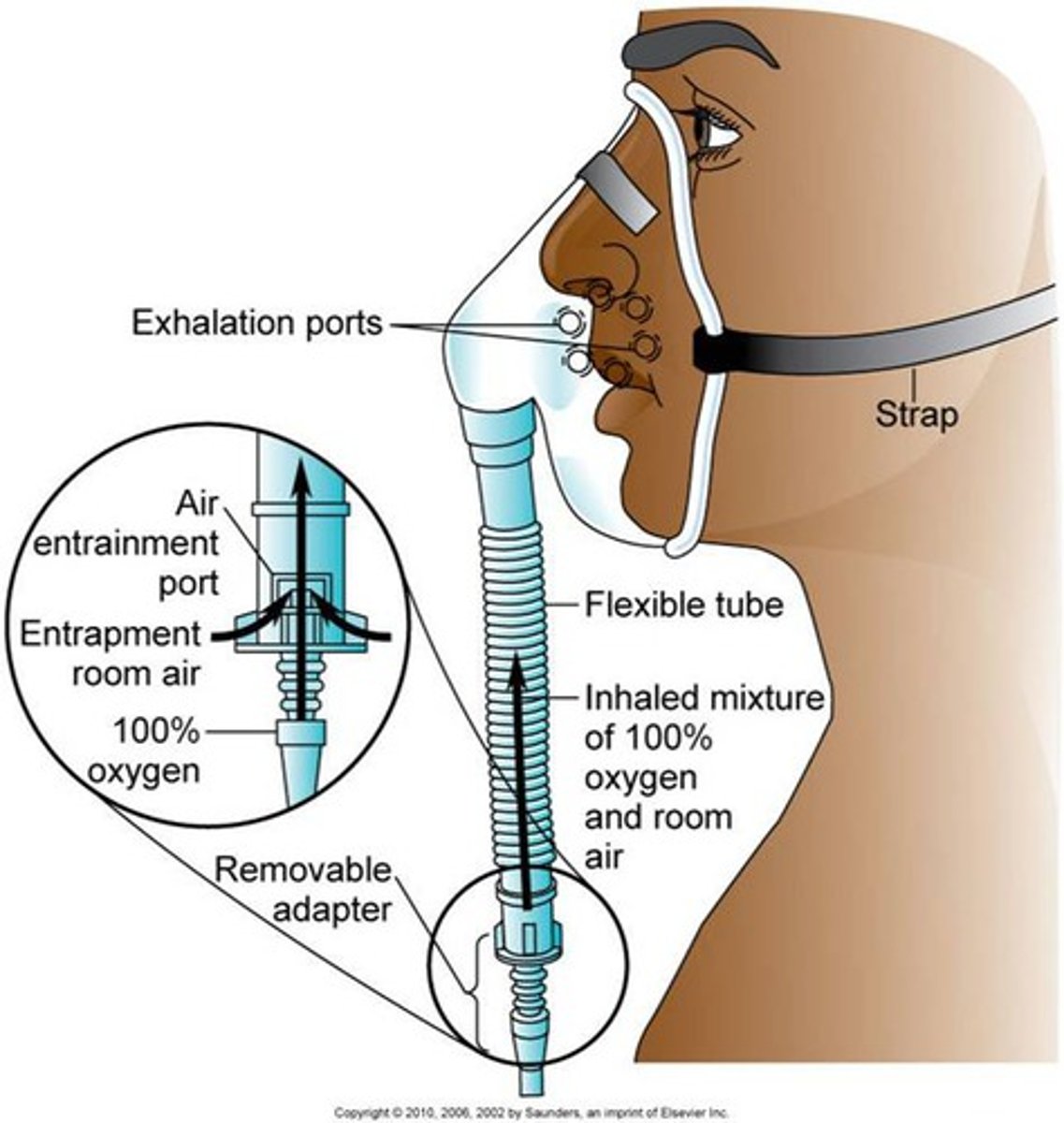
venturi mask
delivers precise amount of O2
-used to prevent oxygen toxicity in pts with COPD
aerosol mask/face tents
fits loosely around the face and neck
oxygen is
combustible
no high levels for
COPD pts
-drive to breath is LOW oxy
oxygen induced hypoventilation
-May occur in COPD patients who have chronic low oxygen (hypoxemia) AND hypercarbia(high CO2)
-This may eliminate their drive to breath! NOT GOOD!
-S/S…Decreased RR rate, decreased LOC
-They may look like they are “sleepy”…But you are actually knocking out their drive to breath.
-NOT GOOD!
-Stay with the patient!
-Need to lower their oxygen delivery!
oxygen toxicity s/s
S/S:
-Nonproductive cough
-Substernal pain
-Nasal stiffness
-Nausea
-Vomiting
-Fatigue
-Headache
-Sore throat
-Hypoventilation
oxygen toxicity interventions
Interventions:
-Use the LOWEST setting of oxygen to maintain adequate O2 sat.
-Monitor ABG’s…Check to make sure SAO2 are adequate for disease process.
-DC oxygen as soon as possible.
-Monitor for s/s of respiratory distress.
-Monitor LOC.
-Notify MD if assessing s/s of respiratory depression.
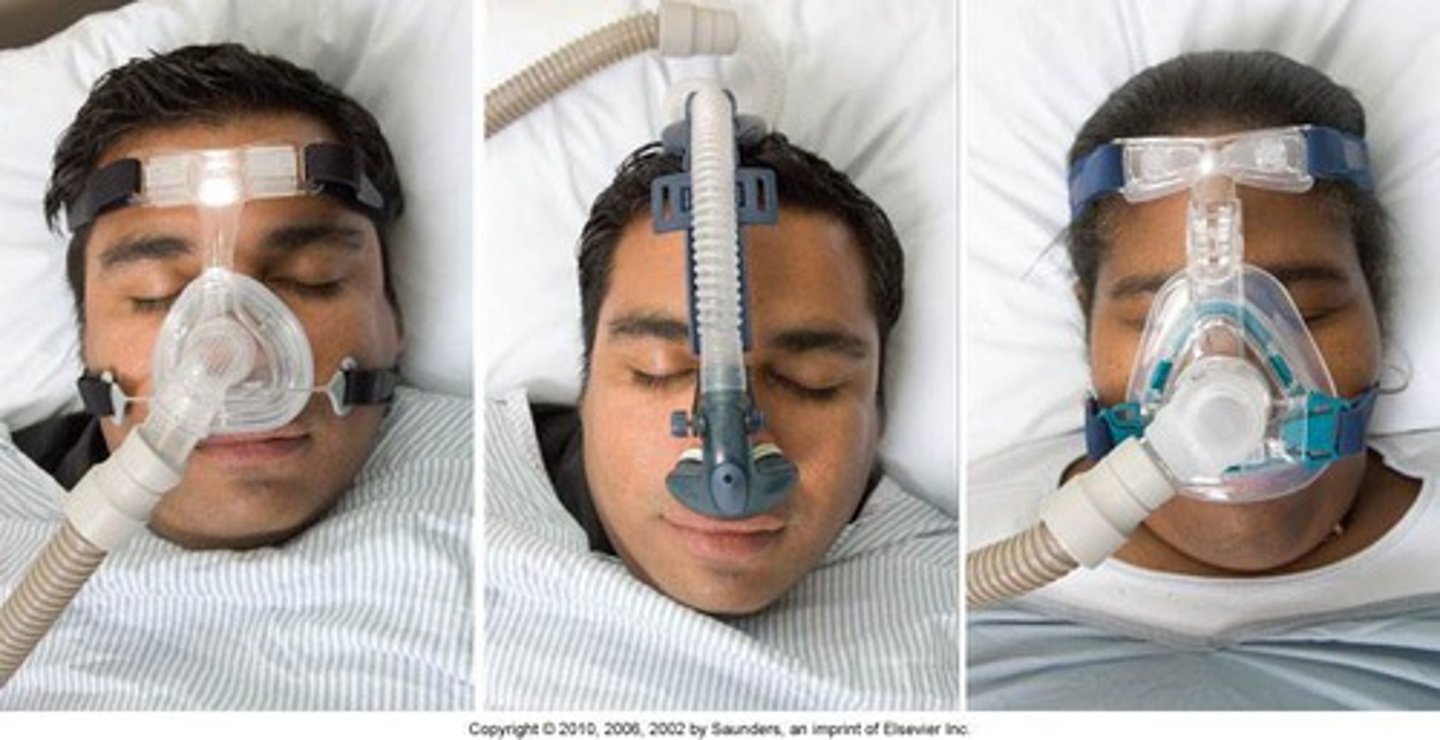
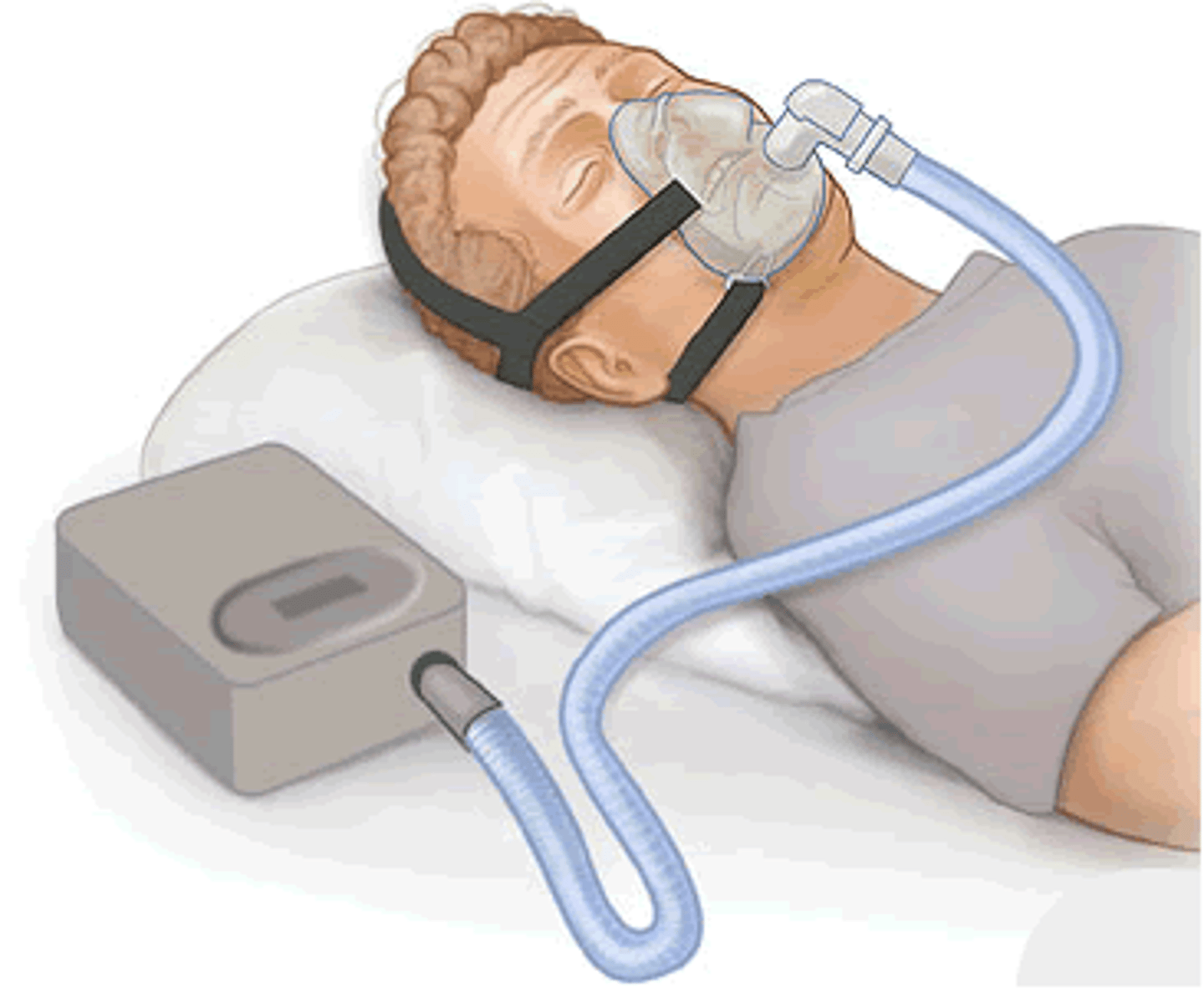
continuous positive air pressure (CPAP)
prevents upper airway collapse

bi-level positive air pressure (BiPAP)
-increases the amount of air in the lungs
-improves oxygen
precautions for oxy administration
-Avoid open flames in the patient's room.
