PT 634 W1: intro and medical management
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
What are some non-modifiable risks of stroke?
Age
Race (Blacks, Hispanics, and Asians increased risk)
Sex (at < 60yrs old, men have increased incidence of stroke, > 60yrs equal incidence)
Genetic disorders, family history
Previous stroke or Transient Ischemic Attack (TIA)
Pregnancy
What are some modifiable and medical risk factors of stroke?
HTN Smoking DM High Cholesterol Obesity Physical inactivity Alcohol Smoking Cocaine Stress Cardiac *Afib Circulation disorders Malignancy Hep C/HIV
Why is important to prevent stroke?
Integral part of rehabilitation
How do we identify patients that are at high risk?
The group at highest risk for stroke is patients with stroke!
What are some life stytle modifications that can reduce SBP?
weight reduction
DASH diet
sodium restriction
physical activity
limit alcohol intact
What is normal BP
systolic less than 120 and less than 80 diastolic
What is elevated BP?
120-129 systolic
and
less than 80 diastolic
What is high BP stage 1
Systolic 130-139 or 80-89 diastolic
What is high BP stage 2?
140 or higher Systolic
or 90 or higher diastolic
What is hypertensive crisis
higher than 180 systolic and/or higher than 120 diastolic
What is the signs of stroke FAST?
face
arm
speech
time
What does F stand for in fast
face ask the person to smile. is one side face drooping
What does A stand for in fast
arms. ask person to raise arm. is one arm weak?
What does S stand for in fast
speech. ask the person to speak. is their speech slurred?
What does T stand for in fast
time call 911 right awway at first sign of stroke
What is BEFAST
balance - does patient have sudden loss of balance
eyes - has person lost vision in one or both eyes
face
arms
speech
time
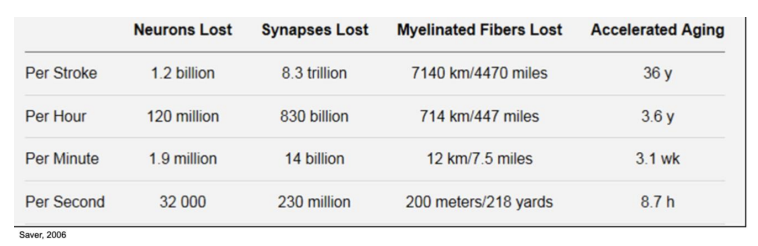
What factor is most important when someone suddenly has stroke
TIME! GET HELP NOW
What are some lifestyle modification for stroke?
Self-directed and self management approaches
Multidisciplinary education
Modifiable risk factors
Mediterranean
Diet
Exercise: 5 days, >150mins moderate
Smoking, alcohol, and drug cessation
Medication compliance: BP (<130/80), cholesterol, HL, afib, etc
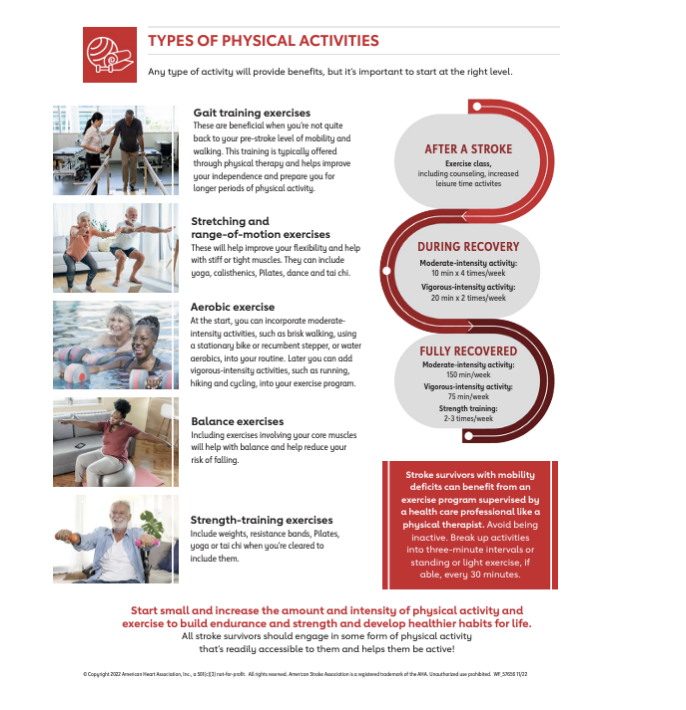
Physical activity recommendations after stroke
What are types of stroke (CVA)?
ischemic (infarcts, infarction) 87%
hemorrhagic (13%)
What are the types of ischemic strokes?
