The Renal System Part 1
1/163
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
164 Terms
Which of the following best describes the role of urine in kidney function?
A. Urine is produced to store electrolytes for future use by the body
B. Urine is a byproduct of the kidney’s filtration, reabsorption, and secretion processes
C. Urine is the primary mechanism by which the kidneys regulate blood cell production
D. Urine is created by the bladder to remove toxins after they pass through the bloodstream
B. Urine is a byproduct of the kidney’s filtration, reabsorption, and secretion processes
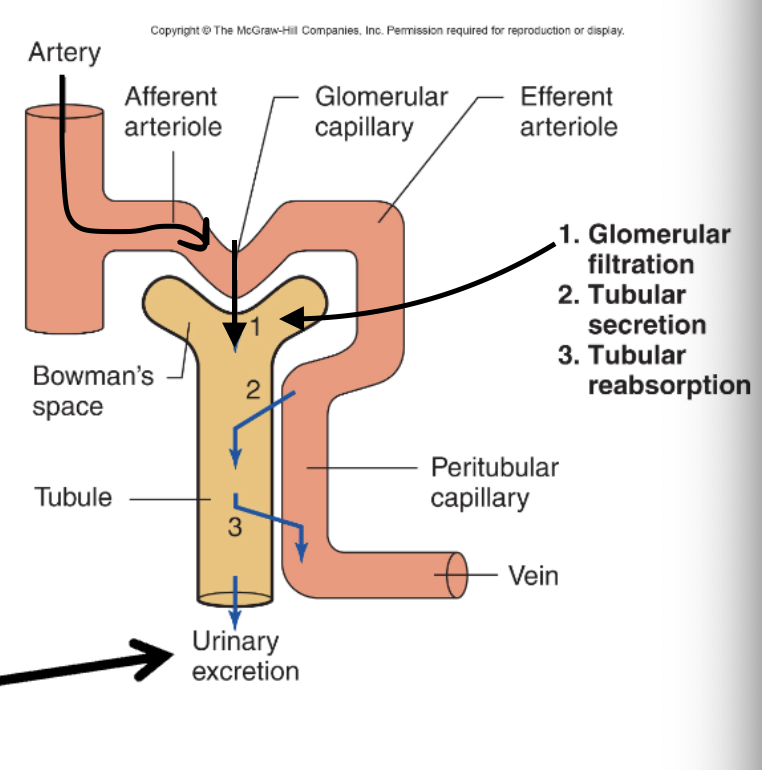
Net filtration Net reabsorption Net secretion Net Excretion
Glomerular filtration rate
What is the primary role of regulating plasma ion concentrations (Na⁺, K⁺, Cl⁻)?
A. To stimulate red blood cell production
B. To maintain electrical gradients and proper nerve/muscle function
C. To promote hormone secretion
D. To regulate water reabsorption in the lungs
Regulating total body water helps the renal system:
A. Prevent muscle fatigue
B. Maintain blood pressure and cell hydration
C. Increase oxygen delivery to muscles
D. Generate heat during cold stress
Plasma pH is maintained around 7.4 by the kidneys to:
A. Activate digestive enzymes in the stomach
B. Support optimal enzyme activity and cellular function
C. Prevent blood clotting
D. Maintain urinary volume
How does the renal system contribute to regulating mean arterial pressure (MAP)?
A. By filtering out all ions from the blood
B. By secreting digestive enzymes
C. By adjusting blood volume through water and sodium regulation
D. By blocking neural signals to blood vessels
What is the function of erythropoietin produced by the kidney?
A. Enhances urine concentration
B. Stimulates red blood cell production in the bone marrow
C. Breaks down waste in the liver
D. Maintains plasma protein levels
B. Stimulates red blood cell production in the bone marrow
Removing toxins and drugs from plasma is important because:
A. It prevents excessive clotting in the bloodstream
B. It neutralizes immune cells
C. It detoxifies the blood and maintains homeostasis
D. It supports protein synthesis in the kidney
C. It detoxifies the blood and maintains homeostasis
watersoluble or through feces
Which of the following is a homeostatic function of the renal system?
A. Digestion of lipids
B. Regulation of plasma ion concentration
C. Synthesis of vitamin D
D. Production of digestive enzymes
B. Regulation of plasma ion concentration
K+, Na+, Cl-
The renal system helps regulate plasma pH. What is the normal value it maintains?
A. 6.8
B. 7.0
C. 7.4
D. 8.0
C. 7.4
Which hormone is produced by the kidneys to stimulate red blood cell production?
A. Renin
B. Insulin
C. Aldosterone
D. Erythropoietin
D. Erythropoietin
Which of the following would be a consequence if the kidneys failed to remove waste from plasma?
A. Decreased blood pressure
B. Muscle hypertrophy
C. Accumulation of toxins and drugs in the body
D. Increased oxygen transport
C. Accumulation of toxins and drugs in the body
The renal system contributes to blood pressure regulation by helping to control:
A. Alveolar ventilation
B. Plasma protein synthesis
C. Mean arterial pressure
D. Cardiac output only
C. Mean arterial pressure
Which of the following compartments contains the greatest volume of water in the body?
A. Plasma
B. Extracellular fluid (ECF)
C. Intracellular fluid (ICF)
D. Interstitial fluid
C. Intracellular fluid (ICF)
6 gallons
Plama & ECF has 3 gallons in total
Approximately how much intracellular water does the human body contain?
A. 2.4 gallons
B. 0.6 gallons
C. 6 gallons
D. 1 gallon
C. 6 gallons
What is the total volume of plasma and extracellular fluid combined?
A. 3.0 gallons
B. 6.0 gallons
C. 2.4 gallons
D. 1.8 gallons
A. 3.0 gallons
How does the body maintain fluid volume homeostasis?
A. By regulating digestion speed
B. By increasing oxygen delivery
C. By matching fluid intake to fluid loss
D. By storing excess fluid in the liver
C. By matching fluid intake to fluid loss
Which system is primarily responsible for adjusting fluid loss?
A. Nervous system
B. Digestive system
C. Endocrine system
D. Renal system
D. Renal system
Which of the following is a metabolic waste product derived from protein metabolism?
A. Urate
B. Creatinine
C. Urobilin
D. Urea
D. Urea
What is the source of urate in the body?
A. Breakdown of red blood cells
B. Breakdown of nucleic acids
C. Breakdown of carbohydrates
D. Breakdown of fats
B. Breakdown of nucleic acids
Creatinine is a waste product that comes from:
A. Liver metabolism
B. Muscle breakdown
C. DNA synthesis
D. Bone remodeling
B. Muscle breakdown
Which of the following is associated with red blood cell breakdown?
A. Urea
B. Creatinine
C. Urobilins
D. Urate
C. Urobilins
What characteristic do toxins and drugs eliminated by the renal system typically share?
A. Fat-solubility
B. Volatile nature
C. Water-solubility
D. Protein-binding
C. Water-solubility
To be excreted in urine, substances must usually be water-soluble, so they can dissolve in plasma and be filtered by the kidneys.
What is the primary responsibility of the renal system?
A. Delivering oxygen to tissues
B. Cleaning and conditioning the blood
C. Producing white blood cells
D. Digesting nutrients
B. Cleaning and conditioning the blood
Why is cleaning the blood considered a conundrum by the renal system?
A. The blood is too acidic to clean
B. Blood contains too many cells
C. Blood is a watery liquid
D. The kidneys have limited filtration power
C. Blood is a watery liquid
Which of the following best describes the unique challenge of filtering blood?
A. Solids are too large to remove
B. The watery nature of blood makes separating wastes complex
C. The kidneys only regulate hormones
D. Blood contains only water and no toxins
B. The watery nature of blood makes separating wastes complex
Which of the following is NOT a direct anatomical component of the renal system?
A. Kidney
B. Ureter
C. Bladder
D. Diaphragm
D. Diaphragm
What is the function of the ureters?
A. Filter blood
B. Store urine
C. Transport urine from the kidneys to the bladder
D. Excrete urine to the outside of the body
C. Transport urine from the kidneys to the bladder
Ureters are tubes that carry urine from each kidney to the bladder
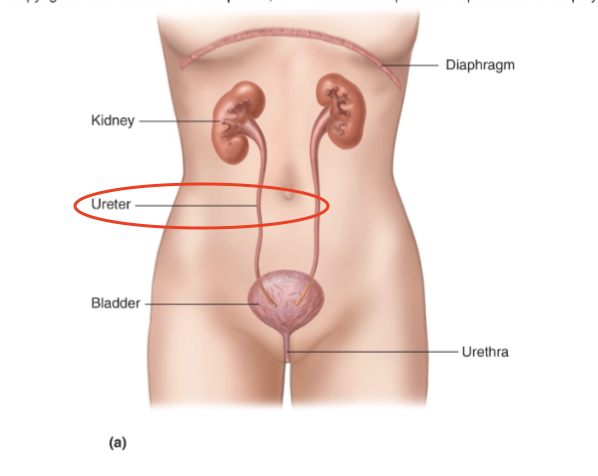
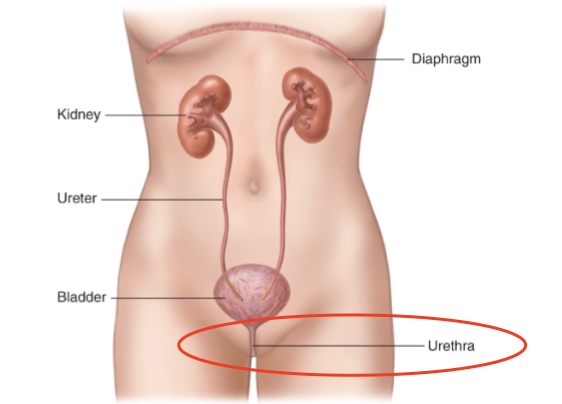
The urethra's primary role is to:
A. Produce urine
B. Transport urine from the kidney to the bladder
C. Excrete urine out of the body
D. Reabsorb water into the bloodstream
C. Excrete urine out of the body
How is the cardiovascular system involved in renal function?
