Pulmonary Physiology: Gas Exchange & Solubility of Gases in Water
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
what does gas exchange encompass?
-transport bwtn the atmosphere & alveolus = breathing
-diffusion across the alveolar/capillary membranes into the blood
Fick's Law
V gas = D x (A/T) x P
-V = vol of gas moving across barrier
-A = area of barrier
-T= barrier thickness
-P = partial pressure gradient for gas across the membrane
-D = diffusion coefficient (mL/min x mmHg)
>directly proportional to solubility of a gas
> inversely proportional to square of its molecular wt
D = k(solubility)/(MW)^1/2
diffusion coefficient (D)
D = k(solubility)/(MW)^1/2
-directly proportional to solubility of a gas
-inversely proportional to square of its molecular wt
henry's law
a gas will dissolve in a liquid in proportion to its partial pressure over the liquid
*actual amount that dissolves = solubility coefficient x partial pressure
How much O2 dissolves in a deciliter of fluid at a partial pressure of 1mmHg?
0.003mLO2/dl/mmHg x PO2
How much CO2 dissolves in a deciliter of fluid at a partial pressure of 1 mmHg?
0.06mL CO2/dl/mmHg x PCO2
Between O2 and CO2 which is more soluble in blood?
CO2 ==> about 20x more soluble than O2 (& diffuses more rapidly even though its MW is higher)
What is the molecular weight of CO2?
28 Da
what is the molecular weight of O2?
16 Da
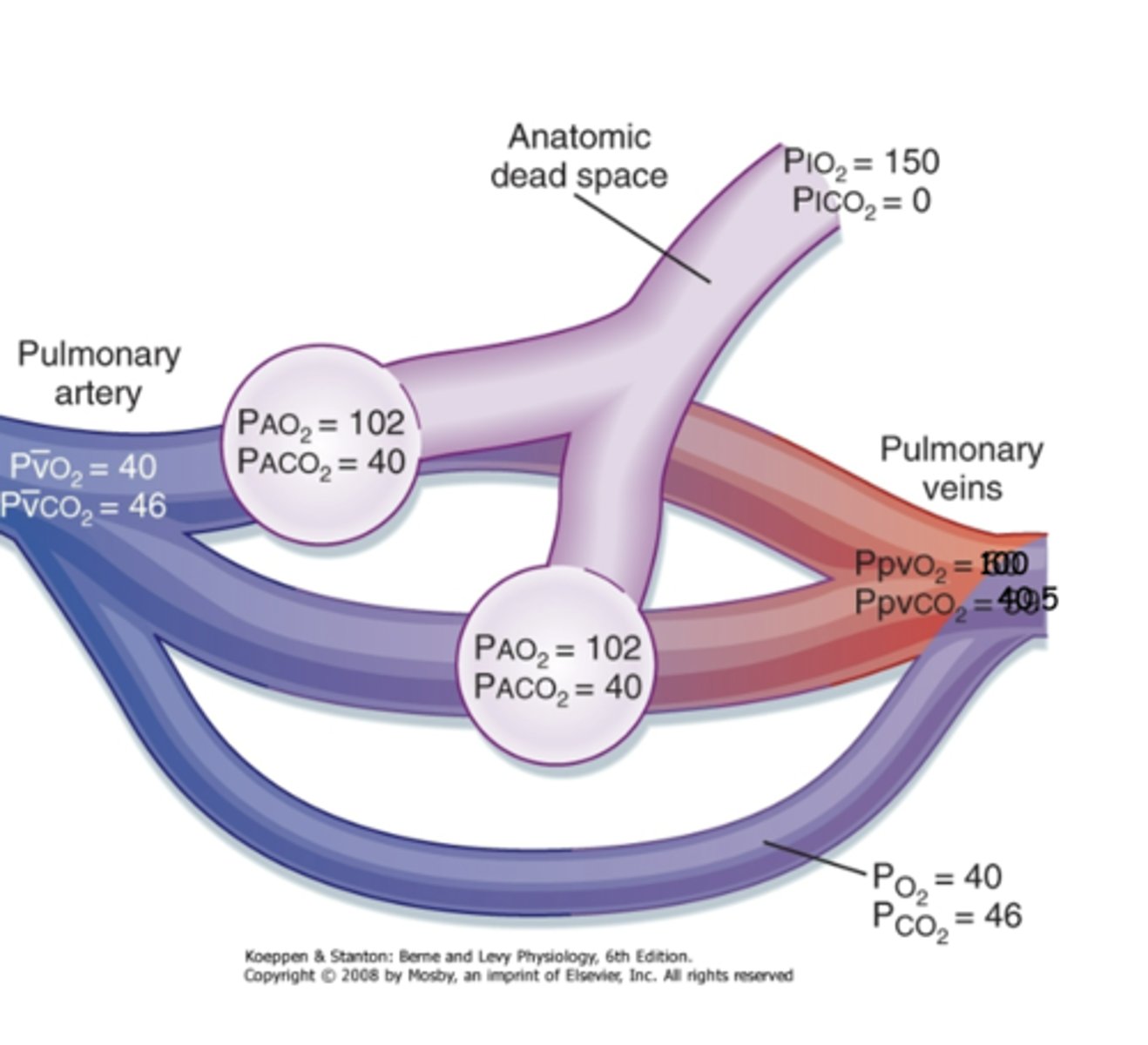
what is the partial pressure gradient of O2 across the alveoli & pulmonary capillaries?