-Place "no smoking" signs in conspicuous places.
-Check to see that electrical equipment in the room is in good working order.
-Avoid wearing and using synthetic fabrics (builds up static electricity).
-Avoid using oils in the area. (Oils ignite spontaneously in oxygen.)
Chest physiotherapy (PT)
Performed to loosen thick secretions and facilitate drainage from the lungs
-Percussing, vibrating, and postural drainage (all three = chest PT)
-Done to facilitate respiratory function
-Help patients to breath deeply and cough
-Need a MD order
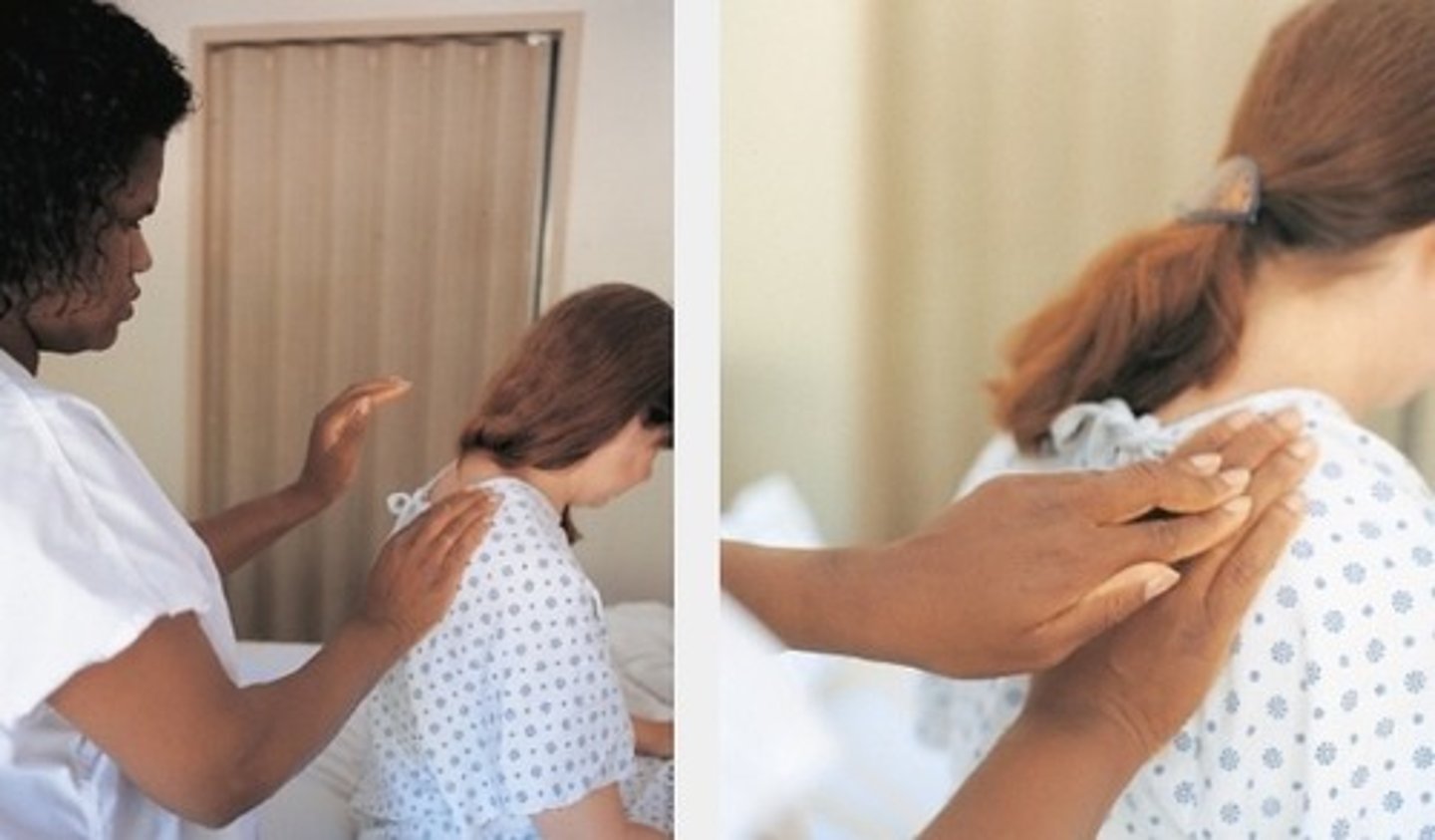
percussion
-Percusssion is the manual striking of the chest with alternating cupped hand, mechanical percussion cups or a vibrator;
-Move from the lower ribs to the shoulder in back and from the lower ribs to the top of the chest in the front.. Helping to move secretions UP!
-Also called clapping or cupping
-Form hand as if to scoop water
-Rapidly, not forcefully, strike the chest
-Percuss each affected lung segment for 30-60 seconds up to 3-5 minutes for viscous secretions. Done multiple times a day.
-Have them take slow deep breaths.
-Do NOT percuss on bare skin.
-Do NOT percuss over spine, breasts, or below the ribs.
vibrating
-Done to increase the turbulence of the inhaled air, aid in the expectoration of fluids,
Series of vigorous quivering or fine, shaking pressure, produced by the contracting and relaxation of the arm and shoulder while holding the hands flat against the patients chest wall
-DO NOT vibrate over spine, breasts, sternum or below the ribs
-Place hands on chest wall, side by side or one on top of the other.
-Have them inhale deeply and exhale slowly.
-As they exhale, rapidly vibrate hands.
-Stop vibrating when they inhale.
-Try for 200 vibrations/min.
-5 cycles over each lung segment.
secretions from upper lobe
high fowlers position
drains posterior lobes
side lying
drains right lobe
left side
lower lobes
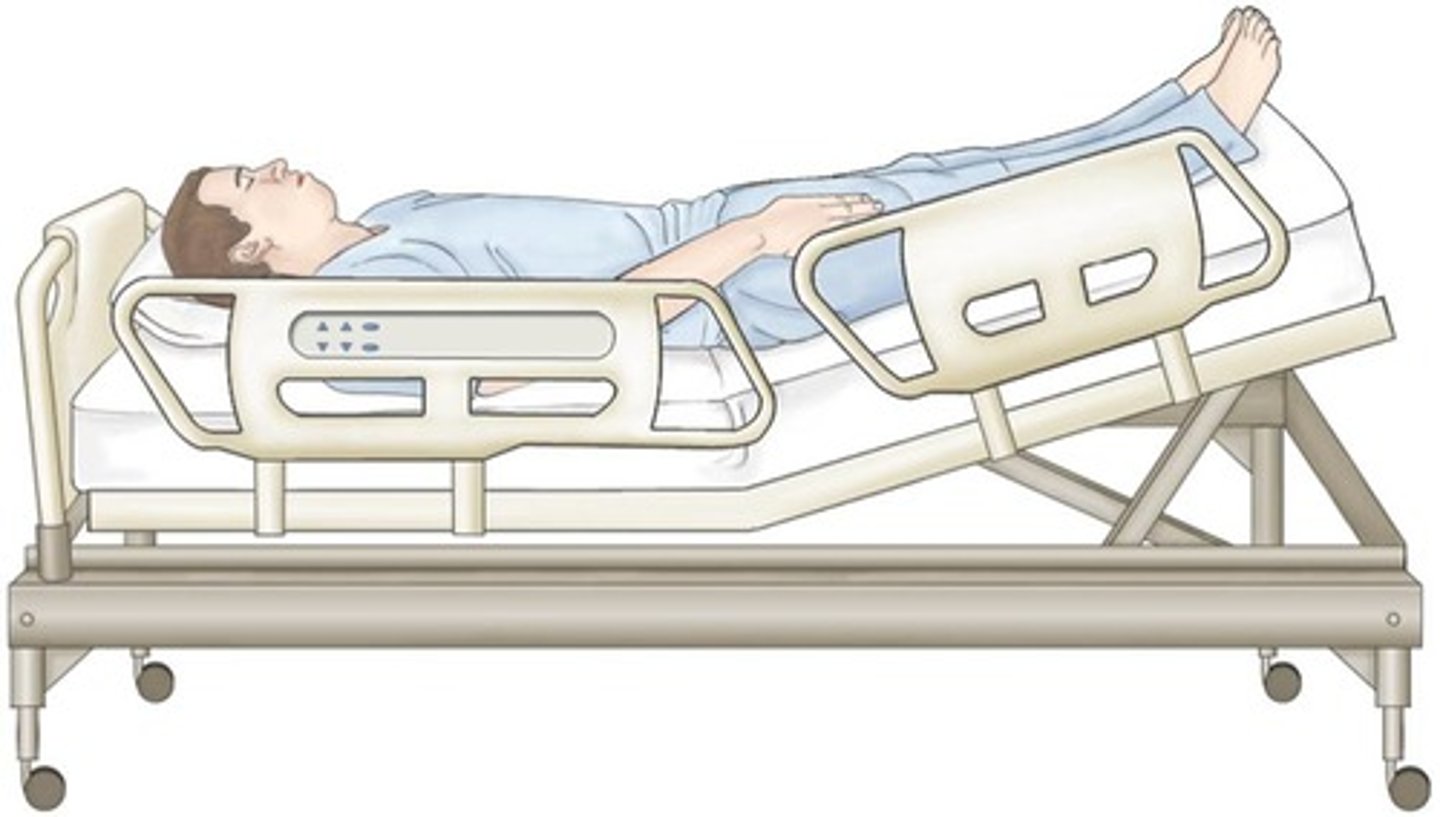
trendelenberg position
contraindications in postural drainage
-Early morning is best to assist with nighttime secretions.
-Assess pre-post to determine effectiveness.
-Usually done 3-4 times a day; schedule 1 hour before meals or 2 hours after meals.
-Administer bronchodilator 30 min-1 hour before to help with drainage.
