CardioVascular System
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Components of the CardioSystem
-heart (pump), the blood vessels (pipes), the blood (fluid)
-main functions : supply oxygen and nutrients, remove wastes, temperature regulation , distribute hormones, clotting of open wounds, immuno-vigilance
Blood Parts
55% is plasma which is made up of 90% water and rest is electrolytes, water, nutrients, waste products, hormones like aulbin hormones
-leukoyctyes and platelets makes up buffer
-erthyocytes makes up 45%
Erthyrocytes (RBC)
biconcave shape: allows for surface area which favors diffusion. no nucleus : no dna/rna, no mitochondira, no organelles, enzymes: glycolytic enzymes and carbonic anhydrase and hemoglobin: binds oxygen and carbon dioxide , filtered in the spleen and made in red bone marrow by erythropoiesis . erythropoietin (hormone) differs stem cells into rbc. short life span =120 days
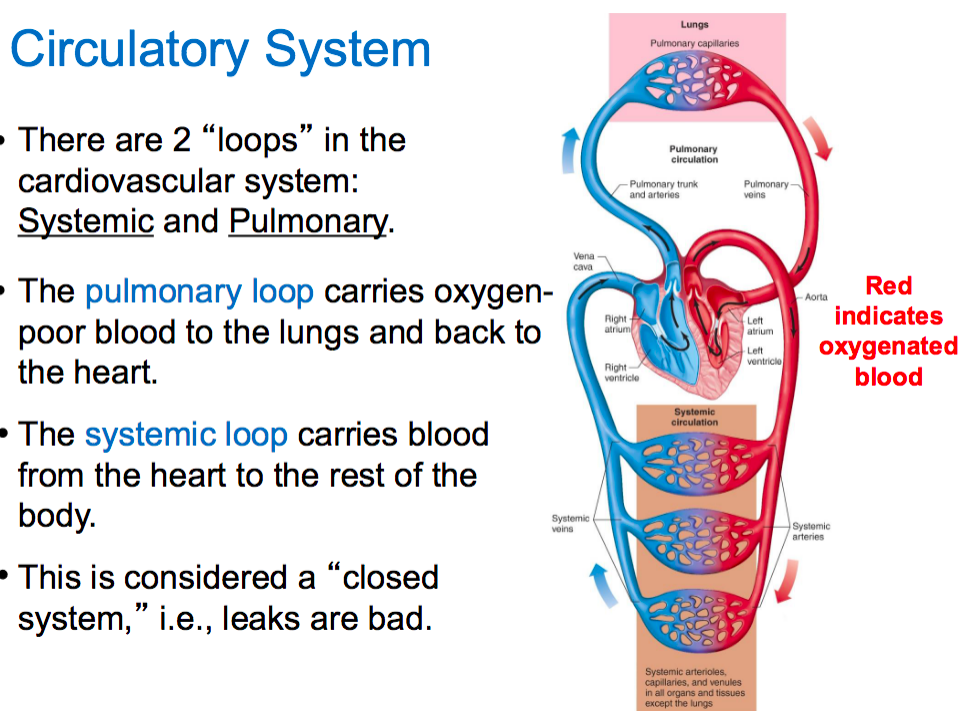
Circulatory System
pulmonary : carries oxygen poor blood to the lungs and back to the heart
systemic : from heart to the rest of the body
-closed system
Heart Valves
AV valves: right atrium to right ventricle (tricuspid valve and bicuspid valve)
SL valves: between right ventricle and pulmonary artery + left ventricle and aorta
Heart Valves
ensure blood flows in one direction : valves open when the backpressure is greater than forward
valves close when the forward pressure is greater than the front
Heart Walls
epicardium : outermost layer of the heart and contains pericardial fluid
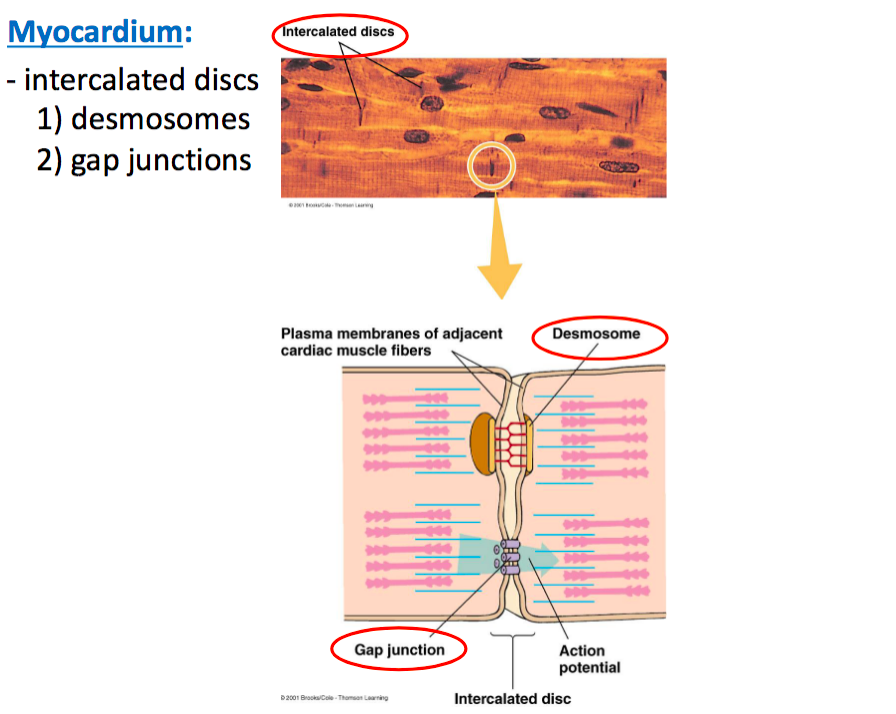
myocardium : middle layer where it contains cardiac muscle. cardiac muscle are connected by intercalated disks where two types of contacts are formed : demosomes and gap junctions
-Demosomes: mechanically hold cells togehter while gap junctions provide paths of low resistance to the flow of electrical current between muscle cells. gap junctions allow cardiac muscle to form a functional synctium ,
