A&P: Lecture 15
1/80
Earn XP
Description and Tags
The Digestive System 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
Overview of the GI System
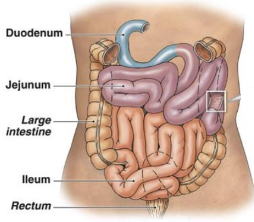
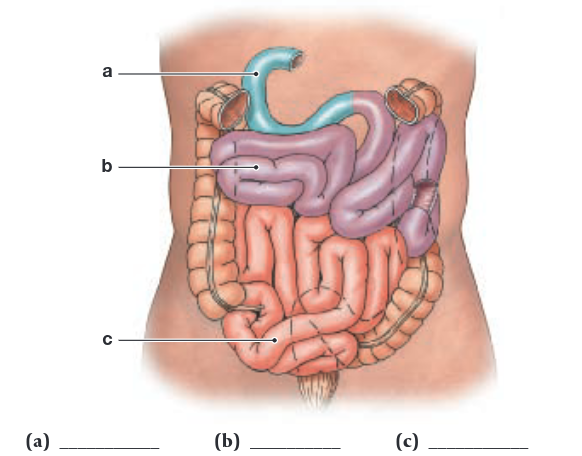
The Small Intestine
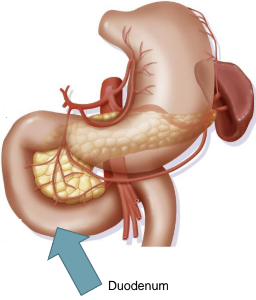
Duodenum
First segment of small intestine
~ 10” long
Receives chyme from stomach and digestive secretions from pancreas and liver
duodenum needs to bring chyme pH from 1.5 - 7.0 using pancreatic buffers (Example: Bicarbonate)
Neutralizes acid before it can damage the absorptive surfaces of the small intestine
The Small Intestine
Jejunum
Middle segment of small intestine
~ 8.2’ long
The location of most:
Chemical digestion
Nutrient absorption
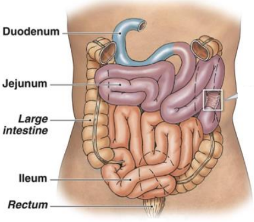
The Small Intestine
Ileum
Final segment of small intestine
~ 11.5’ long
Ends at the ileocecal sphincter
Controls flow of material from ileum into large intestine
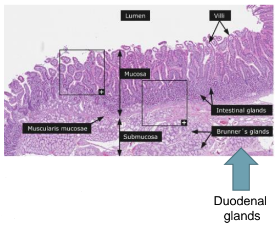
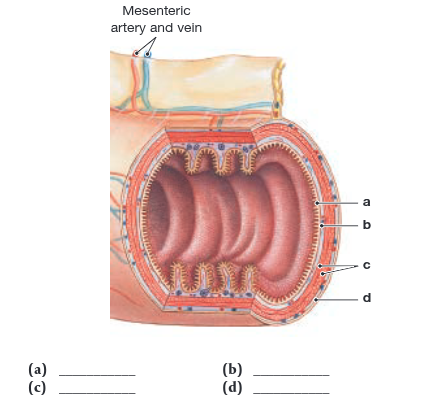
Histology of Small Intestine
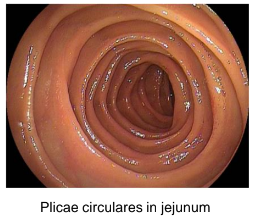
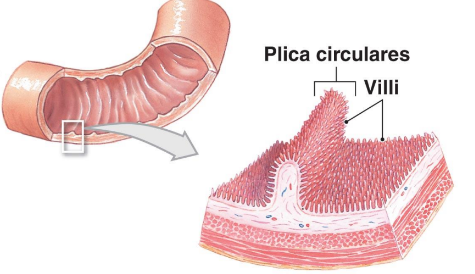
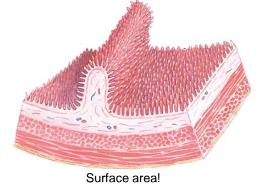
Plicae circulares
Transverse folds in intestinal lining
Permanent features; do not disappear when intestines fill
Slow the passage of chyme (food) through the intestines
Increases surface area of absorption
2200ft² of surface area
Great for absorbing nutrients
Histology of Small Intestine
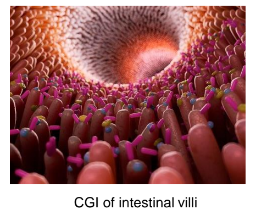
Intestinal villi
Fingerlike projections in mucosa of small intestine
Increases surface area
Covered by simple columnar epithelium
Covered with microvilli
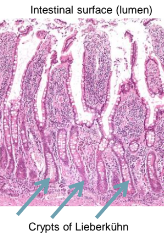
Histology of Small Intestine
Intestinal glands
Mucous cells between columnar epithelial cells
Eject mucins onto intestinal surfaces
Crypts of Lieberkühn
Openings from intestinal glands to intestinal lumen, located at bases of villi
Entrances for brush border enzymes
The Intestinal Wall
The Intestinal Wall
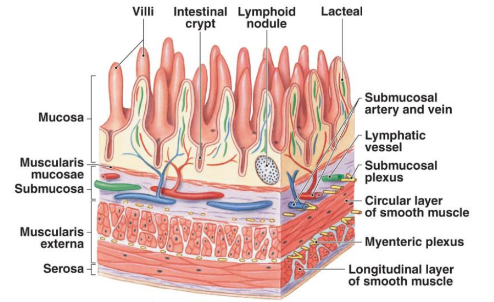
The Intestinal Wall
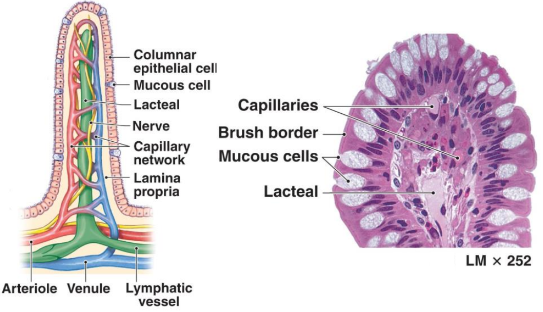
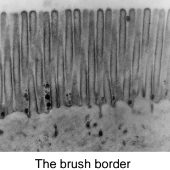
The Small Intestine
Brush Border Enzymes
Integral membrane proteins
On surfaces of intestinal microvilli
Secreted from intestinal glands
Break down materials in contact with brush border
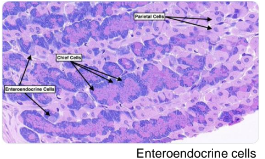
Enteroendocrine cells
