2. Bone Calcium + Homeostasis
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
94 Terms
the skeletal system is composed of
bones, cartilage, teeth, tendons, ligaments, and other tissues that interconnect bones
the skeletal system is about ___% of body mass
about 20% of body mass
reinforce joints
ligaments
cartilage
reduces friction between bones and reduces impact on bones
provides structure
tendons
connect muscles to bones
functions of the skeletal system (5)
support - structural framework for organs and tissues
protect soft tissues and organs
leverage - provides a lever on which muscles can act to generate force (and movement)
mineral storage - largest storage of calcium in the body… also stores phosphate
blood cell production - red and white blood cells as well las platelets are produced in red blood marrow
bone types
flat, irregular, long, short
sesamoid bones
grow in tendons
reduce friction, provide leverage and support
commonly found in: feet, hands, wrists, knee
Flat bones
layer of spongy bone bw two thin layers of compact bone
have marrow, but no bone marrow cavity
irregular bones
no easily characterized shape
layer of spongy bone bw two thin layers of compact bone
short bones
roughly cube shaped
mostly spongy bone, surrounded by a thin layer of compact bone
parts of the long bone (9)
Diaphysis
Medullary cavity
Epiphyses (2)
Epiphyseal plate or line
Articular cartilage
Metaphyses (2)
Periosteum
Endosteum
Bone marrow
diaphysis
tubular, long shaft of the bone
medullary cavity
hollow portion of long bone contains the bone marrow
endosteum
membrane that covers the internal bone surfaces
epiphyses
the ends of the bone
articular cartilage (hyaline)
covers each epiphysis, provides shock absorption and reducing friction in the joint
metaphysis
the flared portion between the diaphysis and the epiphysis
epiphyseal line
bw the epiphysis and the metaphysis
epiphyseal plate
aka “growth plate”
layer of cartilage that grows and is replaced by bone
periosteum
double layered membrane that covers the external surface of the bone
very vascularized and innervated
tendons, ligaments, and aponeuroses insert into periosteum
two parts, fibrous outer layer and the inner osteogenic layer
Fibrous outer layer of periosteum
dense irregular connective tissue
inner osteogenic layer of the periosteum
lays adjacent to bone and houses osteoprogenitor cells, osteoclasts, and osteoblasts
perforating fibres (sharpey’s fibers)
attach the periosteum to the bone matrix and are extra dense and entheses
compact bone (aka cortical bone)
the dense outer layer of bone, provides protection and rigidity to structure
Spongy bone (aka cancellous bone)
thin small pieces of bone called trabeculae that are arranged like a honeycomb
reduces wight of bone, but still provides structure
usually found at the ends of long bones
where bone marrow is found
fills the medullary cavity as well as the spaces between the trabeculae in spongy bone
red bone marrow
produces RBCs, WBCs, and platelets
yellow bone marrow
adipose tissue storage
adipose tissue
basically body fat
can be found under the skin (subcutaneous fat), packed around internal organs (visceral fat), between muscles, within bone marrow, and in breast tissue
blood is supplied to the diaphysis and bone marrow by
at least one nutrient artery and vein
(nerves are often packaged wiht these)
how the nutrient arteries / veins access the inner bone (and sometimes also nerves)
through hole in wall of diaphysis called the nutrient foramen
periosteal arteries and veins supply…
the outer surface of the bone and periosteum
epiphyseal arteries and veins perfuse ….