-endocardium : innermost layer of the chambers of the heart and is continous with the lining of blood vessels
Cardiac Cells
99% are contractile cells (myocytes) and contain striated muscle , muscle contraction follows myosin/actin interaction
-1% cells are part of the electrical conduction system : pacemaker cells, do not have contractile elements
Electrical Activity of the Heart
-heart muscle can conduct it’s own rhytimic activity -autorhythmic -due to specialized cardiac muscle cells that generate pacemaker activity from electrophysiologcial properities
pacemaker cells are grouped together in nodes that control the rate and coordination of cardiac contractions
-pacemaker cells initiate their own action potentials and this is called pacemaker activity -bascially authorhythmic and is controlled by the generation of pacemaker potentials
Pacemaker Potentials
oscillation of the membrane potential which causes the cell to reach thresehold and generate the action potential at a regular interval , involves changes in K, Na, Ca
Steps of Pacemaker Potential
-Hyperpolarizaton leads to increase of premability to sodium , this increase in sodium is first done by F-type Sodium channels (which are the funny type)
-depolariztion leads to increase of calcium premability which further depolarizes the cell to 70 and reach therehold. these are the T-type calcium channels (transient)
-action potential is generated when a second increase of calcium preambility occurs-this is done by L-channel (long lasting , no sodium is here only calcium -spike is generated
-depolarization leads to premablity of potassium and this leads to repolarization , and eventually hyperopolarization of K+ and this leads to premability of sodium again so whole cycle starts over
-autorythmacity is generated because of hyperpolarization
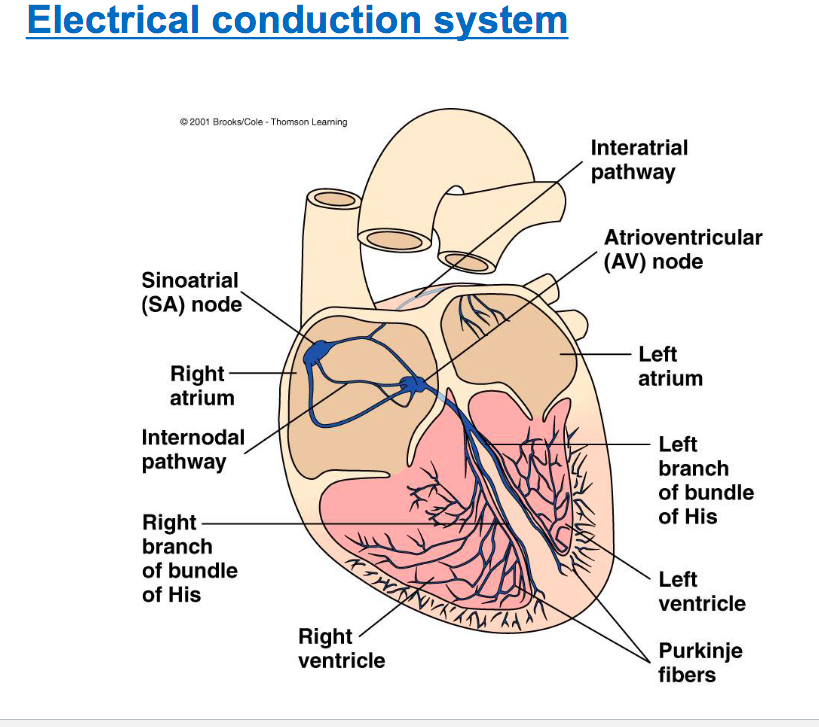
Electrical conduction system
SA node> AV node> bundle of his> purkinjie fibers
Diff Parts
