Introduction to clinical health psychology
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
What is clinical health psychology?
it is rooted in a strong scinetific evidence base and encompass a breadth of inputs to support optimal healthcare provision and improve clinical outcomes.
What does clinical health psychology aim to do?
To provide psychologically informed care pathways, including psychologically informed environments and trauma informed care.
it may offer certain inputs to achieve this. these will include providing speciality needs assessment care planning and delivery of interventions usually within an multidisciplinary care context, to affect positive change for patients.
How is this done?
•A speciality, field and approach which addresses the psychological, social, cultural and biological factors as applied to physical health and wellbeing
•Applying knowledge in medicalised contexts
•Familiarisation with psychosocial dimensions of health
•Familiarisation with health-related behaviour
•Utilising knowledge of cognitive, social and clinical processes’ impacts on health behaviours to understand/address illness, injury and disability
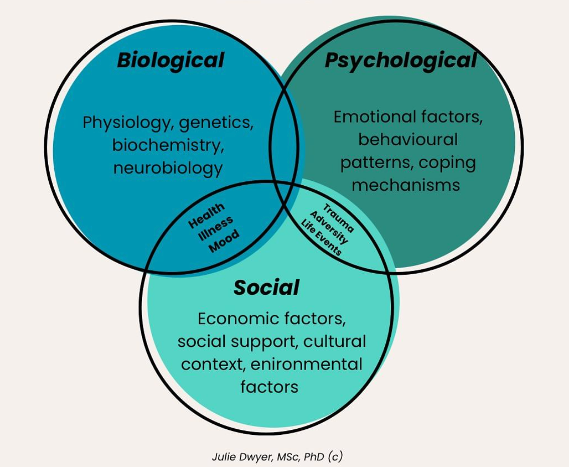
What is the Biopsychosocial model?
a holistic health framework recognizing that health and illness arise from the complex interplay of biological (genetics, disease), psychological (thoughts, emotions, beliefs), and social (family, community, culture, socioeconomic factors) elements, moving beyond a purely biomedical view to understand the whole person and achieve better, person-centered care
physical problems such as unstable blood sugar, shortness of breath incotience, visible scars etc. can adversely impact on psychological wellibeing and social integration e.g., comorbid depression or anxiety.
Therefore, patients with long-term conditions may have unmet needs for psychotherappy, psychoeducation and social support.
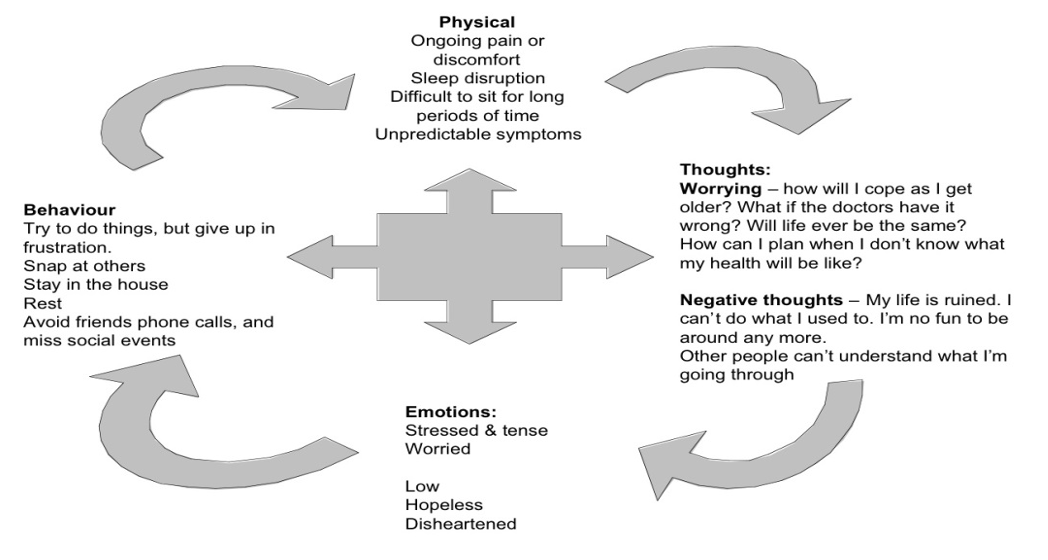
What is a vicious cycle?
