Gastrointestinal Tract Infections
0.0(0)
Card Sorting
1/118
Earn XP
Last updated 6:46 AM on 3/25/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
119 Terms
1
New cards
Gastroenteritis
Syndrome characterized by gastrointestinal symptoms including nausea, vomiting, diarrhea, and abdominal discomfort
2
New cards
Diarrhea
Abnormal fecal discharge characterized by frequent/fluid stool
Usually resulting form disease of the small intestine
Involves increased fluid and electrolyte loss
Usually resulting form disease of the small intestine
Involves increased fluid and electrolyte loss
3
New cards
Dysentery
An inflammatory disorder of the GI tract often associated with blood and pus in the feces
Accompanied by symptoms of pain, fever, abdominal cramps
Usually resulting from disease of the large intestine
Accompanied by symptoms of pain, fever, abdominal cramps
Usually resulting from disease of the large intestine
4
New cards
Enterocolitis
Inflammation involving the mucosa of both the small and large intestine
5
New cards
For a GI infection to occur, a pathogen must do what?
Be ingested in sufficient numbers
Elude the host defenses in the upper tract
Reach the intestines
Elude the host defenses in the upper tract
Reach the intestines
6
New cards
What host defenses provide protection against GI infections?
Lysozyme
Acid pH
Mucus
Bile
IgA
Peyer’s patches
Peristalsis
Acid pH
Mucus
Bile
IgA
Peyer’s patches
Peristalsis
7
New cards
What is the most common outcome of GI tract infections?
diarrhea
8
New cards
In “resource poor” countries, what is the major cause of mortality in children?
diarrheal disease
9
New cards
What are the 6 different distinct pathotypes of *E. coli*?
EPEC – enteropathogenic *E. coli*
ETEC – enterotoxigenic *E. coli*
EHEC – shiga-toxin producing *E. coli* (aka STEC or VTEC)
EIEC – enteroinvasive *E. coli*
EAEC – enteroaggregative *E. coli*
DAEC – diffusely aggregative *E. coli*
ETEC – enterotoxigenic *E. coli*
EHEC – shiga-toxin producing *E. coli* (aka STEC or VTEC)
EIEC – enteroinvasive *E. coli*
EAEC – enteroaggregative *E. coli*
DAEC – diffusely aggregative *E. coli*
10
New cards
*E. coli*
Gram negative rod
Many virulence factors – specifically adhesin and exotoxins
Many virulence factors – specifically adhesin and exotoxins
11
New cards
EPEC – enteropathogenic *E. coli*
Small intestine
Primarily occurs in children
Primarily occurs in children
12
New cards
What virulence factors do EPEC contain?
Adherence factor plasmid
Bundle-forming pili (BFP)
Intimin (adhesin)
Translocated intimin receptor (Tir)
Bundle-forming pili (BFP)
Intimin (adhesin)
Translocated intimin receptor (Tir)
13
New cards
What is the pathogenesis of EPEC?
Plasmid-mediatedA/E histopathology, with disruption of normal microvillus structure resulting in malabsorptionand diarrhea
14
New cards
How can we diagnose EPEC?
Characteristic adherence to HEp-2 or HeLa cells
Probes and amplification assays developed for the plasmid- encoded bundle-forming
Pili and gene targets on the “locus of enterocyte effacement” pathogenicity
island
Probes and amplification assays developed for the plasmid- encoded bundle-forming
Pili and gene targets on the “locus of enterocyte effacement” pathogenicity
island
15
New cards
ETEC – enterotoxigenic *E. coli*
Small intestine
Gram negative rod, **FERMENTS LACTOSE**
Traveler’s diarrhea; infant diarrhea in developing countries
Watery diarrhea, vomiting, cramps, nausea, low-grade fever
Gram negative rod, **FERMENTS LACTOSE**
Traveler’s diarrhea; infant diarrhea in developing countries
Watery diarrhea, vomiting, cramps, nausea, low-grade fever
16
New cards
What is the pathogenesis of ETEC?
