Liver Gallbladder, Pancreas, Spleen
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
What is the anatomy of the liver?
The liver is in the RUQ - inferior to the diaphragm
Neonate- 5% of body weight
Hepatocytes represent 80% of the cytoplasmic mass within the liver
Liver = 4 lobes - each lobe has a ton of hepatocytes
Blood flows past hepatocytes via sinusoids from branches of the portal vein and hepatic artery to a central vein
Central veins join form hepatic veins -which drain into the inferior vena cava
Hepatocytes
Each hepatocyte is located adjacent to bile canaliculi, which coalesce to form the common hepatic duct
The duct and the cystic duct form the gallbladder joins to form the bile duct, which enters the duodenum at a site surrounded by the sphincter of Oddi
What are Kupffer cells
Kupffer cells: macrophages located in the liver that play roles in maintaining liver homeostasis and defending against pathogens
Immune surveillance: cells engulf bacteria, viruses, and other foreign particles, protecting the liver from infections
inflammation regulation: produce inflammatory response mediators such as cytokines and chemokines to respond to infections and tissue damage
lipid metabolism: help regulate lipid metabolism by clearing cholesterol and fatty acids from the liver
fibrosis control: contributes to repair of liver fibrosis by producing collagen and other extracellular matrix components
iron metabolism: they store and release iron maintain iron balance in liver
What are the factors that affect hepatic blood flow??
What are the functions of the liver?
Detoxification
Metabolism
Immune system
Production of Bile
Storage of micronutrients
production of cholesterol
Blood sugar balance
What is the Bile formation of the liver??
What is its function
produced by??
Secreted by??
Bile helps excrete material not excreted by the kidneys and aids in the absorption and digestion of lipids via the secretion of bile salts and acids
Bile is produced by hepatocytes and is mainly composed of water, electrolytes, bile salts, bile acids, cholesterol, bile pigment, bilirubin, and phospholipids.
Secreted by hepaptocytes into bile canaliculi
Functions of the liver, fat soluble vitamin storage and metabolism
what vitamins
Fat-soluble vitamins that reach the liver via chylomicrons or VLDL are stored or metabolized in the liver
these vitamins are A, D, E, K
Vit A: stored in hepatic stellate cells
Vit D: 25-hydroxylation by the hepatic CYP-450 system
Vit E: converts Vit E into active form or excretes it
Vit K: not stored or metabolized in the liver but required for the function of coagulation factors made by the liver
Function of the liver in Drug metabolism
what are the phases
Liver metabolizes a wide range of drugs the end result of which is to produce water-soluble compounds that can be excreted in bile
Phase 1 - mediated by Cytochrome P450 via oxidation, reduction, and hydrolysis
Phase 2 - conjugation of the drug or metabolic byproducts to highly polar ligands
Phase 3 - movement of drug into the bile or bloodstream
