Bovine Reproduction and Neonatal Care Flashcards
1/49
Earn XP
Description and Tags
Flashcards about bovine reproduction, neonatal care, and associated diseases, based on lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Cattle Reproduction
To maintain productivity, cattle should produce a live calf every year.
Any losses, whether during gestation or beyond parturition, represent a significant economic loss to the producer
Success of producing a healthy calf depends on successful reproduction from conception to delivery
Leading causes of death in newborn calves
Starvation and hypothermia.
Type of estrous cycle in cattle
Year-round polyestrous.
Estrus cycle frequency in cattle
21 days.
Gestation period in cattle
Approximately 283 days (276 to 295 days).
Signs of Parturition
Softening of muscles/ligaments of hindquarters, swelling of vulva, mucus discharge, udder enlargement, separation from the herd.
Stage I of Parturition
6 hours on average, restless, off feed, kicking at belly, mild straining, tail raised.
Stage II of Parturition
30 minutes to 4 hours; delivery of fetus.
Stage III of Parturition
4-12 hours, expulsion of placenta.
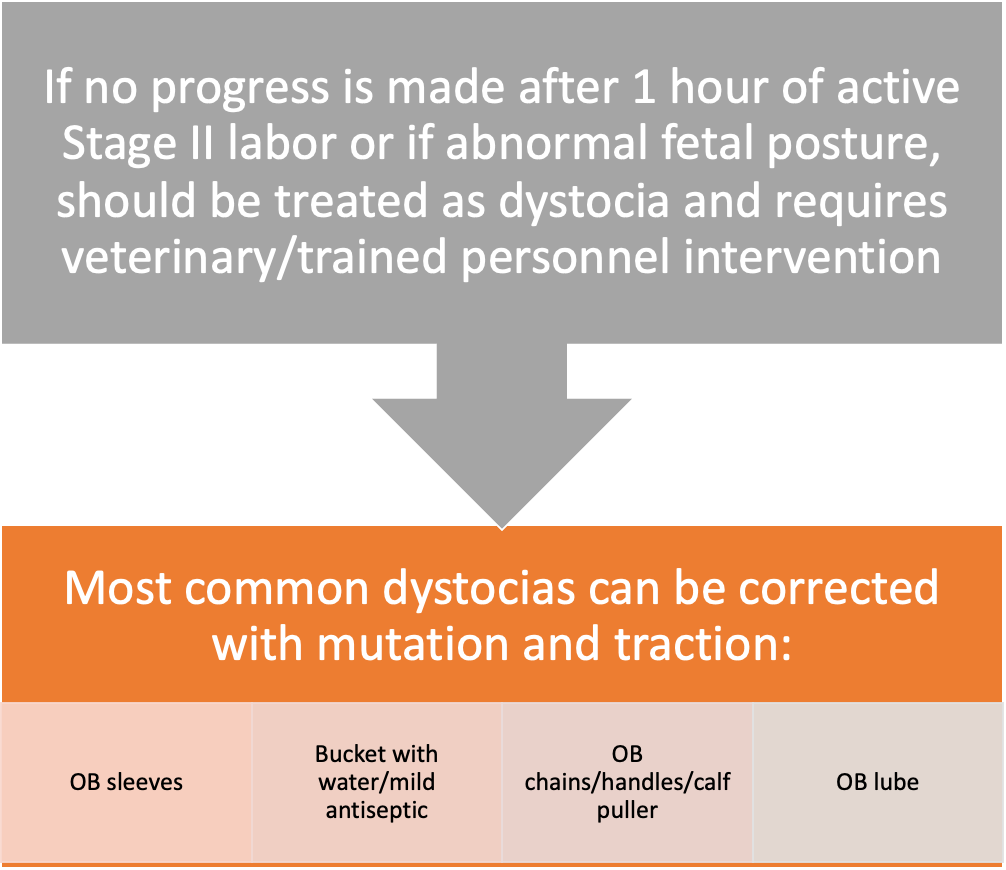
Most common dystocia correction methods
Mutation and traction with OB sleeves, lubricant, chains/handles.
Calf-puller (Calf jack) usage
Calf must be in proper position. Use gentle, steady traction in a downward direction with adequate lubrication.
