SVU Final
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
129 Terms
factors that impact one’s response to maltreatment
Child’s age, Severity of maltreatment,Chronicity of maltreatment, History of past maltreatment or other traumatic experiences, Response from caretakers
Physical neglect
failure to meet adequately the physical needs of children
Emotional neglect:
Absence of emotional responsiveness by a caretaker, rejection, isolation, unreliable or inconsistent parenting that could cause the child to develop behavioral, cognitive, emotional or mental disorders
types of neglect
physical and emotional
While child welfare data show that _______ is the most common form of substantiated maltreatment on the national level…
neglect
Physical abuse has been shown to be associated with:
Serious injury in childhood, Peer relationships in childhood, Aggression in childhood, Physical health problems in adulthood, Mental health problems in adulthood, Alcohol and drug use in adulthood
Until recently ___________ ___________ was considered an appropriate form of discipline
physical punishment
In the literature, most studies have found that corporal punishment is more common among ___________ families compared other families
Black/African-American
long-term effects of corporal punishment
In a study following over 2,500 toddlers from low-income White, African-American and Mexican-American families, spanking at age 1 predicted aggressive behavior problems at age 2 and lower cognitive development scores at age 3 (Berlin et al 2009)
• A study of nearly 7,000 children included in the National Longitudinal Study of Youth found a connection between corporal punishment and both initial levels of children’s anti-social behavior and changes in such anti-social behavior (GroganKaylor 2005)
A study of 649 college students showed an association with corporal punishment in childhood and depression in young adulthood, with high levels of parental anger during punishment having particularly detrimental effects (Turner & Muller 2004)
Although spanking is usually followed by short-term compliance, it does not lead to ______ _______ it can lead to more _______ children and the desired behavior is not usually present when the punitive parent is absent
new learning; aggressive
Why do children not disclose sexual abuse?
• If the abuser is someone the child or the family cares about, the child may worry about getting that person in trouble
• Children often believe that it was their fault (shame, guilt)
• Children may fear disclosure because they think they will get in trouble themselves
• Very young children may not have the language skills to communicate about the abuse • Children may not understand that the actions of the perpetrator are abusive
• Threats of bodily harm (to the child and/or the child’s family) • Fears of being removed from the home
• Fears of not being believed
culture and disclosure of sexual abuse
In cultures where sexuality is not spoken about, children may be less likely to disclose
