Renal Plasma Flow
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
What is RPF?
Amount of plasma perfusing the kidneys per unit time, determines GFR as ↑RPF = ↑filtrate formed. Can use it to estimate renal blood flow as well.
What indicator substance would you use to estimate RPF?
Something where the mass excreted (going into urine) = mass delivered to kidneys. A good indicator is PAH (para-aminohippuric acid).
It is also freely filtered and entirely secreted
What are 2 important indicators of renal health?
RPF (renal plasma flow) and RBF (renal blood flow) but not used widely clinically.
Why is PAH a good indicator of RPF? (2)
1. Freely filtered and secreted so all gets removed in first-pass.
2. So all of it is excreted, but this is only true if you stick to normal PAH conc.
What does it mean by PAH being secreted?
20% of PAH is filtered into the Bowman's capsule
, whilst 80% of it goes into the afferent arterioles, then to the peritubular capillaries. Then actively secreted from here to the tubular fluid @ proximal convoluted tubule by transporters → then into urine
What are the issues with PAH? (2)
1. A very high PAH conc overwhelms the transporters that move PAH from peritubular capillaries to the tubular fluid, so total mass PAH excreted is not equal to total mass PAH presented to kidney.
2. PAH clearance underestimates true value of RPF by 10%.
How do you find out the total mass PAH presented to kidney?
Plasma conc x plasma vol per unit time (RPF).
What is the equation for RPF?
The original equation is:
Urine conc of PAH x Urine flow rate = Plasma conc of PAH x RPF.
Rearranged to:
RPF = Urine conc of PAH x Urine flow rate/Plasma conc of PAH.
What is the normal RPF value for PAH?
600ml/min, hence the GFR.
What is the filtration fraction?
The plasma proportion that forms filtrate, usually, 20%./0.2
FF = GFR/RPF.
120/600 = 0.2.
What is the relationship between filtration fraction and colloid osmotic Pa in peritubular capillaries?
↑FF = ↑ colloid osmotic Pa in peritubular capillaries → more tubular reabsorption. of water and solutes
What is glomeruotubular balance
kidney's ability to reabsorb a proportional amount of the glomerular filtrate and solutes that are filtered by the glomerulus- To prevent large fluctuations in fluid an electrolytes delivered to the rest of the nephron
How do afferent and efferent arteriole constriction affect GFR, RPF and FF?
Afferent arteriole constriction: ↓GFR, ↓RPF, no change in FF.
Efferent arteriole constriction: ↑GFR, ↓RPF, ↑ in FF.
How can RBF (renal blood flow) be derived?
From renal plasma flow and haematocrit (PCV).
N.B. The haematocrit is 40% as in whole blood, cells make up 40% and plasma makes up 60%.
RBF = RPF/1 - PCV.
600/(1 - 0.4) = 1L/min.
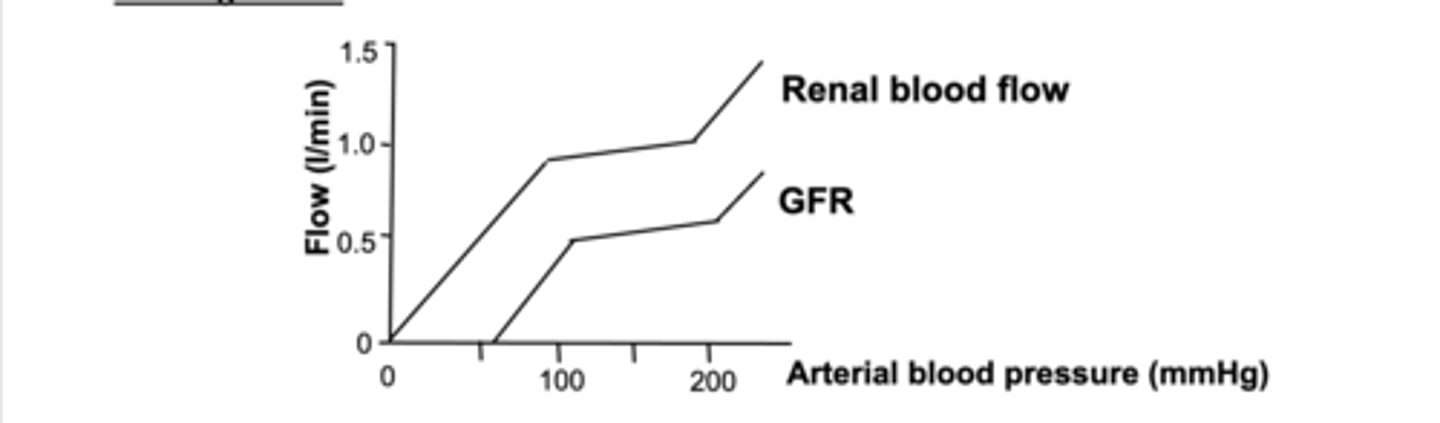
What is the autoregulation in RBF and GFR?
