NURS 372: MedSurg Respiratory I & II and SLC
1/153
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
154 Terms
normal lung sound
Movement of air through the respiratory system when there is no obstruction, inflammation, nor fluid in the airway
-Sounds like a hollow, tubular sound during auscultation
-May sometimes hear it referred to as"bronchial" or "bronchial-vesicular" sounds
abnormal lung sounds
Wheezing
• Rhonchi (low pitched wheeze)
• Crackles (aka "rales")
• Pleural friction rub
• Absent
• Stridor
wheezing
Occurs when there is inflammation and/or narrowing of the airway. Does not clear with coughing.
-Sounds like a loud, high-pitched whistling/squeaky breathing sound.
-Can occur during inspiration, expiration, or both.
-Common causes: Asthma, COPD, emphysema, infection, allergic reaction, obstruction (tumor)
classic sign of asthma
wheezing
asthma
Reversible acute airway obstruction occurs intermittently = reducing airflow
• Characterized by spasms in the bronchi, causing difficulty breathing.
- It is triggered by an allergic reaction or other forms of hypersensitivity.
• Airway become inflamed, narrow and swell, and produce extra mucus =dyspnea
• Inhalers such as bronchodilators and steroids help alleviate asthma s/s
asthma dx
PFT (pulmonary function Test)
dx if PFTs increase by 12%+ after treatment w bronchodilator)
FVC: inhale as deep as possible then exhale as much/as long as possible
FEV1: forced volume in 1 second
PEF: fastest rate of air that a person can blow out of lungs
asthma results in acute airway reduce airflow and leads to
=Airway tissue sensitivity
o Inflammation
asthma triggers
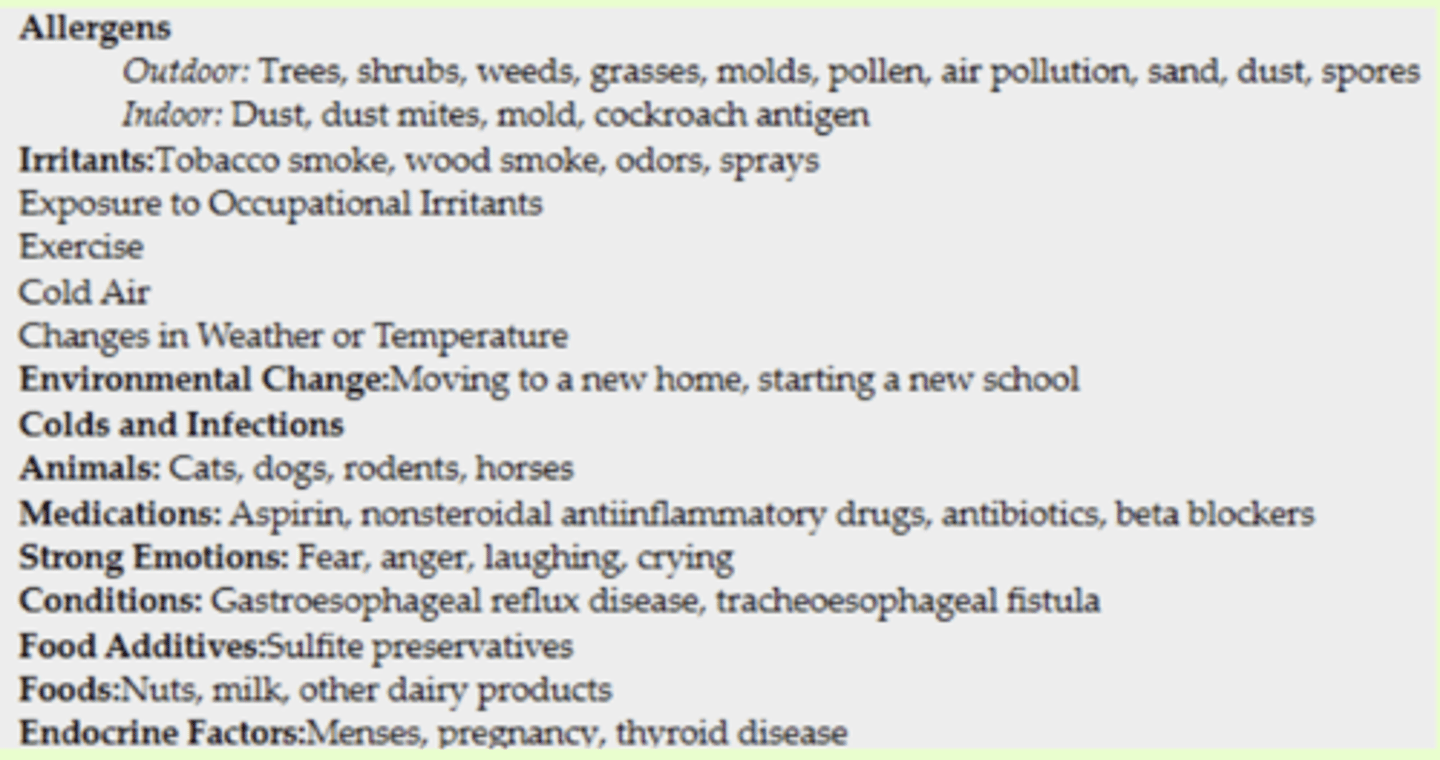
astham cues
Wheezing
o Dyspnea
o Chest tightness
o Coughing
o Increased phlegm (muscus)
o Accessory muscle breathing
hypoxemia
hypoxemia s/s
-Decreased pulse oximetry (< 90%)
-Cyanosis
-Tachycardia
-Decreased LOC (level of conscious)
labs and tests for asthma
Arterial blood gas
o Low pO2, low pCO2
Tests:
• Pulmonary function tests