• If the abuse was perpetrated by someone of the same sex, children may not disclose for fear of homophobic reactions
• In cultures where female virginity is valued, children may not disclose due to fears about being considered “damaged goods”
What are the consequences of sexual abuse?
Increased sexually inappropriate behaviors • Increased episodes of running away and truancy • Decreased sense of self and self esteem • Increased episodes of depression • Increase substance use • Increased suicidality • Increased rates of teen pregnancy • Increased rates of abuse of others; 40% of sex offenders report sexual abuse as children • Increased risk of sexual exploitation
Research has found that emotional maltreatment can lead to:
• Post-traumatic stress • Emotional dysregulation • Maladaptive coping • Disordered eating • Social withdrawal • Aggression • Poor adult relationships • Anxiety, depression and negative self-association • Psychosis
Most child maltreatment reports come from ________ ________
mandated reporters
alternative responses
Designed for “neglect only” allegations • Family assessment (vs. child protective investigation) • Does not result in a determination (indicated or unfounded) • No court involvement • Part of racial equity strategy • “collaborative, unintrusive response”
NYC Preventative Services
• Services to families at risk of foster care placement – functions as social safety net • Run by community organizations who contract with ACS • Most services voluntary • 75+% of families referred by child protection • Joint focus on needs of parents and safety of children • Case management, some on-site services • Mandates for health and mental health care not as strong as for foster care • 12-month length of service goal
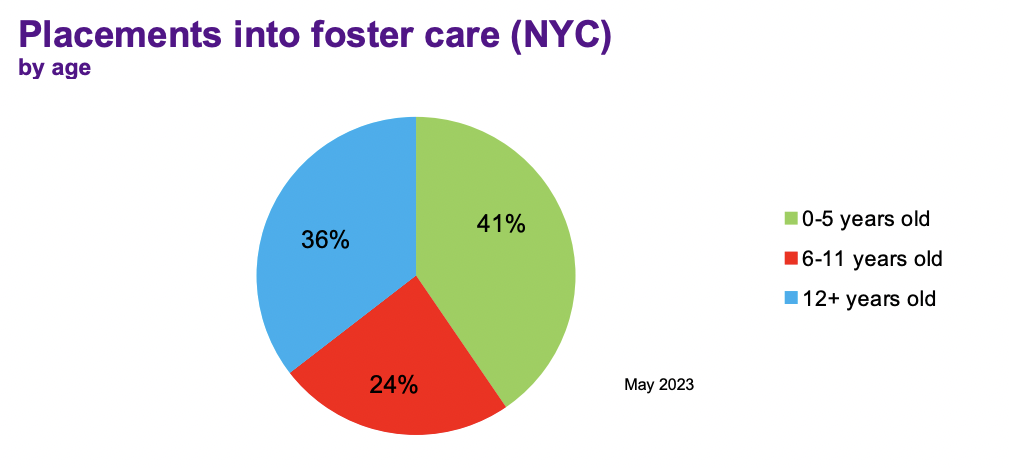
Foster Placements by age
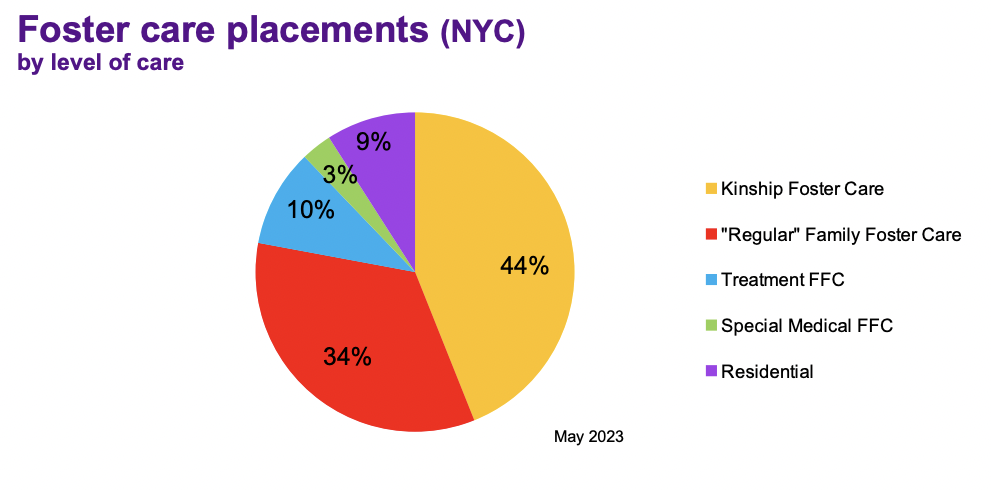
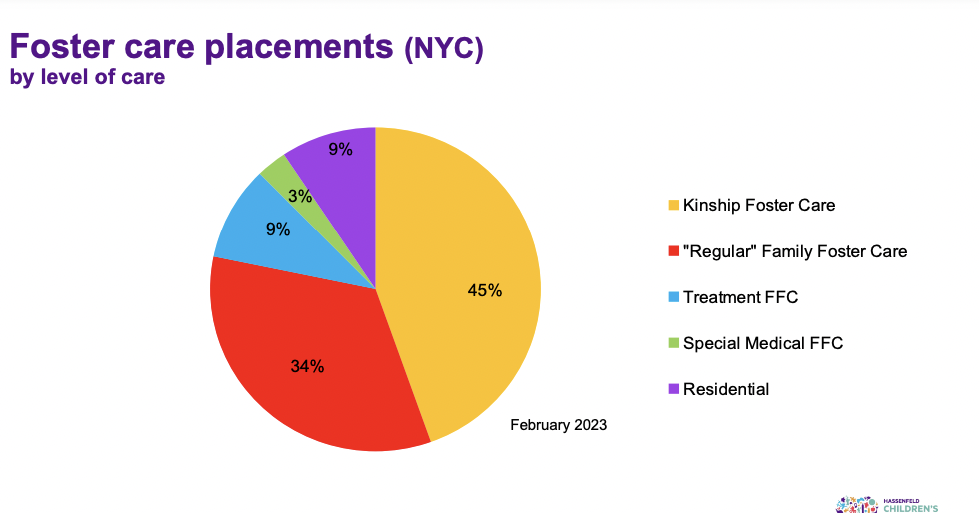
Foster placement stats by level of care
Native American History with CWS
Long history of removing Native American children from their families, placement with white families and/or in institutions that forbade practices related to culture, religion and language • Goal was assimilation into mainstream society: “Kill the Indian, save the man” • Removed impediments to manifest destiny • High rates of institutional abuse • In many states, practice continues in high rates of removal and foster care placement • Canada recently reached billion-dollar settlements to address discrimination within its child welfare system and to pay reparations to indigenous families
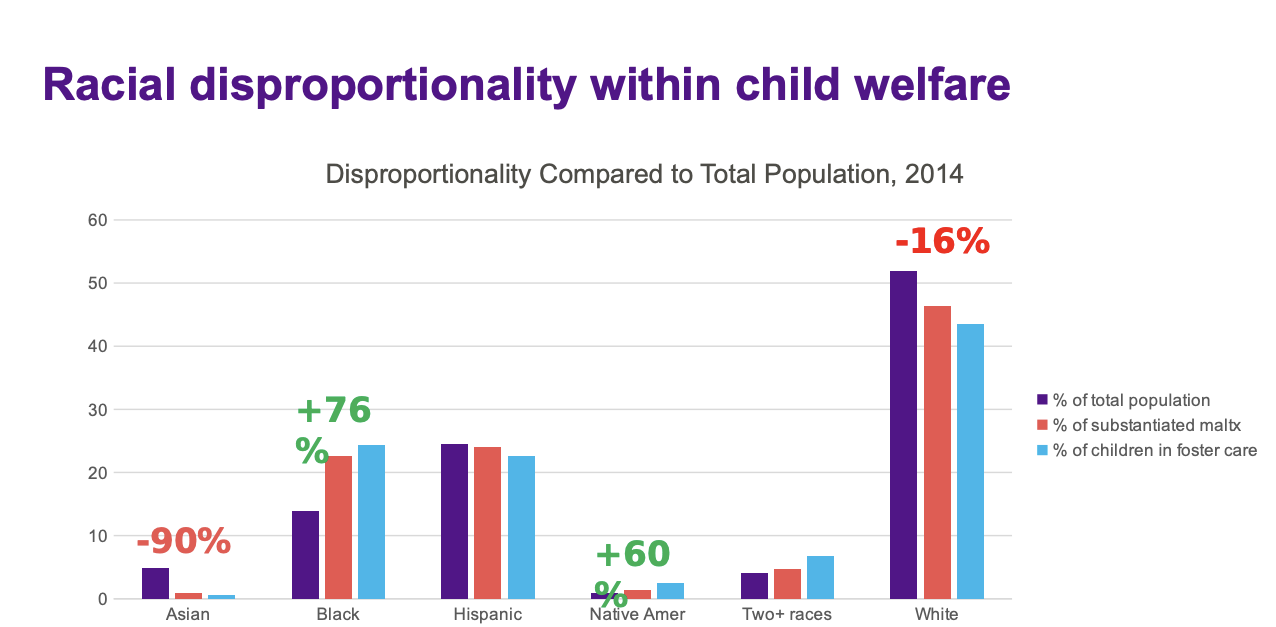
Race proportionality in CWS
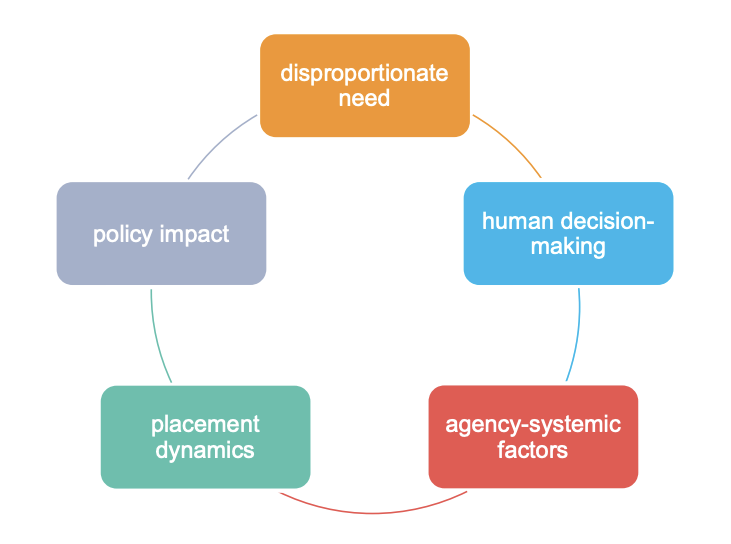
Boyd’s factors of disproportionality
Research on maltreatment and poverty
• Individual poverty- Brown, Cohen et al (1998) found that families’ welfare and income status was linked with neglect (OR=11.01, 95% CI 5.61-21.58 for welfare recipients, and OR=5.11, 95% CI 2.59- 10.07 for low-income families) and physical abuse (OR=3.74, 95% CI 1.78-7.85).
