27 - medical imaging
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
what is the nature of X-rays
- EM waves with wavelength 10^-8 - 10^-13
- travel in a vacuum at the speed of light
How are x-rays produced?
X-ray photons are produced when fast-moving electrons are decelerated by interaction with atoms of metal - the kinetic energy of the electrons is transformed into high-frequency photons of EM radiation - X-rays
what does an X-ray tube consist of?
why is it necessary for it to be a vacuum?
how do X-rays leave from a window?
how is the radiographer protected from X-rays?
X-ray tube - consists of a vacuum tube containing two electrodes
- an external power supply is used to create a large p.d. (30-100kV) between the cathode (the filament) and the anode (the target metal) that has a high melting point
- the filament produces electrons by thermionic emission, which are accelerated toward the target metal via the large P.D.
- the anode is shaped so that the X-rays are emitted in the desired direction through a window
- the tube is lined with lead to shield the radiographer from any X-rays emitted in other directions
- An evacuated tube is needed so electrons pass through without interacting with gas atoms.
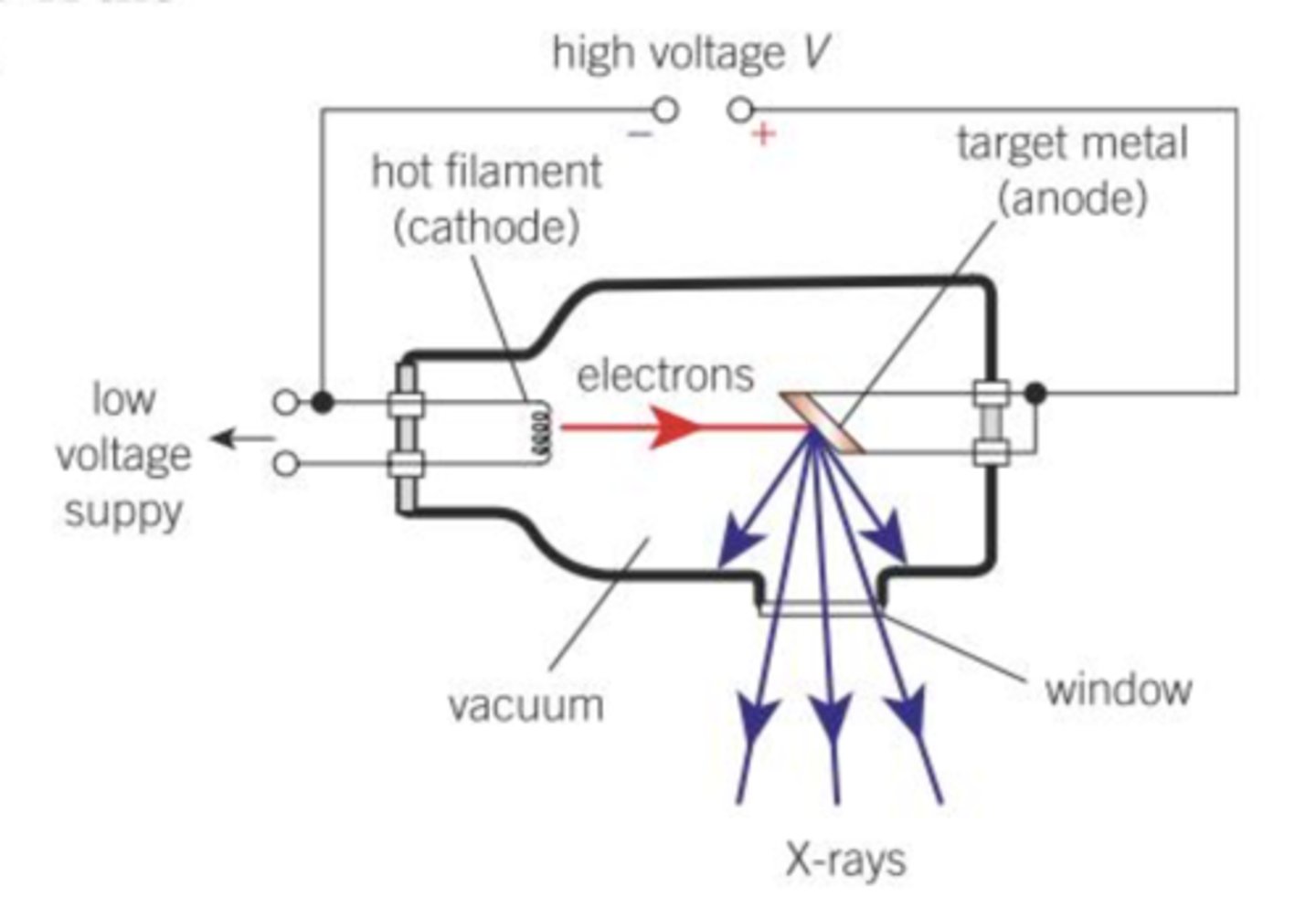
how are X-ray photons produced in the X-ray tube?
what happens in terms of energy transfer?
what happens to prevent overheating of the anode?
X-ray photons are produced when the electrons are decelerated by colliding with the target metal
- upon collision, electrons decelerate rapidly and less than 1% of their kinetic energy is emitted as X-rays.
- the remainder of the energy is lost to thermal energy in the anode
- to prevent the anode from overheating, the anode is either rotated so a new area is constantly exposed to the electron beam or it is cooled with circulating oil supply
state the one-to-one interaction in an X-ray tube and what principle governs this
one electron releases one X-ray photon from the principle of conservation of energy
what effect does increasing the tube current have on the X-rays produced?
increasing the tube current increases the intensity of the X-rays
how is the wavelength of an X-ray and its accelerating potential difference in the X-ray tube related?
whats the equation too?
the wavelength from an X-ray tube is inversely proportional to the accelerating potential difference.
λ = hc/eV
Define attenuation
attenuation - the decrease in intensity of EM radiation as it passes through matter
what are the attenuation mechanisms?
simple scatter
photoelectric effect
Compton scatter
pair production
explain the simple scattering attenuation mechanism & the energy range typically its used for
is it common?
