haemoglobin
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
How is oxygen transported in the blood?
It binds to the haem groups in haemoglobin to form oxyhaemoglobin.
equation of reaction in haemoglobin
Hb + 4O2⇋ HbO8 [reversible reaction]
Affinity:how strongly a molecule binds to another
what affects haemoglobin’s affinity for oxygen?
partial pressure of oxygen (pO2)
partial pressure of carbon dioxide (pCO2)
how does pO2 affect the affinity for oxygen?
what is unit of pO2?
when pO2 is high, haemoglobin has a high affinity for oxygen→ haemoglobin binds to oxygen [high saturation of oxygen]
when pO2 is low, haemoglobin has a low affinity for oxygen→ haemoglobin releases oxygen [low saturation of oxygen]
[KPa is the unit]
what are they referred as:
-oxygen joining haemoglobin (2)
-oxygen leaves haemoglobin (2)
-association and loading
-dissociation and unloading
where is high and low pO2 found? why is it important?
-high→lungs→ oxygen can load onto haemoglobin to form oxyhaemoglobin
-low→respiring tissue→ oxyhaemoglobin releases oxygen so the respiring tissue can use it for aerobic respiration
What do oxygen dissociation curves show?
shows how saturated haemoglobin is with oxygen at different partial pressures of oxygen
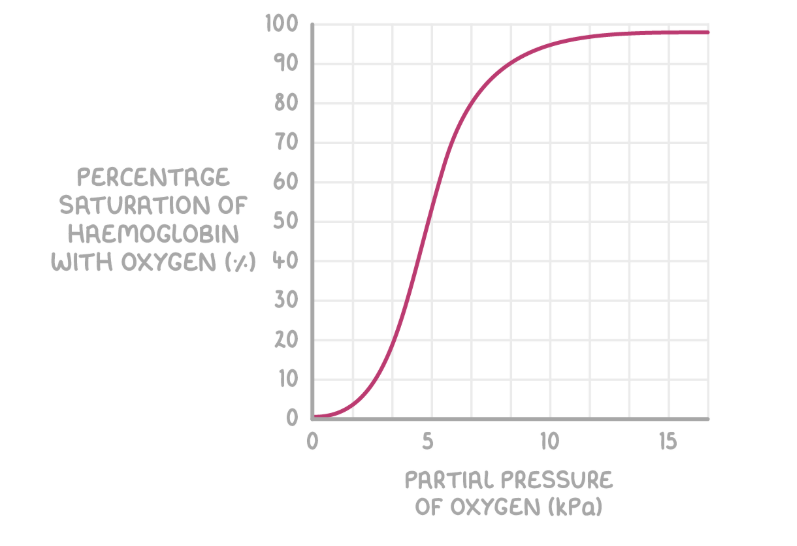
why do oxygen dissociation curves have a S shape?