the epiphyses
the metaphysical arteries and veins perfuse the…
metaphyses
structural unit of compact bone
osteon
central (Haversian) canal
part of the osteon
contains vessels surrounded by concentric lamellae
concentric lamellae
thin layers of bone matrix
formed by many osteons grouped together
compact bone
circumferential lamellae
surround the osteons and form the outermost layers of the compact bone
lacunae
small cavities between lamellae that house osteocytes
one osteocyte in each one
canaliculi
narrow passageways extending from lacunae into the lamellae
connect lacunate to vascular passageways, thus allowing the osteocytes a source of nutrients and a way to dispose of waste products
osteoprogenitor cell (osteogenic)
type of stem cell
found in inner layer of periosteum and endosteum
can divide into osteoblasts
huge role in healing fractures
osteoblast
bone building cell
premature bone cell found periosteum and endosteum
secrete collagen and chondroitin into matrix of bone
the stuff secreted by osteoblasts
collagen and chondroitin
osteocyte
mature bone cell found in lacunae
important for bone turnover and repair
lacunae
small cavity in bone tissue where osteocytes live
osteoclast
different cell base than the other bone cells
found on surface of bone
breaks down bone matrix for resorption
4 main reasons for osteogenesis
embryonic and fetal development
bone growth before adulthood (lengthening)
bone remodeling (throughout life)
fracture healing
what the embryonic skeleton is formed of
fibrous connective tissue and hyaline cartilage
ossification or osteogenesis
the building or remodeling of bone
both processes of ossification begin with this type of cell
mesenchymal cells
intramembranous ossification
the differentiation of (sheets of) mesenchymal cells directly into bone cells
examples of bones formed by intramembranous ossification
cranial bones, mandible, clavicles, sesamoid bones
endochondral ossification is when… (and how does it happen)
bone develops by replacing hyaline cartilage model
mesenchymal cells first transform into hyaline cartilage model or template, which is later replaced by bone as ossification proceeds
bones formed by endochondral ossification
most bones, except those formed by intramembranous ossification (cranial, mandibles, clavicles, and sesamoid bones)
stages of intramembranous ossification (4)
development of ossification centre
calcification
formation of trabeculae and periosteum
formation of compact bone development
when does intramembranous ossification begin?
during embryonic development
what happens during the development of ossification centre in intramembranous ossification
mesenchymal cells cluster together and differentiate into osteoblasts
