LE1_ (8) Oxidation of Hexoses
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
Glycolysis is also known as?
Embden-meyerhof pathway
Glycolysis generates precursors for biosynthetic pathways such as:
Pentose Phosphate Pathway
Glycogenesis
Gluconeogenesis
Glycolysis occurs in which cell compartment?
Cytosol
T or F? Glycolysis is the only source of energy for Erythrocytes.
True
What is the main Glucose Transporter?
GLUT
T or F? GLUT or Na+ independent Facilitated Diffusion is a type of Secondary Active Transport.
FALSE. It’s Passive Transport (Facilitated Diffusion)
SGLT or NA+ Monosaccharide Cotransporters can be found in?
Small Intestine
Renal Tubules
Choroid Plexus
Where can GLUT transporters be found?
Plasma Membrane
GLUT1: The one and only basic transporter. Found everywhere, including the blood and brain.
GLUT2: "Too much" glucose. Handles high levels in the liver, pancreas, and small intestine.
GLUT3: The three most vital things: brain, neurons, and sperm.
GLUT4: For insulin. Found in the muscles and fat (adipose tissue).
GLUT5: F for Five and Fructose. Found in the small intestine and testis.
A person has been fasting overnight. Which glucose transporter, with its high affinity for glucose, ensures a constant supply to the brain, even when blood glucose levels are low?
A. GLUT5
B. GLUT2
C. GLUT1
D. GLUT4
C. GLUT1
GLUT1: The one and only basic transporter. Found everywhere, including the blood and brain.
The high Km of GLUT2 in the liver is physiologically significant because it allows the liver to:
A.Rapidly increase its rate of glucose uptake when blood glucose levels are high after a meal.
B.Maintain glucose uptake even when blood glucose is very low.
C.Transport glucose in an insulin-dependent manner.
D.Saturate its glucose transport at normal blood glucose concentrations.
A.Rapidly increase its rate of glucose uptake when blood glucose levels are high after a meal.
GLUT2: "Too much" glucose. Handles high levels in the liver, pancreas, and small intestine.
A patient is given a dose of insulin. Which of the following is the most likely physiological response involving GLUT4?
A.Skeletal muscle and adipose tissue increase their uptake of glucose from the blood.
B.GLUT4 is removed from the plasma membrane of skeletal muscle cells.
C.The liver increases its rate of glucose transport and storage.
D.The brain begins to increase its glucose uptake and store it as glycogen.
A.Skeletal muscle and adipose tissue increase their uptake of glucose from the blood.
Insulin stimulates the translocation of GLUT4 to the cell surface in these tissues, leading to increased glucose uptake from the bloodstream.
Which of the following describes a key characteristic of the GLUT3 transporter?
A. It is insulin-sensitive and found in skeletal muscle.
B. It has a high Km and is most active after a meal.
C.It transports fructose with a high affinity.
D.It is a high-affinity transporter that provides a continuous supply of glucose to neurons.
GLUT3's high affinity ensures that the brain and neurons, which have a high and constant energy demand, can take up glucose even when blood levels are low.
D. It is a high-affinity transporter that provides a continuous supply of glucose to neurons.
Why would a transporter like GLUT1, which is found in the blood-brain barrier, be insulin-independent?
A.
GLUT1 only transports fructose, which is not affected by insulin.
B.
The brain needs glucose constantly, and its supply cannot be dependent on fluctuating hormone levels.
C.
GLUT1 is only active when blood glucose levels are extremely high.
D.
The brain's energy needs are so high that it can store glucose for later use.
B.
The brain needs glucose constantly, and its supply cannot be dependent on fluctuating hormone levels.
During a period of prolonged fasting, which transporter is responsible for providing the small intestine with glucose from the blood for its own energy needs?
A.
GLUT2
B.
GLUT1
C.
GLUT3
D.
GLUT4
B.GLUT1
As the ubiquitous, insulin-independent transporter, GLUT1 is responsible for providing basal glucose uptake to tissues that need it constantly, including the small intestine for its own energy.
