Oral environment: saliva and bacterial plaque
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Saliva
Not distributed to gingiva and anterior and the middle of hard palate. Saliva secreted in oral cavity is sterile, but moves to other oral regions. Mixes with a) the gingival or crevicular fluid
b) nasal discharge (paranasal sinuses, hypopharynx and larynx)
c) with food debris
d) microorganisms (and the products elaborated by them)
e) and the desquamated cells from the oral mucosa.
THIS IS KNOWN AS "MIXED SALIVA."
Saliva facts
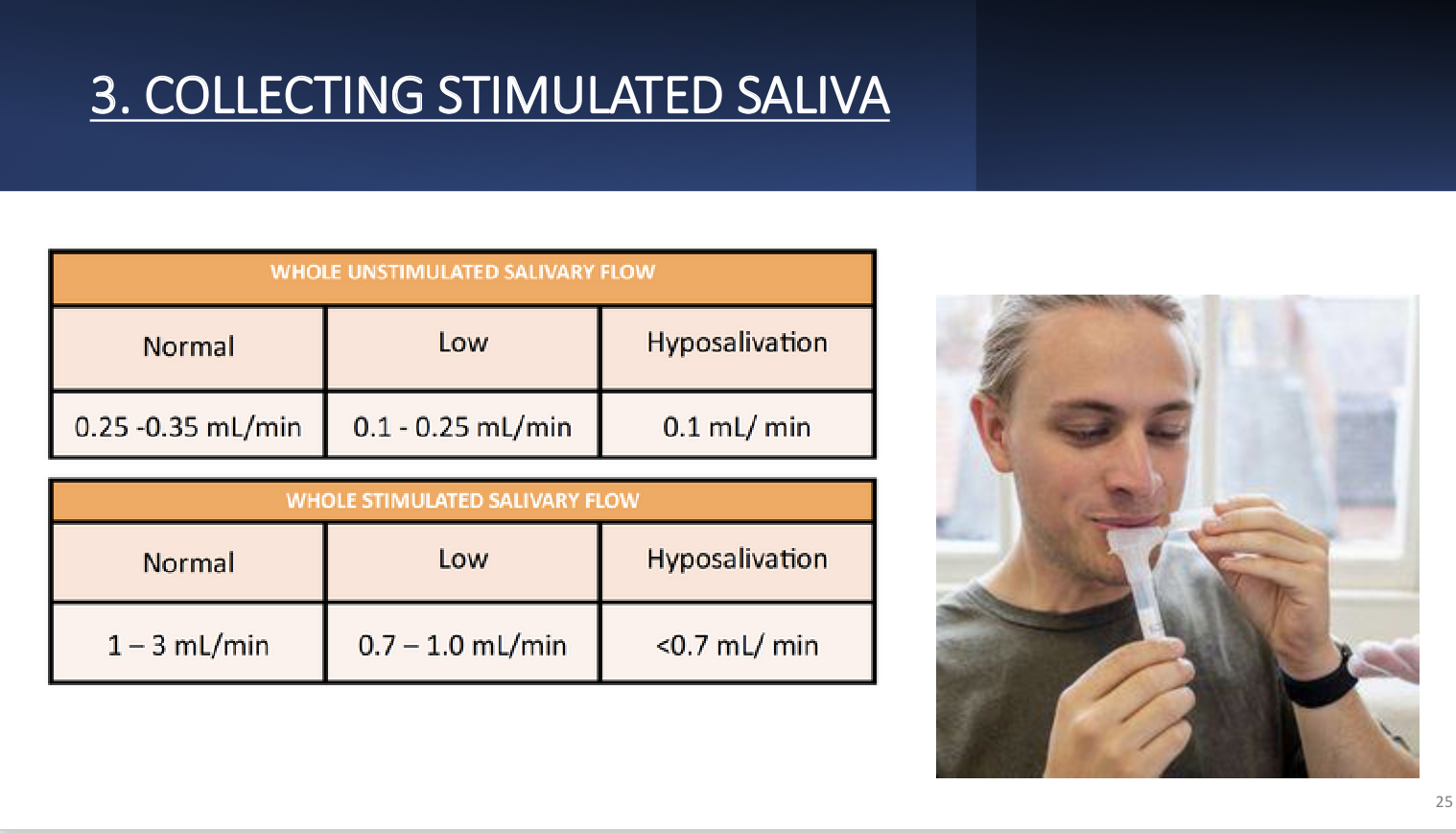
Average volume in mouth is 1.1L. Controlled by ANS. Unstimulated saliva= 0.25-0.35ml/min vs stimulated saliva being 1.5ml/min. Reaches max peak at afternoon and decreases during night rest. Wide variety of factors cause change in production.
Components of saliva
Clear, heterogenous fluid with pH 6.5-7.5 🙂 and composed of water (99%) and 1% organic and inorganic substances. moistens food, remineralizes and maintains homeostasis. Most important elements are phosphates, fluorides and calcium.
Elements of saliva
phosphates- main origin is parotids and important for precipitation of salts on tooth surface.
Fluoride ion- strong affinity for Ca2+ na promotes fluorapatite, which is more resistant to acid disorganisation than hydroxyapatite.
Calcium- comes from submandibular glands, found in stimulated saliva and good at re-mineralization.
Mineralised tissue of teeth doesn’t dissolve in saliva due to oversaturationof calcium and phosphates and hydroxyl ions.
Organic components of saliva
1. Mucus ➔ serves as a lubricant and protection for oral structures.
2. Amylase ➔ initiates the digestion of starch.
3. Lingual lipase ➔ begins digestion of fat.
4. Proteins and enzymes: statherins, proline-rich proteins, histatins, lysozymes, salivary
peroxidase, immunoglobulins, amylase, glucosidase, peptidase, glycoproteins: mucins,
carbonic anhydrase, secretory IgA, kallikrein, lactoferrin, fibronectin.
• Antimicrobial action
• Lubrication
• Buffer capacity and remineralization
5. Glucose
6. Lipids
Also rich with heterogenous proteins.
Major functions of saliva-Digestive
Forming ailmentary bolus-Thanks to the salivary flow, the movement of the muscles of the tongue, of the cheeks and of the lips, and the chewing, it favors the formation of the alimentary bolus.
Swallowing- This is lubricated by the action of water and mucins and thanks to this it facilitates the solubility of the food, which will pass into the digestive tract by a dragging mechanical action thanks to the swallowing.
Also has a major role in flavour.
Protective function of saliva
Mucosal intgrity- forms a protective covering layer over mucosa that prevents desiccation, external aggressions and penetration of irritants. In addition, favours tissue repair and prevent penetration of microorganisms.
Antimicrobial action- it seems that it is directed preferentially to temporary oral microorganisms and, in a lower degree, although not always, to the resident microbiota. It understands a large group of compounds that, in principle are those responsible for the high oral resistance to infectious processes.
Immune action- different types of immunoglobulins, like secretory IgA, that act by fixing micro-organism to their Fab portion. Not able to coloniseother structures. Immune action promoted by different inflammatory mediators.
Saliva relationship with infectious diseases
Sugar elimination- Is produced by the dilution of the sugar in the saliva before swallowing and it´s subsequent later pass to the digestive tract. This "wash"of hydrocarbonated substances from the mouth removes an important cariogenic factor by making fermentable compounds disappear.
Buffer capacity- Maintaining the salivary pH within a few normal limits is a very important function.
-If it decreases, as a consequence of the carbohydrate metabolism, it will stimulate the demineralization of the enamel and the appearance of caries.
