NBEO - Part 1 Ocular Pharmacology
1/250
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
251 Terms
which types of drugs penetrate the cornea the best
weak bases
small, uncharged (non-ionized), lipid soluble molecules
sympathetic cell bodies are located in the
thoraco-lumbar regions
parasympathetic cell bodies are located in the
cranio-sacral region
sympathic preganglionic neurons release
Acetylcholine
parasympathetic preganglionic neurons release
acetylcholine
sympathic postganglionic neurons release
norepinephrine and epinephrine
parasympathic postganglionic neurons release
acetylcholine
preganglionic neurons are longer in which division?
parasympathetic pathway
postganglionic neurons are longer in which division?
sympathetic pathway
organs that innervate the sympathetic division have ___ receptors(s)?
alpha and beta
organs that innervate the parasympathetic division have ___ receptors(s)?
muscarinic
SLUD
major actions of the parasympathetic nervous system
Salvation
Lacrimation
Urination
Defecation
(also bronchoconstriction, mitosis and "rest and digest" functions)
major actions of the parasympathetic nervous system
Salvation
Lacrimation
Urination
Defecation
(SLUD)
also bronchoconstriction, mitosis and "rest and digest" functions
major actions of the sympathetic nervous system
bronchodilation, mydriasis, decrease in secretions, and "fight or flight" functions
iris sphincter receptor
M3 - cholinergic
Causes: miosis
ciliary muscle accommodation receptors
M2, M3 - cholinergic
Causes: constriction, increases accommodation
B2 - adrenergic
Causes: relaxation, opposes accommodation
lacrimal gland receptor
M2, M3 - cholinergic
Causes: increase tear production
iris dilator receptor
trabecular meshwork receptor
B2 - adrenergic
Causes: relaxation, increase outflow
NPCE receptors
B2, B1 - adrenergic
Causes: increase aqueous formation
Ciliary Body vasculature receptors
A2 - adrenergic
Causes: constriction, reduction aqueous formation
pilocarpine reduces IOP by
30% (first ever glaucoma med - 1870s)
3rd nerve palsies will ___ with 1% pilocarpine
constrict
(use 1% pilocarpine to differentiate a 3rd nerve palsy vs sprinter tear)
in Adie's tonic pupil the iris sphincter is ___
super sensitized (wil constrict to 0.125% pilocarpine)
0.125% pilocarpine is used in the diagnosis of _________, and is effective in constricting the pupil because of a supersensitized sphincter muscle that is a result of a _______ lesion.
A. Adie`s tonic pupil, sphenopalatine
B. Horner`s syndrome, lung
C. Adie`s tonic pupil, ciliary ganglion
C
pilocarpine main side effects
broaches, headaches and myopic shifts (HA more common with pre-presbyopes)
cataracts are from longterm use and are only problematic if located centrally
RD (uncommon but well-recognized)
secondary angle-closure glaucoma (due to lens movement forward during accommodation - PAS or PS - pupillary block)
Edrophonium (Enlon) is used in diagnosis of
Myasthenia gravis (Tensilon Test) - rapid onset (30-60 sec) and short duration (10 min)
inhibits acetylcholesterase
if ptosis improves after 1-2 min of injection, (+)myasthenia gravis
"Ed Dx"
Neostigmine (Prostigmin) is used for the treatment of
Myasthenia gravis
also limb strength evaluation (neostigmine test)
Echothiophate (Phospholine)is used in the diagnosis and/or treatment of
accommodative esotropia (direct simulation of CB muscle, decrease CNS accommodation and accommodation convergence)
also rarely used to treat glaucoma
Pyridostigmine (Mestinon) is used to treat
Myasthenia gravis
"get pyRID of the Myasthenia - tx it"
echothiophate and isofluorophate are __ acetylcholinesterase inhibitors, and they are not used for __ because of their high incidence of side effects. They are also found in ___.
irreversible, glaucoma, pesticides
"echo's on and on - irreversible"
atropine is used to reverse __ side effects
muscarinic
Pralidoxime (Protopam) reverses the effects of ____
irreversible acetylcholinesterase inhibitors
Phenelzine (Nardil) is a ___ inhibitor
MOA (mono-amino oxidase) - the enzyme that breaks down epinephrine and norepinephrine
want to be caution when taking these with adrenergic agonists
Donepezile (Aricept)
acetylcholinesterase inhibitor (Tx: Alzheimer's)
2 main symptoms of myasthenia gravis
ptosis and diplopia at the end of the day (diplopia is more common)
Which drug classification exacerbates myasthenia gravis symptoms?
beta-blockers (i.e timolol)
[-stigmine]
Neostigmine and pyridostigmine
(AChE inhibitors - reversible)
"STop ACH"
cholinergic antagonists
Scopolamine
Tropicamide
Atropine
Cyclopentolate
Homatropine
CNS toxicity is ___ likely in scopolamine vs atropine
more
Tropicamide has the ___ onset and the ___ duration of mydriatic effects. It has ___ mydriatic effect than cycloplegic - making it the standard drug for ___.
