Bone Marrow Failure
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
What is the role of healthy bone marrow in the body?
Healthy bone marrow functions as a superb blood cell factory, producing red cells, white cells, and platelets, and increasing production in response to bleeding or infection.
What happens when bone marrow cell production fails?
When bone marrow production fails, normal levels of red cells, white cells, and platelets begin to fall due to inadequate erythroid precursors and altered stem cell differentiation and function.
What is a common laboratory finding in bone marrow failure?
Pancytopenia, a reduction in red blood cells, white blood cells, and platelets, is commonly observed in both peripheral blood and bone marrow.
What are some common causes of bone marrow failure anemia?
infections, drugs, radiation, and chemical exposures.
How does bone marrow failure affect blood cell production?
It results in a reduction or complete cessation of blood cell production, or it may lead to increased destruction of blood cells within the bone marrow.
What can cause destruction or injury to hematopoietic stem cells?
drugs, chemicals, radiation, viral infections, or immune-mediated damage.
What is a consequence of injury to the stem cells in bone marrow failure anemias?
The injured stem cells may undergo premature death and senescence, reducing their ability to produce blood cells.
What factors can lead to ineffective hematopoiesis in the bone marrow?
mutations or nutritional deficiencies such as vitamin B12 or folate deficiency
How does disruption of the bone marrow microenvironment contribute to anemia?
It can decrease the levels of hematopoietic growth factors and hormones, impairing blood cell production.
What happens when the bone marrow hematopoietic tissue is replaced by abnormal cells?
Abnormal cells take their place which disrupts normal blood cell production, contributing to bone marrow failure.
What is aplastic anemia?
a rare disease characterized by the failure of the bone marrow (BM) to produce blood cells
What are the two types of aplastic anemia?
acquired or inherited.
What are the four main elements that characterize aplastic anemia?
Peripheral blood pancytopenia (low RBCs, WBCs, and platelets)
Reticulocytopenia in peripheral blood (no polychromasia due to reduced erythropoiesis)
Bone marrow failure due to depletion of BM cells and replacement with fat cells (hypocellular BM)
Decrease in hematopoietic stem cells (decreased CD34 marker in BM)
What happens to the bone marrow in aplastic anemia?
the bone marrow fails to produce blood cells and is replaced with fat cells, leading to a hypocellular marrow.
What is reticulocytopenia in aplastic anemia?
It is the absence of reticulocytes in the peripheral blood, which occurs due to reduced erythropoiesis
What are the suggested mechanisms for the etiology of aplastic anemia?
It can be caused by immunological mediated suppression or intrinsic abnormalities of stem cells.
What are the two main categories of aplastic anemia?
primary and inherited.
What percentage of aplastic anemia cases are acquired?
80%-85% of cases.
How is acquired aplastic anemia further categorized?
idiopathic (40%-70%) and secondary (10%-15%) causes.
What are some secondary causes of acquired aplastic anemia?
drugs (30%), chemical agents (dose-dependent or idiosyncratic), physical agents, and viral infections.
What percentage of aplastic anemia cases are inherited?
15%-20% of cases.
What is Fanconi anemia, and how is it related to aplastic anemia?
It is a rare, inherited, recessive autosomal disorder that involves defects in DNA repair and is associated with multiple congenital abnormalities. It is one of the inherited causes of aplastic anemia.
What are some common symptoms of aplastic anemia?
pallor, fatigue, weakness, headache, dizziness, nausea, and shortness of breath.
What bleeding-related symptoms are associated with aplastic anemia?
fever, bruising, nosebleeds, blood in the stool, bleeding gums, and sinus tenderness.
Is splenomegaly commonly seen in aplastic anemia?
No, splenomegaly is not typically seen in aplastic anemia. The spleen is usually normal.
What oral symptoms may appear in patients with aplastic anemia?
oral thrush and oral leukoplakia, especially in cases of Dyskeratosis congenita.
What lab findings are typically seen in patients with aplastic anemia?
pancytopenia
leukopenia
thrombocytopenia
reticulocytopenia
What does the peripheral blood (PB) show in aplastic anemia?
normochromic, normocytic
macrocytic anemia
red cell distribution width (RDW) is typically normal.