Produce intestinal hormones
Ex: gastrin, cholecystokinin, and secretin
The Small Intestine
Glands of the Duodenum
aka: Submucosal or Brunner’s glands
Produce large quantities of mucus when chyme arrives from stomach
Intestinal Secretions
Moisten chyme
Assist in buffering acids
~1.8 Liters/day enter intestinal lumen
Keep digestive enzymes and products of digestion in solution
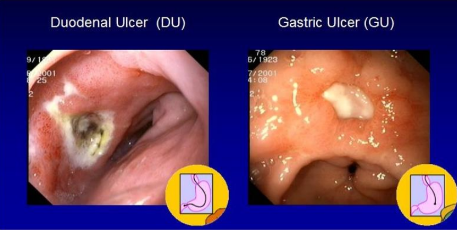
Peptic Ulcers
Esophageal ulcers – in esophagus
Gastric ulcers – inside stomach
Duodenal ulcers – in duodenum
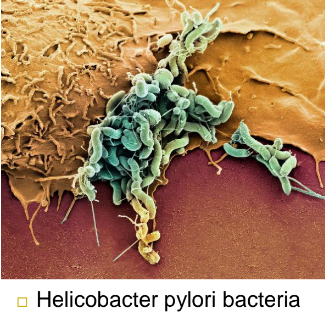
Peptic Ulcers
Helicobacter pylori bacteria
Causes Ulcers
2/3 of people globally have H. pylori
Some people can handle it and some can’t
Gross Anatomy of the Pancreas
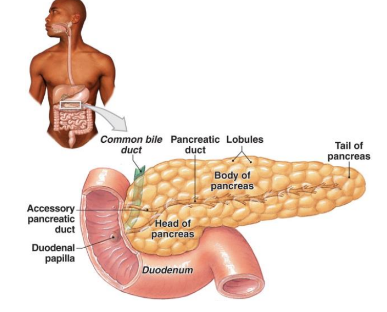
The Pancreas
Functions of the Pancreas
Endocrine cells:
Secrete insulin and glucagon into bloodstream
Exocrine cells:
Secrete pancreatic juice ~1000 mL (1 qt) pancreatic juice per day
Controlled by hormones from duodenum
Contain pancreatic enzymes
Pancreatic Enzymes
Pancreatic alpha-amylase
A carbohydrase
Breaks down starches
Similar to salivary amylase
Pancreatic lipase
Breaks down complex lipids
Pancreatic Nucleases
Break down nucleic acids
Proteolytic enzymes
Break down certain proteins
Proteases break large protein complexes
Peptidases break small peptides into amino acids
Account for ~70% of all pancreatic enzyme production
Secreted as inactive proenzymes, and are activated after reaching small intestine
The Liver
Largest visceral tissue mass ~3+ lbs.
Performs essential (1) metabolic and (2) hematological regulation as well as (3) bile production
Anatomy of the liver:
Wrapped in tough fibrous capsule
Covered by visceral peritoneum
Divided into lobes
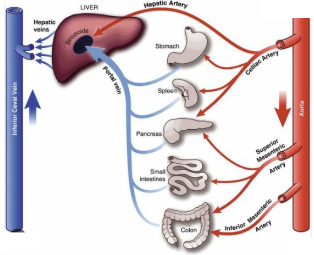
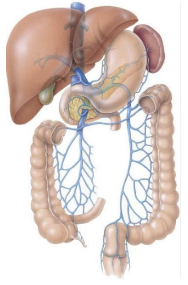
The Liver
Hepatic blood volume
1/3 is Arterial blood
From hepatic artery
2/3 is Venous blood from hepatic portal vein, originating at the:
Stomach
Spleen
Pancreas
Small & Large intestines
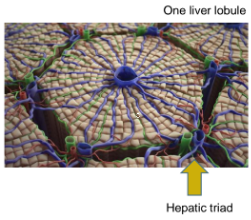
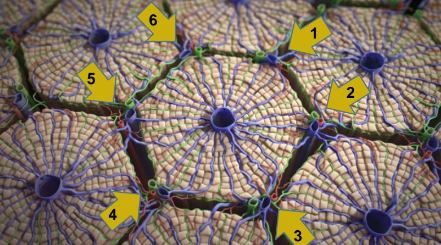
Histological Organization of the Liver
Each lobe of the liver is divided:
Into ~ 100,000 liver lobules
The functional units of the liver
~ 1 mm diameter each
Each Lobule
Hexagonal in cross section
With 6 portal areas (hepatic triads)
One at each corner of lobule
Histological Organization of the Liver
