cardiac physiology combined new
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
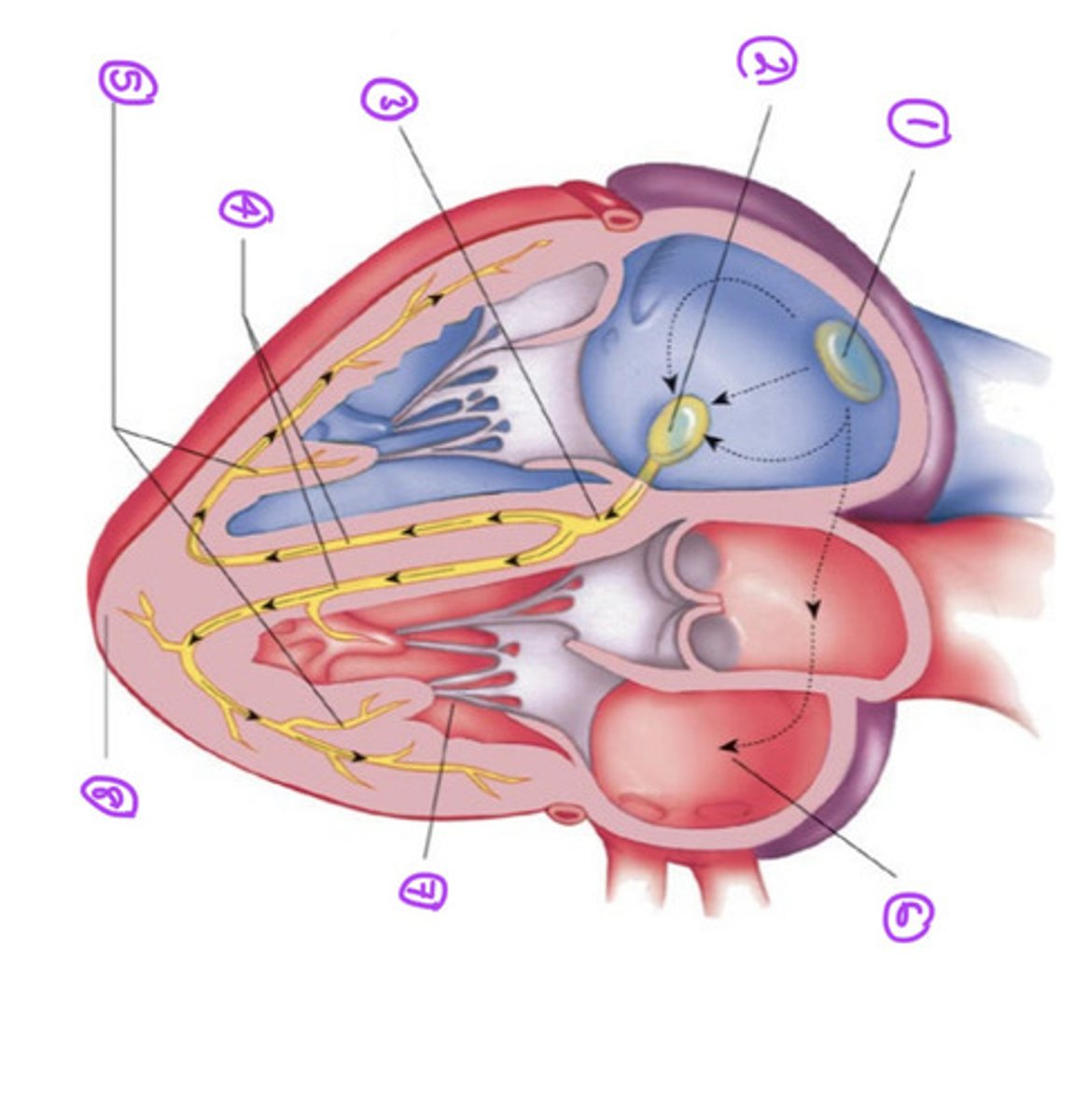
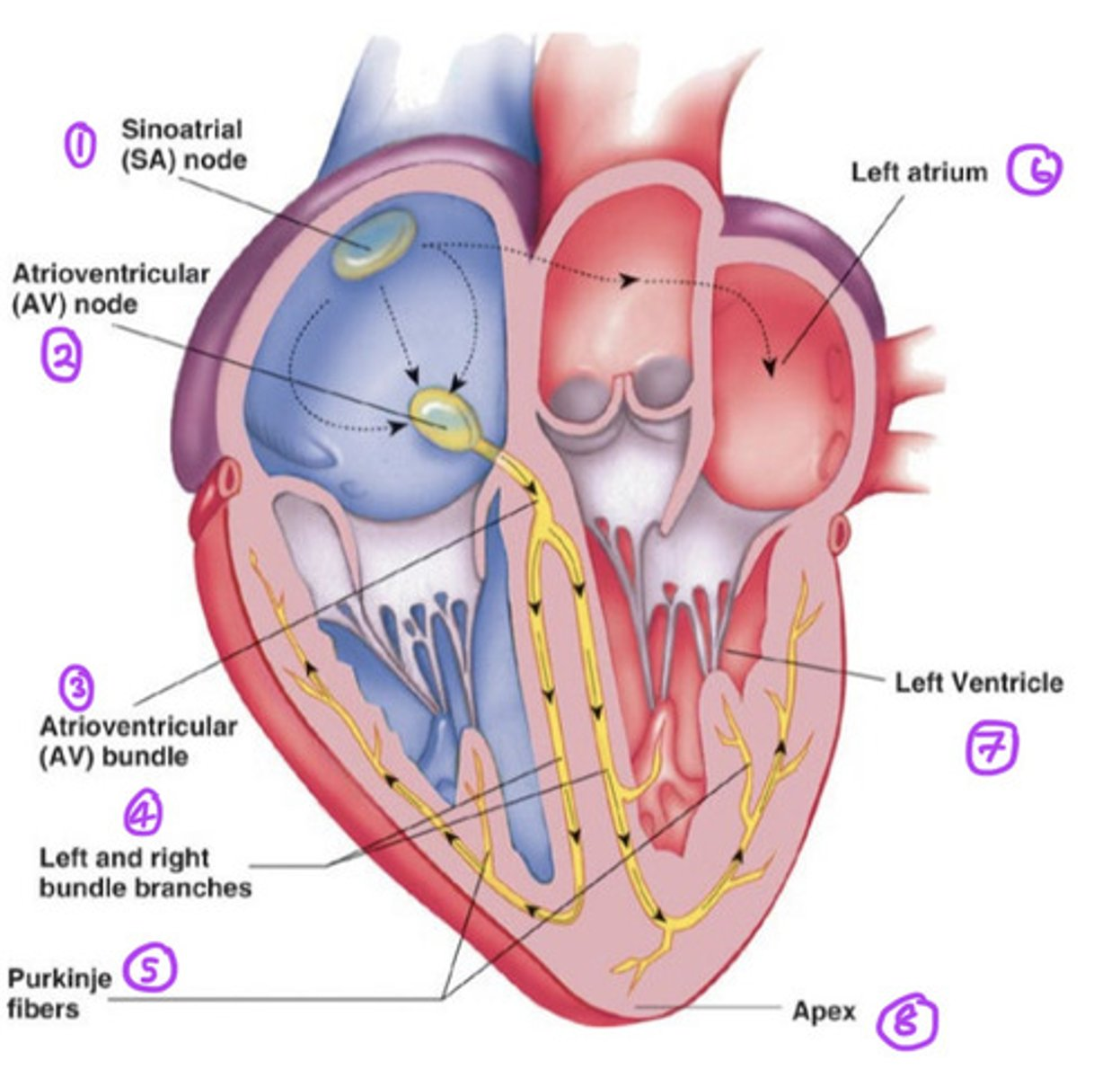
What is included in the conduction system of the heart?
- SA node
- AV node
- AV bundle
- Right and left bundle branches
- Purkinje fibers
What is the SA node and what does it do? (Sinoatrial node)
- The pacemaker of the heart.