-And on the contrary, if it increases, the alkalization will influence in the development of the plaque.
The saliva and the microorganisms present in it, have different regulators to protect themselves
from these extreme situations.
Saliva relationship with infectious diseases 2
Remineralizing capacity and regulation of the mineralization process: Incipient caries lesions can be remineralised, since saliva (especially stimulated) is oversaturated with calcium and phosphate for hydroxyapatite.
Influence on the oral microbiota: Salivary proteins and glycoproteins exert an important role, because they will be part of the acquired film, essential for the formation of the dental plaque, they stimulate the bacterial aggregation and coaggregation phenomena. And also, they are a nutritional source for the resident oral microbiota.
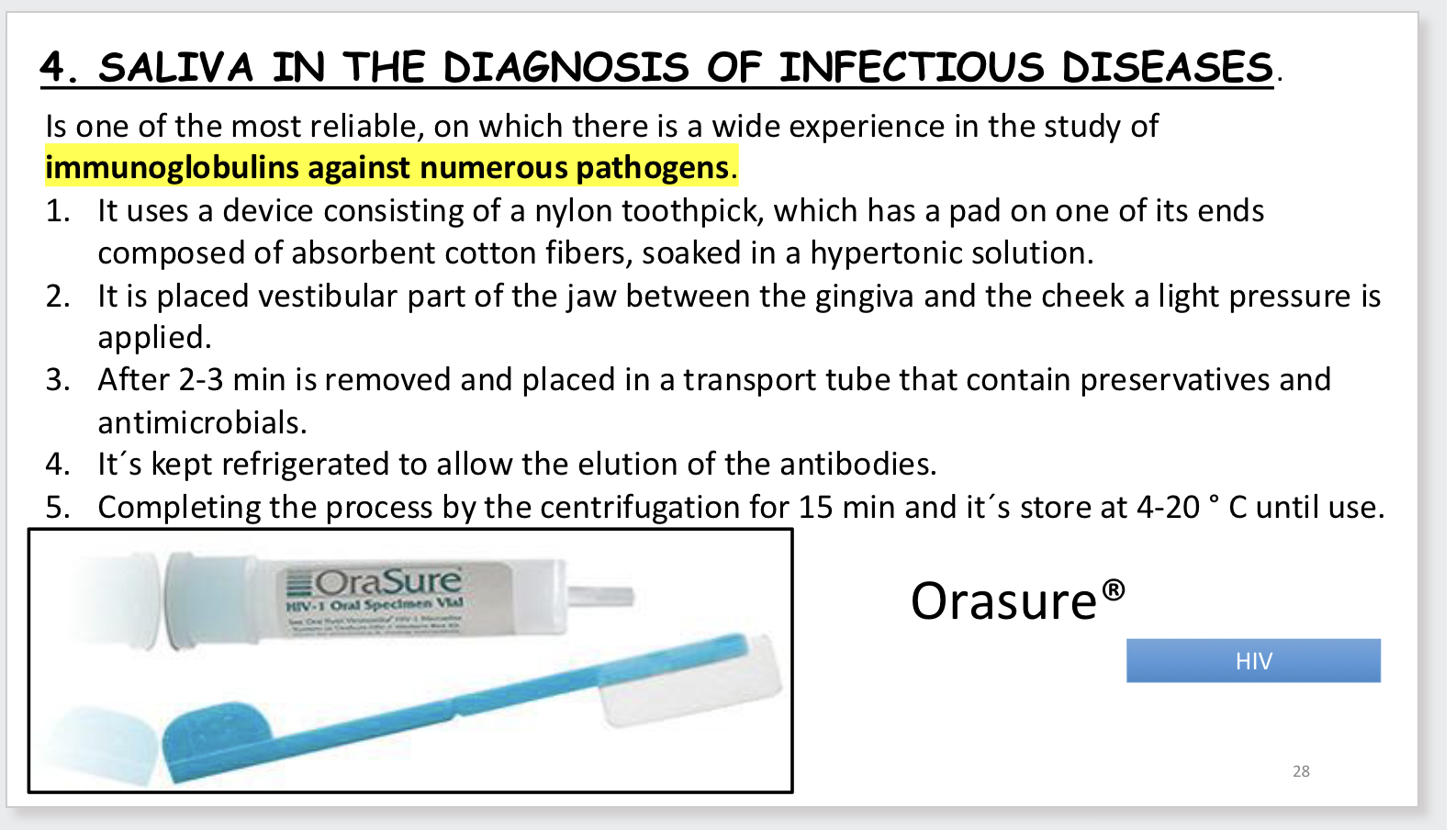
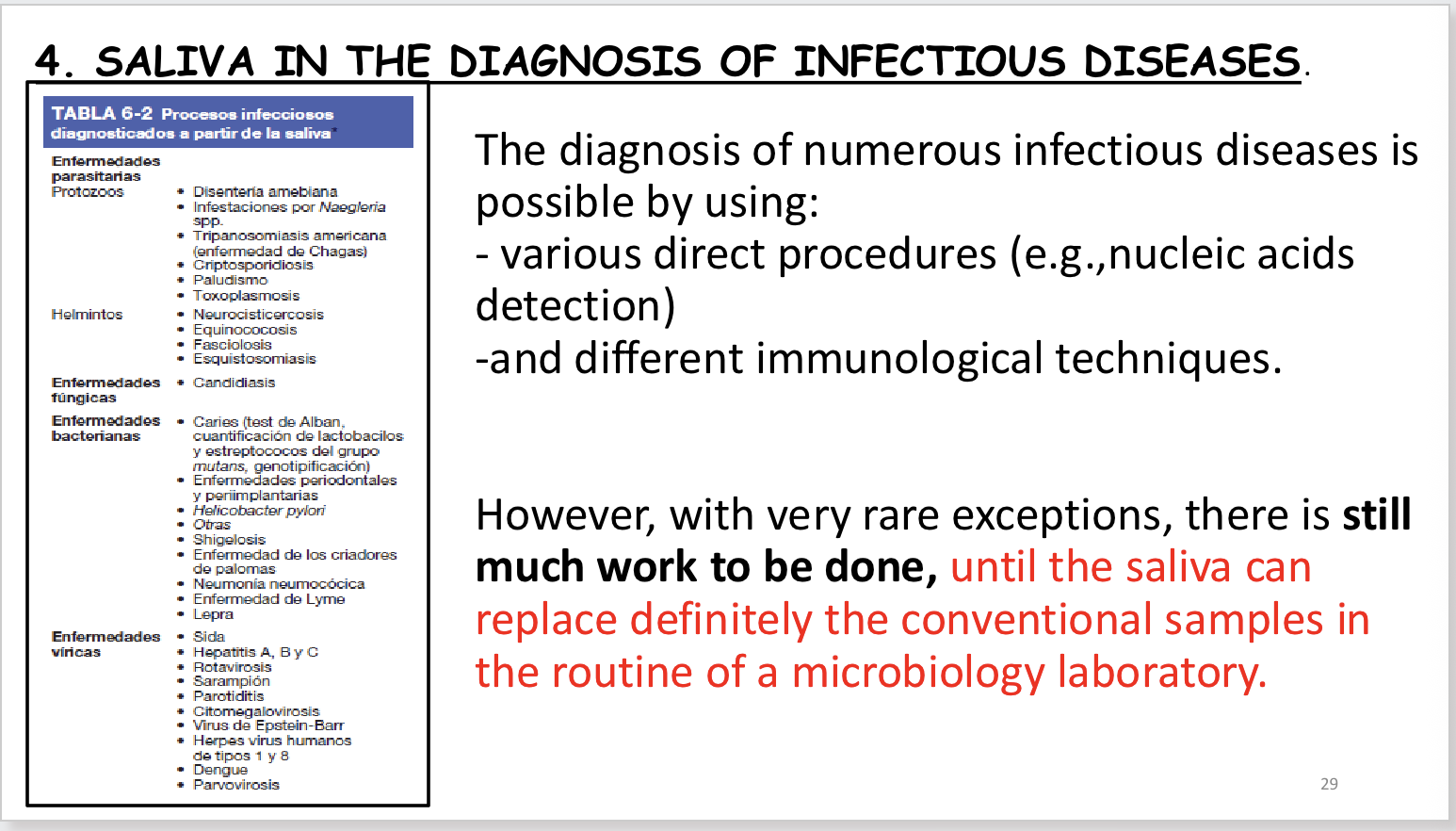
Saliva In use for diagnosis of disease
Used to assess risk of caries. Proficient for diagnosis of HIV.