SA node : bundle of specialize pacemaker cells located in the wall of the right atrium near opening of superior vena cava, node exhibits 70 action potential per minute and leads the other structutes in the heart -forms the functional syncitium
-AV node: pathway from SA to AV is internodal pathway and the AV node is bottom of right atrium , if AV node is seperated from SV node has a autoryhtmicity rate fo 50 but under normal conditions follows the SA node
-Bundle of His: right and left of bundle of his : projects AV node 70 originates at AV node and spreads into right and left ventricles
-Purkinje fibers: small terminal fibers of specialized cardiac pacemaker cells that extend from the bundle of his and spread throughout the myocardium . these fibers exhibit 30 AP , very fast conduction and contraction
after ventricles are contrated-blood is pumped out to for pulmonary circulation and pulmonary circulation
Interartrial pathway
a pathway of specialized cardiac cells, that conducts pacemaker activity from the right atrium to the left atrium
AV node delay
pacemaker activity is conducted relatively slowly through the AV node resulting in a delay of 100ms, this allows ventricles to fill up with blood while the atria contract , can’t have all chambers contracting at once
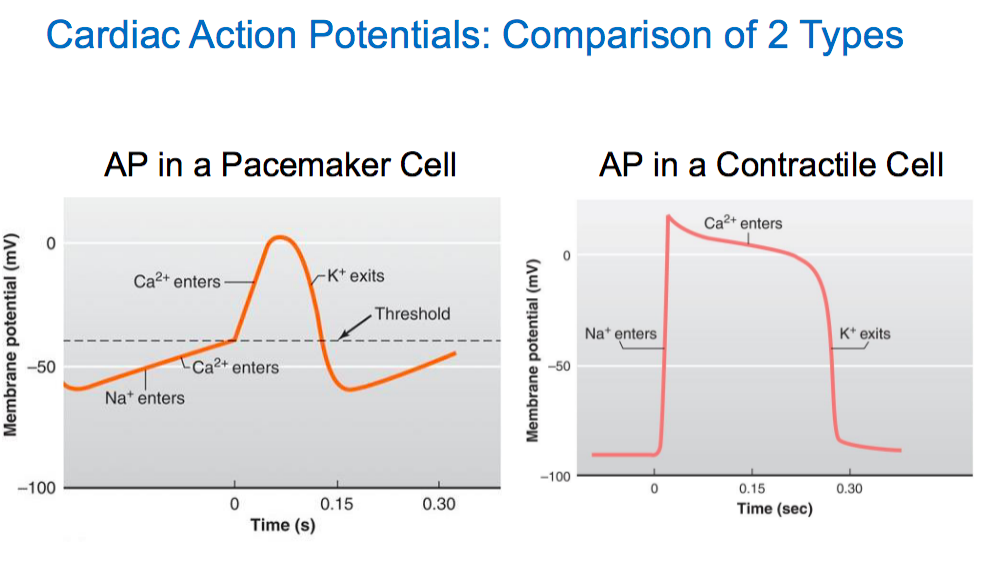
Cardiac Action Potentials : in contractile cells
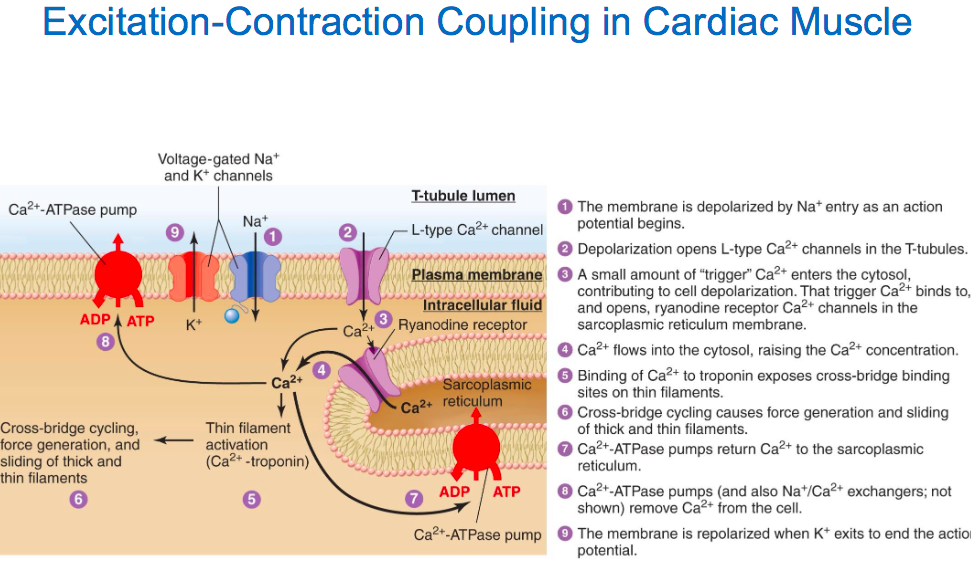
differnce between ap of pacemaker cells: starts off relativey negative around -90mv, rising phase of AP is caused by an influx of Na in from the F-type channel and calcium entering from L-type channel causes the plateau of AP : increases Ca preabmility and decreases K premeabitilty. Falling phase: reduction of Ca preambility and increases of K+ preambillty via VG K channel
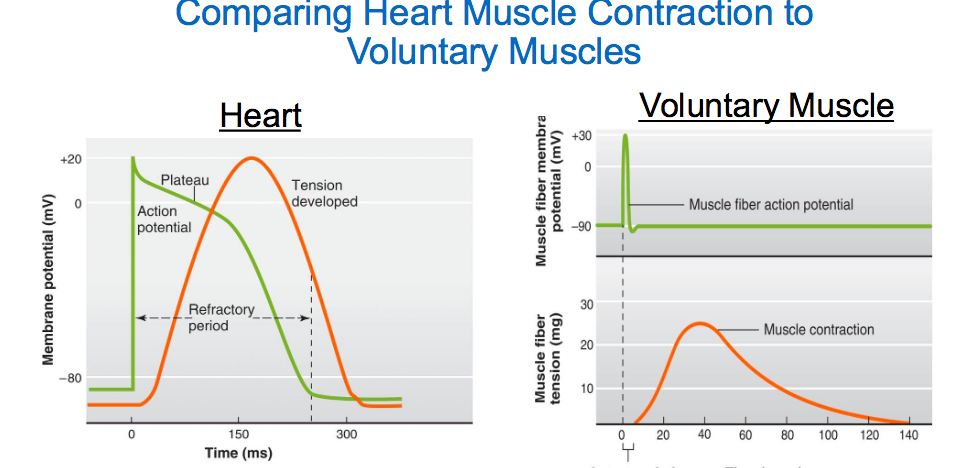
Diff between contraction of heart muscle vs contraction of skeletal muscle