If these needs are unmet, and symptoms are unpredictable- this might affect their thoughts making them more negative.
Unable to plan because of their unexpected situations
Negative thoughts about self
Negative emotions- impact behaviour
what are psychosocial problems in biopsychosocial model?
psychosocial problems such as depression, anxiety, embarrassment, shame, uncertainty etc, can adversely impact on physical status directly- e.g., psychoneuroimmunological pathways. indirectly e.g., poor adherence to treatment, unwilling to report worsening symptoms to get help.
What is the delivery of clinical health psychology?
Usually offered in acute settings and primary care, increasing public.
services may specialise according to age (e.g., peadiatrics) or conditions (e.g., cardiology).
What is MS?
A chronic neurological conditions affecting the brain and spinal core.
Common responses to the diagnosis
Anger
Anxiety
Frustration
Helplessness
Hopelessness
Irritability
Physical impacts
Resentments/envy
Sadness
Stress
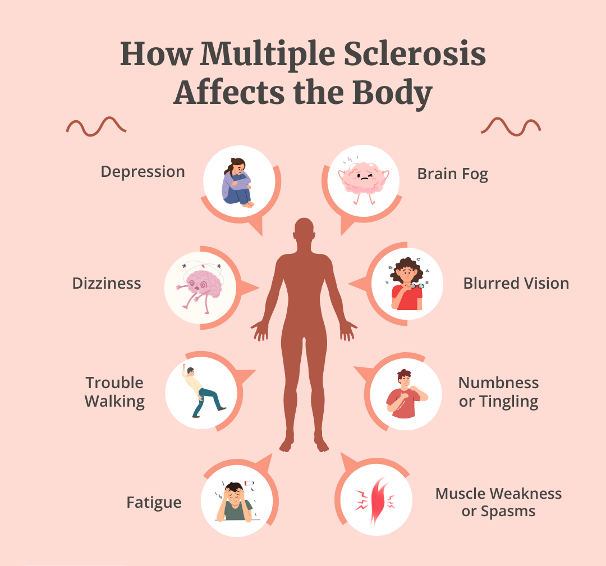
What will affect the impact of diagnosis?
• Diagnosis (how, when, meaning)
• Point in life cycle
• Adjustments
• Treatments (or their absence)/concordance
• Side-effects/iatrogenesis
• Co-morbidities
• Palliation
• End of life
What might a clinical health psychologist see?
Clients with health anxiety
Clients with unexplained physical syptoms
Clients with diagnosed health problems (cardiovascular, diabetes, cancer, pain, renal, dermatological, neurological, disfigurement, sexual)
Staff (delivering care and its impact)
The system (primary/secondary/tertiary/preventative)
how to work with adult clients who are ill?
• Making sense of the condition
• Accommodating change
• Time of life
• Impact on self-identity
• Impact on couple/systems
• Losses and gains
• Impact of gender/ethnicity/religion/community beliefs or other protected characteristics
• Impact of caregiving
• Stigma
• Maintaining dignity and QoL
How might you approach domains to explore?
telling the tale/sharing the story of illness.
reducing the pace
normalising the impact of illness
considering its emotional impacy
meanings of illness and/or disability
impact on relationship
impact on lifestyle
What is the process whilst assessing?
respecting the individual’s agency/family authority
addressing misunderstandings
addressing communication issues with/out family.
identifying rescourses
preparing for the future
What are the models of working?
all the main therapeutic models can be applied to working in clinical health settings, growth of 3rd wave approaches e.g., CFT, ACT.
