Chapter 27 Fluid, Electrolyte, and Acid-Base Balance
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
Describe the distribution of fluids among fluid compartments in the human body
Intracellular fluid (ICF) - 2/3 of total body water
· Extracellular fluid (ECF) - 1/3 of total body water
· Interstitial fluid - 80% of ECF
· Plasma - 20% of ECF
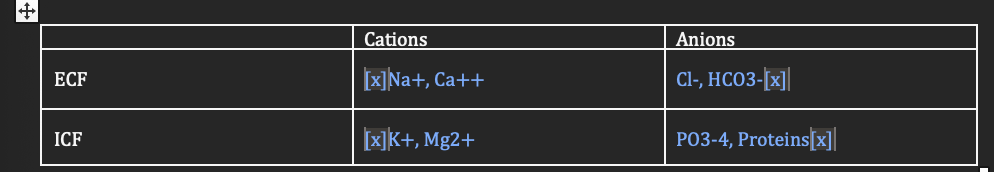
Describe the distribution of electrolytes in the human body by completing the table below
Know this
Homeostatic mechanisms regulate the ________ ONLY
ECF
Water moves by ____ transport ONLY
Passive
How does ADH regulate fluid and electrolyte balance
Increases H2O conservation at the kidneys; stimulates thirst center of the hypothalamus
How does aldosterone regulate fluid and electrolyte balance
Increases conservation of Na+ (H2O follows) and elimination of K+ at the kidneys
How does ANP regulate fluid and electrolyte balance
peptides (ANP and BNP): Promotes diuresis by opposing RAAS and inhibiting thirs
What is the difference between osmolarity and tonicity
Osmolarity: Concentration of a solution; total particles per liter
· Tonicity: Behavior of a solution; non-penetrating particles
Given the tonicity of a solution, predict how cell volume changes
· Isotonic - no net movement of H2O
· Hypotonic - net intracellular shift of H2O
· Hypertonic - net extracellular shift of H2O
Over time, the ECF and ICF equilibrate and become isosmotic due to the free movement of ____. Thus, by directly monitoring and regulating the ECF, we can indirectly regulate the ICF
H2O
The concentration of an electrolyte solution is measured in units of ___
mEq/L
Which physiological functions are affected by [Na+]ECF
Membrane potential and fluid homeostasis
How does the body regulate (i) Na+ balance and (ii) ECF volume
· (i) Changes in [Na+]ECF
· (ii) Changes in ECF volume
Which physiological functions are affected by [K+]ECF
Membrane potential and pH homeostasis
How do (i) acute and (ii) chronic hyperkalemia affect membrane excitability
Increase membrane excitability
How does hypokalemia, regardless of chronic or acute, affect membrane excitability
Decreases membrane excitability
How do (i) acidemia and (ii) alkalemia affect K+ balance
· Acidemia increases K+ concentration in ECF
· Alkalemia decreases K+ concentration in ECF
How does the body regulate K+ balance
Changes in [K+]ECF, changes in pH, aldosterone
What is pH for normal
7
What is normal pH for acidic
Below 7
What is pH for alkaline
Above 7
Describe the relationships between pH, [H+]ECF, and PCO2
· pH = -log[H+]
· PCO2 is a measure of the amount of CO2, which is related to H+ concentration via the bicarbonate buffer system
The normal pH range of extracellular fluid is
7.35 to 7.45
For each change in pH by 1, [H+] changes by a factor of
10
As pH changes from 7 to 6, [H+] [increases by a factor of
10
As pH changes from 7 to 11, [H+] decreases] by a factor of
10,000
Define acid in terms of proton transfer
Causes a decrease in pH, typically by releasing H+
Define base in terms of proton transfer
Causes an increase in pH, typically by accepting H+ or releasing OH−
Define acidosis in terms of pH
Conditions resulting in acidemia (pH of ECF below 7.35)
Define alkalosis in terms of pH
Conditions resulting in alkalemia (pH of ECF > 7.45)
What is the function of buffers
Resist changes in pH
What is the mechanism of buffers
Neutralizing acids or bases
Which two organs play very important roles in acid-base balance
Lungs and kidneys
What are the differences between volatile and non-volatile acids
· Volatile acids can leave solution and are excreted by the lungs, while non-volatile acids cannot leave solution and are excreted by the kidneys.