• Community poverty- Looking at low, moderate and high poverty zip codes, Drake and Pandey (1996) found that poverty was mostly starkly associated with neglect (ratio of 1:9:46) and physical abuse ratio of 1:6:19). Sexual abuse reports were the least common overall and also the least associated with poverty, with an approximate ratio of 1:2:4.
• Disentangling substantiation: The influence of race, income, and risk on the substantiation decision in child welfare (Dettlaff et al 2011) – main findings:
• Looked at the decision to substantiate alleged maltreatment, accounting for families’ race and income • When income was controlled for, race was not a statistically significant factor • When caseworker perception of risk was also controlled for, race was a stronger factor
What is the most common foster care placement?
kinship care
families first prevention services act
Federal funding for most group care is only available if states: • Assess children and determine that a high-quality group care setting will best meet their clinical needs
• Ensure those group settings address child trauma, engage families throughout and after treatment, and meet clinical needs
• To receive federal funding for children in group care, states must ensure that facilities are “qualified residential treatment programs (QRTP)” and have a trauma-informed treatment model that is designed to address and treat the assessed needs of children with serious emotional or behavioral disorders or disturbances.
• There are limited exceptions to the QRTP requirements for federal funding of group care
• Family First also allows states to receive federal funding for eligible children who are placed with their parents in licensed residential substance use disorder treatment facilities, when previously funding was only available for the child if separated from their parents
types of kinship care
Informal kinship care: • When the child’s parent/s and kinship caregiver come to their own agreement that the relative will take temporary physical custody of the child. The parent retains their right to make decisions regarding the child.
• Involuntary kinship care: • When a child welfare agency places the child with a kinship caregiver for safetyrelated reasons but does not take the child into state custody.
• Formal kinship care: • When the child is taken into state custody and placed with a kinship caregiver (who is a licensed caregiver) instead of a non-relative foster family home. This arrangement is analogous to traditional foster care: the agency has the right to make legal decisions on behalf of the child, just as they would with other foster children, but the kinship caregiver retains physical custody of the child. • In some states, kinship foster parents get less financial support than other foster parents
The Kinship Guardianship Assistance Program (KinGAP)
allows foster children to achieve a permanent placement with a committed adult who had been the child’s foster parent for at least six months.
The guardian must be: • Related to the child by blood, marriage or adoption, and the relationship can be to any degree of affinity, or • Related to a half sibling of the child by blood, marriage or adoption (to any degree of affinity) and is also seeking to become, or is, the guardian of such half sibling through KinGAP, or An adult with a positive relationship to the child that was established prior to the child’s current foster care placement
• This program provides financial support and, in most cases, medical coverage for the child, beginning with the child’s discharge from foster care to the guardian
• The level of financial support is similar to the maintenance payments received while the child was in foster care
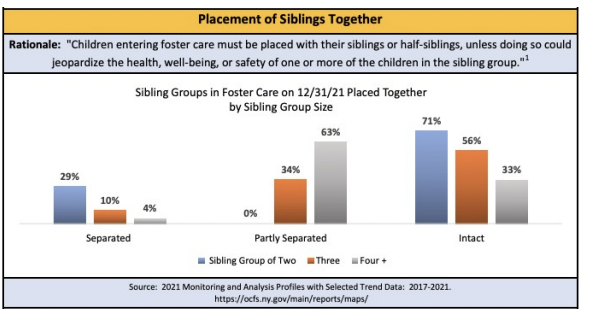
role of sibling connections
• Positive impact on well-being • Fewer internalizing behaviors following trauma • Improved school performance • Better adjustment to foster home setting • Positive impact on permanence • Higher rates of reunification, adoption, guardianship • Fewer placement disruptions
Challenges regarding sibling placements in foster care
Complex sibling groups – full, half and step-siblings • Focus on kinship placement may not align with sibling relationships • Siblings coming into foster care at different times • Siblings having different clinical needs • Foster home capacity for large sibling groups • Weigh desire to keep siblings together and desire for staying in a temporary location C
NJ Sibling’s bill of rights
In addition to cementing the right for children placed outside their home to participate in permanency planning decisions of other siblings and to invite siblings to participate in their own permanency planning decisions, when appropriate, the bill also adds the following rights for children placed outside their homes:
common responses from child to removal/separation
Fear Confusion Stress Self-blame Anger Broken attachments
common responses from parent to removal/separation
Fear Confusion Traumatic stress Self-blame Shame Anger Powerlessness Grief/loss
NYC data on sibling placement
For children who completed a mental health screening they were _________ to have more placements
more likely
Atlas Project
• Implemented mental health screening (general and trauma-specific) at five NYC TFC sites •
Out of 284 children in care for at least 30 days, only 48% had at least one screening
• Most children only had one of two screening tools completed
Factors associated with increased use of services in foster care (Garland et al, 2003):
• Male children • Older children • Non-relative foster care (vs. kinship care) • Entered care due to sexual or physical abuse • Greater severity of emotional/behavioral problems
______ children have been found to use mental health services earlier and use more mental health services than African American or Latino children
White
• Who is at greatest risk of (mental health) service discontinuation?