Irrespective of theoretical orientation, psychoeducation is important.
specific health psychology models should be able to inform assessment, formulation and interventions.
What are illness perceptions?
They provide patients with a framework or schema for coping with and understanding their illness.
these perceptions/ beliefs are influenced by a range of factors:
information presented by healthcare professionals
prior experiences with the illness
information gained with the illness
information gained from the social context
cultural beleiefs.
these beliefs are that they have a significant impact on the behaviours an individual uses to cope and manage their illness and therefore on outcomes including both clinical and quality of life.
What is the model of illness behaviour?
Illness perception stand to be discussed in terms of the self-regulatory model.
self-regulation is a dynamic process in which the individual attempts to preserve the sense of self and to solve the problems of what is happening to their health.
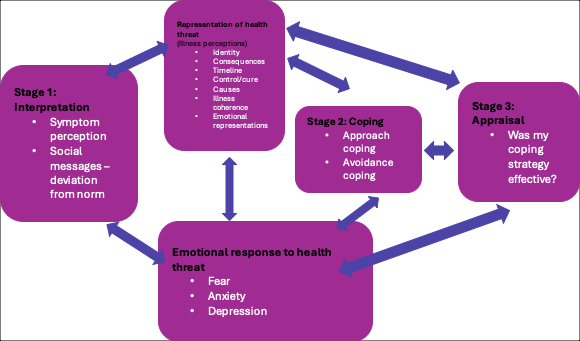
What is the regulatory model?
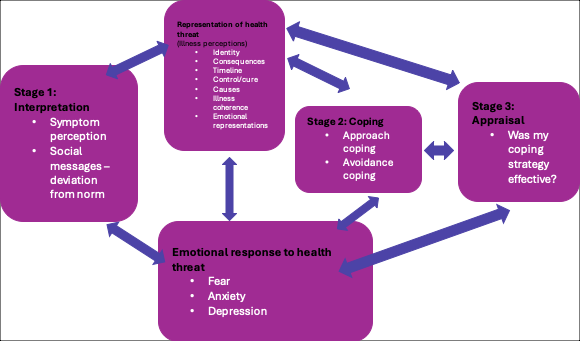
What is illness representation?
•Identity:The label given to the illness (medical diagnosis) and the symptoms experienced.
•Consequences: Patients’ perceptions of the possible effects of the illness on their life. These may be physical, emotional or a combination of factors.
•Timeline: Beliefs about how long the illness will last, whether it is acute or long-term.
•Control/cure: Beliefs about whether the illness can be treated and cured, and the extent to which the outcome of their illness is controllable either by themselves or powerful others (e.g., doctor).
•Causes:Perceived causes (biological or psychosocial).
•Illness coherence: Comprehension or understanding of the illness
•Emotional representations: Perception of negative emotions generated by the illness
how can we elicit illness perception?
• Measure using IPQ-R (Moss-Morris et al., 2002)
• Ask questions during consultations
how can we address illness perception?
• Self-management programmes
• Rehabilitation programmes
• Behaviour change techniques (BCTs)
• CBT
• Providing psychoeducation/information
What are three approaches in coping with illnesses?
coping with the crisis of illness
adjustment to physical illness
benefit finding:post traumatic growth
What is the crisis theory?
Relates to grief and mourning of change after crisis.
the coping process: cognitive appraisal, adaptive, coping skills
What are the cognitive adaption theory?
Adjusting to threatening events
the coping processes: search for meaning, search for mastery, process of self-enhancement.
What is post traumatic growth?
Previous theories focus on return to ‘normality’ but that is often something that is lost and has a negative focus
PTG based in positive psychology
Although some negative consequences for lifestyle and quality of life, people can consider life to have improved
Silver Lining Questionnaire (Sodergren et al, 2002)
Positivity can be improved by rehabilitation
What makes people more likely to adhere to treatment?
perception of symptoms
belief of its seriousness
belief in treatment
family and social input
What is health and health behaviour?
health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.
recent definitions include, cultural, psychosocial, and economic elements.
health and illness are two countries. if we’re lucky we live in the world of leath, but we all hold passports to the world of illness.