i. carcinomas of the orolaryngopharyngeal area,
ii. gastric cancer,
iii. systemic sclerosis,
iv. neurological
v. and psychiatric disorders.
Saliva In use for diagnosis of disease 2
Microbiological diagnosis via direct/indirect methods. Direct reveals presence of pathogenic agent, that cause disease In a clinical sample or its products, antigens, structural elements or their nucleic acids.
• Among the procedures to carry it out, dependent or independent cultivation methods are found, especially by techniques of molecular biology, and they differ from each other according to the microorganisms to be investigated.
• The indirect diagnosis allows evaluating the response of the host. The humoral base one is the one that has a major interest in saliva. It is based on the presence of immunoglobulins in it, especially of IgAs.
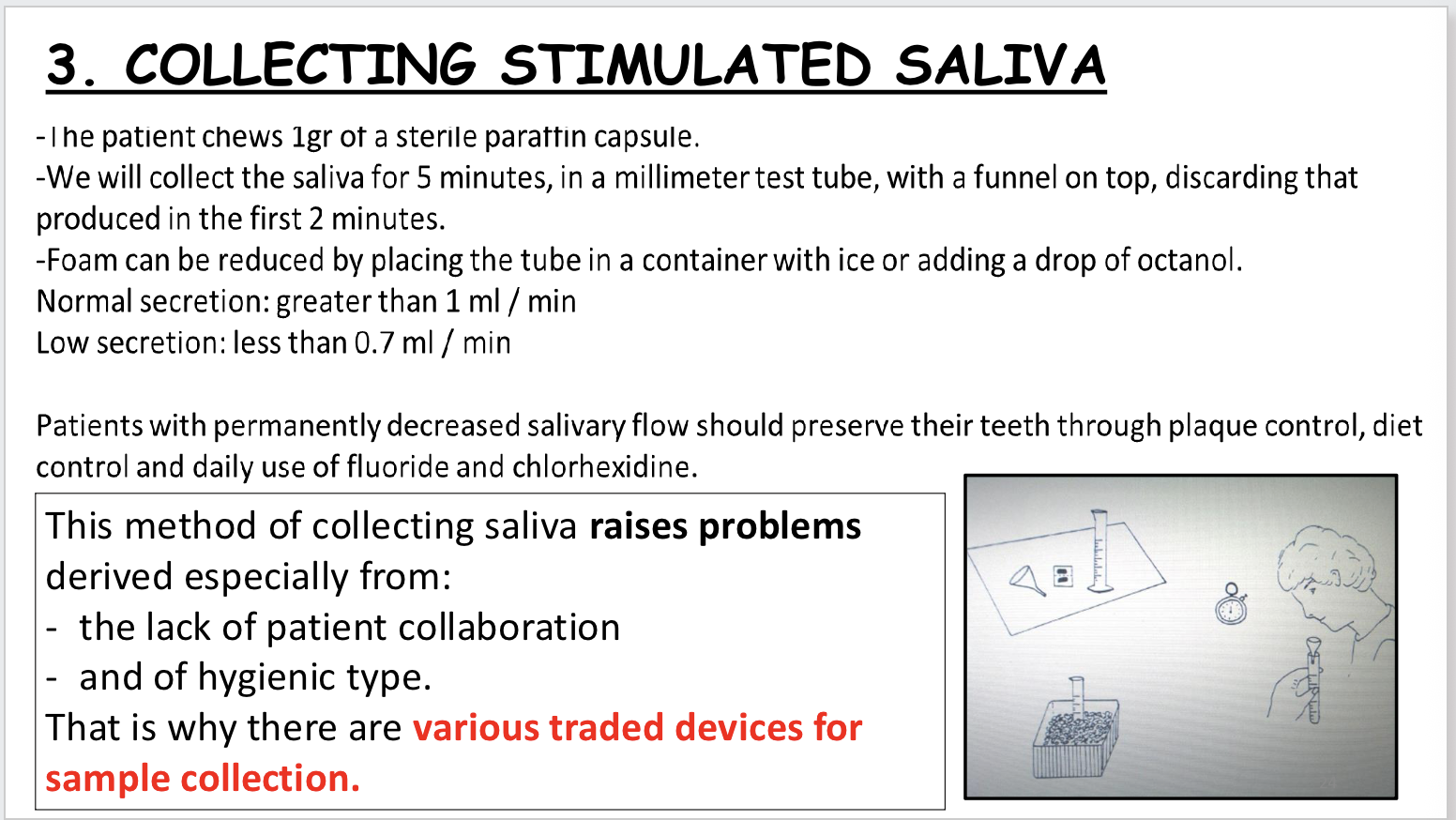
FOR MICROBIOLOGICAL STUDIES STIMULATED SALIVA IS USED
PREFERABLY.
