12 - Health Conditions in Children
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
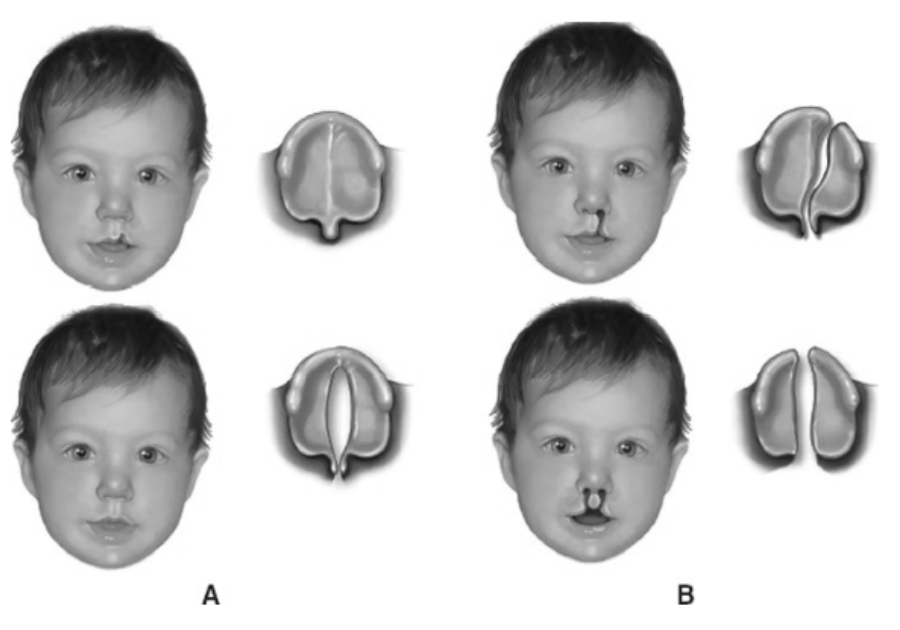
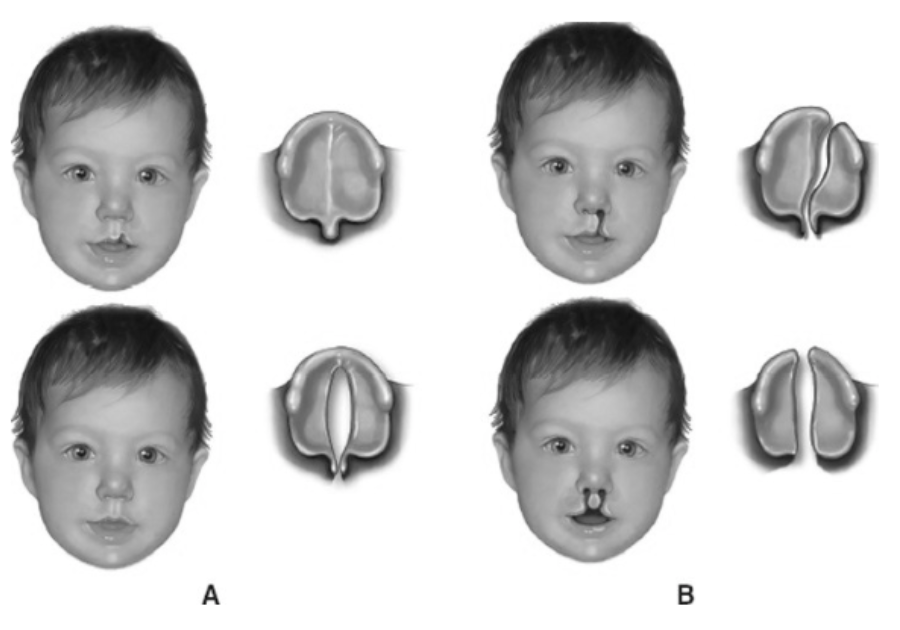
Cleft Lip and Palate
Most common craniofacial anomaly and occurs frequently with other anomalies. Although they can occur separately, usually occur together.
