SkM-Parasites
1/224
Earn XP
Description and Tags
12/17 - "we're intestinal parasites - we don't need to thank the host"
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
225 Terms
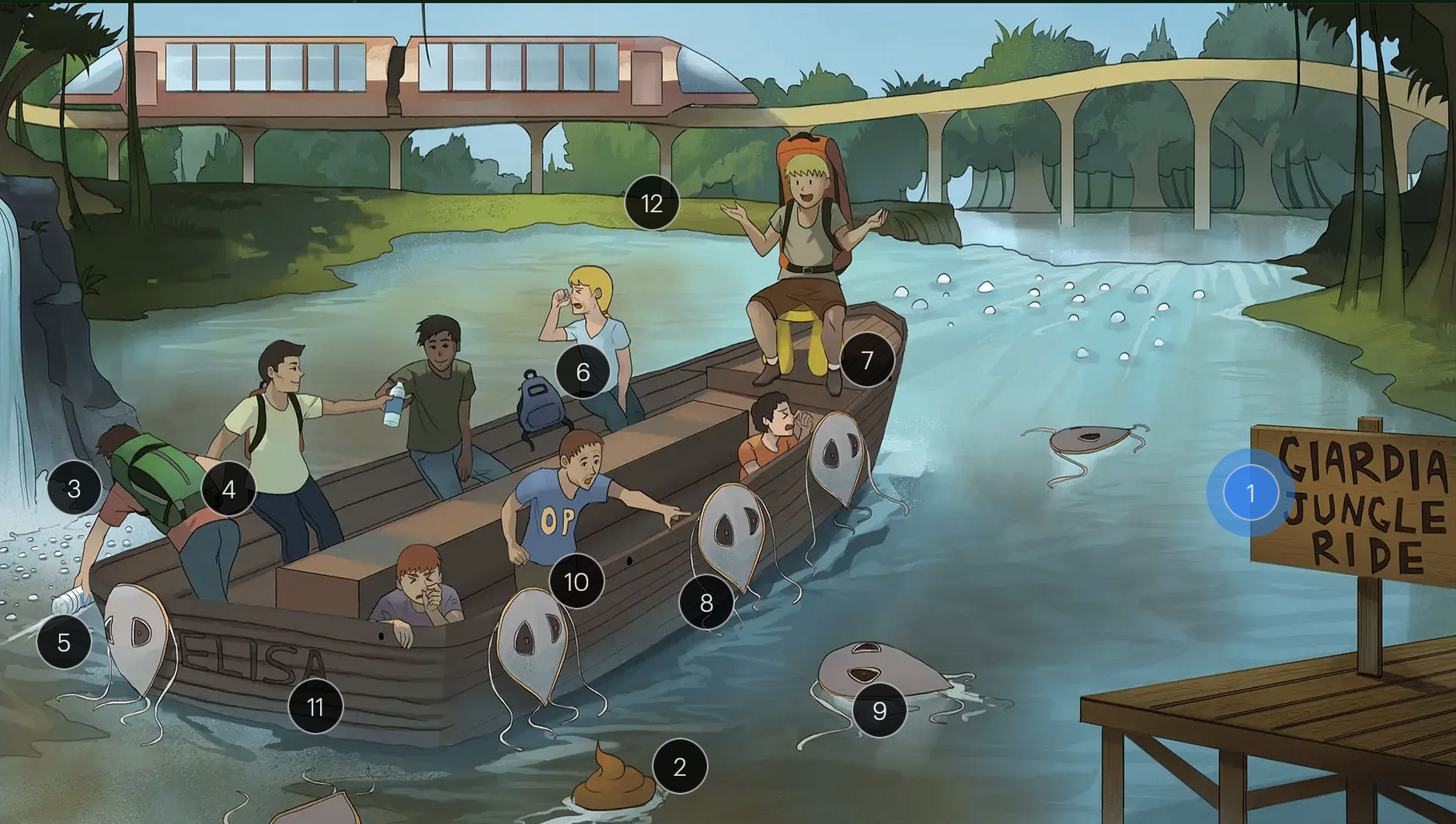
Giardia lamblia
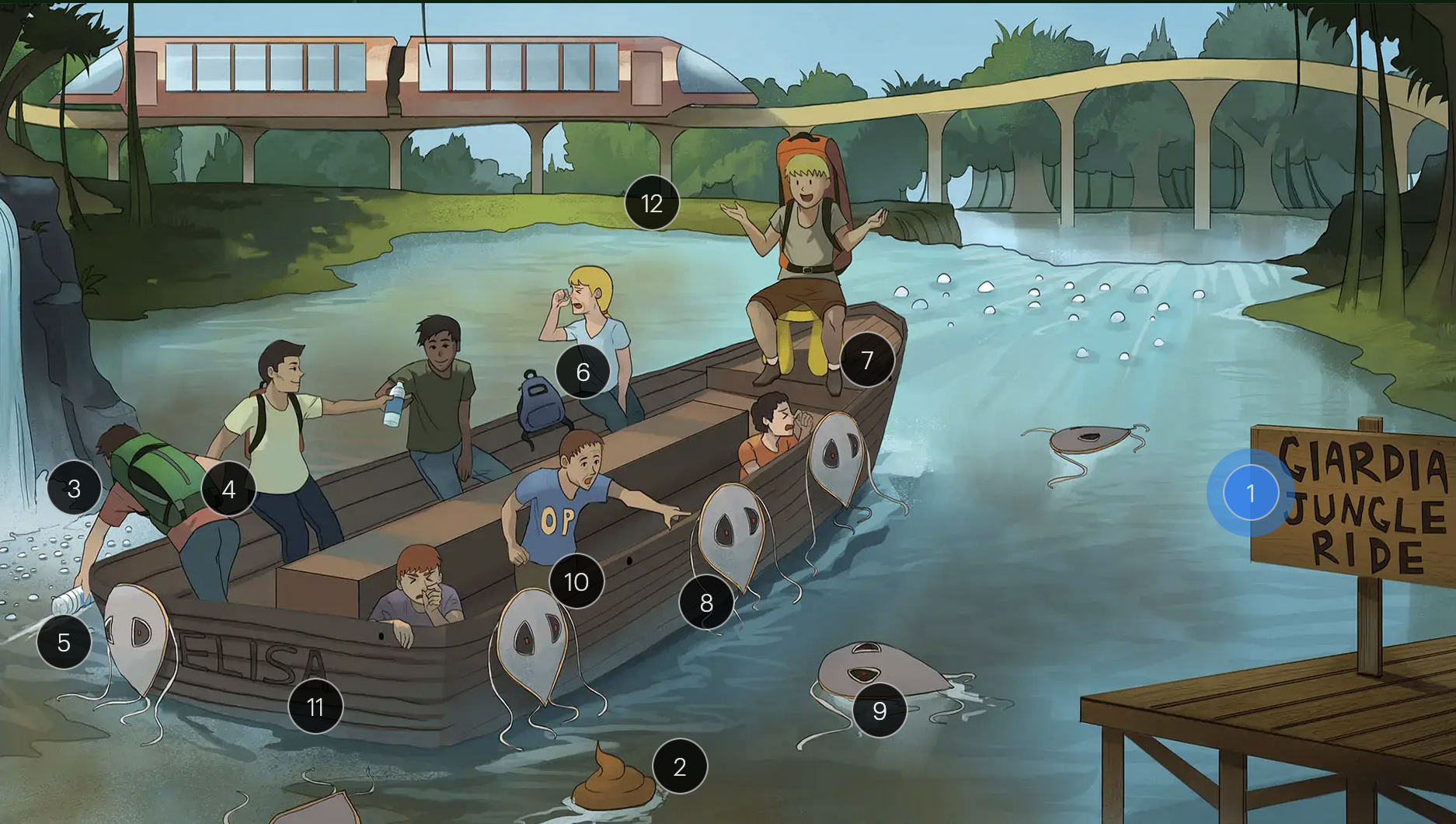
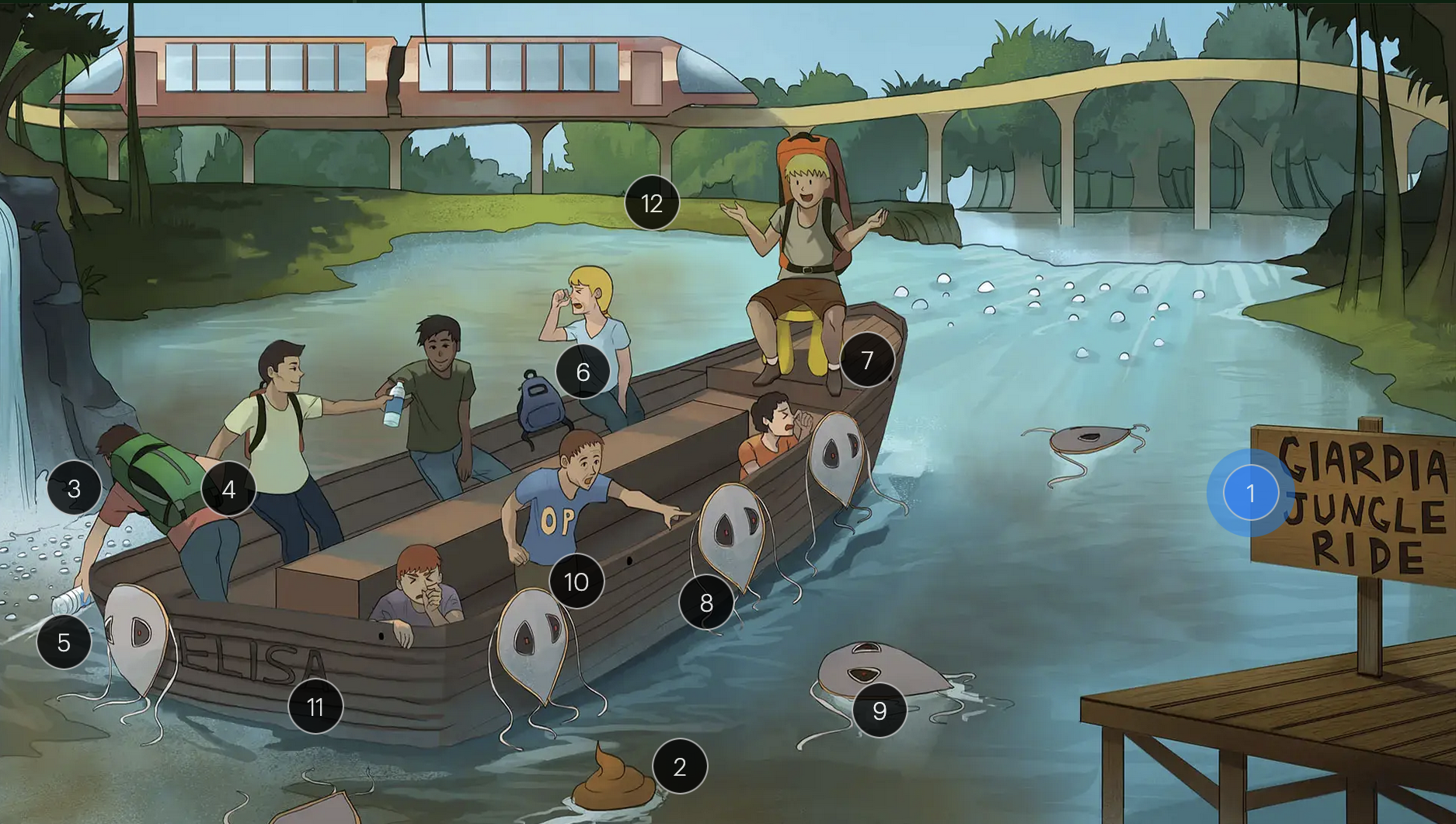
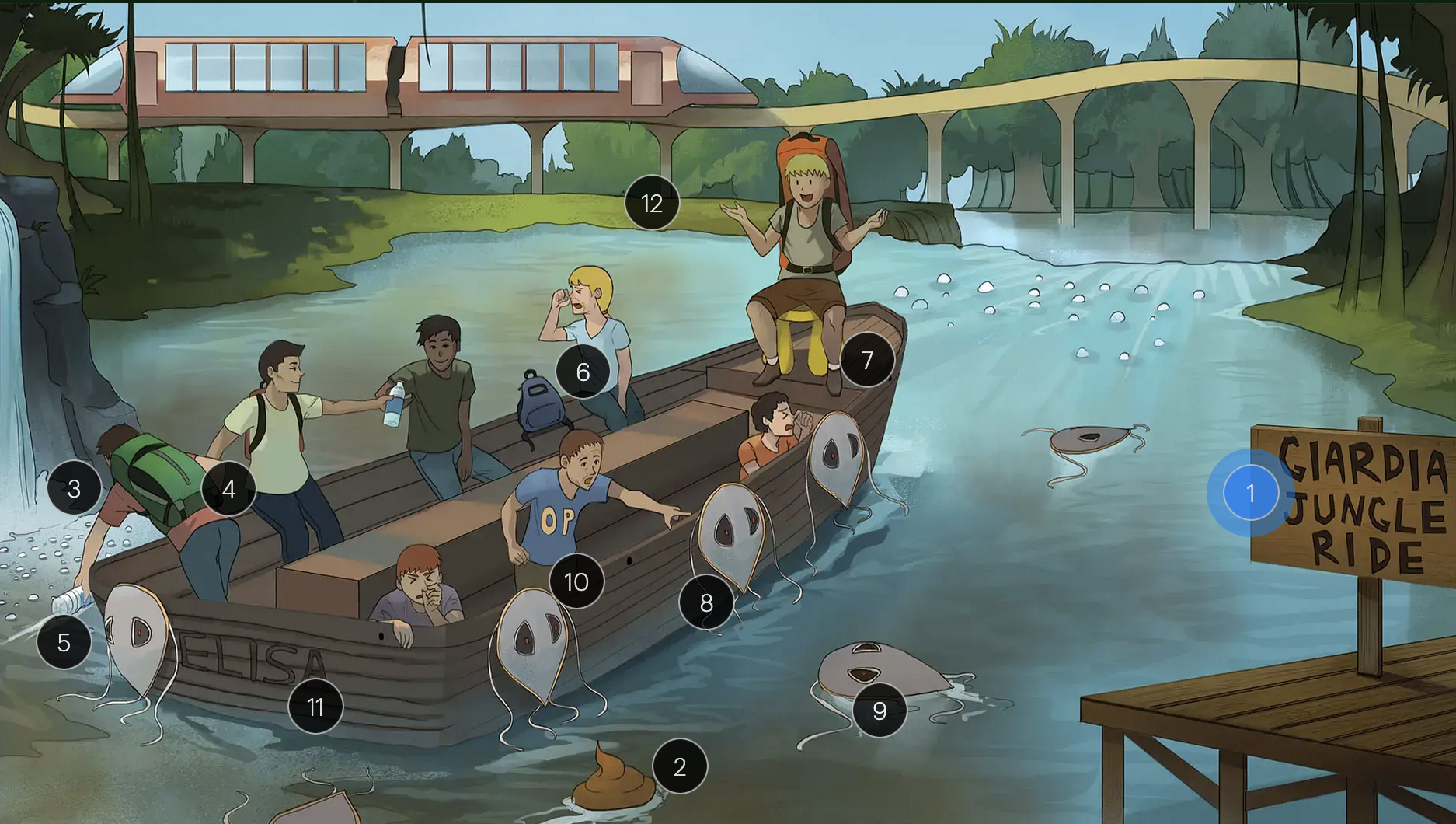
#1 “Giardia Jungle Ride”
Giardia intestinalis (an intestinal protozoan)
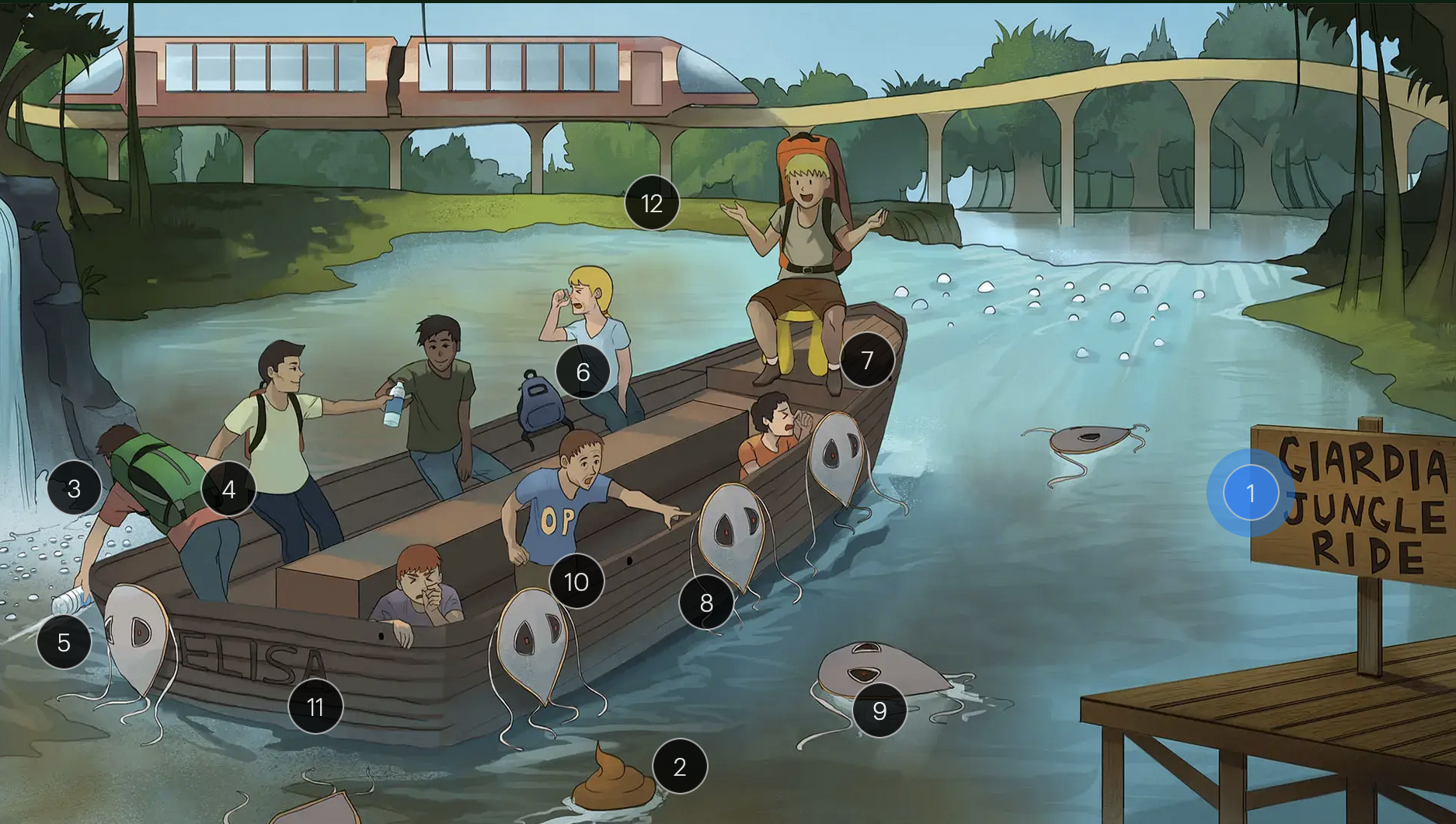
Giardia lamblia
#2 poopy water
cysts (the infectious stage of the parasite) are transmitted via the fecal-oral route, often through contaminated water or food