A scientist develops a drug that blocks GLUT5. What is the most likely metabolic consequence?
A.
Reduced absorption of fructose from the small intestine.
B.
Decreased glucose absorption from the small intestine.
C.
Increased glucose uptake in skeletal muscle.
D.
Inability of the pancreas to sense high glucose levels.
A.
Reduced absorption of fructose from the small intestine.
Heart muscle is a unique tissue because it expresses both GLUT1 and GLUT4. Which of the following best describes the function of both transporters in the heart?
A.
GLUT1 handles insulin-dependent glucose uptake, and GLUT4 handles insulin-independent uptake.
B.
Both transporters are primarily active in the fasted state.
C.
GLUT1 handles glucose uptake in the fasted state, while GLUT4 handles glucose uptake in the fed state.
D.
Both GLUT1 and GLUT4 transport fructose.
C.GLUT1 handles glucose uptake in the fasted state, while GLUT4 handles glucose uptake in the fed state.
A person eats a large meal. In the pancreas, the resulting high blood glucose levels signal for insulin release. Which transporter is responsible for bringing glucose into the pancreatic beta cells to trigger this response?
A.
GLUT1
B.
GLUT3
C.
GLUT2
D.
GLUT4
C.
GLUT2
The testis, like the brain, requires a constant supply of energy. Which transporter found in the testis is primarily responsible for providing energy for sperm?
A.
GLUT2
B.
GLUT4
C.
GLUT5
C.
GLUT5
__glycolysis yields 18x more energy than _
Aerobic Glycolysis > Anaerobic Glycolysis
Where does anaerobic glycolysis occur?
Cornea
Testis
Erythrocytes
Leukocytes
Exercising Skeletal Muscles
Renal Medulla
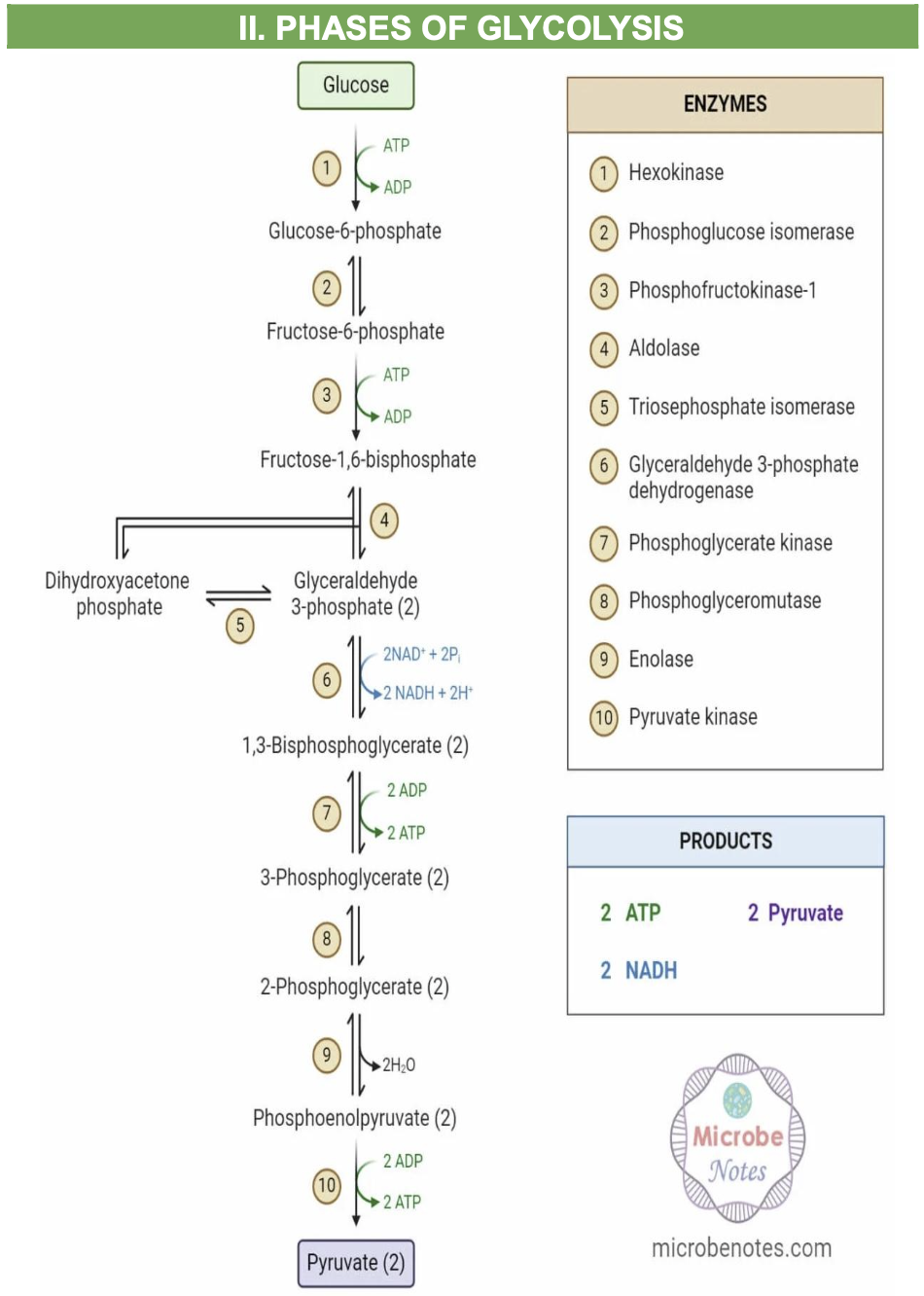