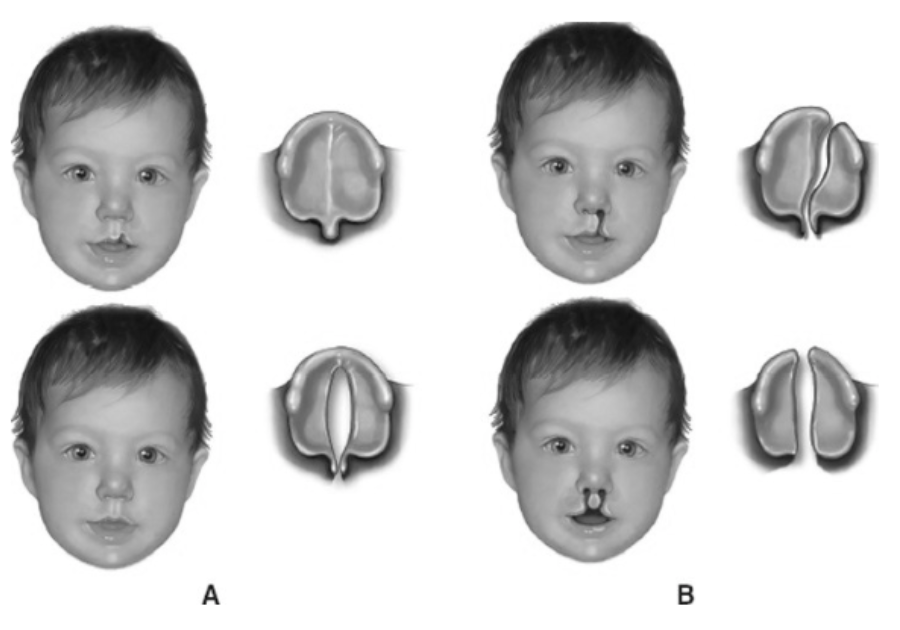
Cleft Lip and Palate
Complications include: Feeding difficulties and delayed or altered speech due to change in dentition. Can lead to more frequent ear infections (otitis media) due to alterations in muscles responsible for draining ear fluids.
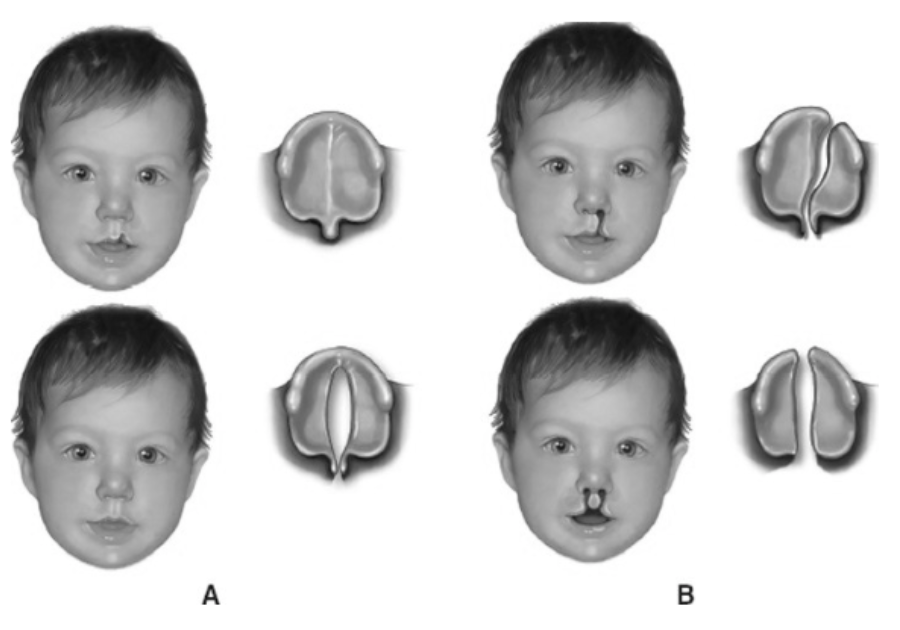
Cleft Lip and Palate
Development of the cleft occurs early in pregnancy when tissue that forms the lip and palate fail to close between 5-9 weeks gestation. Can be unilateral or bilateral.