• Youth aging out of care (vs. those who reunified, were adopted, etc.) • Latino youth in foster care (vs. Black and White youth)
Children in foster care have medication rates of ____, compared to 4% among general population (USDHHS, 2012)
13-52%
Psychotropic medication
There are five main types of psychotropic medications: antidepressants, anti-anxiety medications, stimulants, antipsychotics, and mood stabilizers.
Children with trauma stress are often misdiagnosed with ….
ADHD, Conduct Disorder, Depression, and Anxiety
NCANDS
National Child Abuse and Neglect Data System • Compilation of all states’ and territories’ data related to child abuse and maltreatment • Data are mapped from states’ systems to the NCANDS system • These are the data cited in most publications that reference ”children who are maltreated” • By definition, the NCANDS data do not include children who experience maltreatment that is not reported to child welfare authorities
NIS-4 (National Incidence Survey of Child Abuse and Neglect)
• Cross-sectional study, has been completed four times • NIS-4 was completed in 2005-2006 • Combines NCANDS data with information gathered from other community sources (e.g., schools, hospitals, day care providers, etc.) in a nationally representative sample of counties • Determines whether children’s experiences meet “harm” or ”endangerment” standard • More broadly captures information about children who may have experienced abuse or neglect caused by a parent or other caretaker • In NIS-4, fewer than half of all children identified as maltreated were reported to a child welfare agency
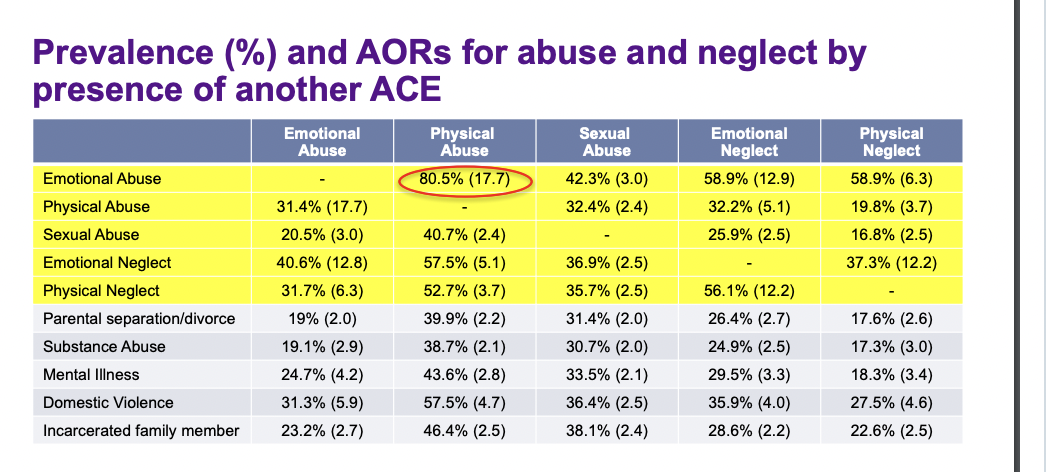
Percentages of abuse present with at least one other ACE present
Children with disabilities are _______-represented in the child welfare system
over-represented
• 5.2% of school age children overall vs. 14% of maltreatment victims (Census Bureau, Children’s Bureau)
• Among children in foster care, 1/3 have a disability (Slater, 2016)
Why are children with disabilities over-represented in the child welfare system?
Children with disabilities may be more vulnerable, more dependent on caregivers
Some children with disabilities may be targeted because they are not able to report their abuse
Families with children with disabilities have additional stressors (financial, emotional, social isolation, etc.)
Role of culture-related parenting practices
Complications with disabilities in foster care
Dual diagnoses
Rate of mental illness in people with intellectual disabilities is 3-4 times that of the general population
“Hot potato” effect: when a child has a physical, intellectual or developmental disability and mental health-related needs, systems may disagree about who has “primary” responsibility for care
Trauma-focused interventions may be a misfit for children with ID/DD, since many models require cognitive-based work, being able to articulate their traumatic experiences, doing some kind of trauma narrative
Caregiver limitations -Parents may have challenges advocating for disabled children, navigating complex systems which may contribute to foster care placement, delays in reunification
Foster home limitations- Training/licensing/regulations, Number of children is (relatively) small, making specialized programs less financially sustainable, Need for physical adaptations
Fostering Connections to Success and Increasing Adoptions Act (2008)
Allowed states to still receive federal reimbursement for foster care services provided up to age 21 under certain conditions
48 states allow youth to stay in foster care beyond 18 and 33 states allow youth over age 18 to return to foster care
Family First Prevention Services Act (2018)
shifting focus of residential care – addressing a clinical need rather than a place for older youth to be housed
FFPSA Legislation does not provide additional funding to expand family foster care resources for older youth
21 is an improvement on 18, but given that about half of 18-29-year-olds in the U.S. live with family, this still requires youth leaving the foster care system to be more __________ than their peers, with less preparation or support
self-sufficient
Teens in nyc foster homes
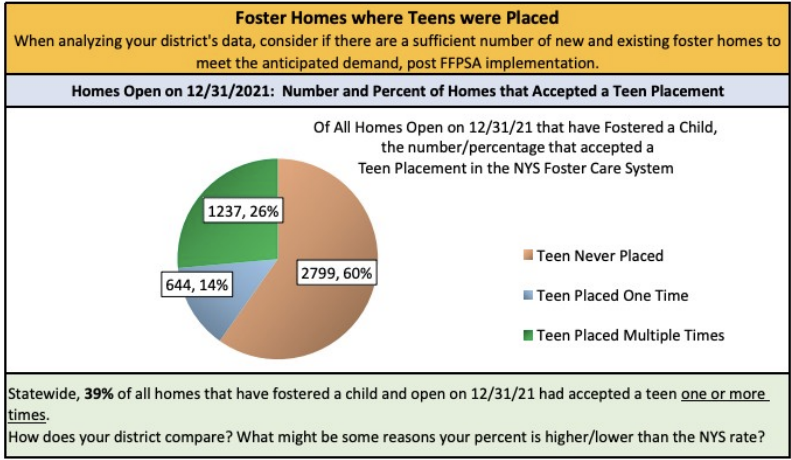
NYC ACS “Home Away From Home” initiative
“One Home, One Family”: place sibling groups together and on their own • Focus on foster parent recruitment and retention
Outreach to current FPs’ networks
’Develop’ homes for teens
Increase support to foster parents
Foster care re-entrance
Disrupted adoptions (from foster care) Can happen before an adoption is finalized and can also happen even after an adoption is finalized. Some return to their adoptive families, others remain in foster care
• Research suggests that disrupted adoptions happens in 5-25% of cases, with older children experiencing more disruption. Returend after adoption is finalized happens in 1-5% of cases
You Gotta Believe
NYC agency founded as a “homelessness prevention” program
Specifically focused on finding forever families for older youth in care
Works with foster care agencies who are looking for adoptive parents for youth in their care
Trains, certifies, and provides ongoing support to families – both parents and youth
LGBTQAI youth in foster care
Large numbers of LGBTQAI youth in foster care
In NYC, 1/3 of 13+-year-olds in care are LGBTQAI
Nationally: LGBTQ youth 2.5x more likely to experience foster care placement than other youth
More likely to experience placement disruptions
Higher risk of homelessness
More likely to be placed in residential settings
Why are LGBTQIA youth more likely to be in foster care?