Changes are constant over normal arterial BPs of 90-180mmHg. This means there are uncoupled from BP (flat region of curve). Fluid and solute excretion are constant although BP fluctuates in this region.
• Without uncoupling: Higher blood pressure → more blood flow → more filtration → more urine.
• With uncoupling (via autoregulation): Kidney resists those changes and keeps filtration and urine output relatively stable over a range of pressures.
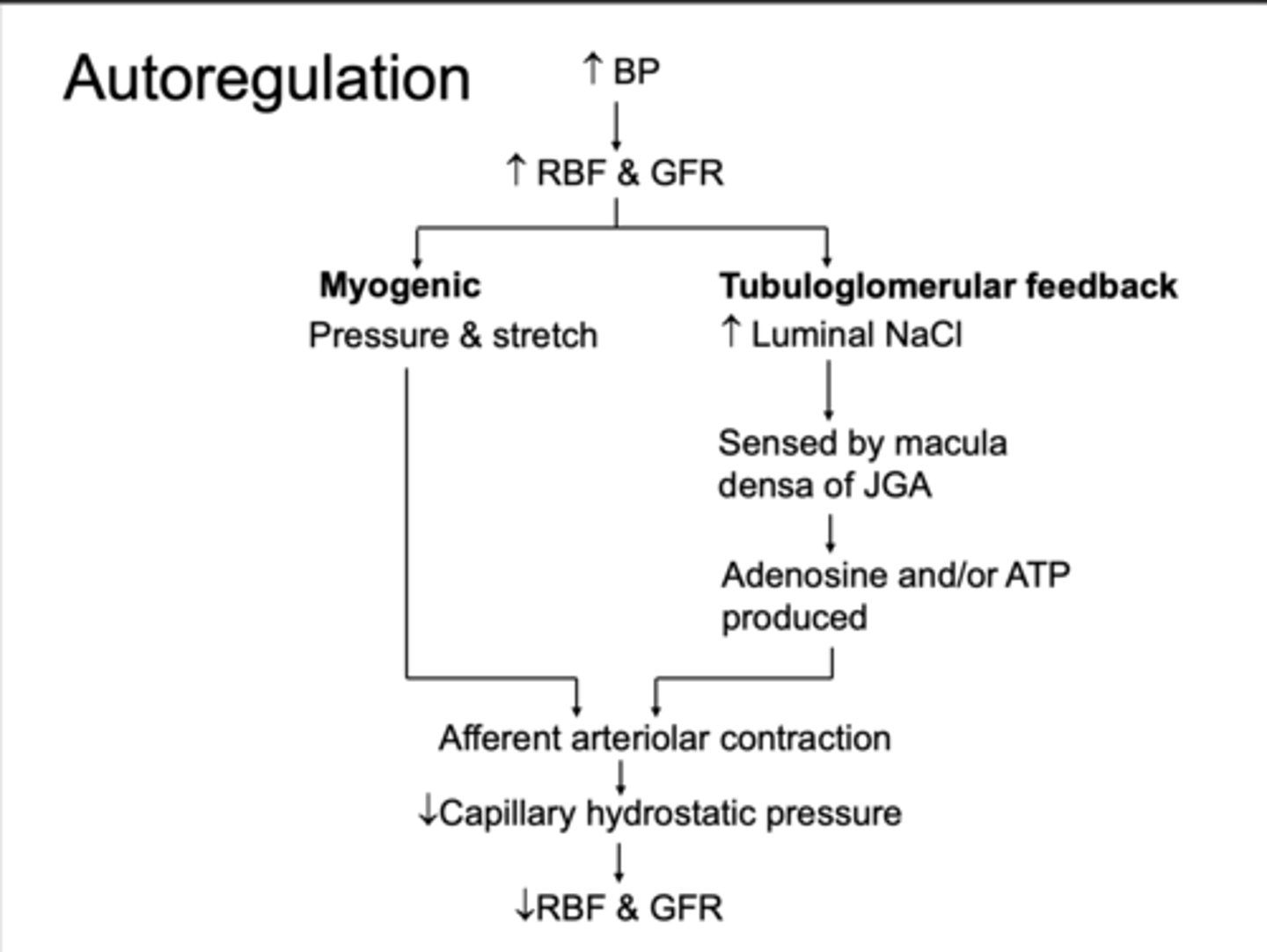
What is the mechanisms of autoregulation in RBF and GFR in terms of myogenic?