- for X-ray with energy range 1-20 keV
- X-ray photon interacts with an electron in the atom but has less energy than the energy required to remove the electron
- so the X-ray photon simply bounces off (scattered) without any change to its energy
- not usually used in hospital radiography
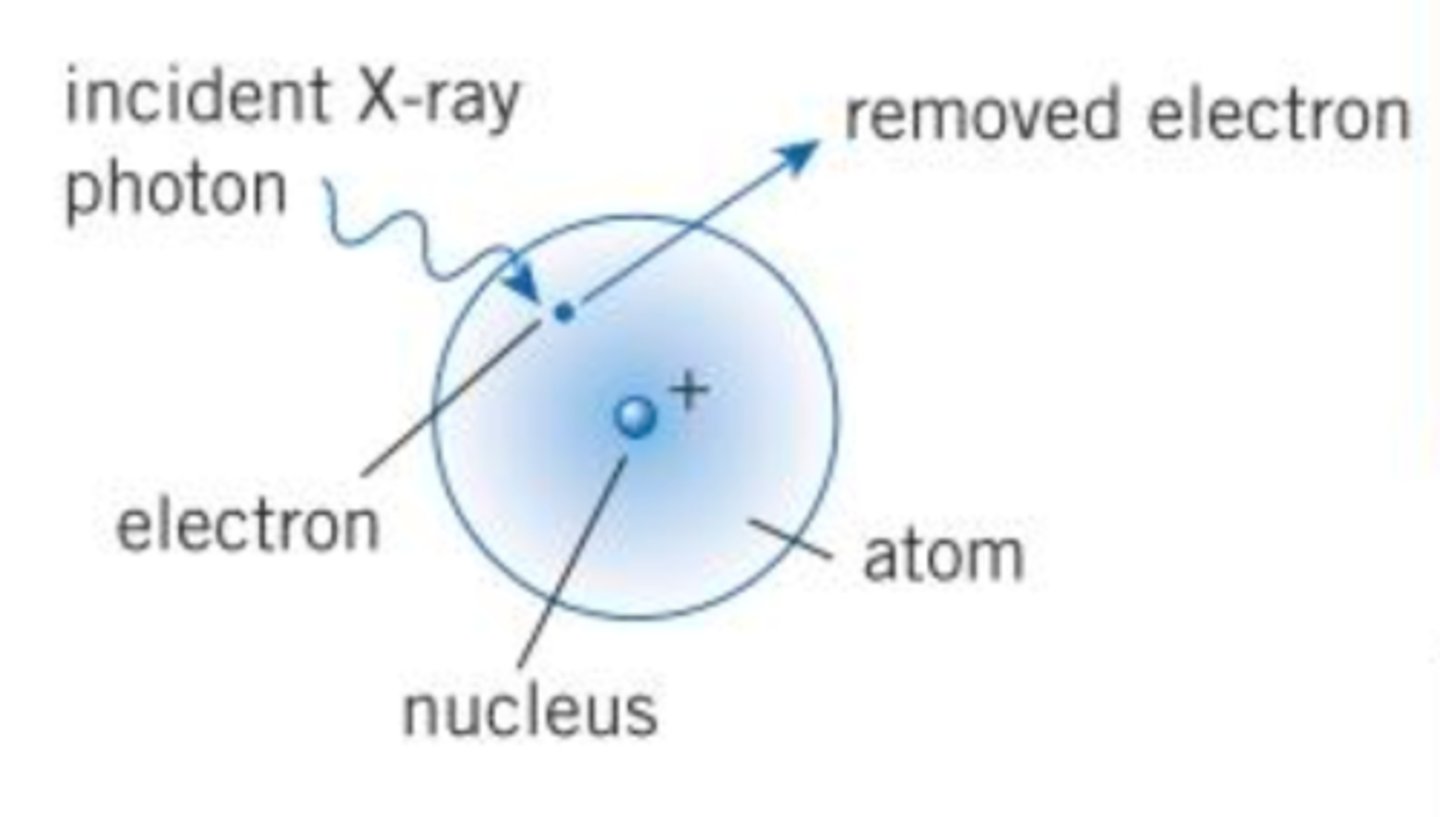
explain the photoelectric effect attenuation mechanism & the energy range typically its used for
where is it usually common?
- for X-ray photons with energy less than 100 keV
- the X-ray photon is absorbed by one of the electrons in the atom
- the electron uses this energy to escape from the atom.
- this attenuation is most common in hospital as their machines typically use 30-100 kV supplies
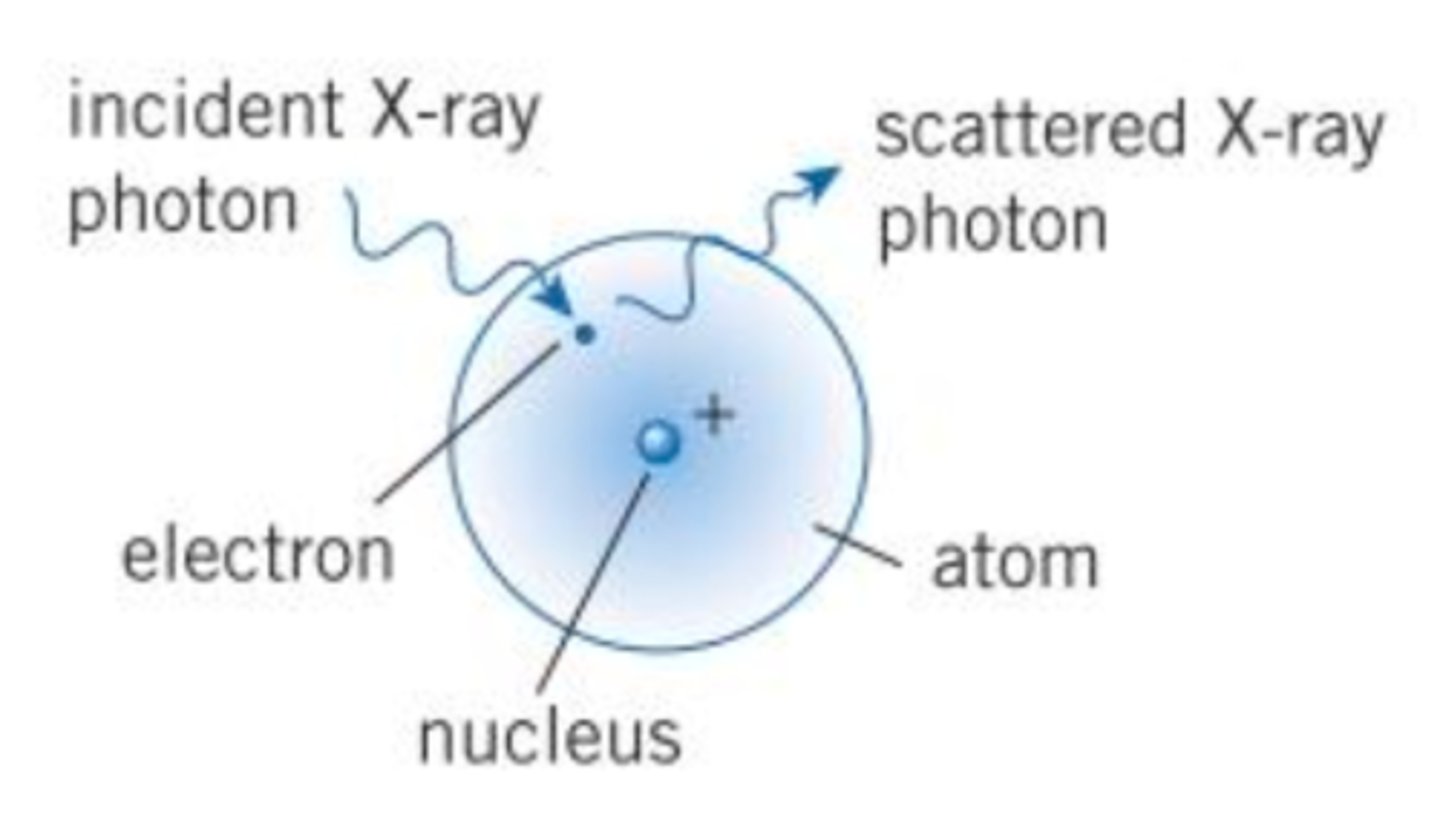