If no progress after 15 minutes, needs a c-section if live calf or fetotomy if dead calf
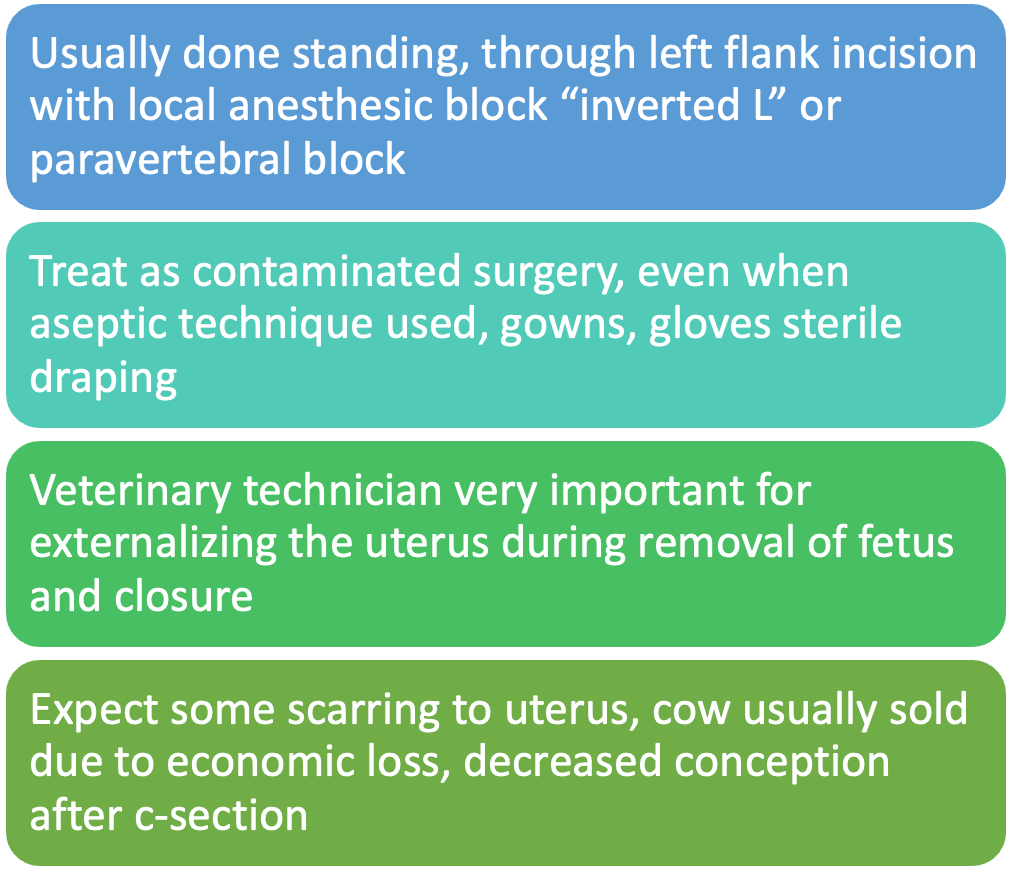
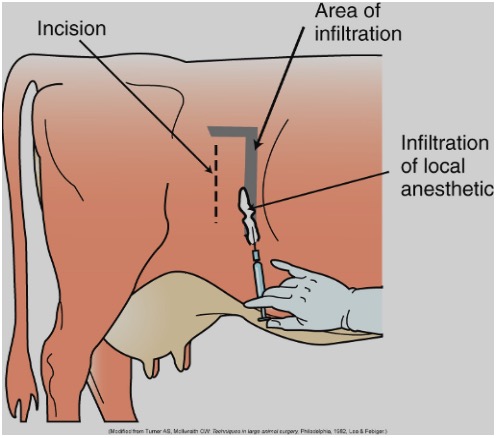
C-section procedure in cattle
Standing, through left flank incision with local anesthetic block.
Uterine prolapse cause and timing
Immediately after calving, due to excessive straining, usually with a large calf
Emergency! Uterine arteries are stretched internally to the point that the cow can bleed internally and die of cardiovascular shock within a few hours
Leave cow in pasture, keep her calm
>50% mortality- if cow lives, she should be culled
Important factors to distinguish a vaginal or uterine prolapse
Size/appearance and reproductive status.
Prolapse Repair Steps
Epidural, clean tissue, replace tissue, suture, antibiotics, culling.