Plasmid-mediated, ST and LT enterotoxins that stimulate hypersecretion of fluids and electrolytes
17
New cards
What are the two toxins ETEC produces?
Heat-stable toxins (STa and STb)
Heat-labile toxins (LT-I and LT-II)
Heat-labile toxins (LT-I and LT-II)
18
New cards
STa
Monomeric peptide
Binds to transmembrane guanylate cyclase C receptor
Increases cGMP → hypersecretion of fluids/inhibition of fluid absorption
Binds to transmembrane guanylate cyclase C receptor
Increases cGMP → hypersecretion of fluids/inhibition of fluid absorption
19
New cards
LT-I
Very similar to cholera toxin
1 A subunit & 5 B subunits
B subunits bind to GM1 gangliosides → internalization of A
A subunit interacts with Gs → dysregulation of adenylate cyclase
1 A subunit & 5 B subunits
B subunits bind to GM1 gangliosides → internalization of A
A subunit interacts with Gs → dysregulation of adenylate cyclase
20
New cards
What is the MOA of ETEC LT-1?
5 B subunits bind to GM1 receptors on intestinal epithelial cells → A (active) subunit is internalized → Interacts w/ G proteins that regulate adenylate cyclase → Increase cAMP → Hypersecretion of water & electrolytes → Adhere to the mucosal layer to avoid flushing
21
New cards
How can we diagnose ETEC?
Plasmid-mediated, ST and LT enterotoxins that stimulate hypersecretion of fluids and electrolytes
22
New cards
EHEC – shiga-toxin producing *E. coli* (aka STEC or VTEC)
Large intestine (attaches to mucosa)
Initial watery diarrhea → grossly bloody diarrhea (hemorrhagic colitis) w/ abdominal cramps
Little/No fever
May progress to hemolytic uremic syndrome
Cattle major reservoirs
Can survive in soil for months
Initial watery diarrhea → grossly bloody diarrhea (hemorrhagic colitis) w/ abdominal cramps
Little/No fever
May progress to hemolytic uremic syndrome
Cattle major reservoirs
Can survive in soil for months
23
New cards
What toxin does EHEC/STEC produce?
Stx1 (identical to Shiga toxin produced by *S.dysenteriae*)
24
New cards
What is the MOA of Stx1/2 toxin?
stimulates inflammation which enhances expression of Gb3
B subunits bind specific glycolipid (Gb3)
A subunit is internalized → cleaved
A1 binds 28s rRNA → stops protein synthesis
B subunits bind specific glycolipid (Gb3)
A subunit is internalized → cleaved
A1 binds 28s rRNA → stops protein synthesis
25
New cards
Hemorrhagic colitis (HC)
Destruction of mucosa
Results in subsequent hemorrhage
Can be followed by HUS
Results in subsequent hemorrhage
Can be followed by HUS
26
New cards
Hemorrhagic uremic syndrome (HUS)
Receptors on renal epithelium for toxins
Acute renal failure (children), anemia/thrombocytopenia, possible neurological complications
Acute renal failure (children), anemia/thrombocytopenia, possible neurological complications
27
New cards
What is the pathogenesis of EHEC/STEC?
STEC evolved from EPEC
A/E lesions with destruction of intestinal microvilli, resulting in decreased absorption
Pathology mediated by cytotoxic Shiga toxins (Stx1, Stx2), which disrupt
protein synthesis
A/E lesions with destruction of intestinal microvilli, resulting in decreased absorption
Pathology mediated by cytotoxic Shiga toxins (Stx1, Stx2), which disrupt
protein synthesis
28
New cards
How can we diagnose EHEC/STEC?