approx 60 mmHg
What is the partial pressure gradient of CO2 across the pulmonary capillaries & alveoli?
approx 6 mmHg
what is the approximate PaO2 in pulmonary veins → L heart → systemic arteries?
100 mmHg
what is the approximate PaCO2 in the pulmonary veins→ L heart → systemic arteries?
40 mmHg
what is the approximate PaO2 in systemic veins → R heart → pulmonary arteries?
40mmHg
what is the approximate PaCO2 systemic veins → R heart → pulmonary arteries?
46 mmHg (then go to lung capillaries to be oxy before going to heart)
PaO2 vs PaCO2 change in tissues
100 to 40mmHg
40 to 46mmHg
what is the approximate PAO2 in alveoli?
105 mmHg
what is the approximate PACO2 in alveoli?
40 mmHg
At the level of the tissues, where does the partial pressure gradient drive oxygen?
into the tissues
why is the PaCO2 in the venous blood approximately 46 mmHg?
CO2 production in the tissues raises the tissue PCO2 to 46 mmHg
*drives CO2 down it's gradient from the cell to the systemic capillaries
what is the capillary transit time for RBCs?
approx 0.75s
How long does equilibration of O2 & CO2 approximately occur?
0.3 s
True or False: Exercise reduced the transit time of RBCs but there's still adequate reserve of time to fully exchange O2 and CO2 gases.
True
When can there not be enough driving force to fully load blood with O2 w/in the RBC transit time?
when low PO2 atm reduces the alveolar - capillary partial pressure gradient (ex: high altitude)
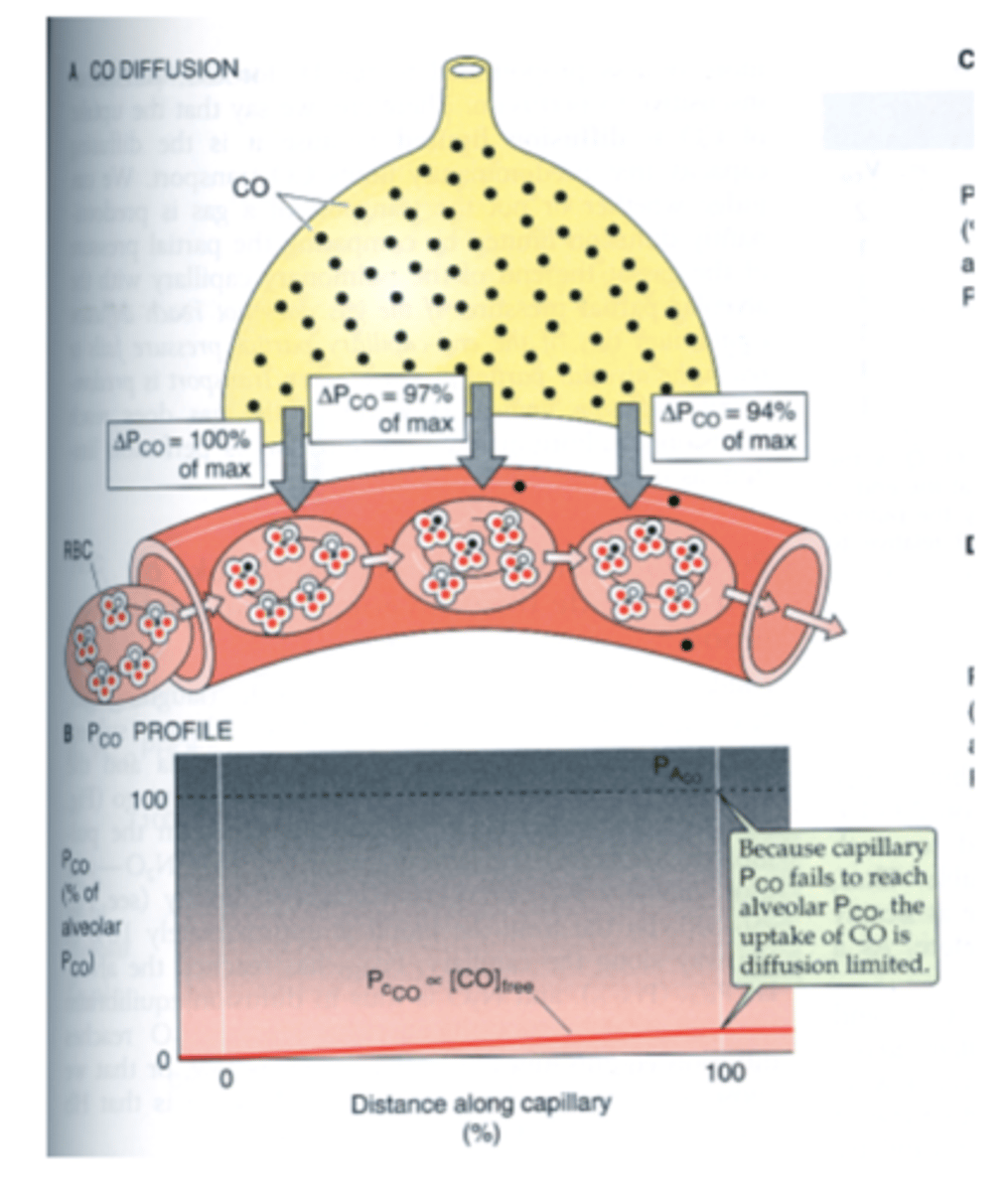
True or False: The uptake of carbon monoxide by the pulmonary capillaries from the alveoli is limited by the amount of blood available
False ==> CO not limited by the amount of blood but is diffusion limited
*CO binds very strongly to hemoglobin = large amount of CO can diffuse into RBCs w/o much increase in PCO--> failure of PaCO to ever reach PACO
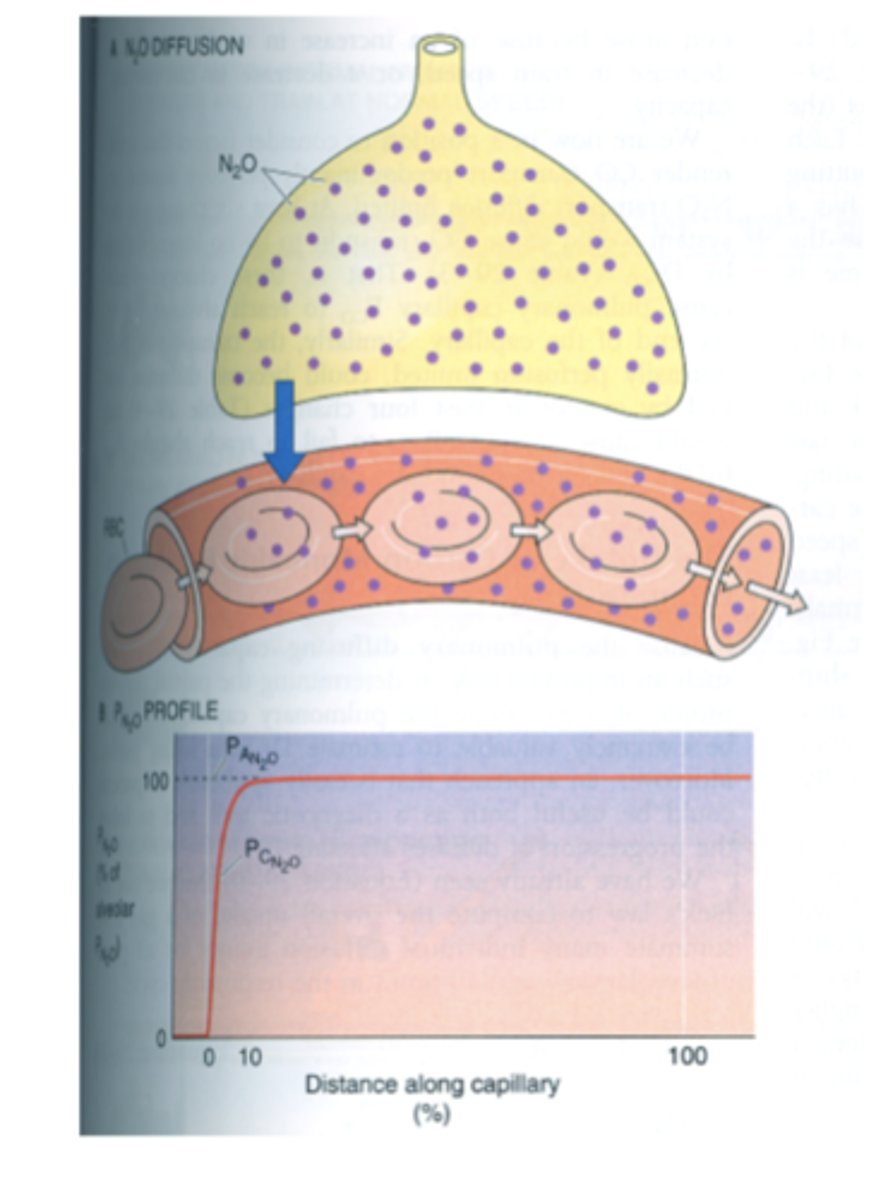
True or False: The uptake of N2O by the pulmonary capillaries from the alveoli is limited by the amount of blood available