-Gradient of the curve is initially shallow because the shape of haemoglobin makes it hard for the first oxygen molecule to bind.
-When haemoglobin binds to the first O₂ molecule, its shape changes slightly so it becomes easier for the next O₂ molecules to bind. This causes the gradient to steepen.
-As the haemoglobin becomes more saturated, it becomes harder for more oxygen molecules to bind. This cause the gradient to flatten and level off
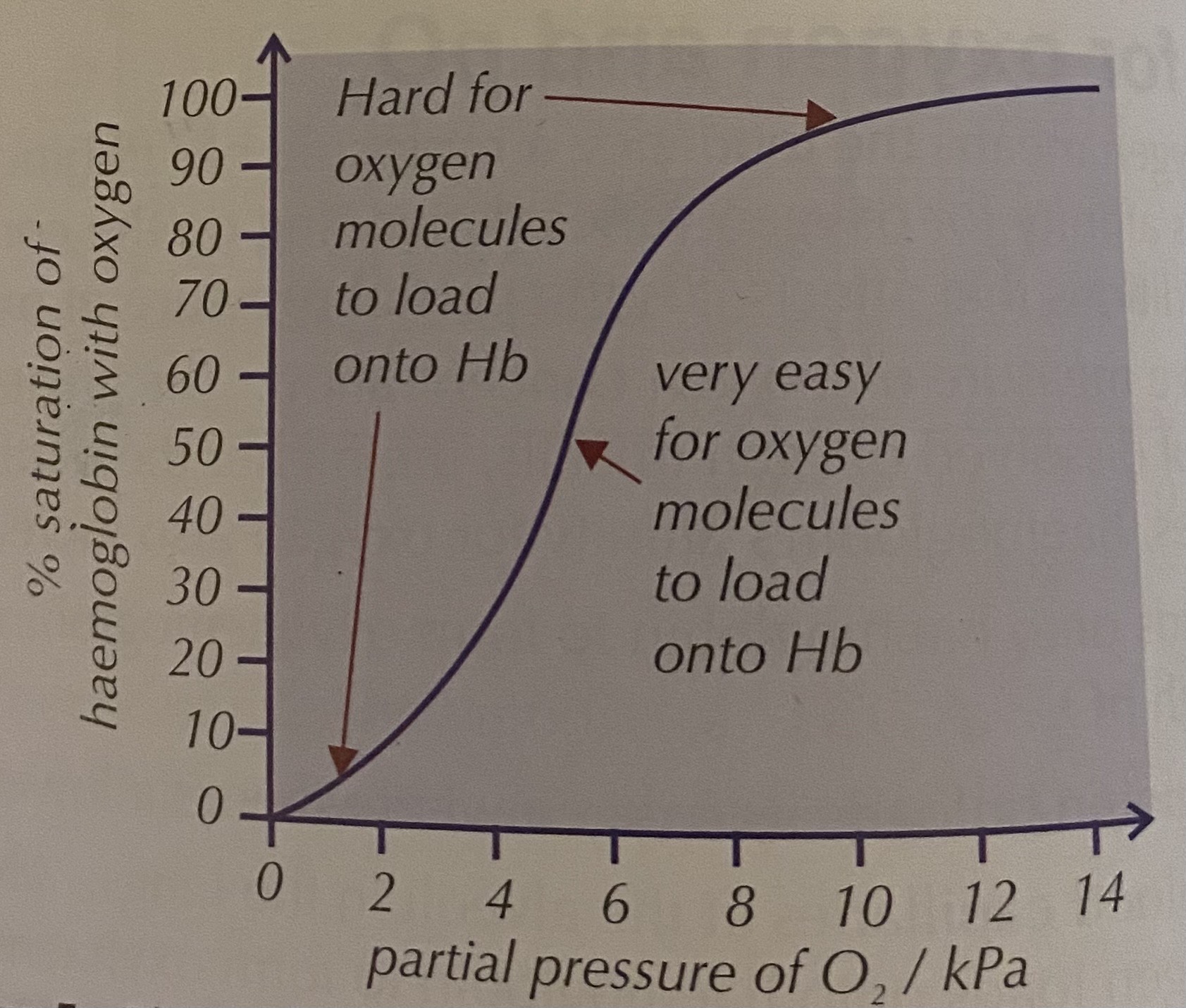
positive cooperativity
when one molecule of oxygen binds to haemoglobin, it makes it easier for the next oxygen molecules to bind.
how does fetus receive oxygen?
from its mother’s blood across the placenta
how does fetal haemoglobin differ from adult haemoglobin?
→why is this difference important?
Fetal haemoglobin has a higher affinity for oxygen.
→so can take up oxygen (becomes more saturated) in lower pO2.The placenta has a low pO2 so adult haemoglobin will release oxygen in placenta .The fetal haemoglobin binds with oxygen at lower pO2.
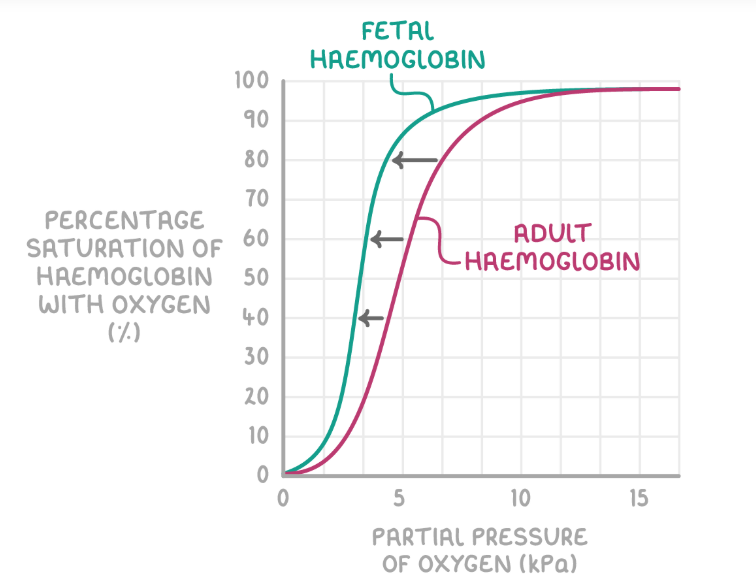
what would happen if the fetal haemoglobin had the same affinity for oxygen as adult haemoglobin?
the fetal blood wouldn’t become fully saturated with oxygen so it wouldn't get enough oxygen for respiration
what would happen if fetal haemoglobin had a very high affinity for oxygen?
it’ll not releases oxygen easily in the fetal tissues
name of effect that links to pCO2?