Each portal area of a lobule contains 3 structures
Branch of: hepatic portal vein, hepatic artery proper, and bile duct
Histological Organization of the Liver
Lobules of the liver
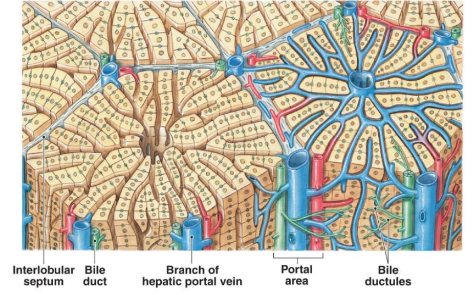
Liver Histology
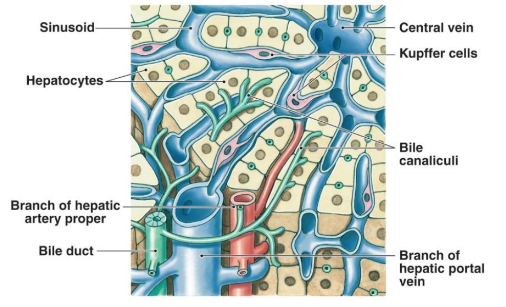
Liver Histology
Hepatocytes (hepato = liver, cyto = cells)
Adjust circulating levels of nutrients
Through selective absorption and secretion
Arranged like wheel spokes
As blood flows through sinusoids, the hepatocytes:
Absorb solutes from plasma
Secrete materials such as plasma proteins
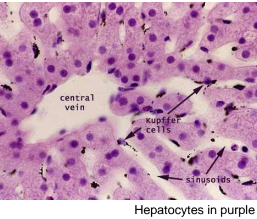
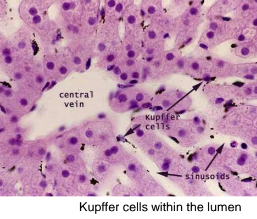
Liver Histology
Kupffer cells aka: stellate reticuloendothelial cells
Located in sinusoidal lining
Line blood vessels
Macrophages that play a critical role in maintaining liver functions
Immune cells that protect liver from bacterial infections
Respond to liver injury by producing cytokines that recruit other immune cells (Monocytes)
The Liver
Main categorical functions:
Metabolic regulation
Hematological regulation
Bile production

Metabolic Regulation of Liver
Nutrient Metabolism
Carbohydrate metabolism
Lipid metabolism
Amino acid metabolism
Nutrient Storage
Vitamin storage
Mineral storage

Metabolic Regulation of Liver
Waste Product Removal
Wastes (not utilized by the liver) are converted and carried out by bile to small intestine
… Or carried by blood to kidneys
Digested proteins → Ammonia → Urea
Drug Inactivation
Removes and breaks down circulating drugs
Ex: Acetaminophen (Tylenol)
Limits duration of their effects
Consider Rx drug dosages
Hematological Regulation of Liver
Composition of Circulating Blood
All blood leaving absorptive surfaces of digestive tract
Enters hepatic portal system
Flows into the liver
Liver cells extract nutrients (or toxins) from blood
Before they reach systemic circulation
Hematological Regulation of Liver
Composition of Circulating Blood
Liver removes and stores excess nutrients
Corrects nutrient deficiencies by mobilizing stored reserves or performing synthetic activities
Largest blood reservoir in the body
Receives 25-30% of cardiac output
Hematological Regulation of Liver
Functions of Hematological Regulation:
Removal of toxins
Synthesis of plasma proteins
Removal of circulating hormones
Phagocytosis and antigen presentation
Removal of antibodies
Bile Production in the Liver