True ==> N2O uptake is diffusion limited (perfusion limited)--> equilibrium is reached rapidly
*N2O doesn't combine w/ hemoglobin so amount of N2O taken up is dependent on the blood flow (b/c it'll be dissolved in straight blood) & not on it's diffusion properties
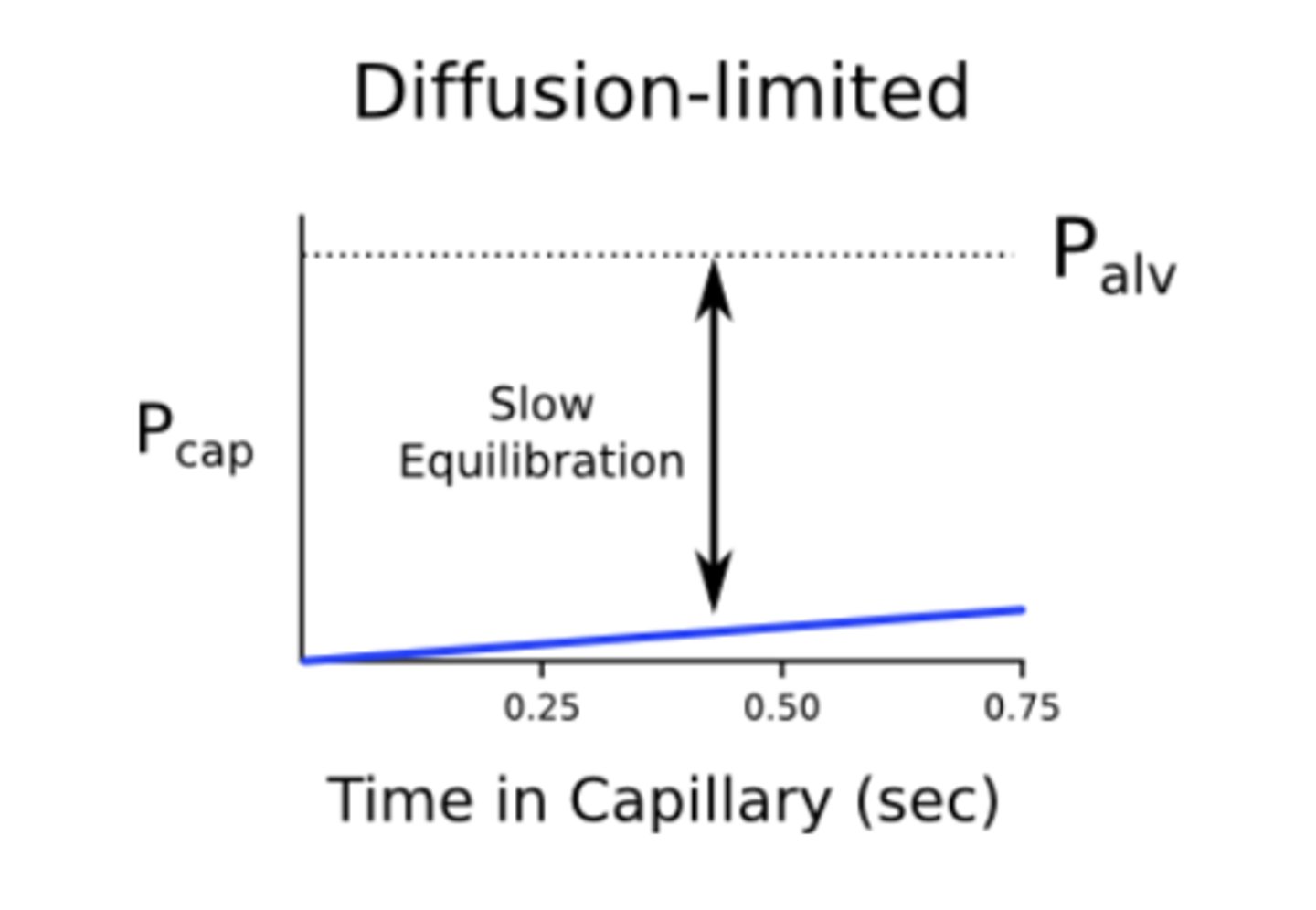
what does it mean if exchange of a certain gas is diffusion limited?
rate of gas uptake in the capillary is determined by the rate of diffusion across the blood-gas barrier ==> equilibrium is not reached
ex: CO
what does it mean if exchange of a certain gas is perfusion limited?
the rate of gas uptake is determined by the capillary blood flow ==> equilibrium is reached rapidly
ex: N2O
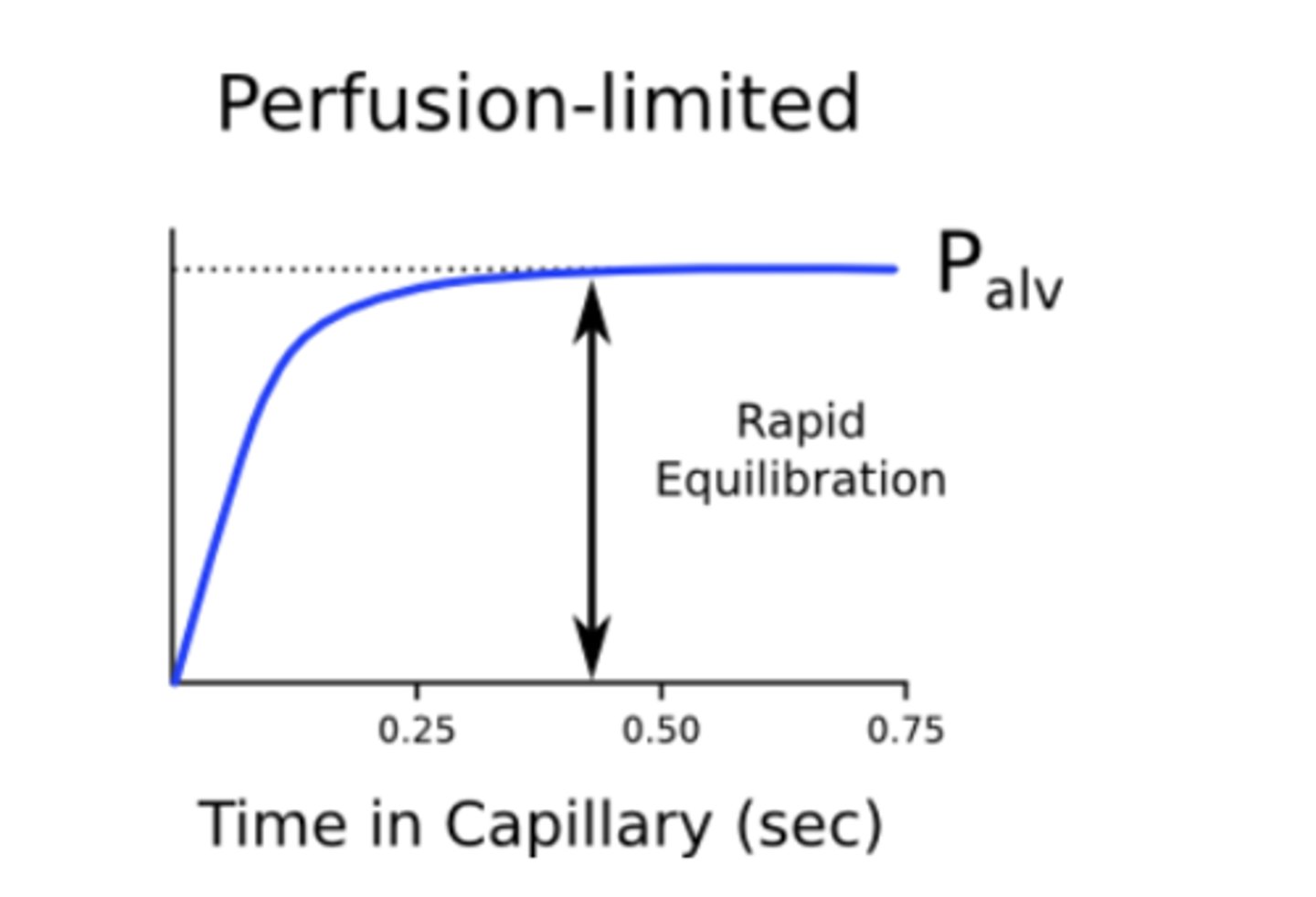
True or False: The exchange of O2 & CO2 are diffusion limited
False ==> perfusion limited in a healthy individual
What is the effect of pulmonary diseases that increase the thickening of the alveolar-capillary walls on the diffusion coefficient (D)?
decreases the diffusion coefficient (D)