Retained placenta
If not passed within 12 hours of calving.
Common in cattle- more likely to occur with dystocia, c-section, abortion, and hypocalcemia
Treatment includes antibiotics, hormone to stimulate uterine contraction/involution, uterine flushing with dilute antiseptic, +/- manual removal-can cause more trauma to uterus or leave pieces of placenta behind
Vaginal prolapse
may prolapse at any point-30-45 days prior to parturition, not pregnant, cold weather
More common in certain breeds, beef breeds more often
Not an emergency
Tend to prolapse again despitE adequate treatment
Recommend owner sell cow
Hypocalcemia (milk fever)
more common in dairy cattle
Often occurs due to a lack of calcium due to milk production; results in appetite loss, lethargy, muscle tremors.
Ketosis
exclusively seen in dairy cattle the first 6 weeks after parturition; see appetite loss and decreased milk production.
Requires IV glucose
Displaced abomasum
Exclusively seen in dairy cattle, shifts position from right side to right or left; causes appetite loss and a ping sound.
80% occur within 1 month of parturition (can occur anytime)
Appetite loss, decreased milk production, ping sound (caused by gas buildup)
Requires surgical correction
Mastitis
Inflammation of the mammary gland.
Clinical mastitis
Changes in milk quality, clinical signs evident (swollen, hot, painful quarter).
Subclinical mastitis
Clinical signs not apparent, but present and can cause decreased milk production and milk quality.
Types of bacteria causing mastitis
Contagious (passed from cow to cow during milking) and environmental (bacterial growth in bedding).
Contagious agents of mastitis
Streptococcus agalactiae, Staphylococcus aureus, Mycoplasma.
strep and staph 95%
Anatomy of the Udder
Four independent glands only interconnected by blood supply.
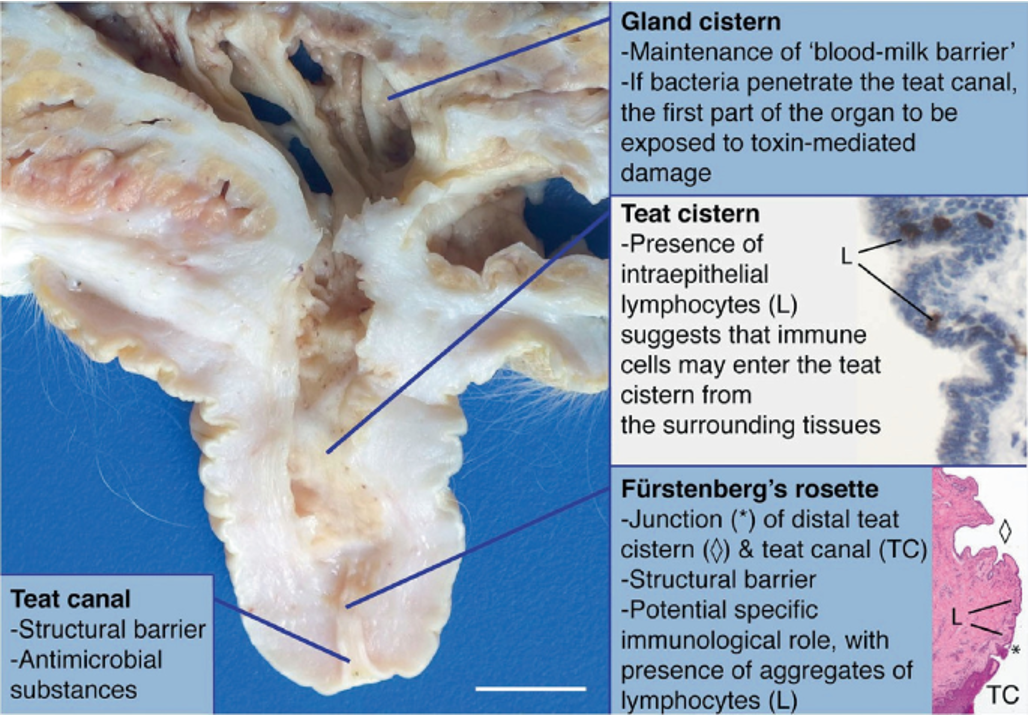
Bacteria enter through the
Teat sphincter.
Somatic Cell Count (SCC)
Under 200,000 cells/mL is acceptable; over 400,000 cells/mL is indicative of mastitis.