this site is called the ossification centre
what happens during calcification in intramembranous ossification
osteoblasts secrete osteoid (bone ECM) until they are surrounded it
these trapped osteoblasts differentiate into osteocytes
osteocytes extend cytoplasmic processes from lacunae into canaliculi that radiate in all directions
within a few days, mineral salts (calcium phosphates) are deposited into the osteoid, which hardens or calcifies (aka bone mineralization)
what happens during the formation of trabeculae and periosteum in intramembranous ossification
accumulating osteoid is laid down between blood vessels forming thin, rodlike bony tissue called trabeculae
the trabeculae fuse together and form a honeycomb structure of spongy bone around the blood vessels
mesenchymal cells cluster on the external surface of the bone and differentiate into periosteum
what happens during the formation of compact bone and marrow in intramembranous ossification
deep to the periosteum, the trabechulae are remodeled and replaced by a layer of compact bone
spongy bone remains at the centre of the bone
blood vessels that are crowded together around the trabeculae differentiate into red bone marrow, which fills the spaces between the spongy bone
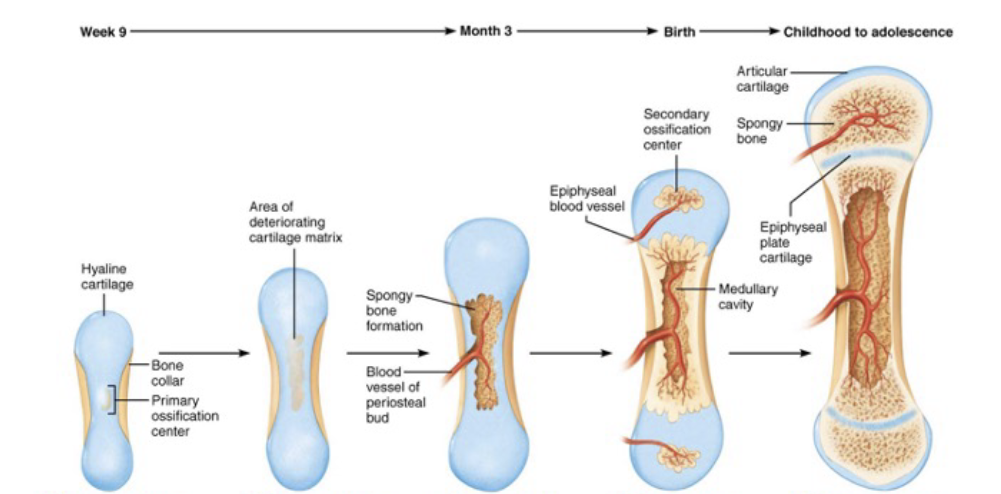
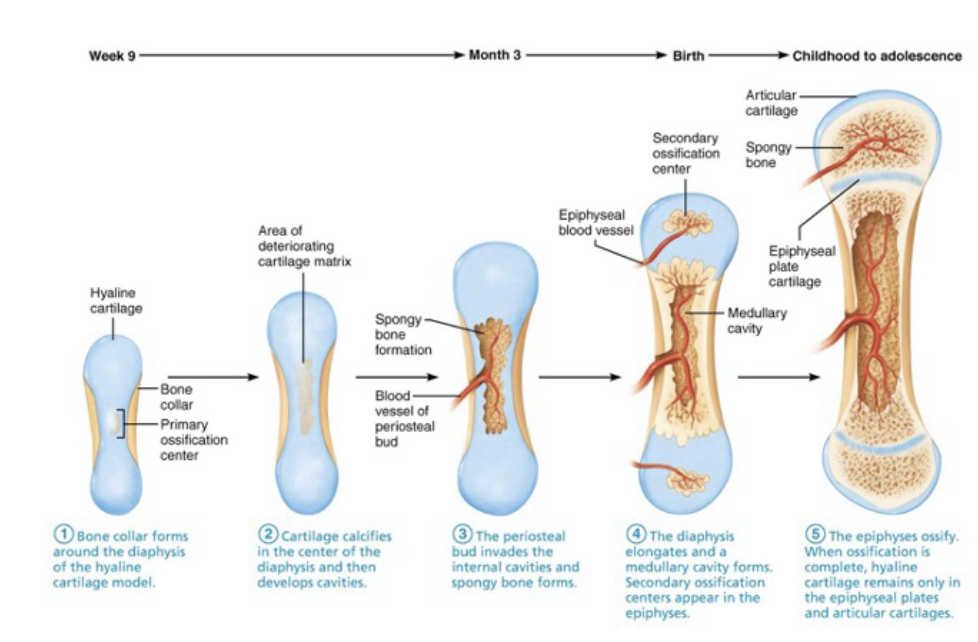
the steps of endochondral ossification
development of cartilage model
development of bone collar and primary ossification centre
development of medullary cavity and secondary ossification center(s)
development of articular cartilage and epiphyseal plates
what happens during the development of the cartilage model
mesenchyme cells crowd together in the shape of future bones
these cells then differentiate into chondroblasts
chondroblasts secrete an ECM, which forms a hyaline cartilage model
more mesenchyme cells condense on the surface of the model and form the perichondrium
the now encased chondroblasts differentiate into chondrocytes
chondrocytes undergo continuing cell division, thus increasing the bone in length (also in width by chondroblasts secreting more ECM)
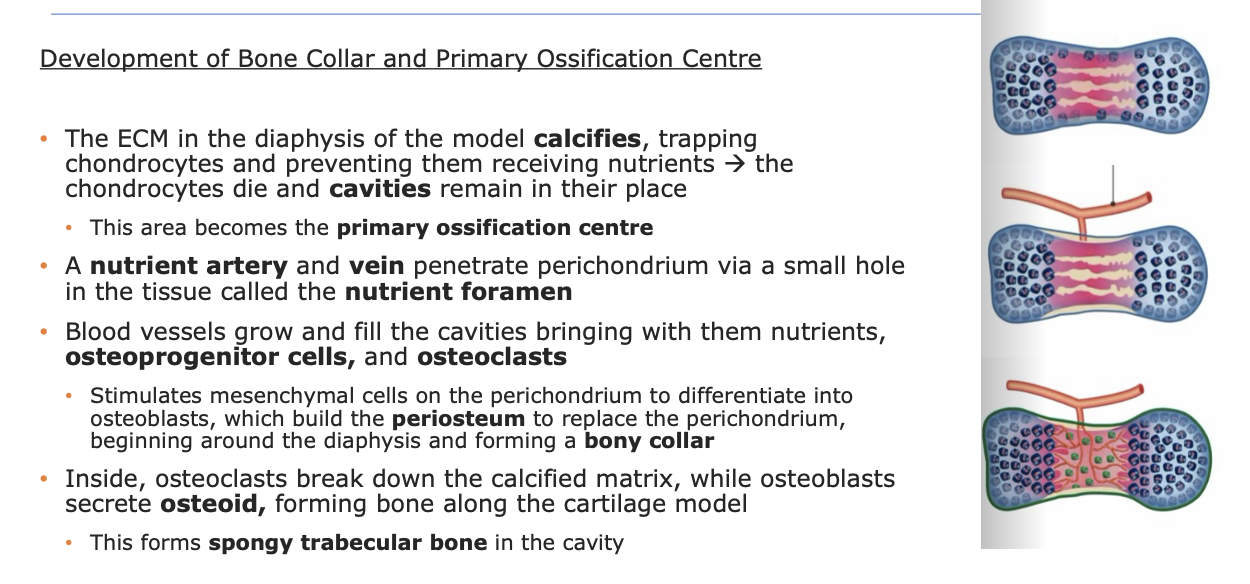
what happens during the development of bone collar and primary ossification centre?
what happens during the development of the medullary cavity and secondary ossification centre(s) in endochondral ossification
osteoclasts break down some of the trabecular bone, forming the medullary cavity
surrounding bone is replaced by compact bone
epiphyseal capillaries grow into the epiphyses and invading cells form a secondary ossification center in one or both ends of the bone (in the spongy parts)