→what is it?
→why is it important?
→what does it do to the dissociation curve?
Bohr effect
-when pCO2 is high, haemoglobin has a low affinity for oxygen→ haemoglobin releases oxygen
-respiring tissue require more oxygen for aerobic respiration. When tissues respire, they produce more CO₂, which increases the pCO₂.This causes haemoglobin to release oxygen more easily.
-it shifts the oxygen dissociation curve to the right [still the same shape]
![<p><strong>Bohr effect</strong></p><p>-when pCO<sub>2</sub> is <strong>high</strong><sub>, </sub>haemoglobin has a <strong>low affinity</strong> for oxygen→ haemoglobin <u>releases</u> oxygen</p><p>-respiring tissue require <u>more oxygen for aerobic respiration</u>. When tissues <strong>respire</strong>, they produce <strong>more CO₂</strong>, which increases the pCO₂.This causes haemoglobin to release oxygen more easily.</p><p>-it shifts the oxygen dissociation curve to the <strong>right</strong> [still the same shape]</p>](https://knowt-user-attachments.s3.amazonaws.com/a3b5f284-23bb-4fef-84a3-db1605acdb43.png)
how does the size of smaller mammals relate to their haemoglobins? where wld the oxygen dissociation curve shift?
-smaller mammals have a large surface area: volume ratio so they lose heat quickly. More oxygen is required to maintain high rate of respiration to generate heat. This helps maintain constant body temp.Therefore, their haemoglobin has a lower affinity for oxygen to release oxygen easily.
→Their oxygen dissociation curve would be to the right of a human’s.
tip: the further left the curve is, the higher the haemoglobin’s affinity for oxygen is
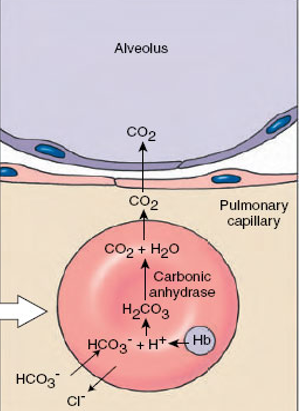
how is CO2 transported in the blood? (3)
-some dissolved in plasma
-some binds to haemoglobin forming carbaminohaemoglobin
-most transported as hydrogencarbonate ions (HCO3-) [bicarbonate ions]
What happens to carbon dioxide (CO₂) once it enters the red blood cell?
-CO2 diffuses into the red blood cell
-CO2 reacts with water to form carbonic acid (H2CO3), catalyzed by the enzyme carbonic anhydrase
-carbonic acid dissociates into hydrogencarbonate ions (HCO₃⁻) and hydrogen ions (H⁺).
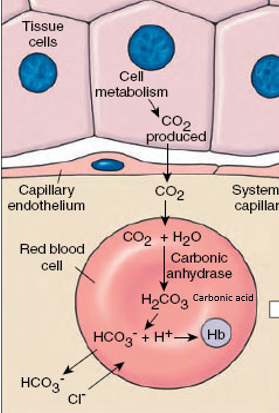
what happens to the released ions?
H+ ions
-H+ ions binds to haemoglobin to form haemoglobinic acid [acts as a buffer (preventing pH change)]
-this reduces haemoglobin’s affinity for oxygen
-this causes haemoglobin to release oxygen
-this prevents the blood from becoming too acidic
hydrogencarbonate ions
-hydrogencarbonate ions diffuse out of the red blood cell and are transported into the plasma
![<p><strong>H<sup>+ </sup>ions</strong></p><p>-H<sup>+ </sup>ions binds to haemoglobin to form<strong> haemoglobinic acid </strong>[<span>acts as a buffer (preventing pH change)]</span></p><p>-this reduces haemoglobin’s affinity for oxygen</p><p>-this causes haemoglobin to release oxygen</p><p>-this prevents the blood from becoming too acidic</p><p><strong>hydrogencarbonate ions</strong></p><p>-hydrogencarbonate ions diffuse out of the red blood cell and are transported into the plasma</p>](https://knowt-user-attachments.s3.amazonaws.com/56144eb7-9ada-44f3-b522-fe4985e6c037.png)
chloride shift
chloride ions diffuse into the red blood cell when hydrogencarbonate ions leave the red blood cell to balance the charges of the red blood cell
what happens when the blood reaches the lungs?
-the low pCO2 in the lungs causes the hydrogencarbonate ions to diffuse back into the red blood cell and react with H+ to reform carbonic acid
-chloride ions diffuses back into the plasma
-carbonic acid is broken down by carbonic anhydrase forming CO2 and water
-CO2 diffuses out of the red blood cell and into the alveoli to be expired