Functions of Bile
Liver breaks down hemoglobin (Heme) to make bile
Mechanical processing in stomach creates large lipid droplets
Dietary lipids are not water soluble
Pancreatic lipase is not lipid soluble
Interacts only at surface of lipid droplet
Bile salts break droplets apart (emulsification)
Emulsification helps break down fats
Increases surface area exposure to enzymatic attack
Creates tiny emulsion droplets coated with bile salts
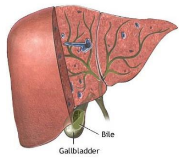
The Gallbladder
Functions of the Gallbladder
Stores bile prior to excretion
Secretes, but only under stimulation of hormone cholecystokinin (CCK)
Without CCK
Hepatopancreatic sphincter remains closed
Bile exiting liver in common hepatic duct cannot flow through common bile duct into duodenum
So, the bile enters cystic duct and is stored in gallbladder
Coordination of Secretion and Absorption
Neural mechanisms coordinate digestion (1 of 2)
Parasympathetic innervation
Prepares digestive tract for activity
Secretes a lot of mucus
Sympathetic innervation
Inhibits digestive tract activity
Coordinate movement of chyme along digestive tract

Coordination of Secretion and Absorption
Hormonal mechanisms coordinate digestion (2 of 2)
Hormones of duodenal enteroendocrine cells include:
Secretin
Cholecystokinin (CCK)
Gastrin
Enterocrinin
Gastric inhibitory peptide (GIP)
Vasoactive intestinal peptide (VIP)
Coordination of Secretion and Absorption
Secretin
Released when chyme arrives in duodenum
Increases secretion of bile (liver) and buffers (pancreas)
First Hormone ever described
Discovered by Earnest Starling
Cholecystokinin (CCK)
Secreted in duodenum
When chyme contains lipids and partially digested proteins
Accelerates pancreatic production and secretion of digestive enzymes
Relaxes hepatopancreatic sphincter and gallbladder
Ejecting bile and pancreatic juice into duodenum
Coordination of Secretion and Absorption
Gastrin
Secreted in duodenum upon exposure to undigested proteins
Stimulates acid and enzyme production
Enterocrinin
Released when chyme enters duodenum
Stimulates mucin production
Gastric Inhibitory Peptide (GIP)
Secreted when fats and carbohydrates enter duodenum
Vasoactive Intestinal Peptide (VIP)
Stimulates secretion of intestinal glands
Coordination of Secretion and Absorption
Intestinal Absorption
90% of absorption happens in the small intestines.
