PHAR 443-Liver, Exocrine Pancreas, and Gallbladder Disease EXAM #3
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Flow of Bile and Pancreatic Secretions
1. The hepatic ducts, which carry bile from the liver lobes, combine to form the common hepatic duct.
2. The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct.
3. The common bile duct and the pancreatic duct combine to form the hepatopancreatic
ampulla.
4. The hepatopancreatic ampulla empties bile and pancreatic secretions into the duodenum at the major duodenal papilla.
5. The accessory pancreatic duct empties pancreatic secretions to the duodenum at the minor duodenal papilla.
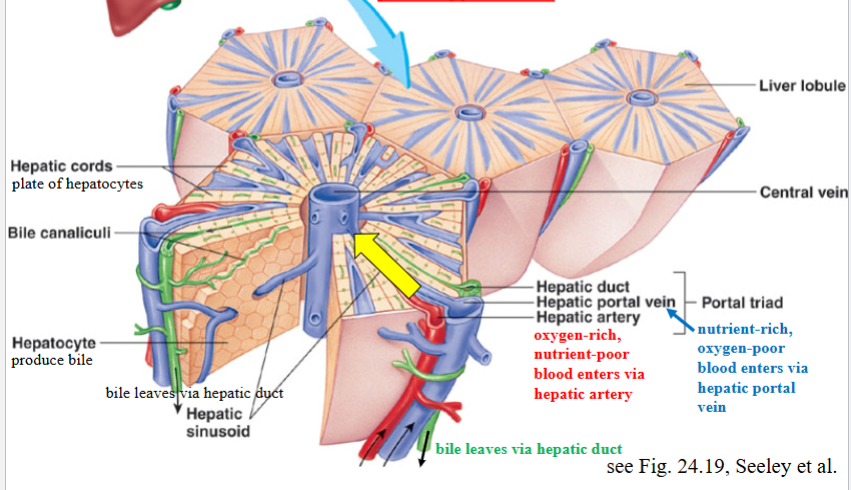
Hepatic Portal Vein: nutrient rich, oxygen poor
Hepatic Artery: oxygen rich, nutrient poor
Functions of the normal liver
1) Energy metabolism and substrate interconversion
◦ Glucose production through gluconeogenesis and glycogenolysis
◦ Glucose consumption by pathways of glycogen synthesis, fatty acid synthesis, glycolysis, and the tricarboxylic acid cycle
◦ Cholesterol synthesis from acetate, triglyceride synthesis from fatty acids, and secretion of both in VLDL particles
◦ Cholesterol and triglyceride uptake by endocytosis of HDL and LDL particles with excretion of cholesterol in bile, β-oxidation of fatty acids, and conversion of excess acetyl-CoA to ketones
◦ Deamination of amino acids and conversion of ammonia to urea via the urea cycle
◦ Transamination and de novo synthesis of nonessential amino acids
2) Protein synthesis functions
◦ Synthesis of various plasma proteins, including albumin, clotting factors, binding proteins, apolipoproteins, angiotensinogen, and insulin-like growth factor l
3) Solubilization, transport, and storage functions
◦ Drug and poison detoxification through phase I and phase II biotransformation reactions and excretion in bile
◦ Solubilization of fats and fat-soluble vitamins (A, D, E & K ) in bile for uptake by enterocytes hepatic artery
◦ Synthesis and secretion of VLDL and pre-HDL lipoprotein particles and clearance of HDL, LDL, and chylomicron remnants
◦ Synthesis and secretion of various binding proteins, including transferrin, steroid hormone–binding globulin, thyroid hormone–binding globulin, ceruloplasmin, and metallothionein
◦ Uptake and storage of vitamins A, D, and B12 and folate and iron
4) Protective and clearance functions
◦ Detoxification of ammonia through the rea cycle
◦ Detoxification of drugs through microsomal oxidases and conjugation systems
◦ Synthesis and export of glutathione
◦ Clearance of damaged cells and proteins, hormones, drugs, and activated clotting factors from the portal circulation
◦ Clearance of bacteria and antigens from the portal circulation
Hepatic Blood Flow
Total hepatic blood flow in normal adults under resting conditions is around 1.5 L/min, or 25% of cardiac output.
Of this, about 2/3 is supplied by the hepatic portal vein and the remainder by the hepatic artery.
Hepatic portal blood flow is normally under low hydrostatic pressure (about 10 mm Hg).