A. It stores urine temporarily
B. It delivers oxygen to the kidneys only
C. It supplies blood to the kidneys for filtration
D. It absorbs nutrients from urine
C. It supplies blood to the kidneys for filtration
Which of the following best represents the kidney's method of cleaning the plasma, based on the closet analogy?
A. The kidney analyzes each item in the blood and only removes what is waste
B. The kidney filters everything out first, then selectively returns what it wants to keep
C. The kidney stores all blood components and later decides what to release
D. The kidney only removes harmful substances from the beginning
B. The kidney filters everything out first, then selectively returns what it wants to keep
Analogy: take everything out of closet→ go through it → put stuff you want to keep back into closet → get rid of stuff you dont want anymore
What is the physiological term for the kidney "putting back" items it wants to keep?
A. Filtration
B. Secretion
C. Reabsorption
D. Excretion
C. Reabsorption
Reabsorption is the process by which the kidney returns valuable substances (like glucose, ions, water) from the filtrate back into the bloodstream
In the closet analogy for kidney function, what does it represent when the kidney "goes back" and grabs additional items to throw out that weren't part of the original cleanup?
A. Returning useful substances from the urine back into the bloodstream (reabsorption)
B. The initial removal of everything from the blood into the nephron (filtration)
C. Actively moving extra waste from the blood into the nephron after filtration (secretion)
D. Drawing out water to reduce the volume of the final urine (concentration)
C. Actively moving extra waste from the blood into the nephron after filtration (secretion)
In the closet analogy, what does the “stuff left on the floor” represent in kidney function?
A. Substances reabsorbed
B. Blood cells
C. Waste products to be excreted
D. Plasma proteins
C. Waste products to be excreted
this can be urea, urate, creatinine, urabicil
Which region of the kidney is the outermost layer where initial filtration occurs?
A. Medulla
B. Renal pelvis
C. Cortex
D. Pyramid
C. Cortex
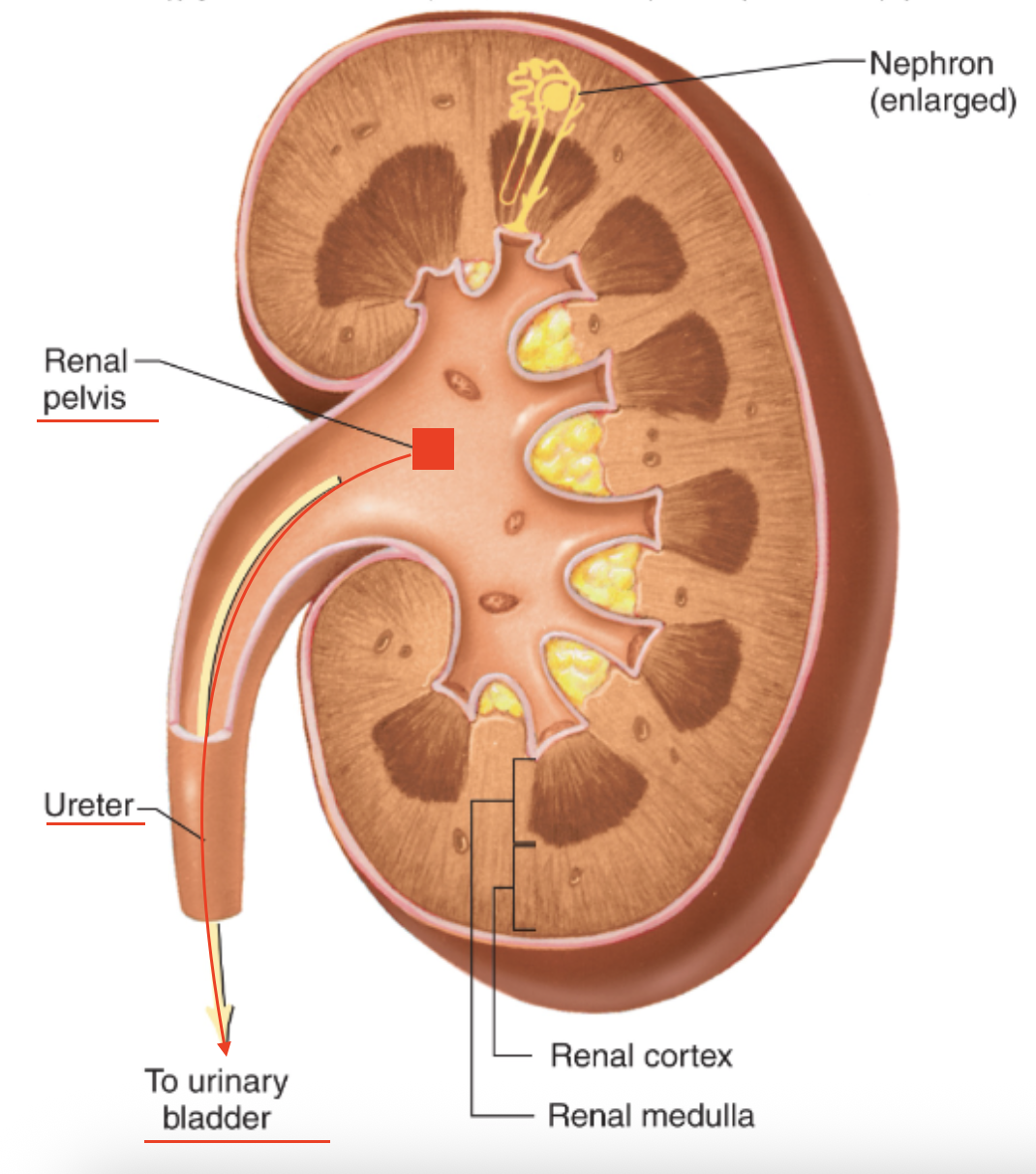
What is the correct flow of urine from the kidney to the bladder?
A. Cortex → Pyramid → Renal pelvis → Calyx → Ureter
B. Pyramids → Calyces → Renal pelvis → Ureter
C. Medulla → Cortex → Calyx → Ureter
D. Cortex → Renal pelvis → Ureter → Calyx
B. Pyramids → Calyces → Renal pelvis → Ureter
and then to the urinary bladder
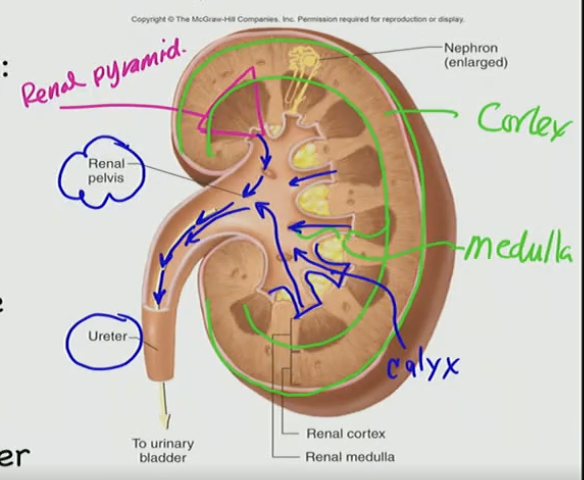
The renal medulla is composed primarily of:
A. Calyces and ureters
B. Renal pyramids
C. Glomeruli
D. Nephrons only
B. Renal pyramids
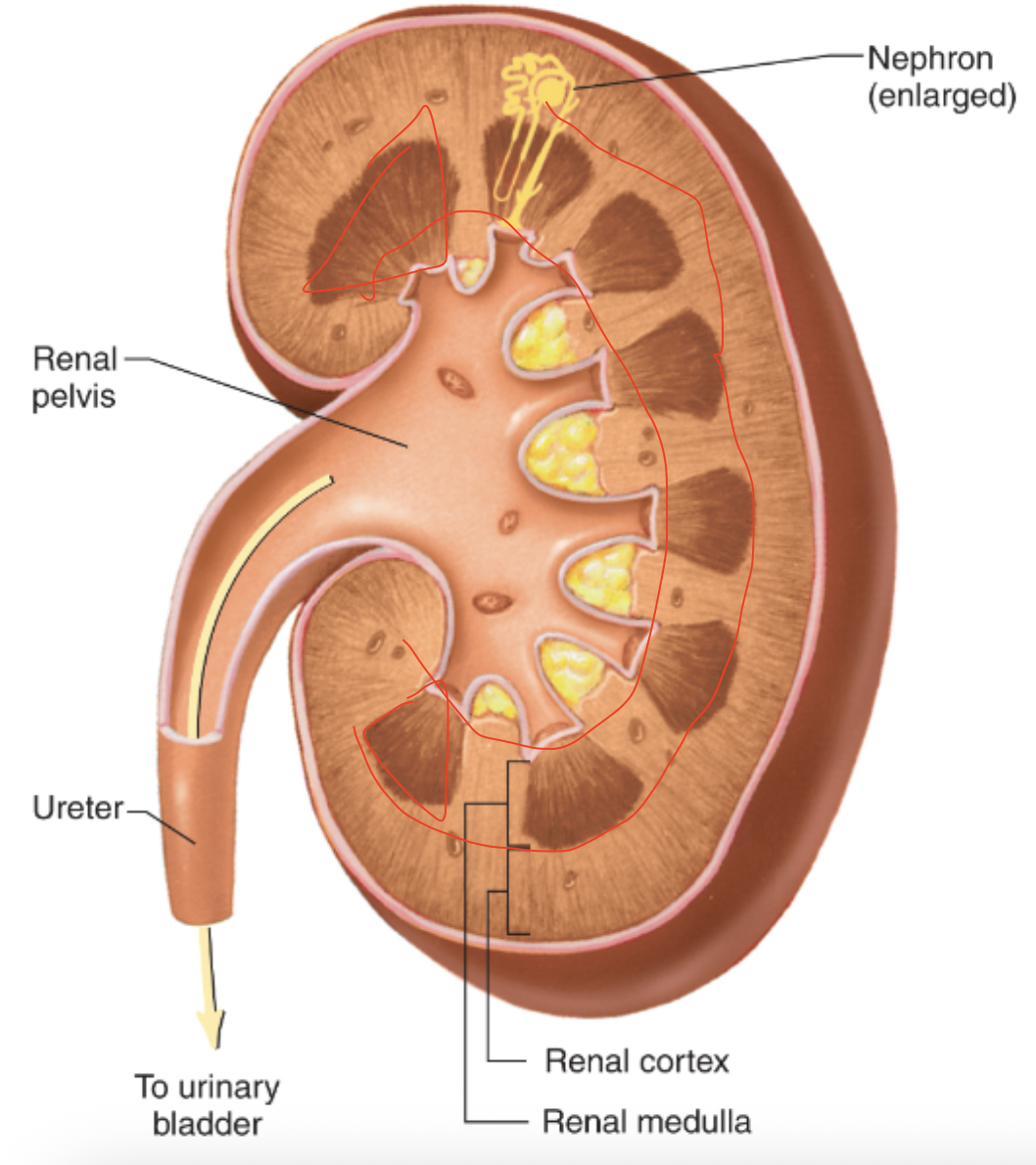
Which structure collects urine directly from the pyramids?