by the time chyme gets into the Large Intestine its about all waste.
Takes ~ 5 hours for materials to pass from duodenum to end of ileum
Movements of the mucosa increases absorptive effectiveness
Stir and mix intestinal contents
Constantly change environment around epithelial cells
The Large Intestine
The colon extends from end of ileum to anus
Frames small intestine ~ 5’ long and 3” wide
Functions to:
Reabsorb water
Compact intestinal contents into feces
Absorb important vitamins produced by bacteria
Vitamins we make in our digestive system are made in the Large intestines.
Store fecal material prior to defecation
Diarrhea = food moves too quickly through large Intestine
Constipation = food moves too slowly through large Intestine

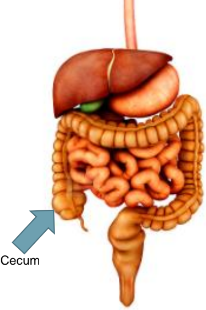
The Large Intestine
The Cecum
Receives material arriving from the ileum
The Colon
Larger diameter and thinner walls than small intestine
Forms a series of pouches
Haustra permit expansion and elongation of colon
The Large Intestine
Rectum
Forms last 6” of digestive tract
Expandable organ for temporary storage of feces
Movement of fecal material into rectum triggers urge to defecate
Anus
Internal anal sphincter
Smooth muscle, not under voluntary control
External anal sphincter
Skeletal muscle, under voluntary control
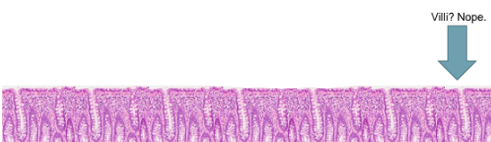
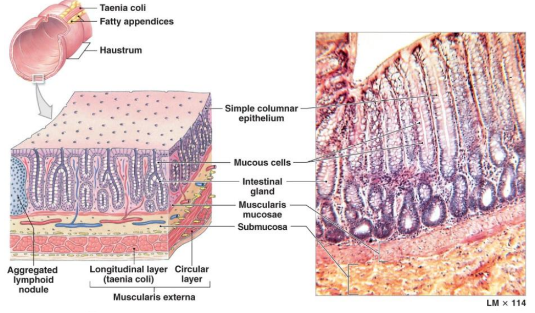
Histology of Large Intestine
Large intestine tissue lacks villi
Does not produce enzymes because nutrient absorption is nearly complete
Presence of distinctive intestinal glands:
Deeper than glands of small intestine
Abundance of mucous cells
Provides lubrication for fecal material
Mucosa and Glands of the Colon
The Large Intestine
Three Vitamins Produced in the Large Intestine
Vitamin K (fat soluble)
Required by liver for synthesizing 4 clotting factors
K for klotting factors
Biotin (water soluble)
Important in glucose metabolism
Sweet Hair (Hlucose metabolism and biotin)
Pantothenic acid, aka B5 (water soluble)
Required in manufacture of steroid hormones and some neurotransmitters
The Large Intestine
Movements of the Large Intestine
Gastroileal reflex
Moves materials into cecum while eating
Movement from cecum to transverse colon is slow
Allowing hours for water absorption
Peristaltic waves move material along length of colon
Stimulus is distension of stomach and duodenum; relayed over intestinal nerve plexuses