Giardia lamblia
#3 bubble in water
form of infectious cysts, which are shed in the feces of infected individuals, contaminating water and food sources
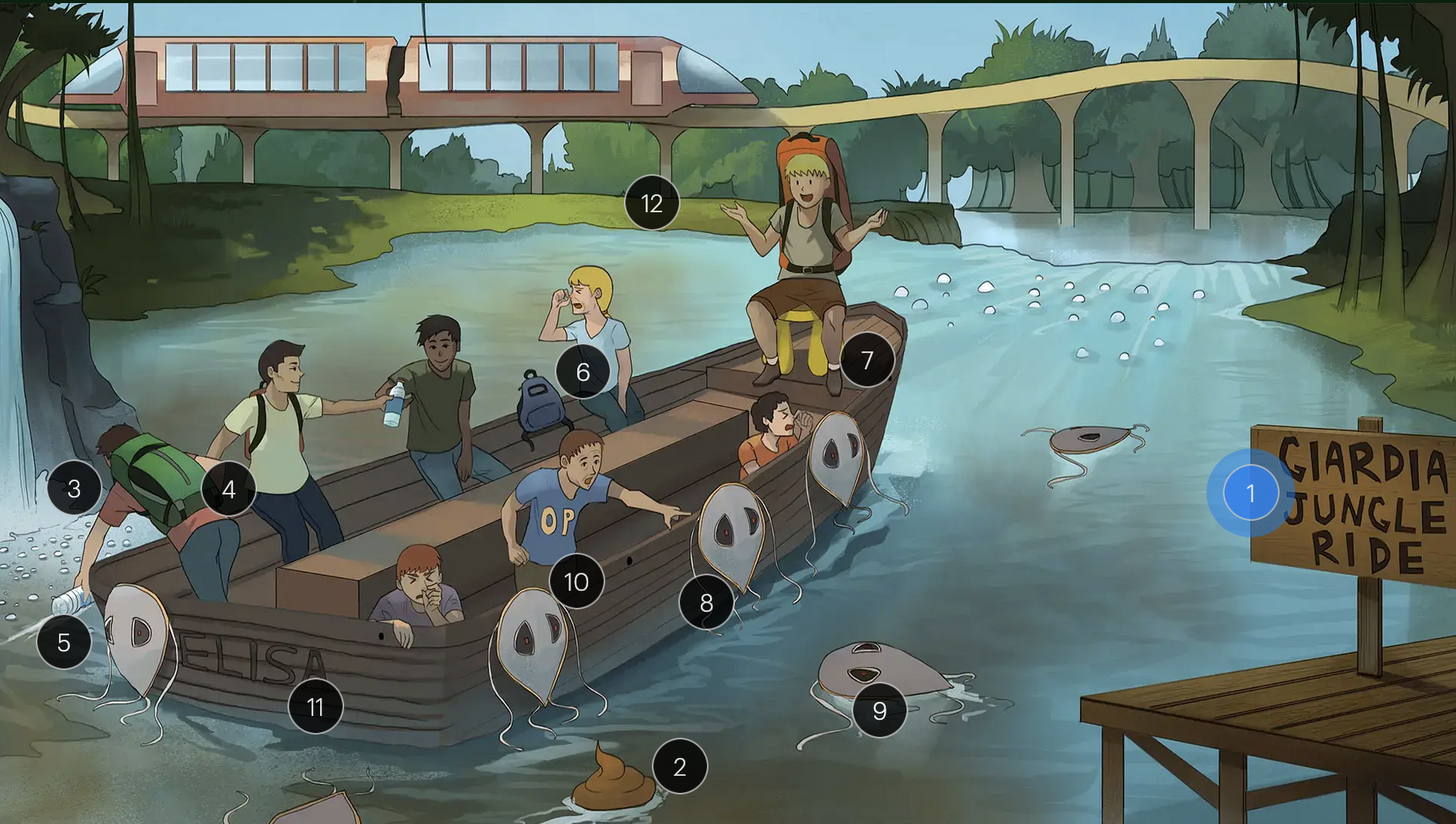
Giardia lamblia
#4 backpacks
giardiasis is a concern for individuals consuming water from natural sources, such as hikers and campers, due to the risk of ingesting contaminated water
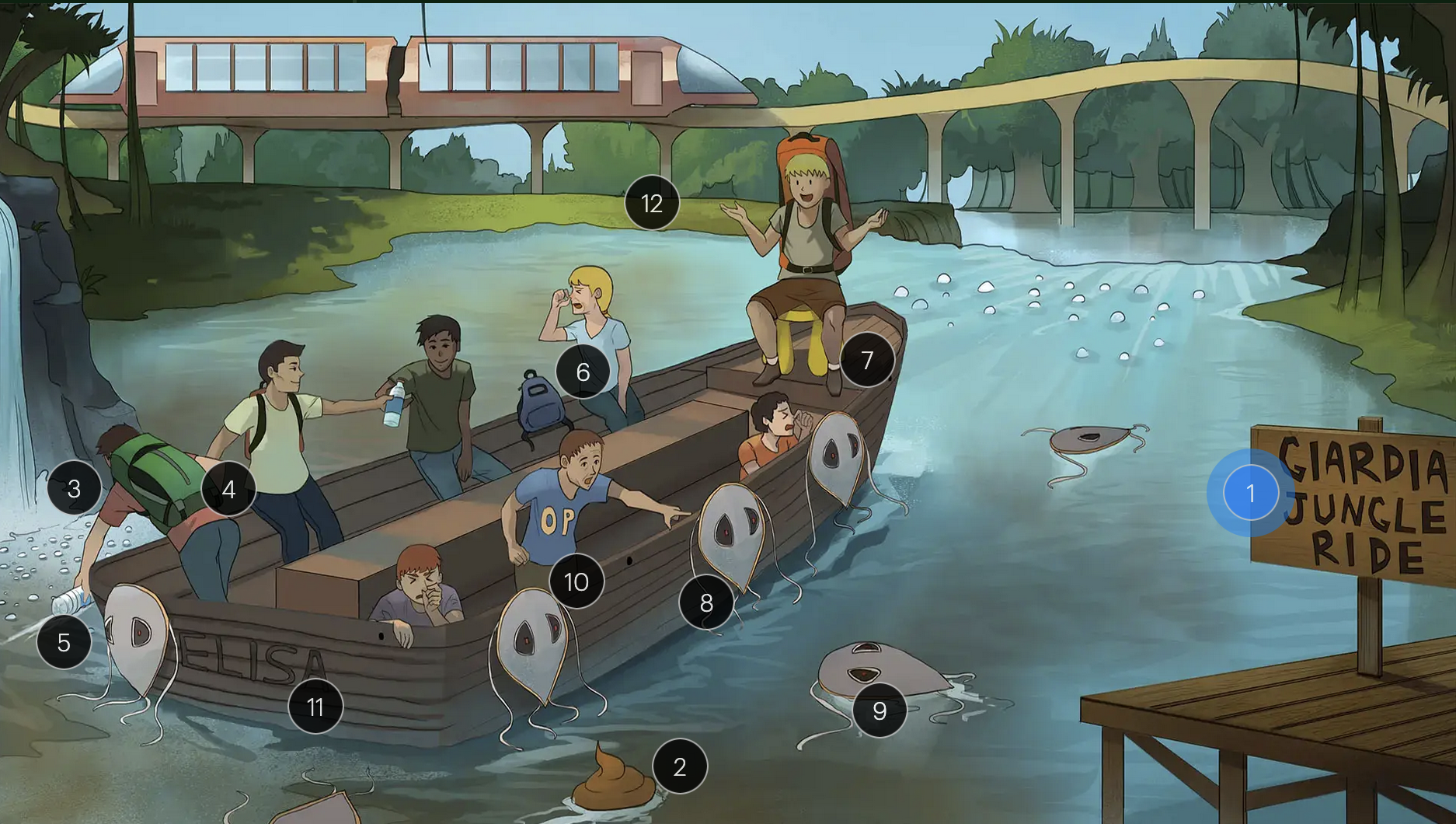
Giardia lamblia
#5 water bottle + poopy water
poorly purified or untreated water is a common vehicle for g. intestinalis transmission
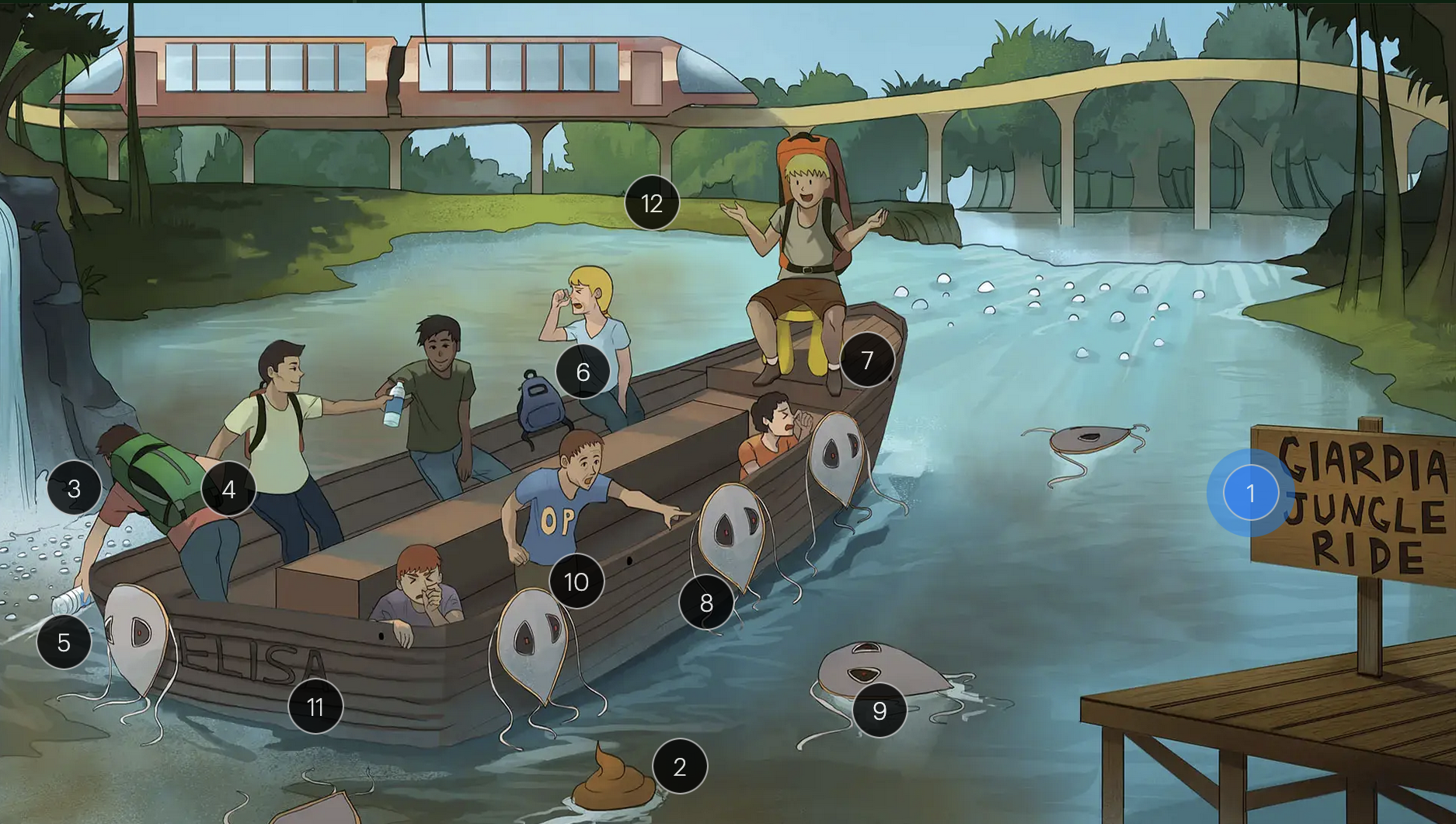
Giardia lamblia
#6 campers holding noses
the clinical presentation of giardiasis includes characterisic foul-smelling, greasy, non-bloody diarrhea
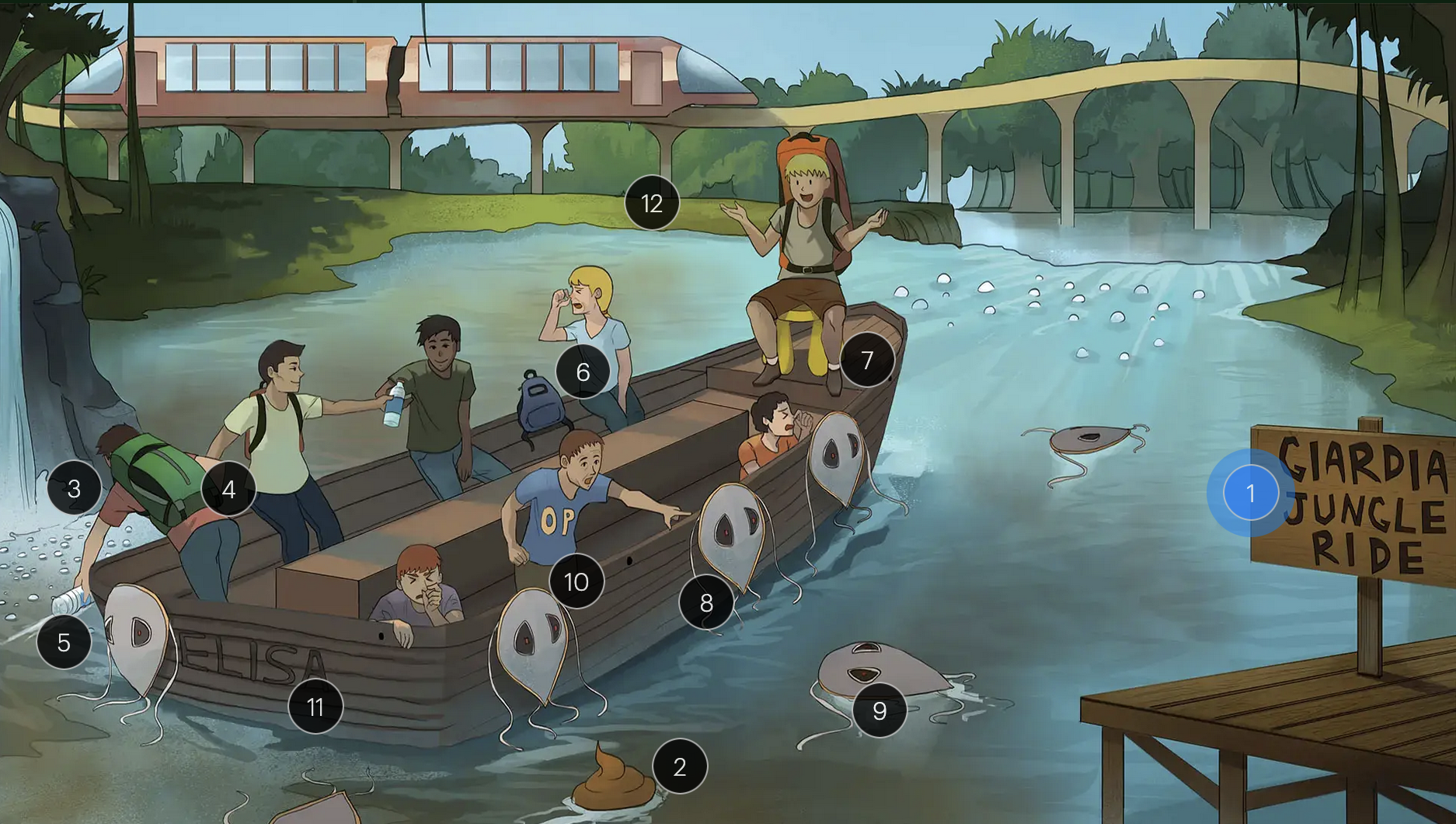
Giardia lamblia
#7 yellow stool
giardiasis may impair nutrient absorption, resulting in steatorrhea (excess fat in the stools), a manifestation of fat malabsorption
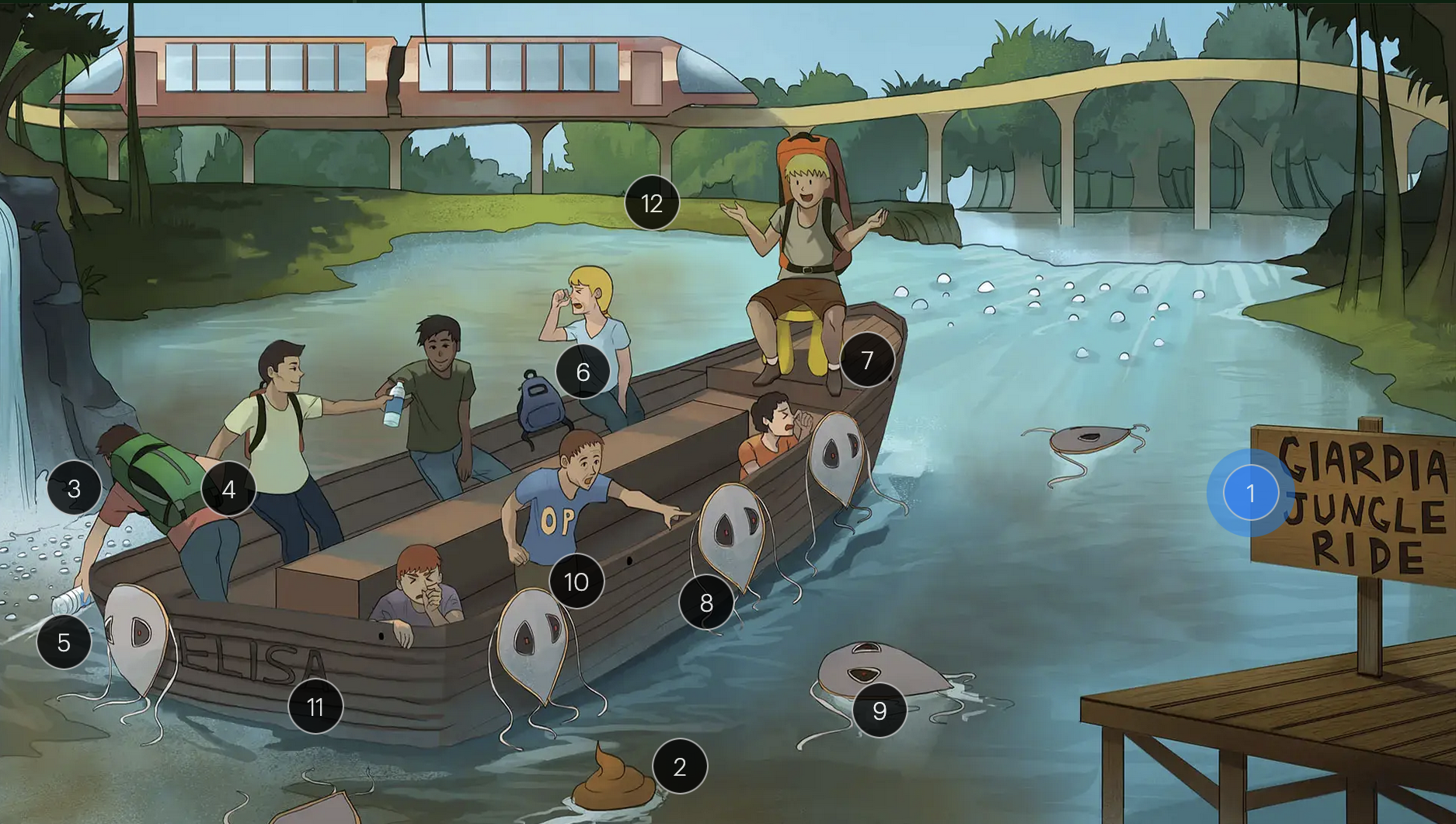
Giardia lamblia
#8 trophozoite shields
the flagellated trophozoites of g. intestinalis have a distinctive pear-shaped morphology
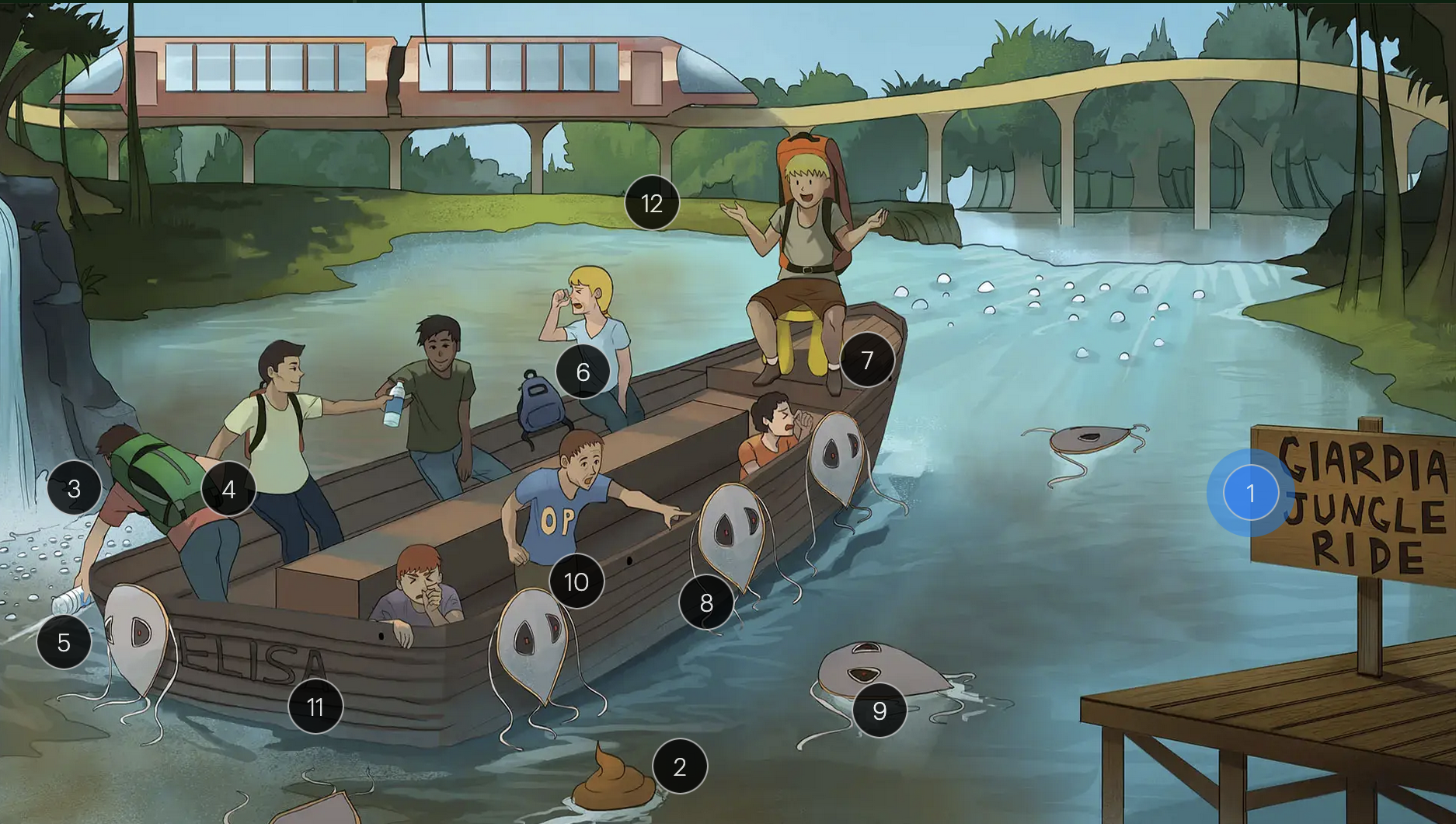
Giardia lamblia
#9 shields in water
detection of cyts or trophozites in stool specimines confirms dx
Giardia lamblia
#10 “O&P”
stool ova and parasite (O&P) examination and ELISA for antigens are reliable diagnostic methods for giardiasis
Giardia lamblia
#11 “ELISA” boat
stool ova and parasite (O&P) examination and ELISA for antigens are reliable diagnostic methods for giardiasis
Giardia lamblia
#12 metro
effective treatments of giardiasis include metronidazole, tinidazole, and nitazoxanide
Entamoeba histolytica
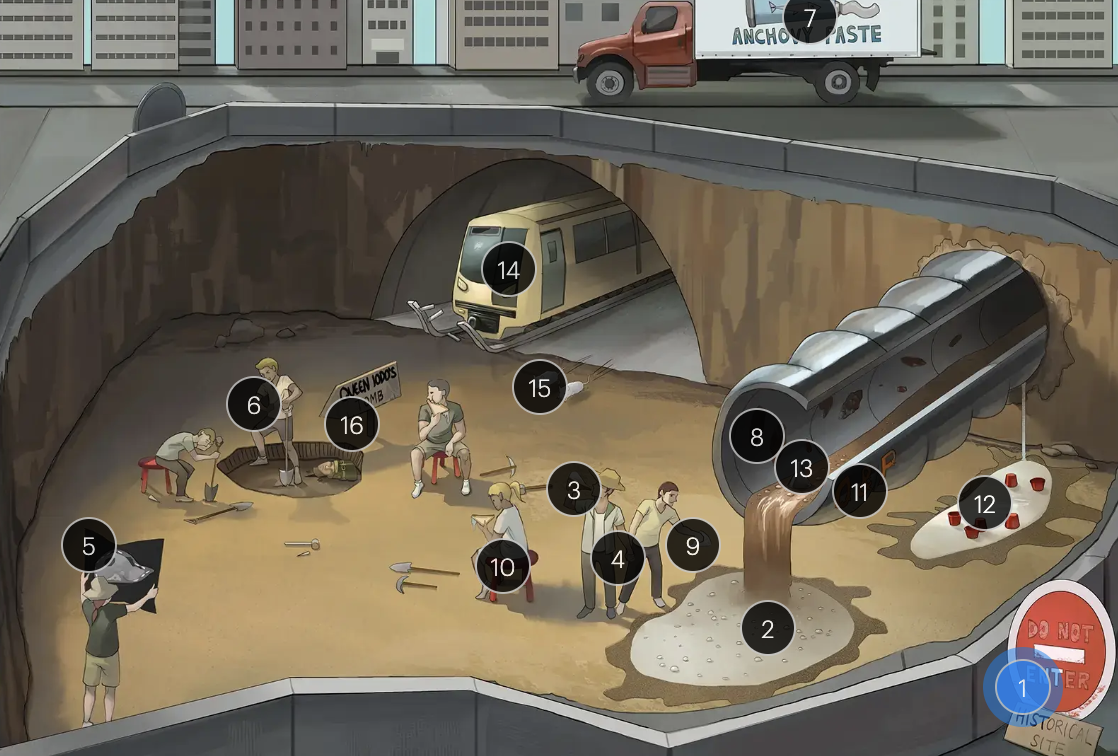
#1 “Do not ENTer - HISTorical site”
E. histolytica (an intestinal protozoan that causes amebiasis)
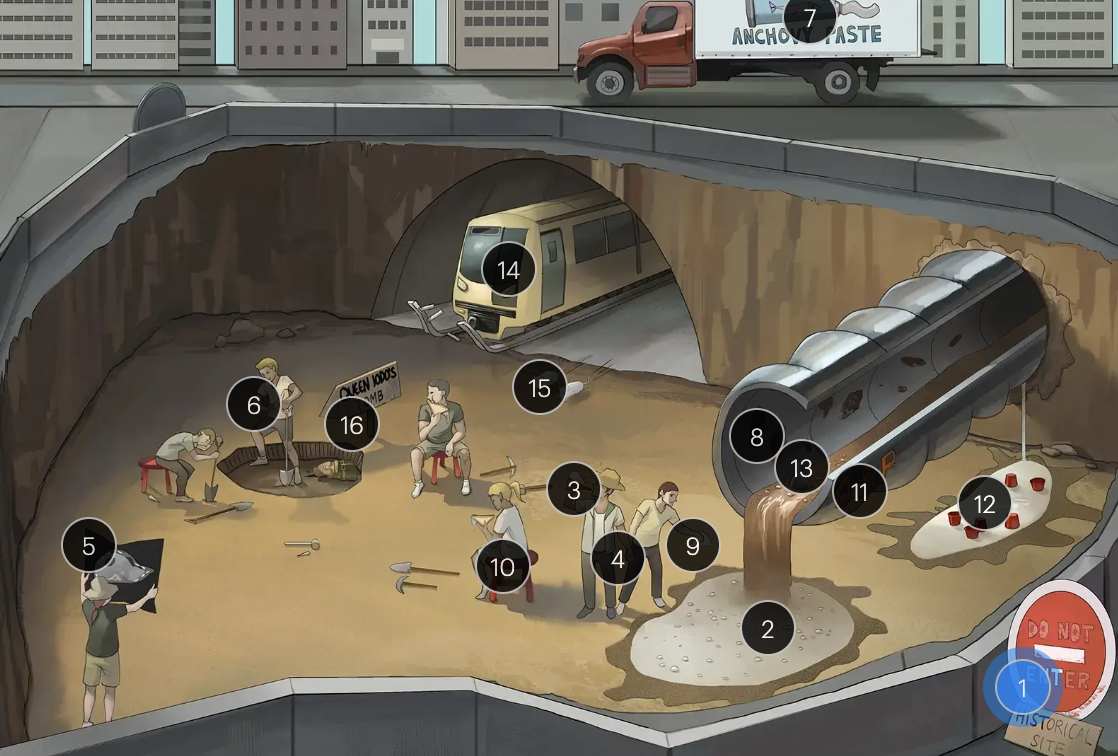
Entamoeba histolytica
#2 bubbles in water
forms infectious cysts that are passed through stool
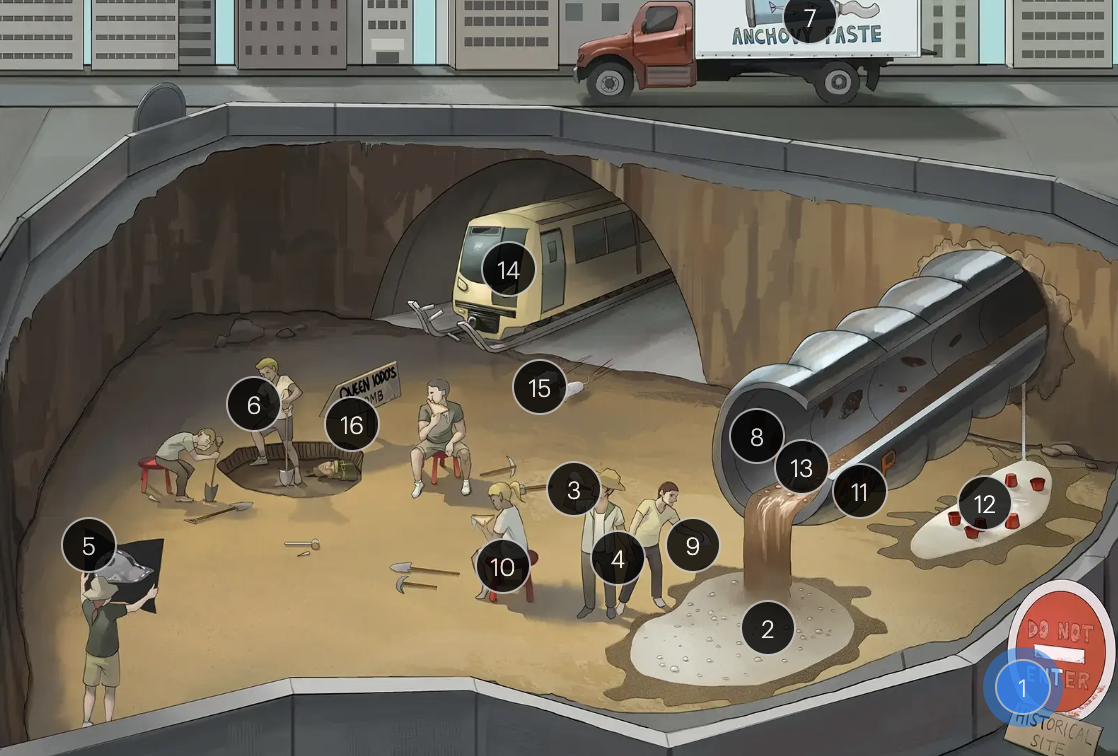
Entamoeba histolytica
#3 drinking bubbly water
amebiasis is primarily acquired through ingestion of food or water contaminated with E. histolytica cysts
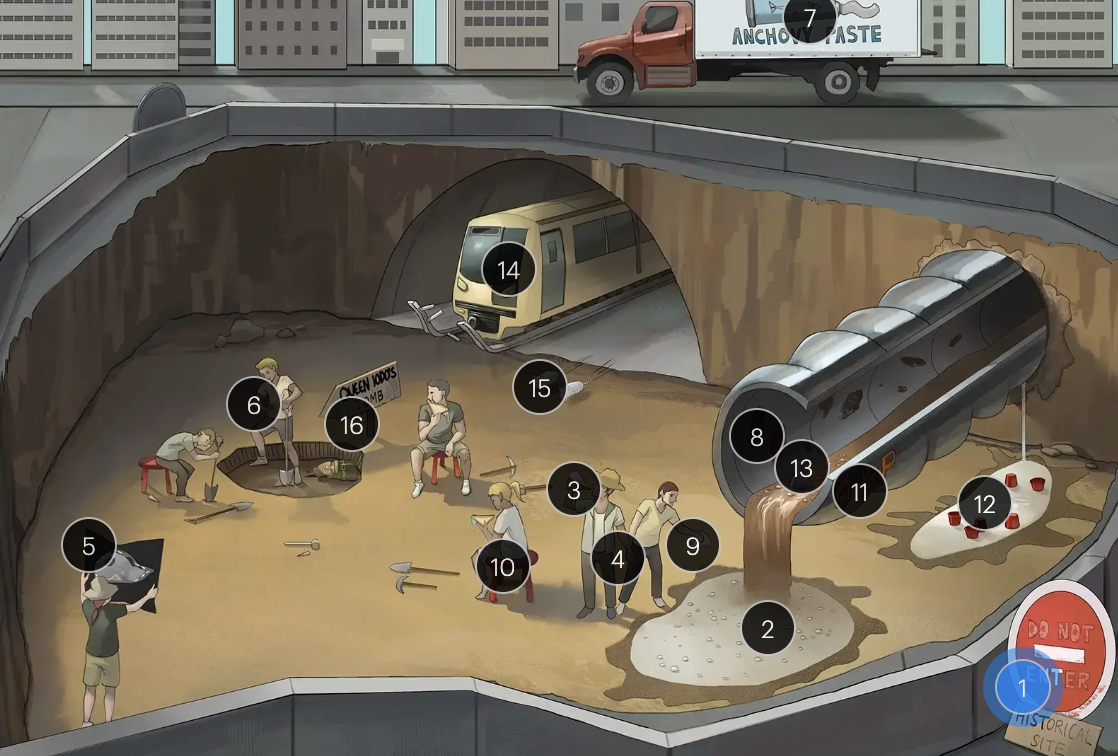
Entamoeba histolytica
#4 holding hands
can be transmitted via anal-oral sexual contact
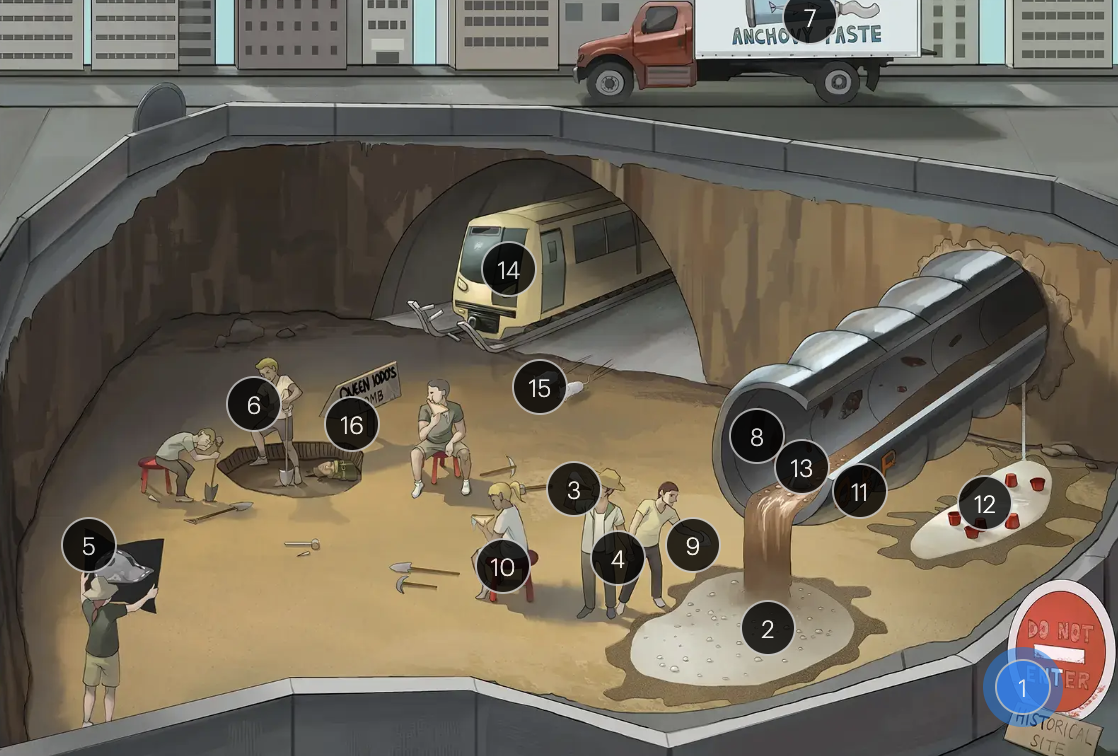
Entamoeba histolytica
#5 R lobe liver dig site
the most common extraintestinal manifestation of amebiasis is liver abscess, typically occurring in the R hepatic lobe
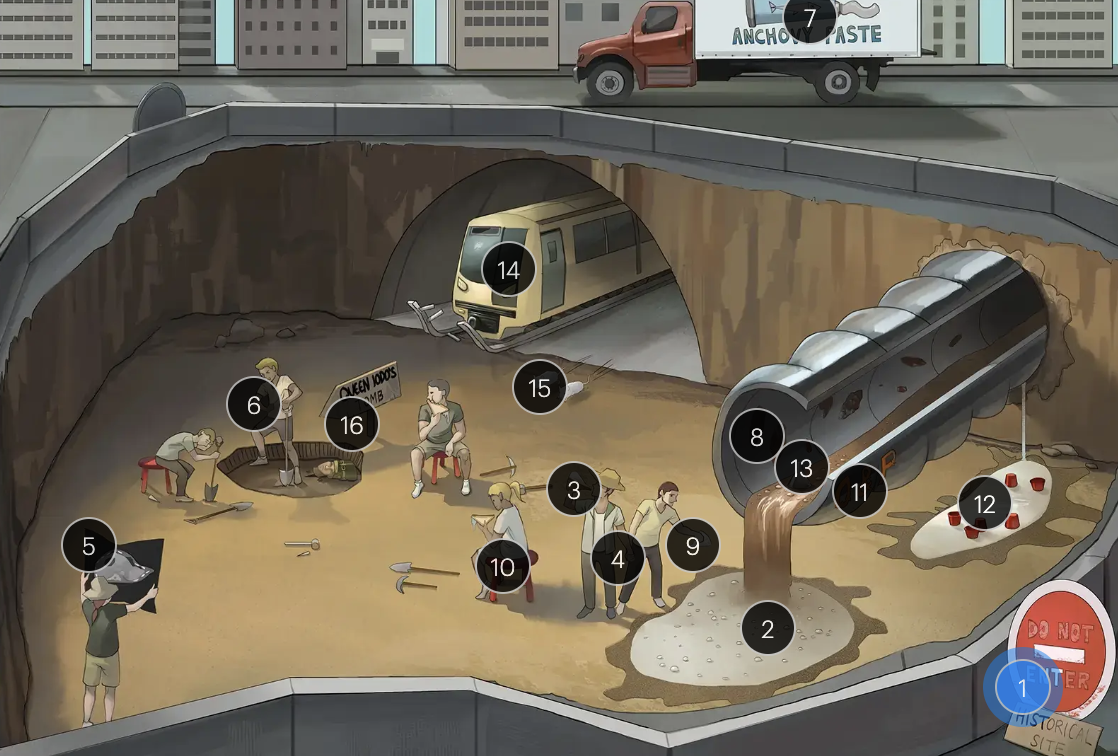
Entamoeba histolytica
#6 clutching right side
clinical presentation of hepatic amebiasis often includes RUQ pain, fever, and hepatomegaly
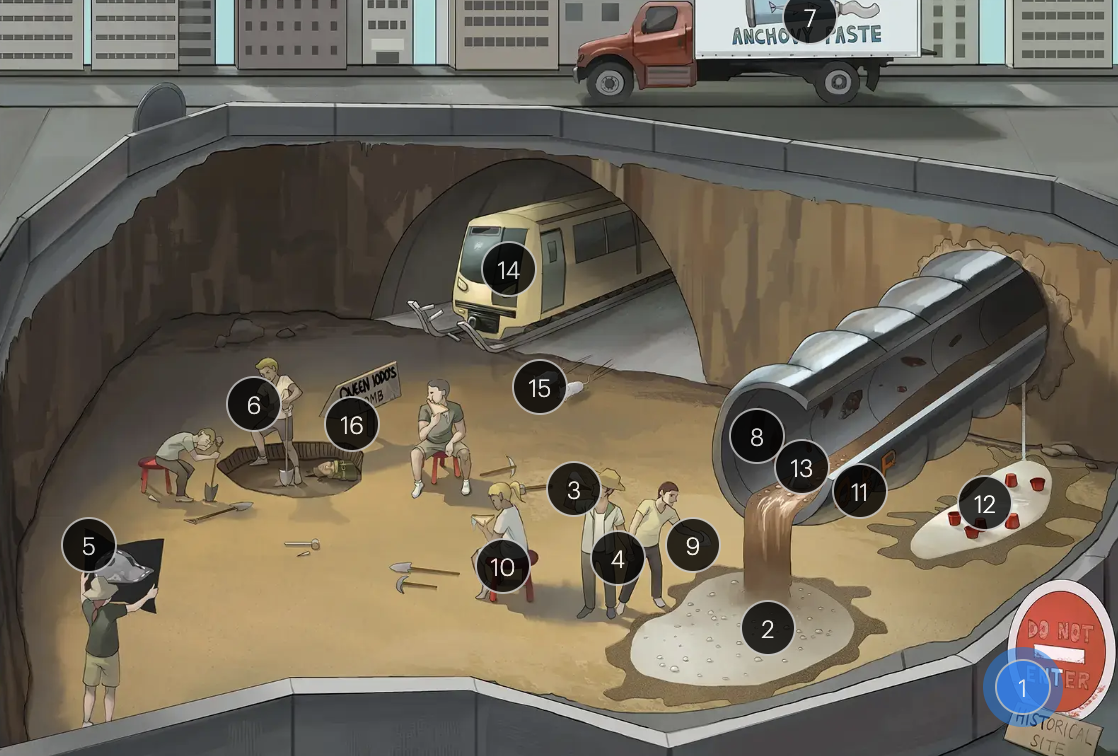
Entamoeba histolytica
#7 anchovy paste truck
aspirates from amebic liver abscesses often have a characteristic “anchovy paste” appearance
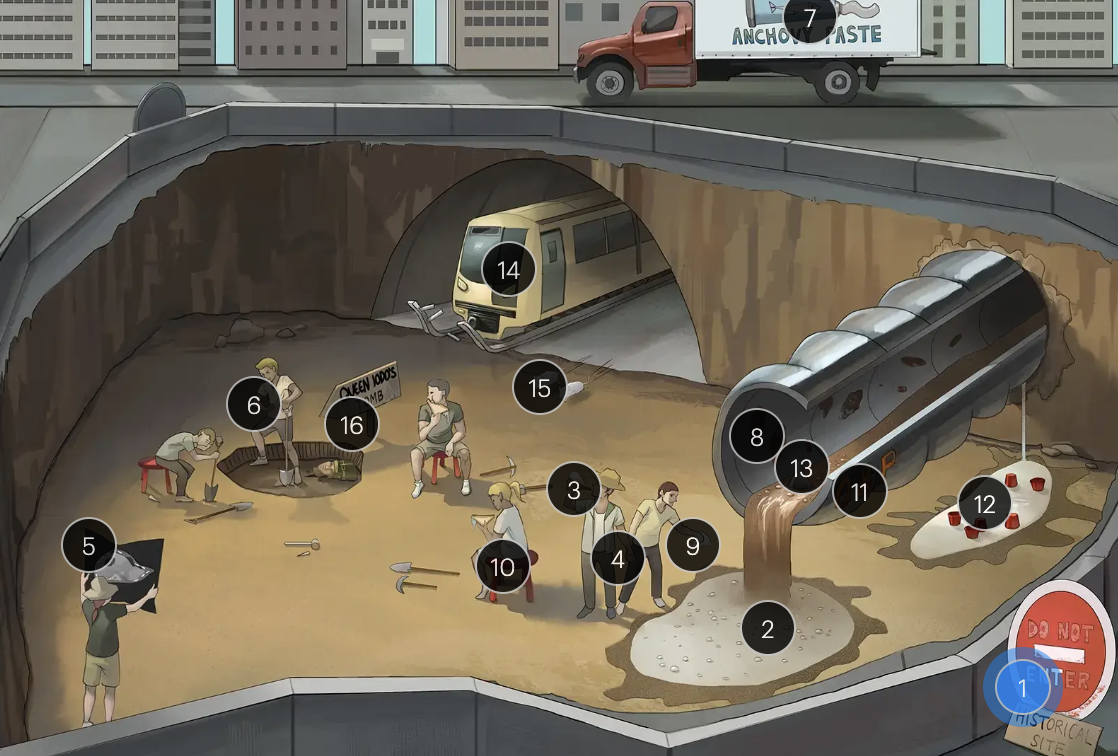
Entamoeba histolytica
#8 colon drainage pipe with rust spots
flask-shaped ulcerations in the colon is a characteristic finding in intestinal amebiasis

