Week 7 - Ruminant/Camelid/Swine Anesthesia
Neonates, functionally, have what type of GI tract?
- Monogastric
The rumen may hold upwards of _________________ of ingesta. Fermentation produces ______________ liters of gas per hour. Salivary glands produce ________________ liters of saliva daily. Fermentation and salivation continue under anesthesia.
- 100 L
- 30-50 L
- 50-80 L
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
Neonates, functionally, have what type of GI tract?
- Monogastric
The rumen may hold upwards of _________________ of ingesta. Fermentation produces ______________ liters of gas per hour. Salivary glands produce ________________ liters of saliva daily. Fermentation and salivation continue under anesthesia.
- 100 L
- 30-50 L
- 50-80 L
Describe the appropriate fasting for ruminants prior to anesthesia.
- Fast adult ruminants for 24 - 48 hours
- Withhold water for 8 - 12 hours
What are options for catheterization in adult catlte/ruminants?
- Jugular catheterization is relatively easy
- Tail veins in adult cattle (caution, but may be used)
Ruminants are profoundly sensitive to _______________________. They should be dosed at __________ the equine dose.
- Alpha-2 adrenergic agonists
- 1/10th the equine dose
Alpha-2 adrenergic agonists may cause ________________________ in sheep
- Pulmonary edema (Acute injury caused by hydrostatic stress (due to pulmonary vasoconstriction) which may result in significant hypoxemia, resolving over several hours)
What are some options for IV or IM sedation of ruminants?
- Xylazine IV or IM
- Dexmedetomidine IM
- Detomidine IV
- Butorphanol IM
- May add morphine for additional sedation/restraint
What are some options for IV or IM restraint of ruminants?
- Xylazine IV
- Romifidine IV
- Dexmedetomidine IM
- Detomidine IV
- May add butorphanol or morphine for additional sedation/restraint
What are some options for IV induction of ruminants?
- Ketamine and Guaifenesin (IV as fast as possible)
- Xylazine IV followed by ketamine IV later (either 20 or 45 minutes later depending on low or high dose of xylazine)
- Midazolam and Ketamine IV
- Telazol IV
- Propofol IV
- Alfaxalone IV
Describe proper ET intubation of ruminants.
- Calves, sheep, and goats: Similar technique as used in camelids -> Visualize arytenoids
- Adult cattle: Digital palpation of the larynx and guidance of the tube by hand
Why should "triple drip" not be used for a duration over 60 minutes in ruminants?
- It is being given at a rate faster than they can metabolize it, so over one hour it will "fill up" places it can redistribute it to, resulting in high plasma concentrations and prolonged recovery
What are options for anesthetic maintenance of ruminants?
- GKX (Triple drip)
- Inhalants (most common method as with other species)
If muscles fasciculations are observed in sheep during maintenance of anesthesia, what can be done to manage this?
- Lidocaine CRI
Describe the appropriate blood pressure of ruminants.
- Small ruminants, calves similar to other species
- Adult cattle are relatively hypertensive (MAP 90-120 mm Hg) and hypotension is relatively uncommon
What is particular about the respiratory management of ruminants?
- They have a smaller residual capacity (therefore small tidal volume) and lung volume than other species -> If they become apneic they will become hypoxic faster relative to other species)
How is blood pressure measured in ruminants?
- Direct (Auricular artery often relatively easy to access)
- Indirect
What is the appropriate respiratory rate of ruminants under anesthesia?
- Relatively rapid RR
- Adults: 20 - 30 breaths/min
- Juveniles: 25 - 40 breaths/min
How can anesthetic depth of ruminants be assessed?
- Ocular reflexes/rotation (eyes rotated ventrally indicates light anesthesia while central eyes indicate surgical anesthetic plane)
- Nystagmus indicates light anesthesia
In ruminant anesthesia, where should the patient's head/mouth be?
- Should be lower to facilitate drainage and reduce risk of aspiration with regurgitation
When recovering a ruminant from anesthesia, how should they be positioned? When/how should the ETT be removed?
- Roll patient to sternal recumbency
- Maintain the ETT until at least a swallow is observed. When removing, leave the cuff partially inflated so it can act as a "squeegy" to clean out the trachea during extubation
Describe the GIT of a camelid.