Higher levels of identity-related maltreatment in homes
Higher numbers of youth leaving home on their own
Fulton v. City of Philadelphia (2021)
Because CSS believes that certification of prospective foster families is an endorsement of their relationships, it will not certify unmarried couples—regardless of their sexual orientation—or same-sex married couples.
The refusal of Philadelphia to contract with CSS for the provision of foster care services unless CSS agrees to certify same-sex couples as foster parents violates the Free Exercise Clause of the First Amendment.
The city’s actions burdened CSS’s religious exercise by forcing it either to curtail its mission or to certify same-sex couples as foster parents in violation of its religious beliefs.
The non-discrimination requirement of the City’s standard foster care contract is not generally applicable.
LGBTQIA statistics
71% of LGBTQ youth felt sad or hopeless
39% of LGBTQ youth seriously contemplated suicide
20-40% of homeless youth identify as LGBTQ
Expectant and Parenting Youth in Foster Care
High rates of early pregnancy among youth currently/ formerly in foster care
Baby is in parent’s custody even when the parent is in foster care •
Pregnancy/parenting can prompt re-placement
Pregnant youth often move to specialized programs; Most such programs are some version of residential care
Young mothers may have to move again shortly after giving birth
Challenges serving sexually active, expectant and parenting youth in care
Difficulty – on the part of resource parents, group home staff, and caseworkers – with discussing sexual activity with teens and confusion regarding who is responsible for providing them with sex education
Limitations regarding outreach to male partners who may not be in foster care
Inaccurate or inconsistent counts of the number of teens in foster care who are expectant or parenting
Insufficient tracking regarding whether teens are receiving the services they need to learn to parent effectively
Teens, staff, and resource parents’ lack of awareness of the outcomes associated with being a pregnant and parenting teen in foster care
Juvenile justice-involved youth
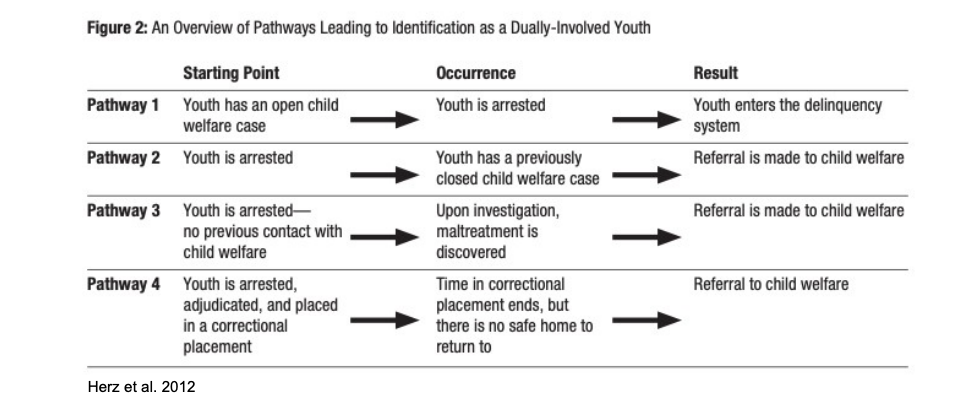
