Anthrax
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
Anthrax is also known as
Woolsorters’ Disease
Cumberland Disease
Maladi Charbon
Malignant Pustule
Malignant Carbuncle
Milzbrand
Splenic Fever
Siberian Fever
Causative agent of Anthrax
Bacillus anthracis
Anthrax morphology
spore-forming
Gram-positive
aerobic rods
Anthrax Family
Bacillaceae
Virulence Factors of Anthrax
pXO1
pXO2
biofilm formation
toxins
edema toxin
lethal toxin
capsule
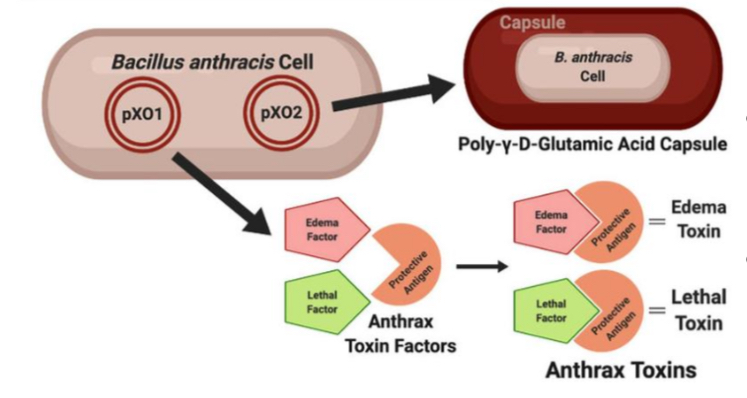
exotoxin complex and is associated with symptoms
pXO1
interferes with phagocytosis
pXO2
serves as a pivotal strategy in B. anthracis virulence by augmenting its survival in hostile environments → enabling resistance to antimicrobial agents & facilitating its persistent environmental presence → contributing to the persistent and chronic nature of anthrax infection
biofilm formation
Epidemiology of Anthrax: Global
80% of herbivore deaths
occurs worldwide
Epidemiology of Anthrax: Philippines
Only 82 suspected anthrax cases were recorded from January 2017 to December 2023
In 2022, 3 cases were confirmed
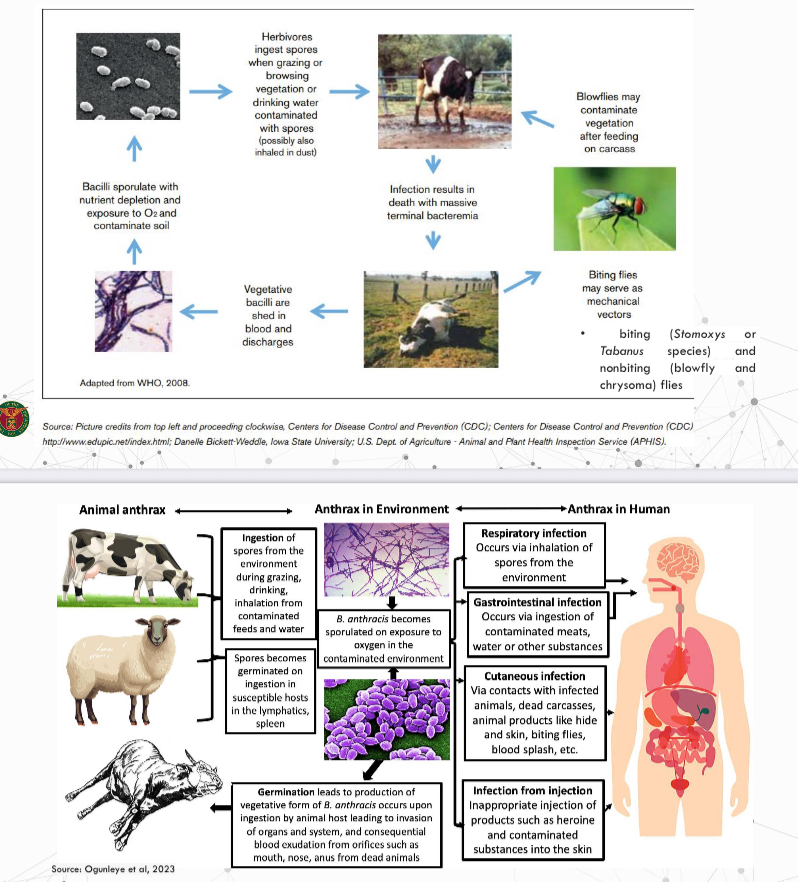
Transmission of Anthrax
ingestion
inhalation
penetration through disrupted skin
infectious dose not known
aerosol challenge is estimated to be 8,000-50,000 spores
infectious dose may be as low as 1-3 spores
Occupational Risk
veterinarian
animal health officers
livestock workers, particularly in anthrax endemic area
workers handling animal products (wool, meat, hair, skin, bone, or bone products)
households or breeders who have discovered their livestock died and consumed meat contaminated with anthrax spores
military personnel
laboratory workers handling anthrax samples
emergency response workers handling bioterrorism are among those at high risk of contracting anthrax

Clinico-pathological features in animals
incubation period: 1-14 days
in herbivores: 3-7 days (inoculated orally)
in pigs: 1-2 weeks (laboratory experiment (oral inoculation) resulted in clinical signs after 1-8 days)
peracute, acute - susceptible species
subacute, chronic - more likely to be reported in resistant hosts

Clinico-pathological features of anthrax in ruminants
peracute systemic disease is common
sudden death is often the only sign
staggering, trembling, dyspnea
sometimes noted shortly before death
followed by rapid collapse and terminal convulsions (in some cases)
acute form
ill for a short period (up to 2 days) before they die
fever and excitement may be noted initially, followed by depression, stupor, anorexia
disorientation
muscle tremors
dyspnea
hematuria
diarrhea
congested mucous membranes
small scattered hemorrhages on the skin and mucous membranes
pregnant cows may abort
decreased milk production
milk may appear bloody or discolored with yellow tinge
bloody discharges from orifices such as nose mouth and anus
some may develop subcutaneous edematous swellings often in the ventral neck, thorax, and shoulders, but sometimes at other sites including the genitalia