- Has specialised cardiac muscle cells, continuous with atrial syncytium.
- Generates spontaneous action potentials (autorhythmic tissue)
- Action potentials pass to atrial muscle cells and to the AV node
What is the AV node and what does it do? (Atrioventricular node)
- Here, the action potentials are conducted more slowly than in any other part of the system
- Ensures the ventricles receive the signal to contract after atria has contracted
What happens at the AV bundle?
- Action potential passes through hole in cardiac skeleton to reach inter ventricular septum
What happens at the right and left bundle branches?
- The impulse extends beneath endocardium to apices of right and left ventricles.
What are Purkinje fibers and what do they do?
- Large diameter cardiac muscle cells with few myofibrils
- Have many gap junctions
- Conduct action potential to ventricular muscle cells (myocardium)
Where does depolarisation occur in the conducting system of the heart? 1
Depolarisation from SA node across atria
How many tracts within atria conduct depolarisation to AV node? 2
3
Which node does conduction slow down in? 3
- Conduction slows in the AV node; allows atria to empty into ventricles before vent systole.
What does the atrioventricular bundle (bundle of his) connect the AV to? 4
Connects AV to bundle branches
What does the SA node generate impulses at? 5
Generates impulses about 75 times/min
What does the AV node delay impulses at? 6
Delays the impulse at approx 0.1 secs.
Label the conducting system of the heart
Label the conducting system of the heart ANSWER
Why does the heart contract?
To empty the heart of blood and pump it around our body
What is the appearance of cardiac muscle fibers?
Faintly striated, with branched, mono-nucleated cells.
• Functional syncytium• Continuous action potential
How are cardiac muscle cells connected?
Cardiac muscle cells are connected by intercalated discs, which contain high-conductance gap junctions (connexons) and desmosomes (cadherin).
How are action potentials propagated in cardiac and skeletal muscle?
- Cardiac = action is propagated from cell to cell
- Skeletal = action along length of single fibre
- There is slow propagation in cardiac muscle because of gap junctions and small diameter of fibres
- Propagation is faster in skeletal muscle due to larger diameter fibres.
Describe the cardiomyocyte contraction mechanism
Sliding filament theory:
1. Ca2+ binds to troponin on thin filaments(causing a conformational chnage that causes tropmysoin to detach from action filaments)
2. This exposes site on actin which can bind to the myosin head
3. ATP hydrolysis supplies energy for actin-myosin conformational change
4. power strokes of actin-myosin and shortening of the sarcomere occur
5. Ca2+ dissociates from TN-C and myosin unbinds from action with energy from ATP
6. Cycle ends when ATP binds to mysoin and the sarcomere returns to the original length.
How does Calcium get into the cell to cause cardiomyocyte contraction?
1. Ca2+ enters through the L type channel
2. Ca2+- induced calcium release (CICR) occurs
3. Stimulates Ca2+ release from SR
4. Intracellular Ca2+ rises ~ 0.5-2 um.
5. Ca2+ interacts with troponin C
6. Myosin binding site on actin freed
7. Actin moves over myosin causing myocyte contraction
8. Intracellular Ca2+ reabsorbed into SR via the sarco-endoplasmic reticulum Ca ATPase (SERCA) pump and removed from the cell via Na+/Ca2+ exchanger and ATP-dependent Ca2+ pump.
9. Ca2+ dissociates from TN-C and the binding site on actin is inhibited.
10. ATP required to unbind myosin from actin and reset the sarcomere to normal length.
What is the resting potential of a cardiomyocyte?
> -96mV
What is the resting potential of a membrane permeable to only K+ of a cardiomyocyte?
> -96mV
What is the resting potential of a membrane permeable to K+ and Na+ of a cardiomyocyte?
> -85mV
action potential?
what is the resting potnetial ?
what vlaue is threshold reached?
what occues when threshold is reached ?