Phases of Glycolysis
What are the NET products of Aerobic Glycolysis?
2 Pyruvate
2 ATP
2 NADH
The first __ reactions of glycolysis corresponds to the energy investment phase in which moles of ATP are used
First 5 reactions = energy investment phase
What are the 2 enzymes responsible for the committed steps?
1) Phosphofructokinase 1
2) Pyruvate kinase
T or F? The Step 1, 3 and 10 are the irreversible and regulated steps in Glycolysis.
True.
This IRREVERSIBLE involves:
Hexokinase/Glucokinase
Phosphofructokinase1
Pyruvate kinase
What is the first Irreversible reaction in Glycolysis that utilizes ATP?
Glucose + ATP → Glucose-6-phosphate (Phosphorylation reaction) + ADP
Catalyzed by: Hexokinase or Glucokinase in the presence of Mg2+
T or F? Hexokinase 1,2 & 3 can be found in the Liver/Pancreas.
False. Hexokinnase 1, 2 & 3 occur in EXTRAHAPATIC tissues.
Hexokinase
1) Occurs in?
2) Km?
3) Affinity to substrate?
4) Specificity?
5) Function?
Hexokinase
1) Occurs in all tissues (extrahepatic)
2) Km LOW Km
3) Affinity to substrate? High affinity to substrate
4) Specificity? Glucose, Fructose, Galactose & Mannose
5) Function? Fasting state
Glucokinase
1) Occurs in?
2) Km?
3) Affinity to substrate?
4) Specificity?
5) Function?
GLUCOKINASE
1) Occurs in Liver & Pancrease
2) Km High Km!
3) Affinity to substrate? Low affinity to substrate
4) Specificity? Glucose ONLY
5) Function? FED state
Glucose-6-p → Fructose-6-p
1) Reaction?
2) Enzyme?
3) Reversibility?
1) Reaction? aldose to ketose isomerization
2) Enzyme? Phosphoglucoisomerase
3) Reversibility? reversible
Fructose -6-p → Fructose 1,6 bisphosphate
1) reaction?
2) Enzyme?
3) Cofactor?