What is the only volatile acid produced in the body
Carbonic acid (H2CO3)
Describe mechanism and site of action for phosphate buffer system
· (i) Mechanism: The dissociation of disodium phosphate provides additional monohydrogen phosphate for use by the buffer.
(ii) Site of action: ICF and urine
Describe mechanism and site of action for protein buffer system
· (i) Mechanism: Amino acids (the building blocks of protein) are amphoteric
· (ii) Site of action: ICF and ECF; hemoglobin buffer system in RBCs
Describe mechanism and site of action for carbonic acid/bicarbonate system
· ( i) Mechanism: Sources of bicarbonate include the bicarbonate reserve and the renal deamination of Glu.
· (ii) Site of action: ECF
What are limitations of the carbonic acid-bicarbonate buffer system? What can it NOT buffer
It cannot protect the ECF from changes in pH that result from increased or decreased levels of CO2
pH imbalances are temporarily managed by
Buffer system
pH imbalances are permanently managed by
Lungs and kidneys
The lungs regulate pH by controlling
Controlling ventilation
The kidneys regulated pH by controlling
H+ sectretion
Acid-base disorders of respiratory origin are caused by
Abnormal handling of volatile acids (CO2)
Acid-base disorders of metabolic origin are caused by
abnormal handling of non-volatile acids (not CO2)
Compensation for acid-base disorders will NEVER
Fully correct the pH to the normal range
Respiratory compensation occurs at the
lungs
Renal compensation occurs at the
Kidneys
Respiratory compensation can compensate for acid-base disorders of
Metabolic origin
Renal compensation can compensate for acid-base disorders of (blank) origin
Respiratory and metabolic
Lung damage may cause
Respiratory acidosis
Kidney damage may cause
Metabolic acidosis
Hyperventilation causes
Respiratory alkalosis
Hypoventilation may cause
Respiratory acidosis
Ascent to high altitudes may cause
respiratory alkalosis
Prolonged exercise may cause
metabolic acidosis
Excessive diarrhea may cause
Metabolic acidosis
Overeating may cause
Metabolic alkalosis
Respiratory compensation for respiratory acidosis
Does not occure
Respiratory compensation for respiratory alkalosis
Does not occur
Respiratory compensation for metabolic acidosis
Increase ventilation
Respiratory compensation for metabolic alkalosis
Decrease ventilation
Renal compensation for respiratory acidosis
Increase H+ secretion, Increases HCO3- reabsorption
Renal compensation for respiratory alkalosis
Increase H+ reabsorption, Increase HCO3- secretion
Renal compensation for metabolic acidosis
Increase H+ secretion, Increase HCO3- reabsorption
Renal compensation for metabolic alkalosis
Increase H+ reabsorption, Increase HCO3- secretion
All possible compensations for respiratory acidosis
Increase H+ secretion, Increase HCO3- reabsorption
All possible compensations for respiratory alkalosis
Increase H+ reabsorption, Increase HCO3- secretion
All possible compensations for metabolic acidosis
Increase ventilation, increase H+ secretion, Increase HCO3- reabsorption
All possible compensations fr metabolic alkalosis
Decrease ventilation, Increase H+ reabsorption, Increase HCO3- secretion
1. What are the effects of age on fluid, electrolyte, and acid-base balance?
· Less Water: Body water decreases, especially after 60.
· Kidneys Weaken: Reduced function, less pH control, more water loss.
· Skin Thins: More insensible perspiration.
· Thirst Declines: Need more water intake.
· Hormones Shift: Less ADH/aldosterone, harder to save water.
· Bones/Muscle Shrink: Mineral loss.
· Lungs Stiffen: Weaker breathing, risk of acidosis.
· Illness Rises: More health issues overall.
Receptors only DIRECTLY monitor
Plasma volume and osmotic concentration
[Na+/K+] imbalances are more common becaus
many common conditions and medications affect fluid balance and kidney function, which are key to regulating these electrolytes.
[Na+/K+] imbalances are more dangerous because
both sodium and potassium are crucial for maintaining critical bodily functions, especially nerve and muscle function, including the heart. Could lead to death