Screen for O157:H7 with sorbitol-MacConkey agar → confirm by serotyping
Immunoassays (ELISA,latex agglutination) for detection of the Stx toxins in stool specimens and cultured bacteria
DNA amplification assays developed for Stx genes
Immunoassays (ELISA,latex agglutination) for detection of the Stx toxins in stool specimens and cultured bacteria
DNA amplification assays developed for Stx genes
29
New cards
EIEC – enteroinvasive *E. coli*
Large intestine; invade & destroy colonic epithelium
Rare in developing and developed countries
Fever, cramping, watery diarrhea
May progress to dysentery w/ scant bloody stools
Rare in developing and developed countries
Fever, cramping, watery diarrhea
May progress to dysentery w/ scant bloody stools
30
New cards
EAEC – enteroaggregative *E. coli*
Small intestine
Infant diarrhea in developing & probably developed countries
Traveler’s diarrhea
Persistent watery diarrhea, vomiting, dehydration, low-grade fever
Infant diarrhea in developing & probably developed countries
Traveler’s diarrhea
Persistent watery diarrhea, vomiting, dehydration, low-grade fever
31
New cards
What is the pathogenesis of EAEC?
Plasmid-mediated aggregative adherence of rods (“stacked bricks”) w/ shortening of microvilli, mononuclear infiltration, and hemorrhage; decreased fluid absorption
32
New cards
How can we diagnose EAEC?
Characteristic adherence to HEp-2 cells
DNA probe and amplification assays developed for conserved plasmid
DNA probe and amplification assays developed for conserved plasmid
33
New cards
DAEC – diffusely aggregative *E. coli*
Produce an alpha hemolysin & cytotoxic necrotizing factor 1
34
New cards
What types of *E. coli* are the most important contributors to global incidence of diarrheal disease?
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
E. EPEC
F. ETEC
F. ETEC
35
New cards
What types of *E. coli* both cause bloody diarrhea?
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
C. EHEC
D. EIEC
D. EIEC
36
New cards
What type of *E. coli* is the most common cause of acute renal failure in children in the UK and USA?
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
C. EHEC
37
New cards
What marker on EHEC is most commonly associated with HUS?
O157:H7
38
New cards
What type of treatment is NOT indicated for *E. coli* diarrhea?
Antibiotic therapy
39
New cards
What types of *E. coli* can result from ingestion of food and unpasteurized milk?
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
\
A. DAEC
B. EAEC
C. EHEC
D. EIEC
E. EPEC
F. ETEC
C. EHEC
D. EIEC
D. EIEC
40
New cards
Salmonella
Gram - rods; doesn’t ferment lactose
2nd most common cause of food associated diarrhea
Human infection: *Salmonella enterica* Typhi and *Salmonella enterica* paratyphi A, B, C
Cause Typhoid fever and paratyphoid fever (both enteric fever)
2nd most common cause of food associated diarrhea
Human infection: *Salmonella enterica* Typhi and *Salmonella enterica* paratyphi A, B, C
Cause Typhoid fever and paratyphoid fever (both enteric fever)
41
New cards
How are we infected with *Salmonella*?
Ingestion of contaminated food or fecal-oral
Most common sources are poultry, eggs, dairy products
Most common sources are poultry, eggs, dairy products
42
New cards
What is the pathogenesis of *Salmonella*?
Attaches to mucosa of small intestine → invade microfold (M) cells in Peyer patches (also invades enterocytes) → bacteria remain in endocytic vacuoles → released into blood or lymphatic circulation → type III secretion system injects proteins into host cell → inflammatory response confines infection to GI tract → mediates release of prostaglandins → stimulates cAMP & active fluid secretion
43
New cards
How does *Salmonella* present?
Symptoms appear 6-48 hrs after ingestion
Nausea, vomiting, and **nonbloody** diarrhea
Fever, abdominal cramps, myalgia, headache are also common
Colonic involvement can be seen in acute forms of the disease
Nausea, vomiting, and **nonbloody** diarrhea
Fever, abdominal cramps, myalgia, headache are also common
Colonic involvement can be seen in acute forms of the disease
44
New cards
Serious infections with *Salmonella* can cause what?
Sepsis
45
New cards
How can we diagnose Salmonella?
Culture on selective media: MacConkey agar (doesn’t ferment lactose)
Classic Ab detection – Widal test (Agglutination assay; detects Ab of LPS (O antigen) & flagella (H antigen))
Classic Ab detection – Widal test (Agglutination assay; detects Ab of LPS (O antigen) & flagella (H antigen))
46
New cards
How can we treat Salmonella?