Function of the liver: cytochrome P450
Large group of enzymes that metabolize a vast majority of substances in the body
inhibitors: block CYP450 enzyme can lead to decreased drug metabolism, causing a buildup of the drug in the body and increasing the risk of toxicity
Inducers: substances that speed up the CYP450 enzyme can lead to faster drug metabolism, which mat result in a sub-therapeutic effect and treatment failure for the drug being broken down more quickly
Functions of the liver: bilirubin metabolism
production of what
what does it transport
what is the coagulation process
what are the excreations
production: RBC - broken down in spleen liver and bone marrow - hemoglobin converted to heme then further converted into bilirubin
Transport: unconjugated bilirubin binds to albumin and is then transported to the liver
Conjugation: bilurbuin is conjugated with glucuronic acid, making it water-soluble
Excreation: conjugated travels into the intestines - converted into urobilinogen and excreted by the feces as stercobilin small amount is reabsorbed into the blood and excreted in the urine as urobilin
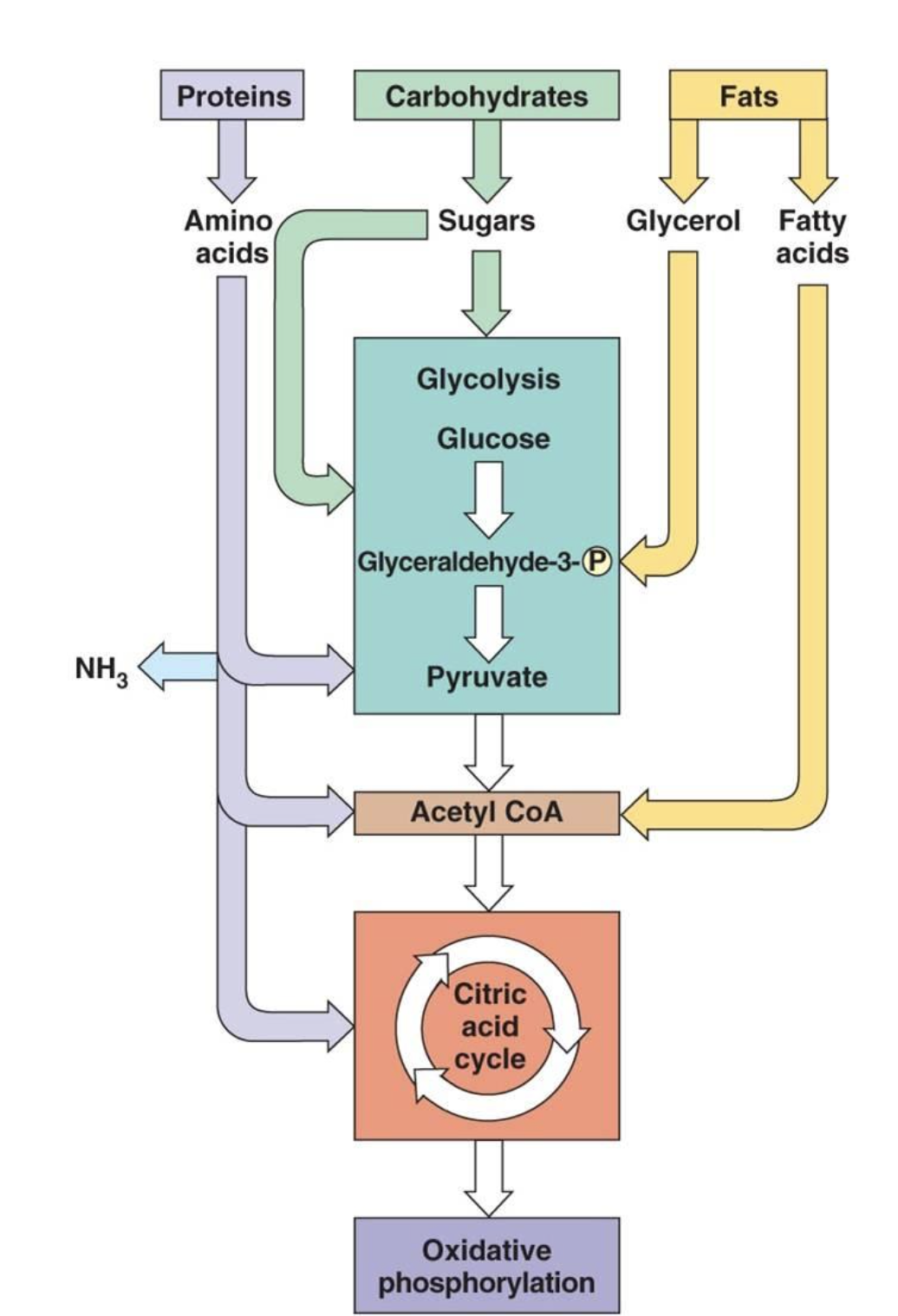
Functions of the liver concerning metabolism
What is glycogenisis
What is glucogensiis
What is glycolysis
what s fatty acid oxidation
Glycogenesis: stored glycogen for breakdown during fasting to release into blood stream to maintain stable blood sugar levels
Glucogenesis: new glucose synthesis - synthesized from non-carbohydrates to produce blood sugar occurs during prolog fasting and requires lots of energy
Glycolysis: glucose breakdown for ATP - liver takes up excess glucose and breaks it down to produce pyruvate to produce atp energy for the liver - happens in a fed state
Fatty acid oxidation and ketogenesis: during fasting or porlonged exercise - fatty acid are broken to produce energy for livers activities and to produce ketones - released into the bloodstream
Function of the liver involving protein metabolism
what is the role of the liver
deamination of amino acids
formation of urea for the removal of ammonia
formation of all plasma proteins except gamma globulin
inter-conversions of the various amino acids and synthesis of other compounds from amino acids
Functions of the liver: metabolism
How is formation of the urea taking place
What is lactulose
Formation of urea:
Ammonia formed from decomposition is highlytoxic to tissue
increased ammonia due to liver dx= hepatic coma
2 molecules of ammonia = urea
Lactulose = a drug used to bind to ammonia in the gut
ammonia will buind to only ammonia formed in the gut and allow the body to ecrete through the bowels
Functions of the liver metabolism
Liver
plays a role in thyroid hormone function as the side of deiodination of T3 and T4 → converts it to the active form
synthesis every plasma protein - protein C and S brakes for the clotting cascade
synthesis of intrinsic and extrinsic clotting factors
production of TPO - this si the main stimulator of platelet production
How do we measure liver function?