Distension of the rectal wall triggers defecation reflex
The Large Intestine
Elimination of Feces
Requires relaxation of internal and external anal sphincters
Reflexes open internal sphincter, close external sphincter
Opening external sphincter requires conscious effort
Digestive System Review (1 of 3)
Oral cavity
Mechanical processing with teeth and tongue
Salivary Glands
Saliva lubricates food; contains enzymes to break down carbohydrates
Pharynx
Musculature propels food toward esophagus
Esophagus
Transportation of food to stomach
Digestive System Review (2 of 3)
Stomach
Chemical digestion – acids and enzymes
Mechanical digestion – muscular contractions
Liver
Generation of bile, nutrient storage, metabolic and hematological functions
Gallbladder
Storage and secretion of bile for lipid digestion
Digestive System Review (3 of 3)
Pancreas
Buffers and digestive enzymes secreted by exocrine cells
Hormones secreted by endocrine cells
Small intestine
Enzymatic digestion and absorption of water, organic substrates, vitamins and ions
Large intestine
Dehydration and compaction of indigestible material
The enzymatic breakdown of large molecules into their basic building blocks is called
chemical digestion
The outer layer of the digestive tract is known as the
serosa
Double sheets of peritoneum that provide support and stability for the organs of the peritoneal cavity are the
mesenteries
A branch of the hepatic portal vein, hepatic artery proper, and branch of the bile duct form
a portal triad
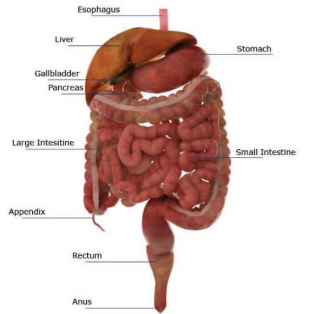
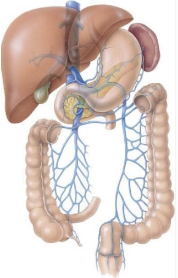
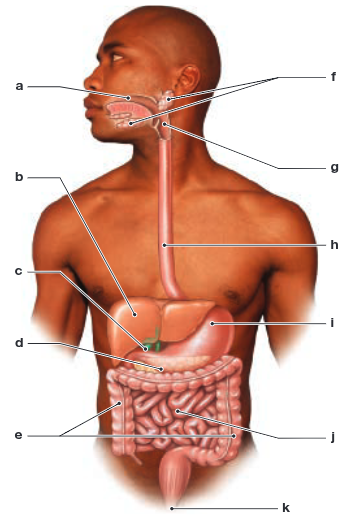
Label the digestive system structures in the following figure.
(a) oral cavity (mouth);
(b) liver;
(c) gallbladder;
(d) pancreas;
(e) large intestine;
(f) salivary glands;
(g) pharynx;
(h) esophagus;
(i) stomach;
(j) small intestine;
(k) anus
Label the four layers of the digestive tract in the following figure
(a) mucosa;
(b) submucosa;
(c) muscular layer;
(d) serosa
Most of the digestive tract is lined by epithelium.
simple columnar
Regional movements that occur in the small intestine and function to churn and fragment the digestive material are called
segmentation
Bile release from the gallbladder into the duodenum occurs only under the stimulation of
cholecystokinin
Label the three segments of the small intestine in the following figure.