Fluid & electrolyte replacement
Antibiotics discouraged (used only for invasive disease)
Antidiarrheal medicine
Antibiotics discouraged (used only for invasive disease)
Antidiarrheal medicine
47
New cards

*Campylobacter jejuni*
S-shaped Gram - rod
Most common causes of bacterial gastroenteritis
Microaerophilic/thermophilic
Can result in Guillain-Barre syndrome
Most common causes of bacterial gastroenteritis
Microaerophilic/thermophilic
Can result in Guillain-Barre syndrome
48
New cards
What is the pathogenesis of *C. jejuni*?
Plethora of adhesin, enzymes & enterotoxins
GI disease characterized by histological damage to mucosal surface of jejunum, ileum, & colon
Mucosal surface appears ulcerated, edematous, bloody
GI disease characterized by histological damage to mucosal surface of jejunum, ileum, & colon
Mucosal surface appears ulcerated, edematous, bloody
49
New cards
Guillain-Barre Syndrome
immune disorder of peripheral nervous system; caused by *C. jejuni*
50
New cards
How is *C. jejuni* transmitted?
Reservoir in cattle, sheep rodents, poultry, wild birds
Acquired through consumption of contaminated food
Most common cause of bacterial diarrheal illness in USA
Acquired through consumption of contaminated food
Most common cause of bacterial diarrheal illness in USA
51
New cards
How does *C. jejuni* present?
Acute enteritis w/ diarrhea, fever, severe abdominal pain (stools may be **bloody)**
Manifestations can include acute colitis, abdominal pain (can mimic acute appendicitis)
Manifestations can include acute colitis, abdominal pain (can mimic acute appendicitis)
52
New cards
*Campylobacter*
Clinically similar to S*almonella* & *Shigella* presentations
Ulceration & inflamed bleeding mucosal surfaces (Jejunum, ileum, colon)
Production of **cytotoxins**
Invasion and bacteremia are possible
Ulceration & inflamed bleeding mucosal surfaces (Jejunum, ileum, colon)
Production of **cytotoxins**
Invasion and bacteremia are possible
53
New cards
How can we diagnose *Campylobacter*?
Cultures (conditions of growth differ from other enterobacteria; elective media; 42°C)
Presumptive identification can be made \~48 hours
Presumptive identification can be made \~48 hours
54
New cards
How can we treat *Campylobacter*?
Azithromycin for severe diarrhea
Fluid/electrolyte replacement
Fluoroquinolone for invasive infection
Fluid/electrolyte replacement
Fluoroquinolone for invasive infection
55
New cards
*Vibrio cholerae*
Comma shaped Gram - bacterium
Acute infection of GI tract (Cholera)
Communities w/ inadequate drinking water & sewage disposal
Free-living bacterium in fresh water; transmitted via contaminated food (shellfish)
Characterized by epidemics and pandemics
Acute infection of GI tract (Cholera)
Communities w/ inadequate drinking water & sewage disposal
Free-living bacterium in fresh water; transmitted via contaminated food (shellfish)
Characterized by epidemics and pandemics
56
New cards
What serogroups of *vibrio cholerae* cause epidemic cholera?
O1 & O139
57
New cards
Serogroup O1 has what two biotypes?
El Tor biotype
Classical biotype
Classical biotype
58
New cards
El Tor biotype
Causes mild diarrhea
Higher ratios of carriers
Higher ratios of carriers
59
New cards
Serogroup O139
Originates from El Tor biotype
New capsular antigen; selective advantage where population is immune to O1 strains
New capsular antigen; selective advantage where population is immune to O1 strains
60
New cards
Cholera toxin
Vibrio pathogenicity islands carry genes for bacteriophage carrying toxin
Permits infection by bacteriophage
Causes cholera symptoms
A subunit (activate adenylate cyclase → increases cAMP → Cl secretion & secretory diarrhea) & B subunit (binds ganglioside GM1 on eukaryotic cells)
Permits infection by bacteriophage
Causes cholera symptoms
A subunit (activate adenylate cyclase → increases cAMP → Cl secretion & secretory diarrhea) & B subunit (binds ganglioside GM1 on eukaryotic cells)
61
New cards
What aids in adherence?
