Exam 3 patho: Respiratory Alterations part 2
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
What type of virus is the flu?
RNA virus
How is the flu transmitted?
Respiratory droplets
Precautions that must be taken around someone with the flu
When within 6 feet of the patient you must wear a face shield and goggles
There are 3 types of influenza (A, B, C). Why is type A more common?
Type A is Most common and most serious because they undergo the most antigenetic shifts (mutations each year)
Type B and C are less common and less serious because there are fewer antigenetic shifts
How long does it take for symptoms of the flu to show up (incubation period)?
1-4 days
Who should we be most concerned about with the flu? (4)
Elderly 65+ (most people who die)
young kids under 5 (bc their immune system isn’t as developed)
Pregnant women
Immunocompromised people (diabetes mellitus (type 1))
What are the 3 types of flu infections?
Upper respiratory infection
Viral pneumonia
Bacterial pneumonia
Upper respiratory infection flu
Infection that affects epithelial cells and cilia
Symptoms of upper respiratory infection flu (4)
Runny nose
Fever
Chills
Malaise
Why do you get a runny nose when you get an upper respiratory infection flu?
Runny nose because the epithelial cells of the respiratory tract are impacted
Symptoms of viral pneumonia flu infection
Non-productive cough
Malaise
Headache
What causes the symptoms of viral pneumonia flu infection?
Inflammation between the alveoli
makes the immune system more susceptible and increases risk of bacterial infection
Bacterial flu infection
Purpose of flu vaccine
Will lessen the symptoms (VERY important for immunodeficient people)
Won’t completely make you immune
Clinical manifestations of the flu (7)
Fever and chills, rigors
Malaise
Muscle aching
Headache
Nasal congestion
Non productive cough
Sore throat
Malaise
general feeling of discomfort, illness, or uneasiness whose exact cause is difficult to identify
Secondary complications of the flu
Sinusitis
Otitis media (ear infection)
Bronchitis
Croup
How long do the respiratory symptoms of the flu last?
10 days