4) Reversibility?
Fructose -6-p → Fructose 1,6 bisphosphate
1) reaction? Phosphorylation
2) Enzyme? Phosphofructokinase
3) Cofactor? Mg2+
4) Reversibility? 2nd IRREVERSIBLE STEP and 1st COMMITTED STEP
Fructose 1,6 -Bisphosphate → DHAP + G3P
1) Reaction?
2) Enzyme?
3) Reversibility?
Fructose 1,6 -Bisphosphate → DHAP + G3P
1) Reaction? Cleavage
2) Enzyme? Aldolase (lyase)
3) Reversibility? Reversible
DHAP → G3P
1) Reaction?
2) Enzyme?
3) Reversibility?
1) Reaction? Isomerization
2) Enzyme? Triosphosphate isomerase
3) Reversibility? Reversible
Each step in the energy-generation phase is done how many times? and Why?
twice! due to the presence of 2 G3P after the energy-investment phase!
What is the 1 and ONLY REDOX reaction in Glycolysis/oxidation of hexoses?
G3P → 1,3 bisphosphoglycerate
G3P → 1,3 bisphosphoglycerate
1) Reaction?
2) Enzyme?
3) Reversibility?
4) Products?
G3P → 1,3 bisphosphoglycerate
1) Reaction? Redox reaction
2) Enzyme? G3P dehydrogenase
3) Reversibility? Reversible
4) Products? NADPH and 1,3 bisphosphoglycerate
What is the effect of Arsenic on Glycolysis?
Arsenic replaces Inorganic Phosphate.
G3P → 1 arseno-3-phospho D-glycerate instead of 1,3, bisphosphoglycerate… kaya 0 NET ATP yield
NADH is formed but cannot be transported into mitochondria
What is the first site of ATP production in Glycolysis?
1,3 Bisphosphate → 3 Phosphoglycerate
T or F? The production of a high energy phosphate bond is usually followed by substrate-level phosphorylation.
True
1,3 Bisphosphate → 3 Phosphoglycerate
1) Reaction?
2) Enzyme?
3) Reversibility?
4) Products?
1) Reaction? Substrate level phosphorylation
2) Enzyme? Phosphoglycerate Kinase
3) Reversibility? Reversible
4) Products? ATP + 3 Phosphoglycerate
What specialized shunt is see in erythrocytes (due to absence of mitochondria)?
Rapoport-Luebering Shunt
The RLS or rapoport-luebering shunt produces (blank) which binds to hemoglobin which reduces hemoglobin’s affinity to oxygen and thus, more unloading of O2 into the tissues.
2,3-bisphosphoglycerate
3 phosphoglycerate → 2 phosphoglycerate
1) Reaction?
2) Enzyme?
3) Reversibility?
1) Reaction? isomerization
2) Enzyme? phosphoglycerate mutase
3) Reversibility? reversible
2 phosphoglycerate → phosphoenolpyruvate
1) reaction?
2) Enzyme?
3) Cofactor?
4) Reversibility?
1) reaction? Dehydration
2) Enzyme? Enolase
3) Cofactor? Mg2+
4) Reversibility? Reversible
Phosphoenolpyruvate +(ADP) → Pyruvate
1) reaction?
2) Enzyme?
3) Reversibility?
4) Product?
1) reaction? substrate level phosphorylation
2) Enzyme? pyruvate kinase
3) Reversibility? Irreversible
4) Product? Pyruvate + ATP
What are the 2 fates of pyruvate in Anaerobic Pathways?
Acetaldehyde + Lactate
What are the 4 fates of pyruvate in Aerobic Pathways?
Alanine
Acetyl CoA
Oxaloacetate
PEP
In Anaerobic glycolysis in the RBC, NAD+ (does or does not?) enter the mitochondria.
DOES NOT. Instead NAD+ is reduced by lactate dehydrogenase to produce pyruvate or lactate.