Both involve afferent arteriolar resistance.
1. Myogenic - vascular smooth muscle in afferent aa contracts is response of Pa and stretch > V-gated Ca channels open to counteract this
What is the mechanisms of autoregulation in RBF and GFR in terms of Tubuloglomerular feedback when renal perfusion pressure decreases ?
2. Tubuloglomerular feedback - ↑blood flow delivers ↑NaCl sensed by the macula densa of juxtaglomerular apparatus (sensed by cotransporters).
Adenosine signal produced → causes afferent arteriole contraction and changes GFR.
↓NaCl delivery = ↑GFR.
What is the mechanisms of autoregulation in RBF and GFR in terms of Tubuloglomerular feedback when renal perfusion pressure increases ?
Tubuloglomerular feedback - ↑blood flow delivers more NaCl delivered to JGA , adenosine from macula densa signals → afferent arteriole constrict → Decreases GFR
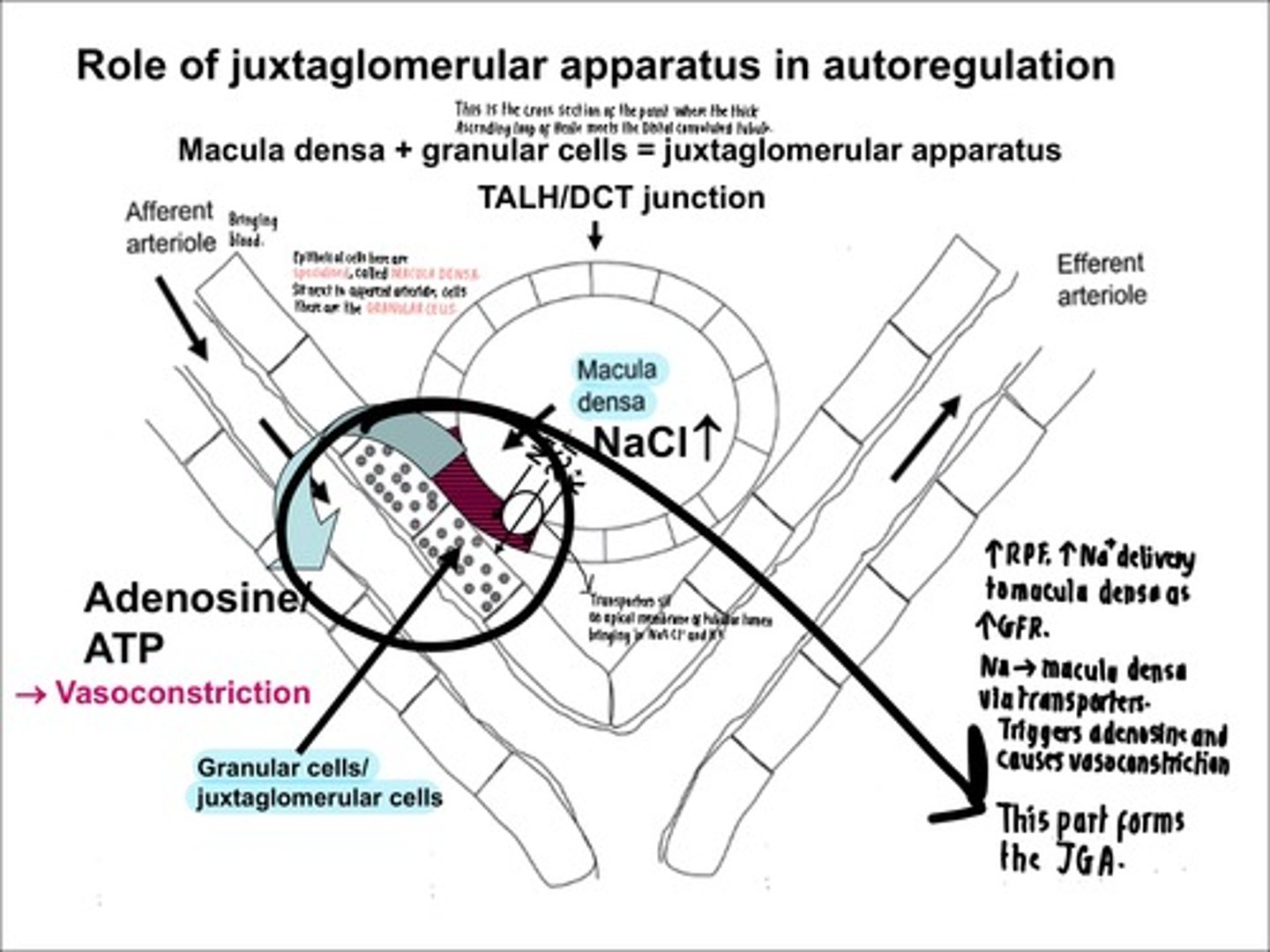
Explain the role of the JGA in auto regulation with this diagram.
Cross-section of junction where thick ascending loop of henle meets DCT.
- Epithelium of tubular lumen is specialised, called macula densa.
- Granular cells sit between the afferent aa and tubular lumen.
- NaCl transporters take in more Na when ↑GFR and ↑RPF, triggering adenosine and causing vasoconstriction of afferent arterioles.
- Reduces blood flow into capillaries, so ↓GFR and corrects high renal flow.
Overview of autoregulation OF MYOGENIC AND TUBULOGLOMERULAR FEEDBACK
What are the factors affecting RBF and GFR despite autoregulation? (2)