What are the determinants of health?
• Although some of the variations in older people’s health are genetic, most is due to people’s physical and social environments – including their homes, neighbourhoods, and communities, as well as their personal characteristics – such as their sex, ethnicity, or socioeconomic status. The environments that people live in as children – or even as developing fetuses – combined with their personal characteristics, have long-term effects on how they age.
• Physical and social environments can affect health directly or through barriers or incentives that affect opportunities, decisions and health behaviour. Maintaining healthy behaviours throughout life, particularly eating a balanced diet, engaging in regular physical activity and refraining from tobacco use, all contribute to reducing the risk of non-communicable diseases, improving physical and mental capacity and delaying care dependency.
• Supportive physical and social environments also enable people to do what is important to them, despite losses in capacity. The availability of safe and accessible public buildings and transport, and places that are easy to walk around, are examples of supportive environments. In developing a public-health response to ageing, it is important not just to consider individual and environmental approaches that ameliorate the losses associated with older age, but also those that may reinforce recovery, adaptation and psychosocial growth.
What are interventions?
Adjustment- CFT
Managing stress, distress, anxiety and depression- CBT, CFT, family therapy, stress/anxiety management
improving and maintaining cognitive function- cognitive stimulation Therapy and maintenance CST.
maintaining quaity of life- cognitive stimulation therapy (CST) and maintenance CST.
What is cardiovascular disease?
• Up to 80% of premature CVD deaths are preventable.
• High blood pressure, high cholesterol, diet, obesity, physical inactivity, smoking and air pollution explain the vast majority of CVD, and in some cases exposure to these risk factors is increasing.
• Action on the wider socio-economic determinants of health also plays a role in reducing CVD. For example, living in cold homes, low income, debt or poor-quality housing, increases the risk of heart attack or stroke.
What are the interventions?
cardiac rehabilitation- BACR specify need for psychologist to be part of cardiac rehab team.
self-management support intervention
MBSR- self-efficacy and quality of life of cardiovascular patients could be improved by providing an MBSR program.
CBT: cognitive behavioural therapy seems to be an effective treatment for reducing depression and anxiety in patients with CVD and should be considered in standard clinical care.
risk factors of Cancer?
obesity and alcohol the risk of several types of cancer; these are the most important nutritional factors contributing to the total burden of cancer worldwide.
stopping smooking, reducing alchol consumption, enagaing in physical activity, improving diet and reducing excess weight can all reduce the risk of cancer.
the incidence of cancer is also associated with deprivation with greater prevalance in more deprived areas.
Interventions for cancer…
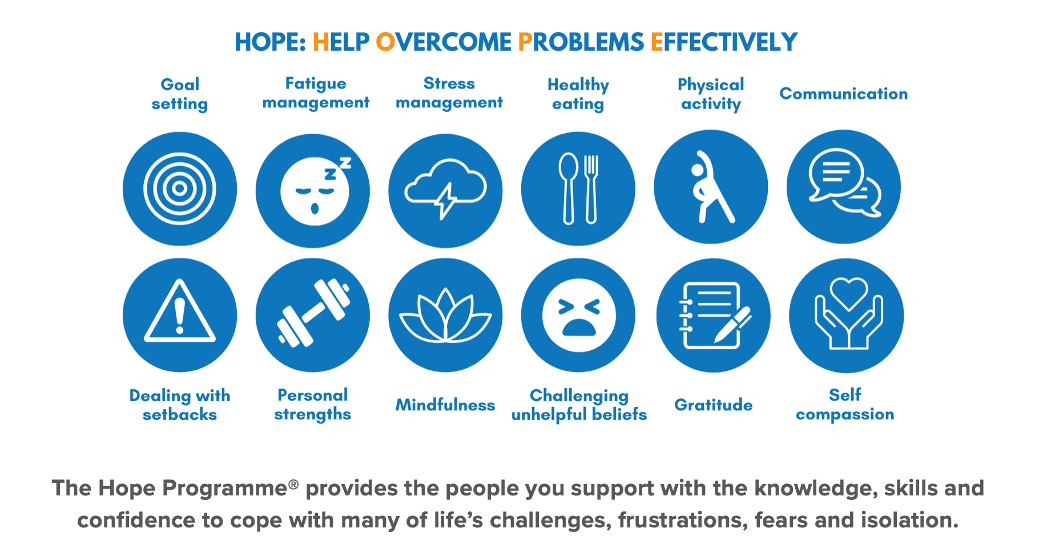
• HOPE Programme
• Other self-management support programmes
• Park et al., (2019): Results suggest psychosocial interventions (e.g., meaning-focussed group therapy, MBSR) are associated with small-to-medium effects in enhancing meaning/purpose among cancer patients, comparable benefits to interventions designed to reduce depression, pain, and fatigue in patients with cancer.