-heart has a longer action potential period and has a plateua period as well. does not require nerve stimulation-stimulated by autorhytmic cell or an adjacent myocyte. calcium enters through L-channel which triggers more calcium to leave SR and contraction occurs during action potential
has a longer refatory period whihc prevents tenatnus and allows ventricles to fill blood up
contraction of heart
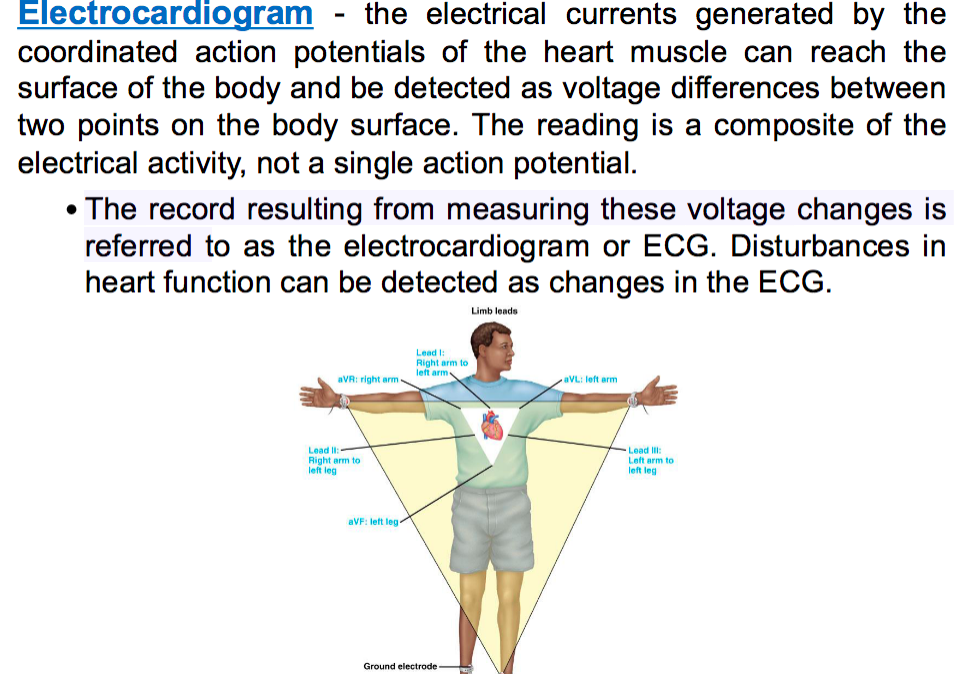
ECG/EKG
looks at sum of all the action potentials that are fired in one moment : all the cardiac cells in the heart and their action potentials summed up
-reads the total electrical activity and looks at the voltage differnce as it goes through depolarization to repolarization at two different points of the body
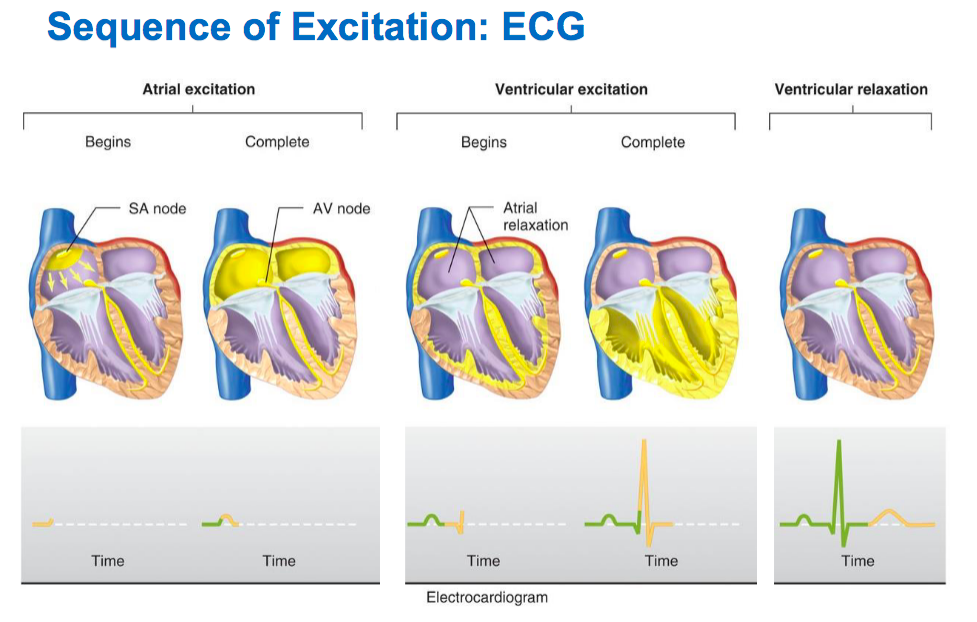
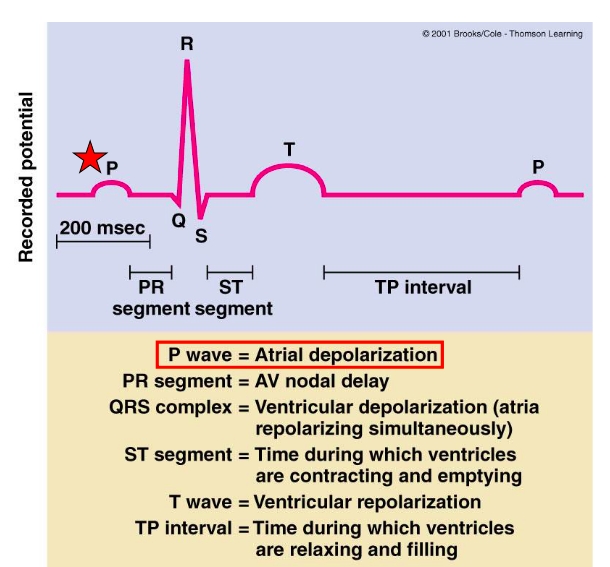
EKG Waveforms
p-wave: atria depolarizatoin which is the SA node-atria contract (SA -AV)
p-r: AV node delay which gives ventricles some time for blood to fill
QRS: ventricle depolarization (ventricle contraction)while atria repolarize : bundle of his and purkinje fibers
ST : ventricles contract and are emptying
T wave: ventricular repolarizton
TP interval: ventricles relax and refill with blood
Pump +heart sounds
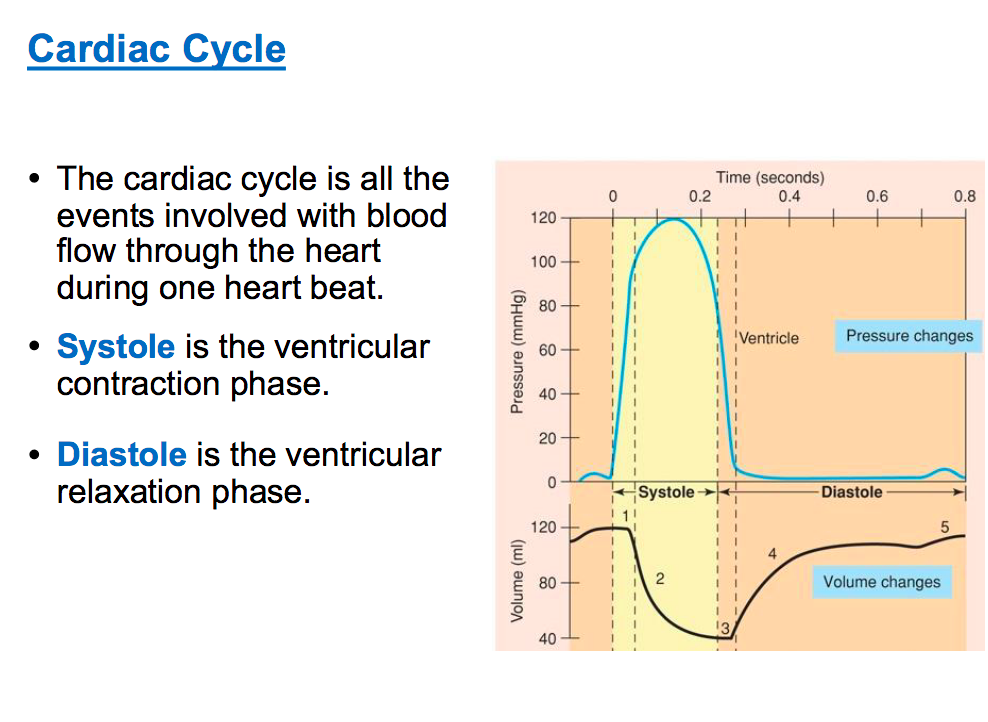
Systole: is contraction of heart ventricle
Dyastole: relaxation of heart ventricle
lub : av valves closing
dub: sv valves closing
Detailed Steps: remember pressure moves from high to low
Venticular Filling: Early Systole: volume is constant while pressure is contracting until it reaches a thresheold -isovolumetric contraction. Late Systole: reaches threshold and SV valve are open- volume decreases and pressure decreases -back pressure is greater than forward pressure: left ventricle pressure is less than aorta=causes SV valves to shut. Early Diastole: isovolumetric relaxtatin: volume is same and pressure decreases however once pressure is below to a threshold , AV valves open. In this case, pressure of ventricles is below that of atria. Late Diastole: forward pressure is greater than back pressure. venticular refilling is a passive pumping and ventricles are relaxed and gets topped off by the atria contracting (active)-AV vavles shut when forward pressure is weaker than back pressure because volume has increased in the ventricles