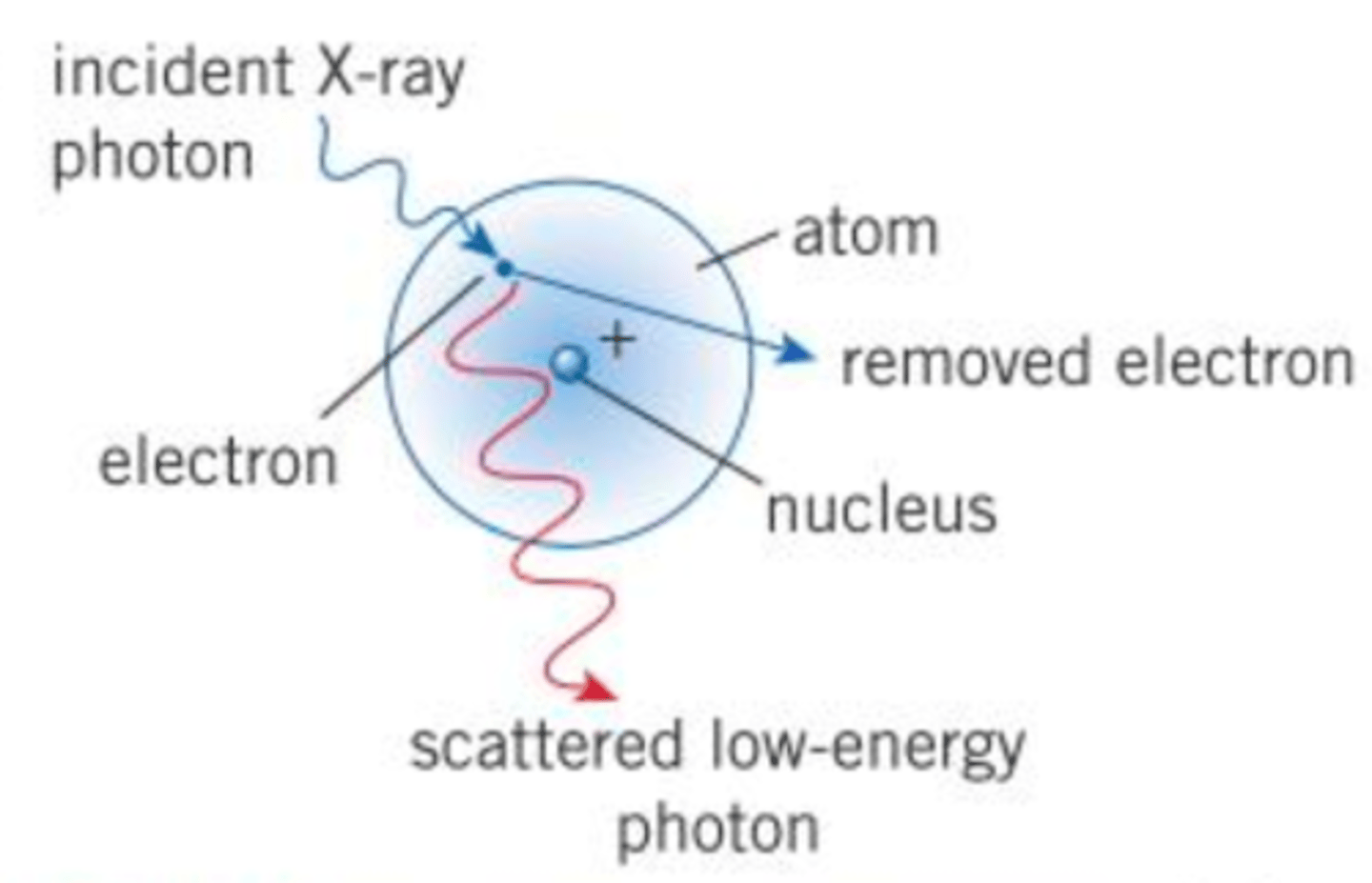
explain the Compton scattering attenuation mechanism & the energy range typically associated with it
what is conserved?
- for X-rays with energy range 0.5-5.0 MeV
- incoming photon interacts with an electron, causing the complete ejection of an electron from the atom
- the photon is scattered with reduced energy
- both energy and momentum is conserved
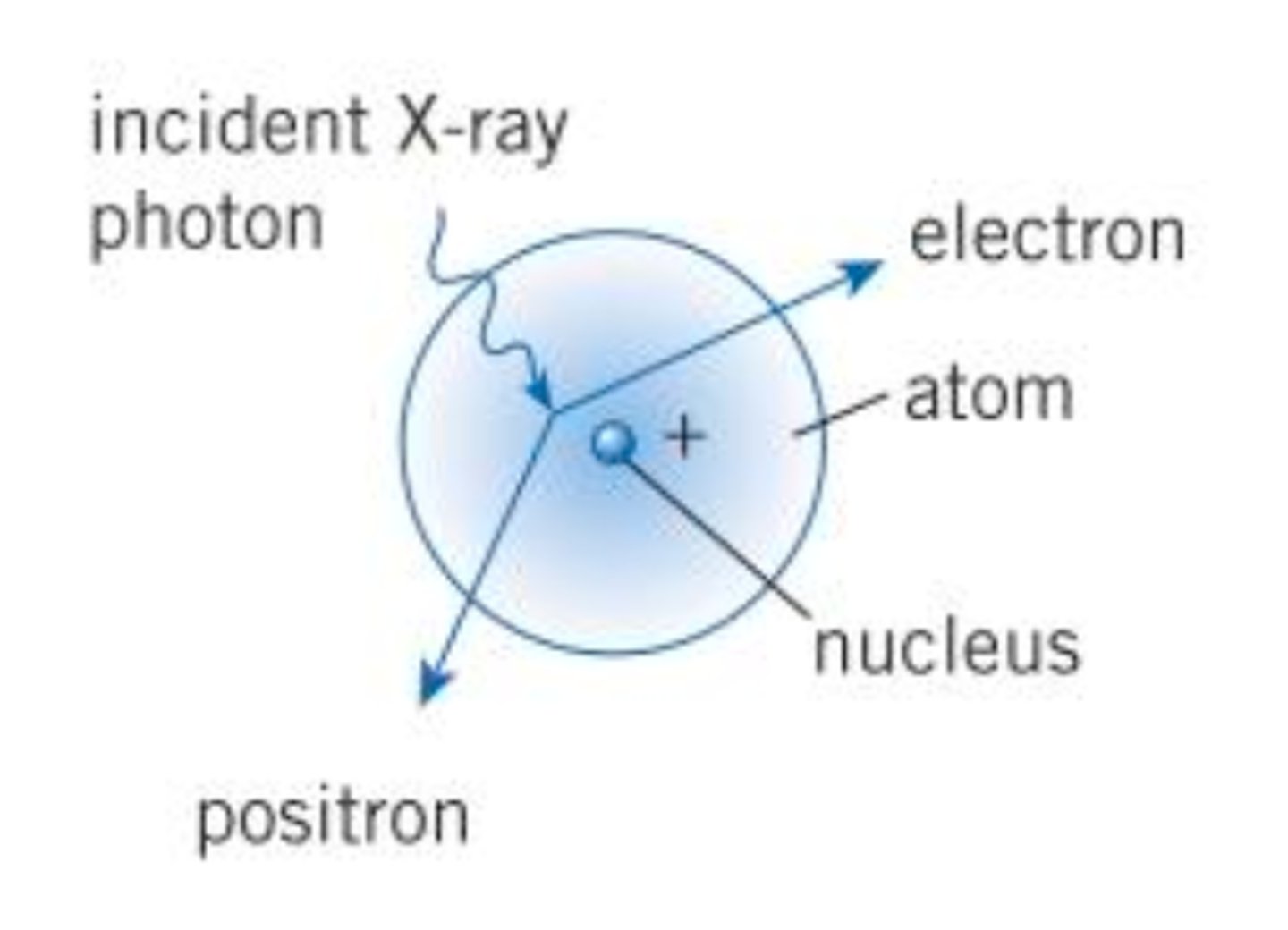
explain pair production as an attenuation mechanism and the energy range typically associated with it
- for X-rays with > 1.02 MeV energy
- X-ray interacts with the nucleus of the atom
- it disappears, EM energy of photon creates an electron-positron pair
what does the transmitted intensity of X-rays depend on?