tests
AST, ALT, Alkaline phosphate, Total bilirubin, D. Bilirubin
Coagulations test: PT, PTT, INR
LDH
Platlet count
glucose levesl
What are ALT tests:
What are AST tests:
What are ALP tests:
ALT: Alt enzymes found in the liver that convert proteins for energy - if the liver is damdged, their will be ALT found in the blood
AST: Enzyme that helps the body break down amino acids - increase AST levels in the blood = liver damage, liver dx, or muscle damage
ALP: Enzyme found in the liver and one that breaks proteins - higher in blood = liver damage or dx - blockade bile duct or certain bone dx - bone enzyme too
How do we measure liver function using the cogulations test
elevated PT or INR
Thromboelstography(TEG)
will be elevated in extensive liver damage
pts with liver dx inc risk for clotting despite having elevated PT and INR
TEG real time measurement of cogulability reliable test with someone who has liver dx
How we mesure liver function based on LDH, Glucose, ammonia?
LDH: can be elevated if the liver dx but also because of other organs used to measure liver dx
Glucose: sudden drop in glucose in a setting of liver function can indicate acute liver failure - a marker for acute liver failure and carries a very high mortality rate
ammonia: normal byproduct of protein metaboilism but in liver dysfunction cannot be excreted properly
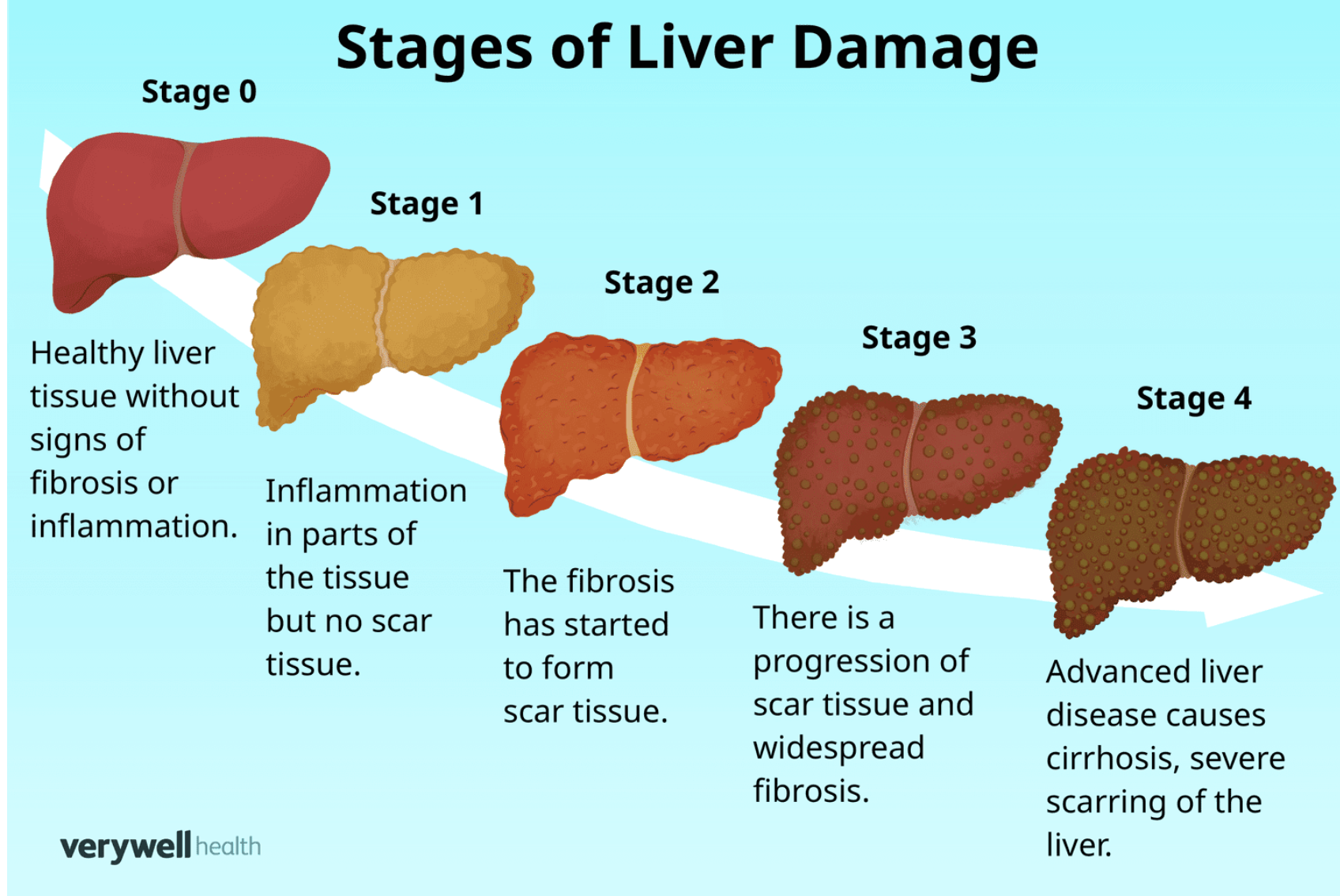
What are the stages of liver function
inflammation
fibrosis
cirrhosis
end-stage liver failure
Inflammation- the liver becomes inflated due to factors such as viral infection, alcohol abuse or autoimmune disorder
sx: pain, tenderness and swelling
Fibrosis: scar tissue formation - blocks blood flow and damages healthy liver cells
sx: fatigue, jaundice, ascities
Cirrhoisis: advanced fibrosis where ther is sever scaring and unable to function properly
sx: advanced jaundice, hepatic encephalopathy, bleeding
End-stage liver failure: loss function
sx: jaundice, coma, organ failure
The gallbladder
what is the gallbladder
RUQ
stores bile produced by the liver for emulsion of fats