◦ Transient Ischemic Attack (TIA)
◦ Embolic or Thrombotic
◦ Lacunar Stroke
What are the types of hemorrhagic strokes?
◦ Subarachnoid Hemorrhage (SAH) ◦ Intracerebral Hemorrhage (ICH) ◦ Intraventricular Hemorrhage (IVH)
What is the initial presentation of a hemorrhagic stroke?
often present with more severe symptoms initially, such as sudden and intense headaches, nausea, vomiting, and rapid neurological deterioration due to the bleeding in the brain. This can lead to a higher mortality rate initially
What is the recovery of a hemorrhagic stroke?
While the initial prognosis can be worse, some individuals with hemorrhagic stroke may show improvement over time, especially if the bleeding is controlled and brain damage is limited. The recovery can be more variable, but there can be significant recovery in certain cases, especially with timely medical intervention and rehabilitation
What is the initial presentation of a ischemic stroke?
Ischemic strokes may not seem as severe initially since they are caused by a blockage (rather than bleeding) and the brain tissue is not immediately exposed to blood. Symptoms might be less dramatic in the early stages
What is the recovery of a ischemic stroke?
However, ischemic strokes tend to lead to greater long-term impairments because the ischemia (lack of blood flow) can cause permanent brain damage if not rapidly treated. In the long term, individuals with ischemic strokes may face more significant functional impairments, as the brain tissue that was deprived of oxygen may not recover fully.
Ischemic stroke causes
embolism or thrombosis
What is an embolic stroke?
occurs when a blood clot or other debris forms elsewhere in the body and travels through the bloodstream to the brain, blocking a blood vessel
is a sudden onset
Sources:
• Patent Foramen Ovale • Ischemic heart Disease • Arrhythmia (A- FIB) • Endocarditis • Valvular Disease • Atherothrombotic, cholesterol
What is a thrombotic stroke?
occurs when a blood clot (thrombus) forms in one of the arteries supplying blood to the brain, leading to a blockage and reduced blood flow
Gradual onset of symptoms, often developing over hours or days
Sources:
• Atherosclerosis • HTN and DM increase risk for plaque formation • Non-atheromatous diseases of the vessel wall ◦ Collagen disease ◦ Vasculitis ◦ Fibromuscular dysplasia ◦ Trauma
What is a transient ischemic attack?
• Sudden onset of focal neurological symptoms due to inadequate blood supply.
• Resolve within 24hrs or less with no residual deficits.
• Most often caused by emboli
• 5-10% of patients will have a stroke within 1yr
• TIAs are often a warning sign for future strokes. Timely medical intervention is crucial to prevent permanent damage
TIAs are often a _______ for future strokes. Timely medical intervention is crucial to prevent permanent damage
warning sign
What is a lacunar stroke?
type of ischemic stroke caused by occlusions of small penetrating arteries in the deep subcortical regions of the brain, leading to the formation of small cavities or "lacunae.“
Onset of focal deficit may be sudden or progress over several hours, some are asymptomatic.
• Associated with hypertension
Best prognosis
• CT – might show deep, small infarct, some too small to visualize
• MRI – shows even small infarcts, preferred
Common location for lacunar strokes?
• Basal ganglia (motor control issues)
• Internal Capsule (motor and sensory deficits)
• Pons (vital functions: breathing & eye movements)
• Thalamus (sensory deficits)
Acute signs and symptoms of ischemic stroke?
Dysarthria
Dysphagia
Hemiplegia/hemiparesis
Acute mental status changes
Ataxia
Facial droop
Sensory loss
Hemianopia or other visual changes
what are Medical Differential Diagnosis-ischemic stroke?
• Hyper/hypoglycemia • Migraine • Seizures • Space occupying lesions (tumor, abscess) • Drug Toxicity • Psychogenic • Hypertensive/Wernicke’s encephalopathy
What are some medical management of ischemic stroke clinical evaluation?
• Sudden onset of symptoms: weakness, numbness, speech, vision, coordination •
Neurologic assessment, NIH stroke scale
• Code stroke
What are some medical management of ischemic stroke imaging?
• CT/A – can show early hemorrhagic changes (bleeding)
• MRI/A – earlier detection of ischemic changes, infarcts
What are some medical management of ischemic stroke additional tests?
• CT/MRI Angiogram- evaluate blood vessel barrowing or blockages
• Carotid ultrasound- plaque or stenosis
• Echocardiogram- find source of embolism
What are some medical management of ischemic stroke lab studies?
• To rule out other conditions (e.g., infections, blood clotting disorders) and assess risk factors (e.g., cholesterol, glucose) • CBC, glucose, electrolyte, PT/PTT/INR, cardiac enzymes, hypercoagulable work up
What are some medical management of pharmacology of ischemic stroke?