In Aerobic glycolysis, NADH is transported into the mitochondria to obtain?
ATP
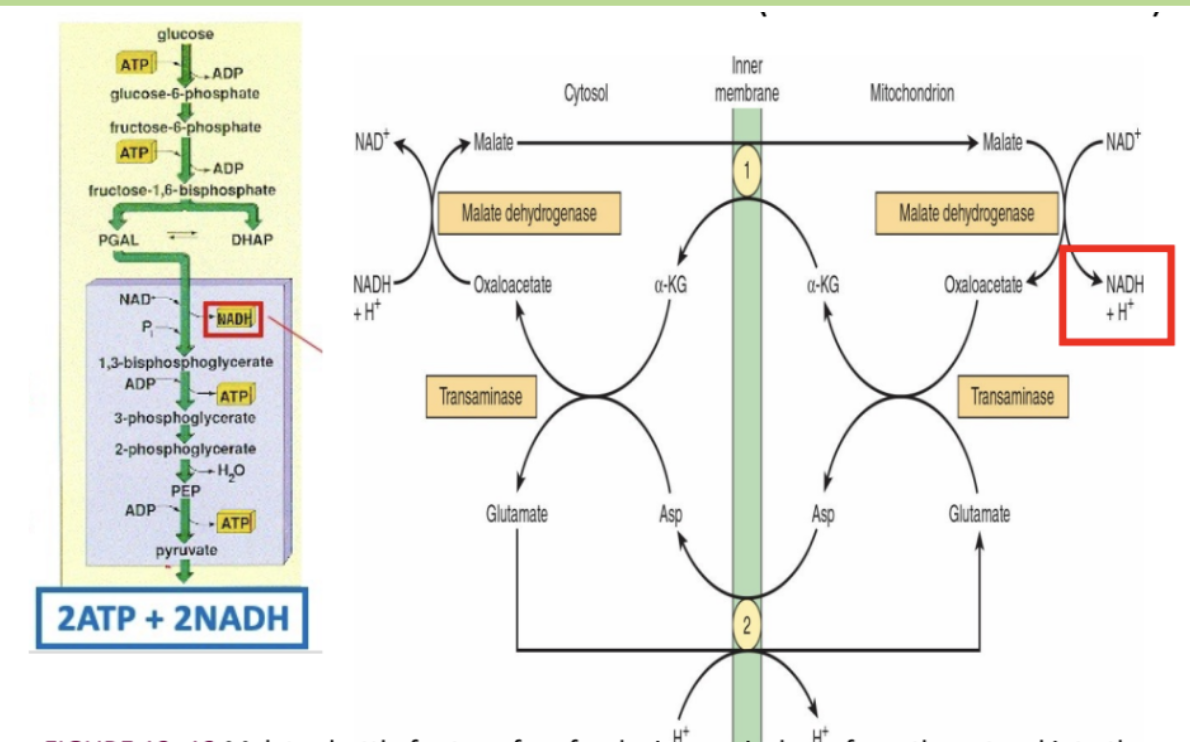
Malate-aspartate shuttle
1) Conversion to FADH2?
2) Where can this process be found?
1) NO need
2) Liver and Heart
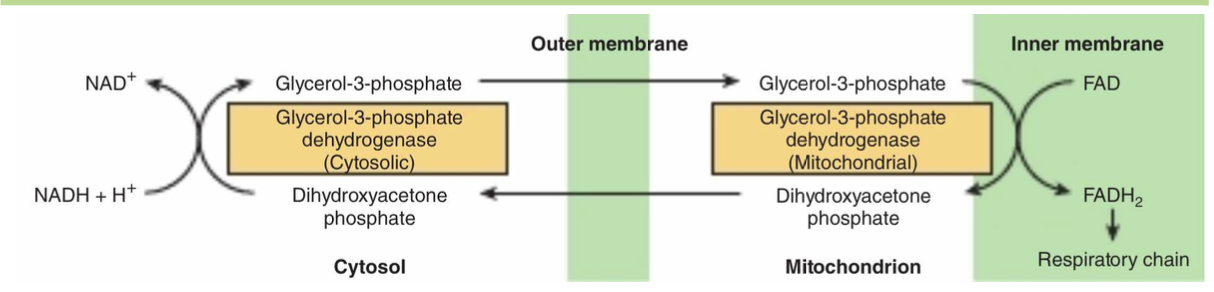
Glycerophosphate shuttle
1) Conversion to FADH2?