(a) duodenum;
(b) jejunum;
(c) ileum
The major function(s) of the large intestine is (are)
(a) reabsorption of water and compaction of feces,
(b) absorption of vitamins liberated by bacterial action,
(c) storage of fecal material prior to defecation
Vitamins generated by bacteria in the colon are
vitamin K, biotin, and pantothenic acid
The final enzymatic steps in the digestive process are accomplished by
brush border enzymes of the intestinal microvilli
What are the six main processes of the digestive system?
The six main processes of the digestive system are
(1) ingestion
(2) mechanical digestion and propulsion
(3) chemical digestion
(4) secretion
(5) absorption
(6) defecation
Name and describe the layers of the digestive tract, proceeding from the innermost layer nearest the lumen to the outermost layer.
Layers of the digestive tract from the innermost layer nearest the lumen to the outermost layer are
(1) the mucosa: the epithelial layer that performs chemical digestion and absorption of nutrients;
(2) the submucosa: the connective tissue layer containing lymphatic and blood vessels and the submucosal nerve plexus;
(3) the muscular layer: the smooth muscle layer containing the myenteric nerve plexus;
(4) the serosa: the outermost layer, epithelium and connective tissue that forms the visceral peritoneum (or connective tissue that forms the adventitia).
What three basic mechanisms regulate the activities of the digestive tract?
Activities of the digestive tract are regulated by local, neural, and hormonal mechanisms.
What are the three phases of swallowing, and how are they controlled?
The three phases of swallowing—the buccal, pharyngeal, and esophageal phases—are controlled by the swallowing center of the medulla oblongata by the trigeminal and glossopharyngeal cranial nerves. The motor commands originating at the swallowing center are distributed by cranial nerves V, IX, X, and XII. Along the esophagus, primary peristaltic contractions are coordinated by afferent and efferent fibers within the glossopharyngeal and vagus cranial nerves, but secondary peristaltic contractions occur in the absence of CNS instructions.
What are the primary digestive functions of the pancreas, liver, and gallbladder?
The pancreas provides digestive enzymes, plus bicarbonate ions that elevate the pH of the chyme. The liver produces bile and is also the primary organ involved in regulating the composition of circulating blood. The gallbladder stores and releases bile, which contains additional buffers and bile salts that aid in the digestion and absorption of lipids
Which hormones produced by duodenal enteroendocrine cells effectively coordinate digestive functions?
The hormones include the following: enterocrinin, which stimulates the submucosal glands of the duodenum; secretin, which stimulates the pancreas and liver to increase the secretion of water and bicarbonate ions; cholecystokinin (CCK), which causes an increase in the release of pancreatic secretions and bile into the duodenum, inhibits gastric activity, and appears to have CNS effects that reduce the sensation of hunger; gastric inhibitory peptide (GIP), which stimulates insulin release at pancreatic islets and the activity of the duodenal submucosal glands; vasoactive intestinal peptide (VIP), which stimulates the secretion of intestinal glands, dilates regional capillaries, and inhibits acid production in the stomach; gastrin, which is secreted by G cells in the duodenum when they are exposed to large quantities of incompletely digested proteins; and, in small quantities, motilin, which stimulates intestinal contractions; villikinin, which promotes the movement of villi and associated lymph flow; and somatostatin, which inhibits gastric secretion.
What are the three primary functions of the large intestine?
The large intestine reabsorbs water and compacts the intestinal contents into feces, absorbs important vitamins liberated by bacterial action, and stores fecal material prior to defecation.
What two positive feedback loops are involved in the defecation reflex?
Positive feedback loops in the defecation reflex involve
(1) stretch receptors in the rectal walls, which promote a series of peristaltic contractions in the colon and rectum, moving feces toward the anus in the intrinsic myenteric defecation reflex; and (2) the sacral parasympathetic defecation reflex, also activated by the stretch receptors, which stimulates peristalsis by motor commands.