what is the formula?
- initial intensity of x-ray
- thickness of the material
- attenuation coefficient of the material
I = Ioe^-μx
SI unit of μ = m^-1
what is the SI unit of the attenuation coefficient?
what does a large attenuation coefficient mean for an X-ray?
SI unit of μ = m^-1
large attenuation coefficient causes an X-ray beam to attenuate (weaken) quickly
what is a contrast medium?
a substance with a high attenuation coefficient used to help better produce x-ray images
what are the two most common contrast media?
what 2 reasons for their use?
iodine and barium compounds
- relatively harmless to humans
- attenuation coefficient is proportional to the atomic number (μ ∝ z³)
what is iodine as a contrast media usually used to examine?
contrast medium in liquids - blood flow
what is barium as a contrast media usually used to examine?
digestive system - 'barium meal'
how are X-rays used therapeutically - specifically with cancerous cells?
what machines are used?
through which scattering processes do the x-rays interact?
high energy x-ray photons produces using machines called linacs (linear accelerators) to then kill cancerous cells through Compton scattering and pair production
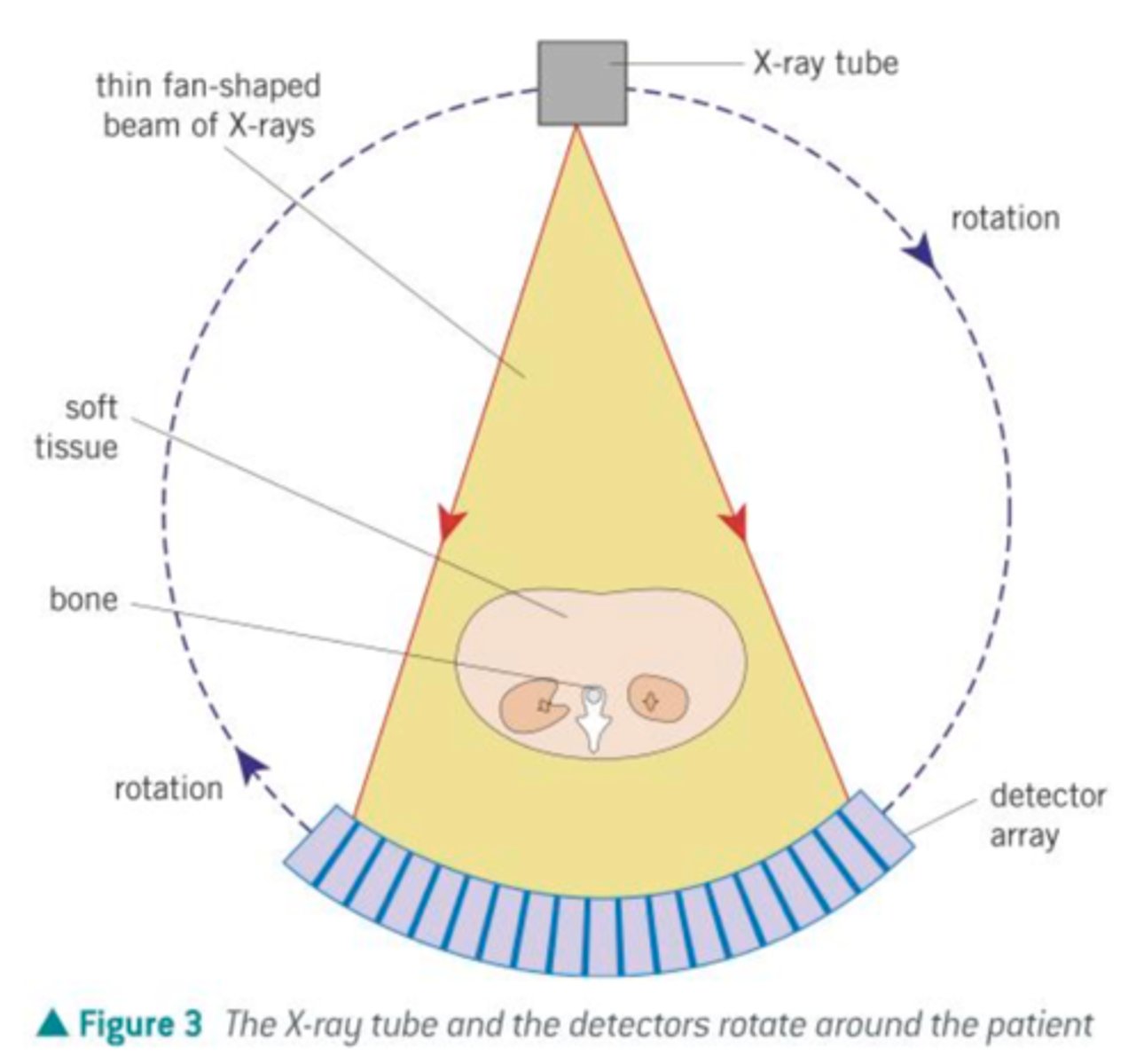
what does CAT scan stand for?
computerized axial tomography scan
how is a CAT scan machine set up with the x-ray tube and the electronic x-ray detector?