- Three compartment stomach
- Functionally like ruminants with the same risks of regurgitation and aspiration under anesthesia
- Less prone to bloating under anesthesia relative to ruminants
Describe how camelids are catheterized for anesthesia.
- Jugular vein catheterization (remember it is in close proximity to the carotid artery)
- The jugular vein has valves to prevent pooling of blood while grazing and venous blood will often look quite red as they are adapted for high altitude and their hemoglobin has a high affinity for oxygen -> When drawing, observe for "pulsing" blood as an indicator of if you have hit an artery
Estimate the weight of the following patients:
A. Female llama
B. Male llama
C. Female alpaca
D. Male alpaca
A. 100-150 kg
B. 125-160 kg
C. 45-70 kg
D. 55-80 kg
What fasting should be performed in camelids prior to anesthesia?
- Fast for 8 - 12 hours
- Withhold water for 6 -8 hours
What "premedication" is commonly required in camelids?
- Preanesthetic sedation is not typically required
- They are prone to vagal stimulation, so you can pretreat with atropine or glycopyrrolate IM
What are some options for IV sedation of camelids (including route of administration)?
- Acepromazine IM or IV
- Butorphanol IM or IV
- Nalbuphine IM or IV
- Xylazine IM or IV
- Dexmedetomidine IM
- Detomidine IV
- Midazolam IM
What are some options for IV restraint of camelids (including route of administration)?
- Xylazine IM or IV
- Dexmedetomidine IM or IV
- Detomidine IV
- Midazolam IM
- Xylazine/Butorphanol
- Midazolam/Butorphanol
- Xylazine/Ketamine
- BKX IM (Butorphanol, Ketamine, Xylazine)
- "Ketamine stun" (Same as BKX but higher doses and longer duration IM)
- Telazol
What are some anesthetic induction techniques in camelids?
- Thiopental
- Ketamine/Guaifenesin
- Ketamine/Xylazine
- Midazolam/Diazepam and Ketamine (+ morphine immediately prior to induction - Dr. M's preferred choice)
- Propofol
- Propofol and Ketamine
- Alfaxalone
What are options for IV anesthetic maintenance of camelids?
- "Triple drip" (GKX) IV (limit infusion to 60 mins or less)
- Propofol IV (may include ketamine or xylazine to decrease propofol dose)
If utilizing propofol in a camelid for anesthetic maintenance, _______________ is highly recommended.
- Intubation
What breathing system is commonly used in camelid anesthesia?
- Circle (non-rebreather in some crias with mask induction in crias)
Describe the appropriate oral intubation of camelids.
- Utilize a mouth speculum or gauze loops
- Adequate anesthetic depth is importnat
- Utilize lidocaine spray and a long laryngoscope blade
- 5-14 mm ETT
- Use a stylet
Describe the appropriate nasal intubation of camelids.
- Pass the ETT (1 size smaller than would be used for oral) through the ventral nasal meatus and avoid the pharyngeal diverticulum
- Use a stylet (pre-bent aluminum rod), lubricant, phenylephrine, and potentially a laryngoscope
How can one confirm they have successfully intubated a camelid?
- Evacuated bulb technique
- Steaming/clearing of tube
- Synchronous movement of chest and rebreathing bag
- Capnography
What is the typical HR of a camelid under anesthesia?
- With atropine: 60-90 bpm
- With Xylazine (w/o atropine): 30-40 bpm
- Crias: 100-120 bpm
What are methods for measuring BP in camelids?
- Direct (More accurate; caudal auricular artery or medial saphenous artery)
- Oscillometric (better than nothing)
- Doppler
Regarding the respiratory system, camelids tend to be relatively _______________ under anesthesia.
- Tachypneic
What are ways/locations to assess pulse oximetry in camelids?
- Tongue
- Tail (Reflectance probe)
- Gum/dental pad (Reflectance probe)
- Vulva/prepuce
What are ways to assess anesthetic depth in a camelid?
- Response to pain
- Ocular reflex (slow palpebral may be present, odd "blink" at surgical plane may be seen and can be confusing - not like a normal blink but can still be surprising)
What are ways to position a camelid under anesthesia?