in these centers, the cartilage is replaced by bone, but no cavity forms
what happens during the development of articular cartilage and epiphyseal growth plate in endochondral ossification
hyaline cartilage on the ends of bone becomes articular cartilage which is a specialized type of hyaline cartilage
articular cartilage forms a protective cap over the epiphyses
a layer of hyaline cartilage remains healthy between either end of the diaphyses and the epiphyses
these chondrocytes remain active and continue to divide and build new tissue, thus progressing growth in bone length
this area is called the epiphyseal growth plate
the growth plates remain active until about age 25, when they ossify and become the epiphyseal line
explain each step
differentiate between the two types of post-natal bone growth
interstitial growth
growth in length from within the tissue
chondrocytes divide and secrete new matrix from within the lacunae, expanding the cartilage and causing the cartilage model to grow
same process happens in bone, but with the bone “chasing” newly formed cartilage, replacing it as it grows. this forces the cartilage to grow unidirectionally towards the ends, thus elongating it
appositional growth
growth in width or diameter through the addition of new layers
osteoblasts secrete new matrix agains existing external face of bone
cartilage grows in the same manner, but chondroblasts secrete matrix onto existing cartilage model
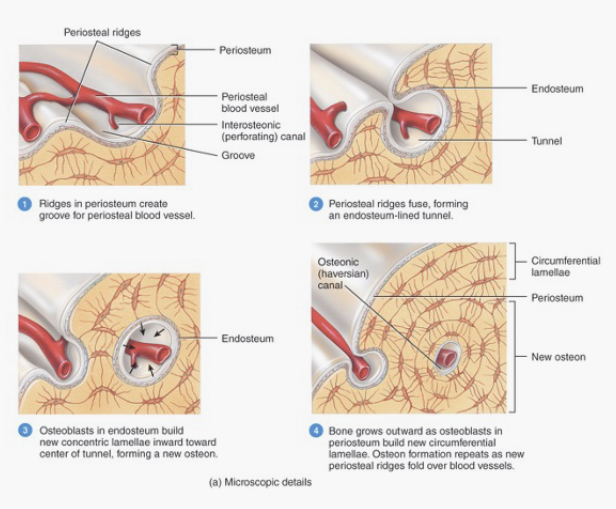
steps of appositional growth
Osteoblasts on the periosteum form new bone tissue — ridges develop around periosteal capillaries that grow and fuse into a tunnel around the blood vessels
Osteoblasts in the endosteum of those canals build new concentric lamellae toward the tunnel which forms a new osteon
Osteoblasts in the periosteum build new circumferential lamellae furthering the outward growth
Osteoclasts on the inside of the bone break down tissue, widening the medullary cavity
appositional growth is stimulated by ___ and requires ___
stimulated by chronic loading
requires adequate nutrient intake
______ load is a major determinant of bone growth
mechanical load
anatomy of the bone reflects the stresses placed on it, and is continuously remodeled (Wolff’s Law)
bones become thicker and stronger to resist forces (gravity, load, muscle contraction), and thinner and weaker if there are no forces placed on them
____ triggers affect bone health
chemical triggers
If calcium or phosphorus are in short supply, regulating hormones will take them out of the bone to serve vital functions in other systems of the body” (Office of the Surgeon General (US), 2004)
peak bone mass
our maximum bone size and strength