- X-ray tube on one side, array of electronic X-ray detectors on the opposite side
what are the components of a CAT scan machine and where are they set up?
describe the beam used in a CAT scan
what does the beam do in the scan?
what do the detectors record?
when will one 2d image be produced?
how is a 3d image achieved at the end?
- X-ray tube generates a fan-shaped beam of X-rays typically 1-10 mm thick
- thin beam irradiates a thin slice of the patient
- x-rays are attenuated by different amounts by different tissues
- the intensity of the transmitted X-ray is recorded by detectors which send electrical signals to a computer
- each time a full rotation occurs, a 2d image is produced
- x-ray tubes and detectors rotate about the patient and move up and down their length
- each 2d image can be compiled into a 3d image
Compare the advantages and disadvantages of using X-rays or CAT scans
- X-ray is quicker and cheaper
- CAT created 3d image
- CAT can distinguish between soft tissues and similar attenuation coefficients
- CAT scans have prolonged exposure to X-rays which are ionising and harmful
- patients have to remain very still for CAT scan.
what do medical tracers do?
-move through a patient's body to the region of interest and emit radiation that is detected with a gamma camera or a PET scanner
what are medical tracers?
radioactive substances that are placed inside a patient and their radiation detected from outside used to show the function and structure of tissues ororgans
how do medical tracers work?
medical tracers consist of a radioisotope bound to a substance that is used by the body
the tracer is injected or swallowed by the patient and moves through the body to the region of interest
why are gamma sources ideal for medical tracers?
what is a common medical tracer used in gamma camera imaging?
- least ionising and can penetrate through the patient to be detected externally
- technetium-99m
what is a necessary requirement for a medical tracer in terms of radioactivity other than it being a gamma source?
why?
- must have a short half-life t to ensure high activity from the source so that only a small amount is required to form the image
- the patient isn't subjected to a high dose of radiation that continues long after the procedure.
What is a radiopharmaceutical?
a radioisotope that is chemically combined with a compound that targets a specific organ tissue or biological process
also known as a medical tracer
what is the function of the gamma camera?
a gamma camera detects gamma photons emitted form the medical tracer injected into the patient
what are the 3 key components of a gamma camera?
- collimator
- scintillator
- photomultiplier
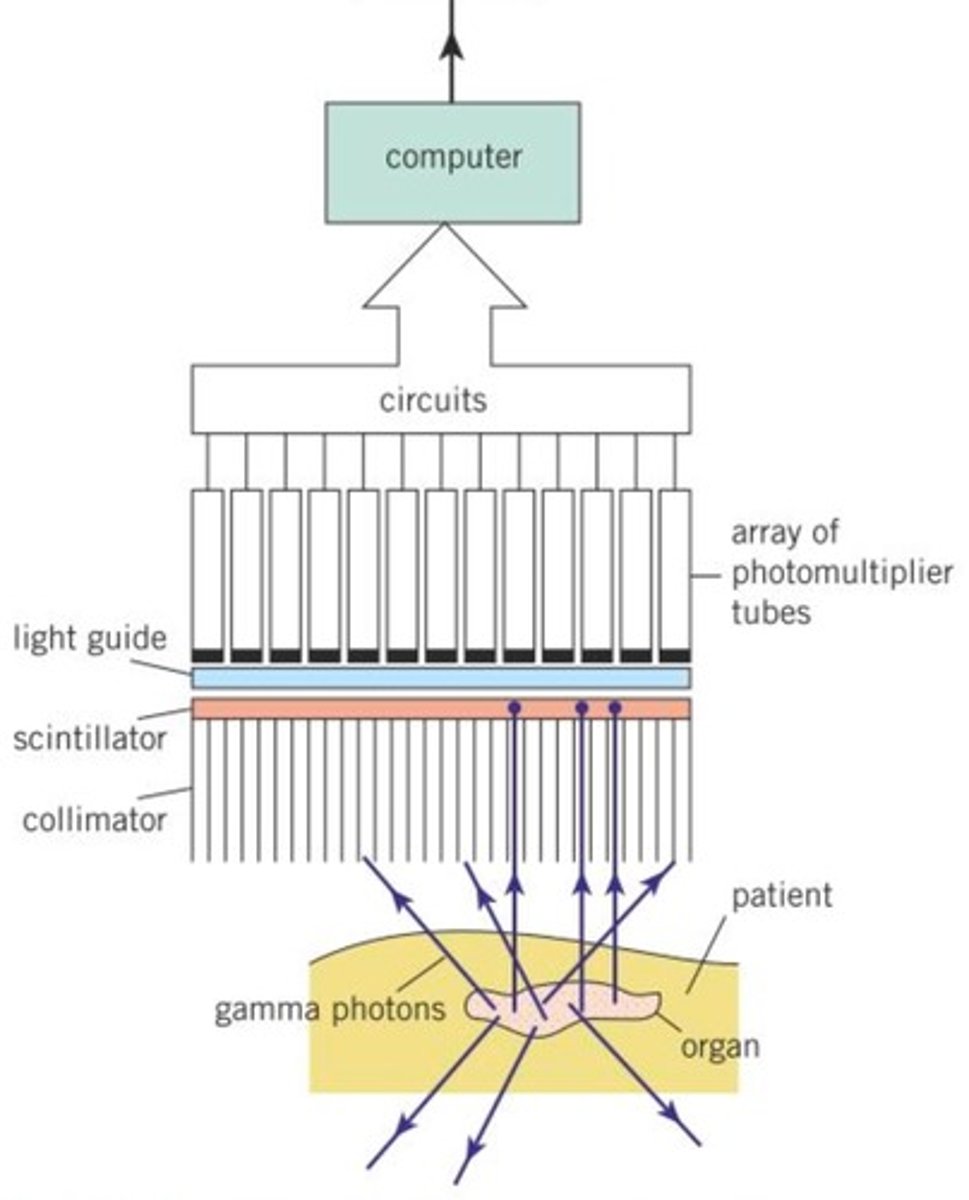
What is the collimator made of, and how is it shaped?
how does it function?
- honeycomb of long, thin tubes made from lead
- any photons arriving at an angle to the axis of the tubes are absorbed by the tubes so only those travelling along the axis of the tubes reach the scintillator
what material is the scintillator often made of?
how does it function?
do all the gamma photons comply with the function of the scintillator?
- often sodium iodide
- a single gamma photon striking the scintillator produces thousands of photons of visible light
- not all gamma photons do this because chance of photon interacting with scintillator is 1 in 10
what is the function of the photomultiplier tubes?
what are they connected to?
how does that help produce a high-quality image?
what is the image of?
the photons of visible light travel into the photomultiplier tubes
a single photon of light is converted into an electrical pulse (voltage)
the electrical signals are connected to a computer
the computer can locate the impacts of the gamma photons on the scintillator, which is then used to construct a high-quality image showing the concentrations of the medical tracer within the patient body.
what is the main difference between x-ray imaging and a gamma camera?
gamma camera can show the function and process of the body
x-ray imaging shows the anatomy
explain in simple terms how gamma camera and medical tracers work?