Cleft Lip and Palate
Treatment includes:
Requires a specialist team approach: plastic surgeon, dentist, speech pathologist, etc. Surgery is always necessary due to issues with growth and development.
· Specialty orthodontics fit at birth to 3 months to allow feeding.
· Cleft lip can be repaired at 2-3 months of age.
· Cleft palate can be repaired at 9-18 months of age.
· Orthodontics and rhinoplasties are needed at 7-16 years.
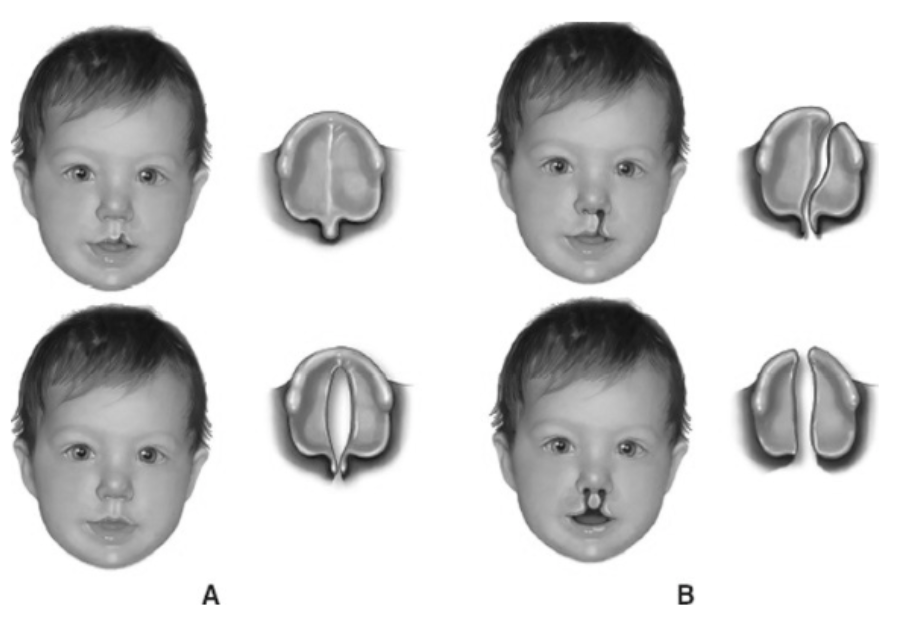
Cleft Lip and Palate
Nursing Management Includes:
• Prevent injury to the suture line by positioning the infant in a supine or side-lying position.
• After surgery, cleanse the suture line and apply protective barrier as ordered by physician. Prevent vigorous crying which causes tension to the suture line.
• Promote adequate nutrition. Enhanced nutrition is received if breastfed due to the better seal on the nipple. Most will require special cleft lip nipples if bottle-fed. Burp frequently due to difficulties sucking and greater risk for aspiration.
Hypovolemic Shock
Complication of dehydration in pediatrics. Occurs more frequently due to extracellular fluid percentage and body water ratios.
Hypovolemic Shock
Possible Causes: diarrhea, vomiting, decreased oral intake, sustained high fever, diabetic keto-acidosis extensive burns.
Hypovolemic Shock
Symptoms: increased heart rate, fever, decreased skin turgor, sunken fontanels, dry oral mucosa, dark circled eyes, pallor, altered mental status, decreased urinary output, delayed capillary refill.
Hypovolemic Shock
Diagnostics: electrolytes (increase) , BUN (increase) , creatinine (increase if DKA).
Hypovolemic Shock
Nursing Management
• Focus on restoring fluid volume. Start with oral rehydration formula, then move on to IV fluids of 20mg/kg of normal saline or ringer’s lactate as a start.