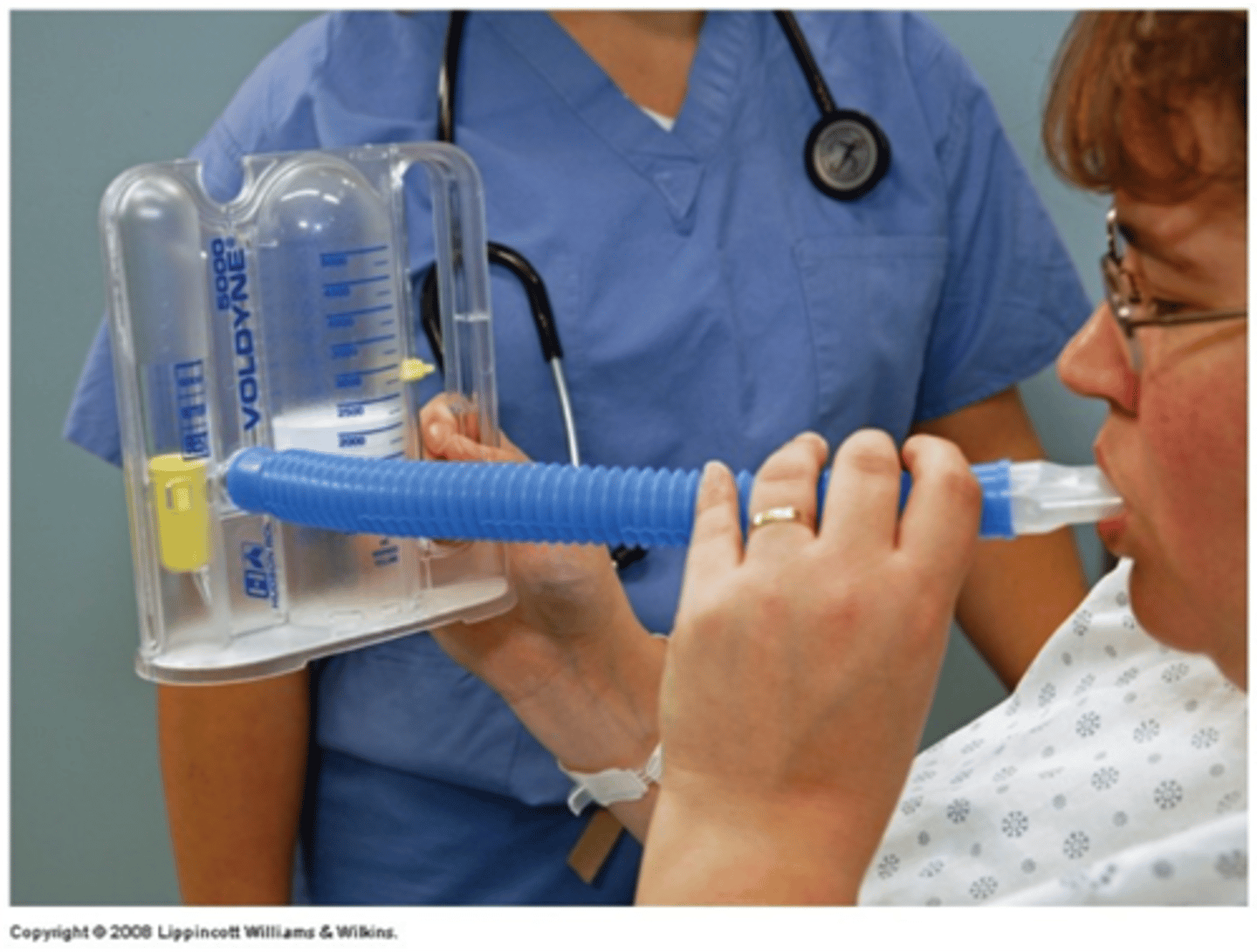
incentive spirometry
-Patients should place the device in their mouth and slowly INHALE.
-Sitting in Fowler's position
-Keep the ball between the lines
-Slowly inhale
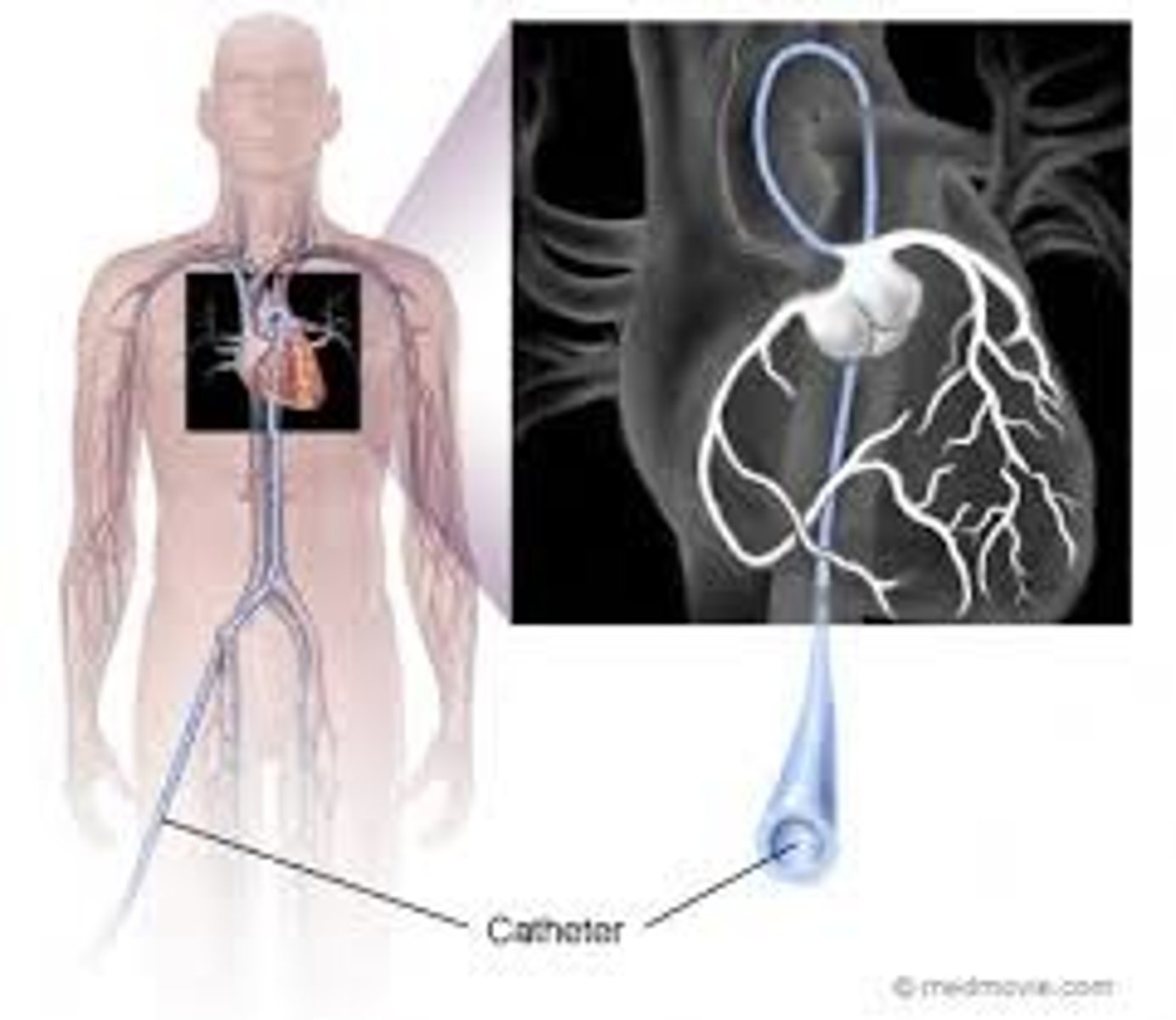
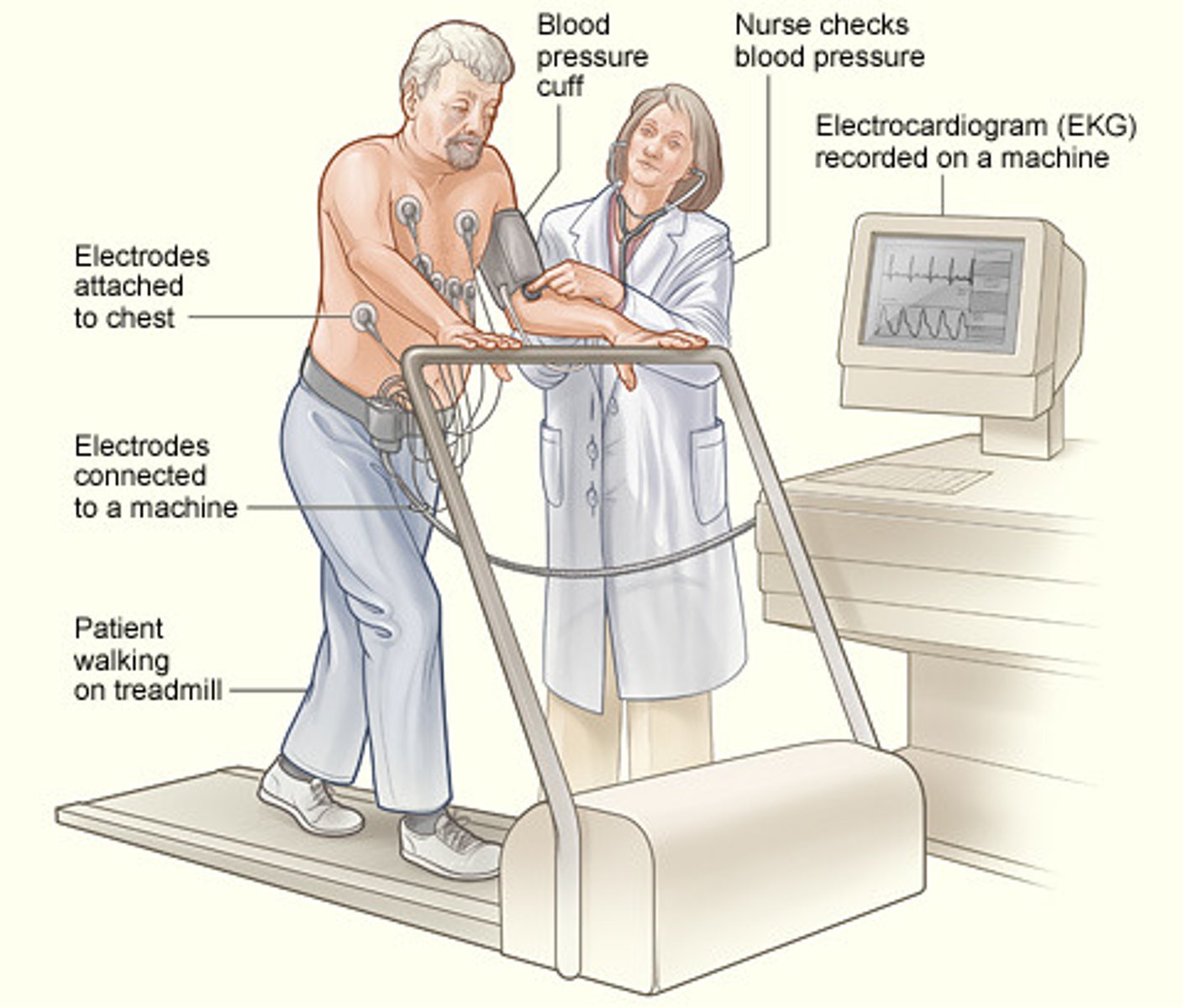
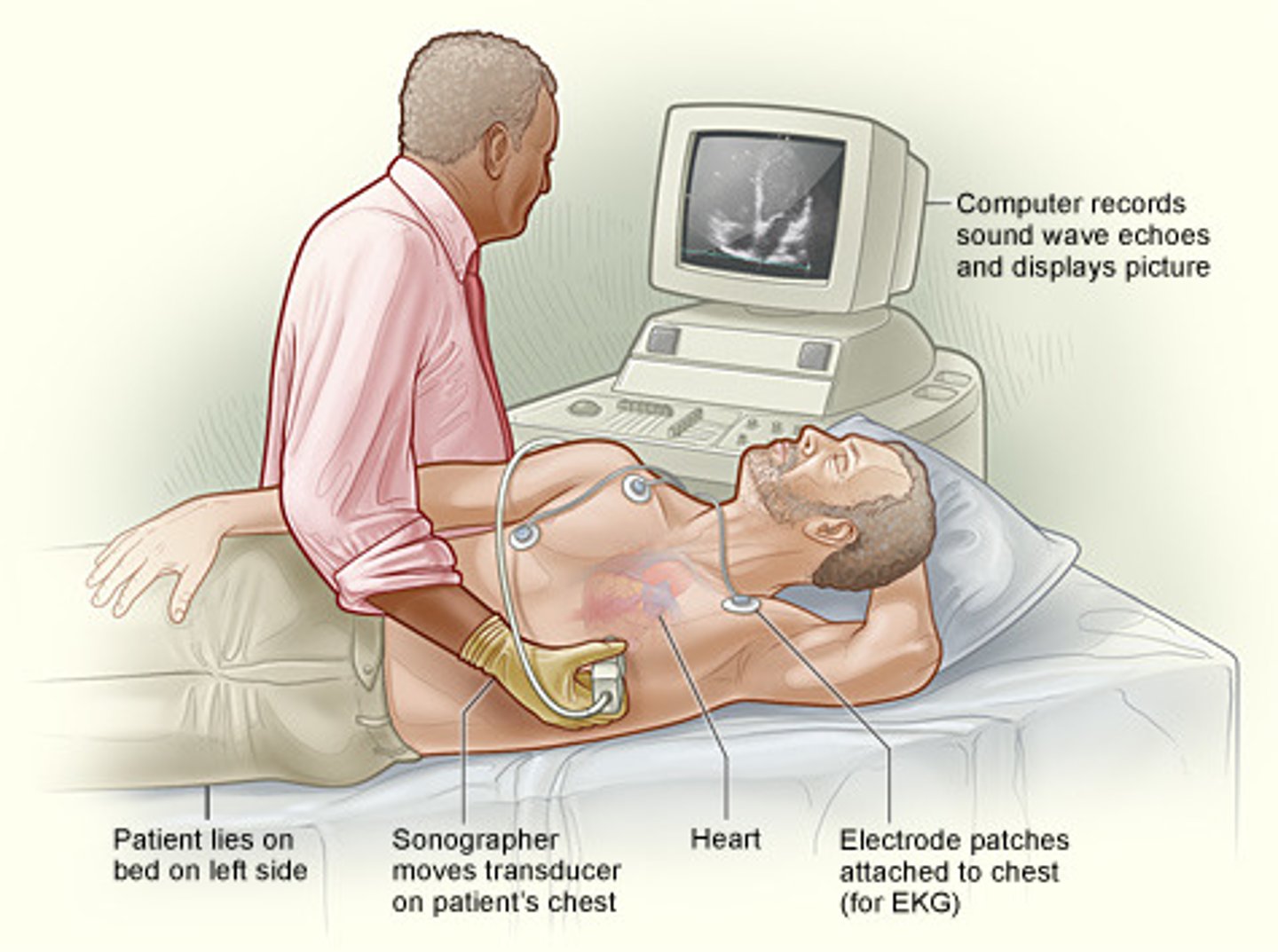
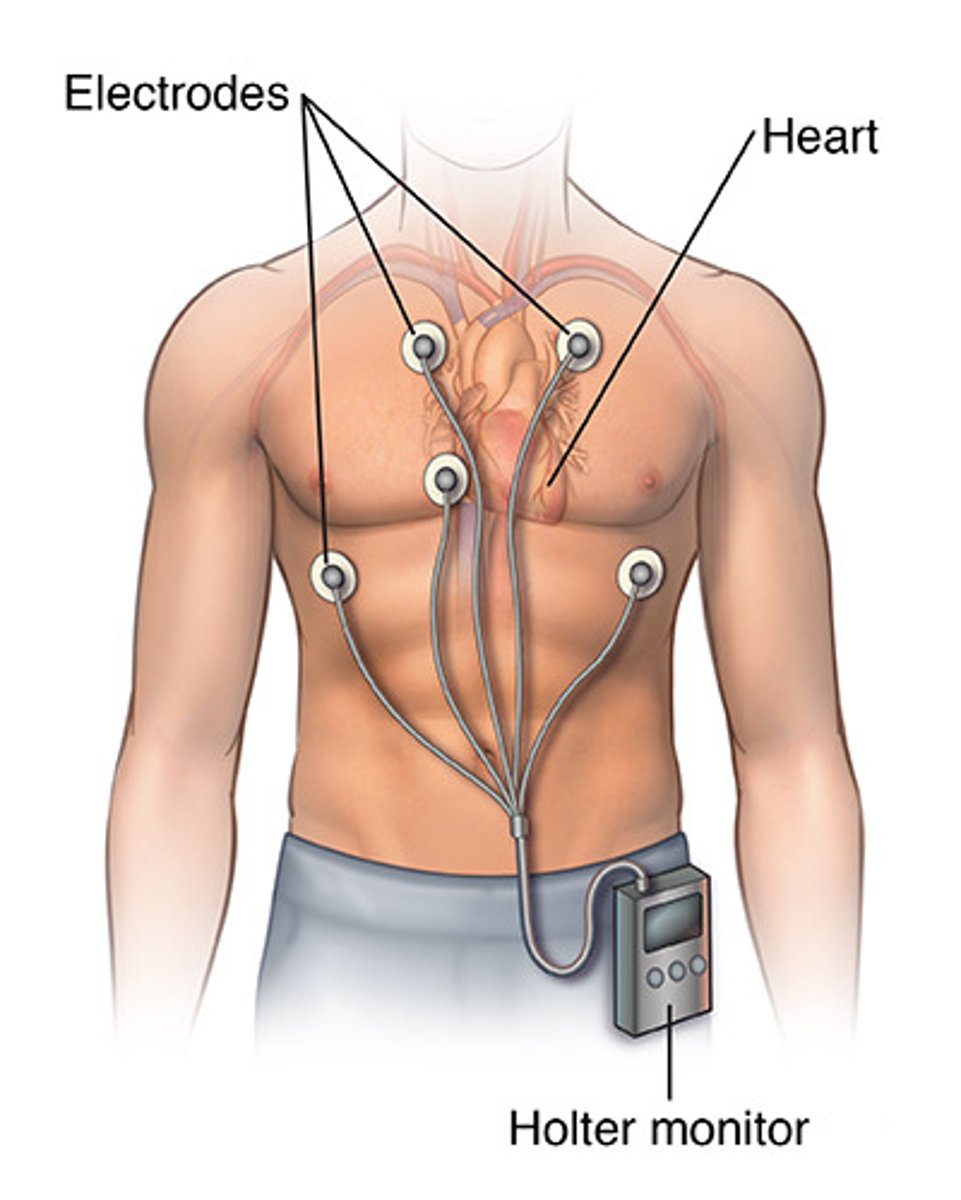
diagnostic testing for cardiopulmonary and respiratory diseases
-cardiac coronary cath
-cardiac exercise stress testing
-echocardiogram
-holter monitor
-arterial blood gases
-cardia biomarkers
-CBC
-cytologic sputum
-thoracentesis