asthma interventions
Goal is to promote airflow & gas exchange
• Supplemental O2 (via NC or mask)
• Drug therapy
Drug therapy for asthma
control or rescue
control drugs asthma
Reduce airway sensitivity to prevent asthma attacks & maintain gas exchange
o Used every day
o Ex: LABAs, corticosteroids, leukotriene modifiers
rescue drugs asthma
Used to stop an active asthma attack
o Used prior to exercise
o Ex: SABAs
status asthmaticus
Medical emergency
Extreme asthma attack that does not respond to regular treatment/rescue meds
Wheezing
SOB
Hypoxemia
Tachypnea
Cyanosis
Respiratory failure
Tx: usually continuous albuterol, steroid, DuoNeb (albuterol + ipratropium bromide), Magnesium
pt interventions with obstructive respiratory conditions
Avoid environmental triggers (smoke, dust, mold, temp changes of warm to cold)
-Wash bedding w/ hot water to destroy dust mites
-Avoid aspirin, NSAIDS, beta blockers
-Avoid food w/ MSG
-For exercise-induced asthma, use rescue inhaler 30 mins before exercise to prevent or reduce bronchospasm
-Teach pts proper inhaler use techniques
-Teach pts when to seek emergency care (difficulty breathing, walking, or talking; retractions of the neck, chest, or ribs; nasal flaring; grey/blue fingertips or lips; failure of drugs to control worsening symptoms)
-Teach pt to always carry rescue drug inhaler & ensure enough drug remains
rhonchi
Caused by blockages to the main bronchi due to mucous. Air is moving through the tracheal-bronchial passages coated with mucous or secretions.
-Sounds like a low-pitched, coarse breathing sound with a rattle-like quality.
-More common during expiration.
common causes of rhonchi
-Common causes: Pneumonia,bronchitis, cystic fibrosis, thick/tenacious secretions, sputum production
pneumonia
most common respiratory illnesses seen in the hospital setting
• PNA is an infection that inflames your lungs' alveoli (air sacs at the end of a bronchiole). Alveoli fill up with fluid or pus, causing cough, fever, chills and dyspnea (difficulty breathing).