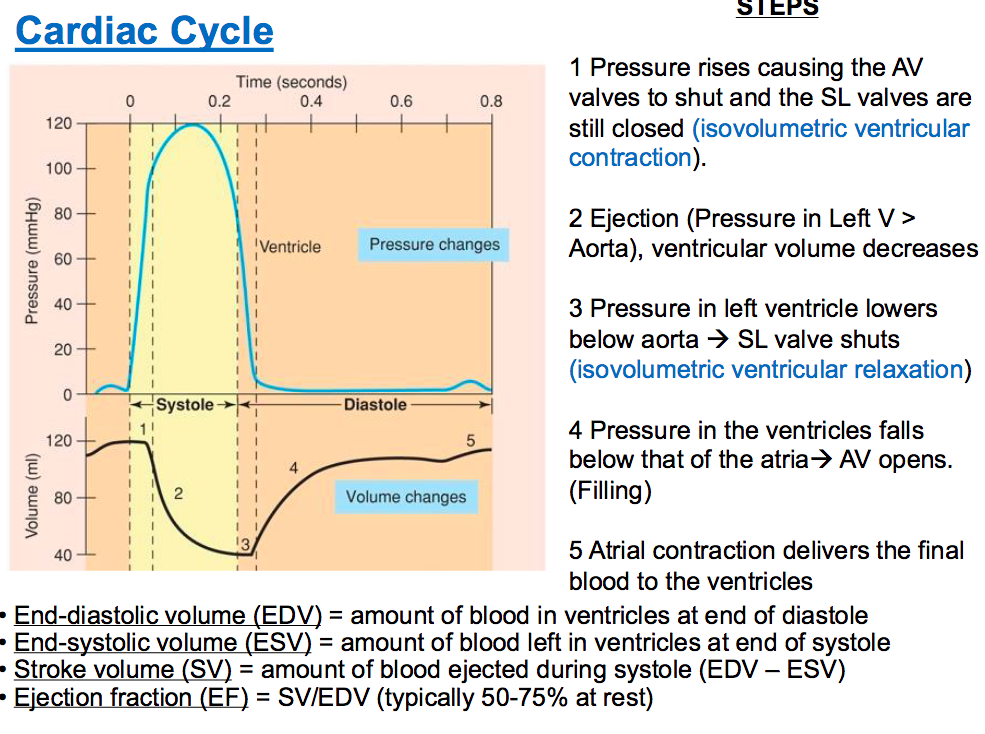
Stroke Volume
EDV-ESV (how much blood after refilling -how much blood after contracting it out)
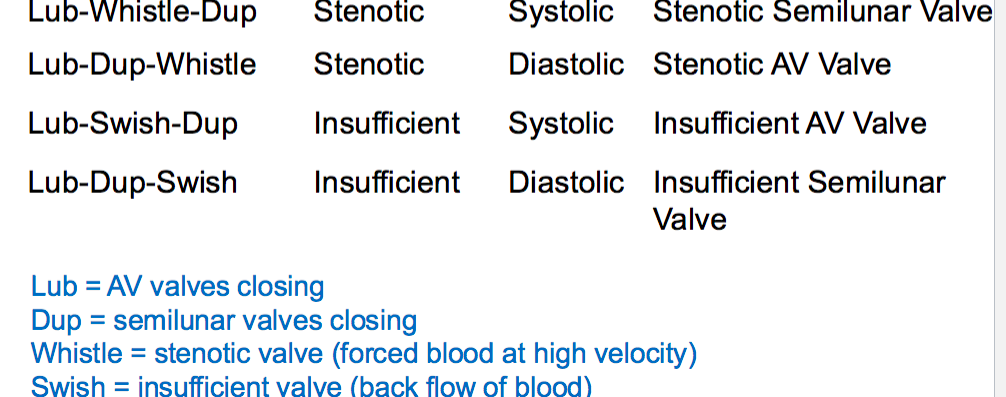
Heart Sounds
murmurs: abnormal sounds made due to turbulent blood flow through malfunctioning valves
stenotic valve: this is a whistling sound made when a valve wants to open , the valve is narrow and does not completely open due to high velocity: ex: lup-whistle-dup: SV stenoic and lub-dub-whistel: AV stenoic
insufficient: swishing sound when closing valve, and turbulent flow because blood flows backwards in the valve and collides with blood going opposite direction structurally damaged valve that does not close properly: lub-swoosh-dub: insufficient av and lub-dub-swoosh- insufficient SV valve
Heart Murmurs Causes
rheumatic fever, mitral stenosis :mitral valve is thickened and calcified and septal defects: holes in heart allows blood to pass between two parts
Cardiac Output
volume of blood pumped out by each ventricle per minute: CO= HR by Stroke Volume. avg HR is 70 bpm per minute and CO is 5 liters per min
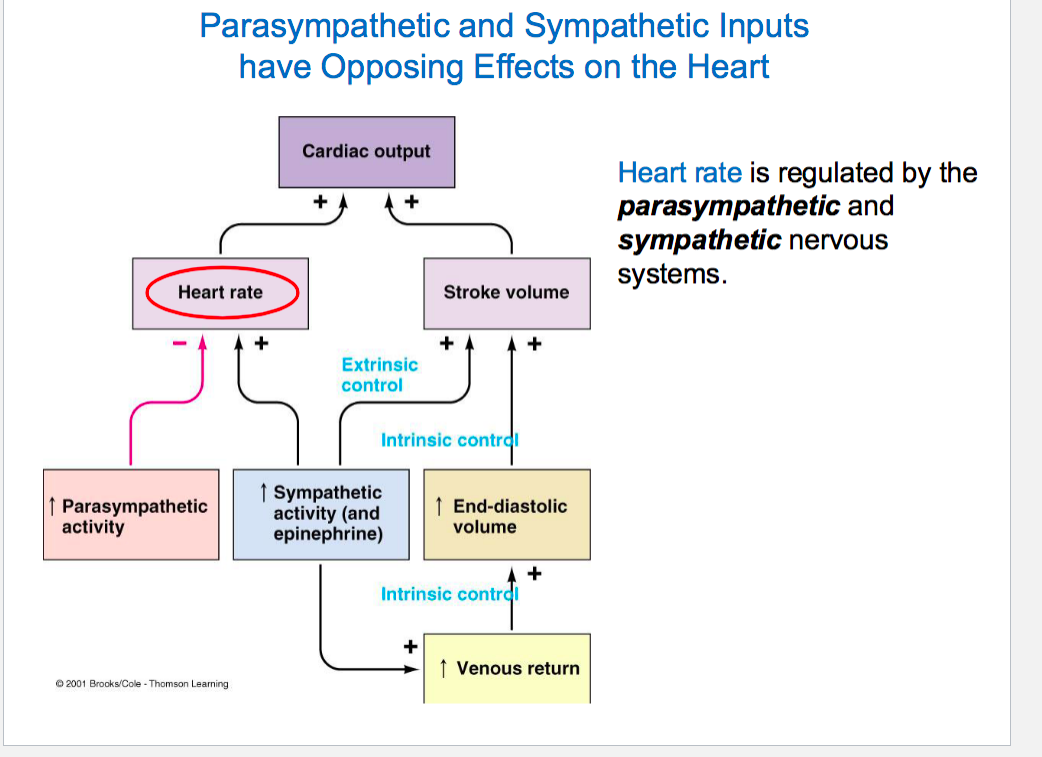
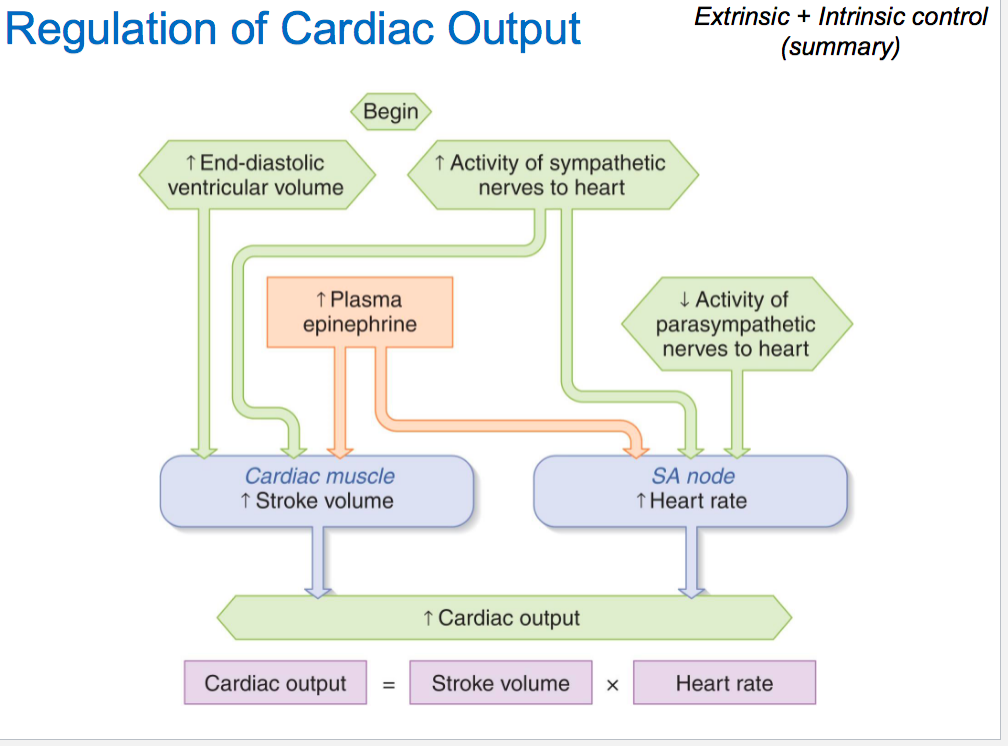
HR is regulated by parasympathetic and sympathetic nervous systems and stroke volume is regualted extrinsically by sympathetic nervous system while nervous system is regulated intrinsically by volume of venous blood returning to ventricles
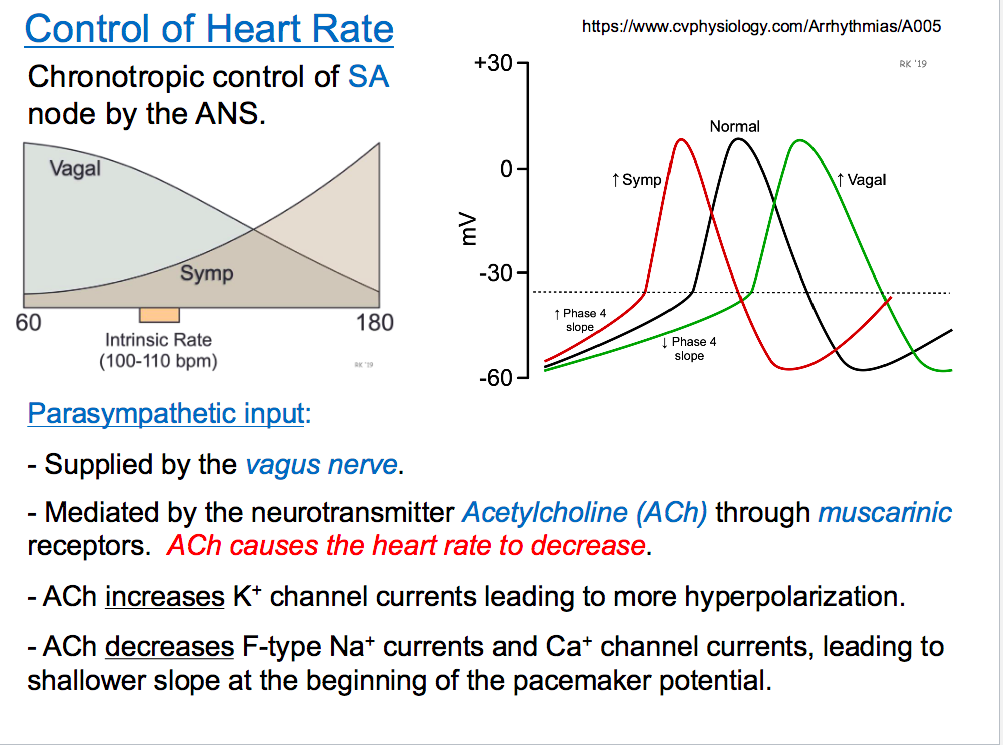
HR regulation
para sympathetic : through vagnus nerve release Ach to muscarnic receptors and HR reduces . Ach increases K+ channels leading to more hyperpolarization and decreases F-type Na+ channels and Ca+ channel currents which causes shallow slop and has a longer latency period: longer time to reach threshold so longer time between spikes and slow HR