determinants of peak bone mass
genes and lifestyle factors (exercise level and type, smoking, alcohol, drug use, diet and nutrition, etc)`
bone mass loss can be significantly slowed by…
regular exercise and adequate nutrition
calcium is crucial in ___ and ___ function
neurological and muscular function
what happens when plasma calcium is too high
hormones are released to stimulate osteoblast activity
what happens when plasma calcium is too low
hormones are released to stimulate osteoclast activity
organs involved in calcium homeostasis
bones kidneys and gastro-intestinal tract
hormones involved in calcium homeostasis
parathyroid hormone
vitamin D
calcitonin
what does parathyroid hormone stimulate?
osteoclast activity
reabsorption of calcium by the kidneys
synthesis of Vitamin D
osteoblast activity
released by parathyroid
what releases parathyroid hormone
parathyroid
what does Vitamin D do
Stimulates calcium absorption by the gut
how does vitamin D enter the body
ingested via the gut as food
synthesized via the skin (sun)
what does calcitonin do
inhibits osteoclast activity
decreases Ca2+ reabsorption by kidneys
released by thyroid
what releases calcitonin
the thyroid
parathyroid hormones are released when..
blood calcium levels are too low
vitamin D is most active when
blood calcium levels are too low
calcitonin is released at a higher rate when
blood calcium levels are too high
osteoporosis
low bone bass and therefore weakened bone
bone becomes brittle light and porous
leads to fragility fractures
osteoclast activity outpaces osteoblast activity
commonly affected bones = hip spine wrist and scapula
no early signs or symptoms
treatment : mostly focused on reducing impagrs or slowing disease process
prevention: resistance training and adequate nutrition
treatment for osteoporosis
mainly focused on reducing impacts or slowing disease progress
prevention of osteoporosis
resistance training and adequate nutrition
process of fracture healing
hematoma forms
blood vessels and periosteum are torn w a fracture
hemorrhaged blood clots at fracture site
fibrocartilage (soft) callous forms
wishing days, new blood vessels grow into the clot
fibroblasts and chondrocytes invade site
fibroblasts produce collagen fibres that connect ends of broken bones
chondroblasts secrete cartilaginous matrix that calcifies to form the soft callus
bony callous forms
wishing a week, osteoblasts lay down new bone around soft callous
gradually replaces soft callus with hard, bony callus
bone remodeling
for several months, bony callus is continually remodeled
excess callus material on diaphysis and medullary cavity is removed
compact bone laid down to reconstruct shaft walls