A. Renal cortex
B. Renal capsule
C. Calyx
D. Renal pelvis
C. Calyx
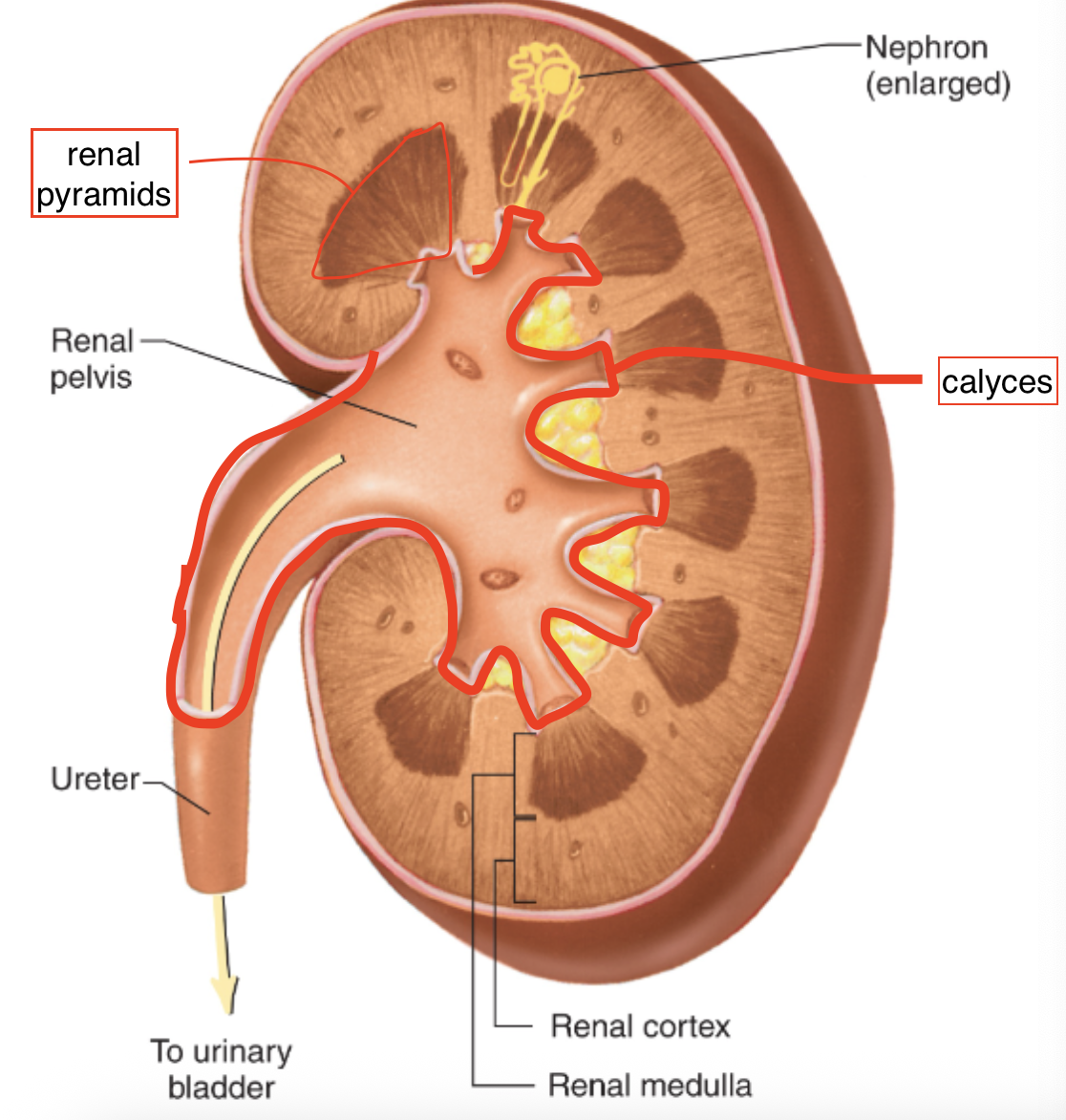
What structure transports urine from the renal pelvis to the bladder?
A. Urethra
B. Ureter
C. Calyx
D. Medulla
B. Ureter
ureter is the tube that carries urine from the renal pelvis to the urinary bladder
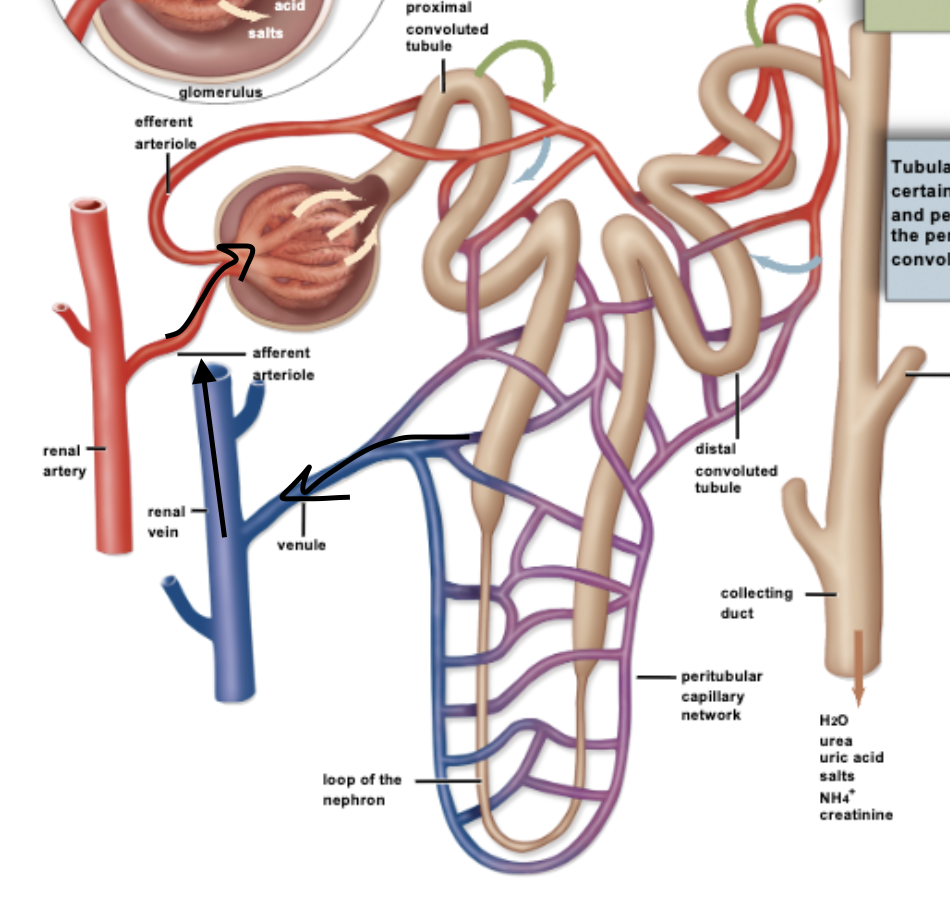
What is the primary urine-forming unit in the kidney?