*Blood flow through the liver slows in people who have liver disease. When this happens, the pressure in the hepatic portal vein goes up and is called PORTAL HYPERTENSION
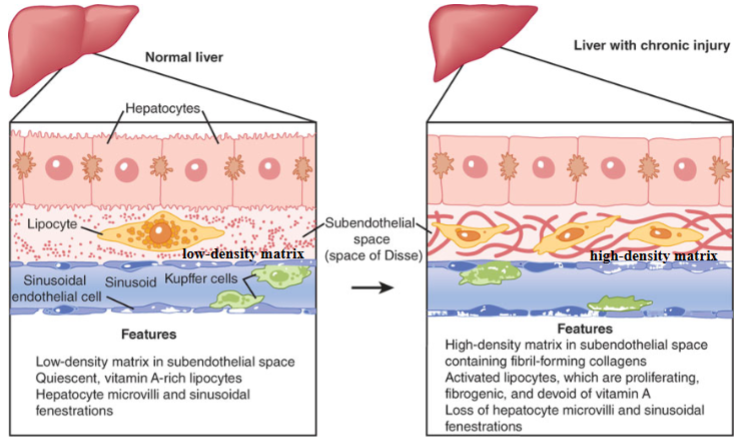
Changes in the Hepatic Subendothelial space during liver injury
Hepatic stellate cells (lipocytes) are normally quiescent but become activated with injury
Changes in the hepatic subendothelial space during liver injury. Cellular and matrix alterations in the space of Disse are critical events in the pathogenesis
of hepatic fibrosis. The activation of lipocytes, characterized by proliferation and increased fibrogenesis, is associated with the replacement of the normal low-density matrix with a high-density matrix. These alterations are likely to underlie, at least in part, the loss of both endothelial fenestrations (pores) and hepatocytic microvilli typical of chronic liver injury.
Portal Hypertension
Blood flow through the liver slows in people
who have liver disease. When this happens, the
pressure in the portal vein goes up
Liver Damage
Liver diseases can be acute or recurrent (chronic), focal or diffuse, mild or severe, and reversible or irreversible.
Inflammation/Steatosis
Liver fibrosis - formation of an abnormally large amount of scar tissue as it attempts to repair and replace damaged cells
Cirrhosis - chronic liver damage from a variety of causes leading to scarring and liver failure
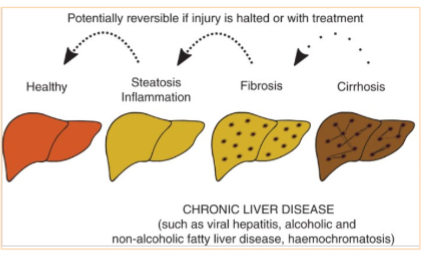
Hepatic Blood Flow-Cirrhosis
With fibrous, the liver becomes hard, shrunken, nodular, and impedes blood flow, this results in elevation of intrahepatic venous pressure, referred to as portal hypertension.
As a result, blood backs up and a substantial fraction of it finds alternative routes back to the systemic circulation, bypassing the liver.
Portal hypertension is a pressure in the portal venous system that is at least 5 mm Hg higher than the pressure in the inferior vena cava.
Sequalae of Cirrhosis
Portal Hypertension
Due to increased back pressure with hepatic obstruction,
Esophageal and intestinal/gastric varices (common circulation of upper GI and spleen)
Splenomegaly
Ascites: resulting from increased back pressure increases passage of fluid from the hepatic circulation into the intercellular space and peritoneal cavity
Peritonitis: stasis of blood flow may allow bacteria to gain entry into the peritoneum and circulation
Liver cell failure
Portal Hypertension → Esophageal Varices
High blood pressure in the portal vein (portal hypertension) pushes blood into surrounding blood vessels, including vessels in the esophagus. These blood vessels have thin walls and are close to the surface. The extra blood causes them to expand and swell. Varices also can develop in the small blood vessels in the upper part of the stomach.
If the pressure caused by the extra blood gets too high, varices can break open and bleed. Bleeding is an emergency that requires urgent treatment. Uncontrolled bleeding can quickly lead to shock and death.