1. Vasoconstrictors - ↓RBF and ↓GFR (with sympathetic nn and AII)
2. Vasodilators - ↑RBF and ↑GFR with PGs (PGE2 and PGI2).
What is the effect of NSAID on vacoconstriction ?
Non-steroidal anti-inflammatory drugs (NSAIDs) inhibit prostaglandin production, which may lead to excessive vasoconstriction and potential renal damage.
Explain how meds like Angiotensin 2 can be protective in CKD
Medications like ACE inhibitors (ACEi) or angiotensin II receptor blockers (ARBs) reduce angiotensin II effects, leading to decreased GFR, which can be protective in CKD
How are vasoconstrictors activated and what happens to RBF and GFR? (3)
1. Activated by ↓BP eg/ haemorrhage.
2. Efferent aa is more sensitive to AgII than afferent aa, so it contracts in its presence, helping keep a ↑GFR during hypotension.
3. If AgII conc is too high, both afferent and efferent aa constrict, cutting off RBF and reduce GFR to protect brain.
How are ACEi and ARB renoprotective?
Block effects of AGII, so less efferent aa constriction and ↓GFR, protecting kidneys in hypertension.
How are vasodilators activated and what happens to RBF and GFR? (3)
1. By prostaglandins, in response to inflammation.
2. Dampen sympathetic nn and AgII effects from vasoconstriction, preventing severe vasoconstriction.
3. This increases RBF and GFR.
What is the clinical relevance of NSAIDs and COX inhibitors on renal vasoconstriction?
Taking them blocks PG synthesis, so interferes with RBF. If taken when there is ↓RBF, XS vasoconstriction and ischaemia > renal tubular necrosis.
What is glycosuria?