A. Glomerulus
B. Renal pelvis
C. Nephron
D. Ureter
C. Nephron
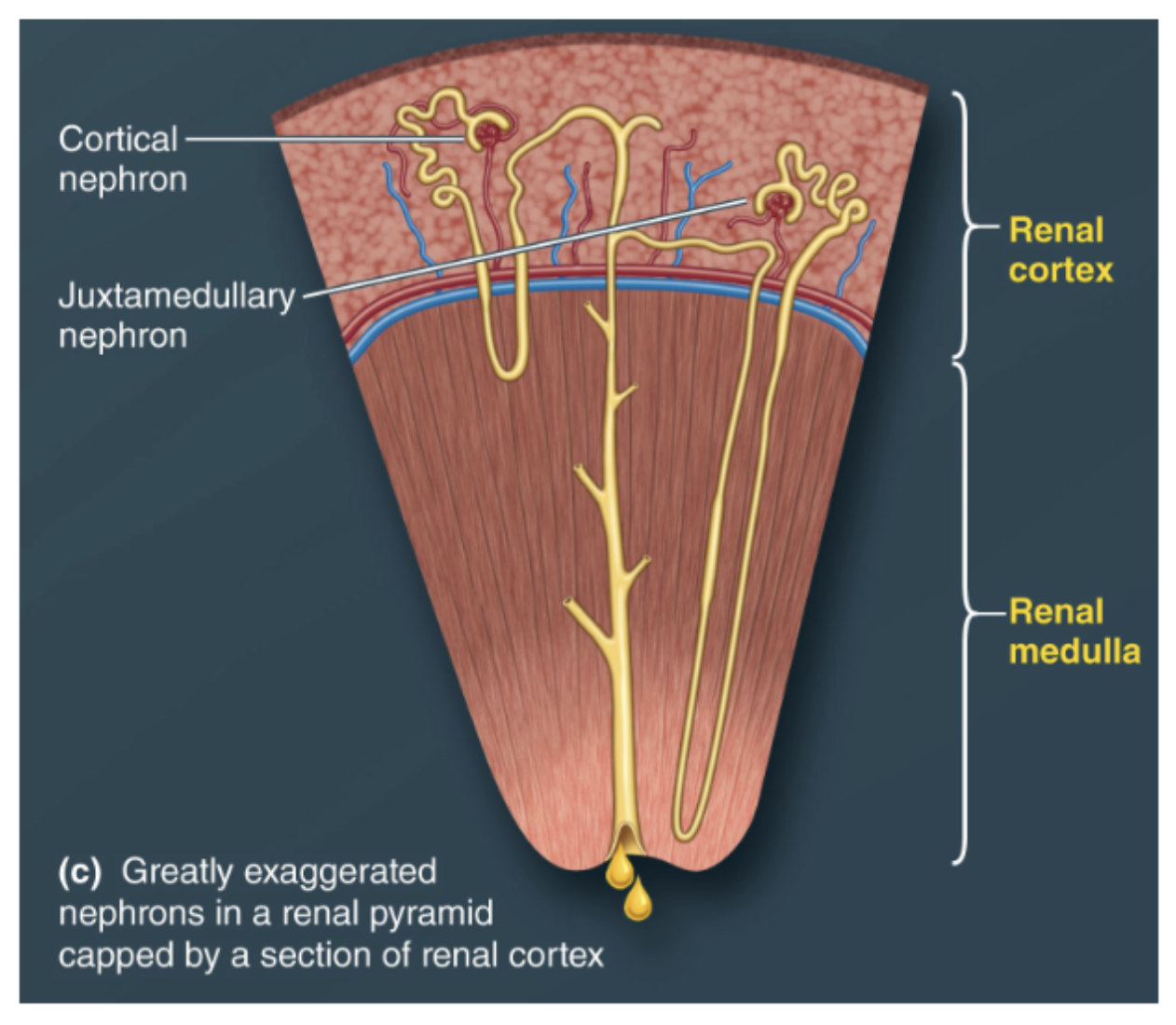
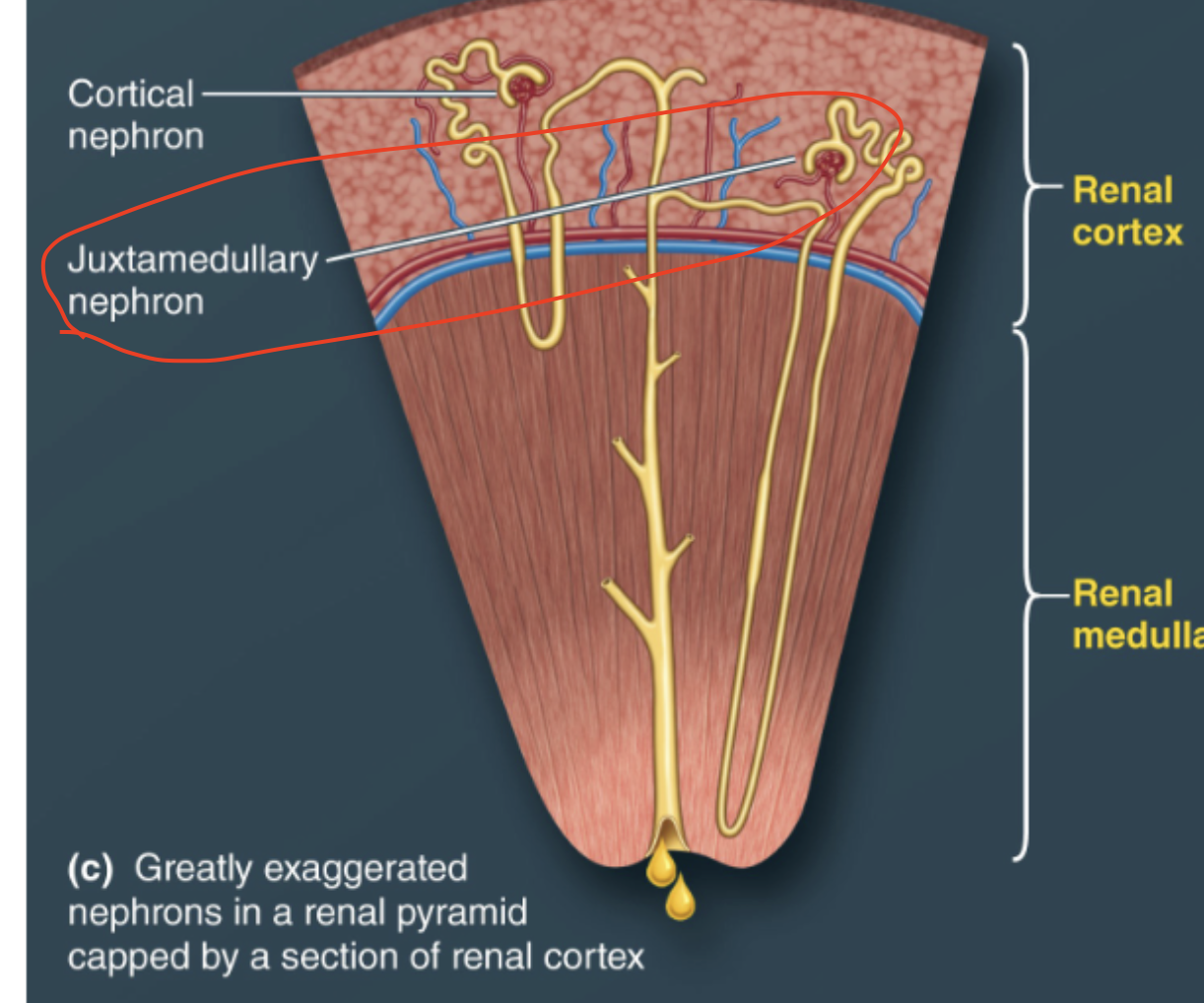
Which type of nephron has a long loop of Henle that extends deep into the medulla?
A. Cortical nephron
B. Juxtamedullary nephron
C. Renal tubule
D. Collecting duct
B. Juxtamedullary nephron
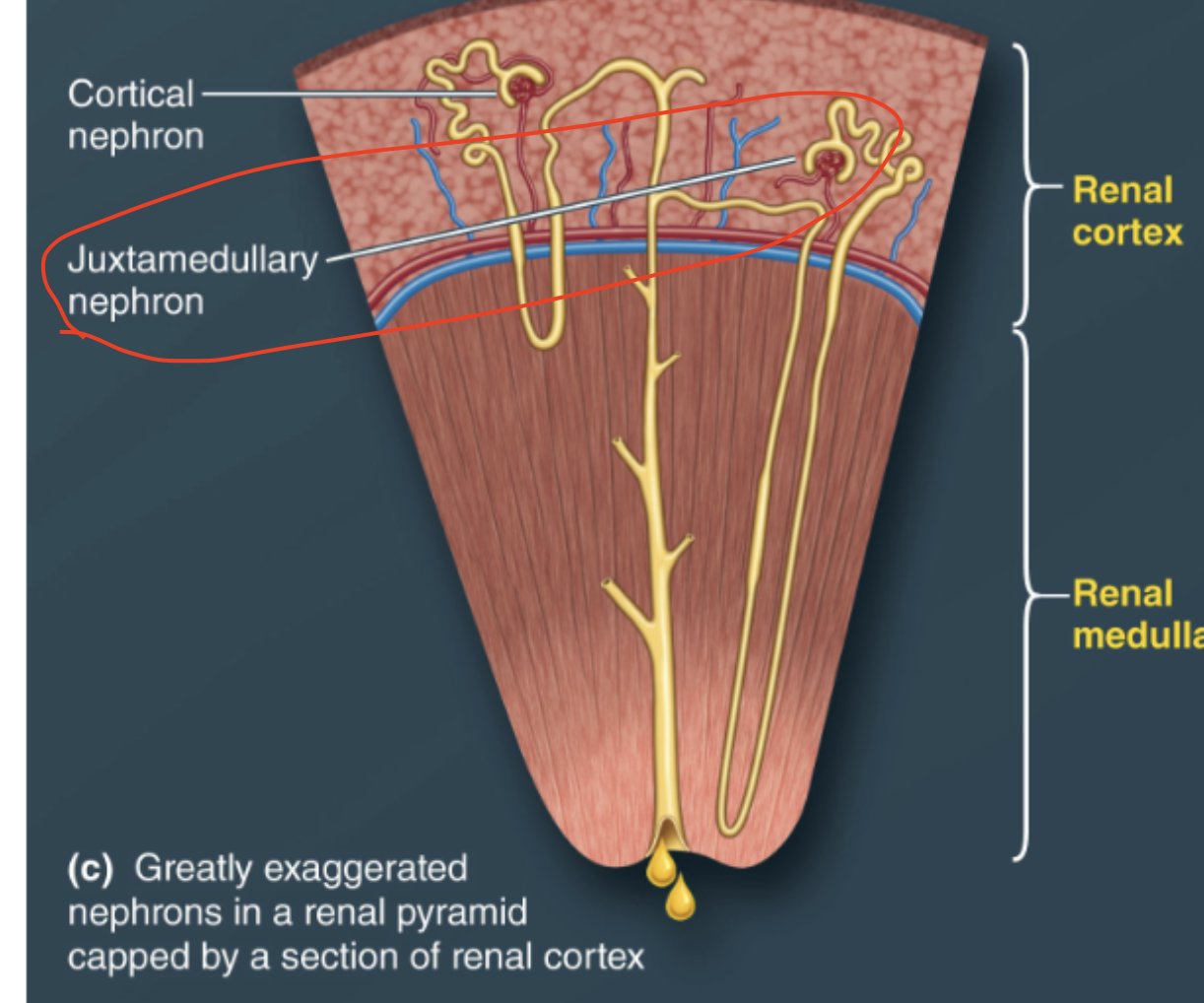
Approximately what percentage of nephrons are cortical nephrons?