• Can be prevented with vaccine
• Treated with antibiotics, steroids, diuretics, breathing treatments
PNA types
CAP (community acquired→ on admission or within 48 hrs of admission)
HAP (hospital acquired → develops >48 hrs after admission)
HCAP
VAP
HCAP PNA
(healthcare associated → develops <48 hrs from admission in pt w risk factors
In hospital for >48 hours in past 90 days, Nursing home or assisted living, IV therapy, wound care, abx/chemo in past 30 days, seen at hospital or dialysis clinic in past 30 days
VAP PNA
(ventilator associated pneumonia → dx within 48-72 hours after endotracheal intubation, often leads to sepsis)
prevention ("ventilator bundles" of interventions): hand hygiene, oral care, HOB elevation
risk for PNA in hospital
stay laying flat for long time
weak immunity
nurses coming in and out of other sick pt rooms
risk factors for PNA
Is an older adult
• Has a chronic lung disease•
Has never received the PNA vaccine or received it more than 5 years ago
• Did not receive the flu vaccine in the previous year
• Has an altered level of consciousness
• Has had a recent aspiration event
• Has presence of endotracheal,tracheostomy, or nasogastric tube
• Has poor nutritional status
• Has reduced immunity
• Uses drugs that increase gastric pH (histamine [H2] blockers, antacids)
• Is currently receiving mechanical ventilation
• Has recently been exposed to respiratory viral or flu infection
• Uses tobacco or ETOH or is exposed to high amounts of second hand smoke
s/s of PNA
Fever=may be blunted in elderly... confusion may be 1st sign
productive cough w purulent sputum
pleuritic pain
differs from cardiac chest pain because it worsens with deep breath
Chills
Myalgia
Headache
Tachycardia
hemoptysis
Resp symptoms: difficulty breathing, use of accessory muscles, hypoxemia, tachypnea, dyspnea, crackles, wheezing, dulled percussion, increased fremitus
concerns for PNA
Decreased gas exchange
• Potential for airway obstruction due to inflammation, pulmonary secretions, fatigue, muscle weakness
• Potential for sepsis due to presence of infectious microorganisms
• Potential for empyema due to spread of infectious organisms from the lung into the pleural space=Empyema:
most common complication of PNA
pleural effusion (fluid gets inside lining btw chest cavity and lungs)
treat w diuretics
other PNA complications
decreased gas exchange
potential for airway obstruction/pulmonary emphyema (alveoli fill with pus)
Sepsis (monitor VS for fever/tachycardia/hypotension)
empyema
collection of pus in the pleural space = impairs gas exchange
= reduces effective ventilation
cues for PNA
o Dyspnea
o Tachypnea
o Cougho SpO2 desaturation
o Cyanosiso Purulent, blood-tinged, or rust colored sputum
o Fever
o Elevated WBC
o Pleuritic chest discomfort
o Diminished breath sounds or crackles
o Altered cognition (older adults)
tests for PNA
o Sputum culture
o Blood culture
o CBC (WBC elevated, except older adults)
o Blood gases
o CXR=(definitive diagnosis...looks white, increased density)
ABGs
Procalcitonin
Inflammatory markers (eg: CRP)
SpO2
bronchoscopy (scope view airways to check for abnormalities and can take biopsy... must check for return of gag reflex before resume PO)
treatment for PNA
o Administer anti-infectives and bronchodilators as prescribed
o Supplemental oxygen
o Incentive spirometry
o Encourage coughing/deep breathing
treatment goals PNA
Maintain adequate gas exchange with SaO2 of at least 95% or pt's baseline level
o Maintain patent airways AEB absence of crackles and wheezes on auscultation
o Patient is free from infection AEB absence of fever and a WBC count within normal limits
o Avoid empyema
nursing considerations for PNA
• PNA can be prevented with vaccine. PNA often follows influenza.Encourage annual flu vaccine too.
• Monitor for complications: sepsis and empyema
• Encourage pulmonary hygiene and progressive ambulation
• Provide adequate hydration
• Assess risk for aspiration
• Monitor for early signs of sepsis
• Provide vigorous oral care
crackles
AKA: rales.
Occurs when there is fluid, pus or mucous in the small airways
. There are 2 types:Coarse and Fine.
Both commonly heard during inspiration.
Common causes: Fluid overload, pulmonary edema, heartfailure, lung infection (PNA).
coarse crackles
Loud, popping, bubbling noise. Sounds like ripping apart Velcro.
Coarse crackles = heard gen'l anterior/posterior area.
fine crackles
Brief popping sounds that are high-pitched. Sounds like wood burning in a fireplace.
heard in lower basesof lungs
pleural rub
Occurs when 2 inflamed pleural linings rub against each other during respirations.