Entamoeba histolytica
#9 flask water bottles
the presence of flask-shaped ulcers is a hallmark of invasive amebiasis, observable through histopathological examination
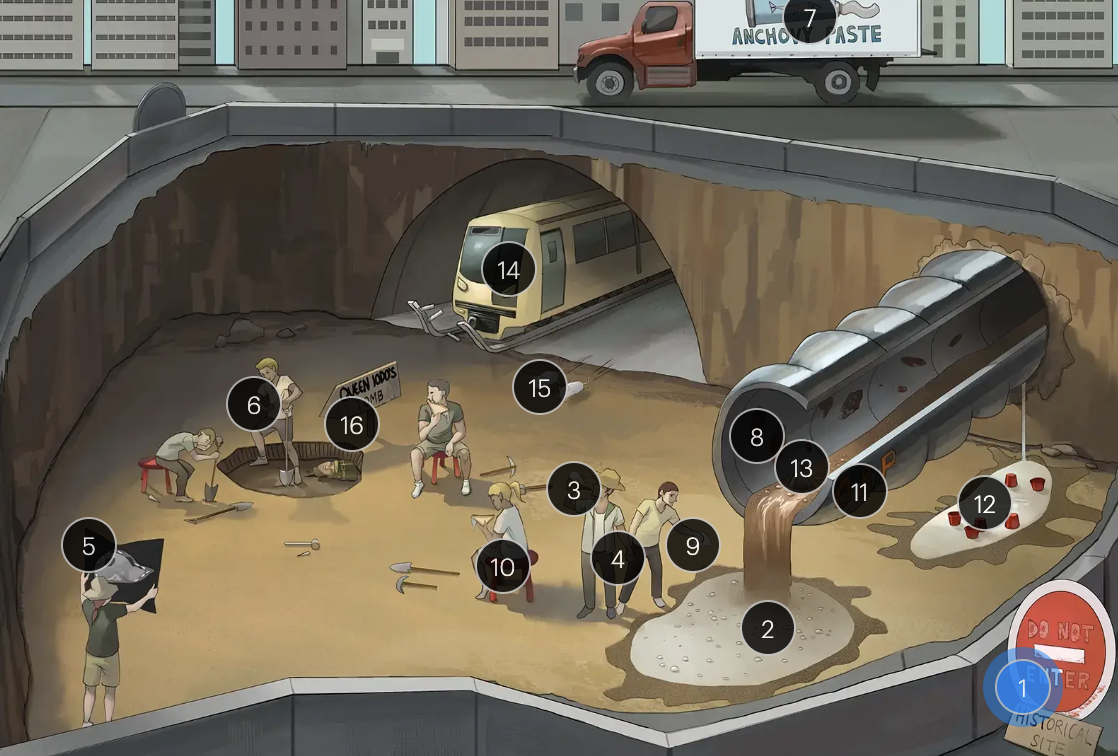
Entamoeba histolytica
#10 red stools
bloody diarrhea in amebiasis is a result of ulceration in the intestinal mucosa
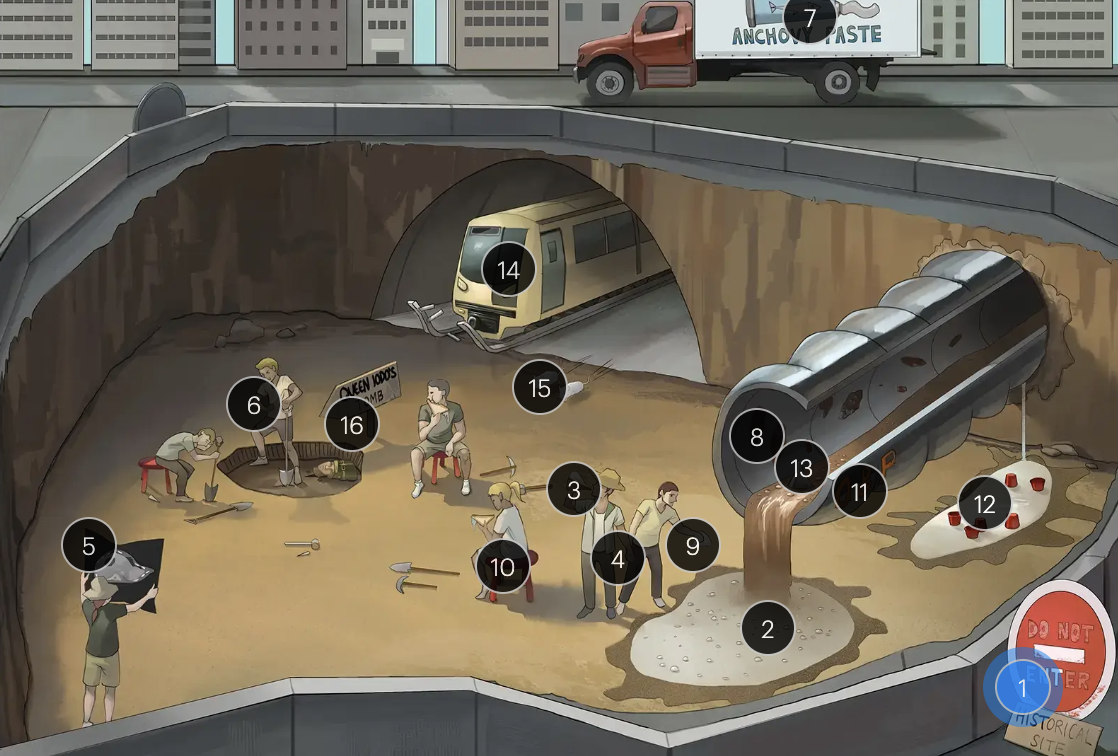
Entamoeba histolytica
#11 “O&P” pipe
Diagnosis of infection can be confirmed by identifying E. histolytica cysts or trophozoites in stool samples using O&P examination
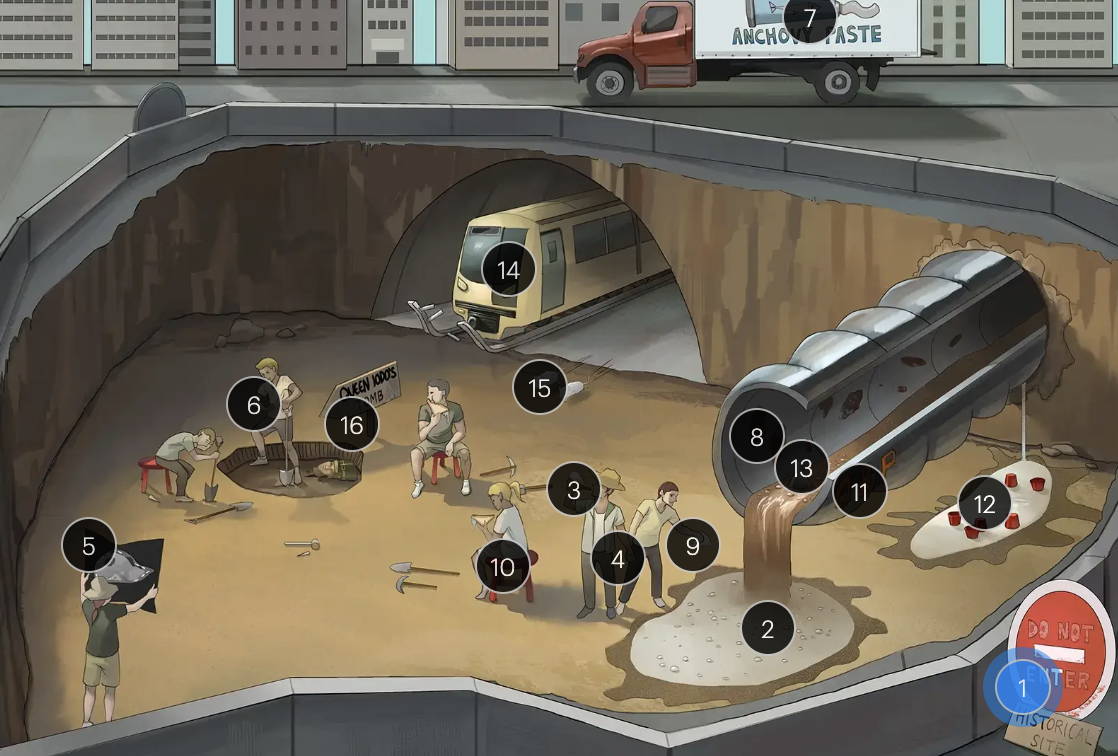
Entamoeba histolytica
#12 trophozoite puddle + red cups
the presence of E. hystolytica trophozoites containing ingested RBCs in stool or tissue samples is diagnostic of invasive amebiasis
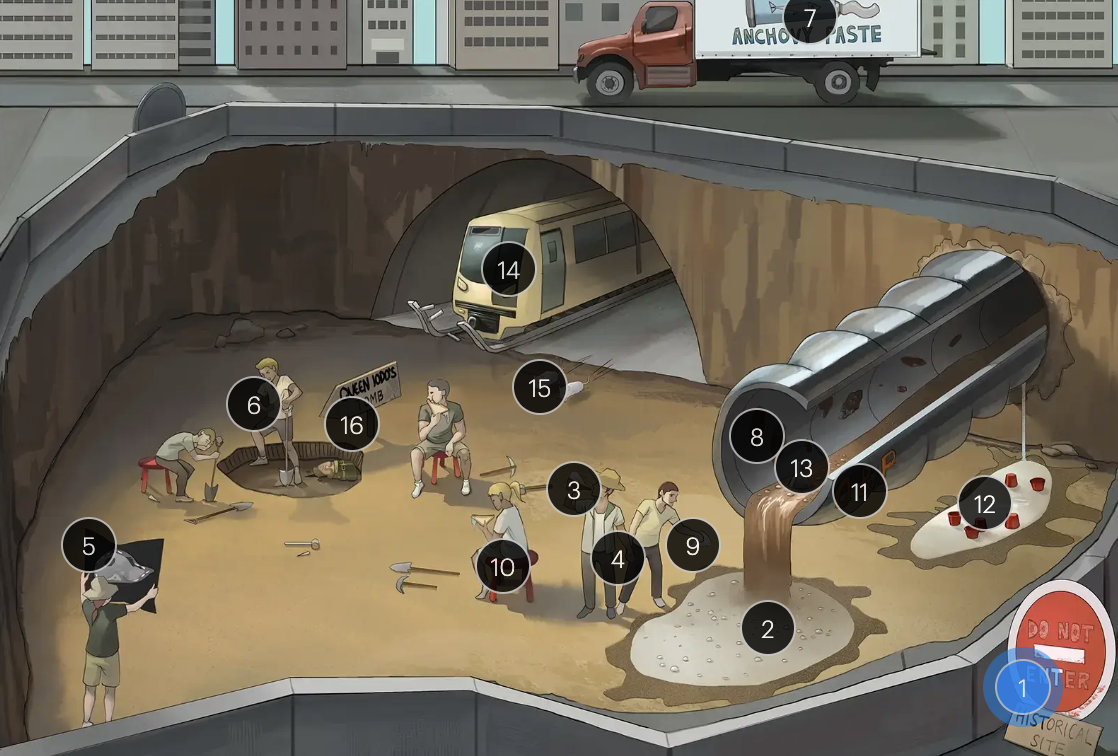
Entamoeba histolytica
#13 flask in colon pipe
intestinal biopsy may show flask-shaped lesions in intestinal amebiasis
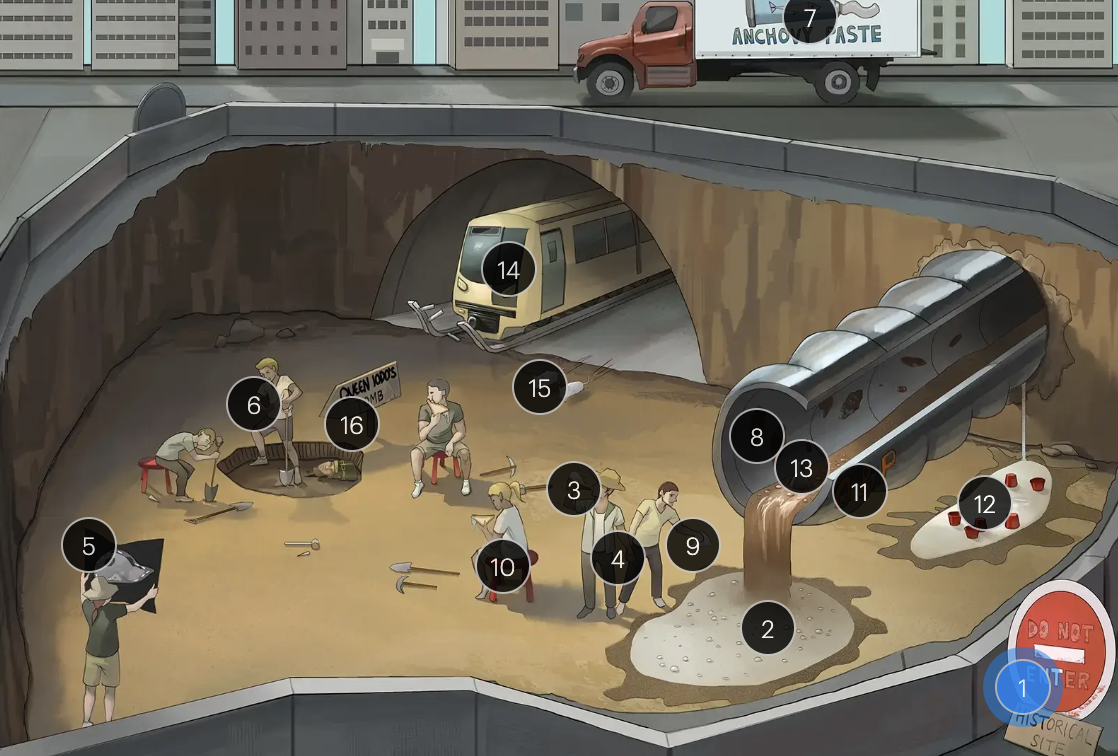
Entamoeba histolytica
#14 Metro
metronidazole is part of the primary treatment for amebiasis, targeting trophozoites

Entamoeba histolytica
#15 pair of mice
Paromycin and iodoquinol are luminal agents used to eradicate residual E. histolytica cysts from the intestinal lumen after treatment with metronitazole or tinidazole
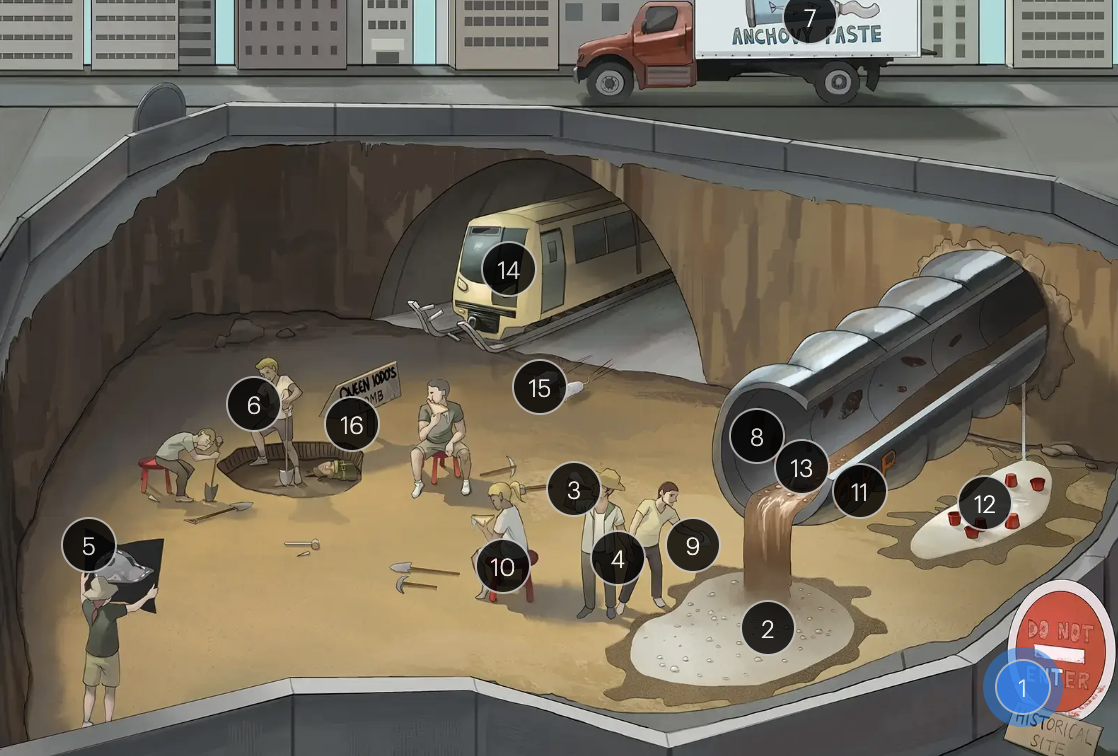
Entamoeba histolytica
#16 “Queen Iodo’s Tomb”
Paromycin and iodoquinol are luminal agents used to eradicate residual E. histolytica cysts from the intestinal lumen after treatment with metronitazole or tinidazole

Cryptosporidium spp.
#1 flooded crypt
cryptosporidium spp. (intestinal protozoa)

Cryptosporidium spp.
#2 immunocompromised cane
cryptosporidiosis is a significant cause of diarrheal illness, particularly in HIV-positive individuals with advanced immunosupression

Cryptosporidium spp.
#3 diarrhea water
in immunocompromised hosts, cryptosporidiosis may manifest as severe, chronic, and watery diarrhea

Cryptosporidium spp.
#4 pink-acid fast poncho
the oocyst walls are acid-fast or partially acid-fast

Cryptosporidium spp.
#5 bubbles
these protozoa form infectious oocysts that are passed through stool

Cryptosporidium spp.
#6 multifaceted amethyst gems
the oocysts are composed of 4 motile sporozoites

Cryptosporidium spp.
#7 broken pipe
upon ingestion, sporozoites invade the epithelial cells of the small intestine, leading to diarrheal illness through direct cellular damage

Cryptosporidium spp.
#8 knitted sock
nitazoxanide is approved for treating cryptosporidiosis in immunocompetent individuals and may offer some benefit in immunocompromised patients, though efficacy is variable

Cryptosporidium spp.
#9 sock filter
effective filtration of drinking water is crucial for removing oocysts, preventing infection

Cryptosporidium spp.
#10 spirit crows
spiramycin, a macrolide antibiotic, may be useful for alleviating cryptosporidial diarrhea in some immunocompromised patients