Maltreated youth are more likely to engage in delinquent behavior, have associated poor outcomes. Given this, in the field there is increased attention to the needs of maltreated youth who become involved in the juvenile justice system (“crossover youth”)
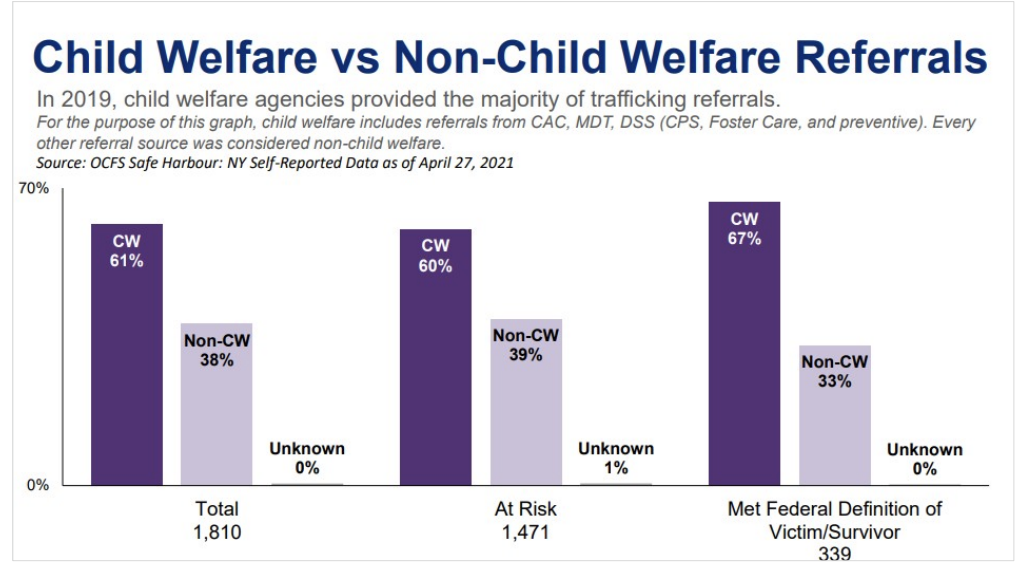
Commercially sexually exploited children (CSEC) and the child welfare system
Increased attention to the needs to CSEC youth within the child welfare system
High levels of child welfare involvement due to histories of sexual abuse
Vulnerability of child welfare population due to separation from family, desire for connection/protection
Understanding that “prostitution” requires consent, which minors cannot provide
Need for a therapeutic rather than a criminal justice approach
Child welfare vs. Non-child welfare referrals
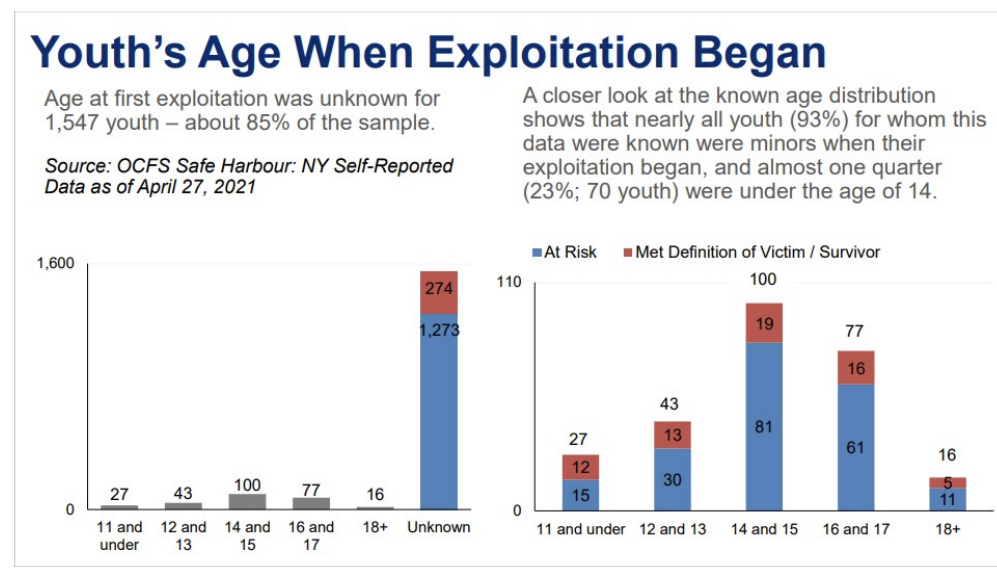
Age and sexual exploitation
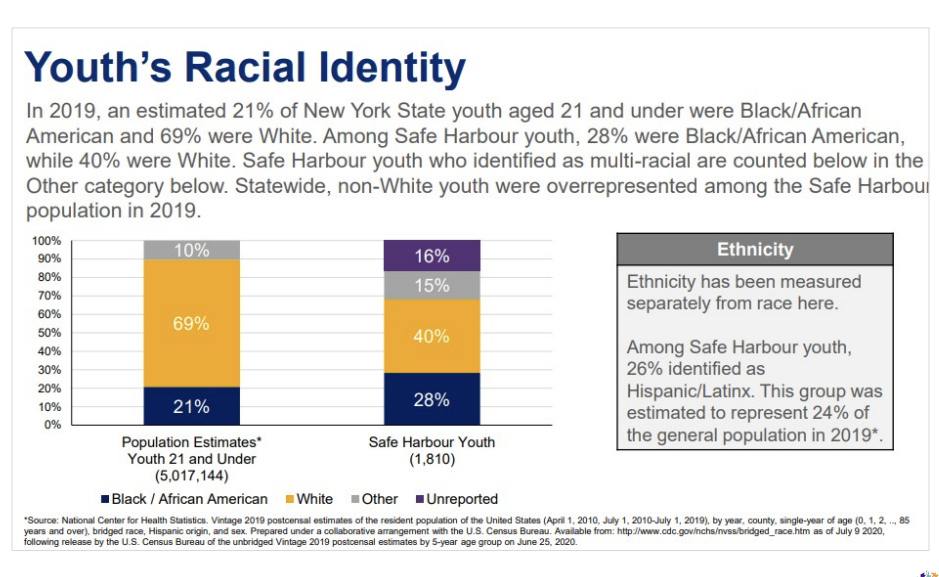
Racial Identity and sexual exploitation
Impact of child welfare system involvement on parents
When children are removed and placed in foster care, it can be very destabilizing for parents – Particularly for parents with their own history of being in foster care
Creates challenges because at the very time when important decisions are being made, parents may not be mentally/emotionally present/engaged – Trauma responses can be misunderstood as anger, disinterest, etc
predictive neglect
the concept that parents with mental health issues are likely to cause their children neglect
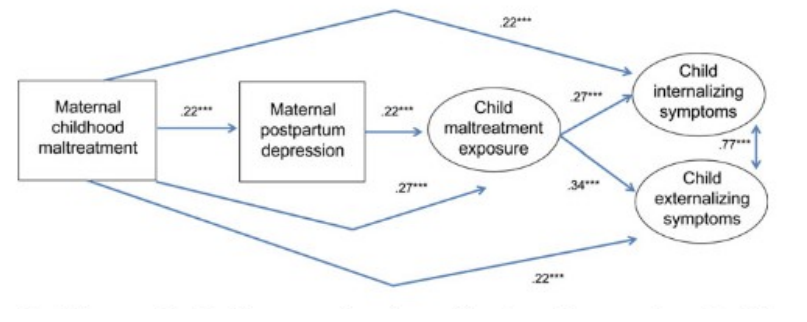
Prevalence of trauma among child welfare-involved families
Among mothers receiving preventive services, 92% had experienced a traumatic event. 19% had experienced 5 or more types of traumatic events. Most participants met probable criteria for PTSD (54%) or depression (62%); nearly half met both criteria
Among mothers receiving preventive services, 92% had experienced a traumatic event, 19% had experienced 5 or more types of traumatic events. Most participants met probable criteria for PTSD (54%) or depression (62%); nearly half met both criteria
Historical trauma
Historical trauma is multigenerational trauma experienced by a specific cultural, racial or ethnic group. It is related to major events that oppressed a particular group of people because of their status as oppressed, such as slavery, the Holocaust, forced migration, and the violent colonization of Native Americans.