-Sound like creaking or grating sounds. Similar to walking on fresh snow or a rough grating sound.
- stop when the patient holds a breath.
common causes of pleural rub
Pleurisy (infected pleural lining), pleural effusion (fluid buildup bxn 2 pleural layers-AKA pleural space), pulmonary infarct, TB, PNA
absent breathe sounds
Occurs when there is complete obstruction of airway by excessive fluid in lungs, tumor or collapsed lung=(Pneumothorax)
-You will not hear any lung sounds because the lung has collapsed or lung is filled with a lot of fluid; thus, no air movement/gas exchange.
common causes of absent breathe sound
Com Collapsed lung from a lung puncture wound or excessive mechanical/artificial ventilation. Fluid overload from HF, pulmonary edema, severe ARDS, tumor
FiO2 with nasal canula
O2 up to 6L (gen care units)
oRoom air = 21% FiO2
o1L NC = 24% FiO2
goes up about 4 per liter of FiO2
max is at 6 L nc =FiO2=44%
nursing considerations for nasal canula and FiO2
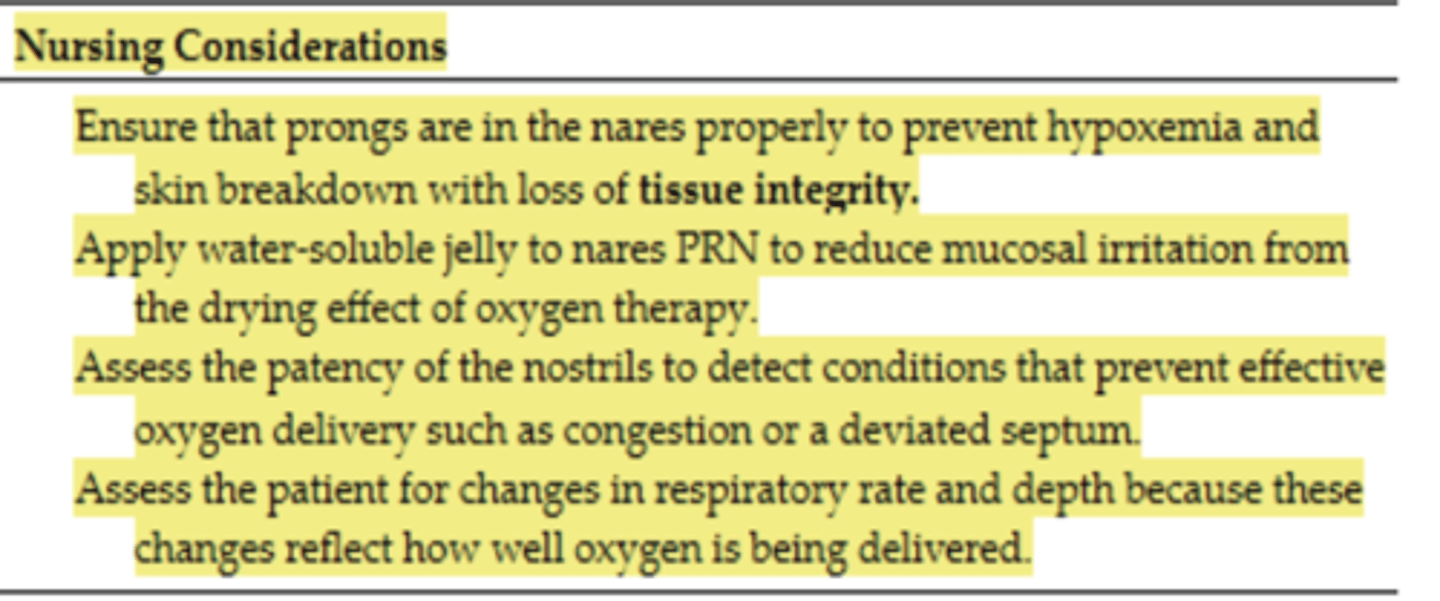
nasal canula safety consideration with oxygen
Oxygen enhances combustion
o No cigarettes, flammable materials (nail polish/alcohol or oil), candles, gas burners/fireplaces/open flames are not to be used in same room as O2
-Inspect electrical cords for fraying
-ambulation/fall risk education
o Educate pt if going home on oxygen
No smoking in the house
No open flames & flammable liquids present
nasal canula skin protection
Check skin underneath NC tubing for skin breakdown(especially behind ears) q 4-8 hours
• Position the tubing so it does not pull on the patient's face and nose (tubing also fall risk)
• During any periods of transport, connect NC to portable oxygen tank and make sure tank is full
• If your patient is requiring an increase in O2 requirement=please notify the RT & MD
-mouth care q 8 hours =check nasal/oral membranes for cracks (lubricate)
-clean tubing
use humidification with NC when
if NC is delivering 4L O2 or higher
how to clean NC
clean cannula or mask & skin beneath tubing with warm water
-Change tubing per policy bc can harbor microorganisms (usually q7days or q24hrs if humidified)
Noninvasive PositivePressure Ventilation (NPPV)
CPAP
BiPAP
CPAP
continuous positive airway pressure
pressure delivery of O2 steady
BiPAP
bilevel positive airway pressure
=inspire=higher pressure
=exhale=lower pressure
-usually more sick pt, insurance doesnt really cover
non rebreather mask
Used in emergencies = for short-term increases in oxygenation
• Delivers up to 95% of O2
• Usually found on crash cart, sometimes in pt rooms near wall oxygen, or RT supplies them
INFLATE BAG FIRST! plug hole w finger
invasive ventilation
Mechanical ventilator
• Delivers 100% oxygen
• Seen in ER or ICU
• Patient will be intubated (aka:breathing tube placed), which will then be hooked up to mechanical ventilation
ambu bag
Can deliver up to 100% oxygen
• Emergency situations
hold chin up, mask over face
tracheostomy
a tracheal stoma (opening) in the neckmade by a surgical incision.