fastest, shortest, stronger, dilation.
adverse side effects for Tropicamide are ___
rare. very safe drug, even with patients with cardiovascular disease
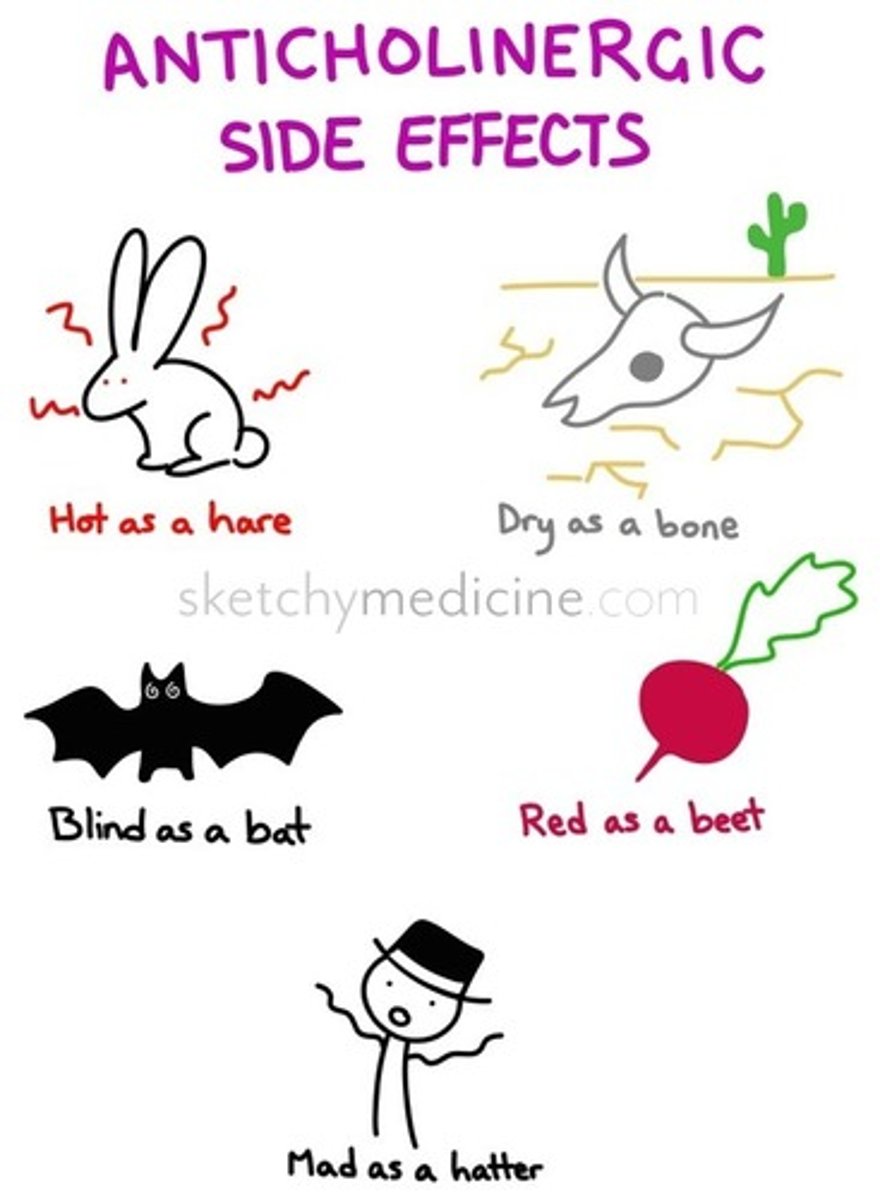
Atropine toxicity (anticholinergic toxicity)
Mad as a hatter (confusion or disorientation due to CNS effects on the hypothalamus - rapid pulse), dry as a bone, hot as a hare, red as a beet, blind as a bat
Which patient(s) should you proceed with caution when using atropine?
patients with Down syndrome, small children, and elderly
cycloplentolate has the ___ onset and the ___ duration of cycloplegic effects. It is the standard drug for ___.
fastest, shortest, cycloplegia
Standard drop for anterior uveitis treatment?
Homatropine
Duration of mydriasis effects with atropine
7-10 days
Duration of mydriasis effects with homatropine
1-3 days
Duration of mydriasis effects with scopolamine
3-7 days
Duration of mydriasis effects with cyclopentolate
24 hours
Duration of mydriasis effects with tropicamide
4-6 hours
Duration of cycloplegic effects with atropine
7-12 days
Duration of cycloplegic effects with homatropine
1-3 days
Duration of cycloplegic effects with scopolamine
5-7 days
Duration of cycloplegic effects with cyclopentolate
24 hours
Duration of cycloplegic effects with tropicamide
4 hours
atropine onset
60-180 minutes (cycloplegic)
tropicamide onset
20-35 minutes (max cycle at 20-45 minutes)
cyclopentolate onset
20-45 minutes for mydriasis and cyclo max effects
Botox MOA
indirect muscarinic and nicotinic cholinergic receptor antagonist (block Ach at the neuromuscular junction)
True or false: epinephrine acts on all 4 adrenergic receptors?