Acute problems of domestic violence or alcohol misuse that are not directly linked to historical trauma may be exacerbated by living in a community with unaddressed grief and behavioral health needs. Parents’ experience of trauma may disrupt typical parenting skills and contribute to behavior problems in children.
Racial trauma
Byproduct of experiences that racial minorities deal with on a regular basis, such as micro and macro-aggressions
Buffered by level of ethnic identity
Similar symptoms to PTSD: Depression, Vigilance, Anger, Loss of appetite , apathy, avoidance, emotional numbing
Historical vs. intergenerational trauma
Intergenerational trauma is
Not experienced by a whole racial/ethnic/cultural community
Not based on the oppression of a community
How can parent’s trauma be properly addressed?
Increase knowledge about trauma
Educate child welfare staff, other stakeholders about how parents’ trauma symptoms may look
Provide information to parents about trauma and its potential impact on them/their children
Implement trauma screening for parents, within the context of effective engagement/relationship building
Increase availability of/referrals to trauma-informed interventions
Ensure that routine child welfare services are trauma-informed
Perinatal depression prevalancies
10%-40% of mothers with young children have postpartum depression (PPD)
Very few have postpartum psychosis (1-2/1,000 births)
10% of fathers have PPD, often correlated with maternal PPD •
10% of mothers in the general population have depression in a given year (Ertel et al 2011)
Higher rates found among white and Native American women, U.S.-born women, those with low levels of education or income, and those unemployed or unmarried
Post-partum depression: Causes and risk factors
Physical/hormonal changes during/following pregnancy - Dramatic drop in estrogen and progesterone following childbirth, Thyroid hormones may also drop after childbirth
Emotional responses to new parenthood (HSS, Office on Women’s Health) -Overwhelm, helplessness, loss of control over life • Lack of sleep, physical fatigue; Stress related to changes in role, routines, etc., Self-doubt, anxiety
Multiple risk factors- Having a high-risk pregnancy, Having a premature/low-birthweight infant, History of depression, Lack of childrearing support/supporting partner, High levels of stress, Low self esteem, Low family income, Distressing life events
Effects of Post-partum depression
Living with morbidity
Less enjoyment from family and life
If untreated, symptoms can worsen over time Impact on families • Mothers less attached to children
Impacts caregiving: unhealthy behaviors towards children, more emergency care, less preventive care
Poor cognitive and mental health conditions among children
Why do so few women ask for help when experiencing perinatal depression?
Supposed to be the most magical time in their lives
Stigma – asking for help means you’re a bad mother
Confusion between postpartum psychosis and postpartum depression
My mother, grandmother, great-grandmother, etc. could handle it – this is what my family/community does
Will someone take my child away?
How is perinatal depression a CW issue?
Effective responses to perinatal depression
Increase knowledge about maternal depression
How can mothers be supported/children be protected without involving the child welfare system?
What would be signs for child welfare staff that maternal depression may be a factor in alleged maltreatment?
How can parents’ fear about losing their children because of their mental health issues be effectively addressed?
Increase availability of/referrals to appropriate clinical services
Intimate Partner Violence (IPV),
also referred to as domestic violence, occurs when an individual purposely causes harm or threatens the risk of harm to any past or current partner or spouse.
IPV and Child Maltreatment co-occurence
Link between childhood exposure to maltreatment and subsequent DV-related victimization
Co-occurrence of different types of family violence
Herrenkohl and colleagues (2008) found an increased risk of physical abuse ranging from 3-15 times among families affected by IPV
Links between IPV and risk of future Maltreatment
Child welfare response to IPV
“Failure to protect” -IPV survivors were considered to be maltreating their children by ‘allowing’ them to witness violence; IPV survivors who did not seek shelter were at risk of losing custody of their children
Nicholson v. Scoppetta (NYC 2004) -A parent’s inability to keep a child from witnessing abuse could not in and of itself be a reason for removal; Agency has the responsibility to make ‘reasonable efforts’ to protect both the survivor and child
substance
“substances” refer to alcohol, nicotine and illicit drugs (both ”street” drugs
Substance use
Substance use: “use of drugs or alcohol, and includes substances such as cigarettes, illegal drugs, prescription drugs, inhalants and solvents” (HealthLinkBC)
Substance abuse (from DSM-IV): “A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12-month period:
Substance use disorders (DSM-5)
“patterns of symptoms resulting from the use of a substance that you continue to take, despite experiencing problems as a result”
Substance Use Disorder Criteria
Taking the substance in larger amounts or for longer than you're meant to
Wanting to cut down or stop using the substance but not managing to.
Spending a lot of time getting, using, or recovering from use of the substance.
Cravings and urges to use the substance.
Not managing to do what you should at work, home, or school because of substance use.
Continuing to use, even when it causes problems in relationships.
Giving up important social, occupational, or recreational activities because of substance use.
Using substances again and again, even when it puts you in danger.
Continuing to use, even when you know you have a physical or psychological problem that could have been caused or worsened by the substance
. Needing more of the substance to get the effect you want (tolerance).
Development of withdrawal symptoms, which can be relieved by taking more of the substance.