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
B. Chemotaxis proteins
62
New cards
What increases fluid secretion?
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
A. Accessory cholera enterotoxin
63
New cards
What loosens tight junctions to increase intestinal permeability?
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
A. Accessory cholera enterotoxin
B. Chemotaxis proteins
C. Zonula occludens toxin
C. Zonula occludens toxin
64
New cards
How does *V. cholerae* present?
Severe watery, non-bloody diarrhea (rice water stool)
Marked dehydration & electrolyte imbalance
Metabolic acidosis, hypokalemia, hypovolemic shock
Can result in cardiac shock
Untreated cholera mortality = 40-60%; treated cholera mortality =
Marked dehydration & electrolyte imbalance
Metabolic acidosis, hypokalemia, hypovolemic shock
Can result in cardiac shock
Untreated cholera mortality = 40-60%; treated cholera mortality =
65
New cards
How can we treat *V. cholerae*?
Rehydration therapy w/ fluids & electrolytes (PO or IV)
Antibiotics in severe cases
Tetracycline-resistant strains are susceptible to quinolones & macrolides
Antibiotics in severe cases
Tetracycline-resistant strains are susceptible to quinolones & macrolides
66
New cards
How can we prevent *V. cholerae*?
A killed, whole-cell vaccine (only effective in \~50%; protection lasts 3–6 mo)
Clean water supply
Adequate sewage disposal
Clean water supply
Adequate sewage disposal
67
New cards
*Vibrio parahemolyticus*
Halophilic
Found in estuarine, marine & coastal environments (consumption of raw seafood & fish)
Produces heat-stable cytotoxin (invades intestinal cells)
Most virulent strains produce thermostable direct hemolysin (Kanagawa hemolysin)
Most common *Vibrio* species in USA
Found in estuarine, marine & coastal environments (consumption of raw seafood & fish)
Produces heat-stable cytotoxin (invades intestinal cells)
Most virulent strains produce thermostable direct hemolysin (Kanagawa hemolysin)
Most common *Vibrio* species in USA
68
New cards
Kanagawa hemolysin
an enterotoxin that induces chloride ion secretion in epithelial cells; increase intracellular calcium levels
69
New cards
How does *Vibrio parahemolyticus* present?
Self-limiting to mild, cholera-like illness
Explosive watery diarrhea
Headache, abdominal cramps, nausea, vomiting, low-grade fever
Explosive watery diarrhea