A. 20%
B. 50%
C. 60%
D. 80%
D. 80%
What happens to the filtrate once it exits the collecting duct?
A. It can still be reabsorbed
B. It becomes urine and can no longer be modified
C. It is returned to the blood
D. It enters the proximal tubule
B. It becomes urine and can no longer be modified
Both cortical and juxtamedullary nephrons drain into which structure?
A. Ureter
B. Renal pelvis
C. Calyx
D. Collecting duct
D. Collecting duct
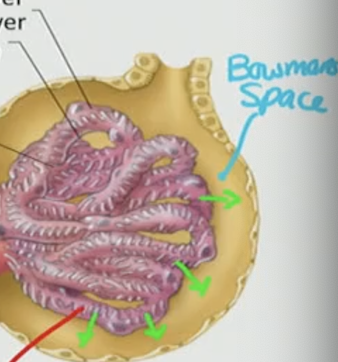
Where does filtration of blood into the nephron occur?
A. Loop of Henle
B. Distal convoluted tubule
C. Bowman’s capsule
D. Collecting duct
C. Bowman’s capsule
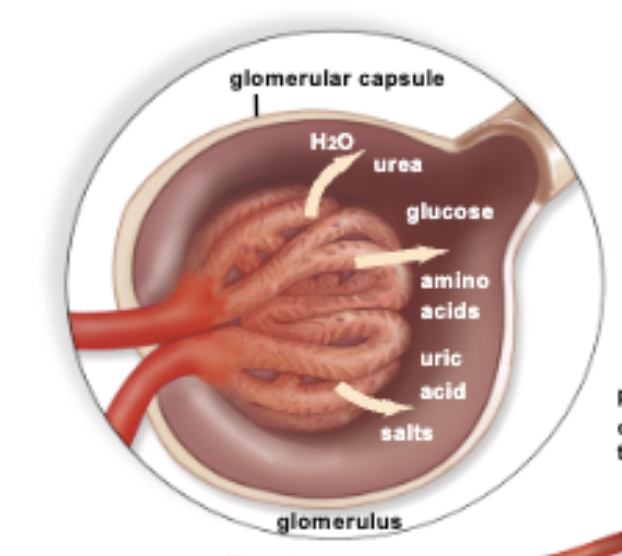
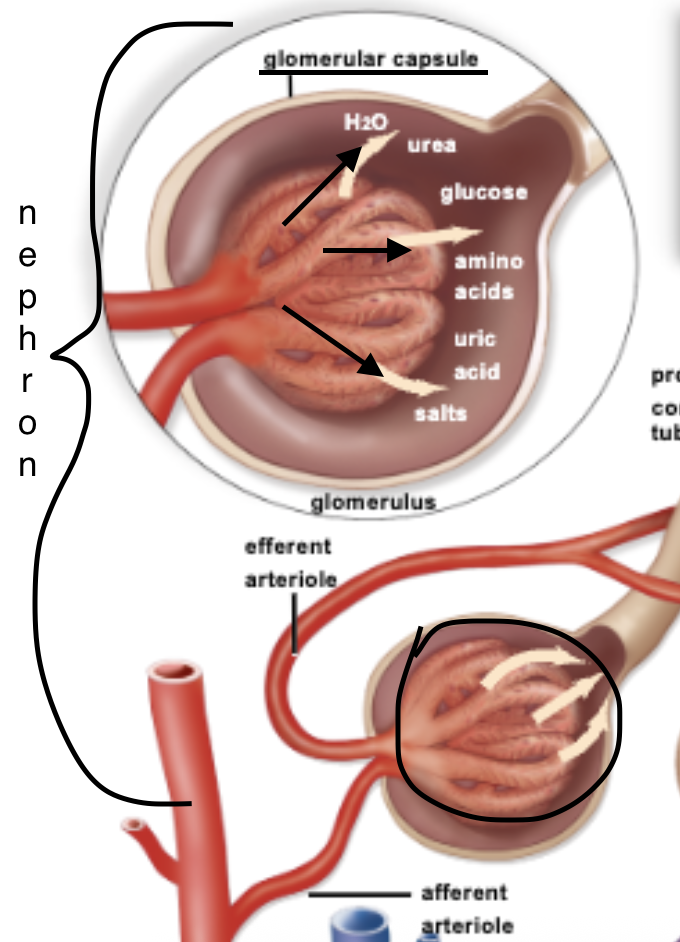
Filtration occurs at the interface of the glomerular capillaries and Bowman’s capsule. Small molecules like water, ions, and glucose pass into the nephron to form filtrate.
What is the primary function of the proximal convoluted tubule (PCT)?
A. Filtration of blood
B. Regulation of reabsorption
C. Reabsorption of water, ions, glucose, and amino acids
D. Secretion of toxins
C. Reabsorption of water, ions, glucose, and amino acids

What structure helps create a standing osmotic gradient in the nephron?
A. Distal convoluted tubule
B. Collecting duct
C. Loop of Henle
D. Bowman’s capsule
C. Loop of Henle
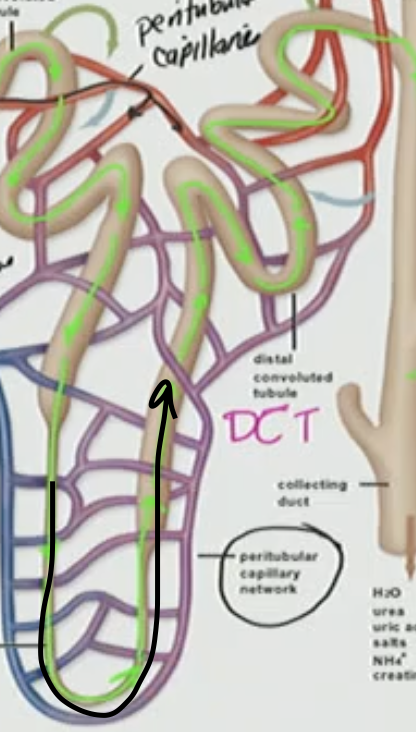
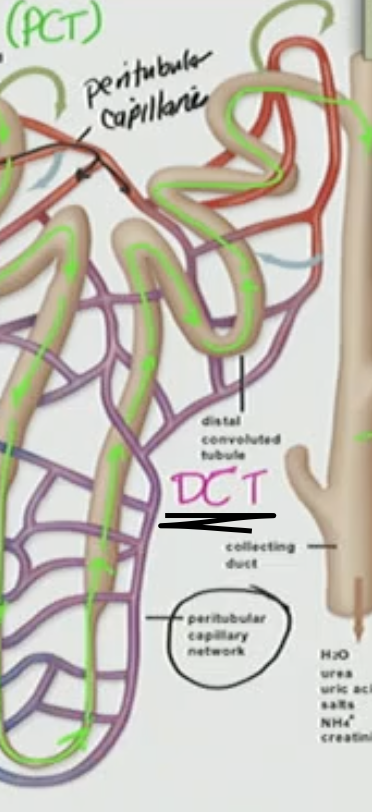
What part of the nephron is primarily involved in regulated reabsorption?
A. Bowman’s capsule
B. Distal convoluted tubule
C. Proximal convoluted tubule
D. Glomerular capillaries
B. Distal convoluted tubule (DCT)
Which capillaries are involved in the initial filtration of blood into the nephron?
A. Peritubular capillaries
B. Afferent arterioles
C. Glomerular capillaries
D. Vasa recta
C. Glomerular capillaries
filtration site inside Bowman’s capsule where plasma is pushed out under pressure to form filtrate
What is the correct order of tubular fluid flow through the nephron?