Normally 100% glucose is reabsorbed at proximal tubule with transporters. But if renal threshold for glucose is increased, then transported get overwhelmed and glucose is excreted in urine.
Which conditions can cause glycosuria? (6)
1. Untreated diabetes mellitus
2. Hyperthyroidism
3. Pregnancy
4. Drugs
5. Fanconi syndrome
6. Familial renal glucosuria.
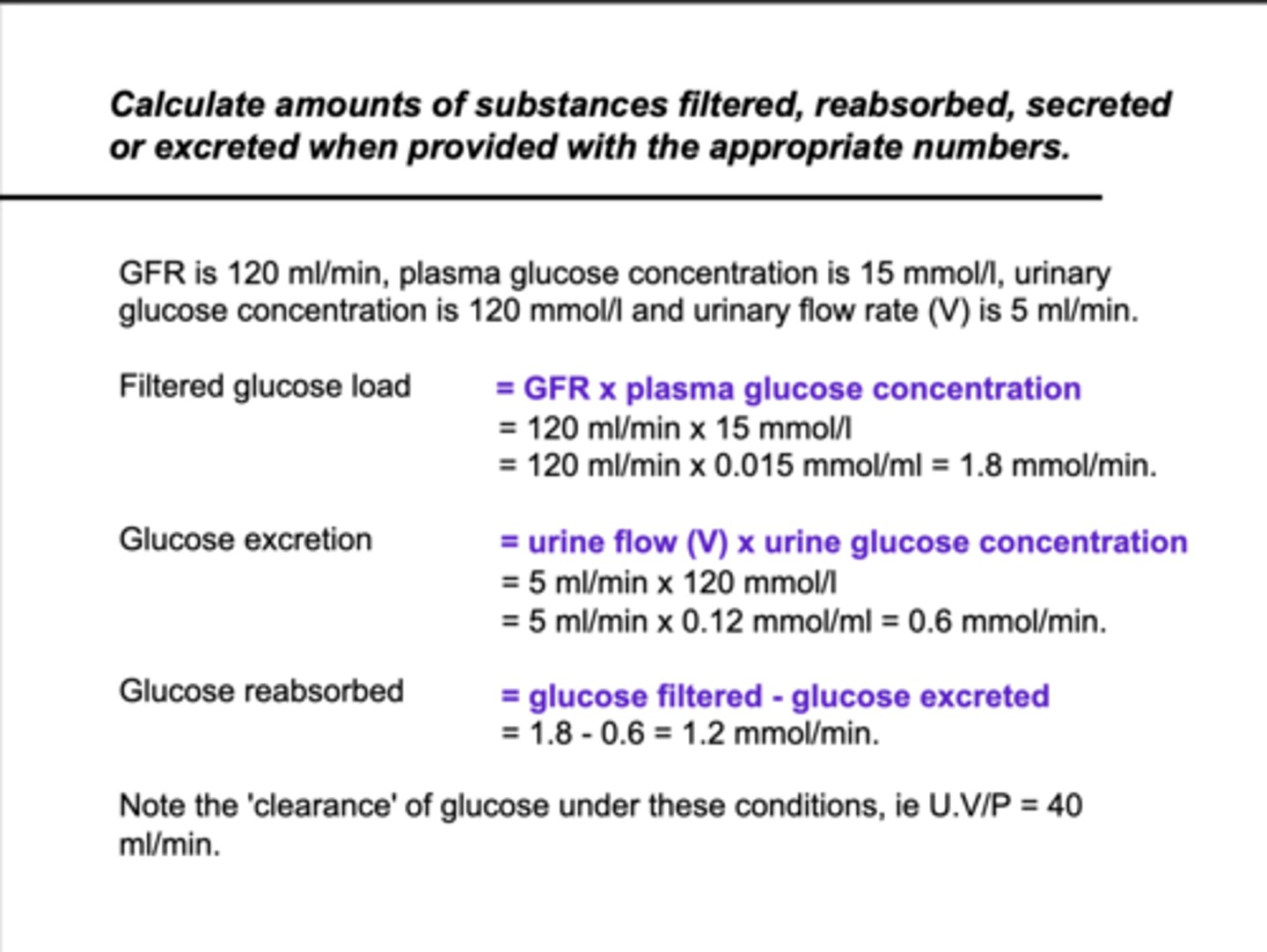
How do you calculate filtered glucose load?