• Conduct necessary diagnostics, including blood work and stool collection
• Treat the cause of dehydration, i.e. use antipyretics, BRAT diet. Antiemetic medication is NOT usually recommended in children.
Appendicitis
Acute inflammation of the appendix. Most common cause of emergent abdominal surgery in children. More common in males than females.
Appendicitis
Pathophysiology: Caused by closed loop obstruction in the appendix often due to fecal material impaction. This leads to increased intraluminal pressure resulting in mucosal edema, bacterial overgrowth, and eventual perforation. Peritonitis (inflammation of the stomach lining) can occur when bacteria and feces leak into the abdominal cavity.
Appendicitis
Symptoms: Vague abdominal pain localized to the RLQ, nausea and vomiting, small-volume and frequent stools, fever, ill appearance. Maximal tenderness over McBurney’s point in the RLQ and tenderness/distention. If pain suddenly and temporarily stops, this is an indication the appendix has perforated.
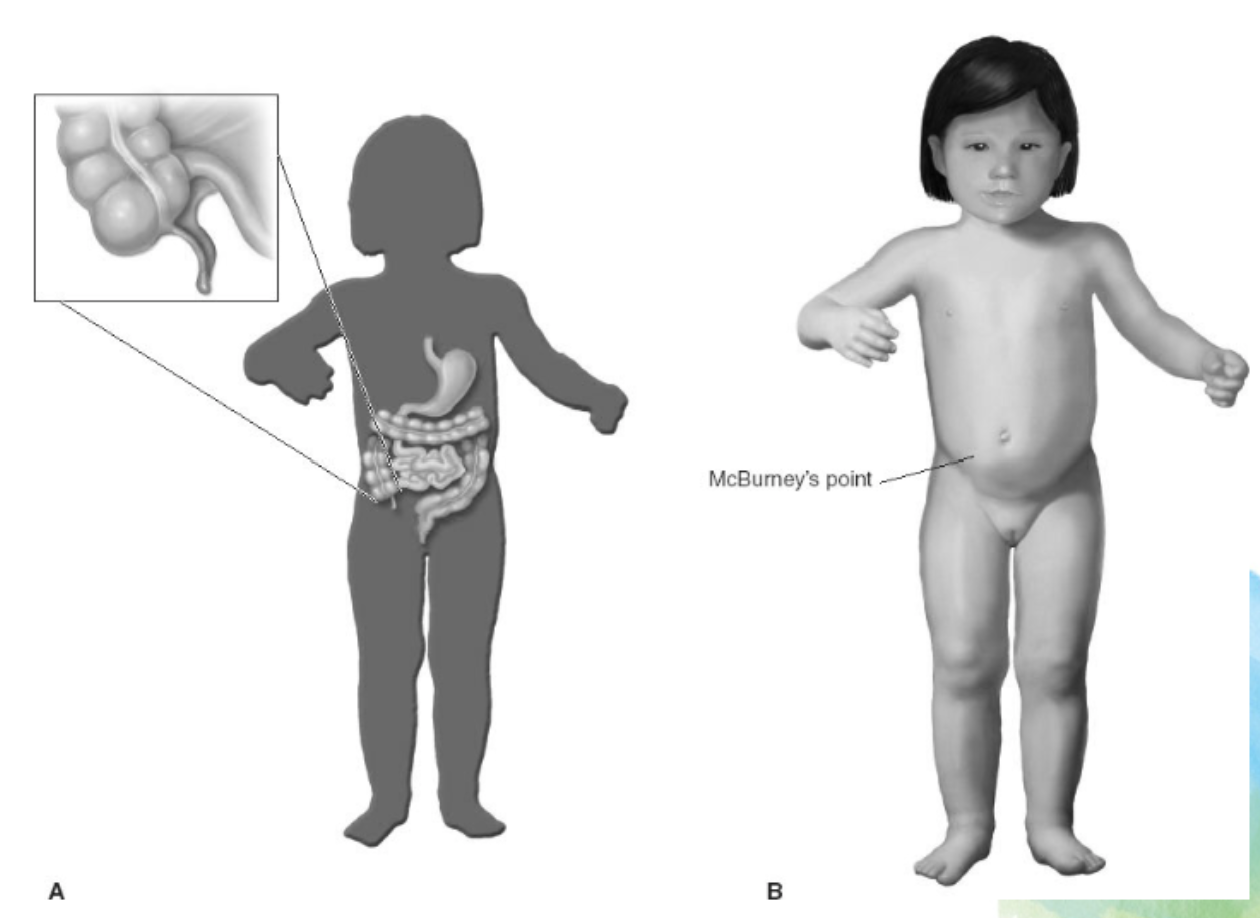
Appendicitis
Treatment: Immediate surgery. The situation gets much worse if appendix ruptures.