A. Glomerulus → Proximal convoluted tubule → Loop of Henle → Collecting duct → Distal convoluted tubule
B. Bowman’s capsule → Distal convoluted tubule → Loop of Henle → Collecting duct → Proximal convoluted tubule
C. Bowman’s capsule → Proximal convoluted tubule → Loop of Henle → Distal convoluted tubule → Collecting duct
D. Bowman’s capsule → Loop of Henle → Proximal convoluted tubule → Collecting duct → Distal convoluted tubule
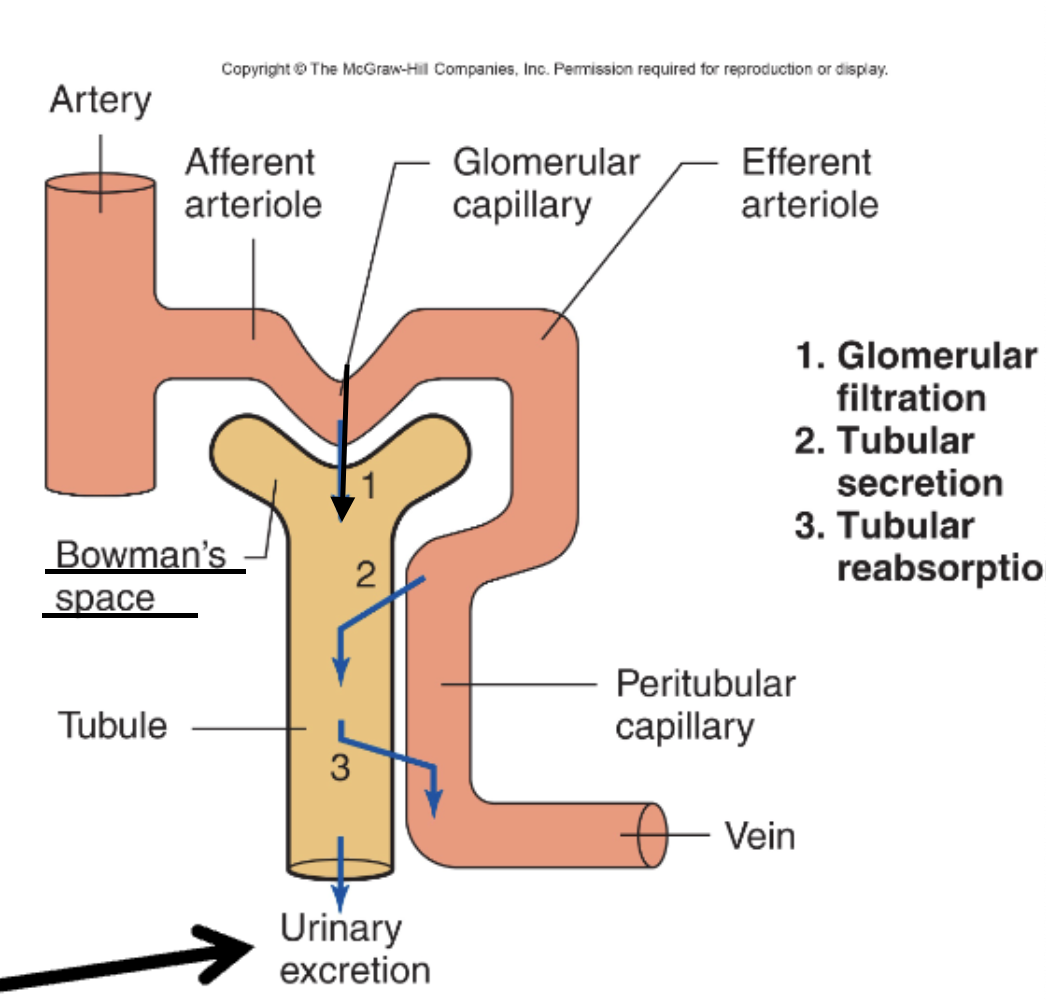
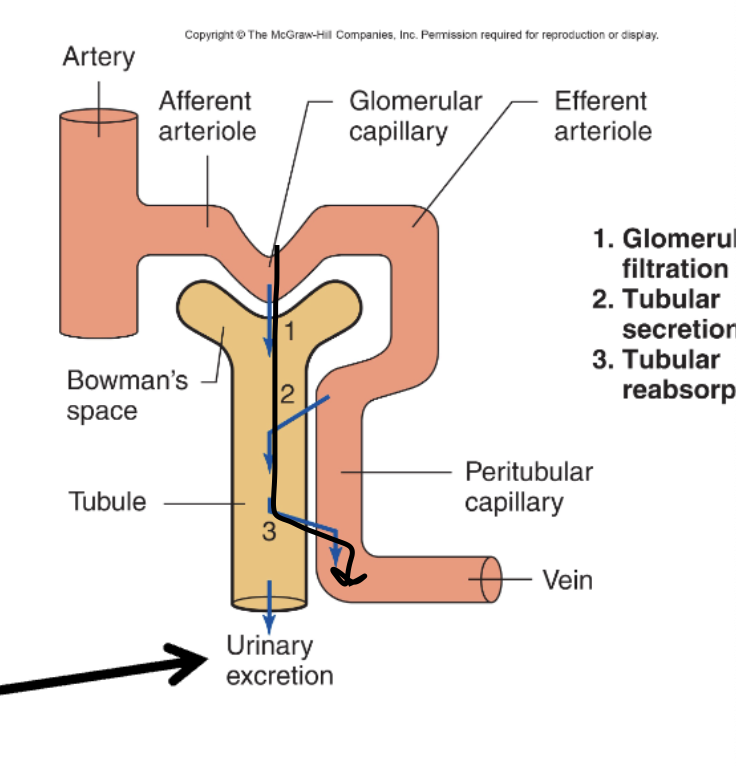
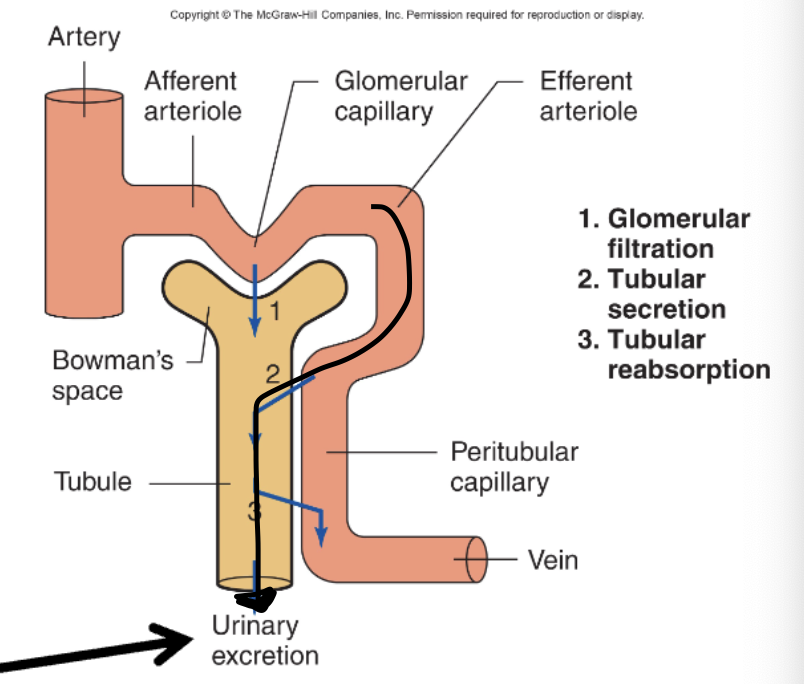
C. Bowman’s capsule → Proximal convoluted tubule → Loop of Henle → Distal convoluted tubule → Collecting duct
Which of the following represents the correct blood flow through the kidney's vascular supply?
A. Glomerular capillaries → Afferent arteriole → Efferent arteriole → Peritubular capillaries
B. Afferent arteriole → Glomerular capillaries → Efferent arteriole → Peritubular capillaries
C. Peritubular capillaries → Efferent arteriole → Glomerular capillaries → Afferent arteriole
D. Efferent arteriole → Afferent arteriole → Glomerular capillaries → Peritubular capillaries
B. Afferent arteriole → Glomerular capillaries → Efferent arteriole → Peritubular capillaries
What is the approximate osmolarity of normal blood plasma?
A. 150–180 mOsm/L
B. 380–420 mOsm/L
C. 100–200 mOsm/L
D. 280–300 mOsm/L
D. 280–300 mOsm/L
What happens to osmolarity as you descend the loop of Henle into the medulla?
A. It decreases
B. It stays the same
C. It increases
D. It fluctuates randomly
C. It increases
Which of the following helps create and maintain the standing osmotic gradient in the renal medulla?
A. Afferent arteriole
B. Proximal convoluted tubule
C. Descending and ascending limbs of the loop of Henle
D. Collecting duct only
C. Descending and ascending limbs of the loop of Henle
These loops use countercurrent exchange and selective permeability to water and solutes to generate and maintain the medullary osmotic gradient needed to concentrate urine
Where does glomerular filtration occur?
A. Distal convoluted tubule
B. Collecting duct
C. Renal corpuscle (Bowman's capsule)
D. Peritubular capillaries
C. Renal corpuscle (Bowman's capsule)
What is the direction of movement in tubular reabsorption?
A. From blood into the nephron
B. From nephron into the blood
C. From collecting duct into ureter
D. From nephron to lymphatic system
B. From nephron into the blood
Tubular secretion is best defined as:
A. Movement of protein into the glomerulus
B. Reabsorption of glucose
C. Movement of substances from blood into nephron
D. Movement of filtrate into collecting duct
C. Movement of substances from blood into nephron
What is the final step in the process that results in waste leaving the body?