The glucose filtered at glomerulus initially.
GFR (ml/min) x plasma glucose conc (mmol/ml).
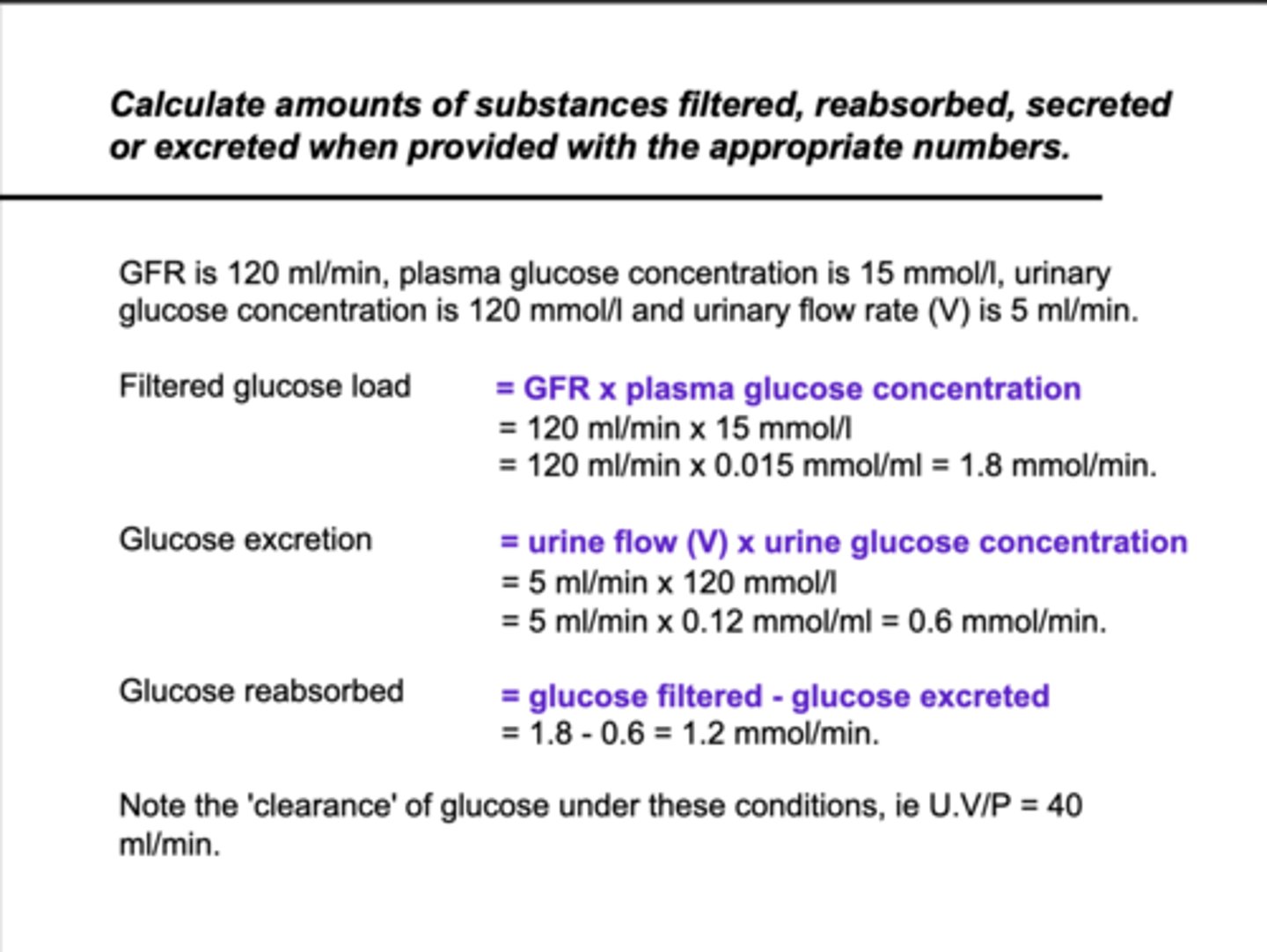
How do you calculate glucose excretion?
