Commensal Bacteria vs Pathogens
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
28 Terms
What is the microbiome
The bacteria on us, in us, and around us, maintaining a balanced microbial community that can shift to a disease state (dysbiosis) if disrupted.
What are virulence factors
Properties / Mechanisms that allow microorganisms to become pathogenic and cause harm to the host.
How can microorganisms be used to treat diseases
Microorganisms, such as probiotics, can treat diseases by maintaining the gut microbiota, helping restore balance and prevent dysbiosis [Diseased state].
This microbiota helps prevent the colonisation of harmful disease causing bacteria
= Using microbiota to treat + maintain microbiota thereby healthy well-being)
Live biotherapeutic product
Diet, prebiotics, postbiotics
Probiotics (e.g. Yakult)
Fecal microbiota transplantation (available now in the NHS and is FDA approved)
BacterioPhage therapy
Engineered bacterial
What is mutualism in symbiotic associations
Mutualism is a symbiotic relationship where both organisms rely on and are dependent on each other for their metabolic needs.
What is commensalism in symbiotic associations
"Commensalism is a symbiotic relationship where the host provides food or shelter, benefiting another organism, which may return the favor without dependency."
What is parasitism in symbiotic associations
Parasitism is a symbiotic relationship where one organism harms the host through its presence and activity
These relationships can dynamically switch to other types.
What is the progression from asymptomatic carriage to disease
Asymptomatic Carriage: (organisms present without symptoms) →
Colonisation: (organisms establish on host) →
Infection: (organisms invade) →
Disease (harmful symptoms manifest).
Why is the skin an inhospitable microbiome for organisms
Skin makes it challenging for microbial growth:
Dry
Sheds hair
Has an acidic pH
Lacks food (only keratinized regions provide nutrients)
How can Staphylococcus epidermidis shift from commensal to parasite
Staphylococcus epidermidis shifts from commensal to parasitic when it enters a surgical wound, changing its anatomical positioning and causing disease."
What is the microbiome of the upper respiratory tract
The upper respiratory tract (nose, oropharynx) has microflora;
Neisseria meningitidis can colonize,
Saliva with lysozymes removes organisms
Virulence factors enable attachment to gingivitis gaps and biofilm formation.
—
Bacteria are commonly found in the gingival grooves.
Saliva washes away the microbiome from exposed surfaces, so bacteria reside in protected gingival grooves.
Saliva contains lysosomes that break glycosidic bonds between NAG (N-acetylglucosamine) and NAM (N-acetylmuramic acid) in the peptidoglycan of bacterial cell walls, making grooves a safer niche.
Poor hygiene allows commensal bacteria in the gingival grooves to become parasitic, leading to infections like gum disease.
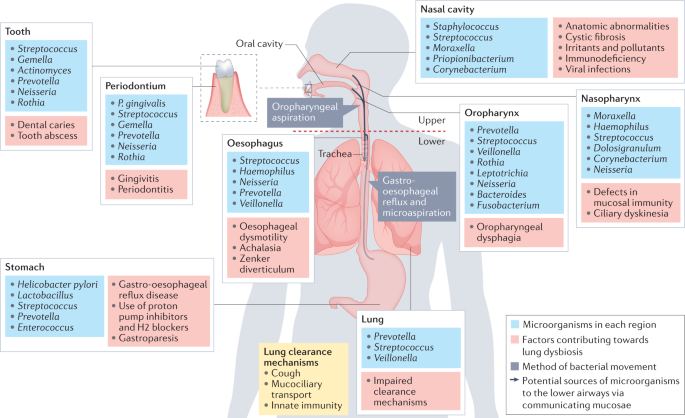
How do phagocytes and mucus protect the lungs in the respiratory microbiome
Phagocytes ENGULFS organisms entering the lungs
Mucus CLEARS them, preventing infection in the lower respiratory tract
How does pH affect the microbiome of the GI tract
The acidic pH of the stomach kills most bacteria
As pH rises along the GI tract, more bacteria grow, with the highest numbers in the large intestine and colon
Microbes can migrate to the appendix causing appendicitis.
What is the role of bacteria in the GU tract microbiome
In the GU [Genitourinary] tract (urethra, rectum, vagina):
Lactobacilli in the vagina feed on glycogen
Produces lactic acid to lower pH, creating a safe environment for childbirth
Prevents uterine infections that could lead to premature birth or miscarriage.
What are Koch's postulates
FOUR criteria to establish a causal relationship between a specific microbe and a specific disease.
1. The organism must be found in all hosts with the disease.
2. It must be isolated in pure culture.
3. It must produce the same disease when reintroduced into a healthy host.
4. It must be re-isolated in pure culture from newly infected individual.
What are the problems with Koch's postulates?
Organisms may only grow in lab conditions (unrealistic)
Genetic diversity
Shifts from virulent (disease-causing) to avirulent (non-disease-causing) state
Ethical issues with deliberately causing disease in humans.