cardiac coronary cath
can view and open up blocked coronary arteries
cardiac exercise stress testing
can detect blocks in the arteries (STRESS the heart)
echocardiogram
measures heart conduction
holter monitor
continuous monitor, can pick up changes in conduction
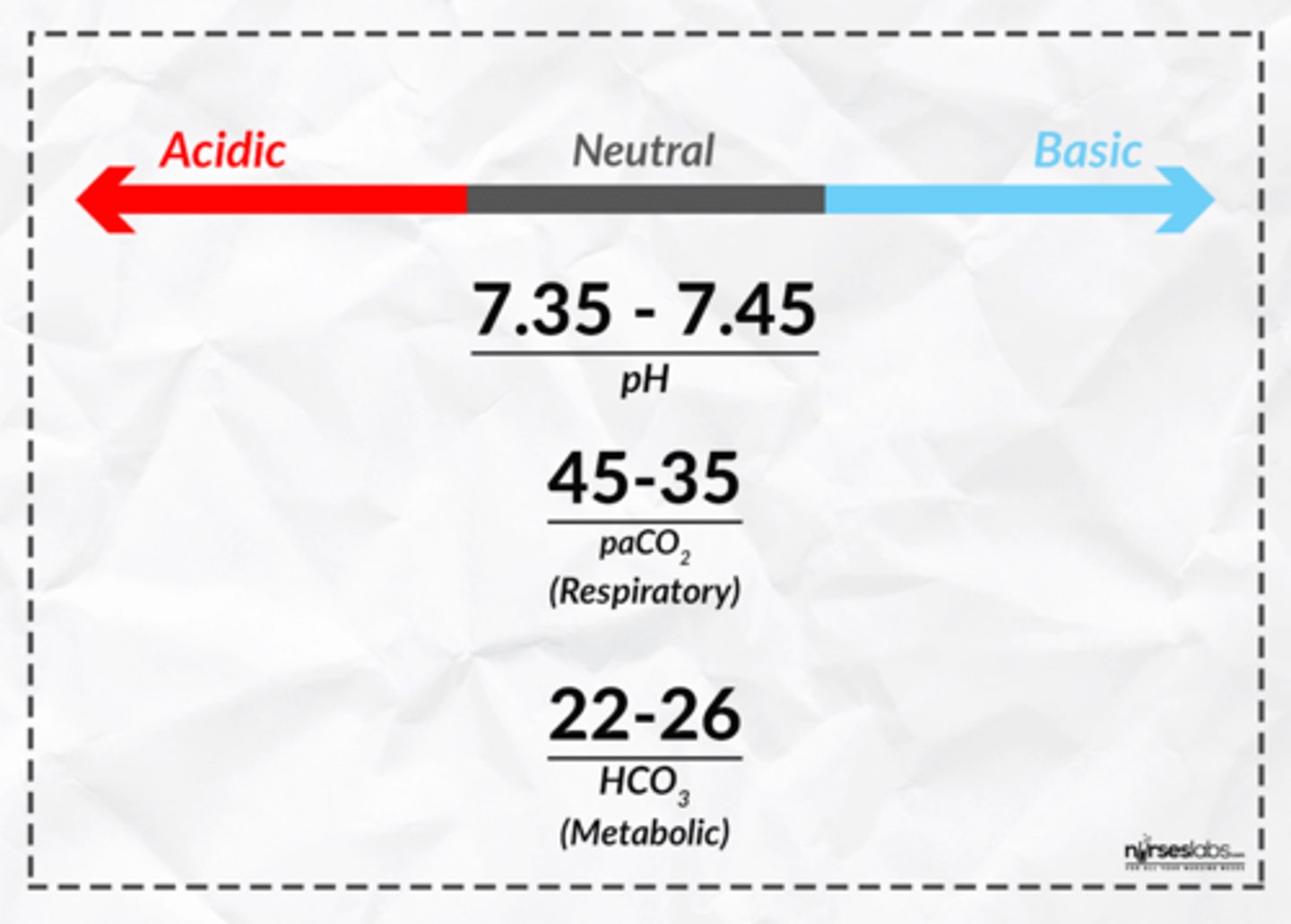
arterial blood gases
-drawn directly from a artery
-direct measurement of O2 and CO2
cardiac biomarkers
-creatinine kinase (CK-BM)
-troponin
-both elevate in the blood due to cardiac damage
complete blood count (CBC)
the body's response to illness
cytologic sputum
may detect cancerous cells