- medical tracer is injected or swallowed
(must be radioactive and emit gamma radiation due to its penetrating nature and must have short half-life)
- moves through the patient's body, as moving gamma photons emitted is detected by the gamma camera
- gamma camera made of collimator, scintillator, and photomultiplier connected to computer
- collimator, made from lead, absorbs all gamma photons not travelling about its axis
- scintillator, sodium iodide produces thousands of photons of visible light when interacting with a gamma photon, 1 in 10 gamma photons interact
- photomultiplier converts the visible light photons into electrical signals which are connected to a computer
- computer locates the impact of gamma photons onto the scintillator which is then used to construct an image of the concentrations of the medical tracer in the patient's body.
what does PET stand for?
positron emission tomography
what radiopharmaceutical can be used in PET scans?
why?
how is it made?
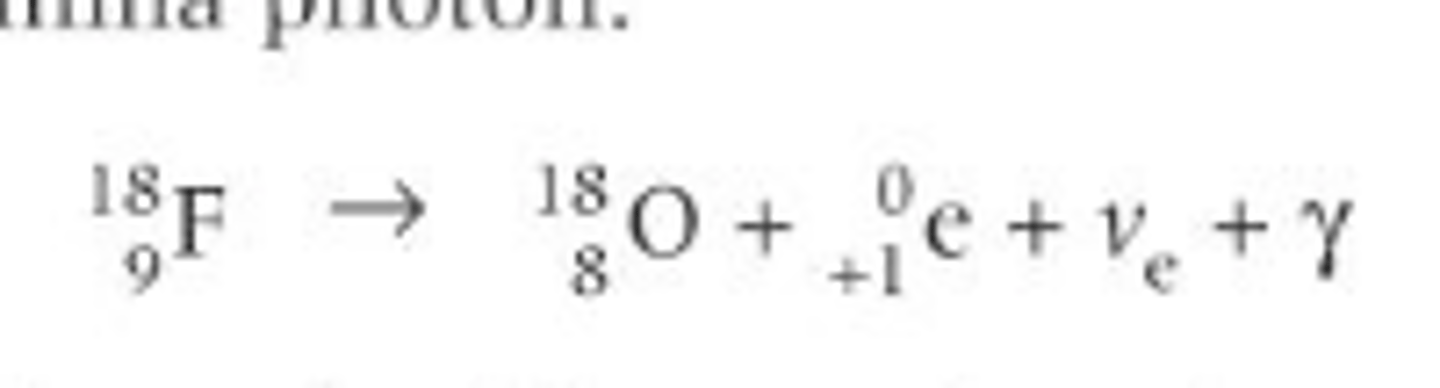
what is the nuclear equation?
what is a typical method using what machine?
- fluorine - 18
the isotope emits positrons with a short half-life - 110 mins
- usually made on-site with a particle accelerator/cyclotron
- cyclotron bombards the Oxygen-18 with protons
- O-18 absorbs a proton and emits a neutron, converting it into fluorine-18
- O-18 + p → F-18 + n
how is a pet scan used simply?
produce slices through the body that can be used to construct a 3d image using gamma radiation
what medical tracer do most PET scans use?
what is one thing its composed of that allows it to be used in PET scans?
what is an advantage of using FDG?
- fluorodeoxyglucose (FDG)
similar to glucose but with radioactive fluorine-18 atom in place of one oxygen atom
- our bodies treat it like normal glucose so it accumulates in tissues with a high rate of respiration
what is a good medical tracer for red blood cells?
why?
- carbon monoxide
- it is very good at clinging onto haemoglobin molecules
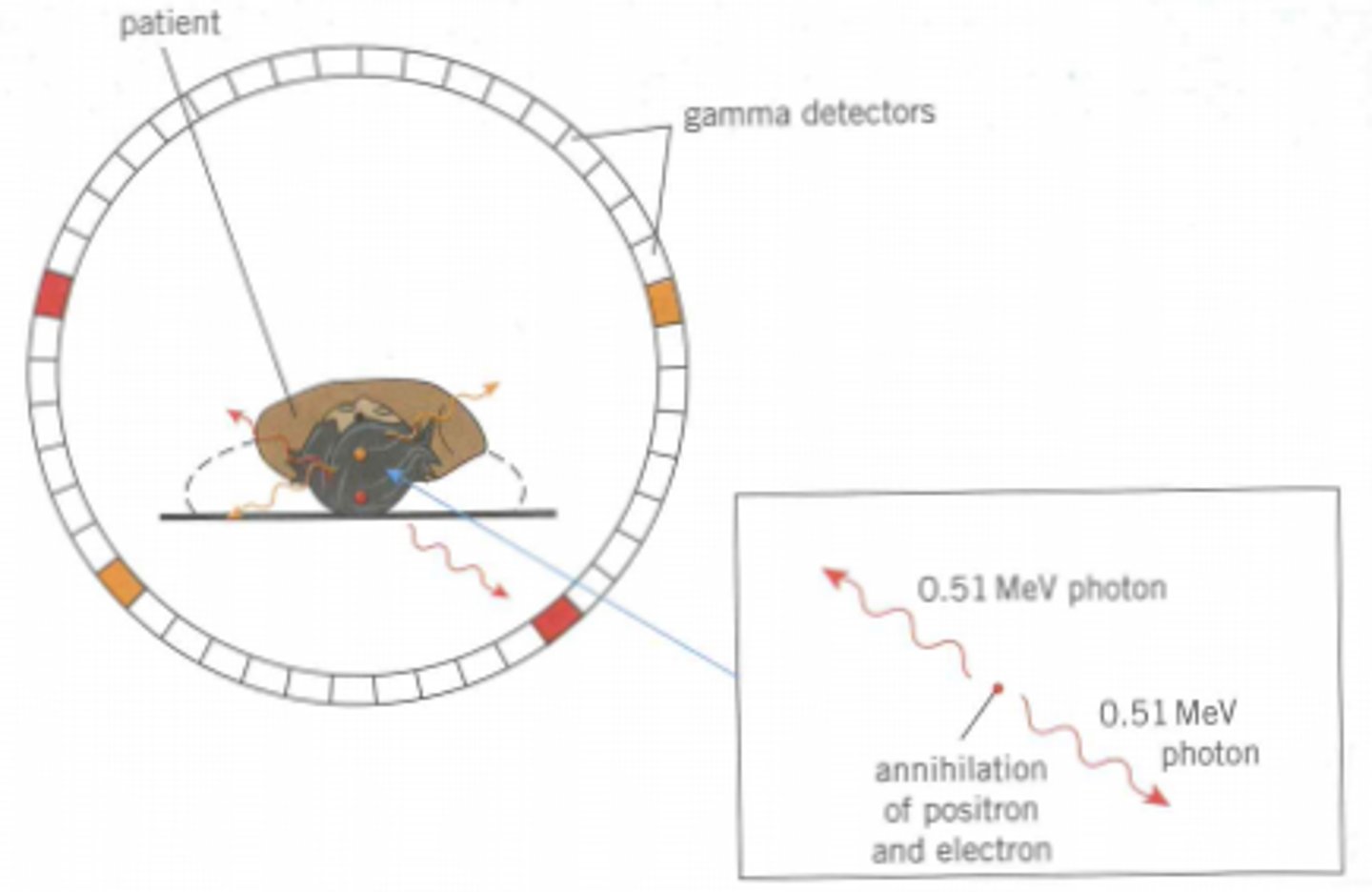
explain briefly what happens during a PET scan:
- what are the components of the PET scanner?