Gastroesophageal Reflux (GER)
Pathophysiology: Transient relaxation of the lower esophageal sphincter that occurs when swallowing, crying, or with anything else that increases intra-abdominal pressure. Other stomach conditions may be contributing factors.
Gastroesophageal Reflux (GER)
Complications: Esophagitis, esophageal stricture, Barret’s esophagus, laryngitis, recurrent pneumonia, asthma or anemia.
Gastroesophageal Reflux (GER)
Treatment:
• Position changes, including elevating the bed after feeds and eating smaller more frequent meals.
• Medication to decrease acid production and pH or prokinetics to improve emptying time.
• Laparoscopic gastric fundus surgery
Constipation
Failure to achieve complete evacuation of lower colon. Very common in pediatrics. Organic causes need to be ruled out (medical and neurological) prior to treatment.
Encopresis
Soiling of fecal content into the underwear beyond the age of expected toilet training (4-5 years of age). Often the result of chronic constipation. As stools withheld in the rectum, muscles can stretch over time and cause fecal impactions. Organic causes need to be ruled out (medical and neurological) prior to treatment.
Constipation and Encopresis
Diagnostics of Organic Causes: stool collection, X-ray, sitz marker study (colonic dysmotility), barium enema (used to examine abnormalities in intestine), rectal manometry (tests for rectal muscle disfunction), rectal suction biopsy (can detect for Hirschsprung’s disease where nerve fibers missing from colon)
Constipation and Encopresis
Dietary/Pharmacological Interventions: Increase fibers and fluids, behavior modification, laxatives, stool softeners.
Gastroenteritis
Short-term illness triggered by the infection and inflammation of the digestive system. Often referred to as “stomach flu”.
Oral candidiasis
Oral thrush
Hypertrophic pyloric stenosis
Acute thickening of the pylorus muscles, blocking food from reaching the small intestine.
Necrotizing enterocolitis
a life-threatening disease that affects the intestines of premature or sick newborn infants. Intestinal tissue becomes inflamed and dies.
Failure to Thrive
a term used to describe children who are not growing and gaining weight at the expected rate for their age and sex. Can be Organic, Non-Organic, Idiopathic.
Celiac Disease
Immunological disorder in which gluten causes damage to the small intestine. The villi of the small intestine are damaged due to the body’s immunologic response to the digestion of gluten. Malnutrition occurs as a result.
Celiac Disease
Symptoms: diarrhea, steatorrhea (fat in stool), constipation, weight loss, distention, fatigue, dental disorders, deficiencies, delayed onset of puberty.
Pediatric Cardiovascular System
• The heart lies more horizontally
• The apex lies higher, below the 4th intercostal space
• In infants, the chest lies higher in the chest and occupies over half the chest width
• Right ventricular function initially dominates, then the left side dominates.
Congenital Heart Disease
Structural anomalies in heart that are present at birth, often not diagnosed until later. Largest percentage of birth defects. Chromosomal defects are associated with CHD including Down Syndrome
Congenital Heart Disease
Complications: Cardiac failure, hypoxemia, delays in growth and development, pulmonary vascular disease.