Fibrinolytics: tPA
Overview of Fibrinolytics: tPA
◦ Alteplase (Activase) for acute ischemic strokes
◦ Dissolves clot and restores blood flow
◦ Needs to be administered within 4.5 hrs of stroke
◦ Optimal 3 hours
◦ Risk of hemorrhagic conversion
◦ Dramatically improves prognosis
tPA outcomes for ischemic stroke from study
◦ Patients treated with tPA are 30% more likely to experience minimal or no disability at 3 months.
◦ Average LOS shorter
◦ Discharge home vs rehab or nursing home
What are some surgical management of ischemic stroke?
•Carotid Angioplasty and stenting •Mechanical thrombectomy •Carotid Endarterectomy
What is a subarachnoid hemorrhage (SAH)?
•Subarachnoid hemorrhage (SAH) is bleeding into the space between the brain and the membranes covering the brain (subarachnoid space)
common causes:
• Ruptured aneurysm (most common cause). • Arteriovenous malformations (AVMs). • Trauma or head injury. • Cerebral vasculitis or other vascular conditions
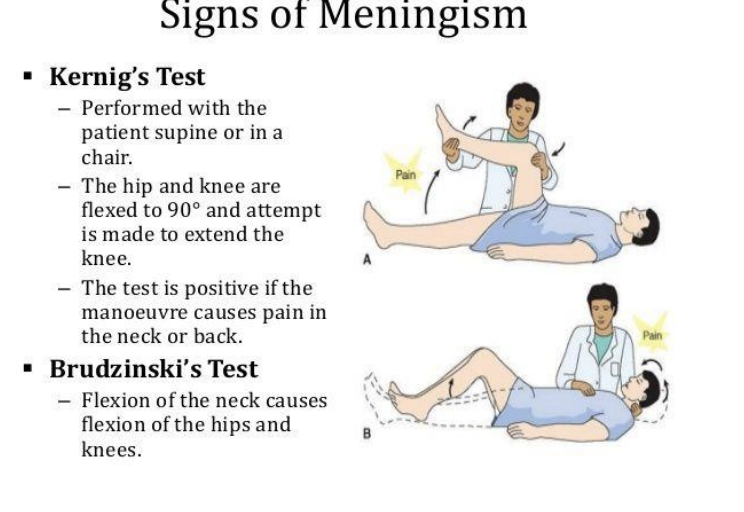
What are some subarachnoid SAH signs/symptoms?
Severe, sudden headache “worst headache of my life”: WHOL
Neck stiffness – Brudzinski sign
Knee extension-Kernig’s sign
Photophobia
Nausea, vomiting
Focal neurological deficits
10-25% of pts also have a seizure in first few minutes
What is kernigs and bruzkinski test?
What are some medical management of subarachnoid hemorrhage?
Imaging
• CT /A– most sensitive • MRI/A – inferior to CT for SAH • Cerebral angiography – looks at vascular anatomy, site of bleed, aneurysms
Lab studies
– CBC, electrolytes, serum chemistry panel, PT/PTT/INR, blood typing/screening
Other
• Protect airway • Manage BP (patient specific) • Manage hydrocephalus/intracranial pressure • Monitor for vasospasm
differential diagnosis of subarachnoid hermorrhage?
• Hyper/hypoglycemia • Migraine • Seizures • Tumor • Abscess • Meningitis
Vasospasm complication for SAH
• Narrowing of IC vessels due to smooth muscle cell contractions
• Delayed cerebral ischemia
• Onset 4-20 days
• Most deadly complication
• Diagnosed by angiogram •
Monitored by Transcranial Dopplers (TCDs) and neuro exams
• HA, lethargy
Vasospasm treatment
• Triple H therapy (hypertension, hypervolemia, hemodilution)
• Meds to increase BP, large amounts of fluids • PT precautions
• Intraarterial vasodilators
• Balloon dilatation
SAH increased ICP complication
• Increased ICP >15mmHg
• Brain herniation: displacement of brain parenchyma
• Midline Shift: lateral displacement of falx cerebri
• Hydrocephalus
symptoms of increased ICP?
papilloedema, AMS, LOC, HA, BP, sz, posturing
ICP medical management external ventricular drain
• Catheter inserted into ventricles to drain excess CSF
• Indications: hydrocephalus, increased ICP, post SAH, post-op
• Short term, Emergency management
ICP medical management external ventricular drain pt considerations monitoring ICP
• SS increased ICP= HA, nausea, AMS, vitals • Avoid sudden head movements
• Keep EVD transducer aligned with external auditory meatus
ICP medical management external ventricular drain pt considerations positioning
• HOB elevated to 3-45 degrees for optimal drainage
• Avoid kinks or tension on tubing
ICP medical management external ventricular drain pt considerations activity tolerance
• Mobilization is safe!