Headache, abdominal cramps, nausea, vomiting, low-grade fever
70
New cards
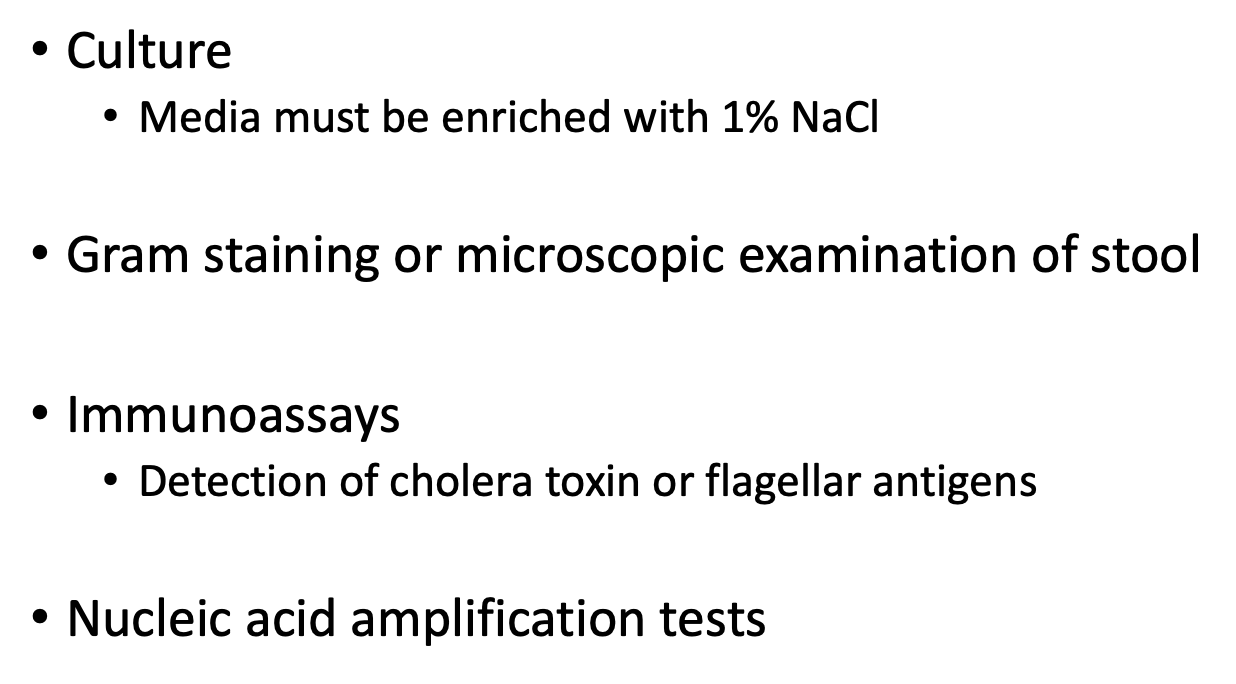
How can we diagnose vibrio?
Culture (media must be enriched w/ 1% NaCl)
Gram staining or microscopic examination of stool
Immunoassays (detection of cholera toxin or flagellar antigens)
Nucleic acid amplification tests
Gram staining or microscopic examination of stool
Immunoassays (detection of cholera toxin or flagellar antigens)
Nucleic acid amplification tests
71
New cards
Shigella
Gram - rod
Causes bacillary dysentery/Shigellosis
Mass inflammation in large intestine (presence of pus & blood in stool)
Primarily a pediatric disease
Easily spread w/ poor sanitation or personal hygiene
Fecal oral route
No animal reservoir (do __**not**__ exist freely in environment)
Secrete proteins that act on epithelial cells → attaches & invades mucosal epithelium in distal ileum & colon
Causes bacillary dysentery/Shigellosis
Mass inflammation in large intestine (presence of pus & blood in stool)
Primarily a pediatric disease
Easily spread w/ poor sanitation or personal hygiene
Fecal oral route
No animal reservoir (do __**not**__ exist freely in environment)
Secrete proteins that act on epithelial cells → attaches & invades mucosal epithelium in distal ileum & colon
72
New cards
Kawshiorkor
Protein deficiency resulting from shigellosis + malnutrition
73
New cards
What are the 4 subgroups of *Shigella*?
*Shigella sonnei* (causes most infections, mild)
*Shigella flexneri* and *Shigella boydii* (causes more severe disease)
*Shigella dysenteriae* (most severe disease)
*Shigella flexneri* and *Shigella boydii* (causes more severe disease)
*Shigella dysenteriae* (most severe disease)
74
New cards
*Shigella* toxin
Similar to EHEC
Causes damage to intestinal epithelium & glomerular endothelial cells
Can lead to kidney failure (HUS)
B subunits bind to host cell glycolipid (Gb3) → allows internalization of A subunit
A subunit cleaved → A1 cleaves 28S rRNA (prevents aminoacyl-transfer RNA binding; disrupts protein synthesis)
Causes damage to intestinal epithelium & glomerular endothelial cells
Can lead to kidney failure (HUS)
B subunits bind to host cell glycolipid (Gb3) → allows internalization of A subunit
A subunit cleaved → A1 cleaves 28S rRNA (prevents aminoacyl-transfer RNA binding; disrupts protein synthesis)
75
New cards
How can we diagnose *Shigella*?