A small plastic tube is then inserted through this opening.
• Surgical incision is made in trachea to create an artificial airway for gas exchange
• Can be temporary or permanent
tracheostomy indications
• acute airway obstruction
• airway protection
• laryngeal or facial trauma or burns
• airway involvement during head/neck surgery
• for prolonged unconsciousness
-paralysis
-inability to be weaned from mechanical ventilation
nursing considerations tracheostomy
Have an extra tracheostomy kit of the same size and one size smaller
• Make sure there is an obturator taped to wall at head of the bed
• Have inner cannulas and suction catheters in the room
• Check if tracheostomy is midline
-have suction available
suction safety
Preoxygenate w 100% O2 for 30s-3 mins
Insert suction catheter until you meet resistance (do NOT apply suction during insertion)
Apply suction as you withdraw but never for more than 10-15 sec at a time
Can repeat up to 3 passes
tracheostomy complications
Tube obstruction (r/t secretions of cuff displacement), tube dislodgement/decannulation (emergency if occurs within 72h post surgery), pneumothorax, subcutaneous emphysema, bleeding, infection
SABA
Bronchodilators
o Induce rapid bronchodilation through relaxing bronchiolar smooth muscle by binding to beta 2 receptors in lungs
o Administered to improve bronchospasm (wheezing, shortness of breath, chest tightness, or cough) within 5 -15 mins and can control symptoms for up to 6 hrs
examples of SABAs
Xopenex, Albuterol inhaler
LABAs
Bronchodilators
o Given for bronchospasm, but onset slow with long duration (within 15-30mins; helps control symptoms for approx. 12 hrs)
o Primary use is prevention of an asthma attack
LABA exmaples
Salmeterol (Serevent)
what are labas given with
Given with an inhaled corticosteroid to reduce risk of rebound bronchoconstriction
-LABAs should never be prescribed as the only drug therapy for asthma
corticosteroid inhalers
Anti-inflammatory
• Help improve bronchiolar airflow by decreasing the inflammatory response of the mucous membranes in the airways
• Primary use is to prevent asthma attacks caused by inflammation or allergies
use daily even if no symptoms present
• Rinse with water or mouthwash after each use, check mouth daily for lesions/drainage to prevent infection
corticosteroid inhaler examples
Flovent (fluticasone), Pulmicort (budesonide)
oral corticosteroids
Anti-inflammatory agents for moderate-to-severe flare ups of obstructive lung diseases that are poorly responsive to bronchodilators
• May be used long-term for difficult to control chronic obstructive lung diseases
• Take on a scheduled basis, even when no symptoms are present, cant stop before surgery
oral corticosteroids examples
Prednisone, Solumedrol
leukotriene modifiers
Preventing the inflammatory mediator Leukotriene from stimulating inflammation
• Purpose is to prevent asthma attacks triggered by inflammation or allergens
• Take daily
• Max efficacy requires continued use for 48-72 hrs