- Lateral recumbency (padding, extend down forelimb, protect dependent eye)
- Dorsal recumbency (support head to prevent hyperextension of neck)
- Position/pad head and neck to allow secretions/regurgitant material to drain from the mouth (reduce risk of aspiration)
What is an appropriate fluid therapy plan for camelids under anesthesia?
- 5-10 mg/kg/hr of LRS, plasmalyte, etc.
What drugs can be used for cardiovascular support of camelids under anesthesia?
- Dobutamine
- Calcium gluconate (over 30-60 mins) if tachycardic and hypotensive
What are options for thermal support of camelids under anesthesia?
- Blankets
- Bair hugger
- Hot dog
- Fiber may help, but may also hinder
Camelids are prone to what following extubation? Why?
- Upper airway obstruction
- Obligate nasal breathers - If they don't get the soft palate back into normal position, they can get into trouble -> An advantage of nasal intubation
How should camelids be positioned during recovery?
- Sternal recumbency with head elevated
How long should a camelid's ETT be maintained during recovery? What should you do when extubating?
- As long as possible, monitoring for chewing and coughing
- Keep head elevated and make sure they are moving air adequately (rarely, may need to re-anesthetize and re-intubate in cases of airway obstruction)
What are options for reversal of alpha-2 agonists?
- Atipamezole IV
- Yohimbine IV
- Tolazoline IV
What are options for local anesthetics in camelids and their maximal doses?
- Lidocaine (10 mg/kg)
- Bupivicaine (2 mg/kg)
- Liposome encapsulated bupivicaine (Nocita) (5.3 mg/kg)
What are methods to perform an epidural in camelids?
- Sacrocaudal injection (perineal anesthesia while the animal is still standing - I.e., castration or urethrostomy, low dose)
- Lumbosacral