Sympathetic: releases NE through beta ardrengenic receptors supplied by sympathetic nerves, has a faster latency period and increases preambility to Na F channels and Calcium L-channels-leading to a steeper slope , decreases preambiliy to potassium
Stroke Volume
SV is the amount of blood pumped out of the chamber in one contraction. SV: EDV-ESV
influenced by preload , contractility and afterload
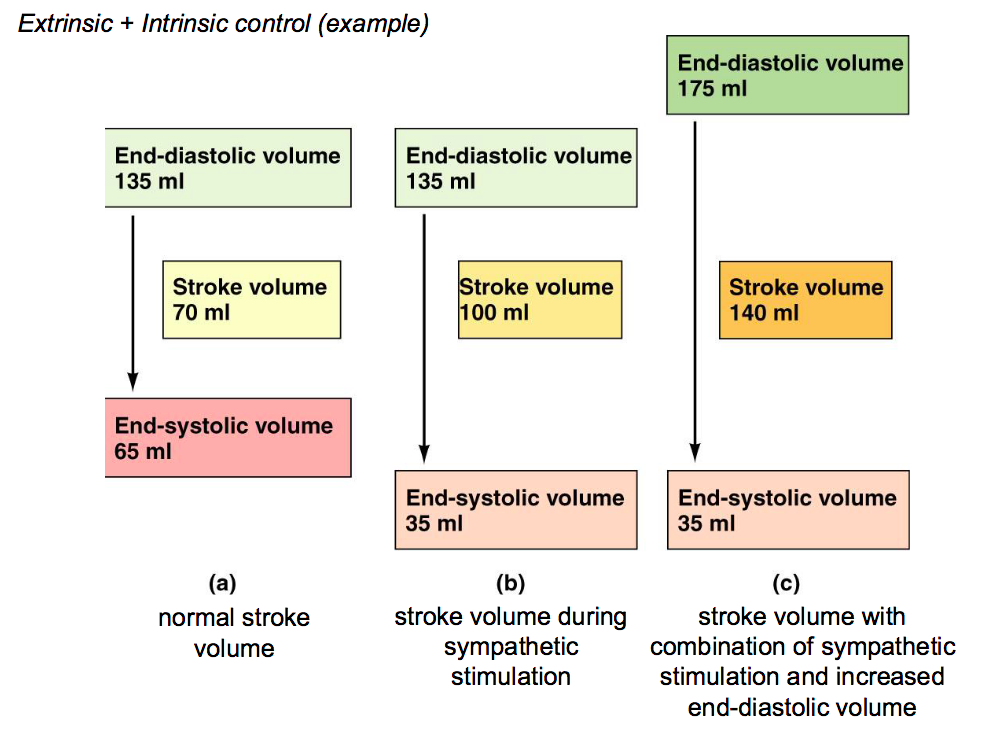
Modulation of Contractility (Extrinsic Control)
very less effect on parasympathetic effect: rrelease of ACH reduces Ca premablity during plateau phase which reduces less contractile strength
Sympathetic effect: release of NE: increse of contractile strength by enhancing Caclium premability during the plateua phase
sympahtetic effect : force increases during contraction and more stroke volume under sympathetic
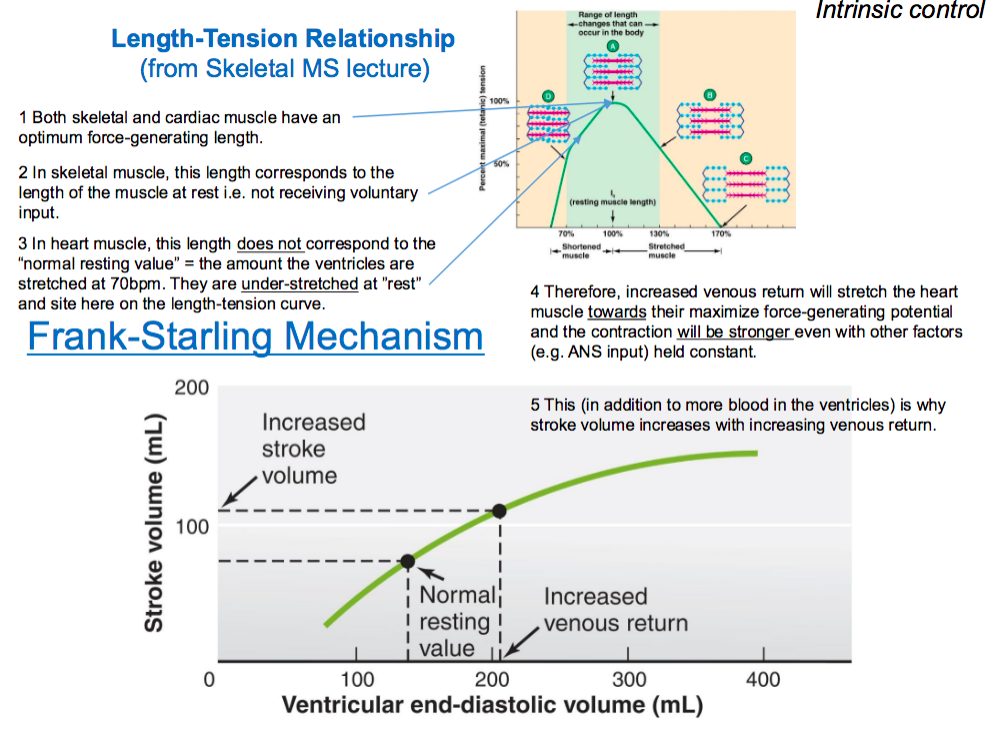
frank strarling force (intrinsic control)
-stroke volume depends on preload. preload is the extent muscels are stretched before they contract and stretch is controlled by the amount of blood in ventricles. this is controlled by venous return
greater venous returen =increase contraction=increase in stroke volume
steps: the cardiac muscles are understretched and this does not allow for optimal stretch , inorder to increase stretch we need to increase venous return which will allow muscles to stretch and reach potential contraction force. this causes stroke volume to increase and contraction to be stronger as well
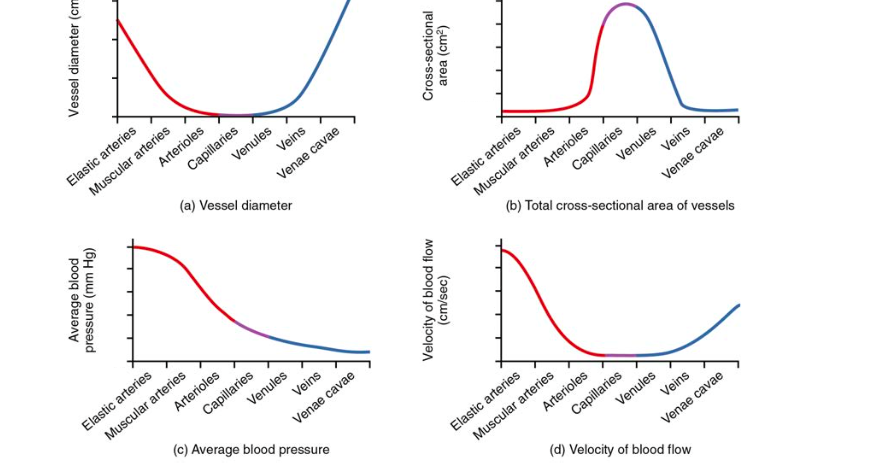
Flow of Blood
arteries, arteroiles, capillaires, venules, veins,
pressures: increasing to decreasing order
cross sectional area: increasing to decreasing, capillaries have less velocity and resistance because large area and ensures blood flows to all parts-reaches more destinations