pulmonary anthrax
with productive cough and an acute course
rare
dying animals are usually found bloated
without or incomplete rigor mortis
absence of clotting - most prominent characteristic
Clinico-pathological features in horses
acute course is common
fever
anorexia
depression
sepsis
severe colic
bloody diarrhea (some)
death within 48-96 hours
some have swelling on the neck, sternum, lower abdomen, genitalia
usually die within 3 days but some survive longer
Clinico-pathological features in pigs
septicemia and sudden death occur occasionally
mild subacute to chronic cases
localized swelling
fever
enlarged lymph nodes
throat can swell rapidly in pigs that develop anthrax lesions in the oropharynx
intestinal involvement can result in anorexia, vomiting, diarrhea (may be bloody) or constipation
some pigs may recover
Clinico-pathological features in other animals
naturally-acquired anthrax in dogs, cats, wild carnivores resemble the disease in pigs, with gastrointestinal and or pharyngeal signs
anthrax in birds is reported to be an acute septicemic disease with death occuring soon after clinical signs appear
Clinico-pathological features in humans
incubation period:
cutaneous: 1-20 days; but most develop within 7-10 days
gastrointestinal: 1-7 days
injectional: 1-10 days
inhalational: highly variable
cutaneous
gastrointestinal
inhalation
uncommon
Diagnosis of Anthrax
detecting the agent in a blood sample from a carcass (blood culture)
obtained by making a small cut in an ear vein
syringe at any available vein
bacteremia is rare in pigs
small piece of affected lymphatic tissue is often collected aseptically
tissue aspirates
pharyngeal swabs
nasal turbinates
useful in older carcasses (more than 3 days)
stained smear
Gram-stain:
Gram-positive, thick, long, straight bacilli with square or truncated ends with parallel sides, usually arranged in single pairs or chains of three or four bacilli
polychrome methylene blue (M’Fadyean stain) stain:
capsulated bacilli (pink capsule surrounding dark blue bacilli, often square-ended, singly, or in short chains)
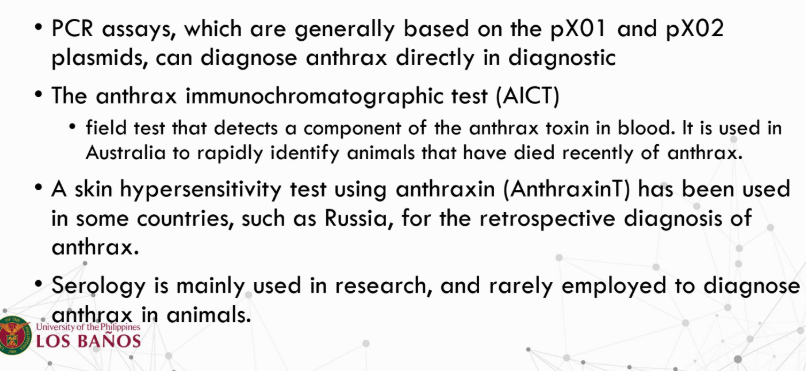
PCR
anthrax immunochromatographic test (AICT)
skin hypersensitivity test using anthraxin (AnthraxinT)
serology
mainly used in research, rarely in diagnosis
Treatment for Anthrax
penicillins
streptomycin may be given to act synergistically with penicillin
tetracyclines
Prevention and Control
modified live vaccines
quarantine
proper carcass disposal
infected carcasses should not be opened, it should
be burned and discharged
• carcass disposal by deep burial (6 feet), quicklime
(calcium oxide) carcass covered with soil mixed
with quicklime (3:1).
improvements in industry standards to reduce occupational exposure
protective clothing and equipment when examining sick animals
postexposure antibiotic prophylaxis, continued for at least 60 days, and vaccination - people exposed to aerosolized anthrax spores