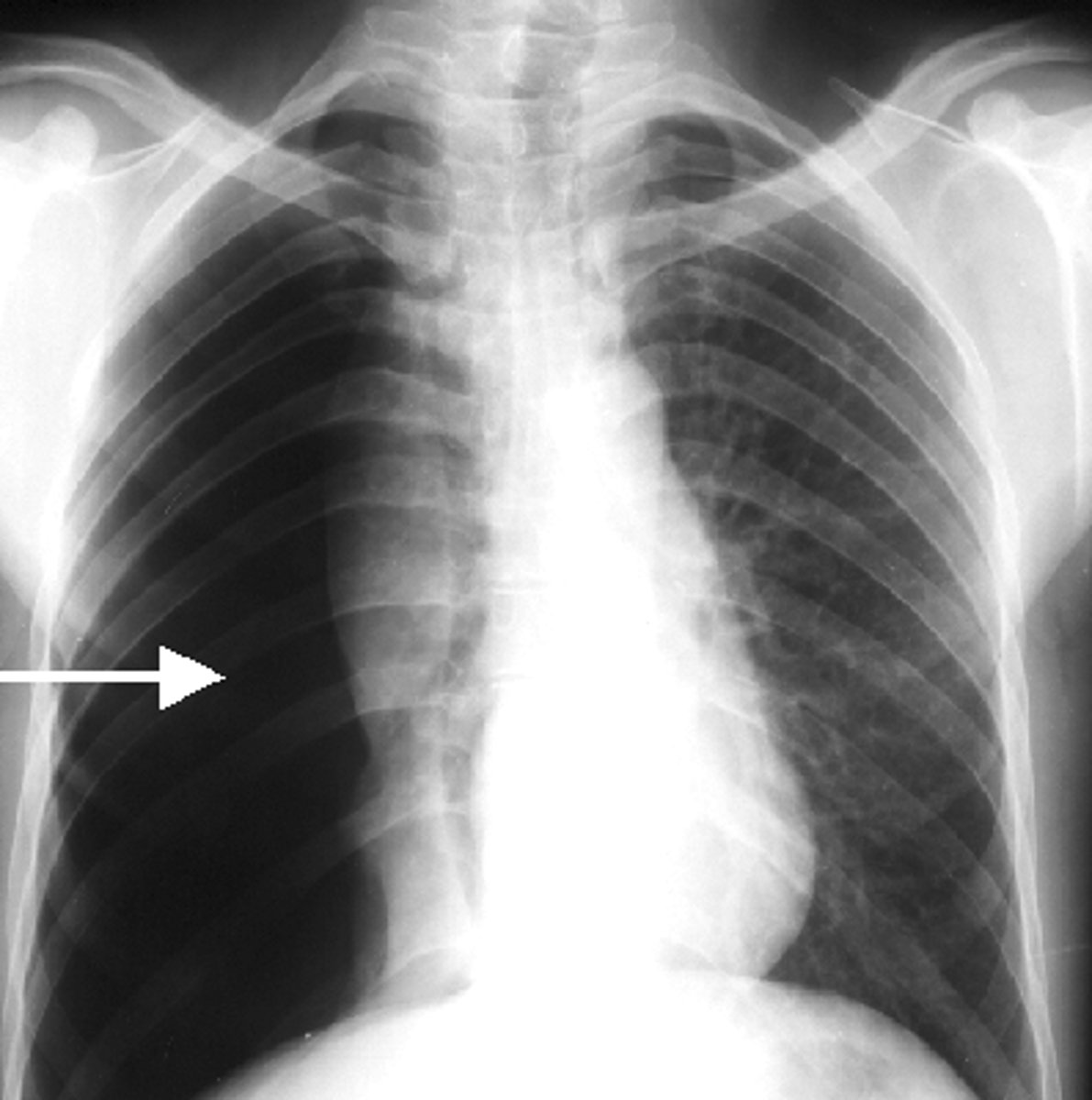
thoracentesis
-Procedure of puncturing the chest wall and aspirating pleural fluid or air from the chest
-At the bedside or under fluoroscopy if they want to really visualize
-Sterile procedure
-Patient sits on side of bed or in a chair
-Monitor VS, ABC’s
-Max amount removed is 1000 ml
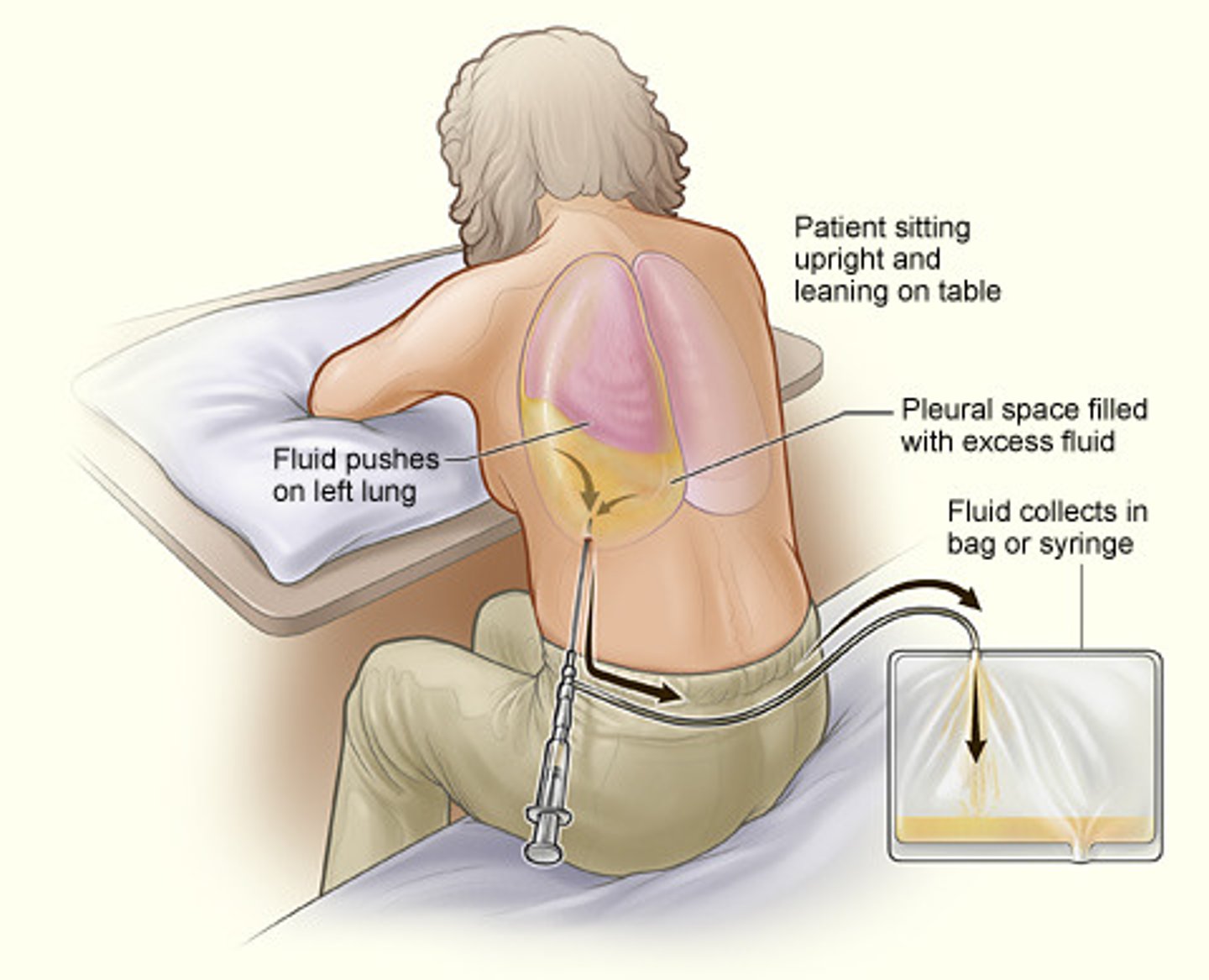
complications to thoracentesis
-Pneumothorax...Collapsed lung
-Pulling off too much volume
-Tracheal deviation
-Dyspnea/ Very labored breathing
-Assess for respiratory distress, blood tinged sputum, severe coughing
-Notify MD immediately.