Saliva In use for diagnosis of disease 3
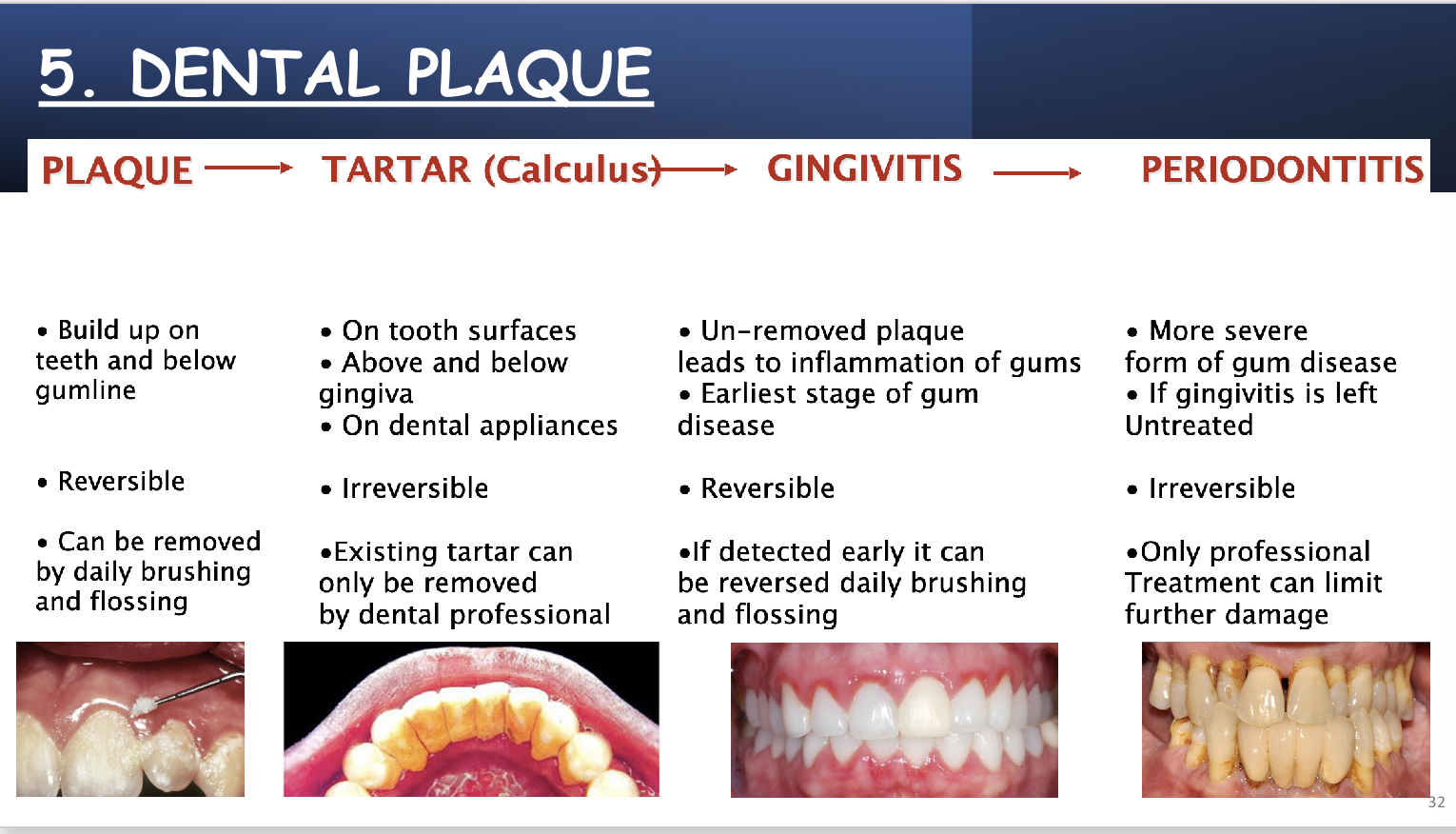
Dental plaque
Accumulation of different species of bacteria, that form dental plaque. naturally acquired bacterial biofilm which develops on teeth. some bacterial species may be in greater relevance in the
development of caries and periodontal diseases.
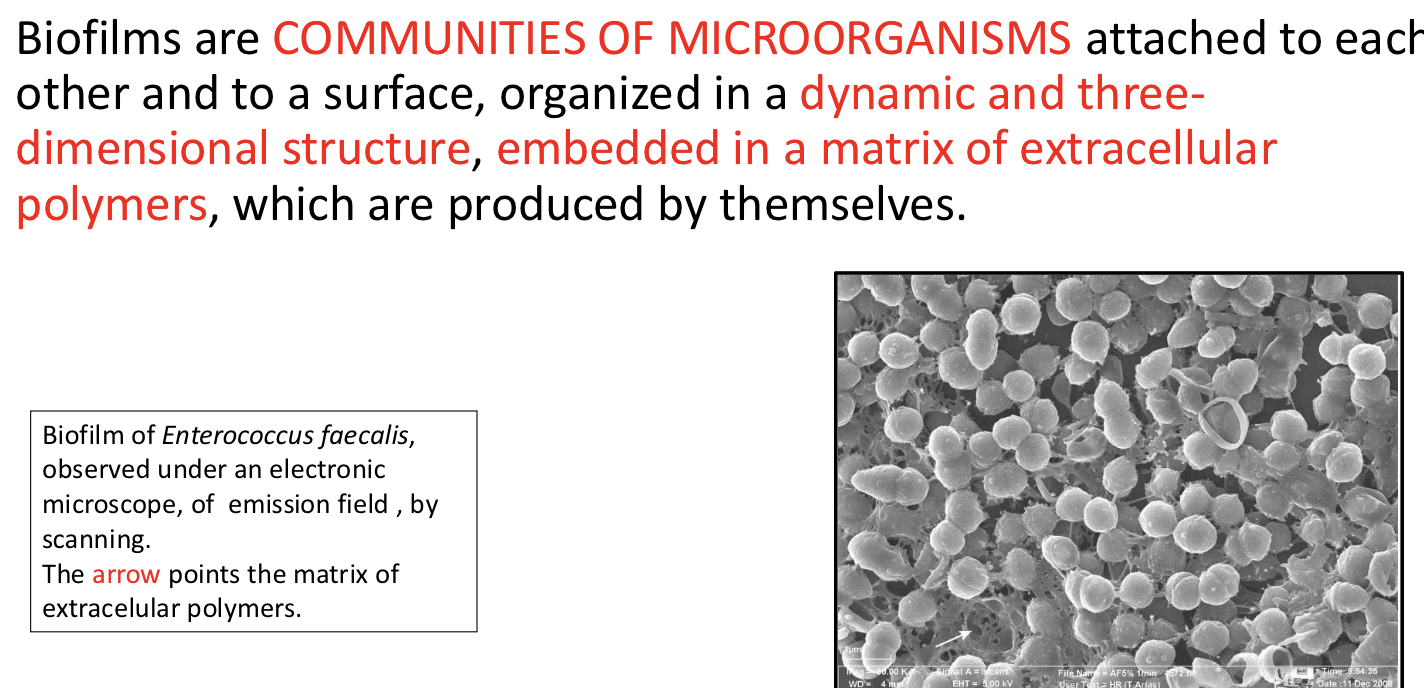
Biofilm is known as plaque, and is defined as a set of microorganisms firmly adhered to each other and to a surface, embedded, intermixed and surrounded by an extracellular matrix of triple origin: bacterial origin, saliva and diet.