*this may cause Po2 at the end of the capillary to be below the PAO2
ex: -COPD
-diffuse fibrosis of pulmonary parenchyma
-loss of functional tissue from tumor or surgery
Which pulmonary diseases increase the thickening of the alveolar-capillary walls which results in a decreased diffusion coefficient (D) ?
-COPD --> destroys pulmonary capillaries
-diffuse fibrosis of pulmonary parenchyma
-loss of functional tissue from tumor or surgery
alveolar gas equation
provides an estimate of alveolar PO2
PAO2 = PIO2 - (PaCO2/0.8)
-PAO2 = O2 in alveoli
-PIO2 = O2 in inspired air
-PaCO2 = CO2 in blood
-0.8 = respiratory exchange ratio (volume of CO2 expired per volume of O2 inspired in a normal diet)
what is the partial pressure of O2 in inspired air?
approx 160 mmHg
respiratory exchange ratio
the volume of CO2 expired per volume of O2 inspired in a normal diet = 0.8
What is the estimated alveolar PO2 using the alveolar gas equation?
PAO2 = 160mmHg - (40mmHg/0.8) = 100mmHg
-PIO2 = 160mmHg
-PaCO2 = 40mmHg
-gas exchange ratio = 0.8
A-aDO2
the difference bwtn PO2 in alveoli & mixed arterial blood
* = 4mmHg in young & healthy
Why is there still a slight difference between the alveolar gas & mixed arterial blood after complete equilibration?
imperfect balance bwtn ventilation & perfusion of the lung ==> small amount of blood gets shunted from arterioles straight to pulmonary vein--> doesn't participate in gas exchange w/ alveoli--> some poorly oxygenated blood gets into pulmonary vein --> dilutes the PO2 of pulmonary vein
*calculated by the A-aDO2 = 4mmHg in young & healthy
Why does A-aDO2 increase with age?
blood shunting away from alveoli & towards pulmonary vein becomes more significant due to natural loss of alveoli & lung compliance with age
What is the A-aDO2 over the age of 30?
A- aDO2 = age x 0.3
what does an abnormally high A-aDO2 indicate?
pathological problem in which gas exchange is compromised
ex: -emphysema
-pneumonia
-asthma
At PaO2 of 100mmHg, how much O2 is dissolved?