Culture & serological typing help distinguish *Shigella* from *E. coli*
76
New cards
How can we treat *Shigella*?
Antibiotics for severe shigellosis
Plasmid-mediated resistance is common in *Shigella*
Rehydration is crucial
Personal hygiene and proper sewage disposal are important
Plasmid-mediated resistance is common in *Shigella*
Rehydration is crucial
Personal hygiene and proper sewage disposal are important
77
New cards

*Yersinia enterocolitica*
Food-associated infections (infants)
Can multiply at refrigerator temperatures
Zoonotic pathogen (rodents, rabbits, pigs, sheep, cattle, horses, pets)
Outbreaks associated with contaminated milk
Virulence factors (Adhesin proteins, Proteins that aid in epithelial cell invasion, Enterotoxin production)
Invasion of terminal ileum; Necrosis of Peyer’s patches; Inflammation of mesenteric lymph nodes
Presentation of enterocolitis & mesenteric adenitis
Can multiply at refrigerator temperatures
Zoonotic pathogen (rodents, rabbits, pigs, sheep, cattle, horses, pets)
Outbreaks associated with contaminated milk
Virulence factors (Adhesin proteins, Proteins that aid in epithelial cell invasion, Enterotoxin production)
Invasion of terminal ileum; Necrosis of Peyer’s patches; Inflammation of mesenteric lymph nodes
Presentation of enterocolitis & mesenteric adenitis
78
New cards
What pathogens are associated with bacterial toxin-associated diarrhea?
*B. cereus*
*S. aureus*
*C. botulinum*
*C. perfringens*
*S. aureus*
*C. botulinum*
*C. perfringens*
79
New cards
*Staphylococcus aureus*
Food-borne illness
Acts on CNS
Implicated in autoimmune dysregulation (Pathogenesis of IBD)
Bacteria grow at room temp and release toxin (heat kills bacteria but __**NOT**__ toxin)
Toxin detected by latex agglutination assay
Enterotoxins – superantigens (bind MHC class II molecules → T cell stimulation)
Infiltration of neutrophils into epithelium & underlying lamina propria
Loss of brush border in jejunum
Acts on CNS
Implicated in autoimmune dysregulation (Pathogenesis of IBD)
Bacteria grow at room temp and release toxin (heat kills bacteria but __**NOT**__ toxin)
Toxin detected by latex agglutination assay
Enterotoxins – superantigens (bind MHC class II molecules → T cell stimulation)
Infiltration of neutrophils into epithelium & underlying lamina propria
Loss of brush border in jejunum
80
New cards
What subtype of S. aureus enterotoxin is most commonly associated with food poisoning?
A. Subtype A
B. Subtype B
C. Subtype C/D
A. Subtype A
B. Subtype B
C. Subtype C/D
A. Subtype A
81
New cards
What subtype of S. aureus enterotoxin causes staphylococcal pseudomembranous enterocolitis?
A. Subtype A
B. Subtype B
C. Subtype C/D
A. Subtype A
B. Subtype B
C. Subtype C/D
B. Subtype B
82
New cards
What subtype of S. aureus enterotoxins are often found in contaminated milk products?
A. Subtype A
B. Subtype B
C. Subtype C/D
A. Subtype A
B. Subtype B
C. Subtype C/D
C. Subtype C/D
83
New cards
*Clostridium botulinum*
Exotoxin
Seven major botulinum neurotoxins (A-G) (4 are associated w/ human disease (A, B, E, and F))
Toxins not destroyed by digestive enzymes
Ingested in food; toxin can be produced in gut after consumption
Absorbed into the bloodstream to reach peripheral nerve synapses
Seven major botulinum neurotoxins (A-G) (4 are associated w/ human disease (A, B, E, and F))
Toxins not destroyed by digestive enzymes
Ingested in food; toxin can be produced in gut after consumption
Absorbed into the bloodstream to reach peripheral nerve synapses
84
New cards
Botulism is characterized by what?
by symmetrical descending flaccid muscle paralysis
Starts in cranial nerves → blurred vision, difficulty swallowing, slurred speech
Respiratory & cardiac muscles affected
Starts in cranial nerves → blurred vision, difficulty swallowing, slurred speech
Respiratory & cardiac muscles affected
85
New cards
What is the MOA of botulism toxin?