bronchodilators
open narrowed airways

nebulizers
disperse fine particles of liquid medication into the deeper passages of the respiratory tract

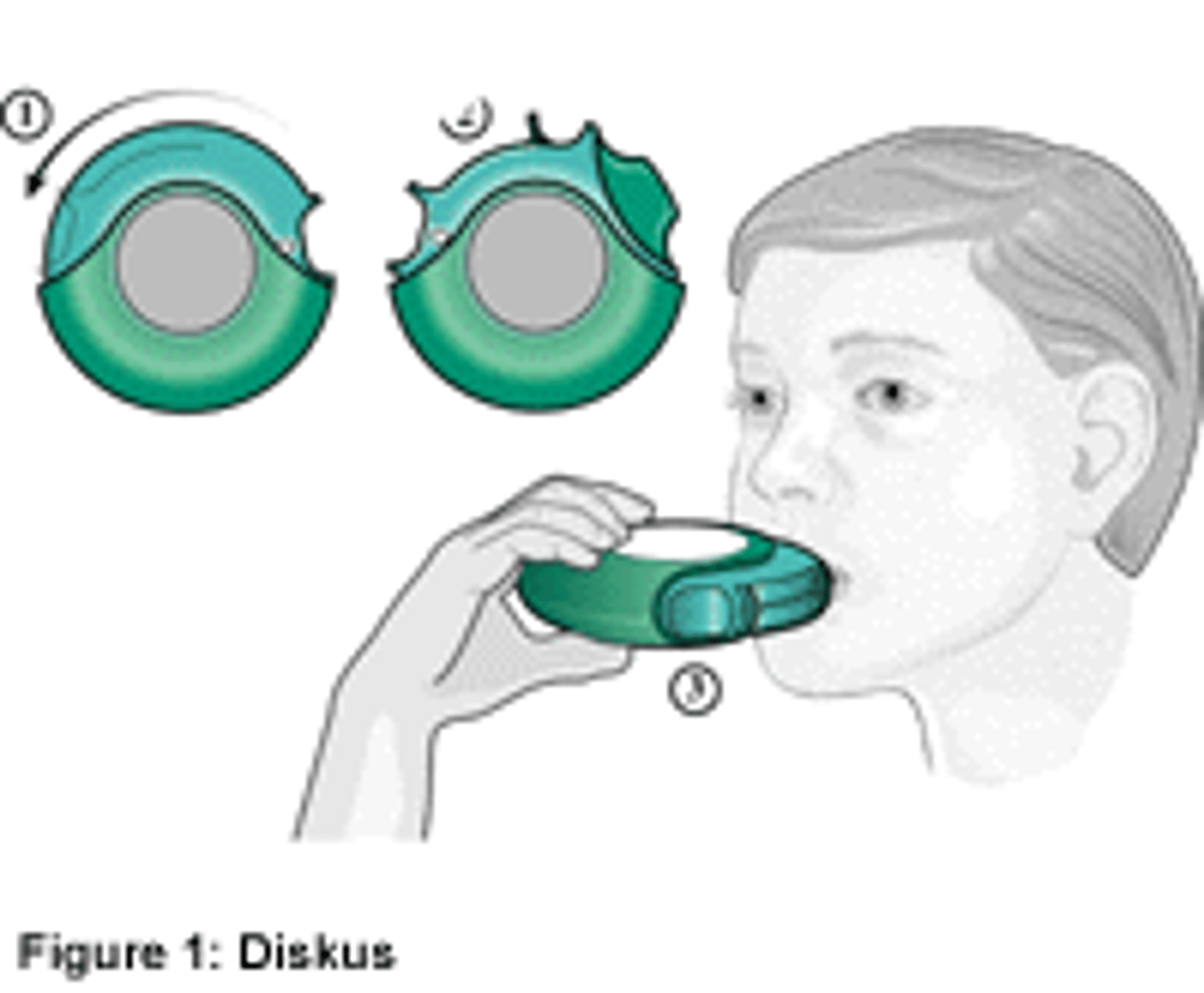
meter-dose inhalers
deliver a controlled dose of medication with each compression of the canister

dry power inhalers
breath-activated delivery of medications
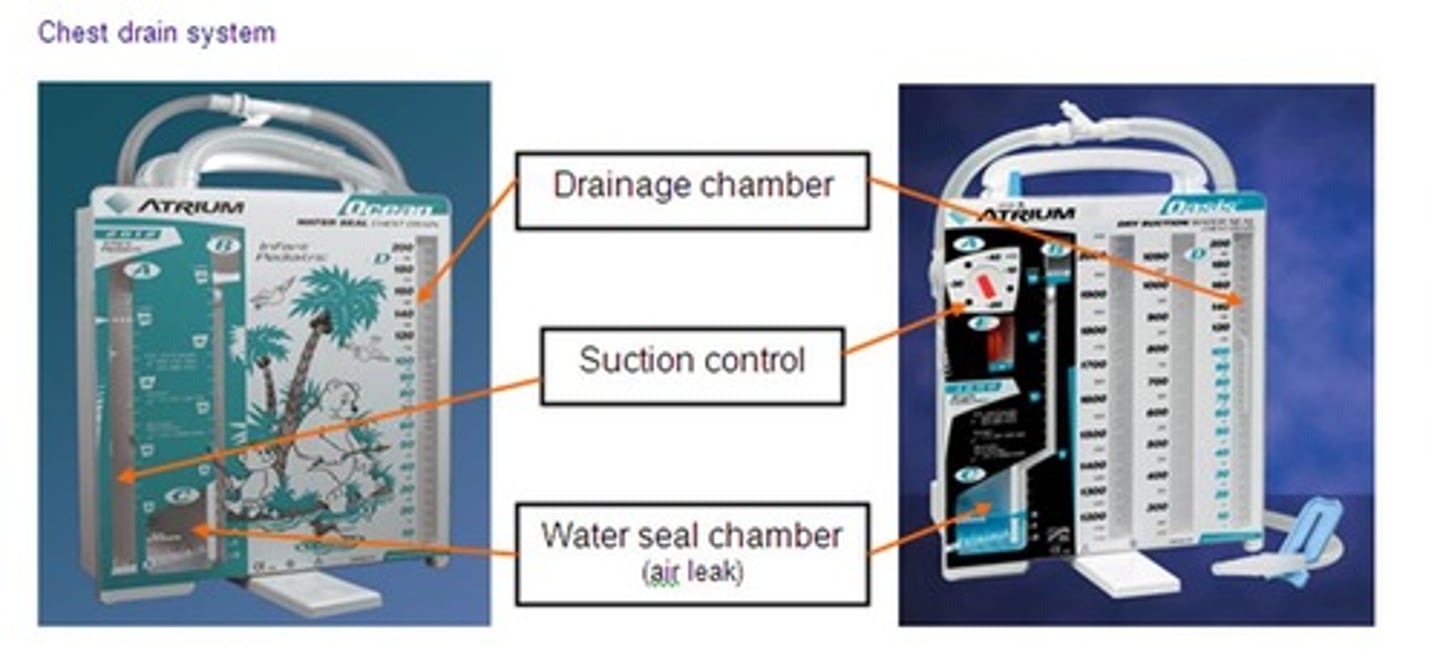
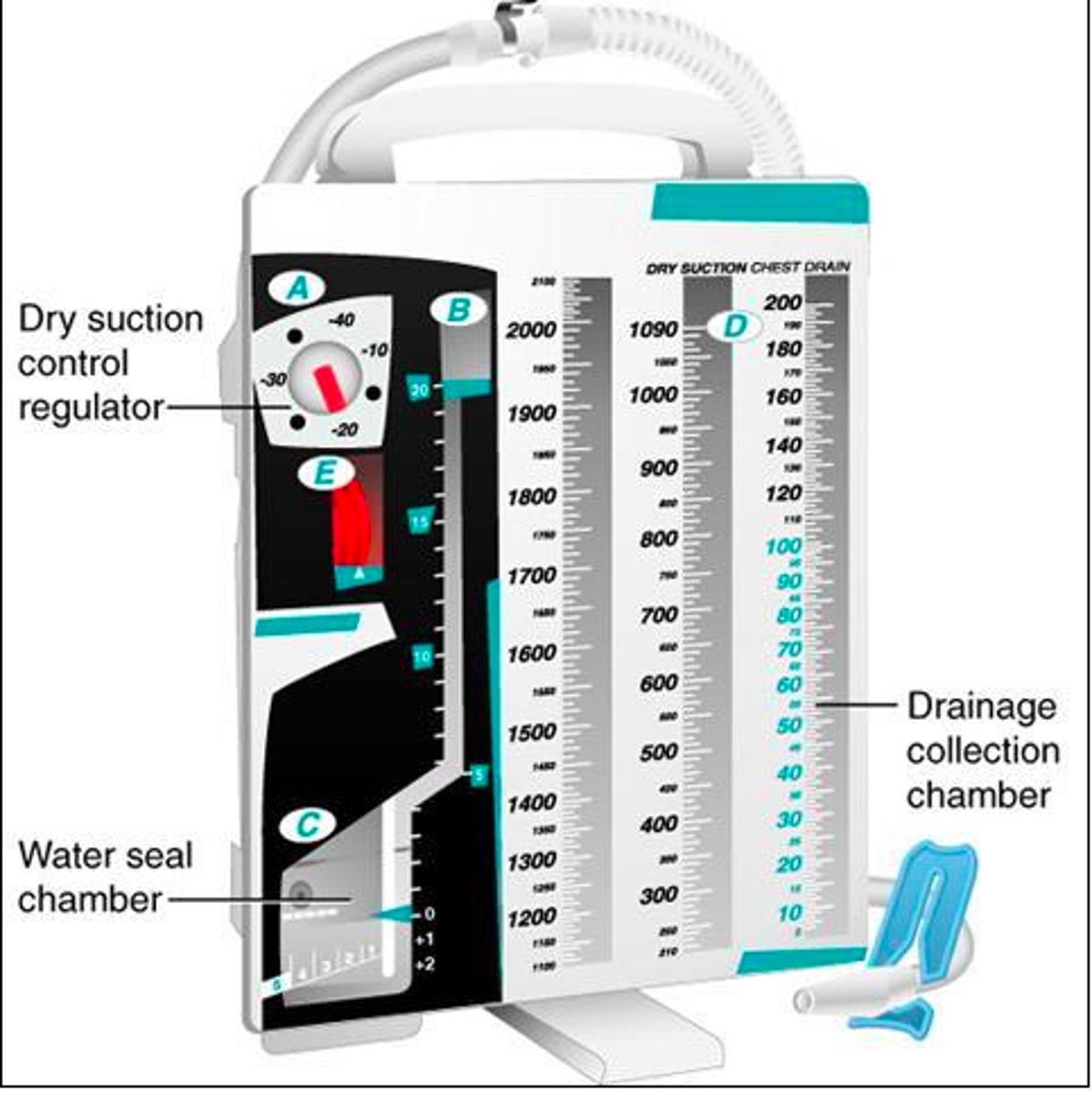
Chest Tube care
-Keep the HOB elevated at least 30 degrees.
-Change positions every 2 hours; ambulate every 4-6 hours.
-KEEP THE CHEST TUBE BELOW THE LEVEL OF THE PATIENT AT ALL TIMES!
-Administer pain meds to control pain...Chest tubes are NOT comfortable.
-Prevent kinking or occlusion of the drainage tubing.
-Assess O2 sat and keep above 90 % .
-Assess chest wall rise and fall. SHOULD be symmetrical if chest tube is working properly
-Assess for tracheal alignment...tracheal deviation is a serious
complication! Notify the provider immediately!
-Do not "strip" chest tubes.
-Assess for bubbling and tidaling.
-Maintain prescribed suction and water level.
-Assess characteristics of drainage... more bloody... less bloody...more yellow/green...sudden stoppage of drainage?
-Document the amount of drainage each shift under output.
-We put marks on the drainage system to denote each shift
output.