• EVD MUST BE Clamped for mobilization- communicate with RN
What is ventriculoperitoneal shunt (VPS)?
•The VPS helps to drain excess CSF from the brain to the abdominal cavity, where the fluid is absorbed by the body, relieving pressure on the brain (internal)
Components
• Ventricular Catheter: inserted into ventricle to drain excess CSF
• Shunt abdomen, regulates flow of the CSF to abdominal cavity
• Peritoneal Catheter: Tube that directs drained CSF to the peritoneal cavity in abdomen so fluid is absorbed by body
• Long-term solution (i.e NPH, congenital conditions)
• Increased mobility & functionality, less monitoring
VPS PT considerations
Monitor for SS indicating increased ICP (can’t see value
What is an intracerebral hemorrhage (ICH)?
• Intracerebral hemorrhage (ICH) is a type of stroke where a blood vessel in the brain ruptures, leading to bleeding within the brain tissue
• 8-13% of all strokes
• Causes: HTN, Aneurysm, AVMs, Trauma, drug abuse, coagulation disorders or anticoagulant use
Intracerebral hemorrhage keypoint?
• Key Point: ICH is a medical emergency with high mortality and acute neurological disability, making rapid diagnosis and intervention critical.
• Rapidly expanding bleed can lead to unconsciousness or death, will cause damage to brain cells surrounding hemorrhage.
• More likely to result in death or disability than an ischemic stroke or a SAH
ICH signs and symptoms
Sudden onset of headache followed by decreased consciousness Hemiparesis Sensory changes Hemianopia Dysarthria Ataxia, LOB Vomiting
most common location of ich?
◦ Basal ganglia (40-50%) ◦ Lobar regions (20-50%) ◦ Thalamus (10-15%) ◦ Pons (5-12%) ◦ Cerebellum (5-10%) ◦ Other brainstem sites (1-5%
ICH differential diagnosis?
Ischemic Stroke SAH AVM HTN Encephalopathy Hyper/hypoglycemia Migraine Seizures Space occupying lesions (tumor, abscess
ICH medical management initial stabilization
• Airway management • BP control <140 mmHg • IV antihypertensives • Labetalol, nicardipine, esmolol • Reduce ICP
ICH medical management imaging
CT
ICH medical management hematoma expansion prevention
• Reverse anticoagulation • Vit K, prothrombin complex concentrates • Platelet transfusion
Medical Management of ICH surgical intervention
• Surgical Evacuation of blood • Craniotomy • Craniectomy
What precautions are present with craniectomy?
helmet precautions
Medical Management of ICH seizure prophylaxis
Anticonvulsants
What is a cerebral aneurysm?
• An abnormal ballooning or dilation of a blood vessel in the brain due to a weakness in the vessel wall.
•Can lead to SAH or ICH
What is a saccular (berry) aneurysm?
• Most common type (80%), often located at branch points in arteries, especially the circle of Willis
What is a fusiform aneurysm?
• Diffuse widening of a vessel, commonly affecting large arteries • Less common than saccula
What is a Mycotic Aneurysms
Caused by infection, usually bacterial, leading to weakened vessel wall
What are some cerebral aneurysm risk factors?
• HTN • Smoking • Family History • Genetic Conditions (Ehlers-Danlos) •Previous SAH •Age (30-60 year) •Gender
What are some cerebral aneurysm signs and symptoms?
Unruptured aneurysm: Often asymptomatic or nonspecific
Ruptured aneurysm
• Sudden severe HA (“Worst HA of my life” • Nausea/vomiting • Neck Stiffness • Photophobia • Loss of consciousness • Neurologic deficits
Cerebral aneurysm diagnosis?
• CT scan: first-line for suspected ruptured aneurysm, reveals blood
• MRI/MRA: Can detect unruptured aneurysm and provide detailed vascular imaging
• Cerebral Angiography: The gold standard for detailed visualization of aneurysms, especially for surgical plannin
Cerebral aneurysms treatment?
• Conservative Management (for small, unruptured aneurysms) • Blood pressure control and lifestyle modification (e.g., smoking cessation)
• Surgical Clipping: Clip aneurysm at base to prevent rupture
• Endovascular Coiling: minimally invasive procedure placing coils inside aneurysm to promote clotting and seal it off
• Flow Diversion: New technique that uses stent to reroute blood flow, reducing pressure on aneurysm
What is arteriovenous malformation AVM?