velocity: high velocity in large arteries and veins, arterioles, capillaries, venules have less because of more cross sectional area
vessel diameter: larger in arteries and veins and continues that way-even though arterioles and capillares, and venules are constricted in diameter-they have more crosss sectoinal area so velcoity is less
Pressure , flow , resistance
pressure: force exerted and measured in mmHg, difference in pressure at the beginning of pressure and end of pressure
flow: volume moved measures in L/min passing through each vessel
resistance: how difficult it is for blood to flow between 2 points given pressure difference
F: detla p/R-proportional to resistance and pressure difference
with pressure constant:if you increase resistance you decrease flow
resistance depends on : 1) blood visocsity (friction in the blood), vessel length (friction between blood and inner surface of vessel is proportional to vessel length): longer vessels means more ressitantce and shorter vessels means less resistance vessel radius: raidus is inveerse to resistance, if radius doubles then resistance is 1/16 and if radius is halfed then resistance is 16 times greater
R (Resistance)=1/radius^4
F=(R)^4
veins have larger diameter to compensate for less pressure and return blood to inferior vena cava
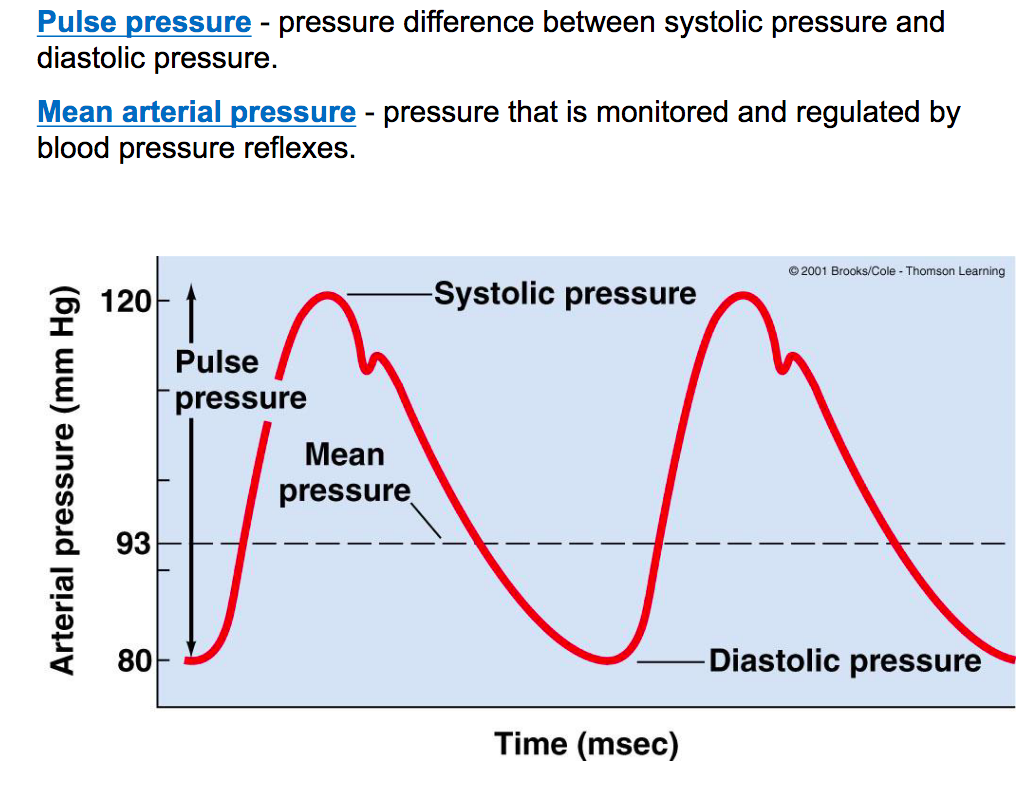
MAP (mean arterial pressure)
MAP= cardiac output X peripheral total resistance
-peripheral total resistance : arterial radius and blood viscosity
-assess the blood flow to the organs by looking at pressure in the arteries
Type of Arteries
Elastic : large arteries which are elastic, ex: aorta , are low resistance due to large lumen vessles. when blood goes from LV to arota, aorta expands to take in the blood and when it leaves, it recoils as the SV valves close to keep flow continous/laminar
Muscular : deliver to specific organs , have less elastin compared to elastic , has thickest smooth muscle and very active in vasoconstriction-play a large role in regulation of blood pressure