2) Where can this process be found?
1) Need pa
2) Brain and muscles
What happens in the malate-aspartate shuttle?
NAD+ is oxidized from NADH in the cytosol via the formation of malate from oxaloacetate.
Malate can cross the inner membrane in exchange for alpha-KG which is eventually converted back to oxaloacetate and release NADH inside the matrix.
NADH is = __ ATP
NADH = 2.5 ATP
For every NADH that enters through the glycerophosphate shuttle, we are getting a FADH2 which is equivalent to ____ATP
For every NADH that enters through the glycerophosphate shuttle, we are getting a FADH2 which is equivalent to 1.5 mol ATP
Which of the following enzyme deficiencies are directly linked to Hemolytic Anemia according to the provided text?
A.
Lactate dehydrogenase and Glyceraldehyde-3-phosphate dehydrogenase deficiency
B.
Hexokinase and Phosphofructokinase I deficiency
C.
Pyruvate kinase and Aldolase A deficiency
D.
Enolase and Phosphoglycerate mutase deficiency
C.
Pyruvate kinase and Aldolase A deficiency
What is the specific type of anemia caused by pyruvate kinase deficiency, as described in the provided text?
A.
Macrocytic anemia
B.
Sickle cell anemia
C.
Iron deficiency anemia
D.
Nonspherocytic hemolytic anemia
D.Nonspherocytic hemolytic anemia
Deficiency of pyruvate kinase →enzymopathies →
alter the shape of the RBC → nonspherocytic hemolytic anemia (destruction of RBC due to nonconformity to predetermined spherical shape)
A deficiency in which enzyme is associated with low exercise tolerance and muscle cramps?
A.
Aldolase A
B.
Glucokinase
C.
Pyruvate kinase
D.
Phosphofructokinase I
D.
Phosphofructokinase I
Tarui Disease is caused by a deficiency of which enzyme?
A.
Pyruvate kinase
B.
Hexokinase
C.
Phosphofructokinase I
D.
Lactate dehydrogenase
C.
Phosphofructokinase I
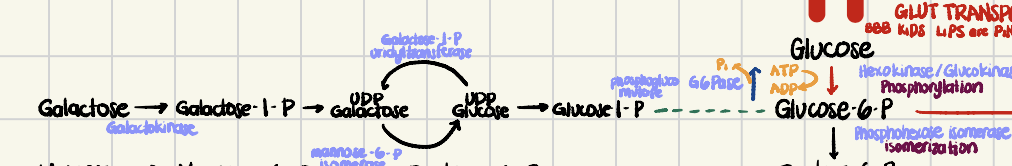
Sucrose is composed of?
Glucose + fructose
T o F? Fructose will yield the Same ATP as glucose.
True
Which steps in Glycolysis did we
bypass in Fructose Metabolism?
The steps catalyzed by
hexokinase
phosphoglucoisomerase
phosphofructokinase 1 (PFK-1) or the rate-limiting step of Glycolysis
Galactosemia is due to the deficiency of?
Galactose-1-phosphate, Uridyltransferase
Galactose metabolism generates, first, ____ which is converted to _____ The end product is glucose 1-phosphate, which is isomerized to glucose 6-phosphate, which then enters glycolysis.
Galactose metabolism generates, first, galactose 1-phosphate, which is converted to UDP-galactose. The end product is glucose 1-phosphate, which is isomerized to glucose 6-phosphate, which then enters glycolysis.