- patient lies on a table
- surrounded by a ring of gamma detectors
- each detector consists of a photomultiplier tube and a sodium iodide scintillator and produces an electrical signal for ever gamma photon incident at its scintillator
- detectors are connected to a high-speed computer
decay for fluorine-18
Fluorine to oxygen plus positron plus electron neutrino plus gamma photon
what is the patient injected with?
the gamma photons detected by the PET scanner - how are they formed?
- how far does a positron on avg travel
- patient injected with FDG
- PET scanner detects gamma photons emitted when positrons from decaying fluorine-18 nuclei annihilate with electrons inside the patient
- positron on avg trables 1mm from emission
after the PET scanner detects the gamma photons emitted from annihilation, how does the computer use this idea of annihilation and conservation of momentum to determine the location of the medical tracer?
when electrical signals are produced by the photomultiplier, what happens to them, how are they used?
- annihilation of positron and electron produces two gamma photons travelling in opposite directions due to conservation of momentum
- the computer can determine the point of annihilation from the difference in arrival times of these photons allowing the site of the tracer to be estimated
- electrical signals from detectors go to the computer, which can generate an image with different concentrations of the tracer
Advantages and disadvantages of PET scans
advantages of PET
- non-invasive
- diagnose different cancers
- plan complex heart surgery
- observe brain function
- used to assess the effect of new medicines and drugs
disadvantages of PET
- very expensive due to the facilities required
explain briefly and simply how PET scanning works
- patient has the medical tracer FDG (type of glucose with fluorine-18 in place of oxygen)
- body treats it as normal glucose so goes to areas of body with high rates of respiration
- fluorine decays by emitting a positron (beta plus decay)
- positron travels 1mm on avg before colliding with an electron and causing annihilation
- annihilation produces 2 gamma photons travelling in opposite directions due to conservation of momentum
- PET scanner comprised of ring of gamma detectors
- each gamma detector consists of a scintillator to emit visible photons and a photomultiplier tube to generate the electric signal to send to connected computer
- computer converts electrical signals into images and complies many 2d slices into one 3d image
- computer also can trace the location of the tracer by making calculations with the difference in time of arrival of 2 gamma photons from annihilation
what is the nature of ultrasound waves?
ultrasound waves are longitudinal sound waves with frequency greater than 20kHz, beyond range of human hearing
what is the function of the transducer
- a device used to both generate and receive ultrasound
- changes electrical energy into sound and sound into electrical energy by the piezoelectric effect
explain the Piezoelectric effect
- a piezoelectric material (e.g. certain crystals) generates a voltage when it is contracted or expanded or will contract and expand if a voltage is applied
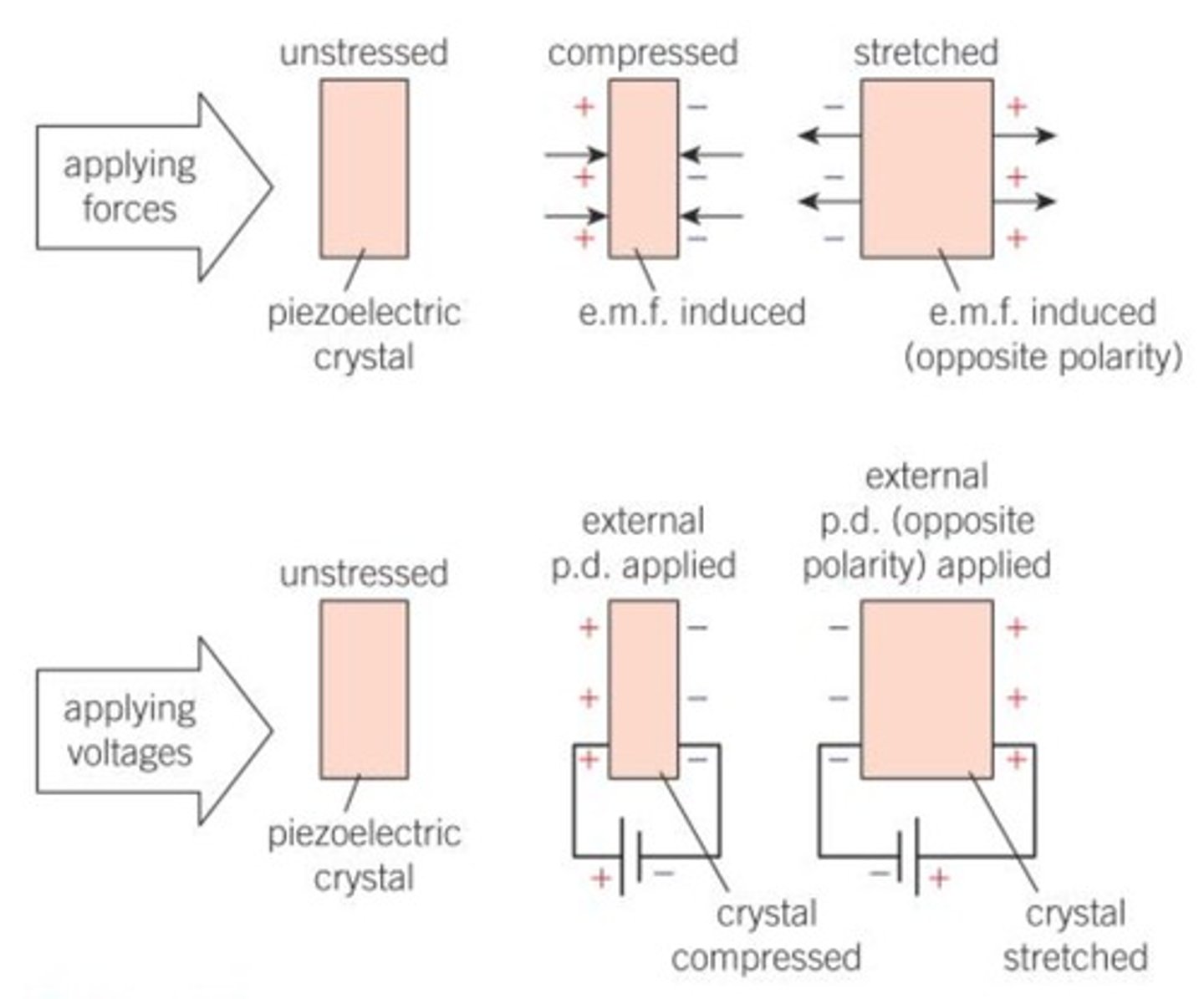
how does a transducer generate ultrasound
- alternating p.d. applied to ends of the crystal with the same frequency as the natural frequency of the crystal
- the crystal will resonate and produce an intense ultrasound signal
how does the transducer detect ultrasound
- ultrasound waves incident on the crystal will make it vibrate so the crystal is compressed and expanded
- the vibration generates an alternating e.m.f. across the crystal which can be detected by electronic circuits
what does A-scan stand for?