Drug additcion
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and selfcontrol. Those changes may last a long time after a person has stopped taking drugs.”
COVID-19 and substance abuse
55% reported an increase in alcohol consumption (67% in states hardest hit by COVID) 18% reported a significant increase in alcohol consumption (25% in states hardest hit by COVID) 36% reported an increase in illicit drug use
When asked for the reasons behind this increase 3% were trying to cope with stress 39% were trying to relieve boredom 32% were trying to cope with mental health symptoms, such as anxiety or depression
Access to treatment for substance abuse during COVID-19
4% of respondents reported an overdose since the start of the pandemic • 20% of respondents reported an increase in their own substance use, or in a family member’s substance use • 34% of respondents reported disruptions accessing treatment or recovery services • 14% of respondents reported being unable to access services
Child maltreatment and substance abuse
15% of victims have a caretaker with alcohol abuse 26% of victims have a caretaker with drug abuse
babies can be born with opioid addictions from drug-addicted parents
Substance abuse in the US stats
US Healthcare uses more than $740 billion dollars a year
In 2016, drug overdoses killed over 63,000 people in America, while 88,000 died from excessive alcohol use
Tabbacco is linked to an estimated 480,000 deaths per year
OD Deaths went up 29.4% in 2020
Impact of the opioid epidemic on child welfare systems
• Between 2012-2016, number of children in foster care rose 10% nationally, by 50% in AK, GA, MN, IN, MT and NH • Radel, Baldwin et al. (2018) estimated that in the average county, a 10% increase in the overdose death rate corresponded to a 4.4% increase in the foster care entry rate
Traditional drug control: a medical model
Supply reduction: • Source country control and Domestic drug law enforcement
Demand reduction: Prevention and Treatment
Harm Reduction
The modification of a behavior, and the conditions around that behavior, in order to reduce many of the most serious risks that the behavior poses to public health and safety.
‘Micro’ harm reduction: reduce average harm per use of drugs • Examples: syringe exchange, low-threshold methadone maintenance, etc.
‘Macro’ harm reduction: reduce total drug-related harm
Challenges with drug abuse treatment/prevention
Screening accuracy/timeliness
Availability of treatment
Misunderstanding/mistrust of medication-assisted treatment
“Trading one addiction for another”
NCTSN Essential Elements of a Trauma-Informed Child Welfare System
1. Maximize physical and psychological safety for children and families.
2. Identify trauma-related needs of children and families.
3. Enhance child well-being and resilience.
4. Enhance family well-being and resilience.
5. Enhance the well-being and resilience of those working in the system.
6. Partner with youth and families.
7. Partner with agencies and systems that interact with children and families.
Trauma-Informed Child Welfare Practice
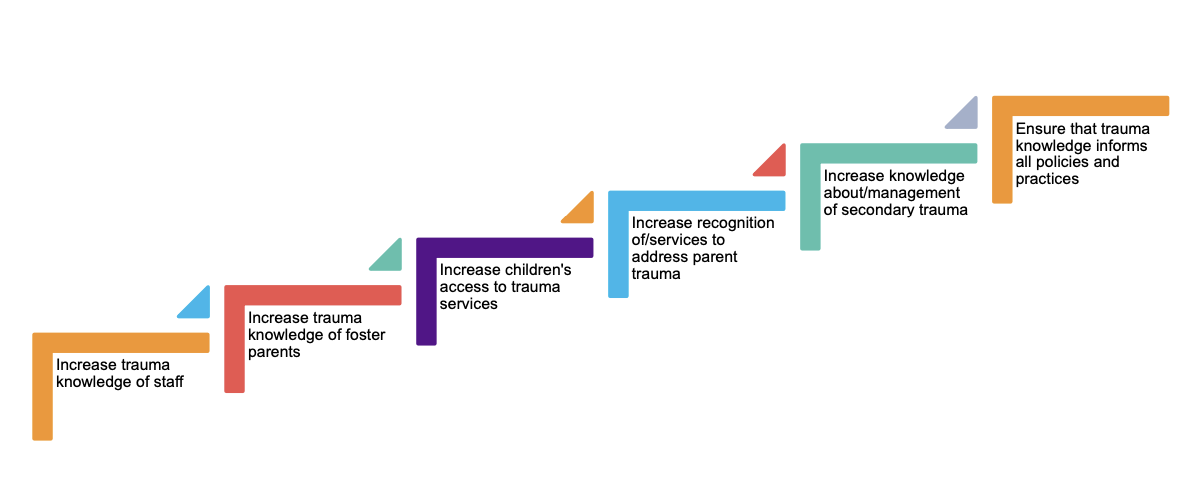
Increase trauma knowledge of foster parents
Foster parent training- Current NYC requirements: • For all foster parents: • 30 hours of MAPP training • In-service training hours annually • For treatment foster parents • 18 additional hours of “therapeutic” training • Additional in-service training annually
Specialized training/ support
CCWPI training – foster parent adaptation Training components: 1. Introduction to training series, survival state responses 2. How you use information you learn about your child – both their trauma history and their current behavior – to understand what things must be changed to better help and protect them 3. How you identify when something you’re doing is ”cat hair” for your child, and how to get help from the people on your team and in your child’s life 4. Why this work is so difficult, and how can you take care of yourself in the process of doing this difficult work`
Reframing challenges in working with traumatized parents
“Universal precautions” • Assume parents you work with have had some degree of trauma exposure • Craft response to behavior, referrals for services, etc. with that assumption in mind • Engagement, engagement, engagement! • Without trust, nothing can follow • Psychoeducation • Information about their kids’ trauma likely apply to them as well!
Child Welfare Traumameter
An organizational assessment tool designed by NYU’s Center for Child Welfare Practice Innovation to support trauma-informed practice within child welfare agencies
Helps child welfare programs fully integrate a “trauma lens” into their day-to-day activities by: Operationalizing different aspects of trauma-informed child welfare practice, Using multiple sources of information to identify areas of an agency’s practice that are currently lacking a trauma focus, Identifying priority areas for practice change and Measuring change in an agency’s practice over time