• Ex: Singulair (montelukast)
COPD
a collection of lower airway disorders that interfere with airflow and gas exchange
•Includes: emphysema & chronic bronchitis
COPD risk factros
-Cigarette smoking, environmental factors, genetics, and asthma
Genetics (AAT deficiency)=Alpha 1 antitrypsin protects lungs/liver
COPD dx
based on FEV1
FEV1= pulmonary function test that measure how much air a person can exhale in 1 second
Other tests: ABGs, sputum samples, CBC (WBC), Hgb/Hct (compensation for hypoxemia), electrolytes (changes r/t acidosis), CXR (hyperinflation and flat diaphragm), nutritional status (total protein, albumin levels)
at what point in pack year history is COPD present
20-pack-year history or longer often have early-stage COPD
how to find pack years
# of packs/day X # of years
complications of COPD
hypoxemia
o acidosis
o respiratory infection
o cardiac failure (cor pulmonale)
o dysrhythmias
o respiratory failure
cardiac failure (cor pulmonale)
R side of heart must work harder to pump blood through narrowed lung blood vessels⇒increased workload⇒systemic backup
cues for COPD
Coughing
• Exertional dyspnea
• Wheezing
• Crackles
• Increased sputum
• SpO2 desat
• Weight loss
• Barrel chest (emphysema)
• Accessory muscle use;
• Prolonged expiration
• Tachypnea w/ activity
• Orthopnea
• Cyanosis
• Delayed cap refill
• Clubbed fingers=late s/s
• Heart dysrhythmias
• Respiratory Acidosis
hypoxemia
priority to notice for COPD
Resp rate
COPD nursing interventions
• Monitor spO2, resp rate/depth, blood gases (resp.acidosis)
• Administer O2 based on blood gases and spO2
• Provide chest physiotherapy (percussion)
• Teach pt about diaphragmatic or abdominal breathing, tripod positioning, pursed-lip breathing techniques
• Activity limitations, alternating rest periods with activity
• Avoid exposure to individuals with infections
• Avoid extremes in temperature, smoke, perfume, other allergens
Trend weight
• Encourage small, frequent meals
• Provide high-calorie, high-protein diet with supplements
• Place pt in a Fowler's position and leaning forward
• Administer bronchodilators, corticosteroids, mucolytics
• Instruct pt on the use of inhaler & oral respiratory meds
• Educate about smoking cessation and immunizations
• Administer antibiotics for infection if prescribed
o2 interventions for COPD
titrate btw 88-92%, usually 2-4 L NC or up to 40% via venturi)
activity with COPD
(2-3x/week)
Walk until symptoms limit walking, rest, then continue until reaching 20 mins of walking (add 5 more minutes of walking as rest time decreases)
diet with COPD
High cal, high protein diet/hydration (at least 2 L/day)
Eat smaller, more frequent meals (4-6) that are easy to chew/non gas forming foods
Avoid caffeine or foods that induce coughing
sx with COPD
bullectomy, lung volume reduction surgery→removal of hyperinflated lung tissue, lung transplant
Chronic bronchitis
airway problem
Inflammation of bronchi/bronchioles due to irritants **esp. smoking!!