Amplitude scan
how does an A-scan work and what does it produce?
- single pulse of ultrasound emitted from a trasnducer into the body
- the ultrasound is partly reflected and partly transmitted between the boundary of two media
- the transducer detects the reflected wave and then a computer will create a time-delay graph
- the distances between the peaks indicate the depths of different structures in the body
how does a B-scan work and what does it produce?
- transducer emits pulses of ultrasound waves
- waves travel and reflect at tissue boundaries
- reflected wave detected and displayed as a bright dot on a screen
- position of the dot represents location of the boudnary and the brightness of the dot represents the intensity of the reflection
- transducer is moved along the skin to collect multiple readings
- a 2D image is built from all the dots showing the different tissues inside the body
what does a B-scan stand for?
brightness scan
define acoustic impedance
what is the formula?
the acoustic impedance Z is defined as the product of the density of the substance and the speed of ultrasound in that substance
Z=𝜌c
what is the intensity reflection coefficient?
what is the formula linking acoustic impedance and the intensity reflection coefficient?
fraction of the incident intensity that is reflected
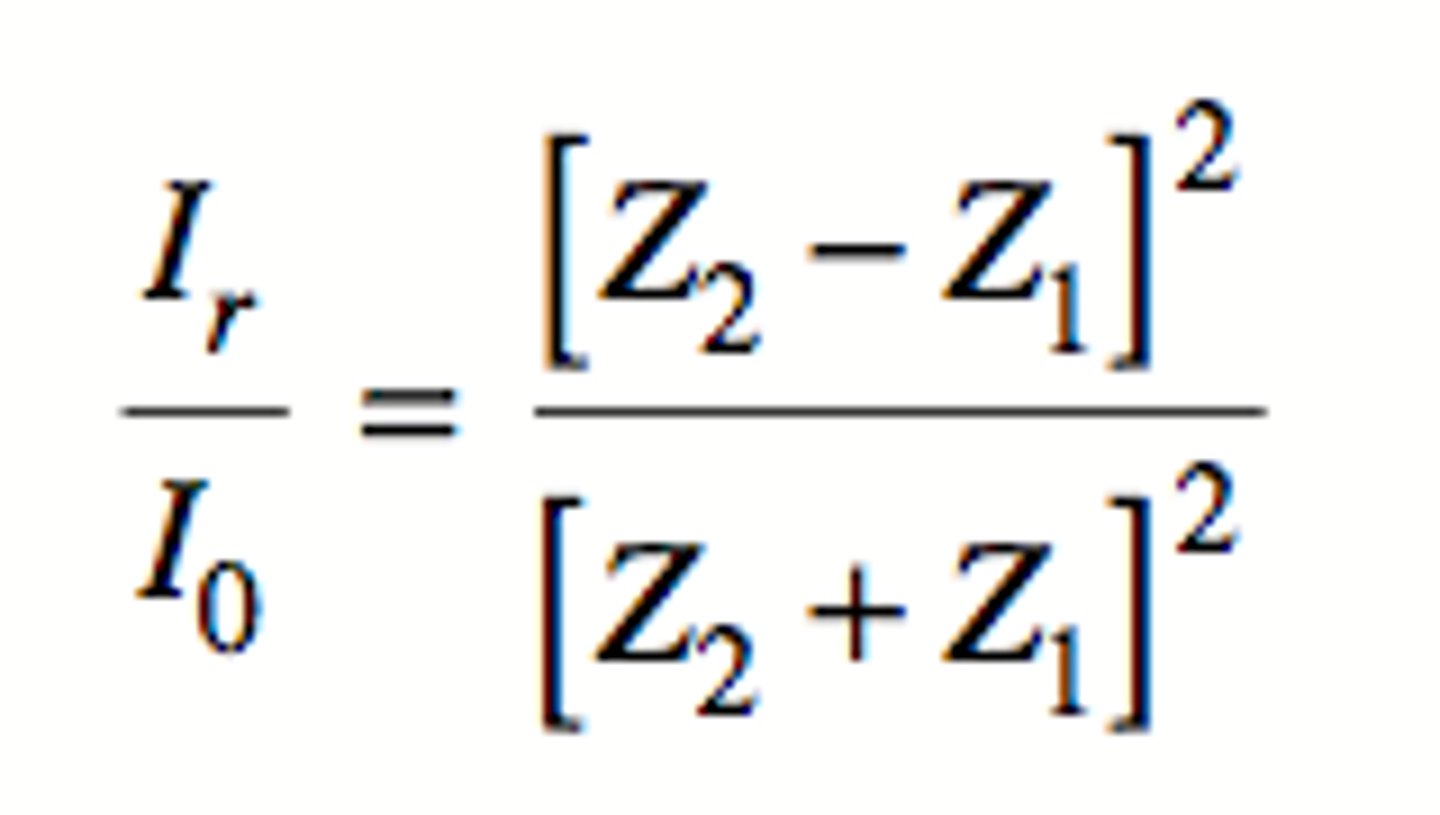
will there be greater or smaller intensity of reflected ultrasound at a boundary when acoustic impedances are the similar
less reflection
Why is coupling gel used?
what does it do?
- the air-skin boundary leads to 99.9% of incident ultrasounds will be reflected before entering the patient
- the coupling gel fills the air gaps and ensures almost all the ultrasound enters the patient's body, as the coupling gel and skin act as an impedance matching system
what does impedance matching mean?
two substances have similar values of acoustic impedance
how does the doppler effect occur in medical imaging?
the frequency of ultrasound changes when it is reflected off moving blood cells
- the ultrasound transducer is pressed lightly over the skin above the blood vessel
- the transducer sends pulses of ultrasound and receives the reflected pulses from inside the patient
- ultrasound refletced off blood cells will have a changed frequency
- if the blood is moving toward the transducer, the frequency increases, if away then decreases
- the transducer is connected to a computer that prodces a colour coded image to show the direction and speed of blood flow
for doppler scans, what is the formula to give the shift in frequency
f - original ultrasound frequency
v - speed of the moving blood cells
c - speed of the ultrasound in the blood
△f - frequency shift