Portal Hypertension → Splenomegaly
Splenomegaly and hypersplenism (overactive) are direct consequences of elevated portal venous pressure. Overactive spleen may lead to premature destruction of blood cells
Clinical Effects of cirrhosis of the liver
In cirrhosis, portal hypertension occurs and the blood is diverted around the liver rather than being filtered through the liver. This phenomenon, termed portal-to-systemic (or portosystemic) shunting
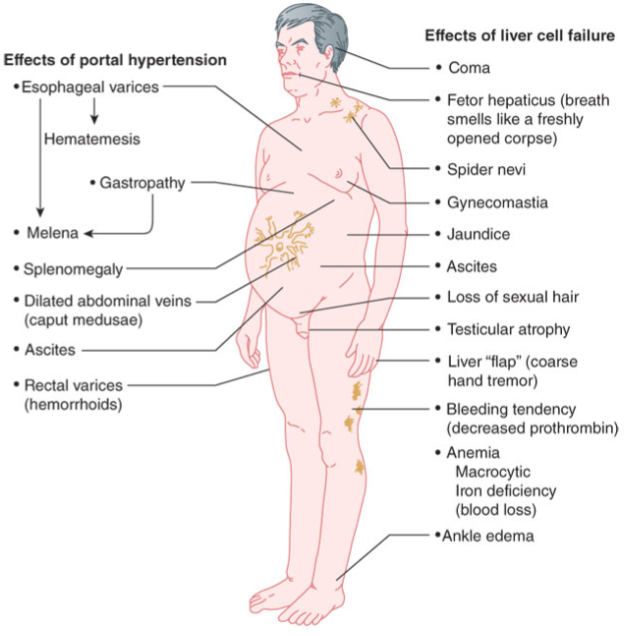
Liver Failure
Esophageal varices
fragile and can burst; bleeding can be fatal
Edema and ascites
decreased production of plasma proteins necessary to sustain proper colloid osmotic pressure and results in activation of the renin-angiotensin system
Fatigue
due to inability of liver to process waste products and other nutrients systemically
Hepatic encephalopathy
ranging from mild confusion to coma, resulting from inability to process intestinal ammonia
Nausea and diarrhea (variable)
inability to process nutrients normally
Jaundice
inability to metabolize heme and bilirubin
Anicteric sclera - white part of eye is white and healthy in appearance
Icteric sclera - white part of eye is yellow, a sign of jaundice
Bleeding
lack of clotting factor synthesis
-Serum testosterone is reduced in up to 90% of men with cirrhosis, with levels falling as liver disease advances.
Manifestations of Liver Dysfunction
Diminished Energy Generation and Substrate Interconversion
Carbohydrate metabolism
Impaired assembly of glycoproteins into membranes
Lipid Metabolism
Disturbance of lipid metabolism can result in syndromes of fat accumulation
In chronic, there is hyperlipidemia leading to subcutaneous accumulations of cholesterol termed xanthomas.
Protein Metabolism
Disturbance of protein metabolism can result in a syndrome of altered mental status and confusion known as hepatic encephalopathy.
Elevated blood concentrations of centrally acting toxins, including ammonia generated by amino acid metabolism.
Loss of Solubilization & Storage Functions
Disordered Bile Secretion – malabsorption of lipids and deficiency of fat-soluble vitamins
Buildup of bilirubin results in jaundice (icterus) in sclera and skin (anicterus=non-jaundice)
Impaired Drug Detoxification
Lipoprotein Dynamics and Dyslipidemias
Diminished Synthesis & Secretion of Plasma Proteins
Loss of Protective & Clearance Functions
Clearance of Bacteria and Endotoxins
Altered Metabolism of Ammonia
Altered Hormone Clearance in Liver Disease
Sodium retention and difficulty excreting water
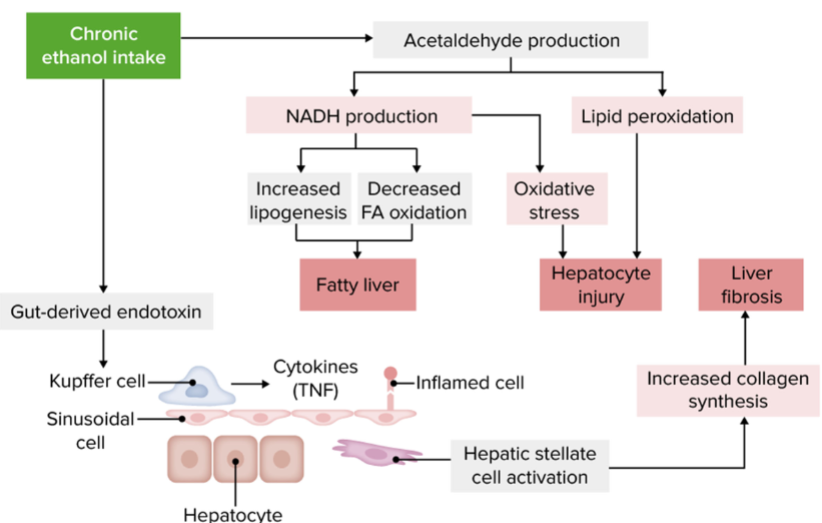
Alcohol and Liver Disease
Alcohol remains the 2 nd most common cause of liver cirrhosis after hepatitis C virus (HCV) infection in the United States, contributing to approximately 20% to 25% cases of liver cirrhosis.