Resting potential = -85mV
• Excitation depolarisation to threshold pot. = -70mV
• Opens Na+ gates: Action Potential
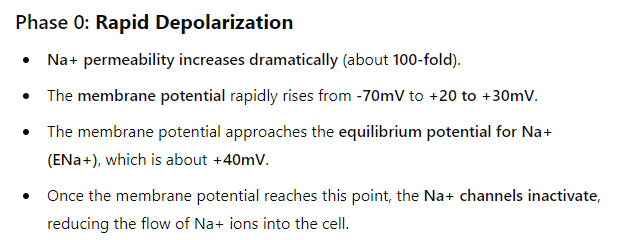
phase 0: rapid depolarisation
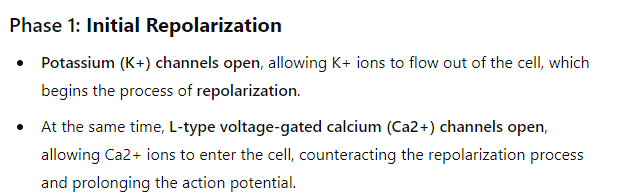
Phase 1: Initial repolarisation
Phase 2: Plateau phase
• K+ balances Ca2+ flow = plateau phase
• Generates cardiomyocyte contraction
• Ca2+ channels inactivated
Phase 3: Repolarisation
• K+ channels remain open,allowing continued outflow of K+ ions.
• Membrane potential falls to ~ EK(equilbriom potentil)
Phase 4: Resting Potential
• Return to resting potential = -70mV
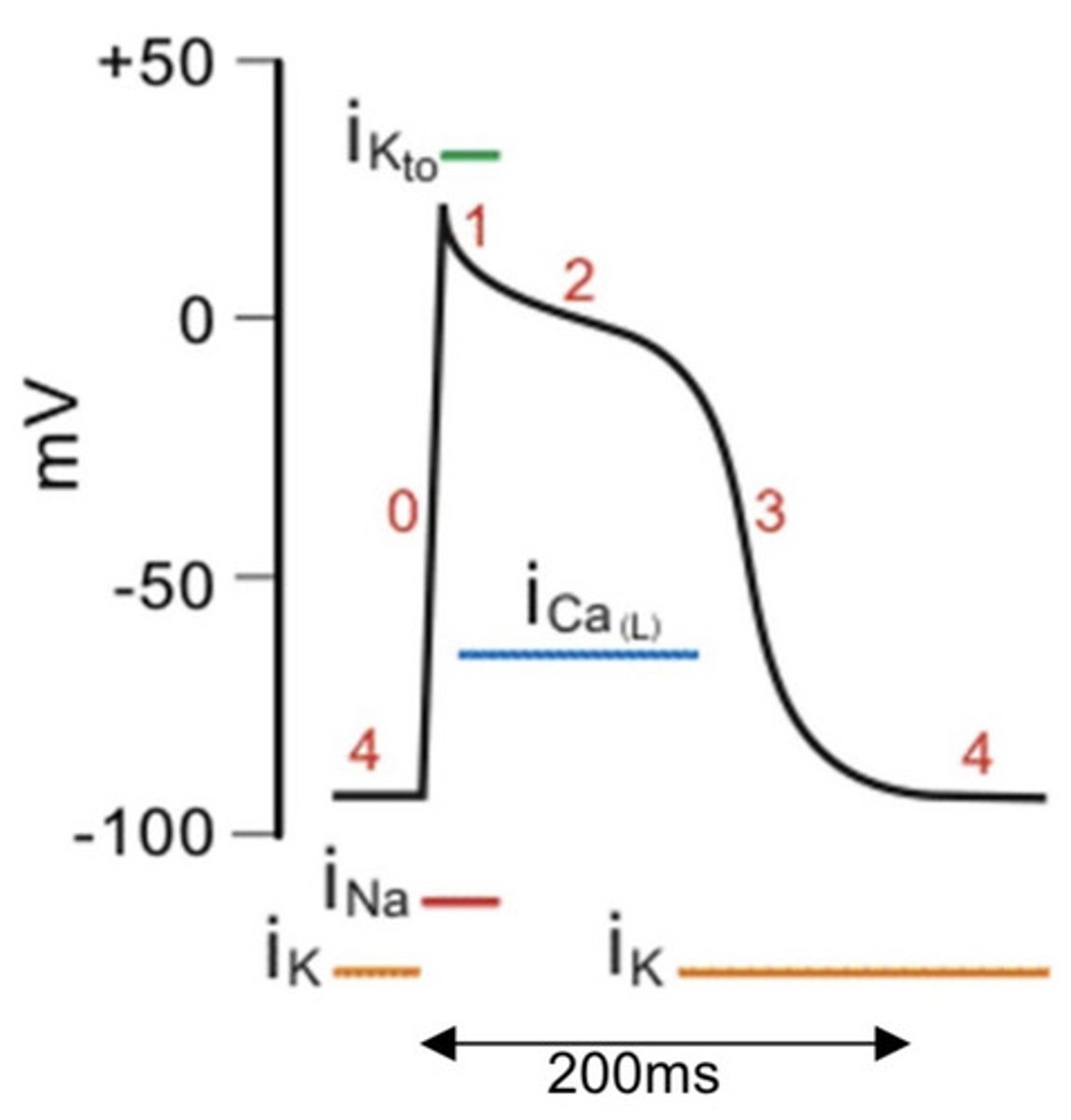
What ion channels are in each of the phases involved in Action Potential?