Stimulated by CCK = release into common bile duct
Bile stored in the gallbladder becomes concentrated 3-10 fold
Gallbladder Pathologies
what are gallstones
What is cholecystsis
What is choledpocholitis
gallstones: form in the gallbladder because of high cholesterol or bilirubin- typically no symptoms will pass - cholelithiasis
Cholecystitis: inflamed and thickened - caused by a blockade of the cystic duct by a gallstone or infection - when it is not caused by obstruction = acalculous cholecystitis
Choledocholithiasis: common bile duct obstruction - depends on the site, obstruction can lead to pancreatitis
sx: RUQ. jaundice, elevated LFT, an elevated lipase
Gallbladder removal

Pancreas
contain??
Contains: the in between number of lobes between called ACINI
In between ACINI, there are groups of endocrine cells called the islet of Langerhans
Small ducts emerge from these lobules and unite and reunite to form pancreatic duct
What does the pancreas secrete
Exocrine and endocrine secretions
Exocrine:
digestive in function it is conveyed to duodenum through pancreatic duct, pancreatic juice contains enzymes:
Lipase: fat fatty acids and glycerol
Amylase: starcth maltose
Trypsin: peprones amino acids
Endocrine:
secreted by the islets of Langerhans ad directly poured into circulation - this secretion has 2 different hormones, which are secreted by 2 different cells of islets of Langerhans
Glucogen : secreted by alpha cells
Insulin : secreted by beta ce;ls
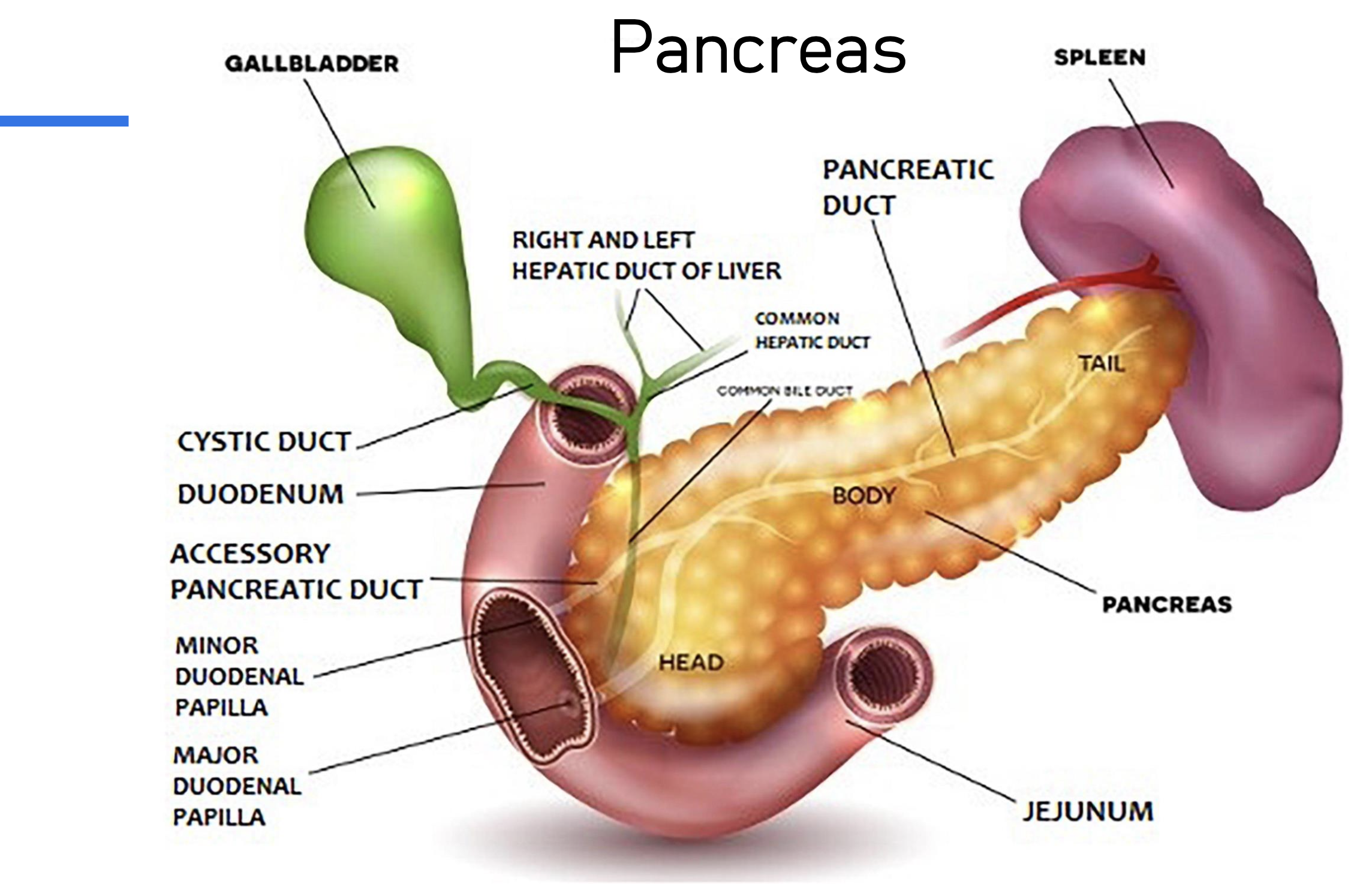
Enzymes: Amylase and lipase are secreted in their active form; ither enzymes need to be activated or else they will auto digets the pancreas itself
symogens or proenzymes are precursors too the activetd enzymes responsible for digesting proteins
Enteroopeptides: Enzyme produced y the duodenum - the first part of the small intestine - critical firs step - it cleaves and activates trypsinogen and trypsin
Trypsin: once activated, this enzyme starts the domino effect activating other pancreatic enzymes
Pancreatitis:
what is it
hows it caused
Sx
Can be acute or chronic - caused by an infection, diet related - alcohol, obstructive, or elevated Calcium
Sx: recurring abdominal pain, weight loss, diarrhea and oily foul- foul-smelling stools due to inability to properly digest food- can lead to the development of diabetes
Necoritizing pancreatitis:
what is it
What can it cause
Pancreatic tissue dies Leads to:
infection
hemorrhage
abdominal compartment syndrome
multisystem organ failure
AKI
Pancratic cancer
What is it caused by
What are the Sx
What is the prognosis
The majority is from Adenocarcinomas, small percentage is from neuroendocrine tumors that arise from hormone-producing cell
Sx: not present until very late in stages - later diagnosis and higher mortality
jaundice, abdominal pain, weight loss, nausea and voimmiiting, dark urine, light-colored stools, fatigue, new-onset diabetes
Prognosis: very poor prognosis 5 5-year - 12% live
Spleen:
Where
Functions??
LUQ - can live without spleen
Filtering blood: remove old
immune function: Contains WBC that help fight infections, stores macrophages
Blood storage: stores and release in an emergency such as bleeding
Regulation of blood cell production: spleen monitors the numebr of RBC in the body and tells the bone marrow to make more
lymphatic drainge: spleen helps drain lymph fluid from abdominal area
What is the Spleens recycling process?
RBC age they become less efficient at carrying oxygen
The spleen detects the old cells and tears them in its red pulp
Macrophages WBC spleen engulf and break down the old red blood cells
iron and other components from are recycled and used to produce new rbc
RBC -breakdown sent to liver and the body - bilirubin and iron
Spleen injuries can be minimal to severe
splenectomy
splenic embolization
Splenectomy: surgical removal of the spleen
Splenic embolization: minimally invasive procedure used to block blood flow in the spleen’s artery using coils or other materials - it is used to treat conditions like tramua, blood disorders, and splenic aneurysms