pleural effusion
fluid in the pleural space
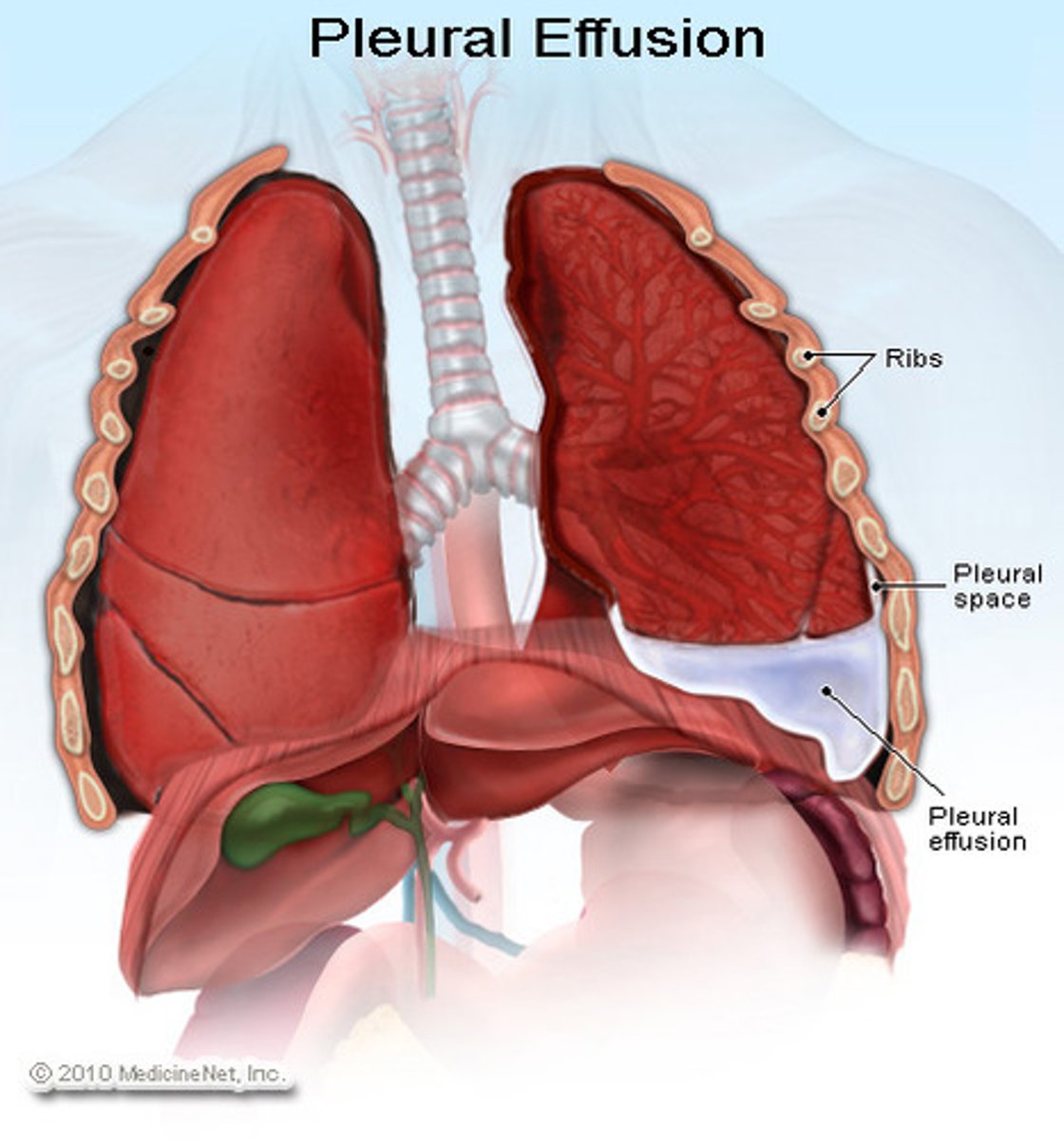
hemothroax
blood in the pleural space
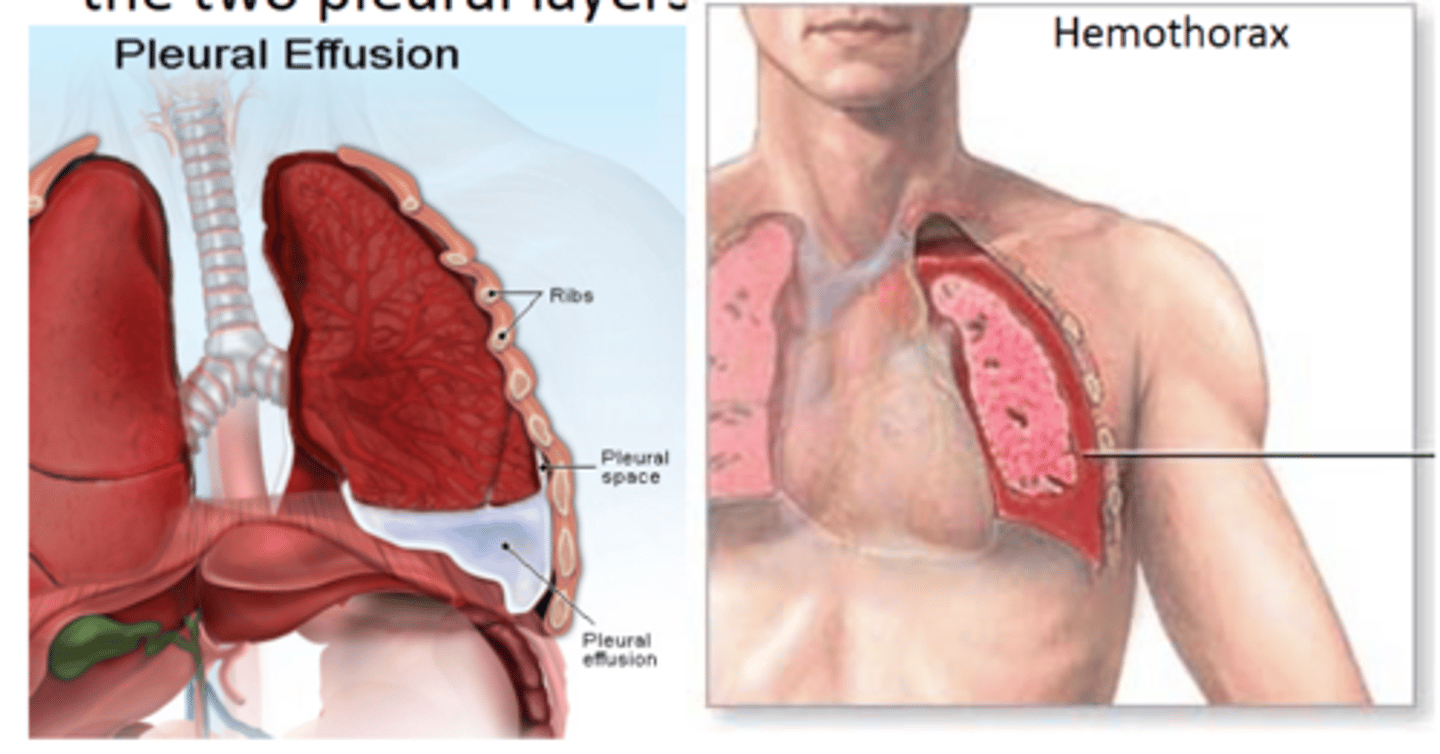
pneumothroax
air in the pleural cavity
Water seal
-This chamber prevents air from moving back up the tubing to the client. This chamber should be checked every shift to ensure the water level is at least 2 cm.
-Allows air to exit the pleural space on exhalation and keeps air in on inspiration= Tidaling (is normal)
-inhale=rise in water(increased pressure)
-exhale=drop in water(decreased pressure)
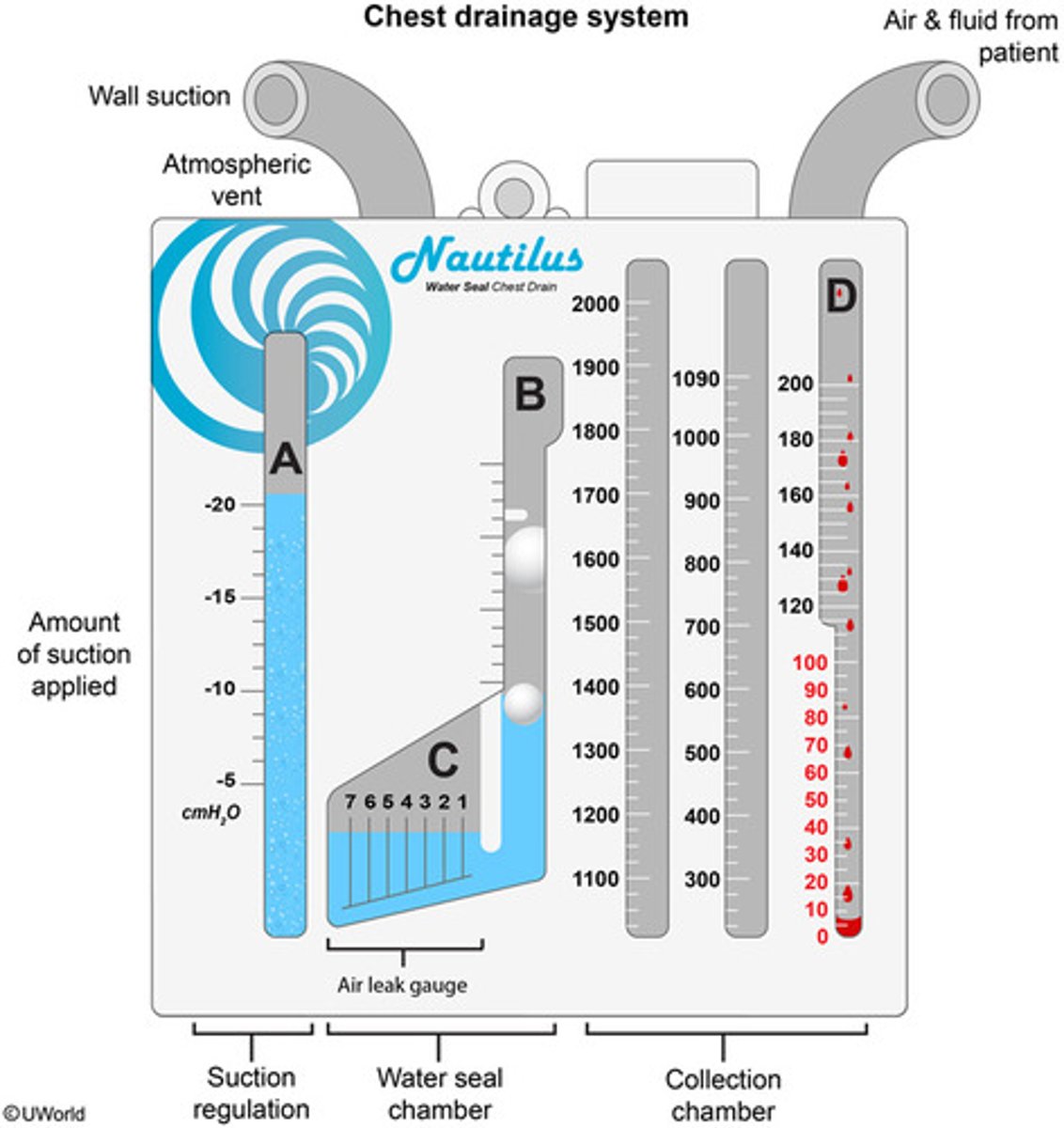
Wet suction
-Using water pressure to apply suction to the lungs to keep them inflated.
-Normal WET SUCTION is 20 cm. This applies a -20 cm of suction to the lungs.
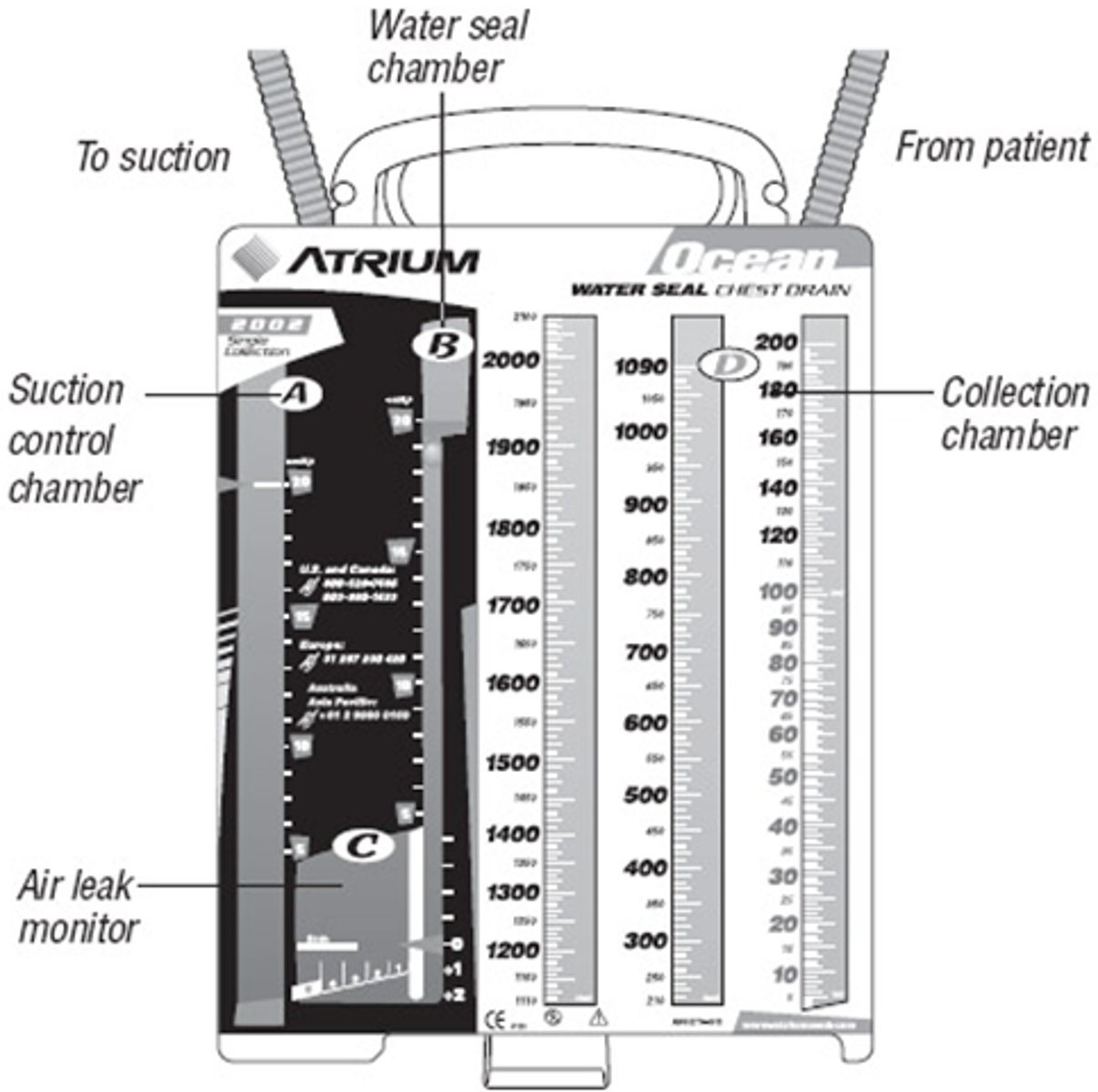
dry suction
-Attached to a suction system (on the wall).