What is seen on a bone marrow biopsy in aplastic anemia?
few blood cells and blood cell precursors, with hypocellularity
What happens to hematopoietic stem cells in aplastic anemia?
there is depletion of hematopoietic stem cells, which is indicated by a reduced CD34 marker in the bone marrow.
How is aplastic anemia suspected?
when two or three of the cell counts (RBC, WBC, and platelets) are extremely low.
How is a definitive diagnosis of aplastic anemia made?
if a marrow sample (biopsy) shows a great reduction in the number of cells in the marrow, specifically a decrease in hematopoietic stem cells, which can be indicated by reduced CD34 markers.
What are the bone marrow findings in aplastic anemia?
a markedly hypocellular marrow with large empty spaces, increased fat cells, fibrous stroma, and scattered or clustered foci of lymphocytes and plasma cells.
What other findings might accompany marrow failure in aplastic anemia?
bacterial infections, hemorrhage, and other complications related to reduced blood cell production.
What other pancytopenia conditions can aplastic anemia be differentiated from
leukopenia or myelodysplastic syndromes
What is the treatment for aplastic anemia?
transfusions
drug therapies
blood stem cell transplantation
immunosuppressive therapy (IST).
What is the survival rate for patients with aplastic anemia undergoing blood stem cell transplantation?
The 10-year survival rate for children is 91%, while for adults, it is 74%.
What are the risks associated with immunosuppressive therapy (IST) for aplastic anemia?
There is a risk of developing conditions such as paroxysmal nocturnal hemoglobinuria (PNH), myelodysplasia, and leukemia.
What is the first step in the autologous transplant process?
The first step is collection, where stem cells are collected from the patient's bone marrow or blood.
What happens after stem cells are collected in an autologous transplant?
The processing step follows, where the collected blood or bone marrow is purified and concentrated to isolate the stem cells.
How are stem cells preserved in an autologous transplant?
Through cryopreservation, where blood or bone marrow is frozen to preserve the stem cells.
What treatment does the patient undergo before receiving the stem cells?
The patient receives high-dose chemotherapy and/or radiation therapy to eliminate diseased cells.
How are the preserved stem cells returned to the patient?
In the reinfusion step, the thawed stem cells are reinfused into the patient's bloodstream.
What is the difference between an autologous and allogeneic transplant in terms of the donor?
In an allogeneic transplant, stem cells are collected from a donor, while in an autologous transplant, they come from the patient themselves.
What defines severe aplastic anemia based on peripheral blood criteria?
PMN (polymorphonuclear cells) < 500/ul
Platelets < 20,000/ul
Reticulocytes < 1% (corrected for hematocrit)
What defines very severe aplastic anemia based on peripheral blood criteria?
PMN (polymorphonuclear cells) < 200/ul
What is Fanconi anemia?
It is a congenital condition characterized by aplastic or hypoplastic anemia with progressive pancytopenia due to a FANC gene defect.
What type of inheritance pattern is seen in Fanconi anemia?
an autosomal recessive inheritance pattern and accounts for about 20% of childhood onset aplastic anemia
What congenital abnormalities are associated with Fanconi anemia?
Microencephaly (small head)
Short stature
Brown skin pigmentation
Thumb malformation
Internal strabismus (crossed eyes)
Genital hypoplasia (underdeveloped genital organs)
Kidney malformation
Mental retardation
How does Fanconi anemia compare to idiopathic aplastic anemia in lab results?
They are similar to those of idiopathic aplastic anemia, with pancytopenia.
Increase in HbF and HbA
Chromosomal fragility.
What is a diagnostic test for Fanconi anemia?
It involves adding diepoxybutane or mitomycin C to cultured cells, which induces chromosomal breakage, a hallmark of the condition.
What are the risks associated with Fanconi anemia?
Leukemia
Myelodysplastic syndrome
Other cancers
What is the prognosis for individuals with Fanconi anemia?
Bone marrow failure typically occurs by age 30 in individuals with Fanconi anemia.