Arterioles: smallest arteries and the function is controlled by neural and horomonal , control minute-they control minute to minute flow by contracting or dilating , smaller ones which lead to capillary beds are made out of single layer of smooth muscle
Flow Trends
-either increase pressure to increase flow or vasodilate to decresase resistance : flow is proportional to pressure
flow is mostly to and from skeltal muscle, kidnesy, heart , GI but they alway maintain a minimal flow -during exercise blood is shunted
Vasoconstriction/Vasodilation
vasoconstriction : sympahtetic NE released by alpha adrengenic recepctors, cold, oxygen increases(body is producing more o2 that it can accomodate), co2 decreaes, vasopressin, agiotensin
vasodilation: heat increase, increase in o2, decrease in co2, plasma epi increase binding to beta
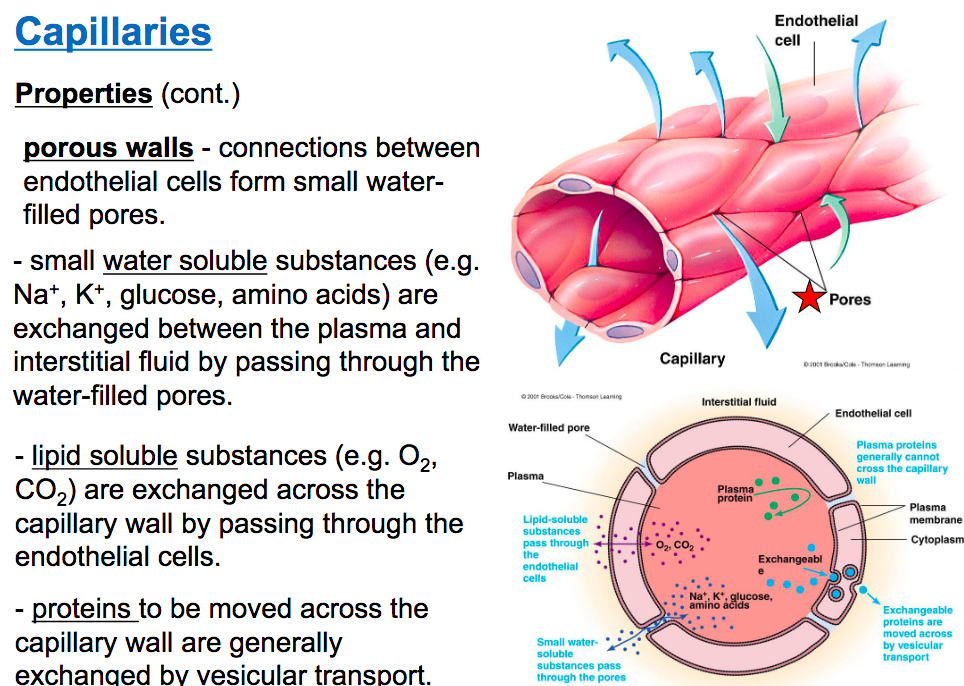
Capillaries
extremely small blood vessels that serve to exchange materials with blood and tissue
-large volume of blood avaliable to distribute, large surface area, and low velocity of blood flow
-smalll water filled pores between capillaries and endothelial cells are called porous walls -in these water pores Na, K, glucose is exhanged .
-lipid soluable substances o2, co2, pass from cappilariy wall to the endotheilial cell
-proteins cannot cross the capillary wall but they can be exhanged via vesicular transport to leave to the endotheilial cells
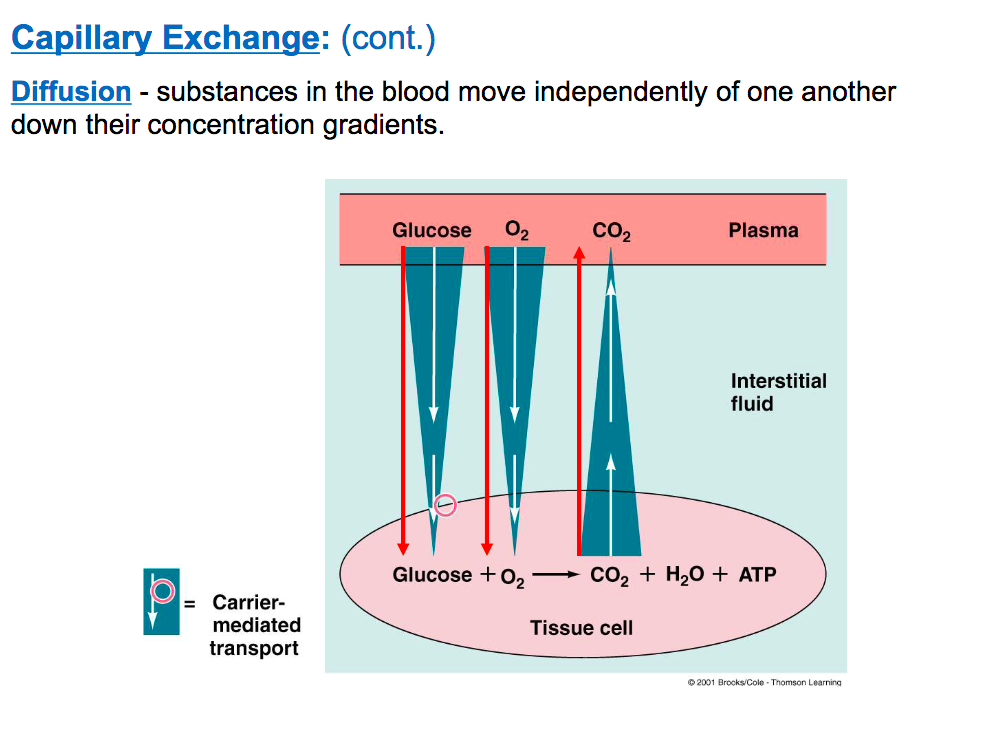
Capillary Exchange
ECF : makes up interestrial fluid and and plasma
exchange occurs between blood and interestrial fluid and exchange occurs via diffusion and bulk flow. glucoses uses a carried mediated transporter when there is too much glucose in the interestitial fluid
Bulk flow two types: into tissues: filtiration and into plasma: reabsorption
Venous System
veins: serve as a reservoir for blood and conduit for blood back to heart,have less smooth muscle and more elastin