true (acts on A1, A2, B1, B2)
true or false norepinephrine acts on all 4 adrenergic receptors?
false; does not act on B2 (acts on A1, A2, B1)
phenylephrine is a ___ agonist
alpha 1 - adrenergic agonist
(dilation only, no cyclo)
phenylephrine is used to differentiate between?
episcleritis and scleritis (blanching of conj vessels on application = (+)episcleritis)
drop will not be able to penetrate and blanch scleral vessels
muller's muscle responds to
alpha 1 receptor stimulation - phenylephrine causes palpebral widening
phenylephrine 10% is used to
break posterior Synechiae only - high dose has adverse cardiovascular effects (HTN crisis, cardias arrhythmias)
Phenylephrine is contraindicated in patients ....
taking MAOIs (monoamine oxidase inhibitors), tricyclic antidepressants (TCAs) and atropine. Also patients with Graves' (increases sympathetic innervation)
[-zoline]
naphazoline (naphcon) and tetrahydrozoline (visine)
topical ocular decongestants
greater alpha than beta effect - potential to depress CNS
nephcon A - OTC drug that contains nephazoline and antihistamine
in isolation phenylephrine is __ to provide a a fixed dilated pupil.
unable
alpha 2 agonists are used for glaucoma Tx for their effects on ____ and ____
aqueous humor production (decreases), uveoscleral outflow (increases)
brimonidine, apraclonidine
[-onidine]
alpha 2 agonist
brimonidine (alphagan), apraclonidine
brimonidine is 30x ___ selective than aproclinidine
more
Alphagan has showed
nueroprotective properties
Alphagan-P decreases the incidence of follicular (but allergic) conjunctivitis vs Alphagan with
purite as the preservative
Alphagan-P comes in 0.15% and 0.1%
Alphagan comes in 0.2%
brimonidine causes mydriasis or miosis
miosis
most common systemic side effect of brimonidine and apraclonidine
dry mouth
brimonidine is contraindicated in patients taking
monoamine oxidase inhibitors (MAOIs)
Tachyphylaxis
rapid decrease in response to a drug
which drug cannot be used for longterm glaucoma treatment due to tachyphylaxis
apraclonidine
not effective in chronic therapy - efficacy is reduced after 8 days of Tx
commonly used for IOP spikes before and after surgery
which drugs can be used to diagnose Horner's syndrome
apraclonidine, phenylephrine, cocaine, hydroxyamphetamine
when is anisocoria greatest in Horner's syndrome?
in the dark
True or false: If a ptosis and dilation lag exists then the diagnosis without pharmacological testing can be made for Horner's syndrome.
True. no pharmacological testing is needed if a biotic pupil is present it lags on dilation in the dark with a ipsilateral lid ptosis.
healthy eye will always ___ with cocaine
dilate
Horner's syndrome eye will ___ with cocaine
not dilate (regardless of the location of the sympathetic pathway lesion)
healthy eye will ___ with apraclonidine
remain unchanged (no effect)
Horner's syndrome eye will ___ with apraclionidine
dilate due to hyper-sensitized alpha 1 receptors
if the pupil does not dilate with hydroxyamphetamine then the lesion is
postganglionic
hydroxyamphetamine causes the release of norepinephrine from postganglionic neurons, so the postganglionic neuron must be damaged
if the pupil dilates with hydroxyamphetamine then the lesion is
preganglionic
hydroxyamphetamine causes the release of norepinephrine from postganglionic neurons, so the postganglionic neuron must still be intact
phenylephrine 1% causes full dilation in Horner syndrome patients with a ___ lesion
postganglionic
mech. unknown - believed to be hypersensitivity of postganglionic adrenergic receptors
why does brimonidine produce miosis?
A1 receptors on the radial dilator muscle cause mydriasis. Brimonidine is selective for α2 receptors, which are present on presynaptic sympathetic nerve terminals, and stimulation of these in a normal pupil causes miosis due to a reduction in norepinephrine production and release at the nerve terminal, combined with the unopposed action of the iris sphincter muscle.
"ASH CiTy"
order of cholinergic antagonistic from longest onset/duration of action
Atropine
Scopolamine
Homatropine
Cyclopentolate
Tropicamide
2 adrenergic receptors that can cause glaucoma if they are overstimulated by adrenergic agonists
B2 - increase secretion of aqueous
A1 - dilation --> PAS
3 MOA for TCA (tricyclic antidepressants)
increase epinephrine, anticholinergic, increase serotonin
"2 lungs, 2 eyes"
Beta-2 mainly in the lungs (bronchi) and eyes (NCPE)
"1 heart"
Beta-1 mainly in the heart
[-olol]
beta blocker
sympathetic nervous system is __ at night
off (causing pupillary miosis, and rendering adrenergic antagonist essentially ineffective at night)
timolol concentration for Caucasian pt
0.25% Qam
timolol concentration for African American pt
0.5% Qam
neuroprotective drugs
brimonidine and betaxolol