• In the dental biofilm,
o microorganisms represent around 15-20% of its volume
o and the matrix the 75-80%
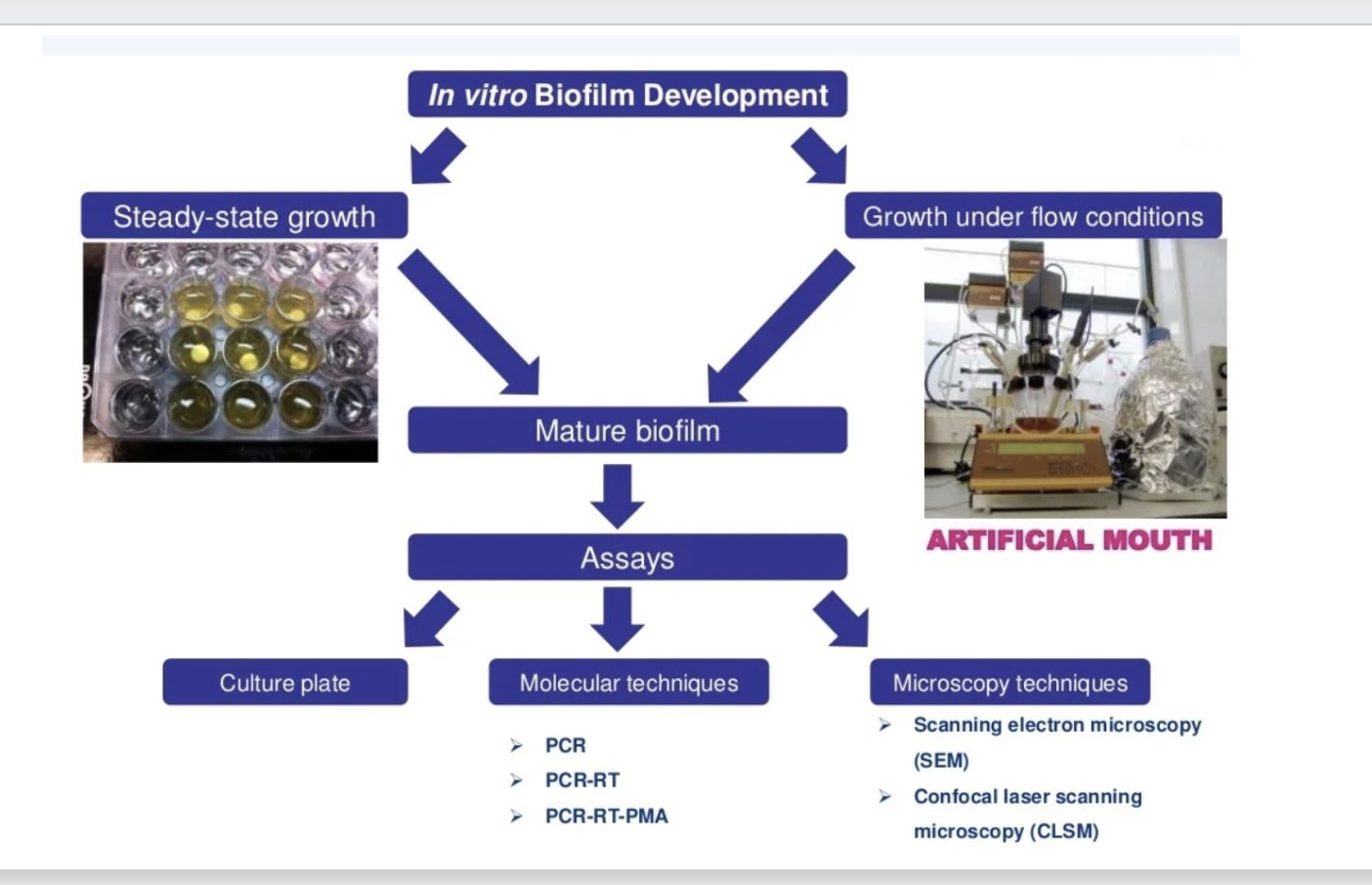
Biofilms
Oral biofilms are groups of bacteria embedded in matrices that attach to surface. 15-20% microbial population. 80-85% matrix with polysaccharides, proteins and Is interprocimal, sub gingival and suprgingival. 700 bacterial species present in oral biofilms.
Biofilms 2
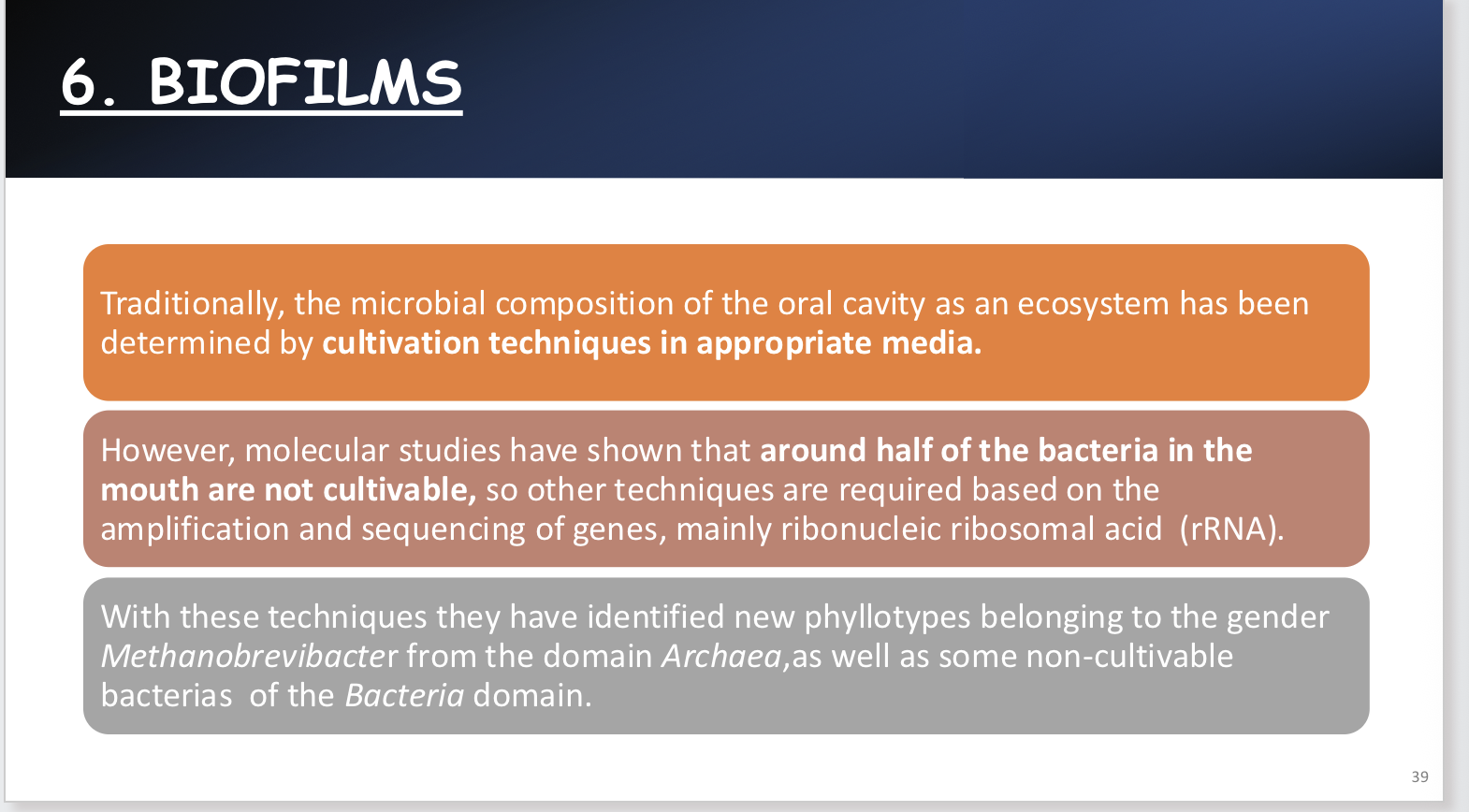
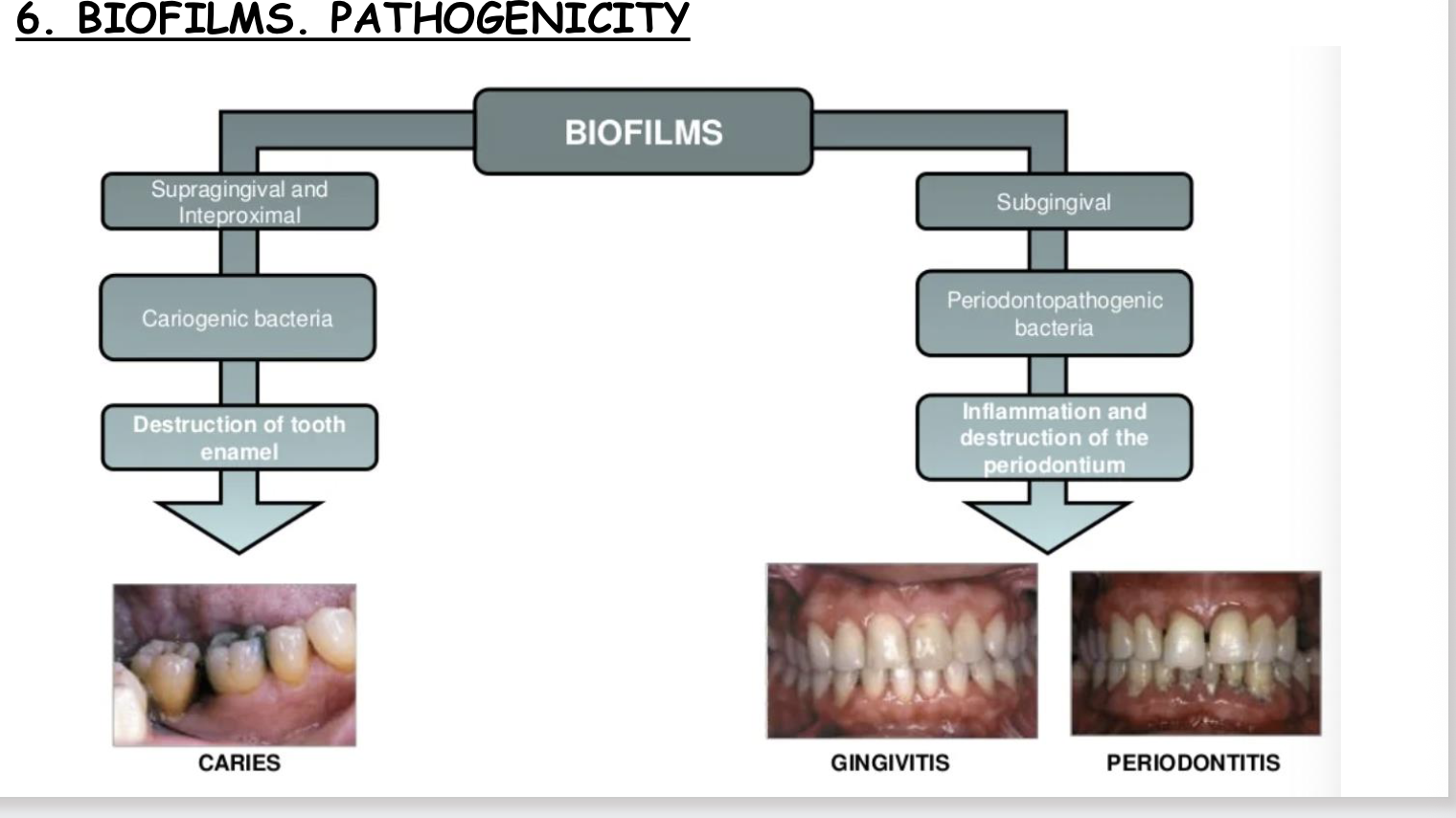
Biofilm pathogenicity
Supra gingival and inter proximal- causes carcinogenic bacteria to thrive,- destruction of tooth and enamel.
Subgingival- periodontopathogenuc bacteria, causes inflammation and destruction of periodontal
Biofilm properties
Bacterial community in biofilm 1000x more resistant.
1. Physiological HETEROGENEITY
2. Increased phenotypic RESISTANCE (external
physical o chemical aggressions)
3. Quorum Sensing (interbacterial
COMMUNICATION)
4. ADAPTATIVE capacity
5. RESISTANCE TO ANTIMICROBIAL AGENTS.
Biofilms have increased resistance to antiseptics andwe must study them. ,
Formation of biofilm
1) Attachment- transient association with surface, followed by adhesion.