Toxoplasma gondii
#1 gandhi cat
toxoplasma gondii (a CNS protozoan)
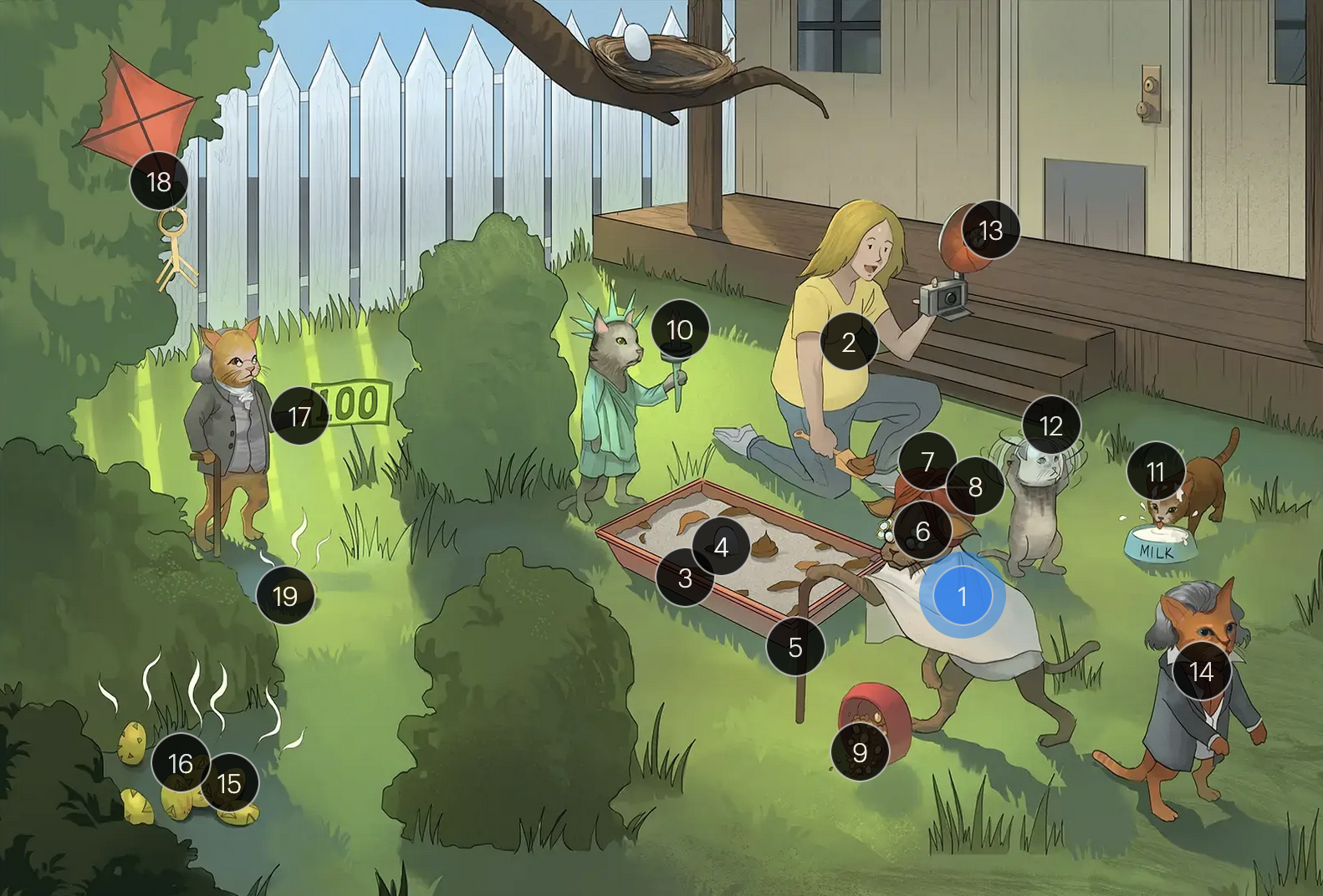
Toxoplasma gondii
#2 pregnant woman
it is considered a TORCHeS infection (“T”) as it can be transmitted transplacentally, leading to congenital infection
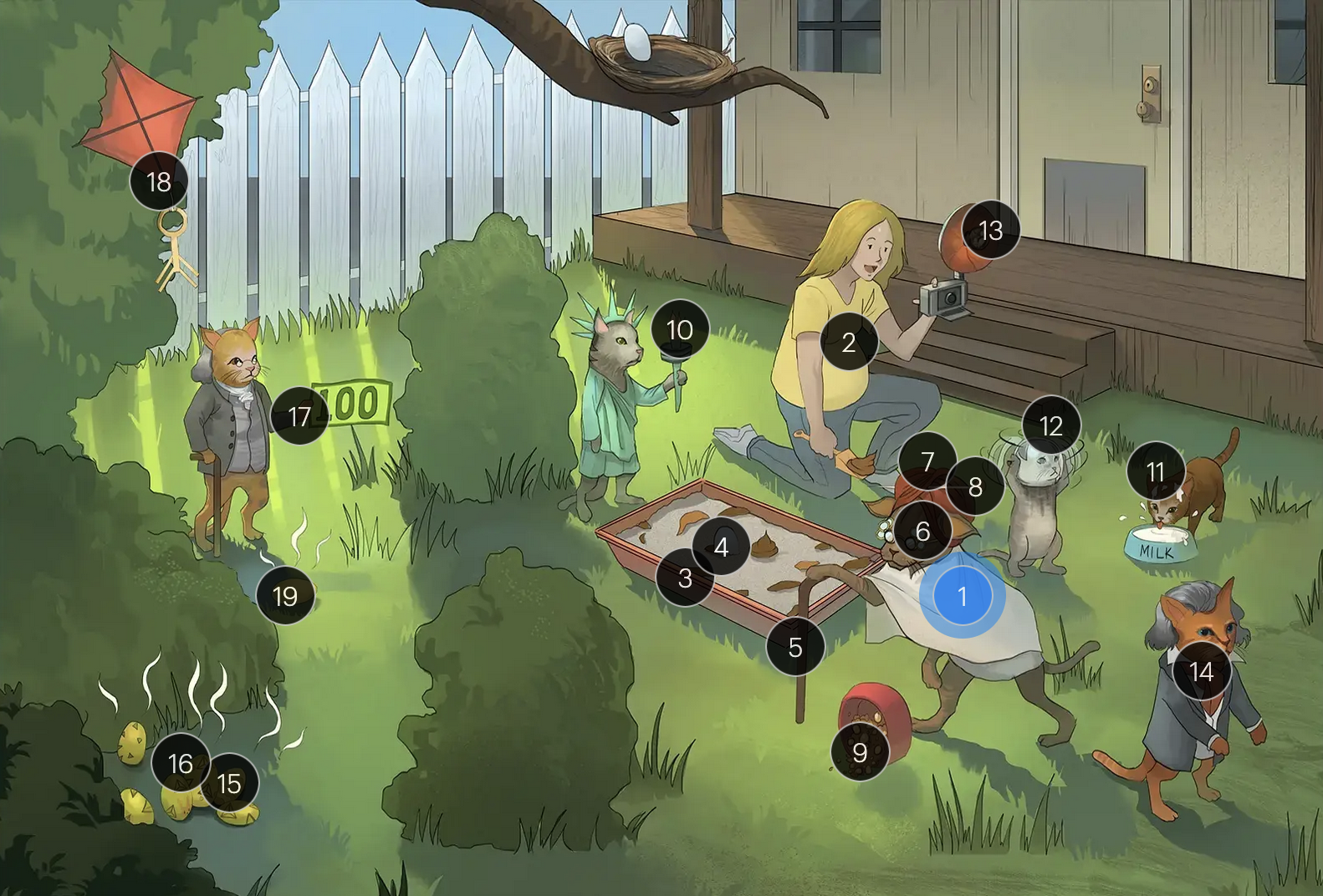
Toxoplasma gondii
#3 litter box
cats are the definitive hosts, and humans are at risk of infection through exposure to oocyst-contaminated cat feces
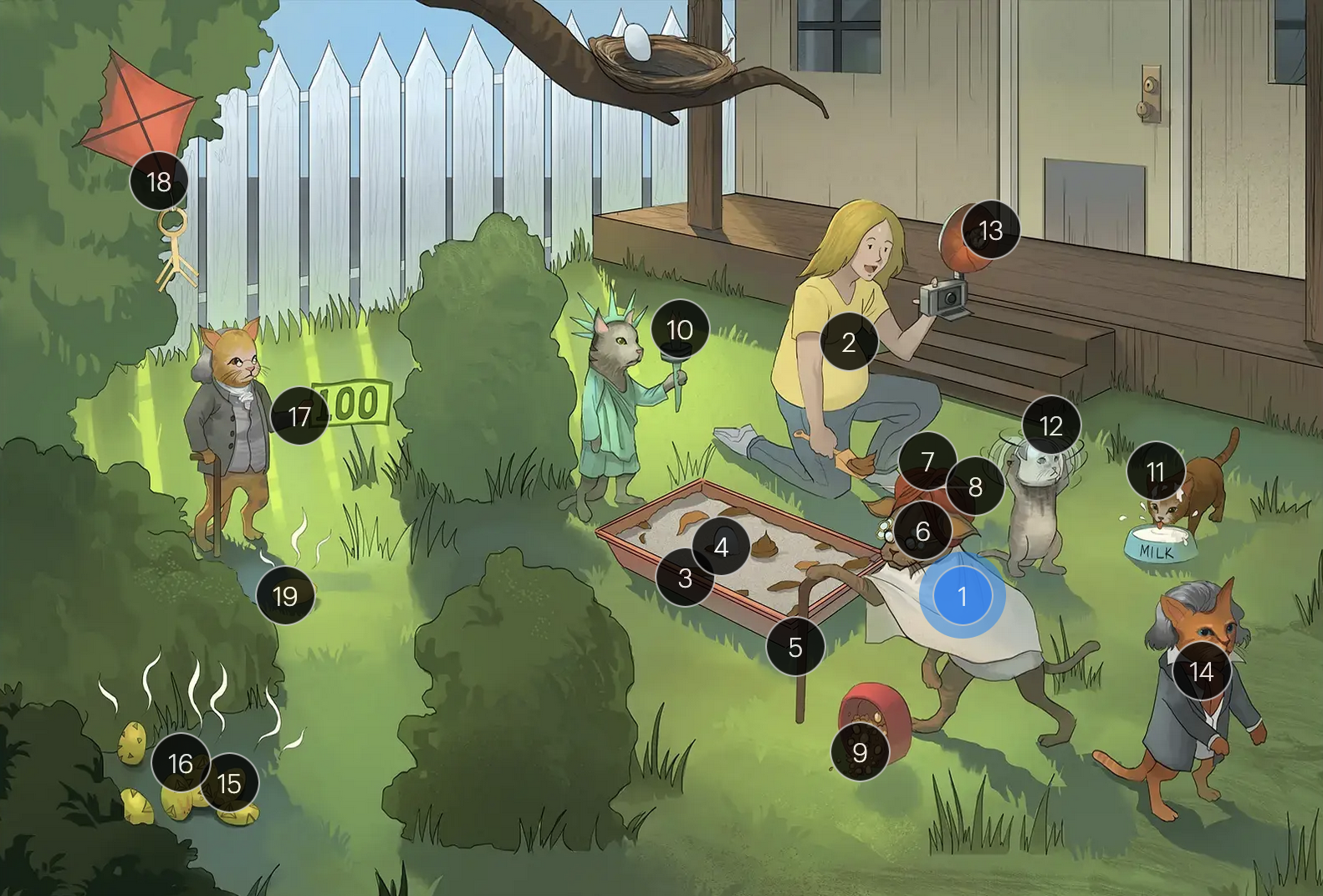
Toxoplasma gondii
#4 egg in litter box
oocysts are shed in cat feces and con contaiminate soil, water, or food
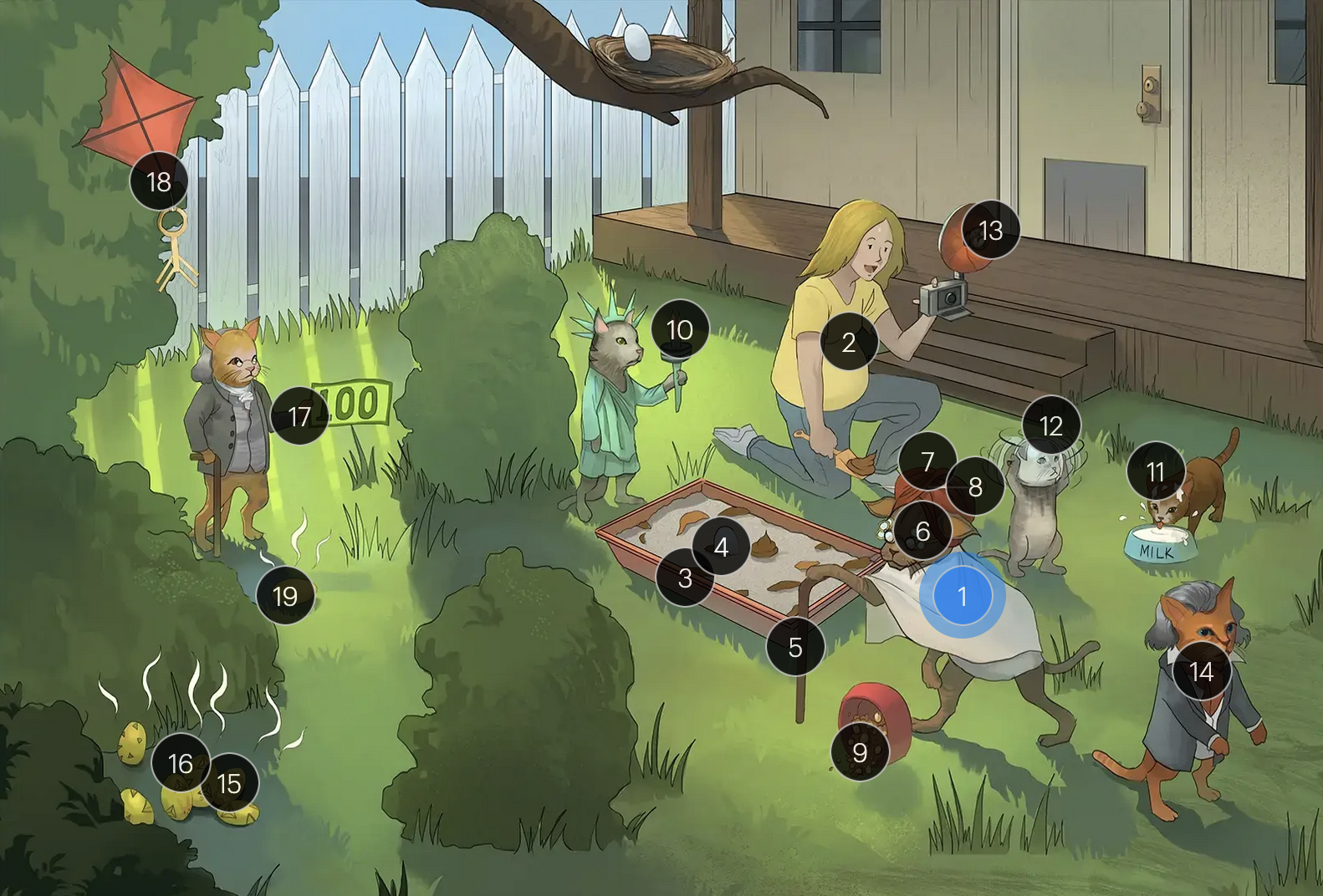
Toxoplasma gondii
#5 immunocompromised cane
individuals with compromised immune systems, particularly those with HIV/AIDS, are susceptible to severe toxoplasmosis
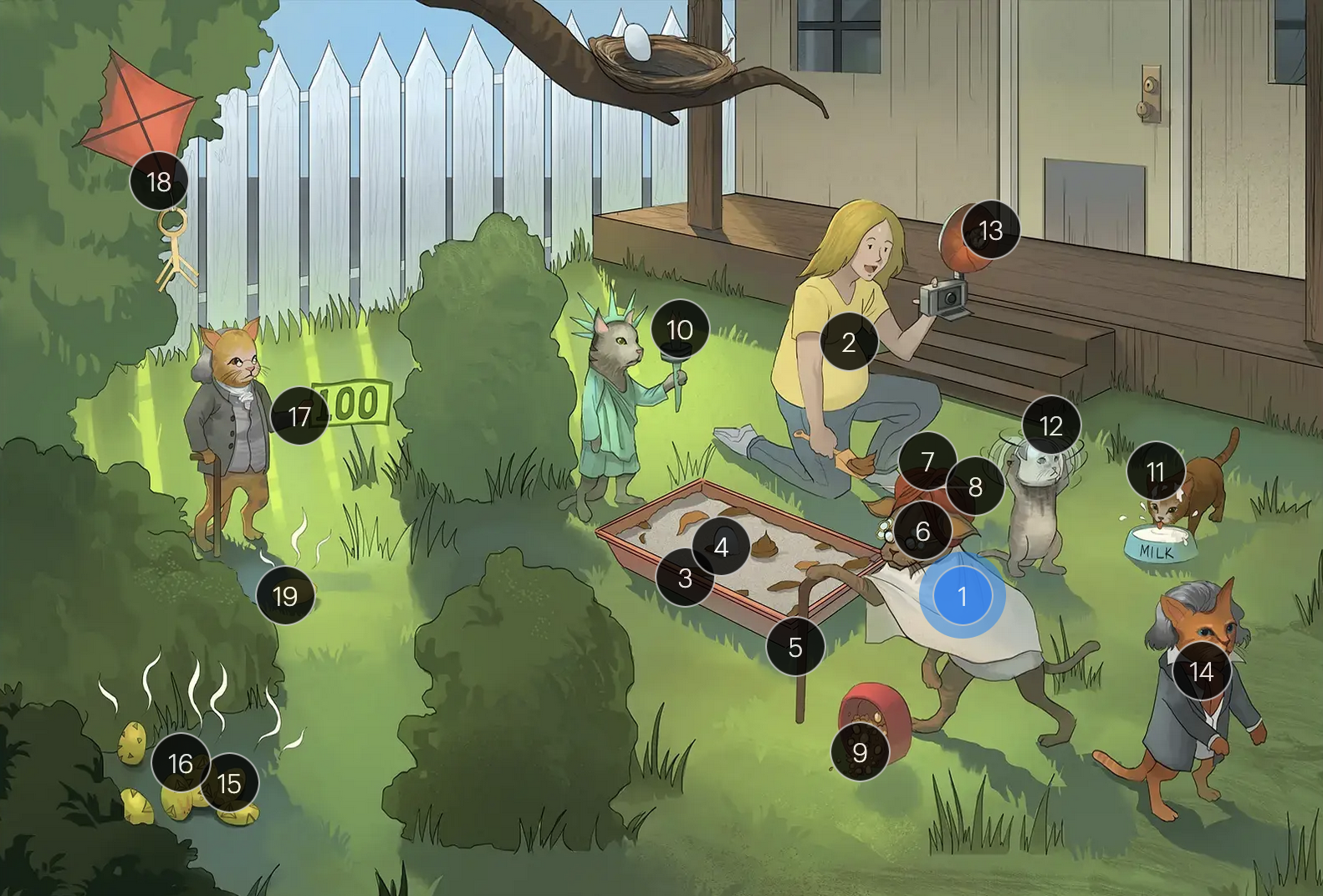
Toxoplasma gondii
#6 ring-shaped glasses
cerebral toxoplasmosis can manifest as multiple ring-enhancing lesions on neuroimaging, especially in immunocompromised individuals
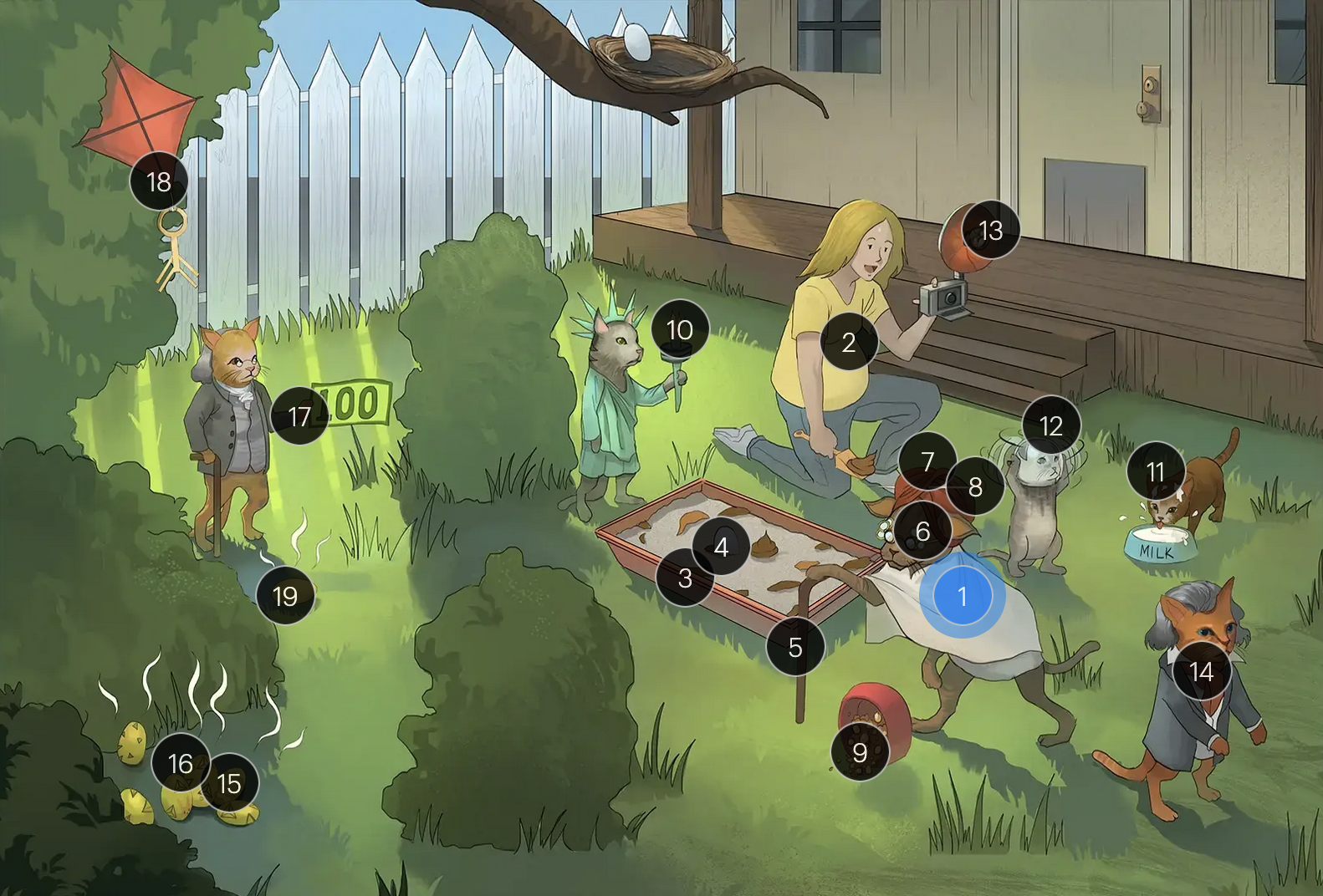
Toxoplasma gondii
#7 red turban
toxoplasmic encephalitis is a common complication of toxoplasmosis in severely immunocompromised individuals
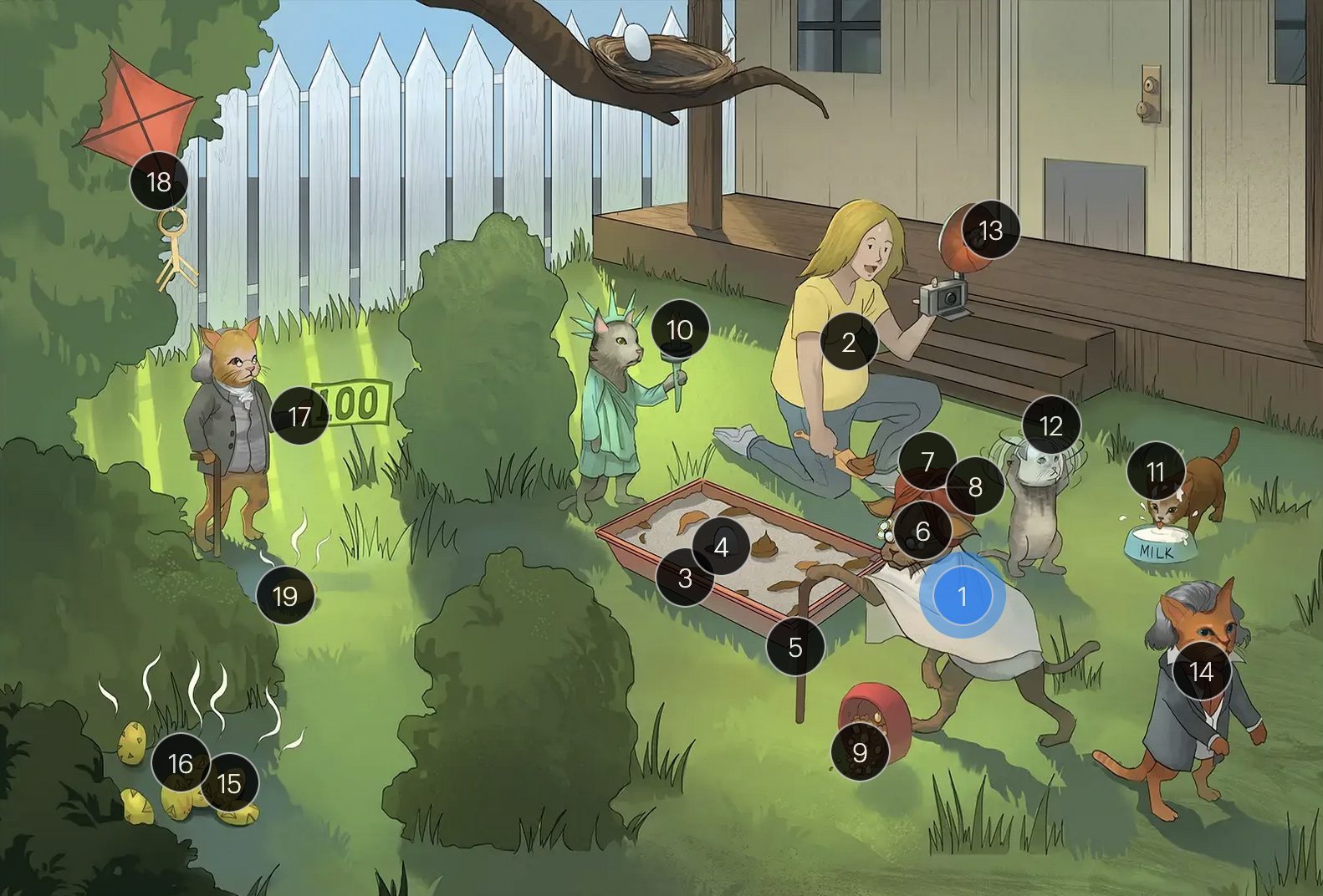
Toxoplasma gondii
#8 turban pin
brain biopsy may be utilized to distinguish between cerebral toxo and CNS lymphoma
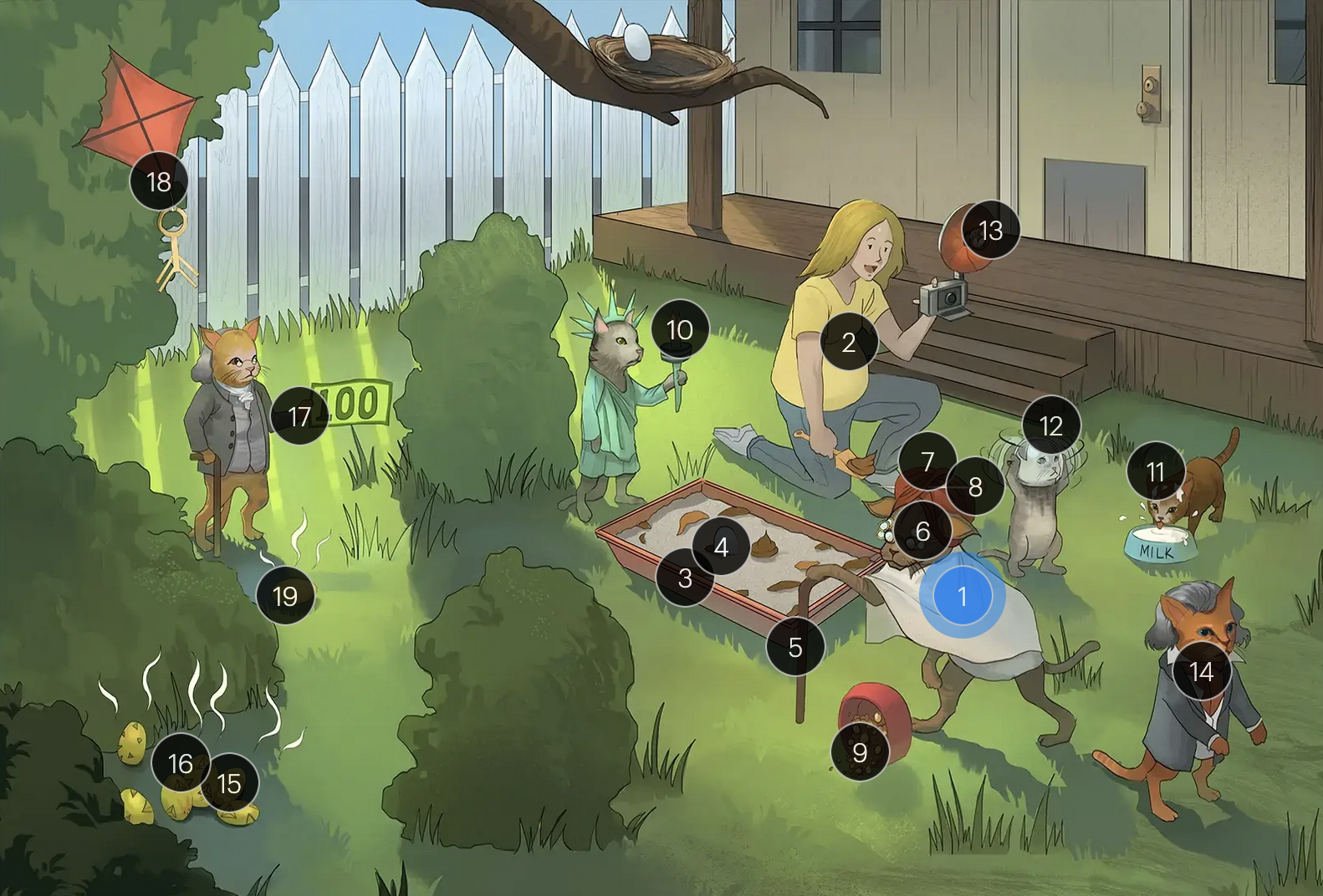
Toxoplasma gondii
#9 meaty cat food
ingestion of undercooked or raw meat containing toxo cysts is a common mode of human infection
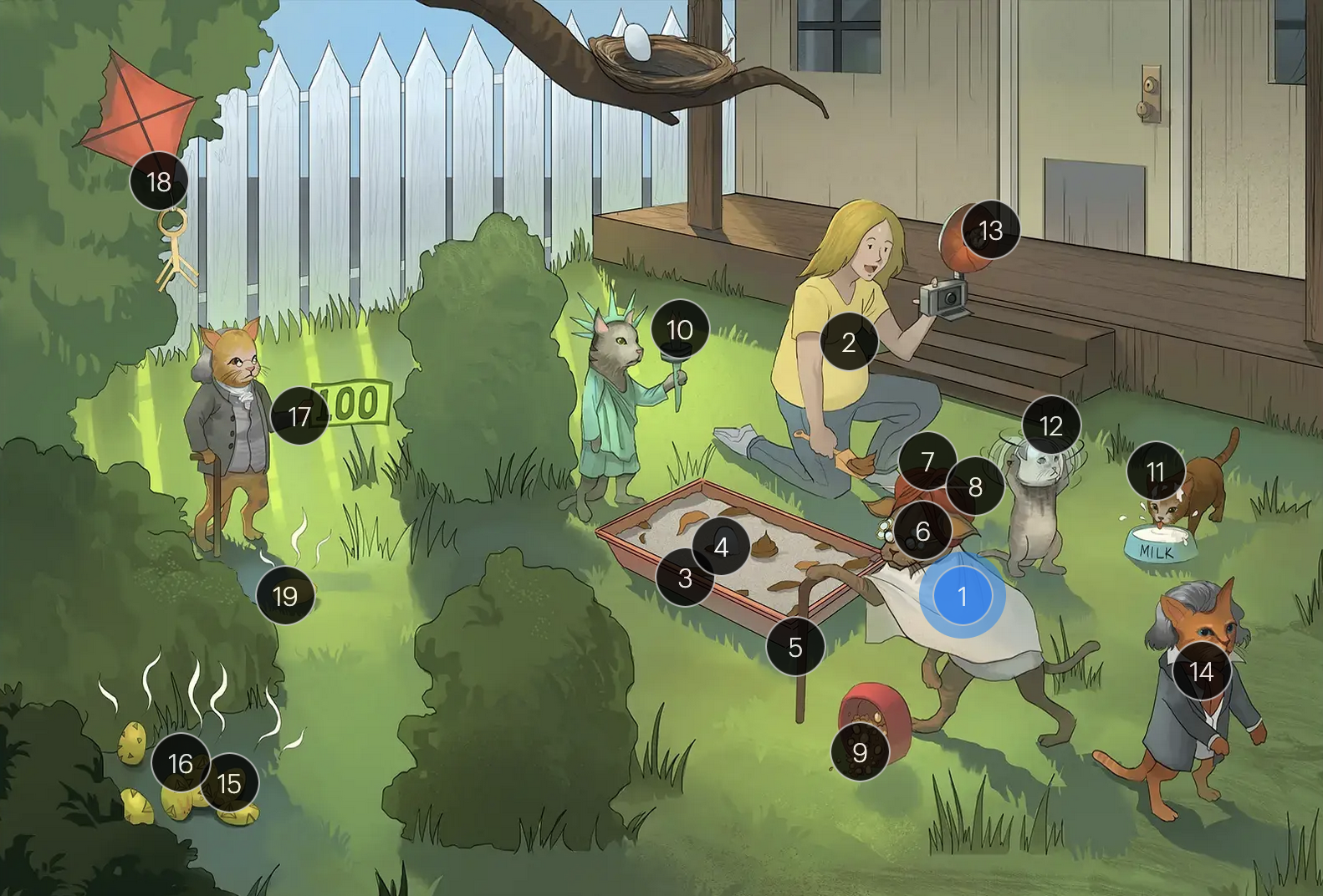
Toxoplasma gondii
#10 torch
it is considered a TORCHeS infection (“T”) as it can be transmitted transplacentally, leading to congenital infection
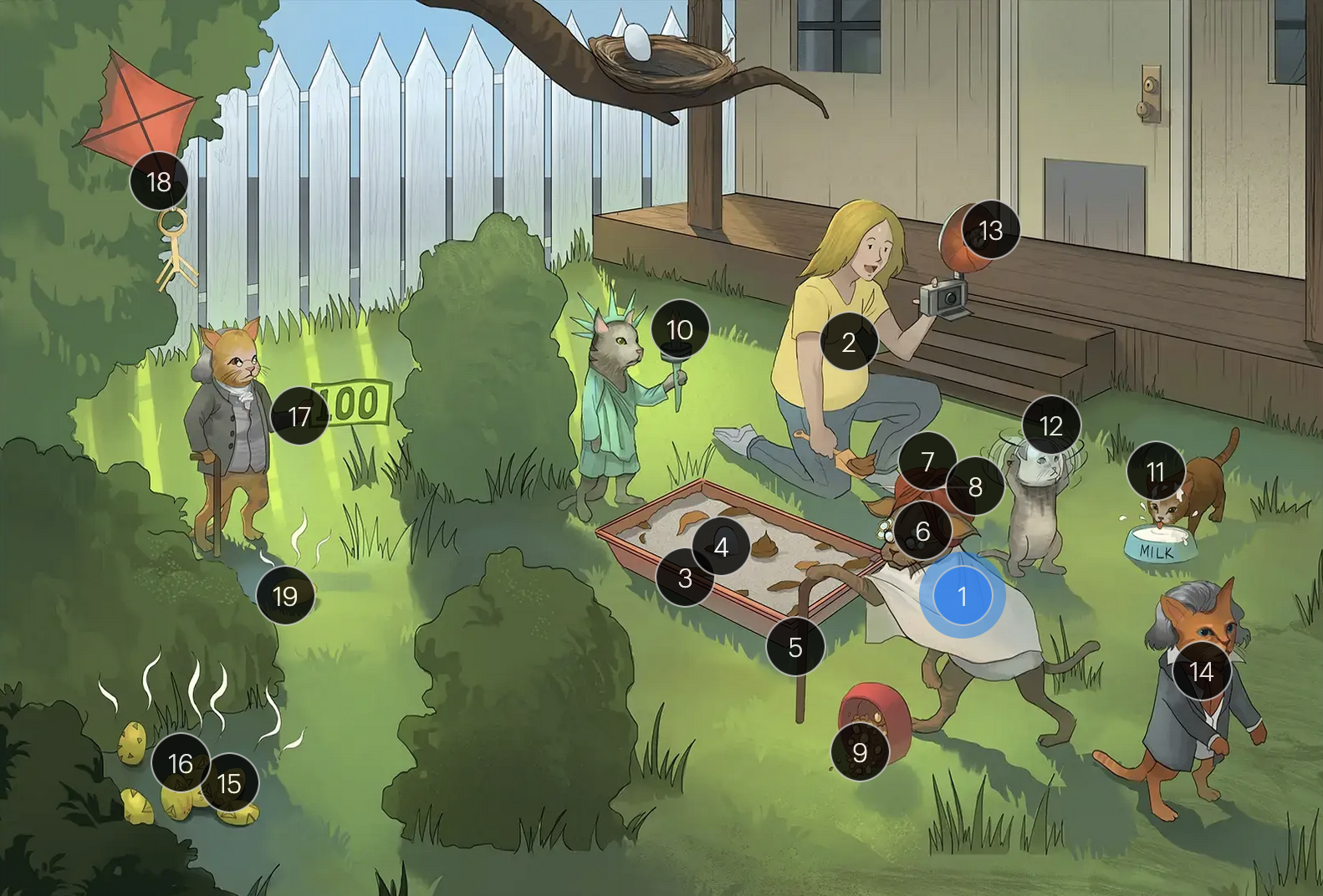
Toxoplasma gondii
#11 milk on head
the classic presentation of congenital toxo includes intracranial calcifications, hydrocephalus, and chorioretinitis
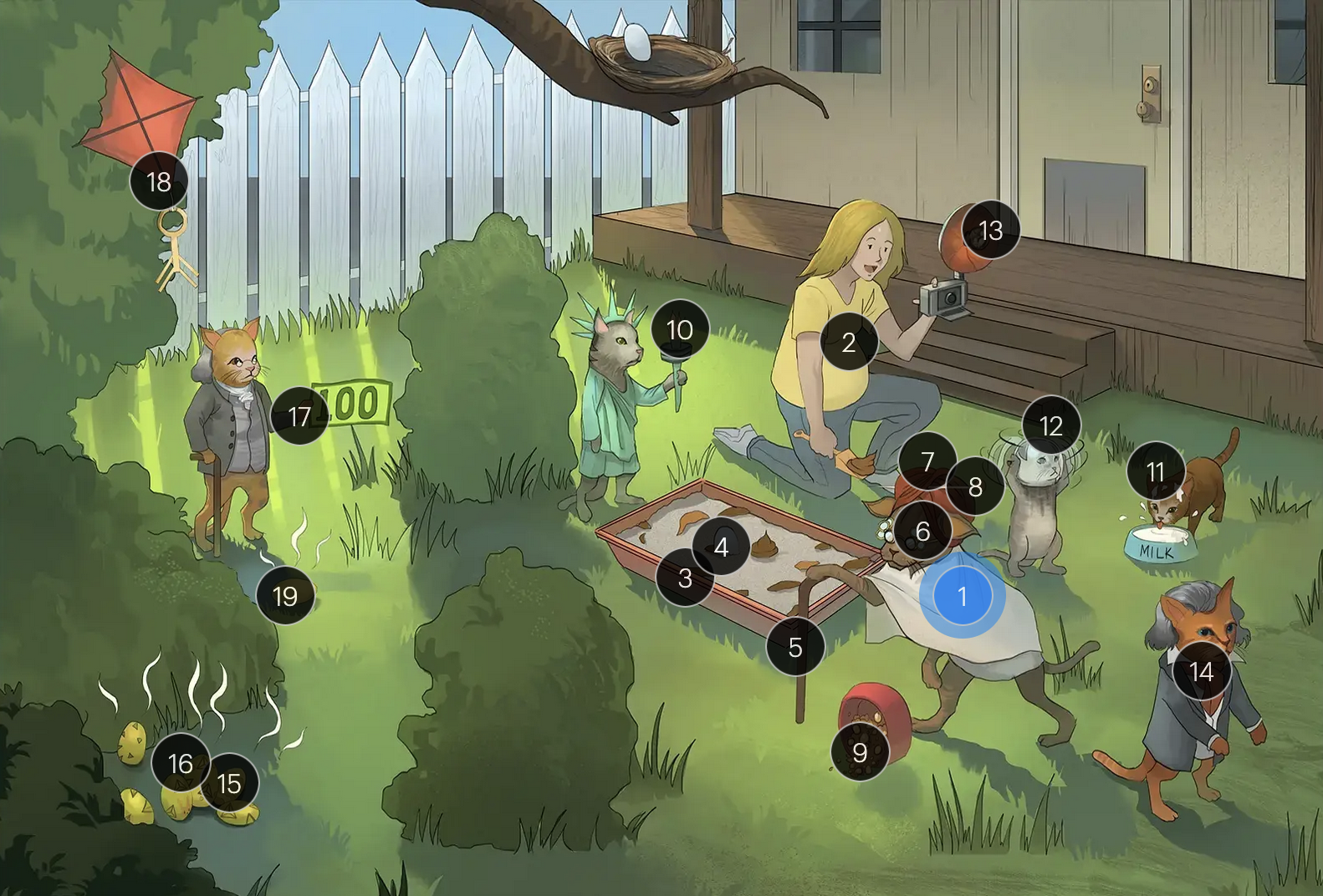
Toxoplasma gondii
#12 water bowl on head
the classic presentation of congenital toxo includes intracranial calcifications, hydrocephalus, and chorioretinitis
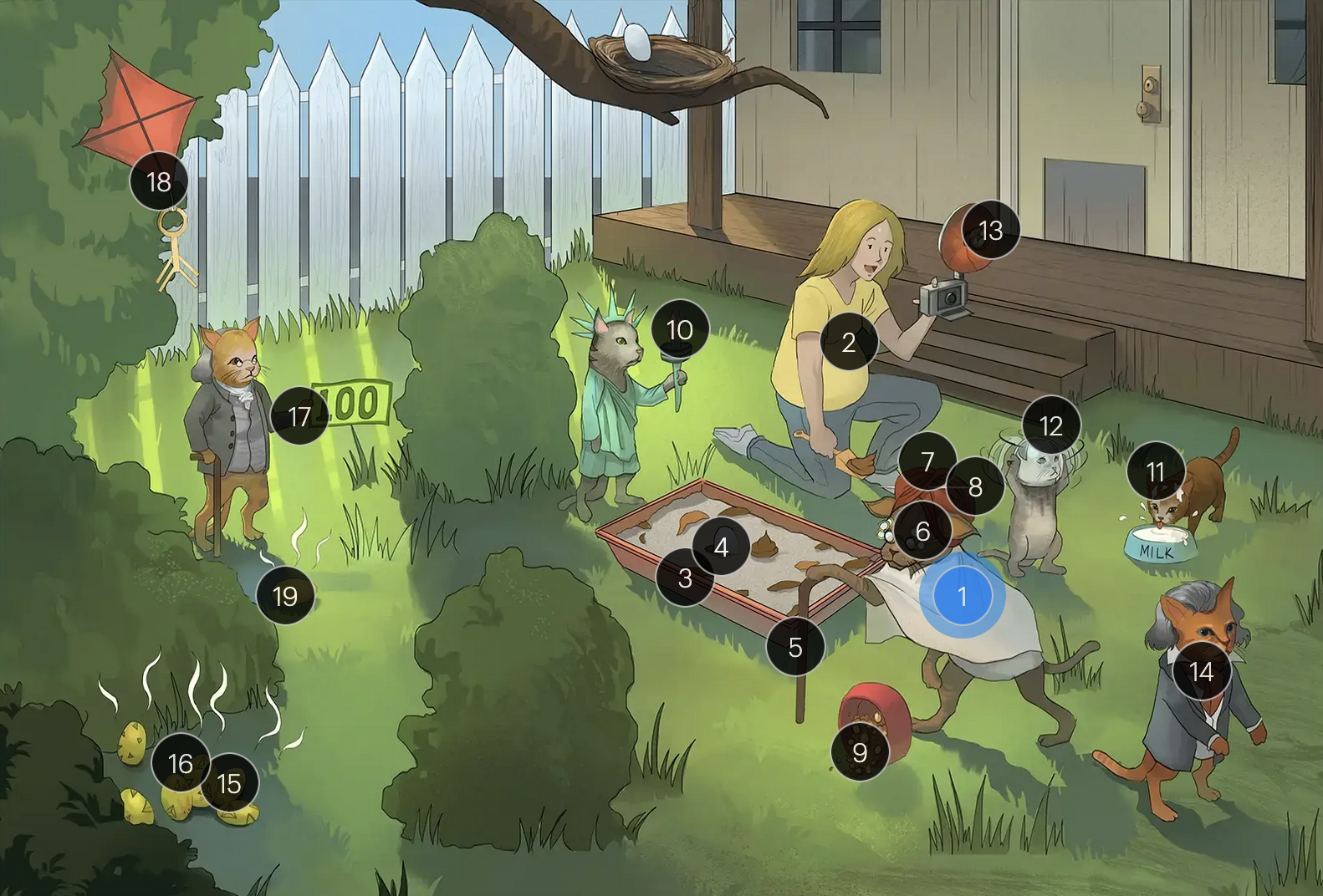
Toxoplasma gondii
#13 flash bulb
the classic presentation of congenital toxo includes intracranial calcifications, hydrocephalus, and chorioretinitis
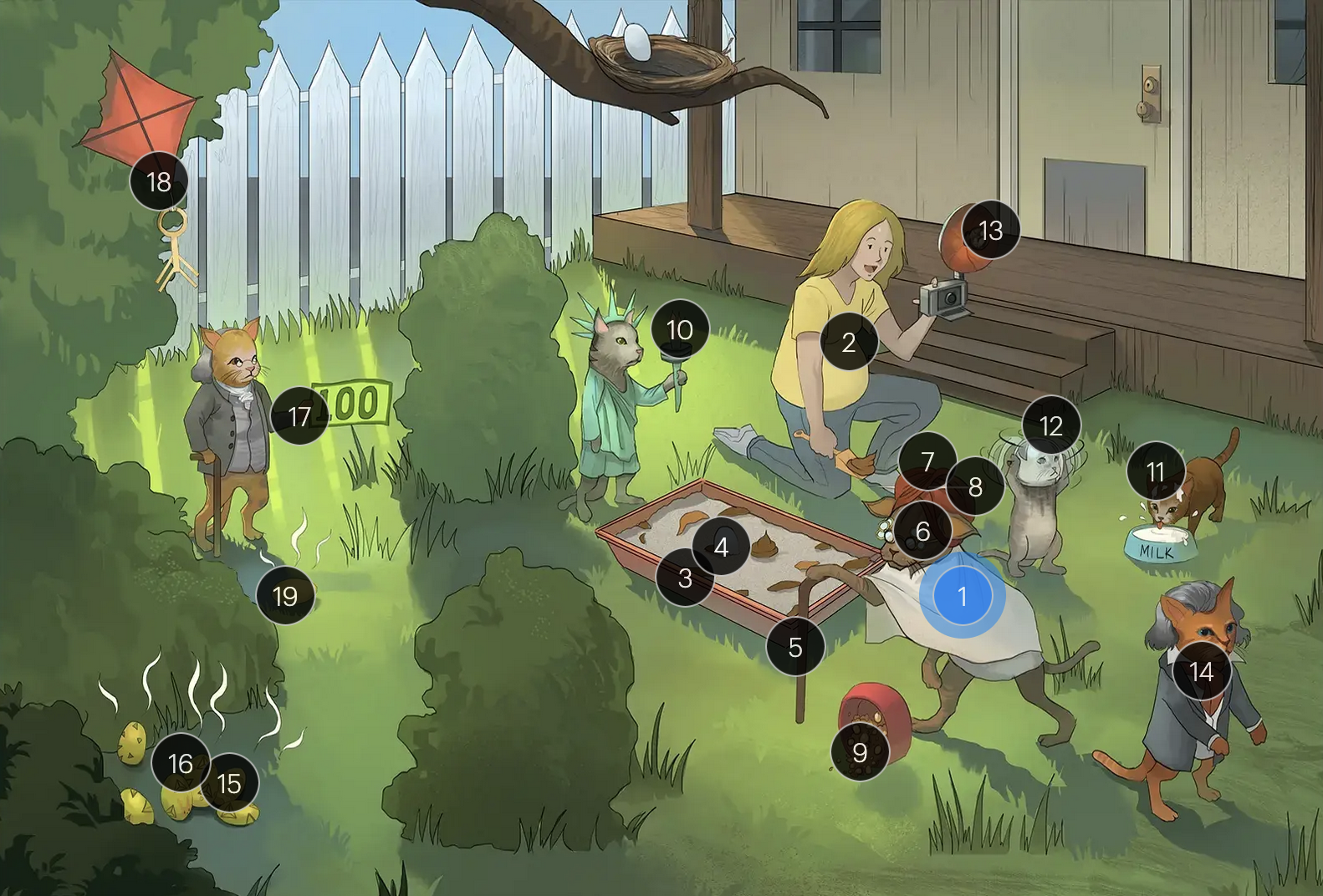
Toxoplasma gondii
#14 deaf Beethoven
congenital toxo is a known cause of hearing loss