Alcohol-related liver disease- caused by excessive consumption
In early stages of the disease, liver damage may be reversed if the person stops drinking.
Virtually all heavy drinkers develop fatty liver.
Up to 35% of heavy drinkers develop alcoholic hepatitis
Between 10-20% of heavy drinkers develop cirrhosis, usually after 10 or more years of drinking
In advanced alcoholic cirrhosis, the only treatment option may be a liver transplant. However, active alcoholics do not usually qualify as suitable organ recipients.
Alcoholic Liver Disease
Three major stages
Alcoholic Fatty Liver Disease – fatty acid oxidation is impaired, hepatocyte triglycerides are increased; readily seen on biopsy. May be seen with only 2 weeks of moderate ethanol ingestion. Reversible
Alcoholic hepatitis – hepatocellular necrosis (chemical damage) with hepatomegaly (enlargement), jaundice (inability to adequately process bilirubin) and fever (bacterial escape from hepatic sinusoids). Produced after many months/years of alcohol abuse (several episodes may occur throughout course of ethanol abuse). May be reversible
Alcoholic cirrhosis – hepatic scarring, collagen formation and diffuse connective tissue replacement. Fibrosis is the first stage of liver scarring. When scar tissue builds up and takes over most of the liver, it’s referred to as cirrhosis. Liver is firm in consistency. Normally low pressure filtration system of liver becomes hypertensive (i.e. portal hypertension). Irreversible
Chronic Ethanol Intake
Hematologic abnormalities
Splenomegaly and hypersplenism are direct consequences of elevated portal venous pressure.
Thrombocytopenia and hemolytic anemia occur as a result of both sequestration of these formed elements by the spleen and the depressive effect of alcohol on the bone marrow.
The frequent bruising and elevated prothrombin time in this patient highlight the coagulopathy seen in cirrhosis and chronic liver disease.
As a result of inadequate bile excretion, there is an impaired absorption of the fat-soluble vitamin K, a vitamin necessary for the activation of specific clotting factors. In addition, the inadequate hepatic synthesis of other clotting factors causes a coagulopathy.
Hepatitis
→ inflammatory process causing global liver cell death either by necrosis or apoptosis → hepatic dysfunction
Viral (ex. Hepatitis A-E)/Chemical (acetaminophen, isoniazid)/
Poison (ethanol) Induction
Symptoms: Highly variable: May be asymptomatic, with abnormalities detected in lab tests.
Various intensities: anorexia, fatigue, weight loss, nausea, vomiting, right upper quadrant abdominal pain, jaundice, fever, splenomegaly, and ascites.
Hepatic dysfunction may correlate with liver injury.
Although fewer than 10% of drug induced liver injury cases progress to acute liver failure, acetaminophen is now the most common cause of acute liver failure in the United States
Acute vs Chronic
Acute hepatitis; resolution in 3–6 months.
Chronic hepatitis; greater than 6 months
Chronic Viral Hepatitis
Viral hepatitis is the most common cause of chronic liver disease in the United States.
In approximately 5% of adult cases of HBV infection and 60– 85% of HCV infections, the immune response is inadequate to clear the liver of virus, resulting in persistent infection.
The individual becomes a chronic carrier, intermittently producing the virus and hence remaining infectious to others.
The severity of chronic hepatitis depends largely on the activity of viral replication and the response of the host’s immune system.
Hepatic Neoplasms
Hepatocellular adenoma
Female prevalence
Most commonly associated with oral contraceptive use
Usually benign, may present a liver function problem if progressive
Hepatocellular carcinoma
Male prevalence
Alcohol and androgen abuse as chemical causes.