-This will cause bubbling in the suction chamber. This is normal.
-No need to fill the suction chamber with fluid. This is controlled via the suction regulator.
-This is NORMAL.
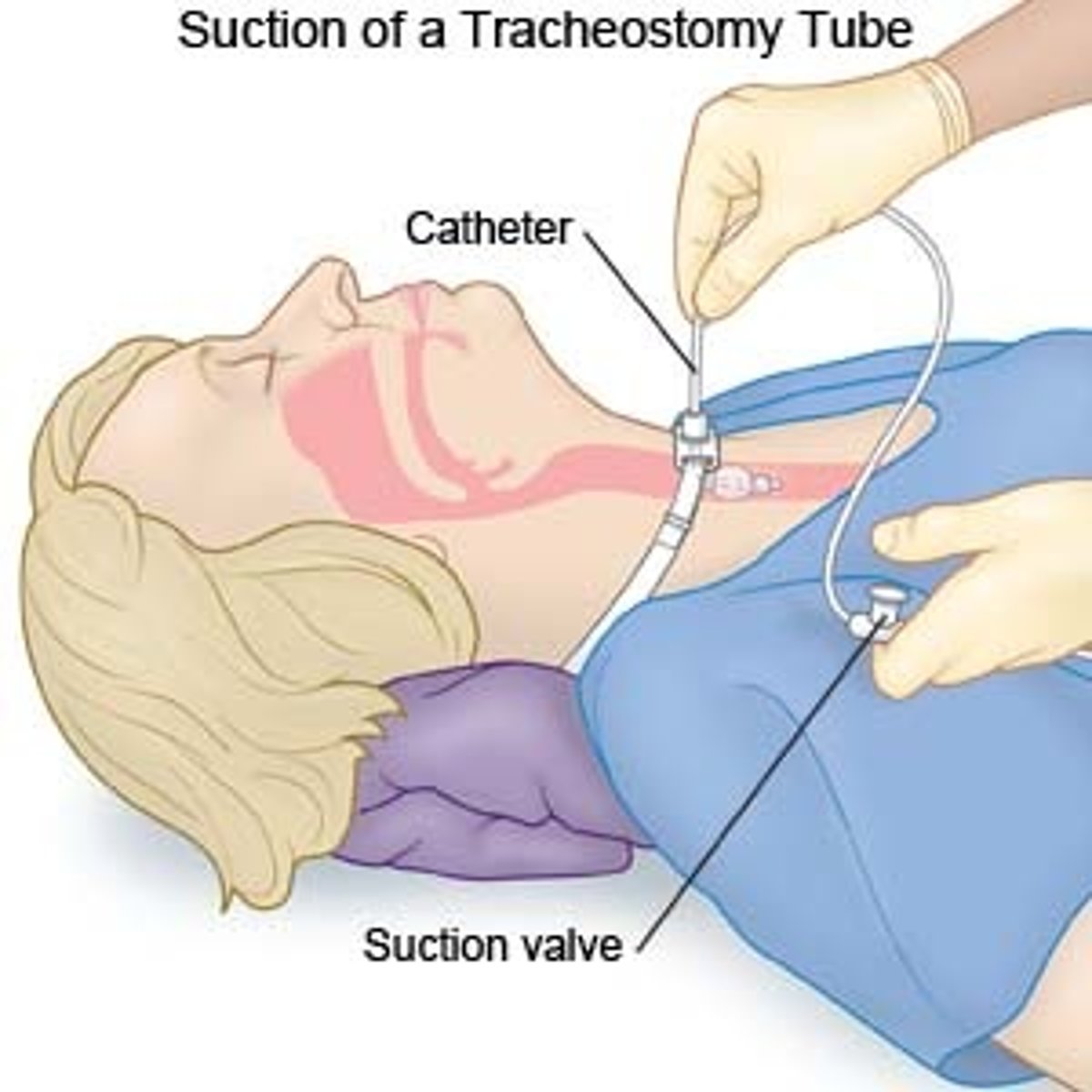
trach care/suctioning
-Keep the following at the bedside: Two extra tracheostomy tubes (one the client’s size and one size smaller, in case of accidental decannulation), the obturator for the existing tube, an oxygen source, suction catheters and a suction source, and a BVM.
-Provide methods to communicate with staff (paper and pen, dry‑erase board).
-Give oral care every 2 hr.
-Provide tracheostomy care every 8 hr to reduce the risk of infection and skin breakdown.
-Apply intermittent suctioning ONLY when removing the catheter…NOT when inserting!
-You will really hurt them if you apply suction while going down!
-Use medical asepsis for suctioning the mouth.
-Use surgical asepsis for all other types of suctioning.
-Use suction pressure no higher than 120 to 150 mm Hg.
-Limit each suction attempt to no longer than 10 to 15 seconds to avoid hypoxemia and the vagal response. Repeat suctioning if needed. Limit total suctioning time to 5 minutes.
-Suctioning is PRN…Coughing, crackles, decreased pulse ox, etc.
-When you suction you “steal” their oxygen, so it is NOT done “just because.”
NT/NG suctioning
-Insert the catheter into the naris during inhalation.
-Do not apply suction while inserting the catheter.
-Follow the natural course of the naris and slightly slant the catheter downward while advancing it.
-Advance the catheter the approximate distance from the tip of the nose to the base of the earlobe.
-Apply suction intermittently by covering and releasing the suction port with the thumb for 10 to 15 seconds.
-Apply suction only while withdrawing the catheter and rotating it with the thumb and forefinger.
-Do not perform more than two passes with the catheter. Allow at least 1 min between passes for ventilation and oxygenation.
-For nasopharyngeal and nasotracheal suctioning, use a flexible catheter and lubricate the distal 6 to 8 cm (2 to 3 in) with water‑soluble lubricant.
Which respiratory organ is the site of gas exchange?
alveoli
Pulmonary ventilation is the process by which oxygenated capillary blood passes through body tissues. T or F
False
Wheezes are continuous, musical sounds, produced as air passes through airways constricted by swelling, narrowing, secretions, or tumors. T or F
True
Which lung value is the amount of air contained within the lungs at maximum inspiration?
total lung capacity
A meter-dosed inhaler delivers a controlled dose of medication with each compression of the canister. T or F
True
A nurse is caring for a client who is having difficulty breathing. The client is lying in bed and is already receiving oxygen therapy via nasal cannula. Which of the following interventions is the nurse's priority?
assist the pt to fowlers position
Mr. Smith is sitting in Fowler's position. He is on 2 liters humidified oxygen via nasal cannula. His RR is 24 and un-labored. The current pulse ox is 96%. He appears to be resting comfortably. The nurse enters his room and begins her morning assessment. When lowering the head of the bed to turn the patient to listen to posterior lung sounds, the patient's RR increases to 36 breaths per minute. The patient is exhibiting signs of which of the following:
orthopnea
Taylor, an RN, is caring for a hospitalized patient with COPD. The patient, who is receiving oxygen at 2 liters per minute through a nasal cannula, has been averaging an oxygen saturation between 88-89% during Taylor's entire shift. Upon the last rounds, Taylor checks the patient's pulse ox and finds it to be 88%. When caring for this patient, the nurse would know to apply which of the following theories concerning the patient's respiratory disorder (COPD) and oxygen delivery?
Turning up the oxygen flow meter may cause the patient's respiratory rate to drop.
A nurse is caring for a patient who is having difficulty breathing and is experiencing dyspnea. The client is lying in bed at a 15-degree angle and is already receiving oxygen therapy via 2 liters nasal cannula. Which of the following interventions is the nurse's priority at this time?
assist the pt to high fowlers sitting position
good Samaritan laws
-laws to protect individuals providing aid
-need to provide aid within training and scope of practice
-do not leave until assistance arrives or becomes dangerous or going to get assistance
safety is the
first priority
ABCs
airway, breathing, circulation
CABs
chest compressions, airway, breathing
-apply AED as soon as its available
external bleeding
find source and apply direct pressure and elevate area above heart

nosebleed
-pinch soft part of nose
-tip head forward
-after 10 mins go to ED

internal bleeding
harder to tell
-monitor ABCs, and LOC
shock
-insufficient O2/nutrients to meet the body's needs=lack of circulation
-SX: First rapid pulse and cold clammy skin; then cyanosis, weakness, N/V, thready pulse; finally lost peripheral pulses, restlessness, yawning/gasping, unconsciousness
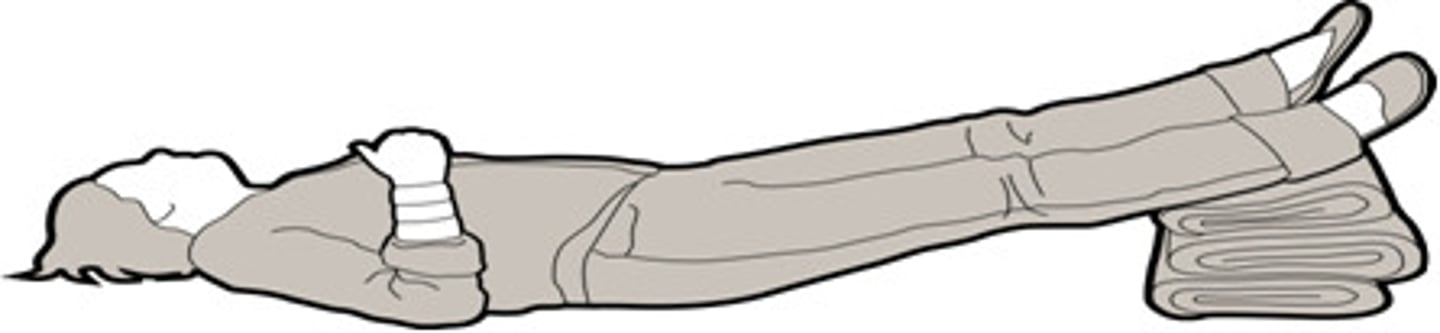
shock treatment
-Try to maintain blood flow: Lay down and raise legs (TRENDELENBURG POSITION)
-cover with blanket.
-Check ABC’s—maintain patent airway.
-Stop bleeding; treat underlying cause.
-Call EMS immediately if unconscious.
-If anaphylaxis, use epinephrine-pen—inject through clothes; need to hold in place for 10 sec prior to withdrawing.
wounds/injury
-do not removed embedded objects, stabilize and get help
-direct pressure
thermal burn
burn caused by heat
-cool with lots of cold water for 15-30min
-cover with non-adhesive dressing
-if large area call for EMS