Milking Procedure
Known mastitis cows are milked last. Udder is cleaned, and first streams are discarded.
Pre-dipping
Dipping teats in antiseptic pre-dip to reduces bacterial counts on teats.
Post-dipping
Applying antiseptic teat dip to help seal the teat until next milking.
Most vulnerable times for environmental mastitis infections
Dry period start, just before and after calving.
Mastitis Treatment
Written, standardized protocols for various degrees of mastitis. Detailed records are a must.
Diagnosis/monitoring for mastitis
California Mastitis Test (CMT)- semi quantitative analysis for SCC-used to monitor herd for mastitis
SCC-individual cows and bulk milk may be evaluated (bulk tank should have less than 300,000 cells/mL)
Milk culture-cows that have just calved, known clinical mastitis cases, high SCC cows
Bulk tank culture
Grading of CMT results
N (Negative): Mixture remains liquid with no evidence of precipitate formation
T (Trace): Slight precipitate formed-best seen when paddle rocked gently back and forth
+1 (Weak positive): Distinct precipitate forms, but no gel forms
+2 (Distinct positive): Mixture thickens immediately with some gel formed
+3 (Strong positive): Gel is formed-sticks to cup, “jelly”
Milk Culture Procedure
Need sterile tubes/bags, pre-dip, antiseptic solution, alcohol swab, sharpie to label with animal id, farm id, date, which quarter
1. Wash hands thoroughly
2. Wash teats with antiseptic solution
3. Dry teats with individual paper towels
4. Strip each teat (discard milk)
5. Use pre-dip (as when milking-allow contact time)
6. Dry teats with individual paper towels
7. Use alcohol swab to clean teat opening starting with far teats, then near teats
8. Collect one to two squirts from each quarter in designated sterile tube or bag without touching tube/bag to teat, beginning with near teats, then far teats
9. Cap tubes/close bags immediately and adequately label each sample
10. Refrigerate tubes until shipment to lab. Processing should occur within 24 hours. If collected and cannot be sent the same day, samples should be frozen.
Newborn calf needs
Oxygenation/pulse assessment, temperature regulation, umbilical cord care, nutrition, passive transfer of antibodies, cow/calf bonding, passage of meconium, physical examination.
Neonatal care actions
Clear airway, stimulate breathing, maintain temperature, dip umbilical cord.
Oxygenation
most immediate need is to clear the airway of fluid/fetal membranes, brisk stimulation of sides of chest with towel while sternal recumbency, remove fluid from mouth/upper airway with bulb syringe
Temperature regulation
calf’s temp should be 100-102⁰F, maintain calving area in dry, draft-free location such as a barn or calving pen
Umbilical cord
should be dipped with 3% povidone iodine or 1:4 diluted chlorhexidine solution
Nutrition of newborn calf
Standing and nursing within 1-4 hours of birth. Colostrum is essential.
Two common problems in neonates
Failure of passive transfer and calf diarrhea.
Adequacy of passive transfer of antibodies
Not routinely checked due to economic costs
Serum IgG should be >1000 mg/dl
Treatment for calf diarrhea
Aggressive fluid therapy and correction of metabolic acidosis.
Cow/calf bonding
Rejection of calves is uncommon, but is more likely in first-calf heifers, twins, or calves born by c-section
Passage of meconium
First feces, should be passed within first 24 hours of life, may have to manually stimulate or give enema if no passage during first day
Neonatal Physical Exam-
“Visual” exam- from a distance-mental alertness, suckling activity, respiratory rate
“Hands-on” exam- simple TPR or systematic approach to all body systems
Neonatal Physical Examination
MM color: pale pink to pink; no petechiae or icterus
CRT: < 2 seconds
Pulse: 90-110 bpm
Respirations: 40-60 breaths per min. (moist sounds in lower airways heard immediately after birth are normal)
Suckling reflex-vigorous
Urination within first 12 hours
Defecation (meconium) within first 24 hours
Remember to check umbilical structures, joints
Calf Diarrhea
Most common cause of death in calves with diarrhea is dehydration and associated metabolic acidosis
Treatment is aggressive fluid therapy and correction of metabolic acidosis with administration of sodium bicarbonate
Hypoglycemia and electrolyte imbalances are also common side effects to calf diarrhea