Chronic inflammation thickens bronchial walls and increases number/size of mucus secreting glands → obstructs smaller airways and narrows larger ones
Hypoxemia=major concern
Body might compensate by producing more RBCs (polycythemia)
Resp. acidosis may also occur but it is more common in emphysema
Exacerbations cause increased purulent sputum & worsening SOB (often leads to pneumonia)
“Blue bloater” (productive cough, edema, cyanosis, wheezing, dyspnea, clubbing of fingers)
emphysema
alveolar problem
destruction of elastic lung tissue/alveolar walls due to chronic inflammation from irritants (such as cigarette smoke… smoke increases protease release which breaks down elastin in lungs)
air trapping occurs due to loss of elastic recoil in alveoli
Causes overstretching/hyperinflation + collapse of small airways + flattening of diaphragm
Increases effort to breathe (“air hunger” sensation)
CO2 retention (hypercapnia)
Chronic respiratory acidosis→ metabolic alkalosis may develop as compensatory mechanism via kidney retention of HCO3
“Pink puffer” (CO2 retention, pursed lip breathing, barrel chest/hyperinflation of lungs/diaphragm flattened, thin/cachectic, orthopneic, wheezes/crackles, neck vein distention, peripheral edema, mental status changes)
diaphragmatic breathing
lie on back with knees bent, place hands on abdomen, breathe from abdomen while keeping chest still
=stregthens diaphram
tripod positioning
=lean forward and then sit up with arms elevated on a table
=gets more air in the lungs when you are feeling short of breath and may make it feel easier to breathe.
pursed lip breathing
breathe in through nose, purse lips, breathe out slowly without puffing cheeks (exhale twice as long as inhale), use abdominal muscles to squeeze out every bit of air that you can
-in two, out 4 seconds
=keep airways open longer so that you can remove the air that is trapped in your lungs by slowing down your breathing rate and relieving shortness of breath
proper coughing technique
cough when waking up and before meals
Sit upright w feet on floor, turn shoulders inward and place head slightly downward, take 3-5 quick breaths, then a deeper breath → lean forward → 2-3 mini coughs, then a comfortable deep breath (repeat entire procedure at least 2 times)
COPD meds
Beta2 agonists (SABA/LABA... usually LABA)
anticholinergics: aclidinium bromide, ipratropium bromide
Corticosteroids
Mucolytics= Guaifenesin, acetylcysteine
Leukotriene Modifiers (Montelukast)=For inflammation
abx PRN (active infection)
SABA/LABA considerations with COPD
Eg: SABA (albuterol), LABA (salmeterol)
SABAs can cause nervousness/anxiety /tachycardia/palpitations/shaking
corticosteroids with COPD
Eg: Fluticasone combo drugs, prednisone
Risk of thrush, hyperglycemia, Gi ulcers, weight gain, do not stop abruptly
goals of tx with COPD
Improve oxygenation and reduce CO2 retention
Prevent weight loss
Minimize anxiety
Improve activity tolerance
Prevent resp infections w vaccines
lung cancer
-result of repeated exposure to inhaled substances that cause chronic tissue irritation/inflammation interfering with regulation of cell growth in lungs
• Lung tumors can grow and obstruct the bronchus=impairs gas exchange
• Tumors in other areas of lung tissue can compress and obstruct the airway
• Lung cancer can spread to lymph nodes, bone, liver, brain, and adrenal glands
lung cancer cues
Hoarseness
o Wheezing
o Persistent cough
o Blood-streaked, rust-colored or purulent sputum
o Hemoptysis
o Chest pain or chest tightness
o Shoulder, arm, or chest wall pain
o Recurrent pleural effusion, PNA, or bronchitis
o Dyspnea
o Fever
o Weight loss
o Clubbing of the fingers
other dx ways of lung cancer
CXR (find lesion), CT scan (identify lesion/guide biopsy), biopsy, MRI/PET scans locate metastases
definitive dx of lung cancer
biopsy (definitive diagnosis, identify cancerous cells)
lung cancer treatement
chemo
radiation
Lobectomy• removal of a lobe
Pneumonectomy• removal of the entire lung
thoracentesis
photodynamic therapy
chemotherapy for lung cancer side effects
N/V, alopecia, open sores on mucous membranes, immunosuppression with neutropenia, anemia, thrombocytopenia, peripheral neuropathy
thoracentesis
removing fluid from pleural space around lungs
Positioning: sitting up and leaning forward on arms/pillows (kinda like tripod), lying supine with arm of affected side raised above head
Major complication is shock (if fluid is taken off too quickly)
BP drops, tachycardia
Post procedure care: monitor for pneumothorax!! (collapsed lung... happens if needle goes too deep into pleural space)
s/s: decreased LS on affected side, tachycardia, trouble breathing, chest pain