2) Aggregation of cells into micro-colonies, and subsequently growth and matured.
3) A return to transient motility where biofilm cells are shed.
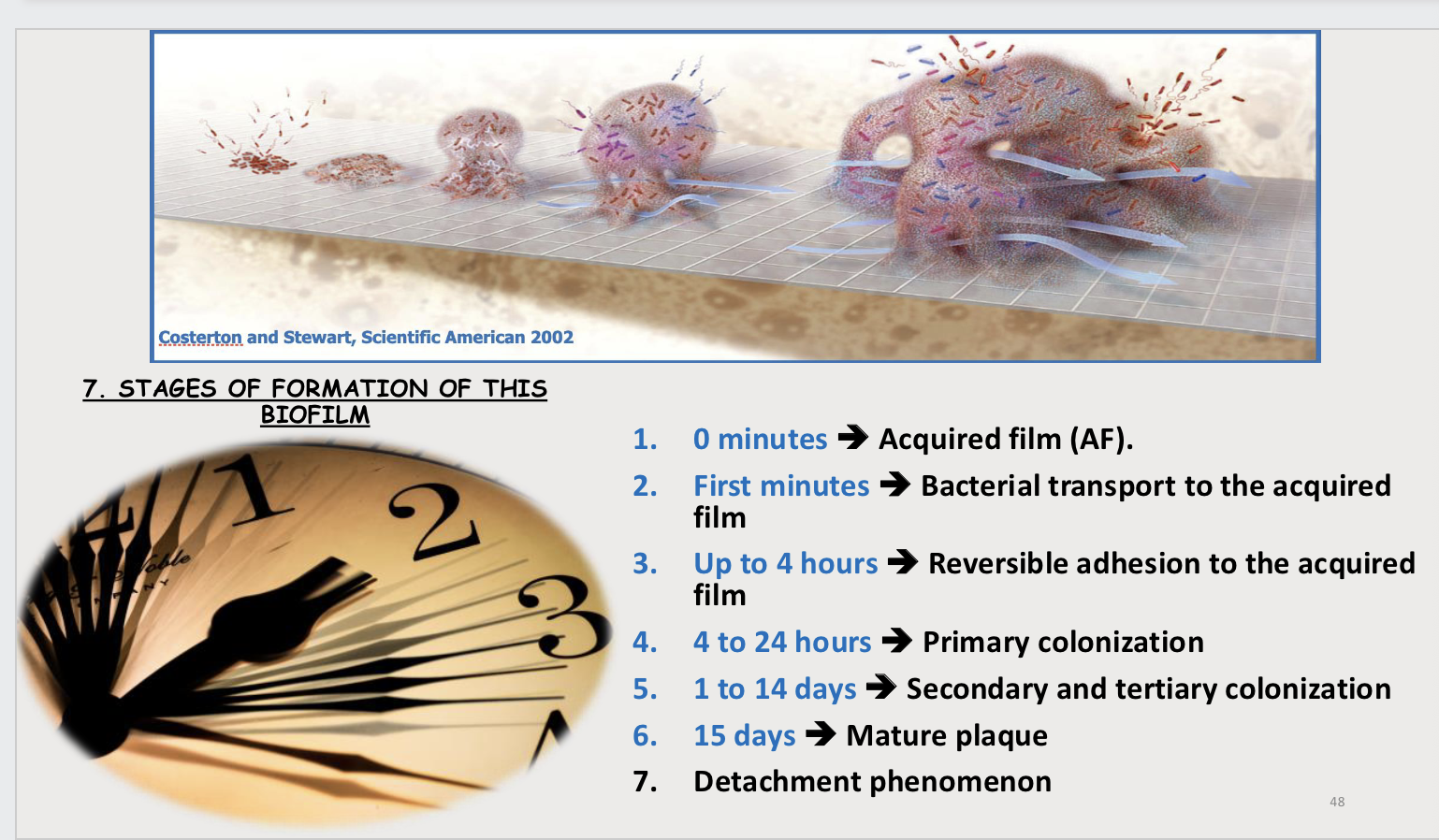
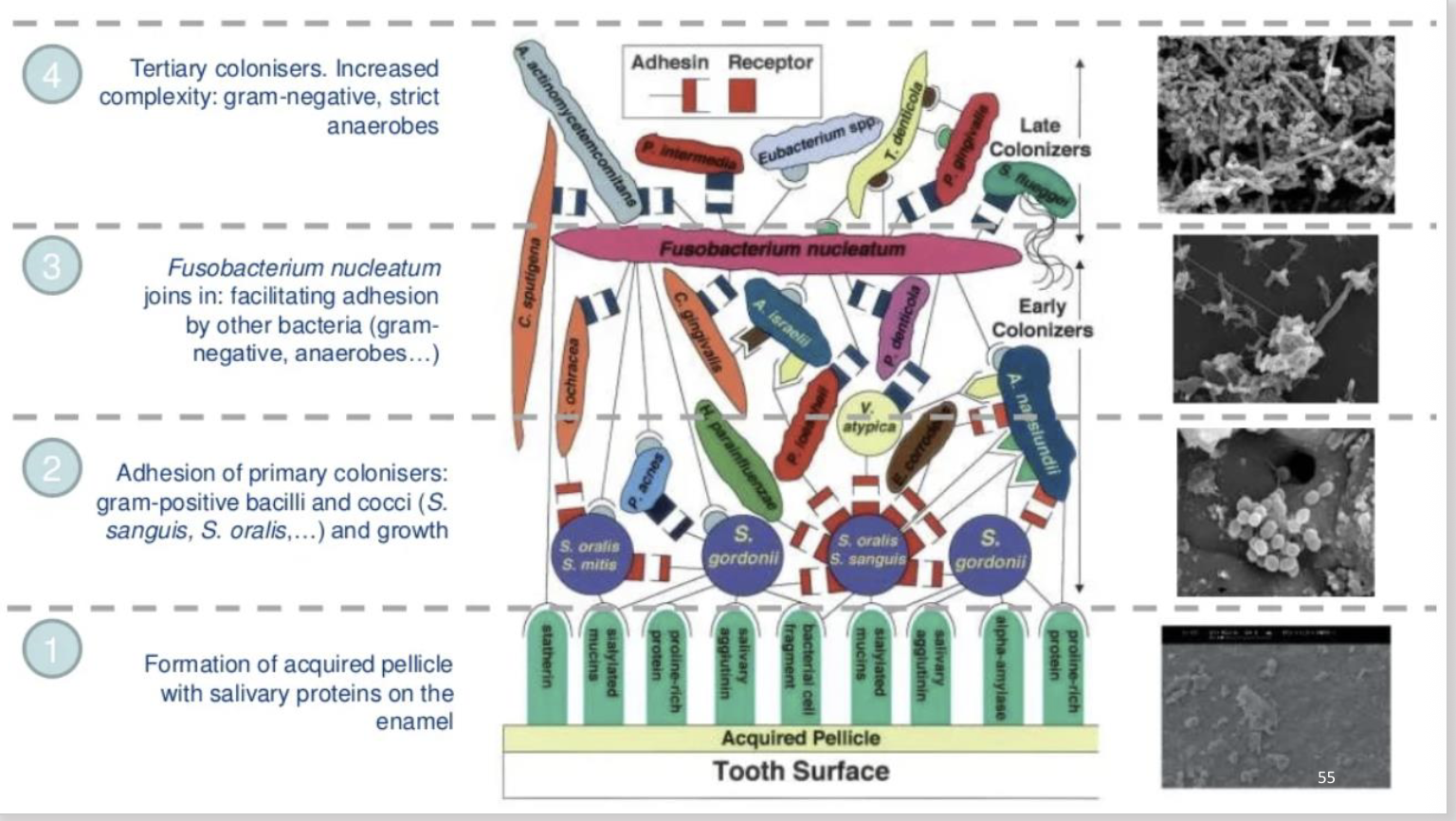
1) Acquired film
It is an amorphous ACELLULAR LAYER of something less than of 1μm thickness, that forms on
the surface of the teeth within a few minutes later, of performing a thorough hygiene of
them.
2) Bacterial transport to acquired film
MICROORGANISMS begin to reach the AF thanks to the salivary flow, carried by scaly cells or
by the mobility of the bacteria that have flagella or other immobile ones that get fixed to the
previous ones.
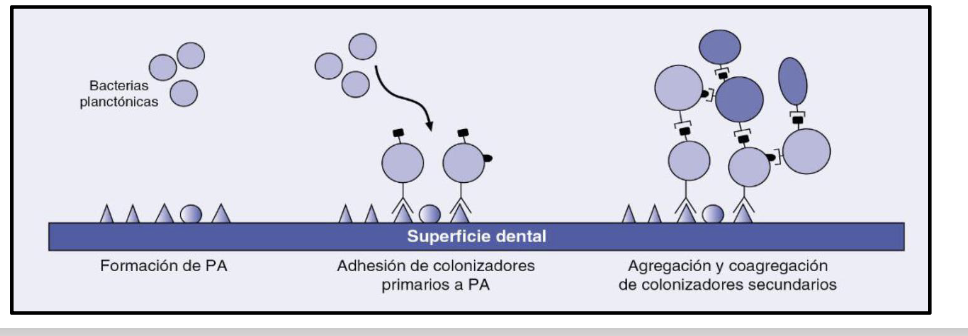
3) Reversible adhesion to the acquired film
It is established between 0 and 4 hours of the formation of the AF. Due to this process, weak bonds are established, such as hydrogen links and Van der Waals forces.
4) Primary colonization
There is an irreversible and specific adhesion between AF receptors and certain molecules located on the surface of bacteria known as "adhesins".
So various ionic and electrostatic interactions are established, covalents bonds and different types of adhesion.
This stage usually lasts between 4 and 24 hours.
The plaque is still very fine, AEROBIC metabolism predominates and the microbial NUTRITION COMES MAINLY FROM THE SALIVARY GLYCOPROTEINS AND DIET, and even of the gum fluid if it exists a certain degree of gingivitis.
The primary colonizers are mainly streptococci belonging to the group mitis, such as Streptococcus
sanguinis, Streptococcus oralis and Streptococcus mitis. Actinomyces spp. are also isolated, Neisseria spp.,
Haemophilus spp., Rothia dentocariosa, Corynebacterium matruchotii and, to a lesser extent, other
bacteria, almost all of them aerobic and facultative anaerobes
5) Secondary and tertiary colonisation
It can last between 1 and 14 days.
If until this stage, what has predominated is adhesion (bacterial union to a surface), from
now on, although that can continue, an active multiplication by aggregation occurs and
coaggregation.
The plaque increases in thickness, and in the deepest areas.
At this stage anaerobic facultative bacilli stand out, such as Eikenella corrodens,
Capnocytophaga spp. or Propionibacterium spp., and strict, such as Selenomonas spp.,
Porphyromonas spp. or Prevotella spp.