A. Glomerular filtration
B. Tubular secretion
C. Urinary excretion
D. Tubular reabsorption
C. Urinary excretion
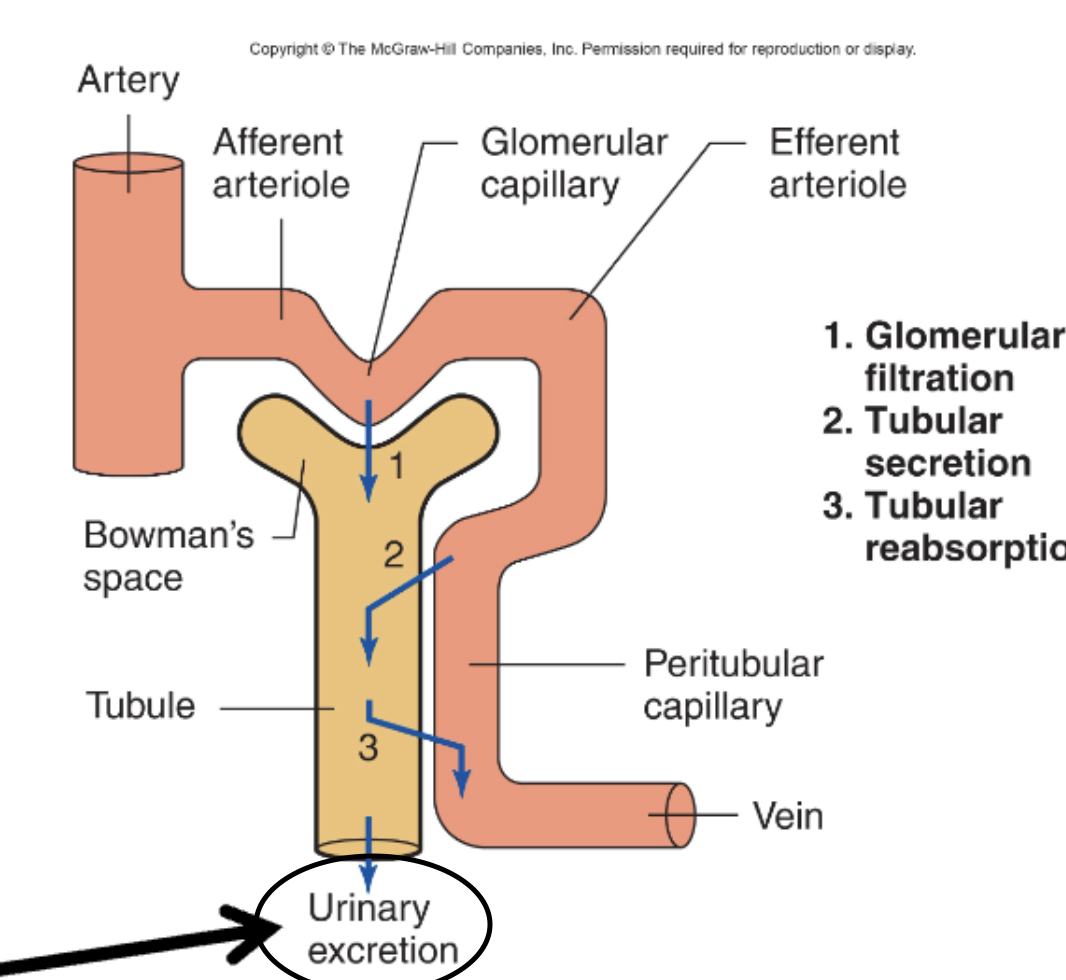
Which process specifically creates the initial, protein-free filtrate?
A. Tubular secretion
B. Urinary excretion
C. Tubular reabsorption
D. Glomerular filtration
D. Glomerular filtration
Where does glomerular filtration occur?
A. Renal pelvis
B. Proximal convoluted tubule
C. Renal corpuscle
D. Loop of Henle
C. Renal corpuscle
What best describes the composition of the filtrate produced at the glomerulus?
A. Mostly proteins and red blood cells
B. Pure water
C. Nearly the same as plasma but protein-free
D. Mostly glucose and amino acids only
C. Nearly the same as plasma but protein-free
Filtrate is mostly water, ions, glucose, and amino acids, similar to plasma, but it is ~99% protein-free and cell-free due to the filtration barrier.
How much filtrate is formed per minute in a healthy adult?
A. 15 mL
B. 60 mL
C. 125 mL
D. 250 mL
C. 125 mL
Approximately what percent of plasma entering the kidneys is filtered into the nephron?
A. 100%
B. 50%
C. 20%
D. 1%
C. 20%
How much filtrate is produced per day?
A. 18–20 L
B. 80–100 L
C. 180–200 L
D. 280–300 L
C. 180–200 L
Which of the following substances are filtered at the glomerulus and must be reabsorbed to prevent their loss in urine?
A. Red blood cells and large proteins
B. Glucose and amino acids
C. Urea and creatinine only
D. Platelets and white blood cells
B. Glucose and amino acids
Which of the following is the first barrier in the glomerular filtration membrane?
A. Basement membrane
B. Podocytes
C. Capillary endothelium
D. Parietal layer of Bowman’s capsule
C. Capillary endothelium
labeled #1
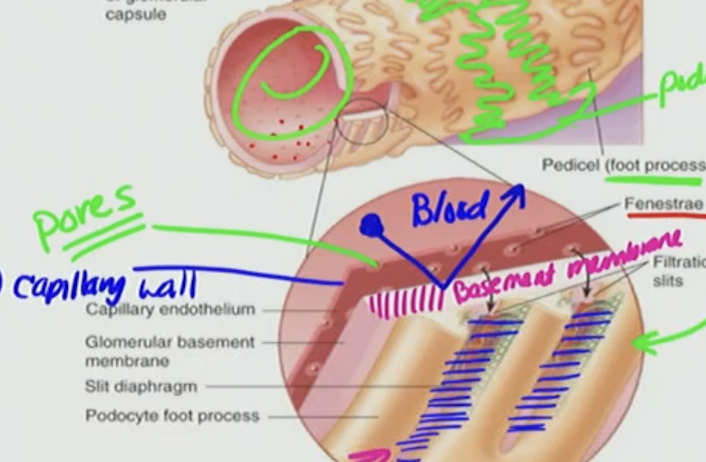
What characteristic of the capillary endothelium facilitates the movement of fluid out of the glomerular capillaries?
A. Negative charge
B. Tight junctions
C. Large fenestrations (pores)
D. Smooth muscle lining
C. Large fenestrations (pores)
These pores allow fluid to leave the capillaries but are too small for cells to pass (RBC & WBC)
Which component of the filtration barrier contributes most to preventing plasma proteins from entering Bowman’s space due to charge repulsion?
A. Podocytes
B. Basement membrane
C. Capillary endothelium
D. Bowman’s capsule parietal layer
B. Basement membrane
The basement membrane of the filtration barrier is made up of what substance that gives it a net charge?
A. Positively charged phospholipids
B. Negatively charged glycoproteins
C. Fenestrated epithelial cells
D. Podocyte foot processes
B. Negatively charged glycoproteins
causing blood to bounce off
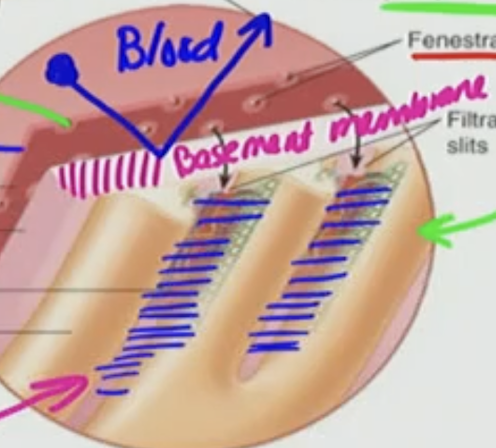
Which of the following is true about podocytes?
A. They are part of the parietal layer of Bowman’s capsule
B. They create fenestrations that allow blood cells to pass
C. They form the visceral layer and have negatively charged proteins
D. They directly produce the filtrate
C. They form the visceral layer and have negatively charged proteins
podocytes form around capillaries
form slit diaphragms that prevent protein passage
Why can proteins generally not pass through the glomerular filtration barrier?
A. They are too small
B. They are actively pumped out
C. They are negatively charged and repelled by the negatively charged barrier
D. They bind to glucose in the plasma
C. They are negatively charged and repelled by the negatively charged barrier
This is referring to the podocytes and basement membrane
Which of the following structures is NOT directly part of the glomerular filtration barrier?
A. Podocyte foot processes
B. Glomerular basement membrane
C. Afferent arteriole
D. Capillary endothelial layer
C. Afferent arteriole
It brings blood to the filtration site but is not itself part of the barrier
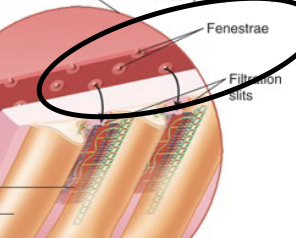
Which of the following best describes the role of podocyte filtration slits?
A. They allow all blood cells to pass into Bowman’s space
B. They increase surface area for reabsorption
C. They regulate protein and macromolecule passage
D. They secrete hormones
C. They regulate protein and macromolecule passage
the slits (foot processes: PEDICEL) acts as a final filtration
What type of charge is associated with both the basement membrane and podocytes?
A. Positive
B. Neutral
C. Negative
D. Variable
C. Negative
Where does the filtered fluid collect immediately after passing the filtration barrier?
A. Proximal tubule
B. Peritubular capillary
C. Bowman’s space
D. Efferent arteriole
C. Bowman’s space
Which structure does blood flow through immediately after the glomerular capillaries?