- May add adjuncts of morphine and xylazine
Venous access can be particularly challenging in what species commonly seen at the VTH?
- Swine
What are some peculiarities regarding swine management and anesthesia to be aware of?
- Restraint difficult (Consider forking)
- Intubation difficult
- Venous access difficult
- Malignant hyperthermia risk
Swine require relatively high doses of which anesthetics?
- Alpha-2 adrenergic agonists
What are some options for injectable sedation of swine? Include route of administration.
- Xylazine IV or IM
- Dexmedetomidine IM
- Midazolam IM or intranasal
What are some options for injectable restraint of swine? Include route of administration and duration of effect.
- Xylazine IM followed 5 minutes later with ketamine IM (20-30 minutes duration, may require additional drug IV)
- Xylazine, Butorphanol, and Ketamine administered together IM (30-45 minute duration)
- Telazol and Xylazine administered together IM (60 minute duration with slow recovery)
What fasting is appropriate prior to anesthesia for swine?
- Fast 8 - 12 hours
- Withhold water for several hours
Where are the ideal places to administer IM injections in pigs and why?
- Heavy fat layer often present along the back ("backfat") which is especially prominent in most pot-bellied pigs (don't administer here)
- Common site is the neck (important in commercial pigs, less fat here)
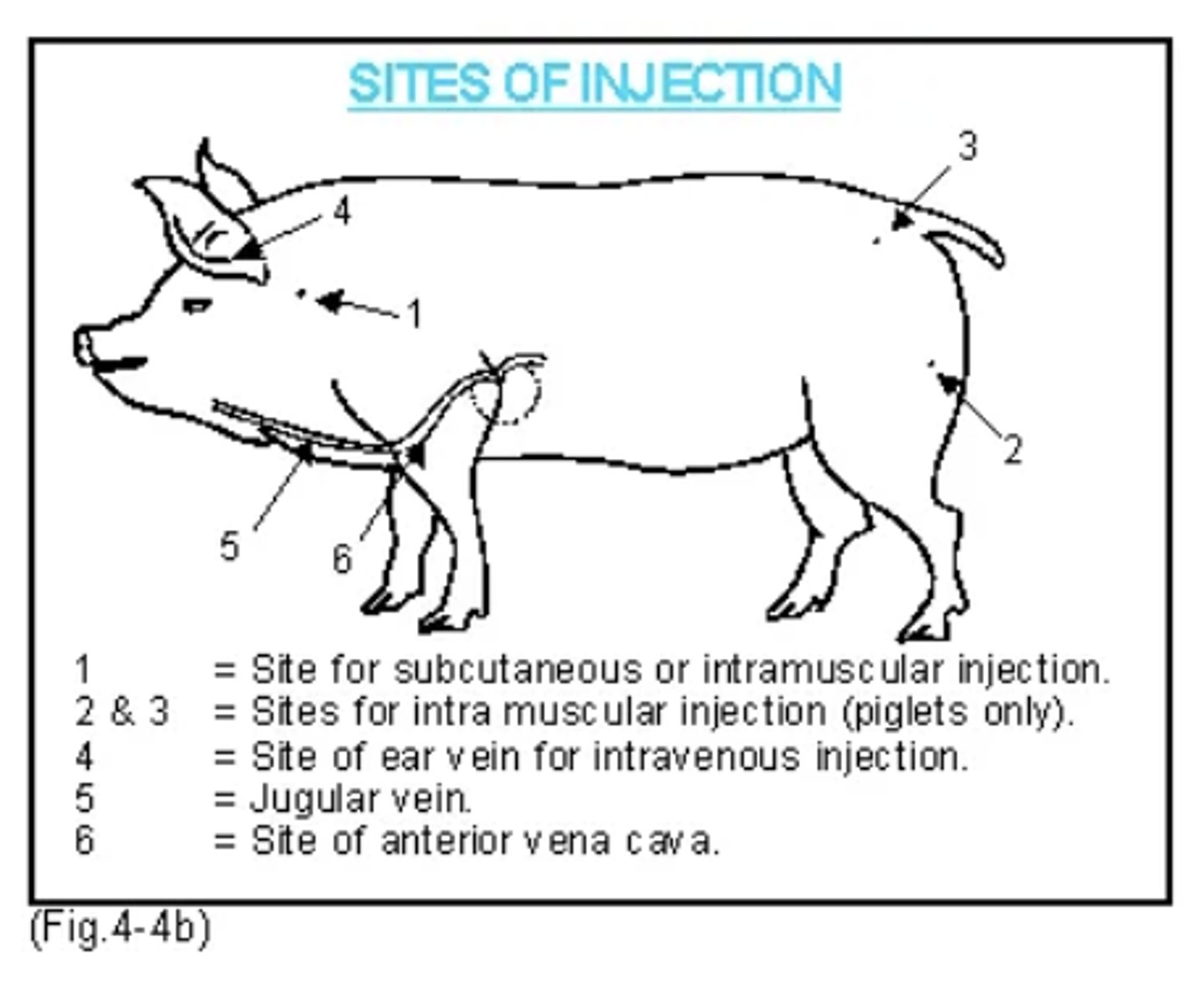
Where/how is IV catheterization performed in swine?
- Auricular vein (Can use rubber band at base of ear to get vein to pop)
- Often performed after heavy sedation or anesthetic induction
- Can also attempt cephalic vein in piglets, intraosseous route when all else fails, and a jugular cut down (may be difficult)(
What are methods for induction of swine?