What treatments are available for Fanconi anemia?
Transfusions
Androgens (hormones to stimulate red blood cell production)
Bone marrow transplantation (a potential cure)
What is Pure Red Cell Anemia (PRCA)?
It is a rare disorder characterized by erythropoiesis failure in the bone marrow, specifically affecting the Burst-Forming Unit-Erythroid and Colony-Forming Unit-Erythroid precursors only.
What causes Pure Red Cell Aplasia (PRCA)?
It can be acquired or hereditary. In acquired cases, it may be associated with viral infections, drugs, or autoimmune disorders.
Is Pure Red Cell Aplasia more common in males or females?
It is more common in females than in males, with a female-to-male ratio of 2:1.
What is Diamond-Blackfan Syndrome?
It is a congenital erythroid hypoplastic disorder that typically presents in early infancy, characterized by a defective stem cell function, specifically involving ribosomal proteins (RPS genes).
What causes Diamond-Blackfan Syndrome?
a genetic defect in ribosomal proteins (RPS genes), leading to impaired erythropoiesis, and the condition is resistant to erythropoietin.
What type of anemia is associated with Diamond-Blackfan Syndrome?
normocytic, normochromic, or macrocytic in nature, with reticulocytopenia
What does the bone marrow look like in Diamond-Blackfan Syndrome?
It shows erythroid hypoplasia, meaning a reduced number of erythroid precursors, while the myeloid and megakaryocyte cellularity remains normal.
What is the M:E ratio in Diamond-Blackfan Syndrome?
The M:E ratio is increased in Diamond-Blackfan Syndrome, reflecting a decreased number of erythroid precursors compared to other blood cell lines.
What is Congenital Dyserythropoietic Anemia (CDA)?
a hereditary anemia characterized by ineffective erythropoiesis and splenomegaly
How many types of CDA are there, and how are they classified?
There are three types of CDA, classified based on bone marrow findings and serological tests:
CDA-I
CDA-II (HEMPAS)
CDA-III
What are the characteristics of CDA-I?
Megaloblastic changes in the erythroid precursors
Presence of binuclearity and internuclear chromatin bridges
Macrocytic anemia (large red blood cells)
This type follows an autosomal recessive inheritance pattern.
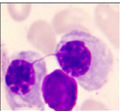
Chromatin bridging seen with CDA I
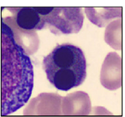
Binuclearity seen with CDA II
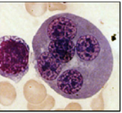
Giant erythroid precursors seen with CDA III
What is HEMPAS and which type of CDA is it associated with?
Hereditary Erythroblastic Multinuclearity with Positive Acidified Serum is associated with CDA-II, the most common form of CDA.
What is HEMPAS or CDA II characterized by
Binuclearity and multinuclearity of erythroid precursors
Normocytic anemia (normal-sized red blood cells)
Positive acidified serum test and negative sucrose lysis test
What are the features of CDA-III?
Giant erythroid precursors with more pronounced multinuclearity
Macrocytic anemia
Unlike CDA-I and CDA-II, CDA-III follows an autosomal dominant inheritance pattern.
How does the inheritance pattern differ between CDA-I, CDA-II, and CDA-III?
CDA-I and CDA-II are inherited in an autosomal recessive manner.
CDA-III follows an autosomal dominant inheritance pattern.
What is Anemia of Systemic Disorders?
It refers to anemia that arises as a result of chronic systemic conditions such as chronic renal disease, endocrine disorders, and other disorders that affect the bone marrow.
How does chronic renal disease contribute to anemia?
In chronic renal disease, anemia occurs due to a decrease in erythropoietin production. Erythropoietin is a hormone that stimulates the bone marrow to produce red blood cells. When erythropoietin production decreases, the production of red blood cells is reduced, leading to anemia.
What is myelophthisic anemia?
a type of anemia where myeloid and erythroid cells in the bone marrow are replaced by abnormal cells, such as cancer cells. This displacement of stem cells leads to an insufficient amount of blood cells, which causes anemia.