What is the molecular version of Koch's postulates
Koch’s Postulates: Establish a causal relationship between microbe and disease
1. Genes (or products) have pathogenic potential.
2. Genes are in pathogenic strains, NOT avirulent ones.
3. Disrupting the gene reduces virulence.
4. Cloning the gene transforms avirulent strains to virulent.
5. The gene is expressed during infection.
6. The gene product elicits an immune response.
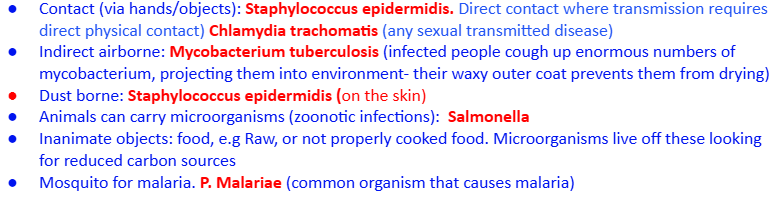
What are the methods of pathogen transmissibility
Direct airborne contact (e.g., coughing) Mycobacterium tuberculosis
Indirect airborne contact (e.g., wind), direct contact (e.g., touching) Staphylococcus epidermidis (on the skin)
Contact via inanimate objects (e.g., handrails, contaminated food) Staphylococcus epidermidis
Sexual contact: Chlamydia trachomatis (any sexual transmitted disease)
Vectors (e.g., mosquitoes causing malaria) Salmonella / Plasmodium malariae
How do pathogens adhere to and colonize the host
Pathogens use pili for transient adhesion to membranes, easily breaking off to evade immune response, and produce mucous slime (Biofilms) to attach and grow on surfaces."
What occurs during colonization of mucosal surfaces
"Enzymes break down epithelial tissues, aiding pathogen colonization on mucosal surfaces."
How do pathogens invade the host
Hiding from immune detection
Rearranging the host cell cytoskeleton
Forcing uptake into the cell
How do pathogens grow and multiply in the host
Iron is vital for DNA synthesis, respiration, and metabolism, but the host’s immune system limits its availability to hinder pathogen growth via Nutritional Immunity.
Pathogens use:
Siderophores (catechols/hydroxamates) to chelate free iron (scarce in natural environments)
Exotoxins (secreted proteins from vegetative cells) to release bound iron by breaking down tissues.
How do pathogens evade the complement pathway
"Pathogens evade the complement pathway leading to opsonisation (marking pathogens for destruction), inflammation, and direct pathogen lysis as part of the immune response, using anti-phagocytic strategies to avoid destruction."
Prevent migration of phagocytes to the site of infection and to limit effectiveness.
Bacteria that degrades C5a- chemoattractant for phagocytes. S. pyogenes.
Some bacteria have developed the ability to survive inside phagocytic cells.
All of these are virulent factors that cause evasion from the host immune response.
What is opsonization in immune evasion
Opsonization tags pathogens for phagocytosis, being engulfed and destroyed.
Pathogens employ anti-phagocytic strategies.
Involves the coating of the pathogen's surface with molecules called opsonins (e.g., antibodies or complement proteins like C3b).
What are nosocomial infections
"Nosocomial infections are hospital-acquired diseases caused by pathogens present in healthcare settings."
Explain the difference between colonization and infection, and provide an example of how one person’s colonization could be another person’s infection.
Colonization refers to the presence of microorganisms in a specific body part without causing disease, while infection occurs when a microorganism causes disease, which may or may not produce symptoms.
For example, Staphylococcus aureus may colonize the nasal passages of one person without causing harm (commensal), but if transmitted to another person with a compromised immune system, it could cause an infection like pneumonia.
True or False: The upper and lower respiratory tracts have a diverse normal microflora similar to the skin.
False
The upper and lower respiratory tracts do not have a normal microflora due to mucus clearance and phagocytic activity.
How do siderophores contribute to bacterial growth and survival in the host?
Siderophores are molecules (e.g., catechols or hydroxamates) produced by bacteria to chelate free iron from the host environment, where iron is scarce due to binding by proteins like hemoglobin. The bacteria take up iron-siderophore complexes, cleave them inside the cell, and release free iron for growth and survival.
Using the molecular version of Koch’s postulates, outline the steps a microbiologist would take to test whether a bacterium’s fimbriae are a virulence factor in causing liver disease in rats.
To test if fimbriae are a virulence factor:
Confirm the fimbriae gene is present in all pathogenic strains causing liver disease in rats but absent in avirulent strains.
Disrupt the fimbriae gene in a pathogenic strain and verify reduced virulence in rats.
Introduce the fimbriae gene into an avirulent strain and check if it becomes virulent, causing liver disease.
Confirm the fimbriae gene is expressed during infection.
Verify that the fimbriae protein elicits a protective immune response in non-immunosuppressed rats.