- Mask induction works well in small pigs or after heavy sedation
- Xylazine/Ketamine or Midazolam/Ketamine IV also works well if you have venous access
- Propofol or Alfaxalone IV in smaller pigs or as a "top off" to aid in intubation
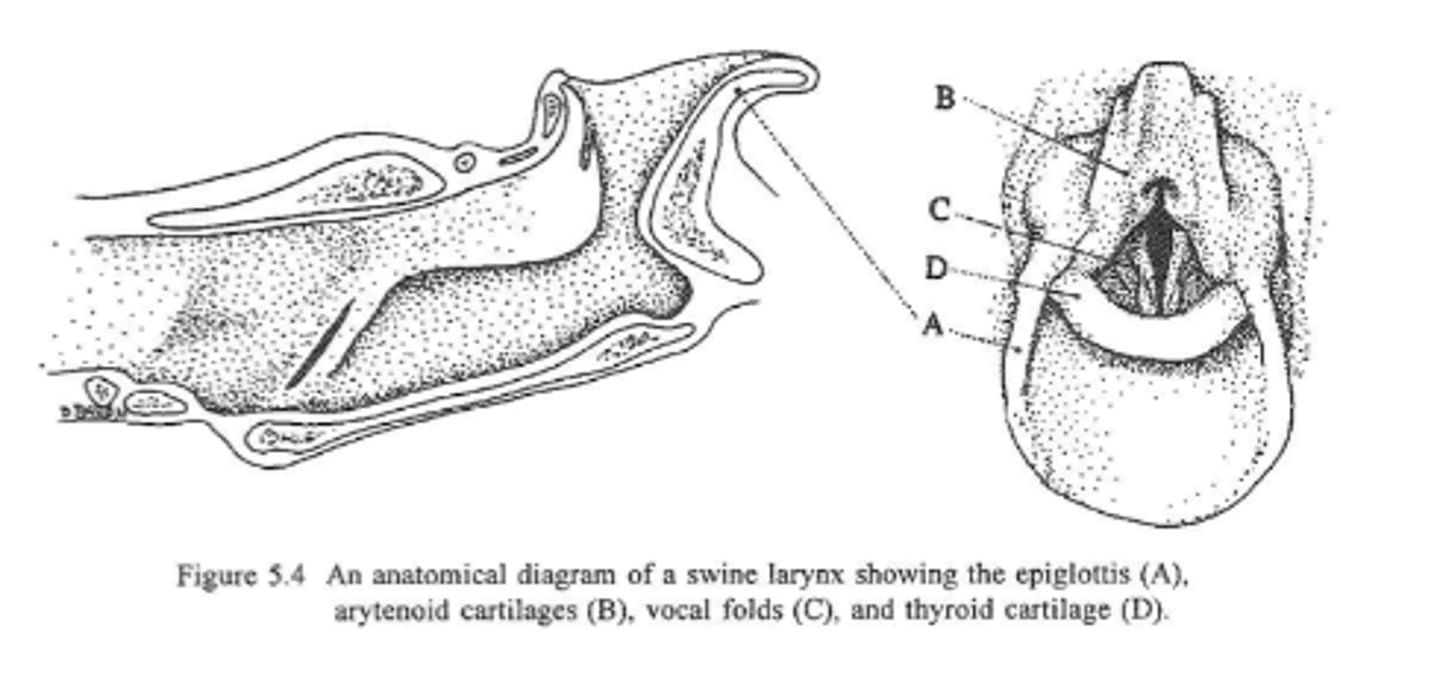
What about the pig's anatomy makes intubation difficult?
- Tracheal diameter is smaller than laryngeal opening
- ET Tube gets caught on floor of the larynx due to angle of pharynx/nasopahrynx/larynx
If recovery of swine is slow and alpha-2 adrenergic agonists were use as part of the anesthetic plan, what should you consider?
- Reversal of alpha-2 adrenergic agonists
What is malignant hyperthermia?
- Genetic (autosomal recessive), rare hypermetabolic syndrome in humans and pigs
What breeds are most susceptible to malignant hyperthermia?
- Breeds with high rate of growth and heavy muscle mass most susceptible (Pietran, Landrace, Spotted, Large White, Hampshire, Poland-China)
What can trigger malignant hyperthermia?
- Stress
- Environmental: high temperature, capture, movement
- Pharmacologic: Inhalant and injectable anesthetics
What is the physiologic mechanism of malignant hyperthermia?
- Single amino acid mutation in ryanodine receptor type 1 (RYR1) associated with calcium channels in skeletal muscle, meaning cells cannot control calcium efflux and calcium activates myosin to cause muscle contraction, and muscle metabolism "goes nuts"
What are components of diagnosing/signs of malignant hyperthermia?
- Rapid rise in core body temperature
- Muscle rigidity
- Tachycardia
- Tachypnea
- Extreme hypercapnia
- Hypoxemia
- Metabolic acidosis
How is malignant hyperthermia treated?
- Remove trigger (e.g., inhalant anesthetic)
- Aggressive cool patient
- Hyperventilate the patient
- Dantrolene (expensive, rarely available)
What is the prognosis of malignant hyperthermia?
- Extremely poor, even with aggressive treatment