• Saur et al., (2024): Recent meta-analyses and reviews suggests that ACT interventions are an effective and evidence-based treatment for increasing HRQoL and reducing psychological distress in patients with cancer.
How is smoking a mediator?
• Smoking is the leading cause of preventable ill health and death in England, and a significant contributor to inequalities in life expectancy. It is also the single biggest avoidable cause of death and disability in developed countries.
• It puts people at high risk of developing cancer, cardiovascular and respiratory diseases, and was responsible for nearly 75,000 deaths and more than 500,000 hospital admissions in England in 2019 (Health Foundation, 2020).
• Smoking increases as SES diminishes - although reduction in overall prevalence, masks relative static use in socially disadvantaged groups.
How is exercise/physical activity a mediator?
•Physical activity can help to prevent and manage overweight and obesity and protect against a range of noncommunicable diseases including cardiovascular disease and diabetes.
•Has positive effects on mental health and can support social inclusion.
•In 2019, an estimated 10,000 deaths were attributable to low physical activity. Although the relative impact on morbidity and mortality is lower for physical activity than poor diet, increased physical activity provides additional benefits, including prevention of falls and fractures (Health Foundation, 2020).
•Obstacles – time, lack of support/norms, self-image, energy, skill, fear of injury, resources
How is alcohol a mediator?
Alcohol consumption can negatively impact nearly every organ in the body, causing liver disease, heart disease, cancer, and mental health problems. It was the main reason for 320,000 hospital admissions in 2019/20, with 6,984 alcohol-specific deaths in England in 2020, a 20% increase on the previous year.
• Harmful alcohol use also has a significant social impact, increasing the risk of accidents, violence, child neglect and antisocial behaviour (Health Foundation, 2020).
What are other practical factors/ considerations as a clinical psychologist assessment and obstacles?
legitimacy (end of road, scrutinised, medical context)
engagement/wariness particularly if referral poorly communicated.
physical difficulties (where and when seen)- what of the acute setting?
therapist potentially feeling overwhelmed since not their domain, yet need familiarity with medical terminology.
expertise of an individual/family.
Other Practical factors/considerations as a clinical health psychologist- Healthcare settings?
Ensure able to preserve client:
Dignity
Privacy
Confidentiality
To foster honesty, trust and compassion
How to establish a rational?
acknowlegde the medical route of referral and consider/shape role of pscyhologist
establish nature, history, impact of health problems thoroughly
acknowledge rality of patients experiences since may have been dismissed
normalise the referral
explore links between health and psychological factors which are acceptable to the patient,
remember language
What are further important considerations?
Be flexible in timing and negotiate movement during session if discomfort/fatigue an issue. Invite clients to let you know of discomfort. Consider how/what you modify if at bedside.
Seek to structure and prioritise problems – physical and broader psychosocial issues.