How much glucose is excreted.
Urine flow (V) x Urine glucose conc.
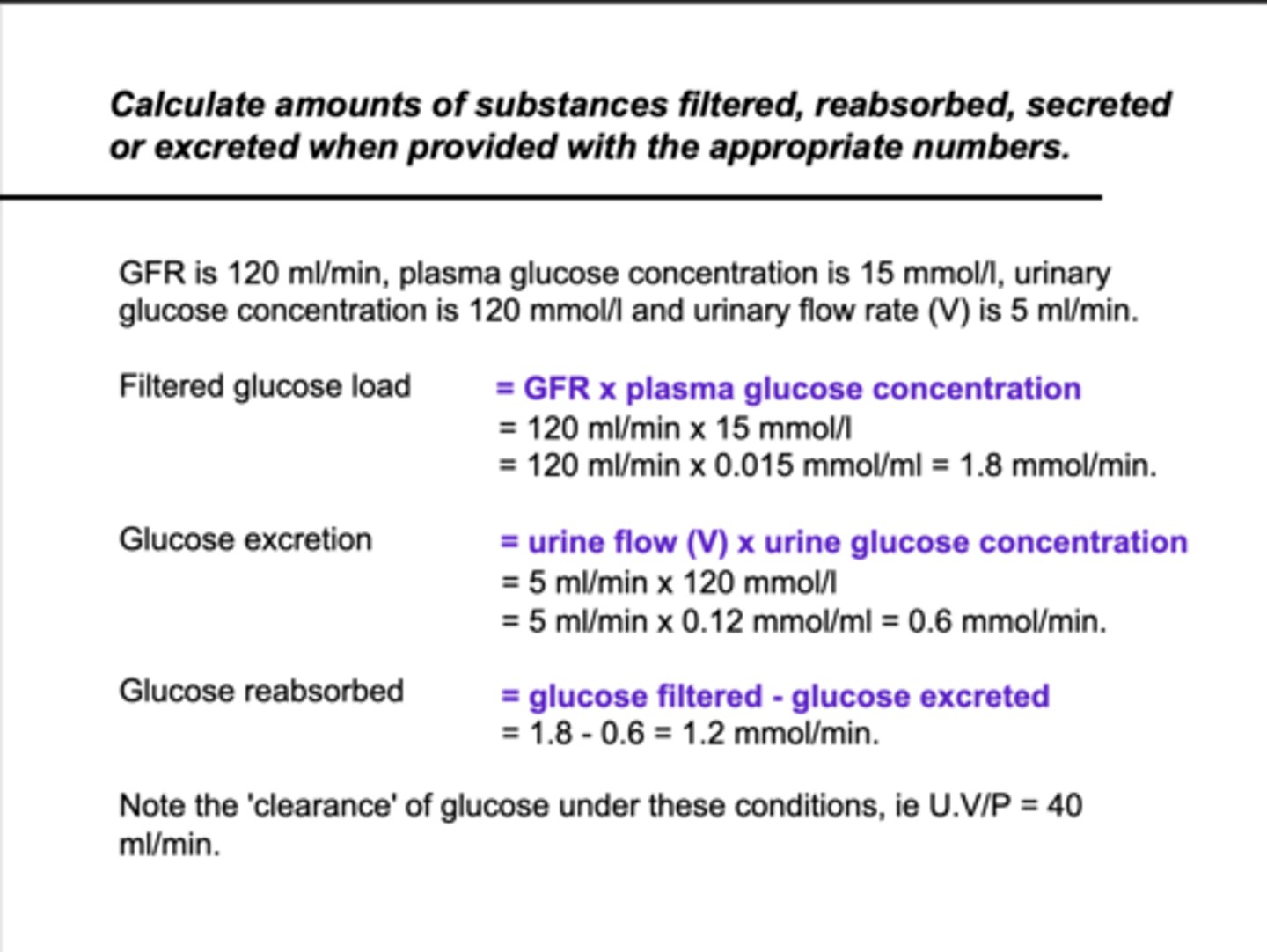
How do you calculate glucose reabsorbed?