Toxoplasma gondii
#15 sulfur eggs
sulfadiazine, in combo with pyrimethamine, is a cornerstone in the tx of toxo
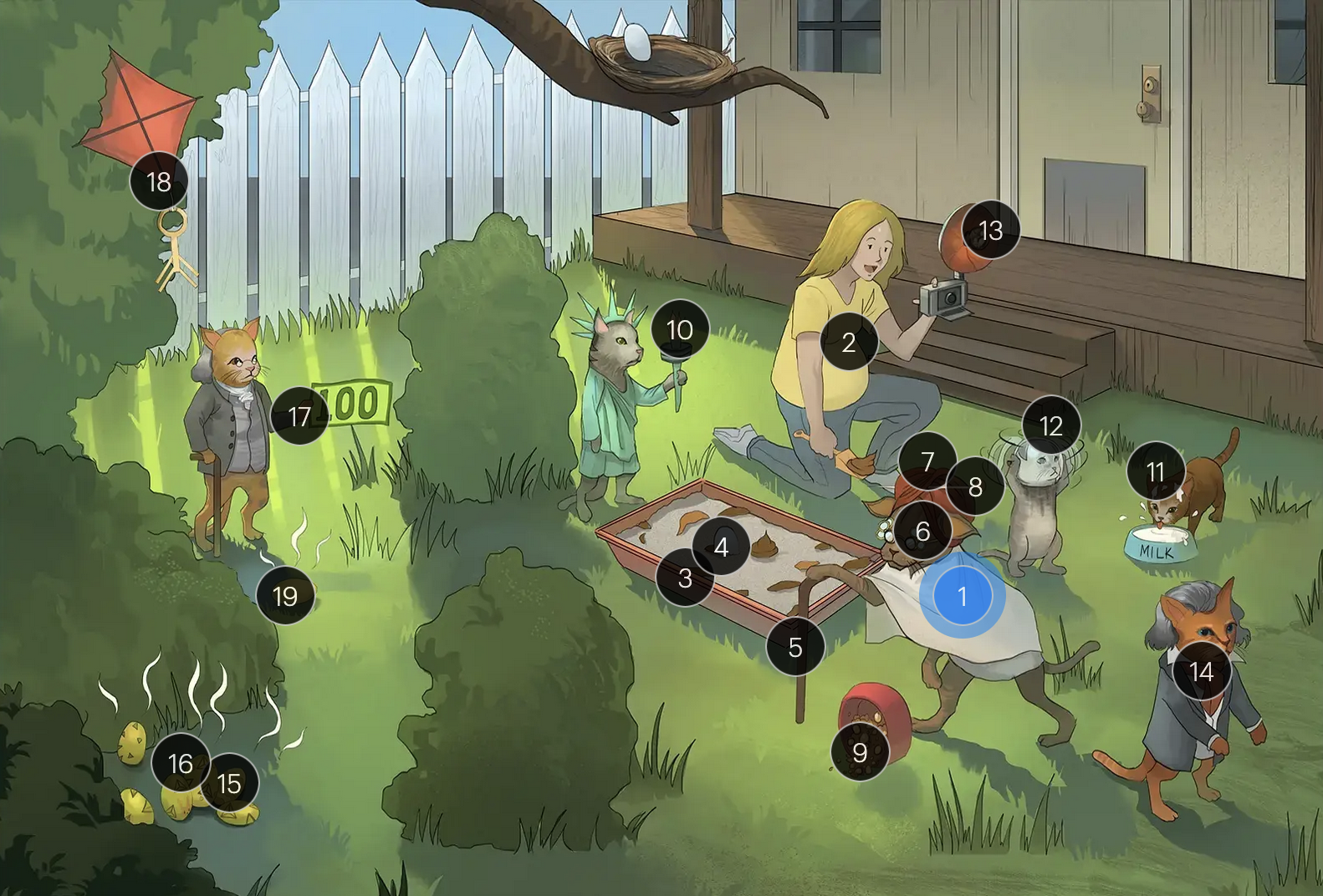
Toxoplasma gondii
#16 pyramid pattern
sulfadiazine, in combo with pyrimethamine, is a cornerstone in the tx of toxo
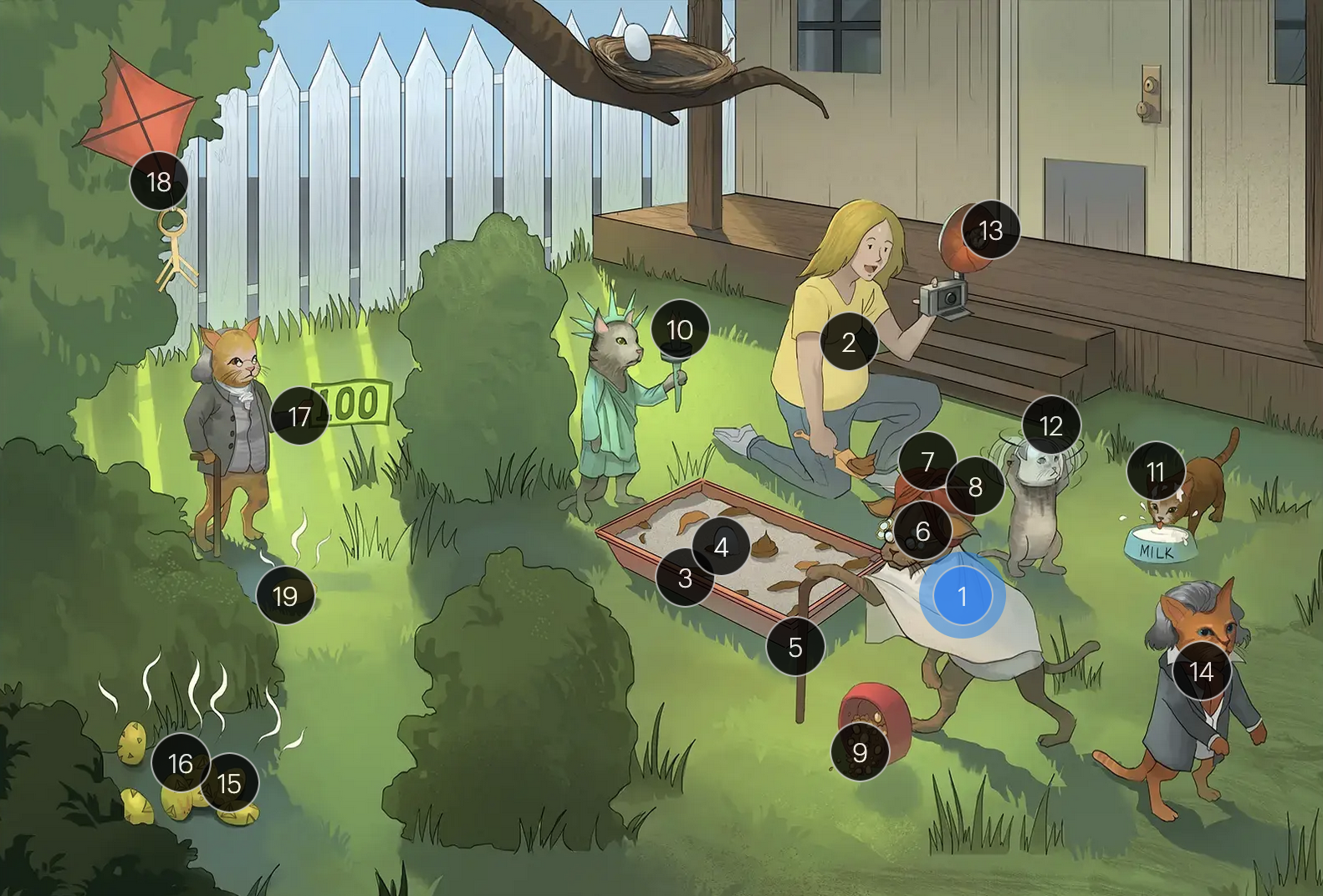
Toxoplasma gondii
#17 immunocompromised cane + $100 bill
prophylaxis with TMX-SMX is recommended for toxo IgG positive HIV patients with a CD4+ count below 100 cells/microL to prevent reactivation of toxo

Toxoplasma gondii
#18 “+” kite with IgG antibody key
prophylaxis with TMX-SMX is recommended for toxo IgG positive HIV patients with a CD4+ count below 100 cells/microL to prevent reactivation of toxo
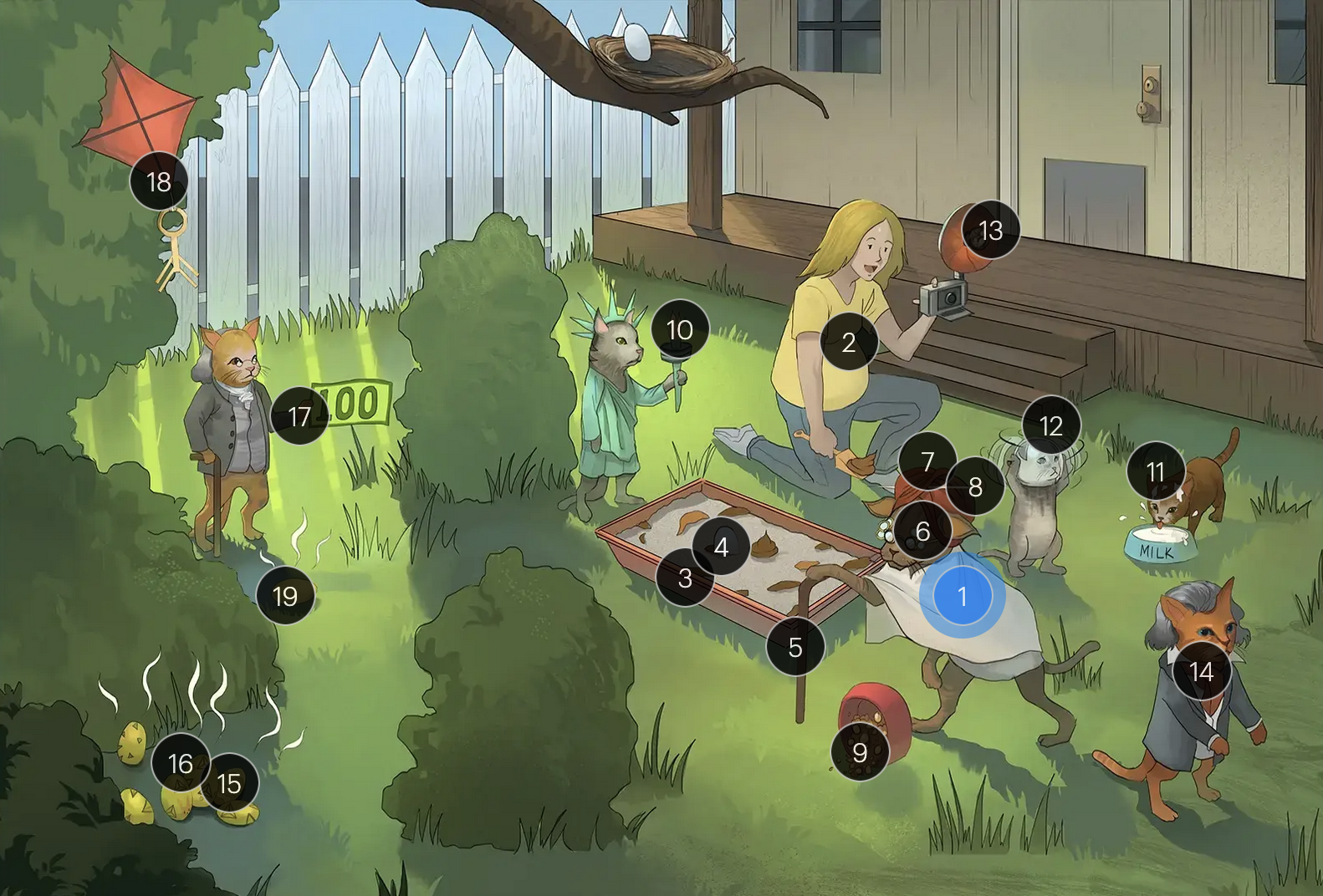
Toxoplasma gondii
#19 sulphur egg by $100
prophylaxis with TMX-SMX is recommended for toxo IgG positive HIV patients with a CD4+ count below 100 cells/microL to prevent reactivation of toxo