Acquired Heart Disease
heart disorders that occur after birth. They develop from a wide range of causes and can occur as complications.
Tetralogy of Fallot
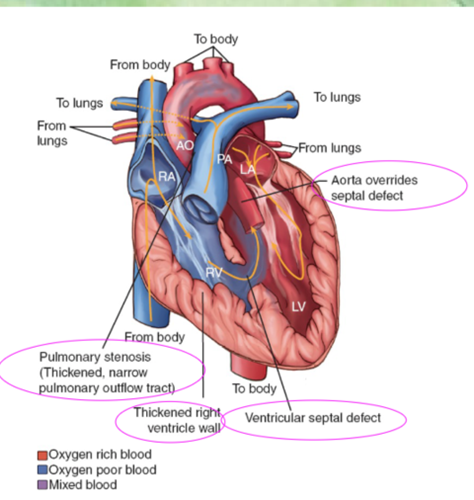
Tetralogy of Fallot
Congenital heart defect of four heart defects causing decreased pulmonary blood flow. Blood flow from the right ventricle is obstructed and slowed, leading to a decrease in blood flow to the lungs and issues with the pressure gradient.
Tetralogy of Fallot
Results from 4 alterations to the heart that decrease blood flow:
1. Pulmonary stenosis: narrowing of the pulmonary valve and outflow tract, creating an obstruction of blood flow from the right ventricle to the pulmonary artery.
2. VSD: Ventricular Septal Defect
3. Overriding Aorta: enlargement of the aortic valve to the extent that it appears to arise from the right and left ventricles rather than the anatomically correct left ventricle.
4. Right Ventricular Hypertrophy: The muscle walls of the right ventricle increases in size as the right ventricle attempts to overcome a high pressure gradient
Tetralogy of Fallot
Symptoms: color changes with feeding, activity, or crying. Hypercyanotic “tet spells”, dyspnea, use of specific posturing such as fetal positioning, squatting. Clubbing, use of accessory muscles, low SPO2, adventitious breath sounds, loud and harsh murmur.
Tetralogy of Fallot
Diagnostics: increased hematocrit, hemoglobin and RBC associated with polycythemia, echocardiogram, ECG, cardiac catheterization and angiography.
Tetralogy of Fallot
Treatment: shunting systemic-to-pulmonary anastomoses, patch closure of the VSD and repair of the valve.
Ventricular Septal Defect
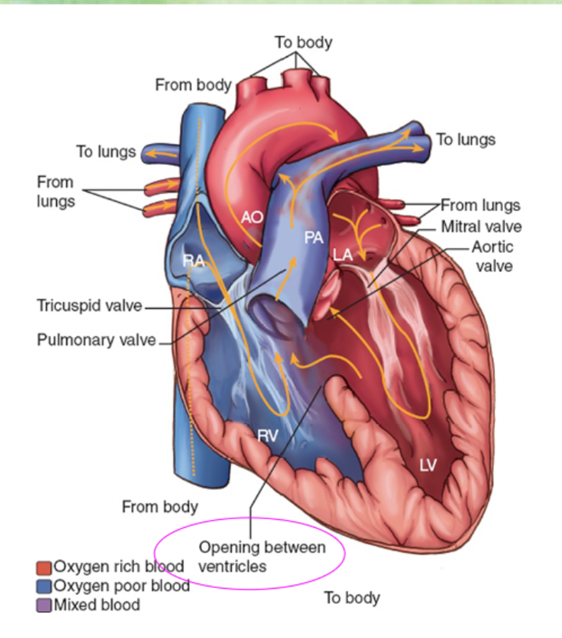
Ventricular Septal Defect
Pathophysiology: defect in the opening between the right and left ventricular chambers of the heart. Leads to increased pulmonary flow. One of the most common congenital heart defects. Spontaneous closure can occur (45%).
Ventricular Septal Defect
Complications: pulmonary hypertension, heart failure, aortic valve regurgitation, infective endocarditis.