During defecation
(a) stretch receptors in the rectal wall initiate a series of peristaltic contractions in the colon and rectum,
(b) stretch receptors in the rectal wall activate parasympathetic centers in the sacral region of the spinal cord
Increased parasympathetic stimulation of the intestine would result in
none of these:
(a) decreased motility,
(b) decreased secretion,
(c) decreased sensitivity of local reflexes,
(d) decreased segmentation
A drop in pH below 4.5 in the duodenum stimulates the secretion of
secretin
Through which layers of a molar would an oral surgeon drill to perform a root canal (removal of the alveolar nerve in a severely damaged tooth)?
A root canal involves drilling through the enamel and the dentin.
How is the stomach protected from digestion?
The stomach is protected from digestion by mucous secretions of its epithelial lining and by neural and hormonal control over the times and rates of acid secretion.
How does each of the three phases of gastric secretion promote and facilitate gastric control?
(1) The cephalic phase of gastric secretion begins with the sight or thought of food. Directed by the CNS, this phase prepares the stomach to receive food. (2) The gastric phase begins with the arrival of food in the stomach; this phase is initiated by distension of the stomach, an increase in the pH of the gastric contents, and the presence of undigested materials in the stomach. (3) The intestinal phase begins when chyme starts to enter the small intestine. This phase controls the rate of gastric emptying and ensures that the secretory, digestive, and absorptive functions of the small intestine can proceed reasonably efficiently.
Nutritionists have found that after a heavy meal, the pH of blood increases slightly, especially in the veins that carry blood away from the stomach. What causes this increase in blood pH?
After a heavy meal, bicarbonate ions pass from the parietal cells of the stomach into the interstitial fluid. The diffusion of bicarbonate ions from the interstitial fluid into the bloodstream increases blood pH. This sudden influx of bicarbonate ions into the bloodstream has been called the alkaline tide.
Some people with gallstones develop pancreatitis. How could this occur?
If a gallstone is small enough, it can pass through the bile duct and block the pancreatic duct. Enzymes from the pancreas then cannot reach the small intestine. As the enzymes accumulate, they irritate the duct and ultimately the exocrine pancreas, producing pancreatitis.
Harry is suffering from an obstruction in his colon. He notices that when he urinates, the color of his urine is much darker than normal, and he wonders if there is any relationship between the color of his urine and his intestinal obstruction. What would you tell him?
The darker color of his urine is probably due to increased amounts of the pigment urobilin, which gives urine its normal yellow color. Urobilin is derived from urobilinogen, which is formed in the large intestine by the action of intestinal bacteria on bile pigments. In an intestinal obstruction, the bile pigments cannot be eliminated by their normal route, so a larger-than-normal amount diffuses into the bloodstream, where the kidneys eliminate it.
A condition known as lactose intolerance is characterized by painful abdominal cramping, gas, and diarrhea. The cause of the problem is an inability to digest the milk sugar lactose. How would this cause the observed signs and symptoms?
If an individual cannot digest lactose, this sugar passes into the large intestine in an undigested form. The presence of extra sugar in the chyme increases its osmolarity, so less water is reabsorbed by the intestinal mucosa. The bacteria that inhabit the large intestine can metabolize the lactose, and in the process they produce large amounts of carbon dioxide. This gas overstretches the intestine, which stimulates local reflexes that increase peristalsis. The combination of more fluid contents and increased peristalsis causes diarrhea.The overexpansion of the intestine by gas, which is directly related to increased gas production by the bacteria, causes the severe pain and abdominal cramping.
Recently, more people have turned to surgery to help them lose weight. One form of weight control surgery involves stapling a portion of the stomach shut, creating a smaller volume. How would such a surgery result in weight loss?
The primary effect of such surgeries would be a reduction in the volume of food (and thus in the amount of calories) consumed because the person feels full after eating a small amount. This can result in significant weight loss.