Glucose filtered - glucose excreted.
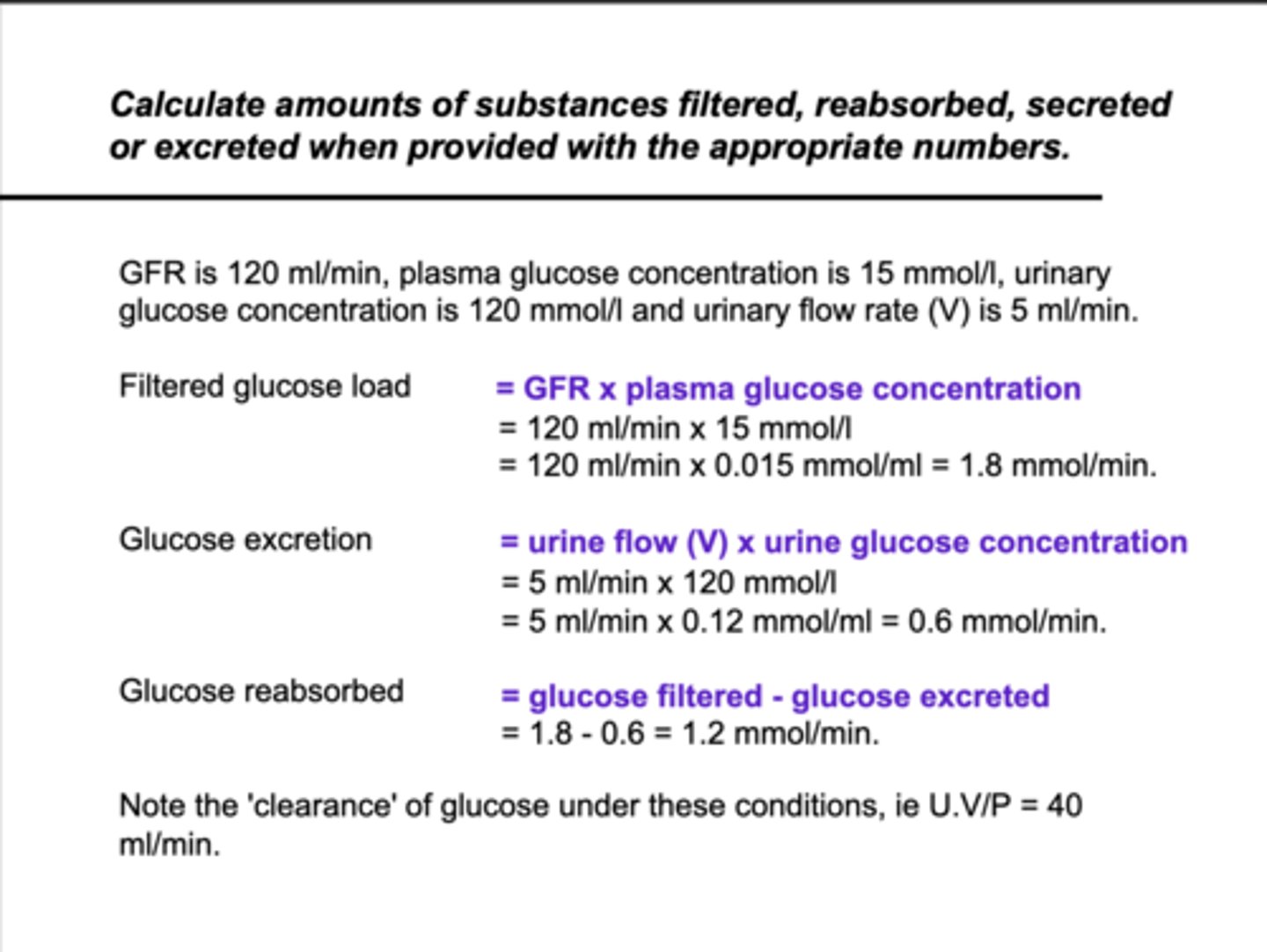
How can you work out the glucose clearance?
Glucose clearance = Urine conc of glucose x Urine flow rate/Plasma glucose conc.