Phase 0:
- Na+ channel open
Phase 1:
- K+ channel open
Phase 2:
- Na+ channel closed
- Ca2+ channel open
- K+ channel open
Phase 3:
- Ca2+ channel close
- K+ channel open
Phase 4:
- K+ channel
What is the pacemaker tissue?
Areas of the heart where 'resting potential' is unstable
What is the pacemaker potential?
- After an action potential, the membrane potential drifts up (depolarises) until the threshold potential is reached.
- This causes the Na+ ion channels to open; triggering another AP.
- This is called the packemaker potential.
> Ends up causing a rhythmic depolarisation resulting in a rhythmic contraction.
What is automaticity?
- The ability to spontaneously depolarise and trigger an action potential.
> active in the SA node; Av node and bundle of his
> not in normal ventricular muscle cardiomyocytes
What is unique about the resting potential of pacemaker cells in the sinoatrial node?
Pacemaker cells in the sinoatrial node do not have a true resting potential. Instead, they undergo regualar spontaneous depolarization.
What happens during Phase 4 (Spontaneous Depolarization) of the sinoatrial node action potential?
In Phase 4, the pacemaker potential gradually depolarizes to -55mV due to:
Inward movement of Na+ and outward movement of K+.
K+ movement decays over time.
The Ca2+ inward current accelerates the depolarization to the threshold potential of -40mV.
What occurs during Phase 0 (Depolarization) in the sinoatrial node?
During Phase 0, Ca2+ influx increases through L-type calcium channels, leading to the depolarization of the cell.
What happens during Phase 3 (Repolarization) of the sinoatrial node action potential?
In Phase 3, voltage-controlled K+ channels open, allowing K+ to exit the cell and repolarize the cell.
Simultaneously, Ca2+ channels inactivate, contributing to the repolarization process.
Sympathetic & Parasympathetic systems regulate heart activity
Cardiac centres in medulla oblongata receive input from hypothalamus
Monitor blood pressure & dissolved gas concentrations
Parasympathetic Nervous System (Dominant Effect)?
Cardioinhibitory centre via vagus nerve
Innervates SA and AV nodes
Releases acetylcholine → hyperpolarises heart
Decreases heart rate
Sympathetic Nervous System (Minor Effect on Rate)
Cardioaccelerator centre activates sympathetic neurons (cardiac nerves)
Releases norepinephrine
Increases force of contraction → boosts contractility
conudcution system of the heart
Sinoatrial node (SAN) acts as pacemaker caused depoalrisation acrosds atria +Causing atria to contract simultaneously
Non-conducting tissue between atria prevents impulse passing directly to ventricles
3 Waves of electrical activity reach atrioventricular node (AVN) which delays impulse
○ Allowing atria to fully contract and empty before ventricles contract
4 AVN sends wave of electrical activity down bundle of His, c into Purkyne tissue
○ Causing ventricles to contract simultaneously from the base up