Commonly associated with hepatitis B and C
The risk of developing HCC is increased 100-fold in those with chronic hepatitis B infection
The risk of developing HCC is increased 15- to 20-fold in those with chronic hepatitis C infection
Chronic hepatitis B and C account for 60–70% of all HCC cases in the United States.
Alcoholic cirrhosis, nonalcoholic steatohepatitis, and other causes account for most of the remaining U.S. cases
Cholelithiasis (gallstones)
Formed in gallbladder due to precipitation of cholesterol and other bile tract components (bilirubinates, calcium, etc)
May grow to large size stones, over years to decades, with or without symptoms (pain after meals, most common)
Cholesterol Stones
account for 80% of gallstones and are more commonly involved in obstruction and inflammatory
> 50% cholesterol
greater prevalence in women
Pigment Stones
Make <20% gallstones
Black pigment (calcium bilirubinate) – hemolysis and cirrhosis may be predisposing factors.
Brown pigment (calcium bilirubinate with salts of fatty acids) higher incidence in Asia, pathogenesis is highly debated.
Pathology of Cholelithiasis
Obstruction (pain, nausea and vomiting) due to increased contraction pressure of the gallbladder after meals.
If obstruction blocks the opening to the pancreas, pancreatitis may result (flank pain, nausea, increase in serum amylase and lipase).
A variety of surgical methods may be employed to treat these conditions.
Duodenum and Pancreas
As much as 1500 mL of pancreatic juice is secreted each day by a normal pancreas. Pancreatic juice contains water, ions, and a variety of proteins. The principal ions in pancreatic juice are HCO3−, Cl−, Na+, and K+. Of these, HCO3− is particularly important.
Acute Pancreatitis
Results from acute inflammation and destructive autodigestion of the pancreas and peripancreatic tissues
3rd most common hospital admission, when classified as a GI disease.
Common causes:
1st : Ethanol (occurs in less than 2–3% of heavy drinkers).
Tobacco increases incidence in drinkers.
2nd: Biliary disease
Viral (mumps virus, hepatitis A virus, HIV, cytomegalovirus), bacterial (Salmonella typhi, hemolytic streptococci), parasitic infection
Autoimmune disease
Hypertriglyceridemia, ketoacidosis
Drugs (including corticosteroids, thiazide diuretics, immunosuppressants, and chemotherapeutic agents) and toxins
Common symptoms:
*Sharp, deep abdominal flank pain, patient’s left abdomen, may radiate to the back.
Nausea and Vomiting
Fever (in 2/3 of patients)
Serum amylase elevation (may return to normal within 48-72 h even in the presence of progressive disease)
Serum lipase (declines more slowly)
Pathogenesis
Proteolytic activation due to obstruction, chemical/biochemical disruption and systemic release of proteolytic agents, pancreatic autodigestion and inflammatory response with cytokine release.
→Disease Progression:
Shock with severe hypotension and associated renal failure
Disseminated Intravascular Coagulation
Respiratory distress (pancreatic enzyme damage to the alveoli)
May be fatal if unresolved
Chronic Pancreatitis
In chronic pancreatitis, the parenchyma is chronically inflamed, leading to the progressive destruction of the acini, stenosis and dilation of the ductules, and fibrosis of the gland.
Symptoms may or may not mimic acute phase.
The major cause of chronic pancreatitis is chronic alcoholism, which accounts for about 70–80% of cases.
Pathologically, chronic pancreatitis is characterized by scarring and shrinkage of the pancreas resulting from acinus fibrosis and atrophy, and by ductule stenosis and dilation.
Pancreatic Carcinoma
3rd leading cause of cancer-related deaths in US.
Cigarette smoking has the strongest overall association and is thought to account for 1/4 of cases diagnosed. Exposure to N-nitroso compounds leads to pancreatic ductal hyperplasia, a possible precursor to adenocarcinoma.
Increased risk with chronic pancreatitis and genetics.
Abdominal pain, weight loss, anorexia most common, with jaundice in advanced disease.
Labs: increased lipase, LDH and AST increased, CT scan essential in diagnostics/grading.
Aggressive metastasis to liver, lung, etc.
Pancreatic Insufficiency
Reduction in exocrine pancreatic secretions.
Associated with chronic pancreatitis in adults vs. cystic fibrosis in children.
Weight loss, steatorrhea, diarrhea, hypocalcemia, Vit B 12 deficiency.
Exocrine enzyme substrate testing is essential for diagnostics.