Trichomonas vaginalis
#1 magic trichs
trichomonas vaginalis (a unicellular protozoan parasite of the reproductive system)

Trichomonas vaginalis
#2 magic scarves
is a motile organism with whip-like flagella and an undulating membrane

Trichomonas vaginalis
#3 trophy
exists ONLY as a trophozoite form, it does NOT have a cyst form

Trichomonas vaginalis
#4 couple kissing
is a sexually transmitted infection of the urogenital tract

Trichomonas vaginalis
#5 cobblestone sidewalk
has a tropism for squamous epithelial cells —> infection and inflammation of the vulva, vagina, cervix, and urethra

Trichomonas vaginalis
#6 smiling delivery man
asymptomatic carriage, primarily in MEN, contributes to the spread of trich infection; tx of sexual partners reduces this risk

Trichomonas vaginalis
#7 vaginal flowers
causes vulvogaginitis, inflammation of the vulva and vagina marked by erythema, burning, pruritis, and discharge

Trichomonas vaginalis
#8 burning trash can
causes vulvogaginitis, inflammation of the vulva and vagina marked by erythema, burning, pruritis, and discharge

Trichomonas vaginalis
#9 itching dog
causes vulvogaginitis, inflammation of the vulva and vagina marked by erythema, burning, pruritis, and discharge

Trichomonas vaginalis
#10 leaking fluid
causes vulvogaginitis, inflammation of the vulva and vagina marked by erythema, burning, pruritis, and vaginal discharge

Trichomonas vaginalis
#11 frothy green puddles
causes a classically copious, yellowish-green, frothy, malodorous vaginal discharge

Trichomonas vaginalis
#12 strawberry hat trick
cervical inflammation marked by erythema, edema, and punctate hemorrhages (AKA strawberry cervix)

Trichomonas vaginalis
#13 “4.50 and up”
thrives in a basic environment, so vaginal pH testing will show a pH of 4.5 or greater

Trichomonas vaginalis
#14 leaking package
in men, usually asyptomatic, but may present as urethritis, marked by dysuria and thin, white discharge

Trichomonas vaginalis
#15 pear puddle
performing a wet mount (saline microscopy) on a collected sample will show a moving, pear-shaped trophozoite

Trichomonas vaginalis
#16 metro
metronidazole is effective against t. vaginalis

Trichomonas vaginalis
#17 metro couple
tx of sexual partners for those with infection is recommended to reduce risk of recurrence and spread

Trichomonas vaginalis
#18 condom hat
consistent use of barrier contraception prevents retransmission of trich until treatment is complete
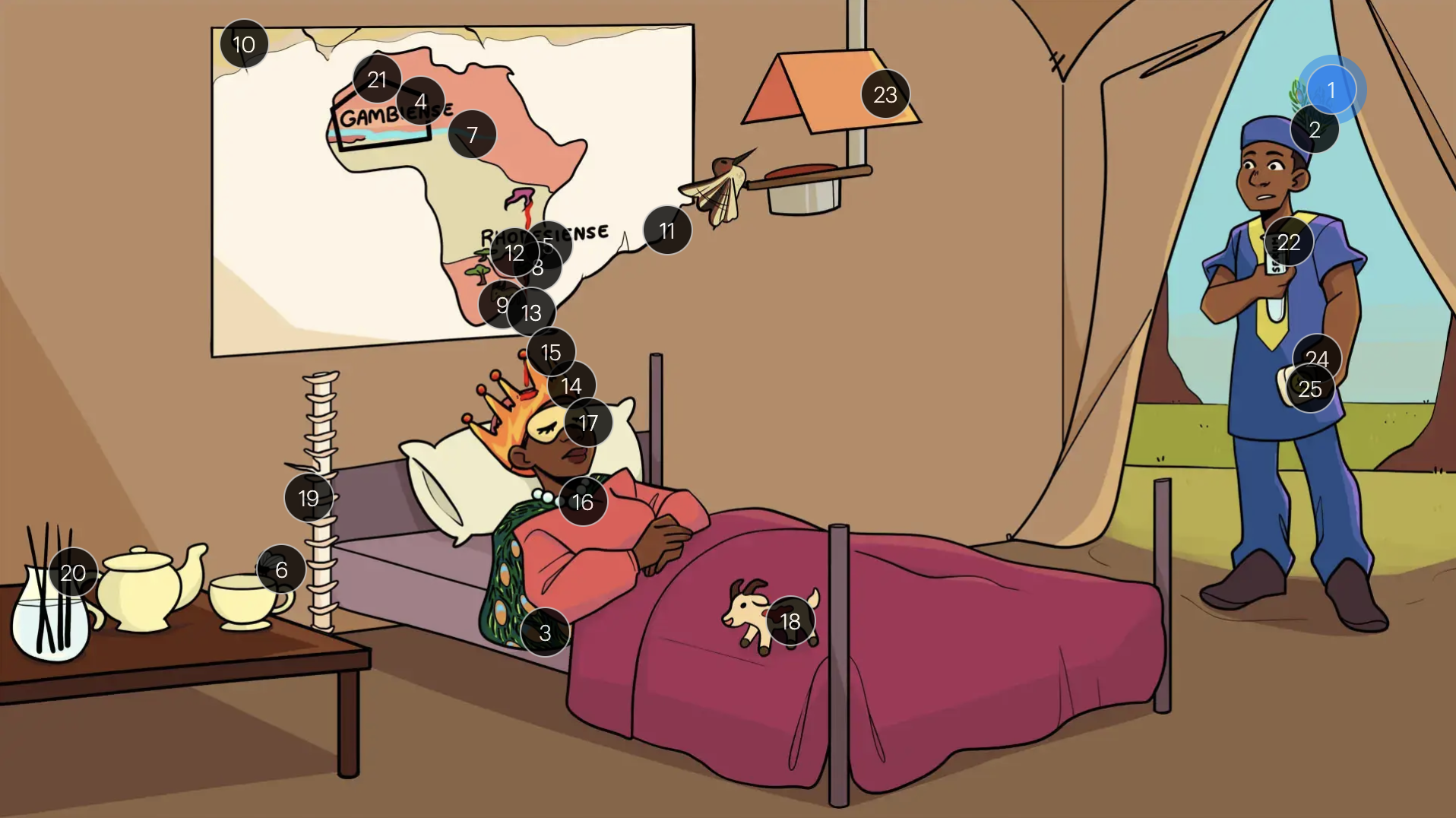
Trypanosoma brucei
#1 3 feathers
trypanosoma brucei, the causative agent of sleeping sickness
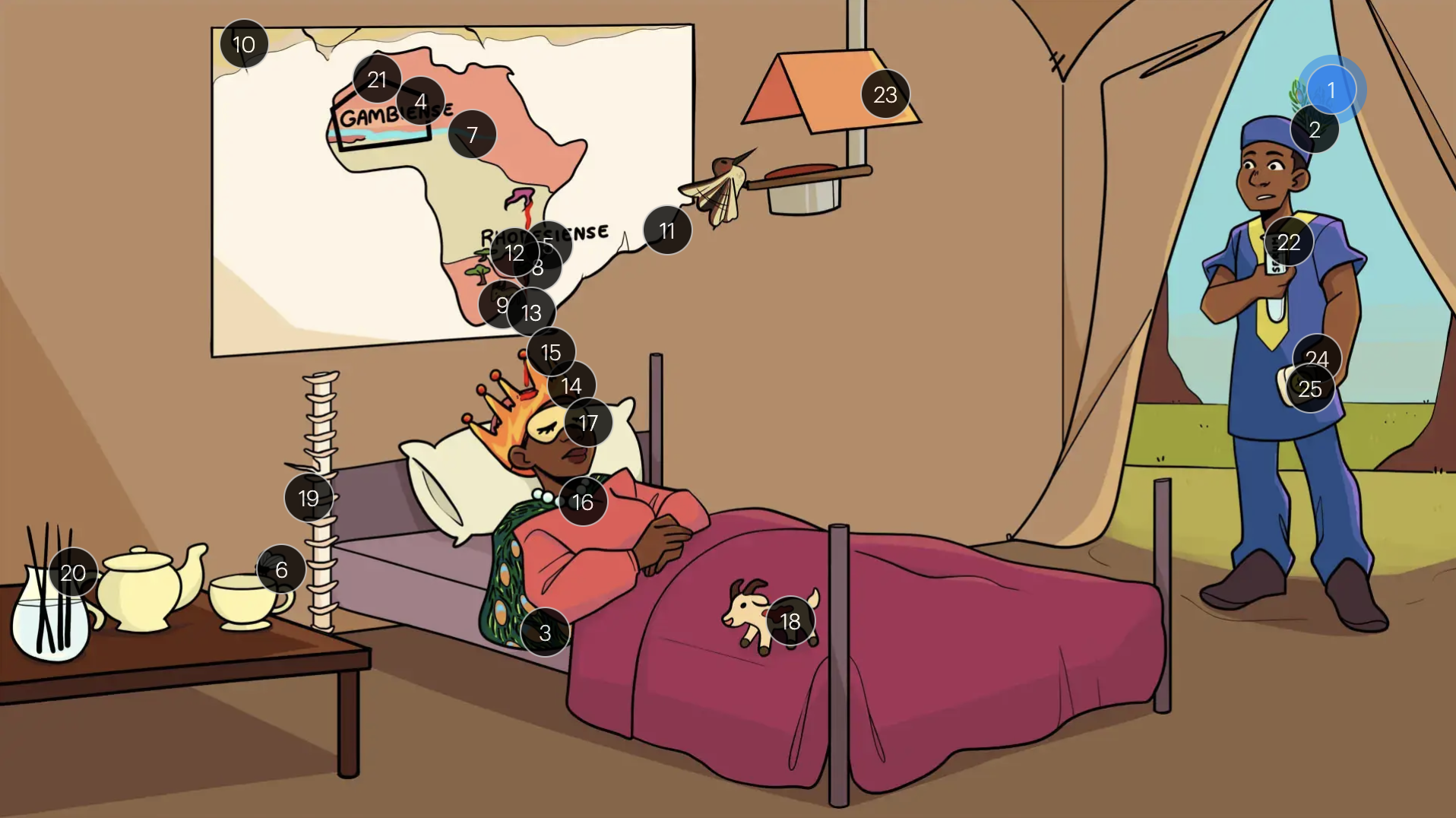
Trypanosoma brucei
#2 feather’s stem
t. brucei protozoa are motile with a single flagellum

Trypanosoma brucei
#3 variable peacock cloak
t. brucei protozoa have variable surface glycoprotein coats which constantly undergo antigenic variation
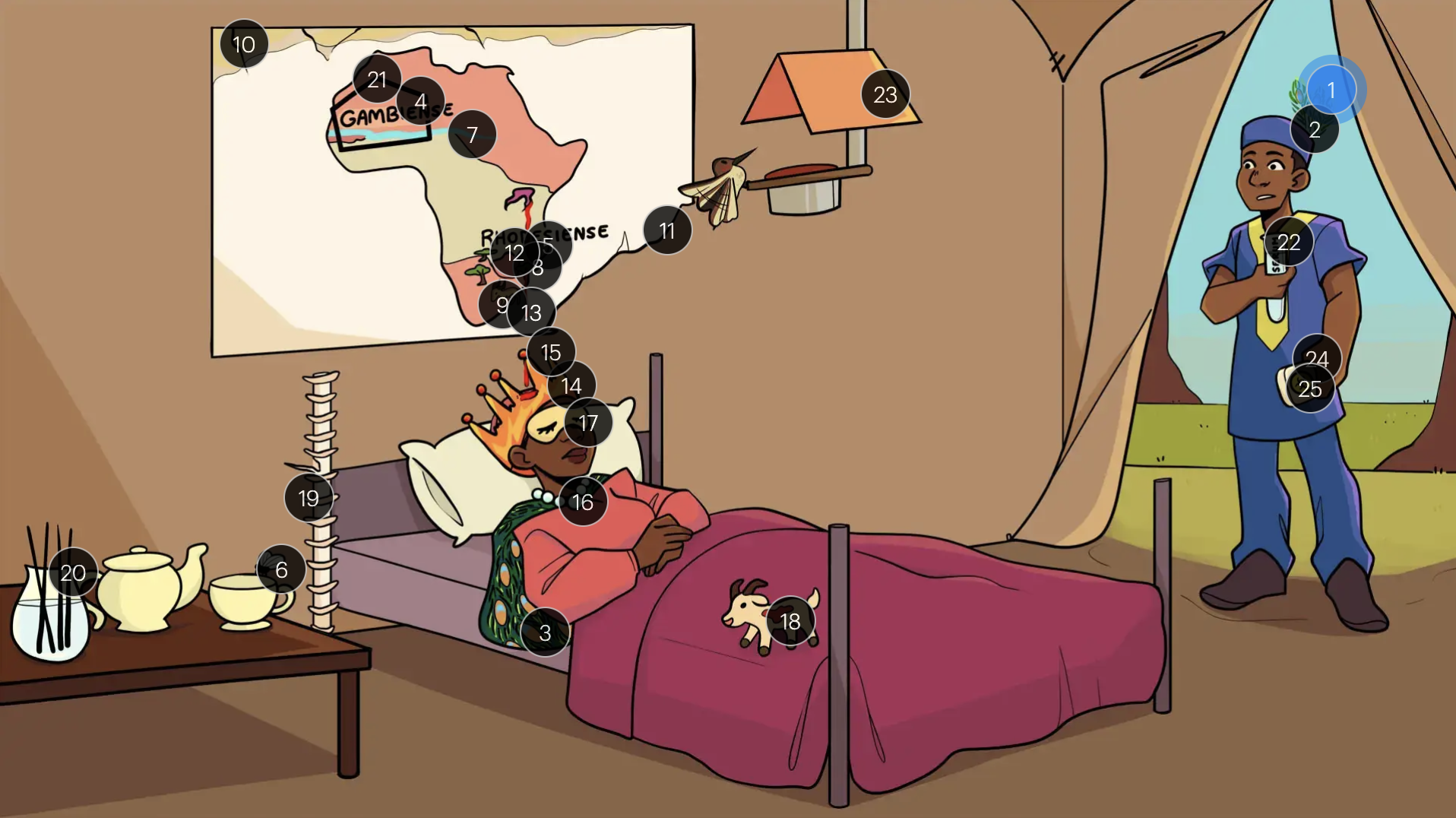
Trypanosoma brucei
#4 gambia spot on map
t. brucei gambiense
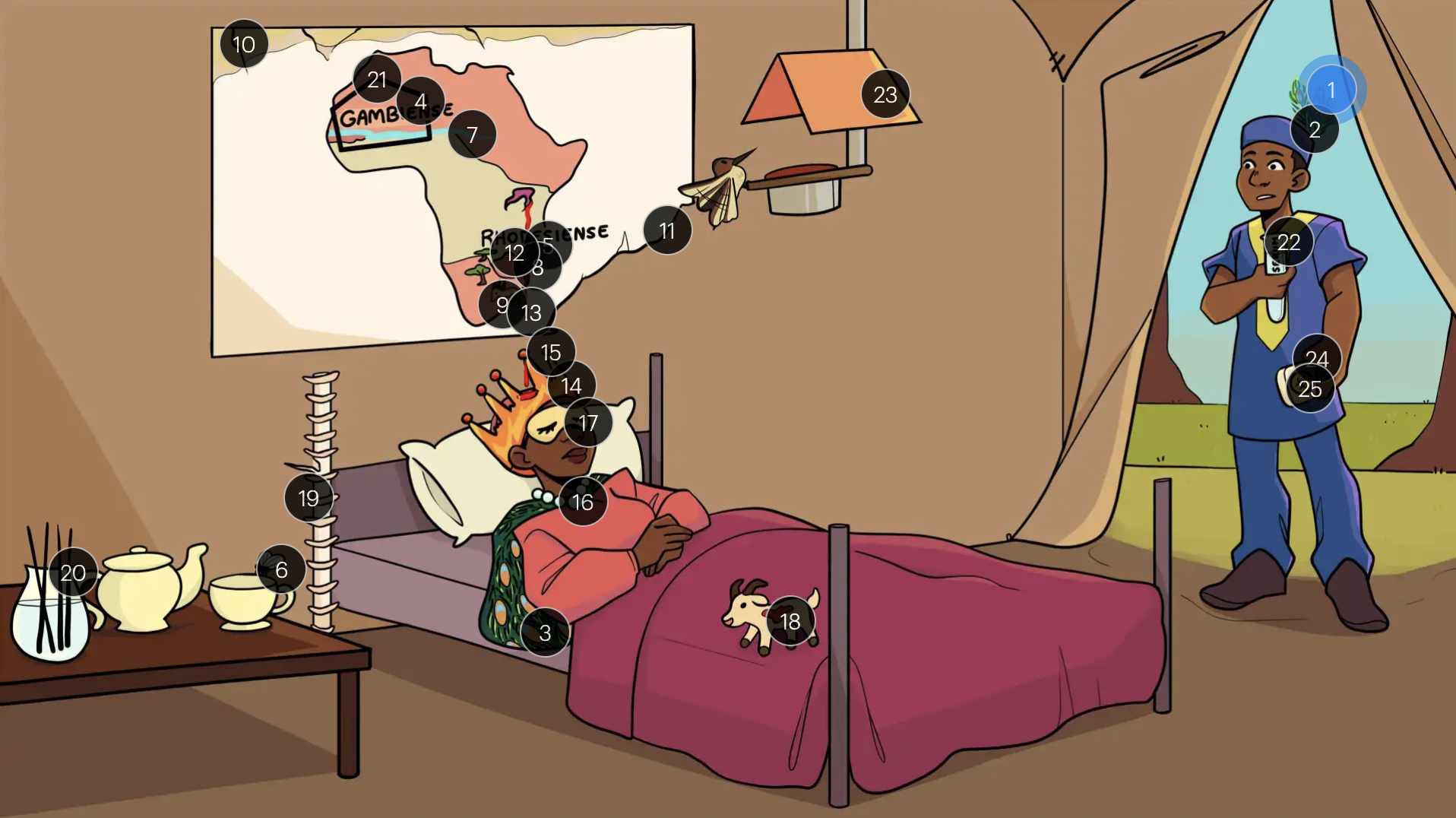
Trypanosoma brucei
#5 rhodesiense spot on map
t. brucei rhodesiense
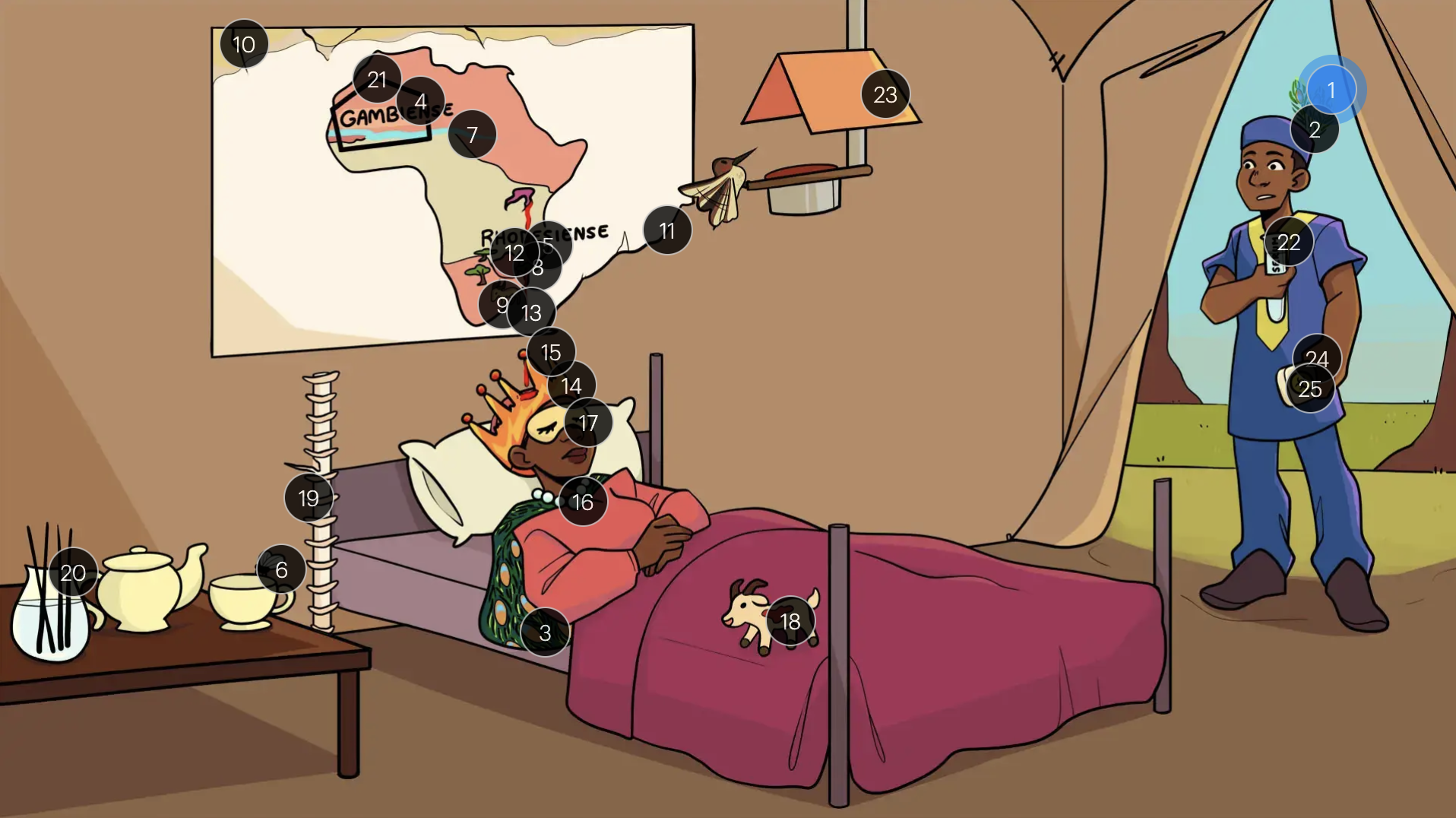
Trypanosoma brucei
#6 tea fly
the tsetse fly is the insect vector for trypanosomiasis
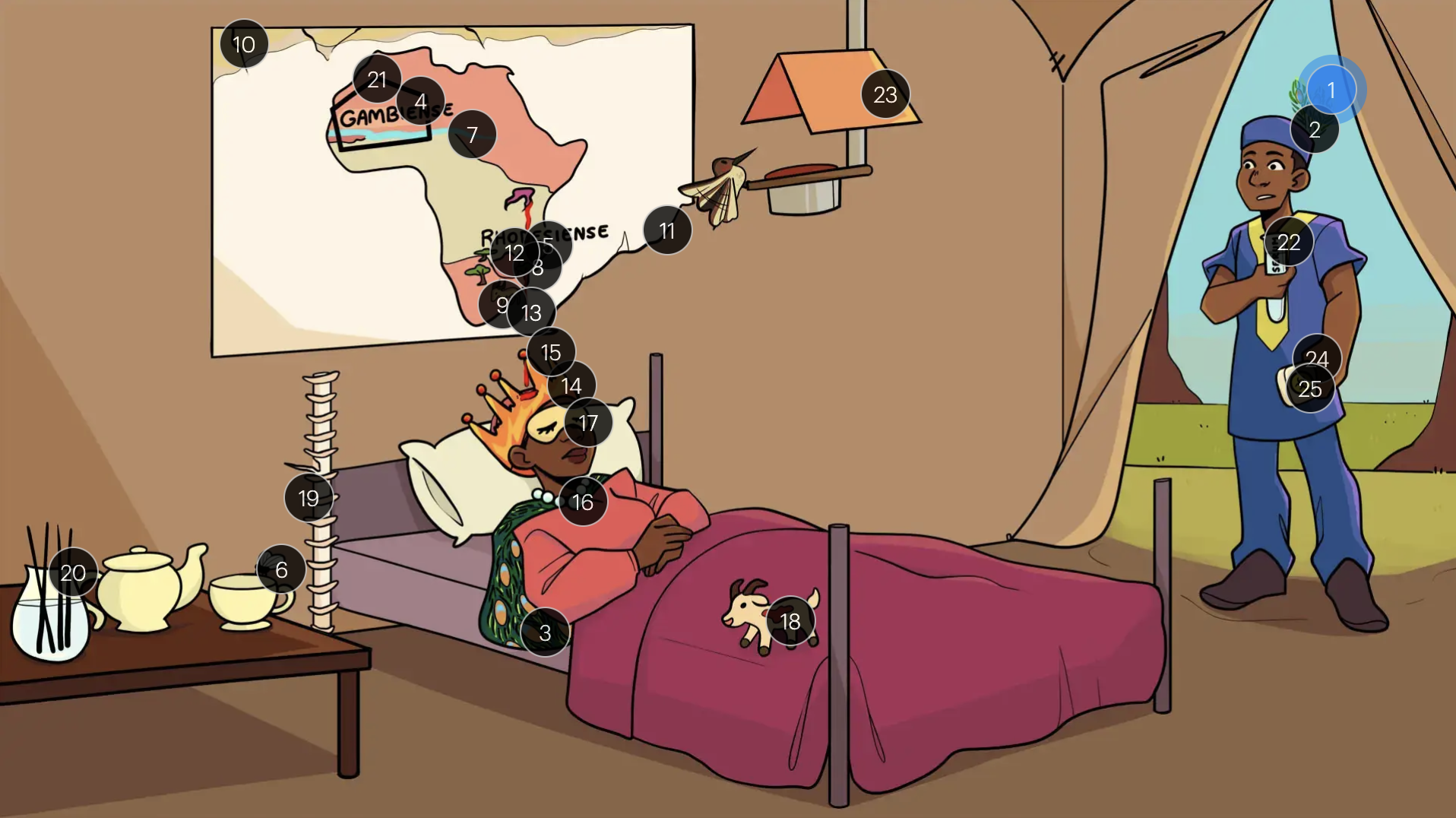
Trypanosoma brucei
#7 gambia stream
T.b. gambiense found in streams in Western to Central Africa