What type of virus is SARS-CoV-2?
Single-stranded RNA virus
How is SARS-CoV-2 transmitted?
Droplet
Labwork done for COVID (2)
+PCR (nasal swab)
Radiography (bilateral lower-lobe infiltrates on x-ray)
Labwork to do for hospitalized patients for COVID
leukopenia?
elevated ESR & CRP and cytokines (TNF‐a, IL‐1, IL‐6)?
elevated PT, low platelets, elevated d‐dimer and fibrinogen?
Complications from COVID
ARDS
Kidney failure
Strokes
Incubation
Early and late stages of COVID
Early: migration of COVID and makes T-cells ineffective (?)
Late: leads to thickening of the alveolar cells
If the gas exchange has further to go to exchange CO2 and O2, you will get severe hypoxemia
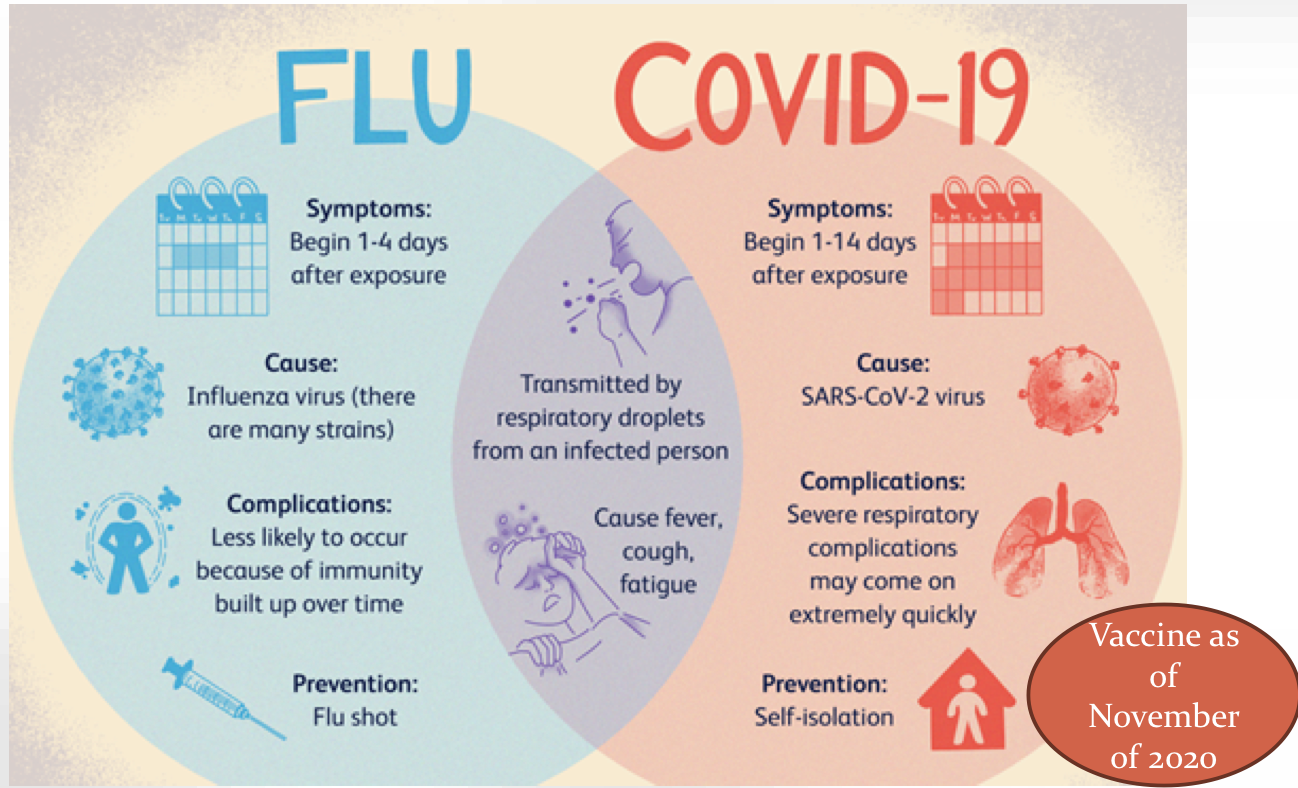
Flu vs COVID
Acute respiratory distress syndrome (ARDS)
Severe lung diseases caused by a variety of direct and indirect insults, which involves inflammation of lung parenchyma
What can inflammation of lung parenchyma from ARDS cause?
Hypoxemia due to impaired gas exchange
Multiple organ failure
Risk factors to contract ARDS
**Sepsis
Pneumonia
Chest trauma
Berlin definition of ARDS
X-ray — bilateral opacities = on both sides and is hazy
Consistent with pulmonary edema, but the heart is a normal size so it’s not HF
The edema occurs due to the inflammatory process — accumulation of WBCs
PF ratio <300 (PaO2/FiO2 ratio)
FiO2 — fraction of inspired O2
When it gets to 150 it’s really bad
What happens when exudate enters the alveoli during ARDS?
Blocks CO2 and O2 gas exchange
also loses surfactant
What cells go into the alveoli when exudate enters the alveoli in ARDS? What do they do?
Neutrophils enter alveoli and release:
inflammatory mediators
proteolytic enzymes
ROS
What is the most common protease enzyme released during ARDS? What does it impact?
Elastase
impacts the elasticity of the lungs
What happens when there is endothelial damage due to acute lung injury in ARDS?
O2 and CO2 exchange can’t occur effectively
What happens when there is epithelial damage due to acute lung injury in ARDS?
Lose surfactant
What occurs between these to get from endothelial damage to ARF?
Acute lung injury
Endothelial damage
?
?
?
?