B protects A → A subunit inactivates proteins that regulate release of ACh → Block neurotransmission at peripheral cholinergic synapses → Flaccid paralysis
Recovery depends on regeneration of nerve endings
Recovery depends on regeneration of nerve endings
86
New cards
Food-borne botulism
Produced by ingested foods, typically from home-canned foods
87
New cards
Infant botulism
Most common form; associated w/ feeding honey to babies
88
New cards
Wound botulism
Implanted into a wound during injury
89
New cards
How can we diagnose *C. botulinum*?
Demonstrate presence of toxin in clinical specimens or food
Culture of bacteria
Bioassays are used if serum is available
Culture of feces or wound exudate
Toxin detection by PCR or ELISA
Culture of bacteria
Bioassays are used if serum is available
Culture of feces or wound exudate
Toxin detection by PCR or ELISA
90
New cards
How can we treat *C. botulinum*?
Polyvalent antitoxin recommended
Mechanical ventilation may be necessary
IV or nasogastric nutritional support
Antibiotics for 2º infection
Mechanical ventilation may be necessary
IV or nasogastric nutritional support
Antibiotics for 2º infection
91
New cards
How can we prevent *C. botulinum*?
Prevention of germination by spores in food by maintaining food at an acid pH, storing food at
92
New cards

*Clostridium perfringens*
Gram +
**Enterotoxin** – enhanced activity when exposed to trypsin
Consumption of contaminated meat; associated with pig feasts
Can occur in people released from POW camps
**Enterotoxin** – enhanced activity when exposed to trypsin
Consumption of contaminated meat; associated with pig feasts
Can occur in people released from POW camps
93
New cards
What are the 4 “major lethal” toxins produced by *Clostridium perfringens*?
Alpha, Beta, Epsilon, Iota
94
New cards
What toxins produced by *Clostridium perfringens* causes hemolysis, increased vascular permeability, and bleeding?
A. Alpha
B. Beta
C. Epsilon
D. Iota
A. Alpha
B. Beta
C. Epsilon
D. Iota
A. Alpha
95
New cards
What toxins produced by *Clostridium perfringens* causes intestinal stasis, loss of mucosa, formation of necrotic lesions?
A. Alpha
B. Beta
C. Epsilon
D. Iota
A. Alpha
B. Beta
C. Epsilon
D. Iota
B. Beta
96
New cards
What toxins produced by *Clostridium perfringens* causes protoxin, activated by trypsin, increases permeability in the GI wall?
A. Alpha
B. Beta
C. Epsilon
D. Iota
A. Alpha
B. Beta
C. Epsilon
D. Iota
C. Epsilon
97
New cards
What toxins produced by *Clostridium perfringens* causes necrotic activity, increases vascular permeability?
A. Alpha
B. Beta
C. Epsilon
D. Iota
A. Alpha
B. Beta
C. Epsilon
D. Iota
D. Iota
98
New cards
How can we diagnose *Clostridium perfringens*?
Grown on routine laboratory media (enterotoxin confirmed by latex agglutination assay)
ELISA and PCR detection are more sensitive tests
ELISA and PCR detection are more sensitive tests
99
New cards
How can we prevent *Clostridium perfringens*?
Thoroughly reheating food, avoid overcooking
100
New cards
*Bacillus cereus*
Gram +, spore former (spores & vegetative cells contaminate many foods)
Infection can be diarrhea from production of enterotoxin in gut or vomiting due to ingestion of enterotoxin in food
Vegetative cells secrete enterotoxin in small intestine causing diarrheal disease
Emetic toxin produced in food products & ingested preformed
Infection can be diarrhea from production of enterotoxin in gut or vomiting due to ingestion of enterotoxin in food
Vegetative cells secrete enterotoxin in small intestine causing diarrheal disease
Emetic toxin produced in food products & ingested preformed