A. Bowman’s capsule
B. Afferent arteriole
C. Loop of Henle
D. Efferent arteriole
D. Efferent arteriole
Why are large blood cells normally not found in urine?
A. They are positively charged and repel water
B. They are filtered by podocytes
C. They are too large to pass through the fenestrated endothelium
D. They are reabsorbed by the loop of Henle
C. They are too large to pass through the fenestrated endothelium
Which of the following best describes the visceral layer of Bowman’s capsule?
A. It lines the outer wall of the capsule and is made of simple squamous cells.
B. It is in contact with the glomerular capillaries and made of podocytes.
C. It forms the basement membrane that repels proteins from filtrate.
D. It creates a space for urine storage before it enters the proximal tubule.
B. It is in contact with the glomerular capillaries and made of podocytes.
The visceral layer of Bowman’s capsule is the inner layer that wraps around the glomerular capillaries and is made of specialized cells called podocytes, which help form the filtration slits.
Which of the following correctly describes the filtration slits formed by podocytes in the renal corpuscle?
A. They are fenestrae with positive charge, allowing all solutes to pass through.
B. They are called slit diaphragms and are negatively charged to repel proteins.
C. They are tight junctions with a neutral charge, regulating glucose movement.
D. They are gaps in the parietal layer of Bowman’s capsule that attract ions.
B. They are called slit diaphragms and are negatively charged to repel proteins.
Which structure forms the fenestrated capillary wall in the glomerulus?
A. Podocytes
B. Basement membrane
C. Endothelial cells
D. Bowman’s space
C. Endothelial cells
What characteristic of the basement membrane helps prevent filtration of most proteins?
A. Its high osmotic pressure
B. Its positive charge
C. Its tight junctions
D. Its negative charge
D. Its negative charge
Which of the following best describes the charge of the podocyte filtration slits?
A. Positively charged to attract chloride ions
B. Negatively charged to repel proteins
C. Electrically neutral to allow all molecules through
D. Positively charged to block potassium
B. Negatively charged to repel proteins
Which of the following would pass through the glomerular filtration barrier most easily?
A. Albumin (MW > 66 kDa)
B. Red blood cells
C. Sodium ions (Na⁺)
D. Immunoglobulins
C. Sodium ions (Na⁺)
What is the size limit (MW) above which proteins are completely impeded from crossing the glomerular filtration barrier?
A. 10 kDa
B. 50 kDa
C. 100 kDa
D. 150 kDa
C. 100 kDa
Which combination of features allows a molecule to pass easily through the filtration barrier?
A. Large size, negative charge
B. Small size, negative charge
C. Small size, neutral or positive charge
D. Large size, positive charge
C. Small size, neutral or positive charge
Which of the following is true about chloride ions (Cl⁻) and glomerular filtration?
A. They cannot pass because they are negatively charged.
B. They are filtered despite their negative charge.
C. They require active transport into Bowman’s space.
D. They are repelled by the endothelial layer only.
B. They are filtered despite their negative charge.
Cl⁻ is small enough to be filtered even though it's negatively charged.
Which structure forms the filtration slits in the glomerulus?
A. Endothelial fenestrae
B. Basement membrane
C. Tight junctions of epithelial cells
D. Podocyte foot processes
D. Podocyte foot processes
Which of the following structures is NOT part of the glomerular filtration barrier?
A. Fenestrated endothelium
B. Basement membrane
C. Podocyte filtration slits
D. Peritubular capillary endothelium
D. Peritubular capillary endothelium
This capillary is involved in reabsorption and secretion, not filtration
Which of the following is repelled by the negative charge of the basement membrane?
A. Water
B. Na⁺
C. Small negatively charged proteins
D. Glucose
C. Small negatively charged proteins
Which pressure is responsible for pushing fluid out of the glomerular capillaries into Bowman’s space?
A. Plasma oncotic pressure (πGC)
B. Bowman’s hydrostatic pressure (PBS)
C. Glomerular capillary pressure (PGC)
D. Osmotic pressure of filtrate
C. Glomerular capillary pressure (PGC)
Which of the following pressures opposes filtration?
A. PGC only
B. πGC and PBS
C. PGC and PBS
D. πGC only
B. πGC and PBS
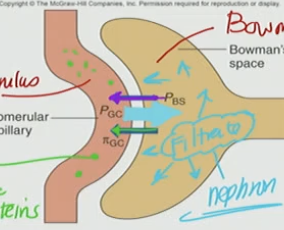
What is the approximate value of glomerular capillary pressure (PGC)?
A. 15 mmHg
B. 29 mmHg
C. 55–60 mmHg
D. 125 mmHg
C. 55–60 mmHg
What is the net filtration pressure (NFP) if PGC = 60 mmHg, PBS = 15 mmHg, and πGC = 29 mmHg?
A. +14 mmHg
B. +16 mmHg
C. +29 mmHg
D. –16 mmHg
B. +16 mmHg
NFP = PGC – PBS – πGC = 60 – 15 – 29 = +16 mmHg
Which pressure is due to the presence of plasma proteins and draws water back into the capillaries?
A. PGC
B. πGC
C. PBS
D. Filtration pressure
B. πGC
Bowman’s hydrostatic pressure (PBS):
A. Favors filtration
B. Equals glomerular capillary pressure
C. Is caused by filtrate volume in Bowman’s space
D. Increases when blood pressure drops
C. Is caused by filtrate volume in Bowman’s space
the blood filtered → volume → Bowman’s Space → PBS
Bowman’s hydrostatic pressure results from filtrate volume in Bowman’s space and opposes filtration
The correct equation for calculating net glomerular filtration pressure is:
A. PGC – πGC – PBS
B. πGC – PGC – PBS
C. PBS + πGC – PGC
D. PGC + πGC – PBS
A. PGC – πGC – PBS
If πGC increases due to more plasma proteins, the net filtration pressure will:
A. Increase
B. Decrease
C. Stay the same
D. Be unaffected
B. Decrease
Increased πGC draws more water back into blood ← , decreasing filtration.
this is due to πGC increases, that “pulling back” force becomes stronger.
So instead of fluid leaving the capillary into Bowman’s space, more of it is pulled back in to the blood and wont get filtered hence the big green arrow going to efferent arteriole
if πGC increases, less filtrate enters → PBS would decrease.
But technically, they are not directly generating each other — they are linked through filtration rate.
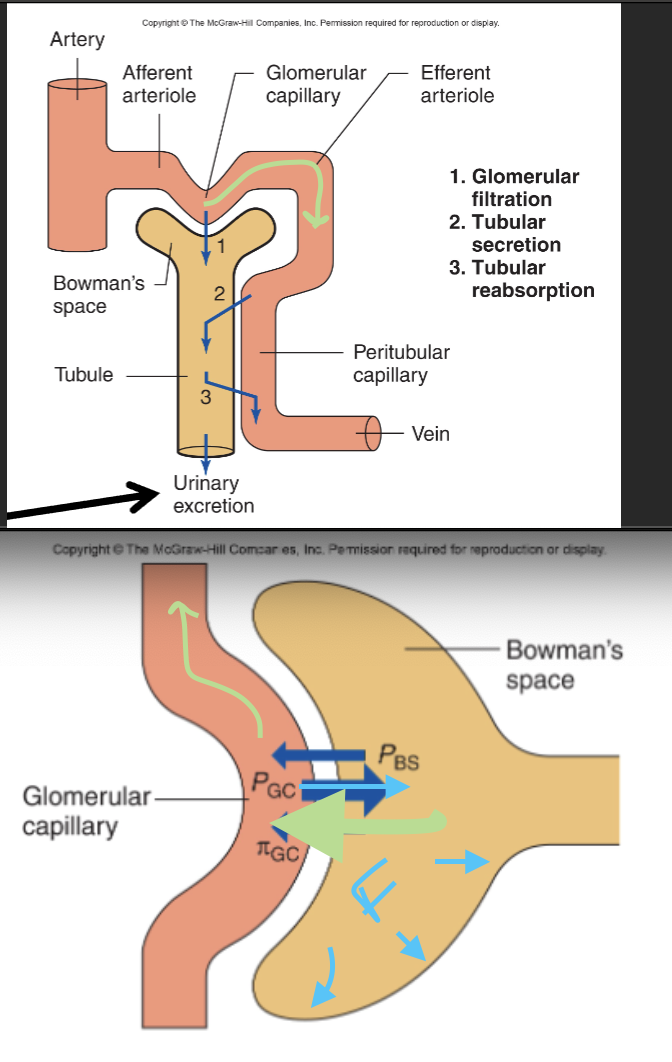
A decrease in which pressure would most likely increase filtration?
A. PGC
B. πGC
C. Net Filtration Pressure
D. Blood volume
B. πGC
Less opposing pull = easier filtration
Lower πGC means less osmotic pull into capillaries, increasing filtration.
Which of the following best describes the consequence of fluid buildup in Bowman’s space on glomerular filtration?
A. It increases filtration by pulling fluid across the basement membrane
B. It decreases filtration by contributing a hydrostatic force opposing fluid entry
C. It promotes reabsorption of plasma proteins into the filtrate
D. It increases glomerular oncotic pressure directly
B. It decreases filtration by contributing a hydrostatic force opposing fluid entry
Which of the following correctly represents the formula for net filtration pressure (P_filtration) in the glomerulus?
A. P_GC + π_GC − P_BS
B. π_GC − P_GC − P_BS
C. P_GC − π_GC − P_BS
D. P_BS − π_GC − P_GC
C. P_GC − π_GC − P_BS