Acute respiratory failure
Acute lung injury
Endothelial damage
Activation of neutrophils and platelets
Release of inflammatory cytokines
Increased alveolocapillary permeability with alveolar flooding (edema)
V/Q (ventilation-perfusion) mismatch and hypoxemia
Acute respiratory failure
What occurs between these to get from epithelial damage to ARF?
Acute lung injury
Endothelial damage
?
?
?
?
Acute respiratory failure
What occurs between these to get from endothelial damage to ARF?
Acute lung injury
Epithelial damage
Type II pneumocyte damage (surfactant-secreting cells)
Decreased surfactant
Atelectasis and decreased lung compliance
Decreased tidal volume and hypercapnia
Acute respiratory failure
Pulmonary embolism
a blood clot travels to the lungs and becomes lodged in a pulmonary artery and will prevent BF
Air pulmonary embolus
occurs when air enters the venous system and travels to the pulmonary circulation, potentially blocking blood flow to the lungs
can occur during a surgical procedure
Fat pulmonary embolus
fat deposit flows into lungs and blocks BF to lungs
Plaque pulmonary emboli
plaque that broke off of the vessel wall and travels to a pulmonary artery and blocks BF
Amniotic pulmonary emboli
amniotic fluid, fetal cells, or other debris enter the mother's bloodstream during pregnancy or childbirth
The damage to a patient’s lung due to a pulmonary embolism depends on… (2)
Size of embolus
Degree of BF obstruction
Small pulmonary embolism manifestations
may not have symptoms
subtle change in oxygenation
Moderate pulmonary embolism manifestations (5)
Respiratory changes
SOB
RR increased
O2 intake affected (decreased O2 exchange)
Pleural chest pain
Massive pulmonary embolism manifestations (6)
Very obvious and occur quickly
SOB immediately
O2 decreases
Tachycardia
Chest pain from inflammatory process
JVD bc blood is backing up
Due to a massive pulmonary embolism, blood may not be able to go through lungs, which could result in the heart… (2)
it can majorly strain the R side of the heart
if blood can’t get to the L side of the heart it will be damaged
Pulmonary embolism diagnosis methods (3)
Bloodwork
Radiology studies
EKG
How does blood work identify if there is a pulmonary embolism?
D-dimer indicates the breakdown of the coaggulation factors, indicating a clot
How does an EKG aid in pulmonary embolism diagnosis?
EKG of legs can help determine if it was a DVT that broke off
Can help determine R heart strain
Hypoxemic
Inadequate exchange of O2 between alveoli and capillaries
Treatment for hypoxemia
O2 delivery
Hypercapnia
increased levels of CO2 in BS due to inadequate ventilation of lungs
Treatment for hypercapnia
Must have a ventilator or something non-invasive (CPAP) to help force air in, and for CO2 out of the body
Hypoxemia neurological manifestations (4)
Delirium
Restlessness
Confusion
Anxious
Hypoxemia respiratory manifestation
Tachypnea
Hypoxemia cardiovascular manifestations — initial and late
Initial:
Tachycardia
Hypertension
Possible arrhythmias
Late:
Bradycardia
Hypotension
Hypoxemia skin color manifestation
Cyanosis
Hypercapnia carbon dioxide narcosis
high levels of carbon dioxide in the blood lead to decreased consciousness, potentially causing confusion, lethargy, coma, and even death
Hypercapnia neurological manifestations (3)
headache
disorientation
progressive somnolence (abnormal drowsiness or excessive sleepiness)
Hypercapnia cardiovascular manifestations
acidosis causes depressed cardiac contractility
Hypercapnia respiratory manifestations
decreased respiratory muscle contractility
Hypercapnia skin manifestations
Warm and flushed
Why can hypercapnia cause respiratory acidosis?
because CO2 is an acid and there is more present
Does high CO2 level cause vasodilation or vasoconstriction? Why?
Vasodilation because acidity causes BV smooth muscle relaxation