Trypanosoma brucei
#8 trees
t.b. rhodesiense found in woodlands in East and SE African Savannahs
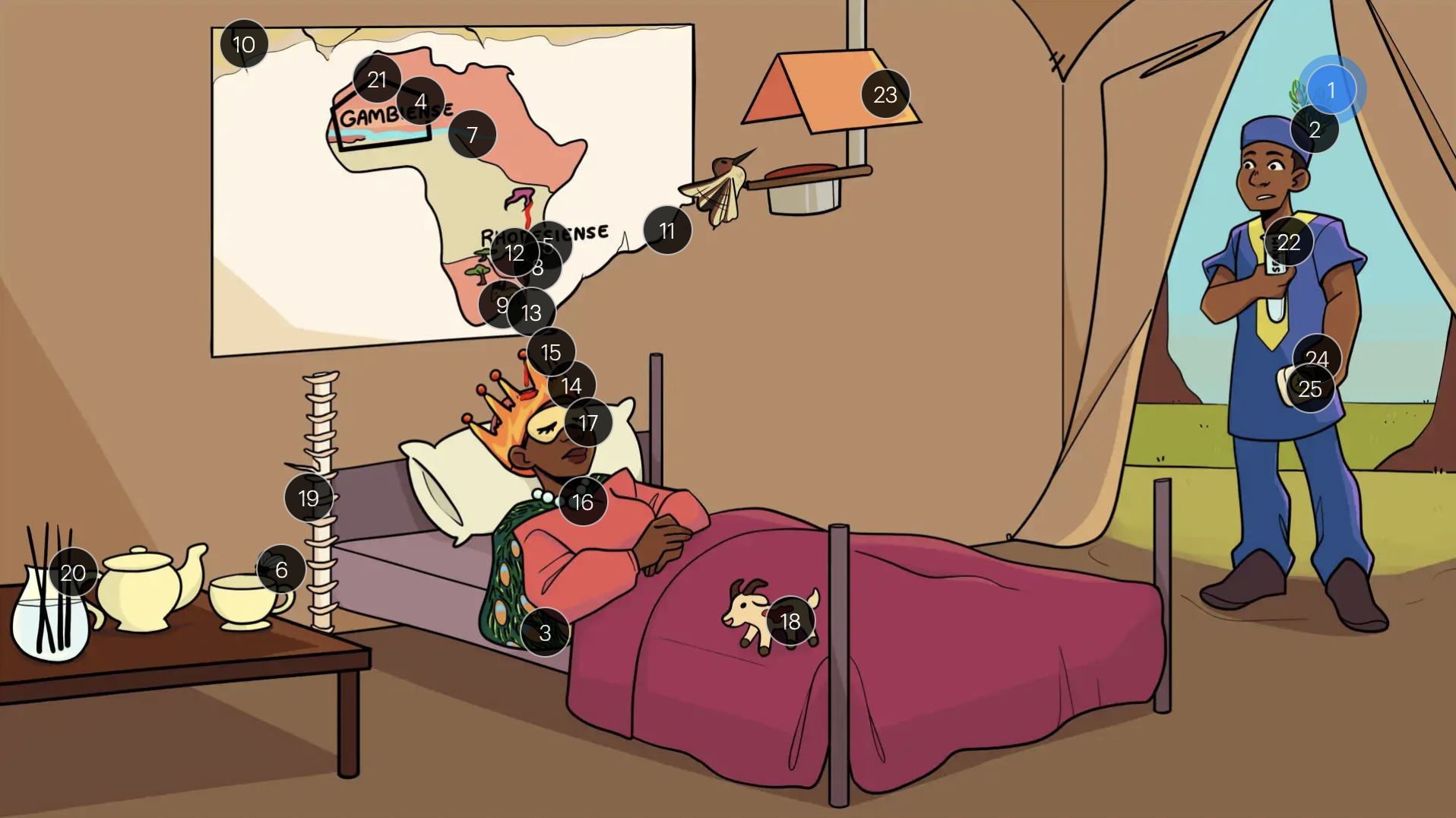
Trypanosoma brucei
#9 antelope mark
t.b. rhodesiense are found in an animal reservoir (antelope and other wild game)
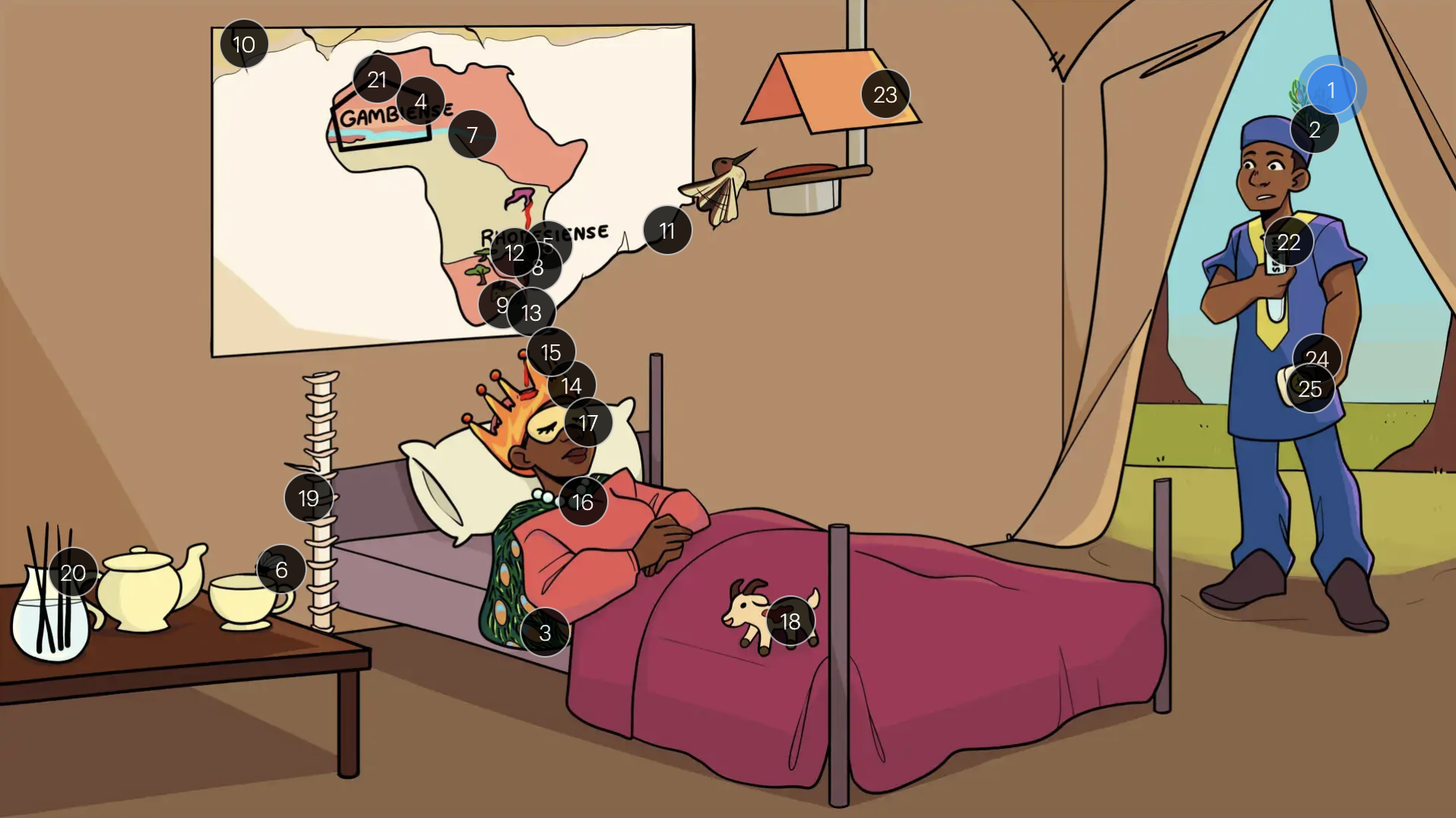
Trypanosoma brucei
#10 withering map
t.b. gambiense causes a slowly progressing, chronic infection
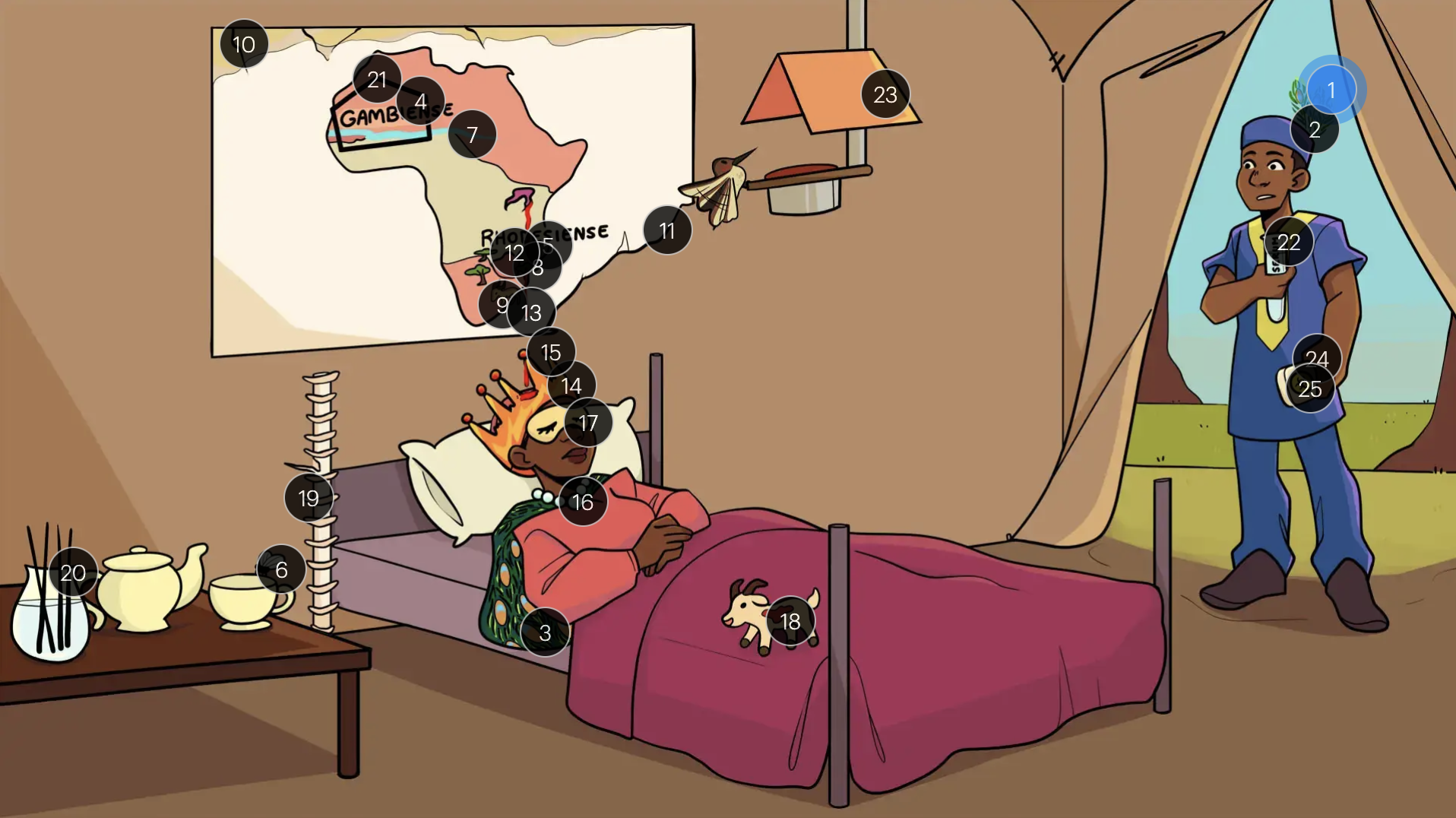
Trypanosoma brucei
#11 torn map
t.b. rhodesiense causes a severe, rapidly progressing, acutely fatal illness

Trypanosoma brucei
#12 great lake sore
a trypanosomal chancre may develop at the site of inoculation (1st stage)
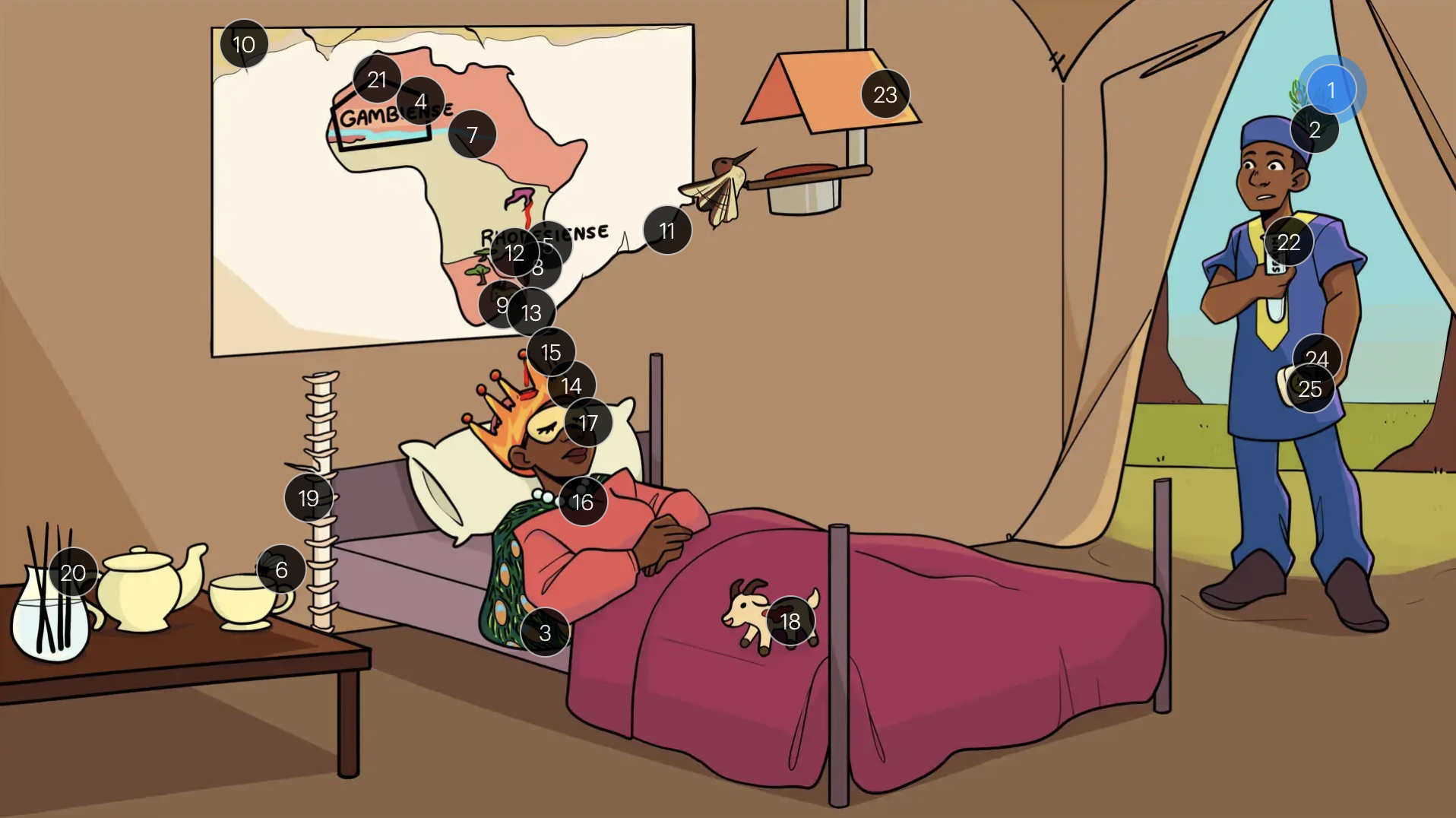
Trypanosoma brucei
#13 dripping red ink
trypanosomes travel from the skin to the blood and lymphatics (i.e. hemo-lymphatic/1st stage)
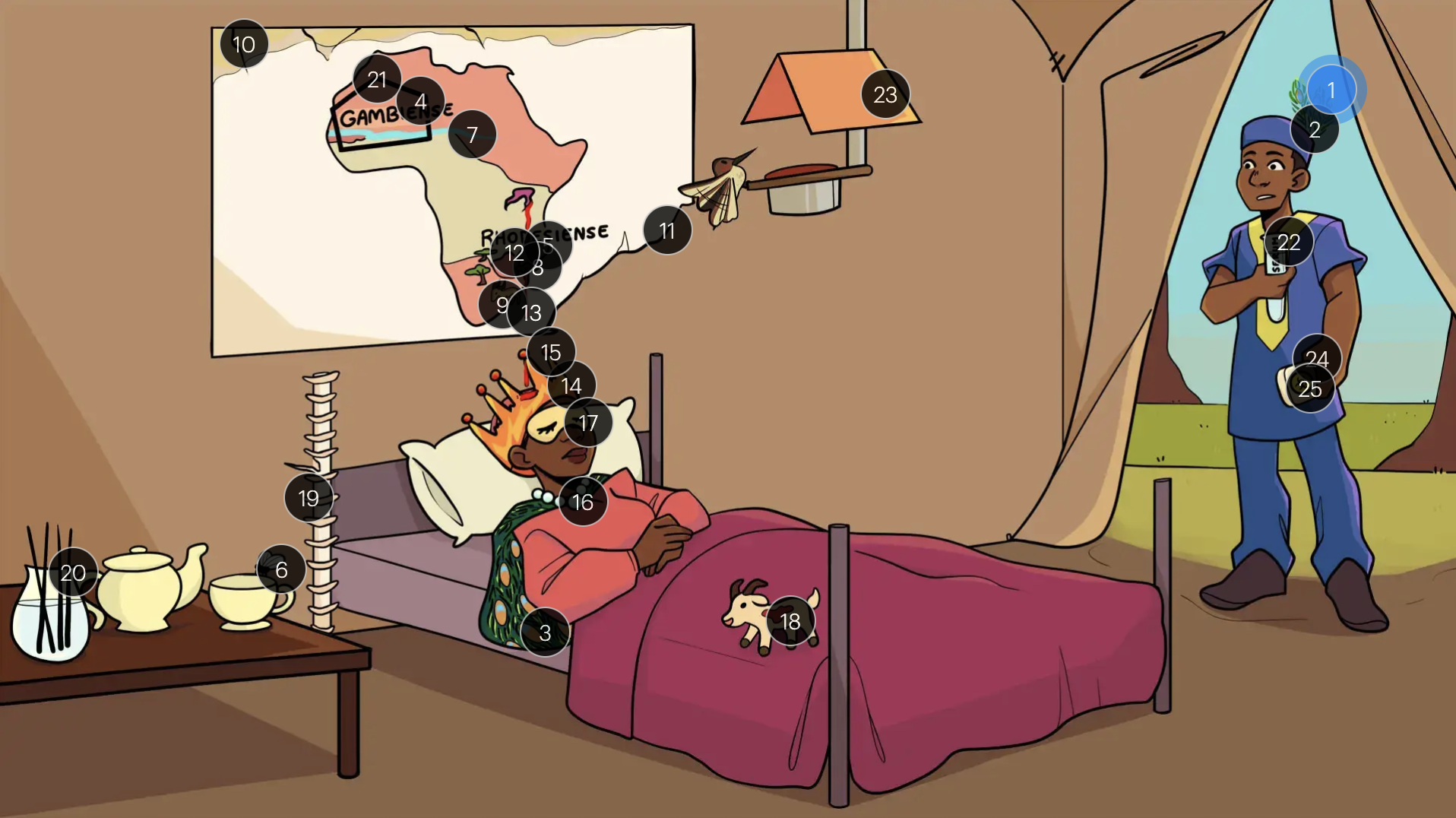
Trypanosoma brucei
#14 flame headband
the first stage of disease is a nonspecific febrile illness with associated headache, malaise, weakness, lymphadenopathy, and puritus
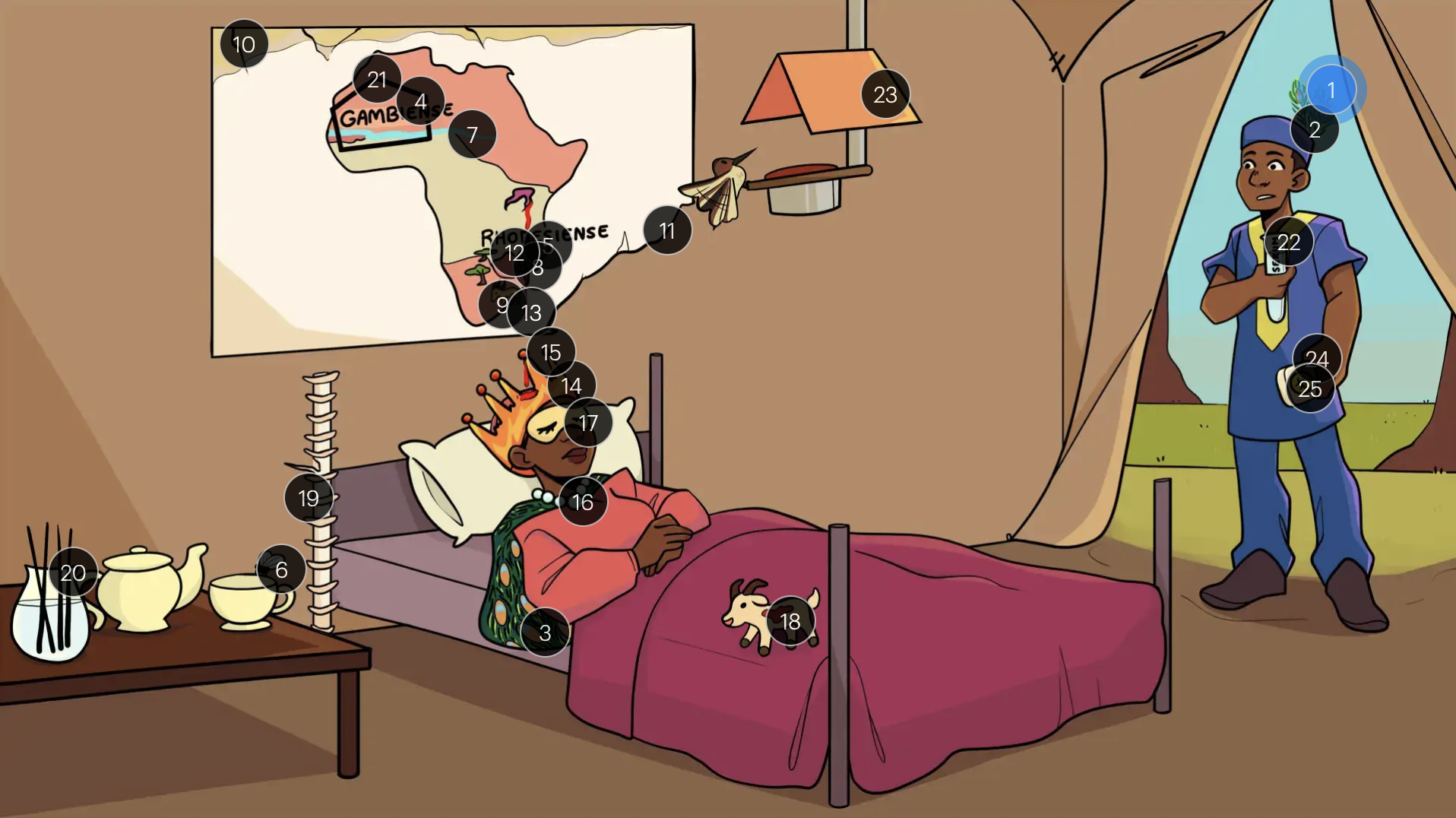
Trypanosoma brucei
#15 intermittent spikes on crown
sleeping sickness presents with a characteristic intermittent, spiking fever (where intervals can vary from days to months)
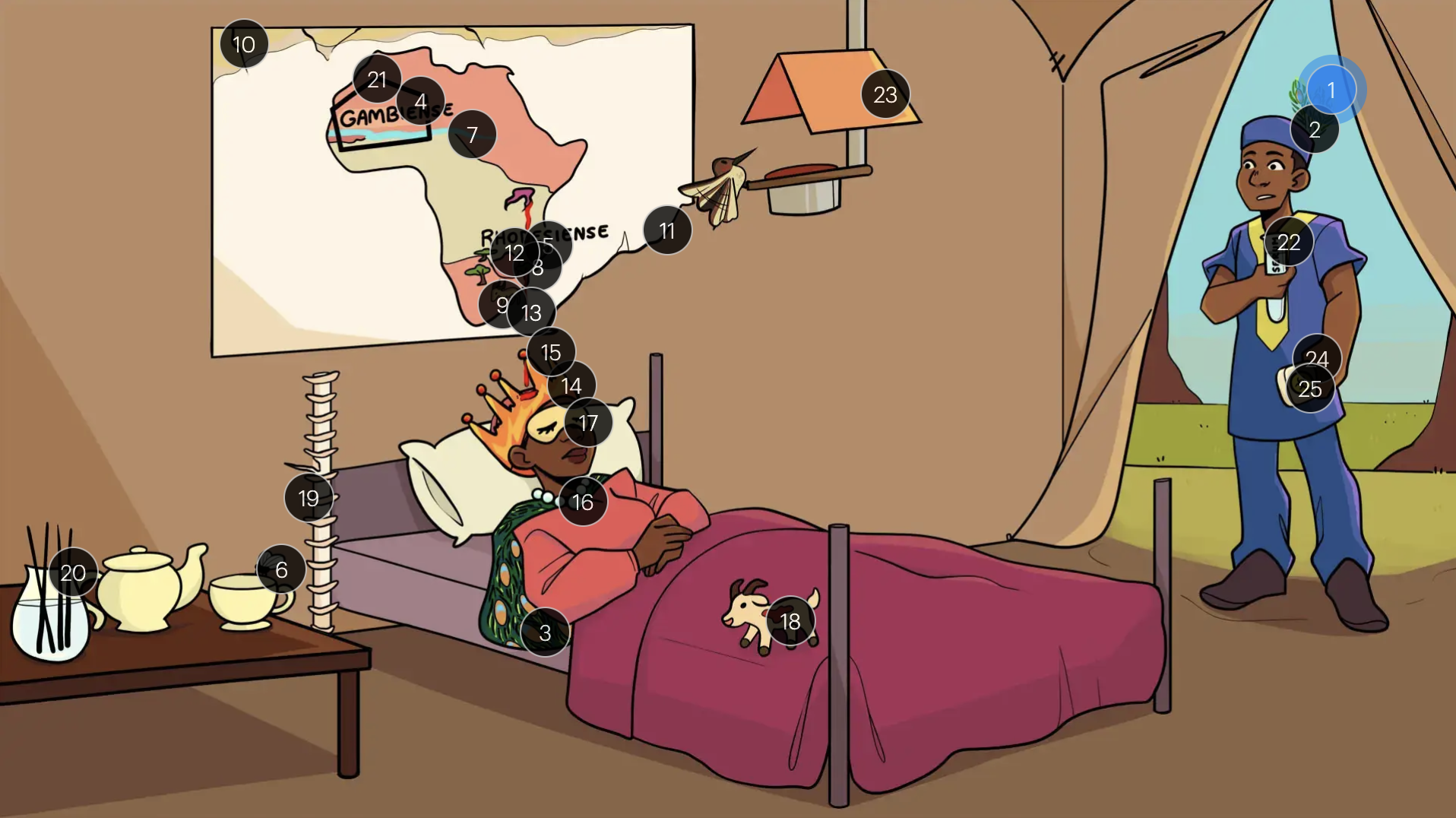
Trypanosoma brucei
#16 string of pearls
t. brucie infections can lead to cervical and axillary lymphadenopathy
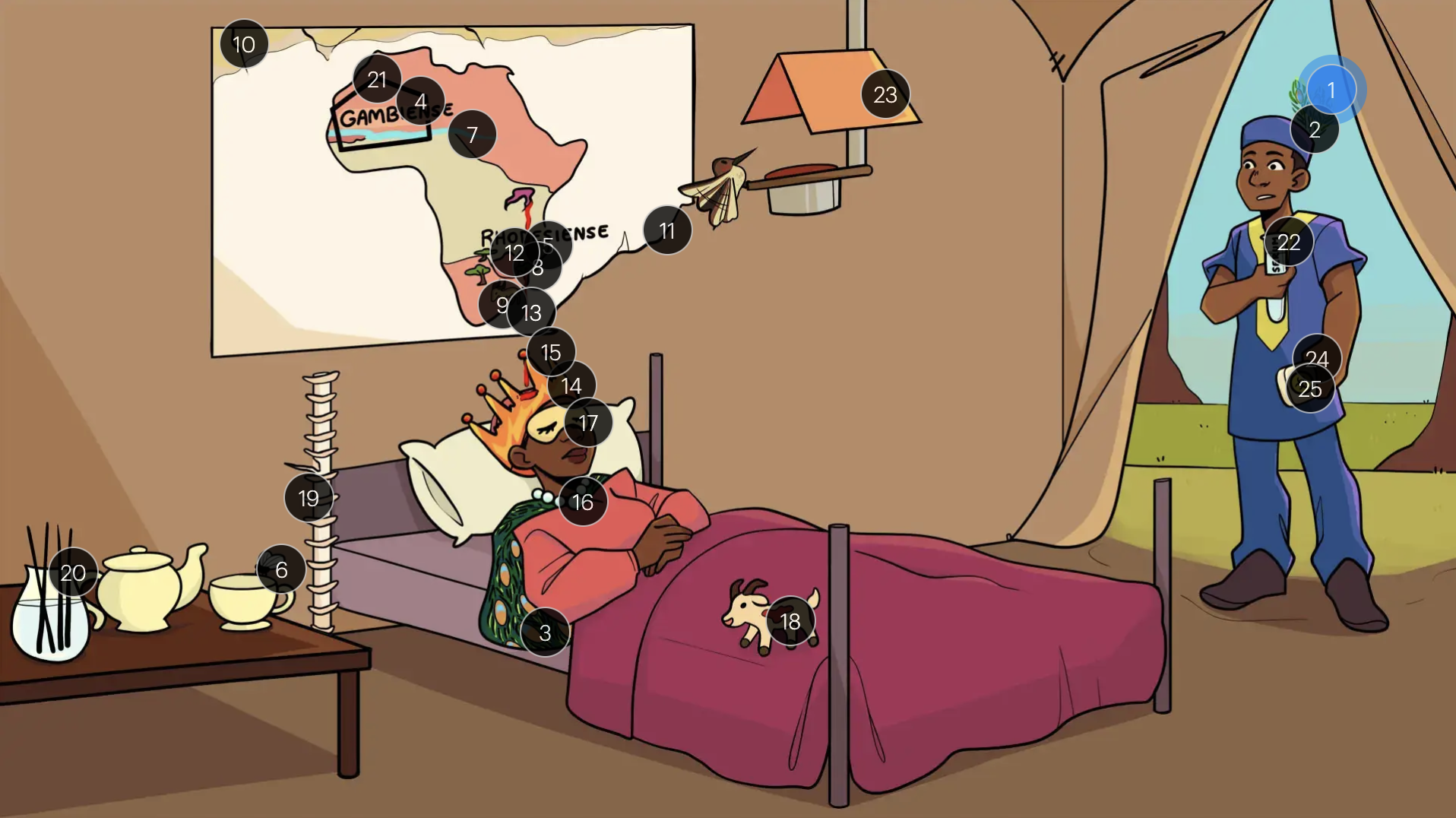
Trypanosoma brucei
#17 sleep mask
the second stage of illness is marked by daytime sleepiness (among other neuropsychiatric abnormalities; mood changes, psychomotor slowing, seizures, and coma)
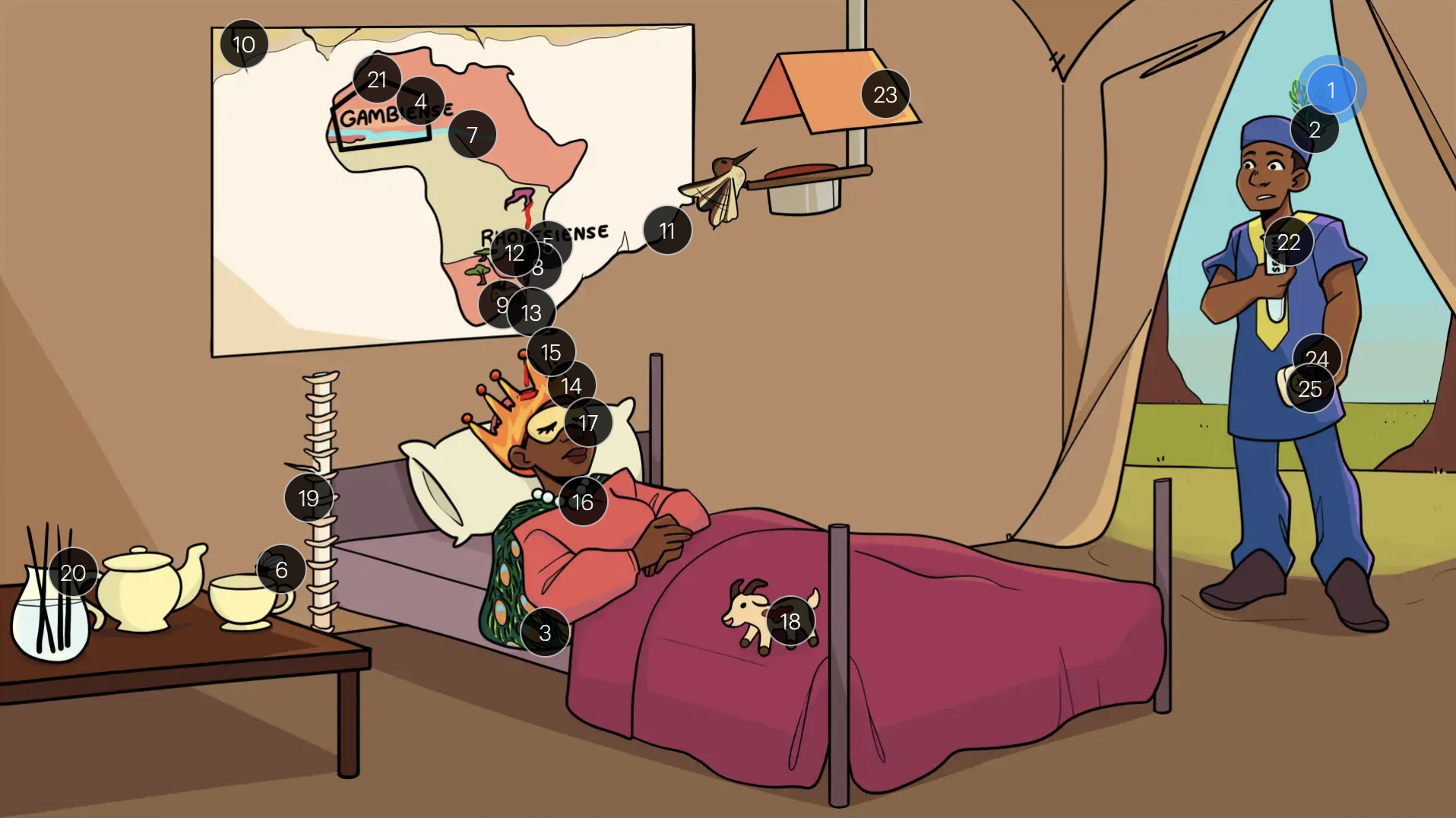
Trypanosoma brucei
#18 trypomastiGOAT + blood spot
trypomastigotes are seen on blood smear
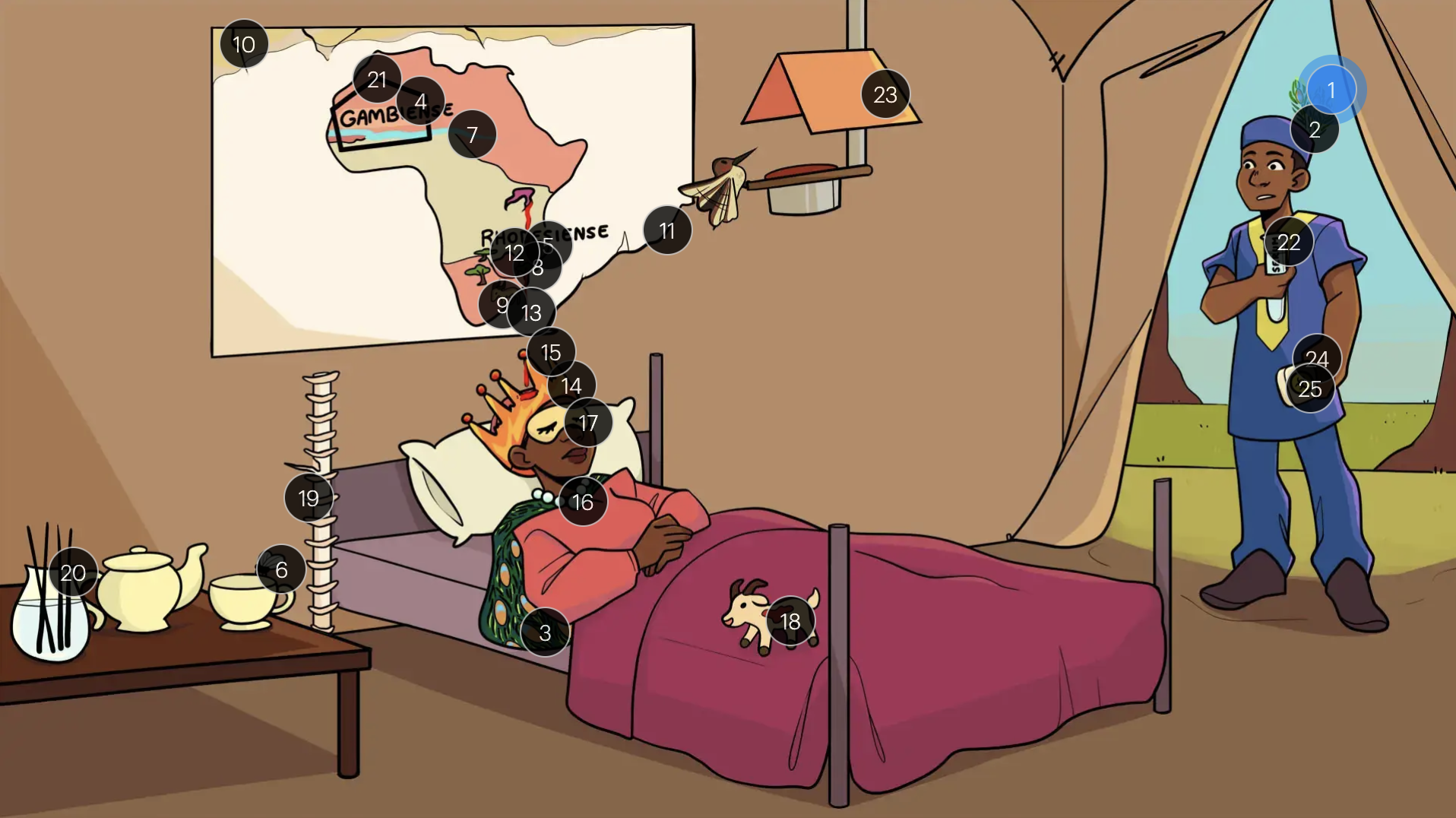
Trypanosoma brucei
#19 spine splinter
CSF analysis enables definitive staging of sleeping sickness (1st stage: scant WBC, NO organisms vs. 2nd stage: high WBC count, organisms present)