Ventricular Septal Defect
Treatment: surgery if does not spontaneously close. Good long-term outcomes for surgical repair.
Ventricular Septal Defect
Symptoms: difficulty with growth and development, poor feeding, color changes, diaphoresis, pulmonary infections, shortness of breath, edema, tachypnea, harsh murmur, adventitious lung sounds, thrill
Ventricular Septal Defect
Diagnostics: MRI, echocardiogram, cardiac catheterization.
Patent Ductus Arteriosus (PDA)
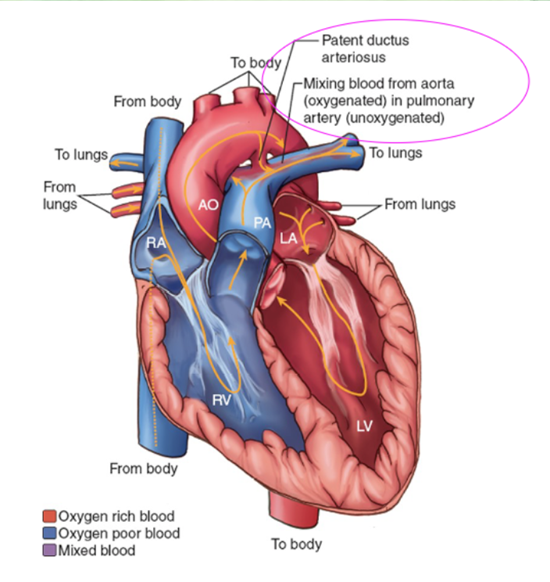
Patent Ductus Arteriosus (PDA)
Pathophysiology: failure of the ductus arteriosus to close within the first weeks of life. Continuous connection between the aorta and the pulmonary artery. Second most common CHD and frequently seen in premature infants. Blood returning to the left atrium passes the left ventricle, enters the aorta, and then travels to the pulmonary systemic circulation. This increases the workload of the left side of the heart. Pulmonary congestion occurs and the right ventricular pressure increases in an attempt to overcome the pressure dysfunctions. The right wall becomes hypertrophied. Pulmonary flow increases.
Patent Ductus Arteriosus (PDA)
Complications: Heart failure, frequent respiratory infection
Patent Ductus Arteriosus (PDA)
Symptoms: may be asymptomatic, fatigue, poor growth and development, tachycardia, tachypnea, bounding pulse, hypotension, adventitious breath sounds, harsh continuous machine-like murmur
Patent Ductus Arteriosus (PDA)
Diagnostics: echocardiogram, electrocardiogram, chest x-ray
Heart Failure
Refers to a set of clinical signs and symptoms that reflect the heart’s inability to pump effectively and provide adequate blood, oxygen, and nutrients.
Heart Failure
Pathophysiology: Cardiac output is controlled by preload (diastolic volume),
afterload (ventricular wall tension), myocardial contractility and heart rate.
Alterations in any of these factors lead to heart failure.
ACE Inhibitors
Used to treat heart failure by stopping production of angiotensin 2, which constricts blood vessels
Digoxin
Inhibits sodium pump which increases intracellular sodium and increases the calcium level in the myocardial cells, causing an increased contractile force of the heart. Toxicity symptoms include confusion, loss of appetite, vomiting, diarrhea, vision problems.
Status Asthmaticus
Life-threatening medical emergency that occurs when a severe asthma attack doesn't respond to standard treatments
Status Asthmaticus
Symptoms: Difficulty breathing, wheezing, coughing, crepitus, cyanosis, confusion, loss of consciousness
Methylprednisolone
drug with anti-inflammatory and immunosuppressive properties that is administered IV as a last resort to treat status asthmaticus.
Salmeterol
Long-acting beta agonist that is used to prevent flare-ups of asthma. Should never be used to treat acute symptoms of asthma.
Albuterol
Short-acting beta agonist used for acute flare-ups of asthma. Beta agonists should be administered before corticosteroids to provide bronchodilation.