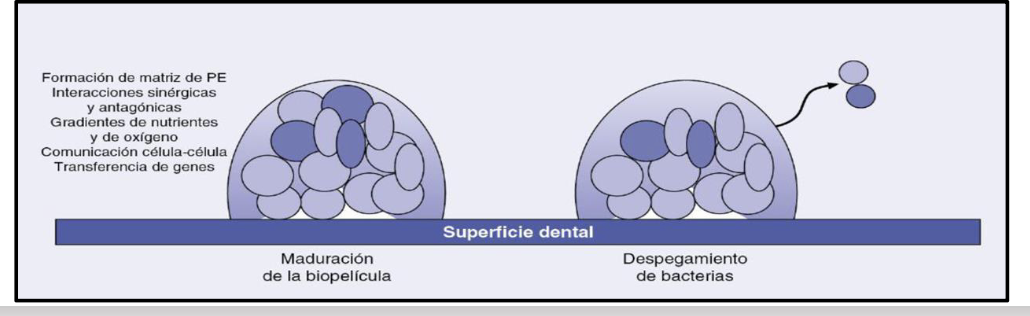
Mature plaque
It can be set after 2 weeks.
As the plaque matures, it generates the acellular matrix or extracellular polymers matrix.
It settles between the microorganisms, it surrounds them and serves as a nutritional
element, and contributes significantly to the structural integrity and tolerance of the biofilm
to the environmental conditions (e.g. desiccation) and to the antimicrobials agents.
Basically, it is constituted by organic compounds, water, carbohydrates, proteins,
glycoproteins, and some lipids.
7. Detachment phenomenon:
It´s due to the action of certain proteases that break the adhesive bonds, aggregations and
co-aggregations.
Thus, the released microorganisms return to the saliva, from where they will be ready again
to start new colonization, unless they are dragged into the digestive tract.
The end result is the development of a complex biofilm, interactive, polymicrobial
and functionally organized
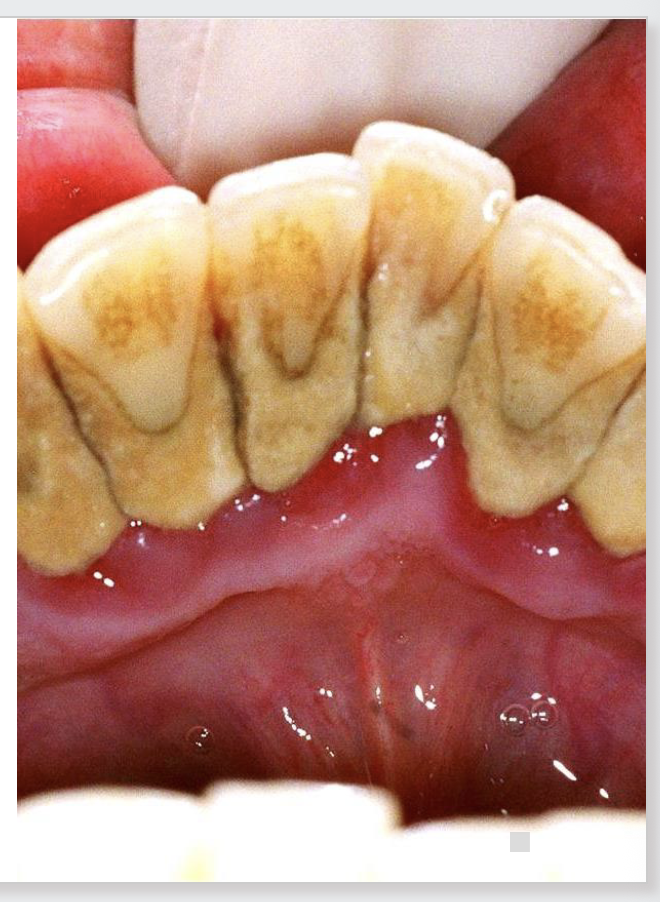
Calculus, scale and tarts
After a variable time, the MATURE PLAQUE CAN MINERALIZE and form
calculus, tartar or scale.
Its microbial composition is usually very similar to the mature plaque, at
least in its qualitative aspects, although it has fewer number of viable cells.
Tartar is constituted by 70-80% of inorganic salts and the rest of
proteins, carbohydrates and small amounts of lipids.
The four most common inorganic components are hydroxyapatite,
whitlockite, phosphate octocalcium and brushite.
Regarding to its genesis, various theories have been proposed:
1. Oversaturation of salts in saliva and in the matrix.
2. Pyrophosphate-pyrophosphatase system in the matrix.
3. Deregulation of the mineralization process.
4. Intracellular crystallization.
On the constituted calculus a new AF can develop and restart all the
process indicated previously.
Plaque types
There are different types of plaques
in function of their location:
1. free surfaces plaque
2. pits and fissures plaque
3. proximal plaque
4. subgingival
5. root plaque.
Despite the proximity of these surfaces, on each one of them it will be possible to form a biofilm
with different characteristics and compositions.
Biofilm and caries links
1. NON-SPECIFIC PLAQUE HYPOTHESIS. Every of the microorganisms present in it are
implicated in the tooth caries in such a way that the greater the quantity, the greater
the risk of suffering it.
2. SPECIFIC PLAQUE HYPOTHESIS. The responsibility of the process is only due to
concrete and determined microorganism.
3. HYPOTHESIS OF THE ECOLOGICAL PLAQUE. Disease-related microorganisms may be
present on the plaque associated to healthy places, but at so lower levels, that they
are not able to produce disease. Environmental changes on that plaque can lead to
alterations in the microbiota and, consequently, the disease appears.
4. MIXED HYPOTHESIS. It is a compendium of the previous three.
Cariogenicity
• In relation to caries, they are many microorganisms that produce acids, although this three groups will be especially involved: streptococci of the
mutans group, lactobacilli and actinomyces.
• Of all of them, the most cariogenic microorganism is Streptococcus mutans.
Cariogenicity 2
1. Acidogenic power or fast production of acids from sucrose and other sugars.
Streptococcus mutans, the most acidogenic.
2. Aciduric power or ability to continue producing acids at acidic pH.
Streptococcus sobrinus is the most aciduric. This means it has a strong ability to continue
producing acids even in acidic conditions, which allows it to thrive and contribute to dental caries
in low pH environments
3. Acidophilic power or high tolerance to acids.
4. Storage of reserve products.
5. Adherent capacity to the AF (acquired film)
Periodontal diseases
• Periodontal diseases reflects AN INFLAMMATORY TISSUE RESPONSE of the insertion tissue of
the tooth, to the bacterial accumulation at the subgingival level.
• It appears in two forms: GINGIVITIS AND PERIODONTITIS.
• The etiology of these processes is complex.
• The diseases are the result of the disequilibrium between the host and subgingival biofilm, so
they can be framed within the hypothesis of the ecological plaque.
• In this way, ENVIRONMENTAL CHANGES ON THE PLAQUE, such as the ones originated from
smoking, can lead to changes in the subgingival microbiota.
• In other changes in the subgingival environment, genetic factors are involved. (eg, neutrophil
defect).

Periodontal disease 2
• This disequilibrium leads to the increase of the biofilm above the compatible
levels with health, for which an inflammatory response is originated.
• If this is insufficient to control plaque, changes will occur in the ecosystem of
the gingival sulcus, which will favor the establishment and growth of a
periodontopathogenic microbiota.
• Under healthy conditions, peridontopathogenic microorganisms are found in
very low, almost imperceptible concentrations.
• These are Porphyromonas gingivalis, Tannerella forsythia, Treponema
denticola and Agregatibacter actinomycetencomitans.