Trypanosoma brucei
#20 fogger
control the fly population with aerial insecticides and other environmental controls
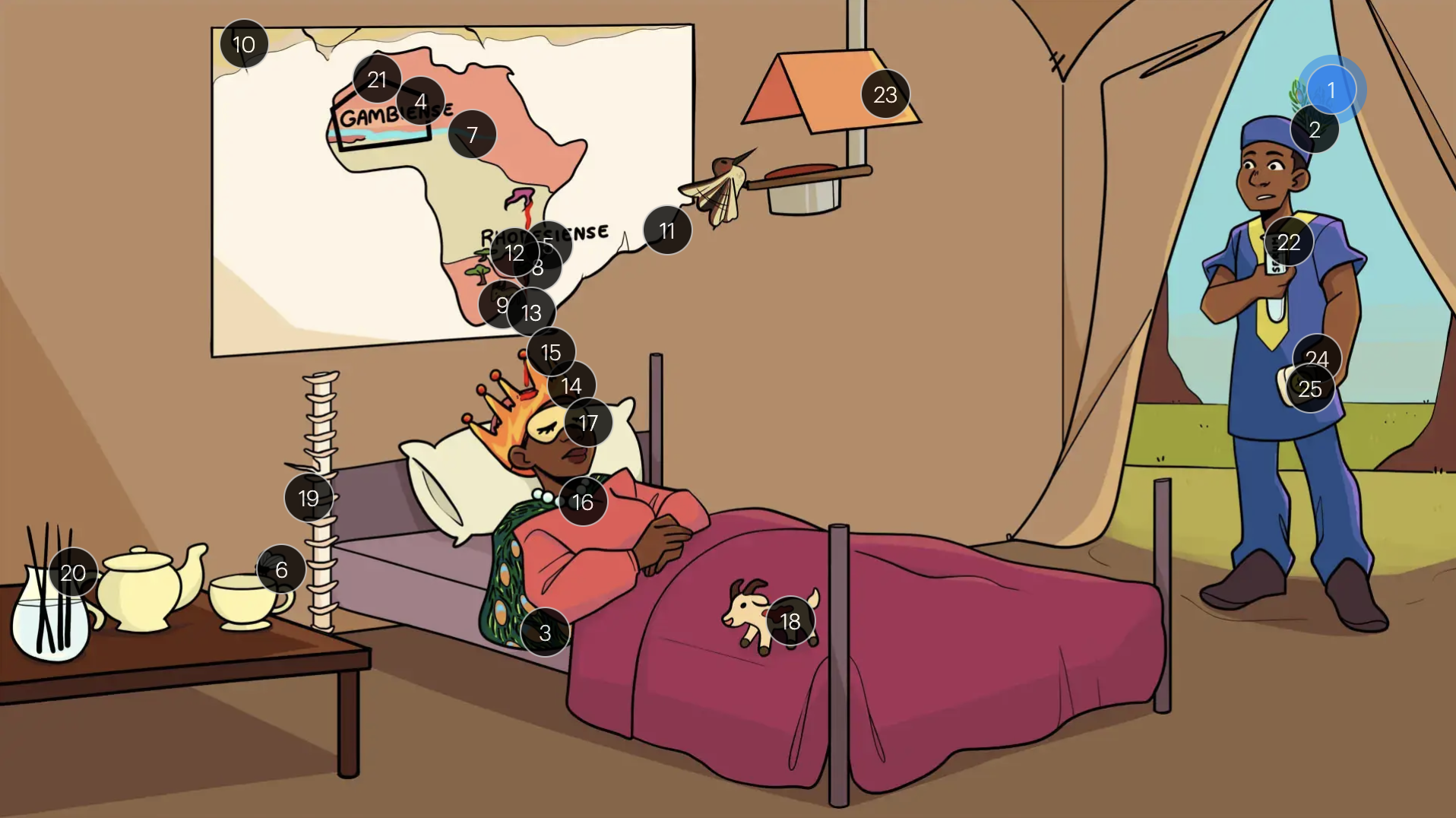
Trypanosoma brucei
#21 pentagon around gambia
pentamidine is reserved for 1st stage t.b. gambiense infections ONLY
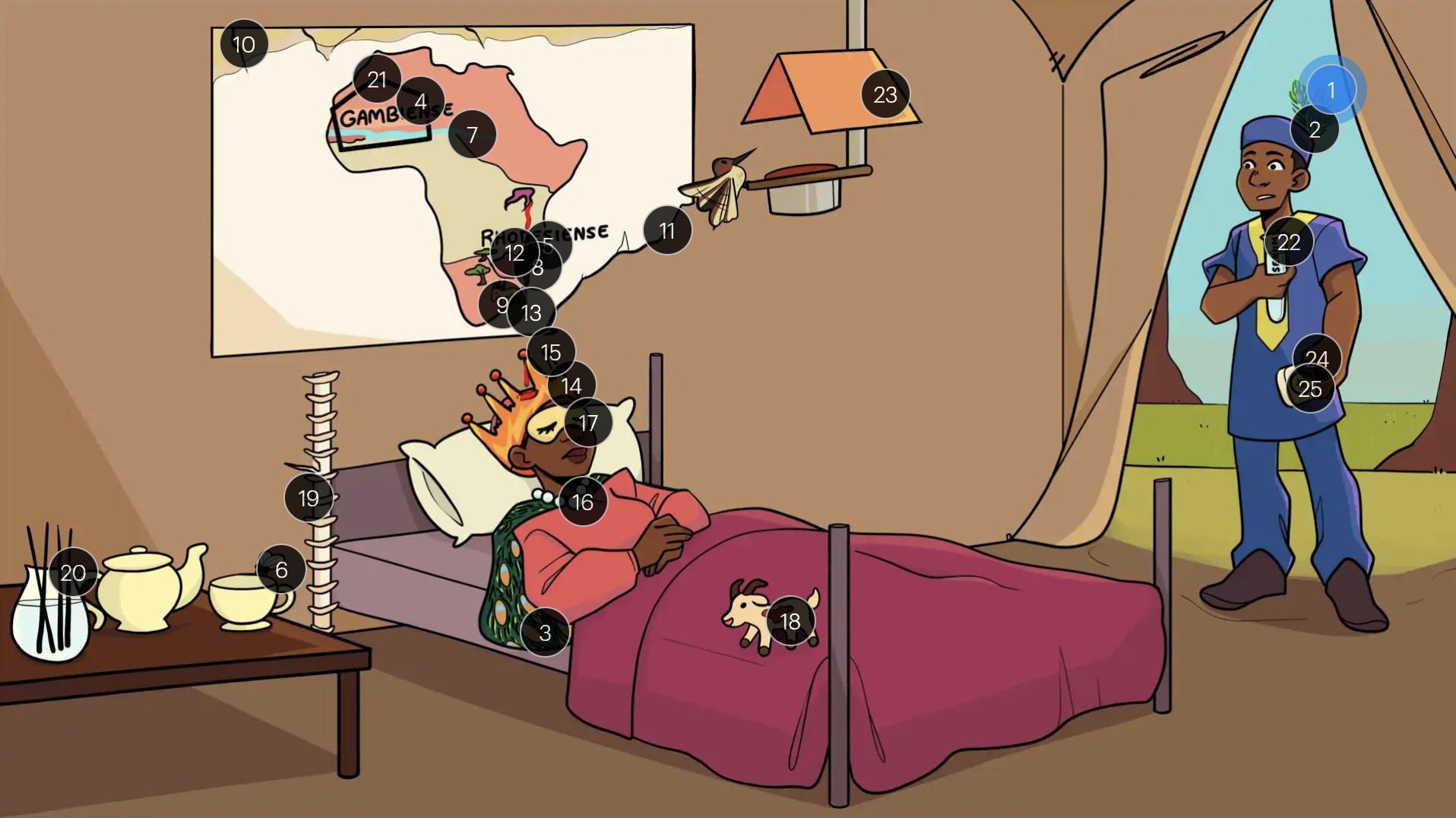
Trypanosoma brucei
#22 serum
suramin is reserved for 1st stage t.b. rhodesiense infections ONLY
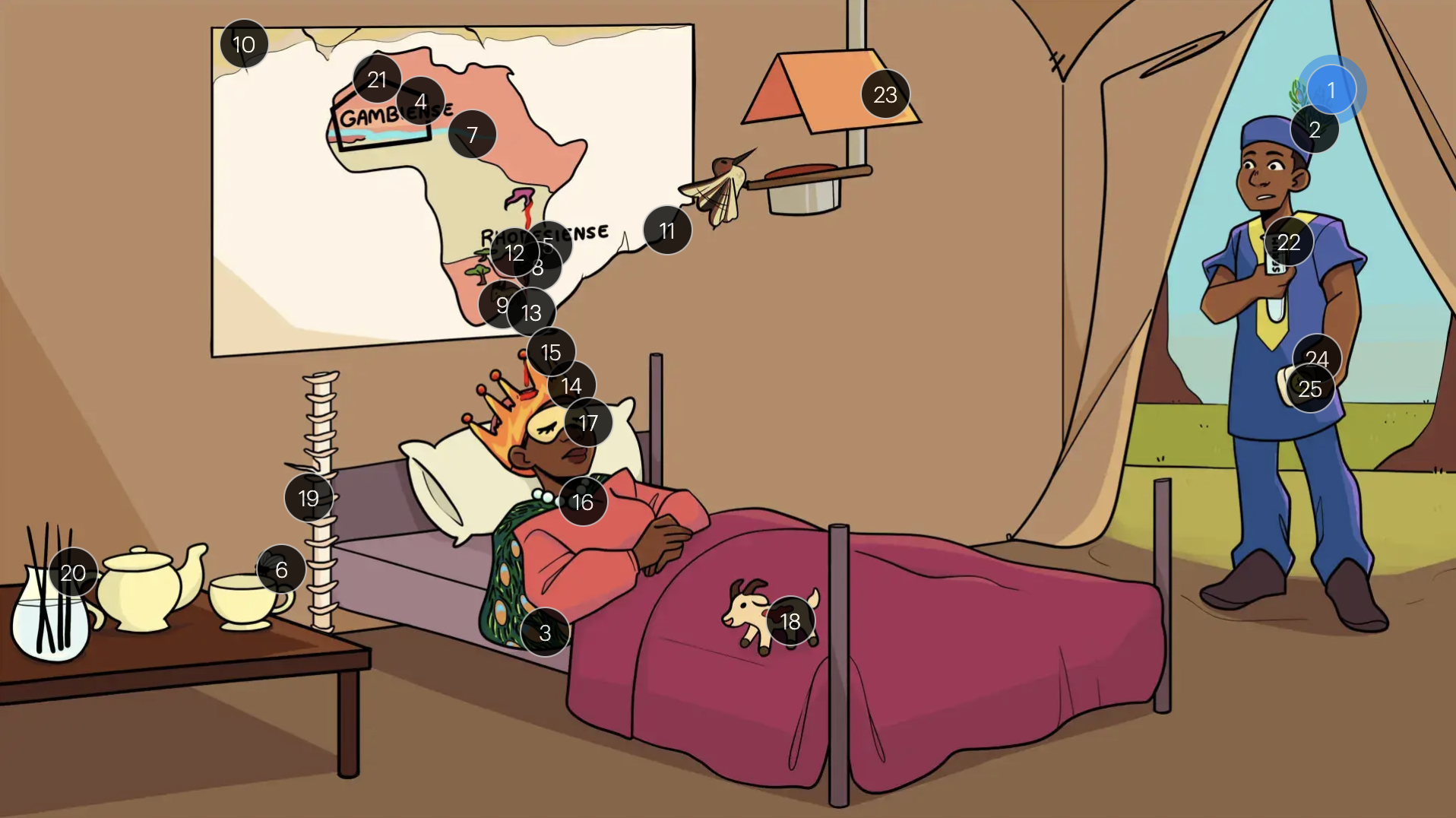
Trypanosoma brucei
#23 hummingbird feeder near gambia
NECT (2nd stage t.b. gambiense infections only!)
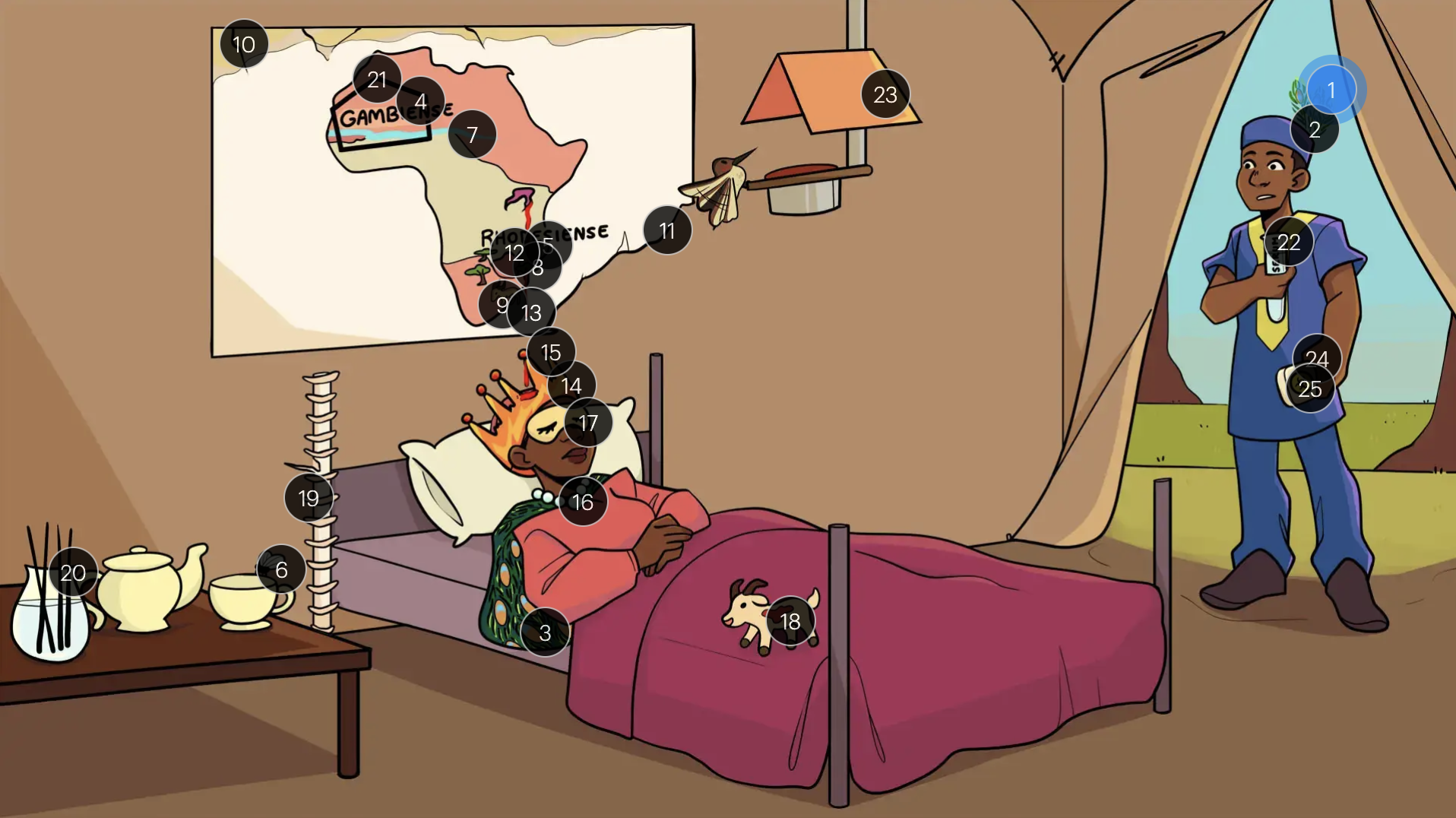
Trypanosoma brucei
#24 soap
melarsoprol is reserved for 2nd stage t.b. rhodesiense infections
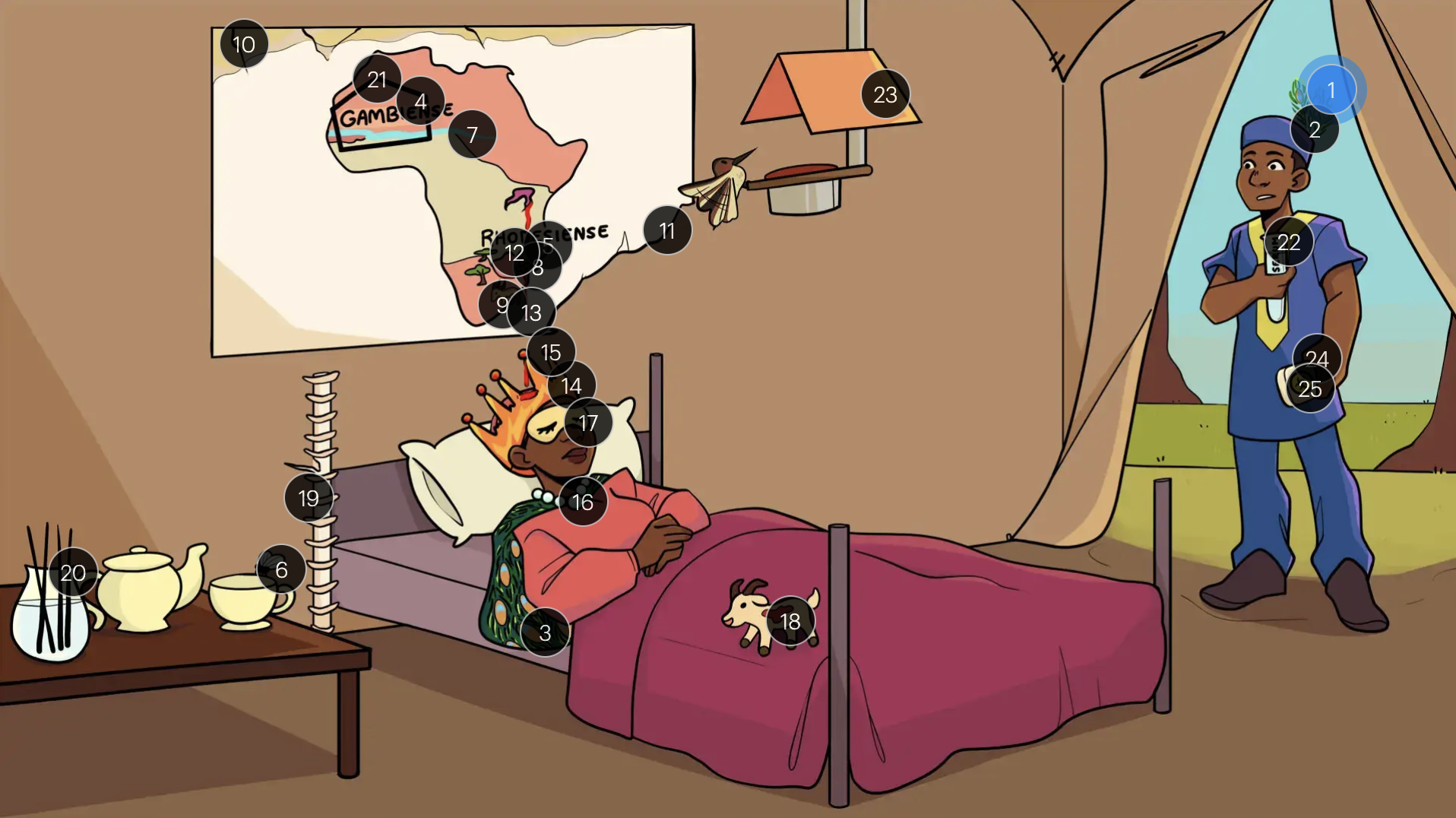
Trypanosoma brucei
#25 toxic soap
melarsoprol is a highly toxic treatment for 2nd stage sleeping sickness (thus, NECT is preferred for t.b. gambiense)