• AVM is a rare, abnormal tangle of arteries and veins that disrupts normal blood flow, bypassing the capillary system. This creates a high-flow, low-resistance pathway between arteries and veins
Etiology
• Most AVMs are congenital, arising during fetal development • Acquired AVMs can occur due to trauma, surgery or radiation therapy • Often diagnosed in young adults • Tend to present with hemorrhages at a younger age compared to aneurysms (20-40 years old)
imaging for AVM?
• CT scan: Initial imaging for hemorrhage or mass effect- may mask AVM if large bleed
• MRI/MRA: Provides detailed information about the location, size, and structure of the AVM
• Cerebral Angiography: Gold standard for definitive diagnosis, used to visualize the blood vessels feeding the AVM and draining veins.
AVM complications?
• Asymptomatic until they cause significant neurological deficits or bleeding.
• Early detection, through imaging, and appropriate treatment are essential to minimize complications.
• SAH or ICH
• Neurologic Damage 2/2 to bleed or ischemia
• Recurrence after treatment
AVM treatments?
• Surgical Resection via craniotomy
• Endovascular Embolization (glue or coils) to decrease AVM blood supply
• Sterotatic Radiosurgery (Gamma knife) to shrink or obliterate the AVM
• Useful in deep or hard to reach AVMs
What are medical complications post stroke?
Neurologic
Musculoskeletal
Cardiopulmonary
Integumentary
Gastrointestinal
Urinary
Depression
Fatigue
Central pain
Insomnia
Examples of antiplatelet medications?
Aspirin, Aggrenox, Clopidogrel
Examples of anticoagulants medication?
Warfarin, Heparin
What are examples of statin medication?
: simvastatin, atrovastatin
to lower cholesterol
What are some blood pressure medications?
ARBs (valsartan), ACE inhibitors (lisinopril) , Beta-blockers (metropolol), Calcium channel blockers (nicardipine), Diuretics (lasix)
What are some examples of antieleptics medications?
carbamazepine, valproic acid, phenytoin
Settings for Patients with Stroke: acute inpatient care consist of?
Acute IP care
◦ Primary Stroke Center, Comprehensive Stroke Center, Acute Stroke-Ready Hospital ◦ ICU/step-down ◦ Triage- Discharge planning
Settings for patients with stroke: acute inpatient care discharge planning locations
◦ Acute Rehabilitation
◦ Subacute Rehabilitation
◦ LTACH
Home with
◦ Outpatient
◦ Day Rehab
Stroke early mobility: immobility and ICU
• Impact on strength/function, LOS, cost, delirium, QOL, infection, pulmonary system
Stroke early mobility: AVERT study and expansion with 24H
• RCT comparing usual care and VEM
• Unfavorable outcome of disability at 3 months
• QOL and disability the same at 12 months
Stroke early mobility: recommendations
after 24 hours
short and frequent mobility
interdisciplinary communication
Safety checklist for stroke patients
EVD closed
ICP controlled for 24H with no mannitol or hypertonic saline
No active titration of vasopressors or antihypertensives
CAM-ICU negative for delirium
Stable neurologic exam
SAH-aneurysm treated
24H after onset of symptoms
What is a inpatient acute rehab setting?
• Free standing or hospital based
•CARF accredited, stroke certified
•Must have a medical necessity
• Must tolerate 180 minutes of therapy daily for at
least 5 days week
• Split between PT, SLP, OT
• Goal: Bridge between Acute care and next level of
care
◦ Possible Discharge locations
◦ Home PT
◦ Outpatient PT
◦ Skilled Nursing with or without subacute rehabilitation
◦ Back to acute care
Goal is Home
◦ Assess current function + prognosis
◦ Assess home environment
◦ Caregiver support
◦ Equipment needs
What is the subacute rehab setting?
◦ Located in a SNF(skilled
nursing facility) or hospital
based
◦ Not CARF accredited
◦ Less intense
◦ Needs 24hour care
What is the long-term acute care hospital setting (LTACH)
Under Medicare, the patient must need
more than 25 days of hospitalization.
◦ Average LOS =30 days
Typically, patients require:
• Prolonged ventilator use or weaning
• Ongoing dialysis for chronic renal failure
• Intensive respiratory care
• Multiple IV medications or transfusions
• Complex wound care/care for burns
•May Discharge to
• AIR
• Subacute rehabilitation
• Home
What is the home/outpatient setting for patients post stroke?
Outpatient
◦ 1 discipline
Day Rehab
◦ 2-3 disciplines
◦ 3 hours a time
Home Therapy