0.3 mL/dL
*only 1.5% of total O2 (small amount) b/c the majority of O2 is carried by hemoglobin
describe hemoglobin
-4 polypeptide chains
-each chain has a heme group = porphyrin ring w/ ferrous ion
-each heme binds one O2 = each hemoglobin binds 4 O2
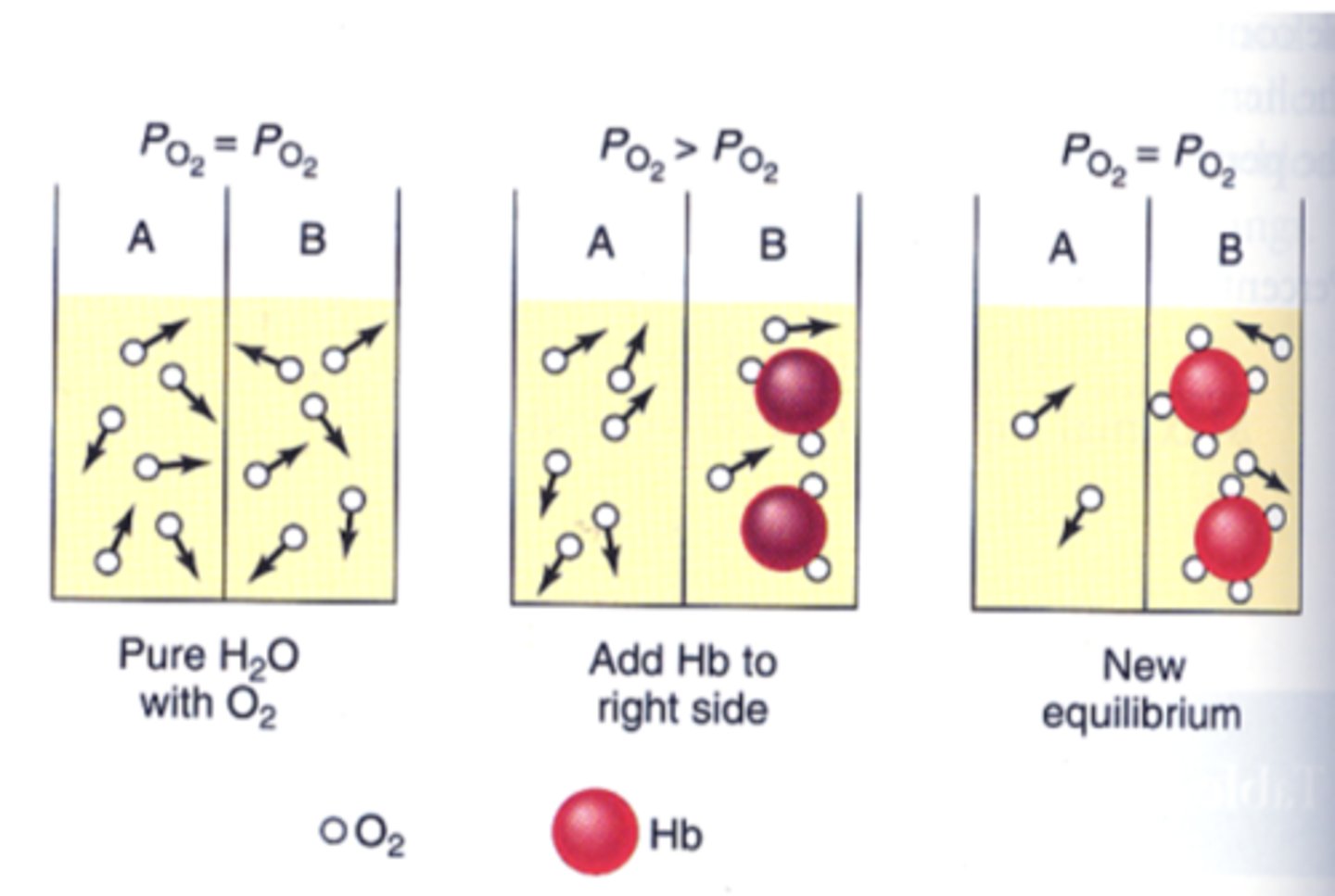
True or False: The O2 bound to hemoglobin does not contribute to the PaO2
True ==> only free oxygen contributes to PaO2
*when O2 is bound to hemoglobin it is not dissolved so it doesn't contribute to PaO2 --> reason oxygen content of side B is greater than side A although the PO2 is the same on both sides of the diagram
How much O2 is released by hemoglobin into tissues under normal resting conditions?
only 1 of the 4 O2 molecules are released
*Hb is 75% saturated in venous blood returning to the lungs, so it picks up a single O2 molecule at the alveoli
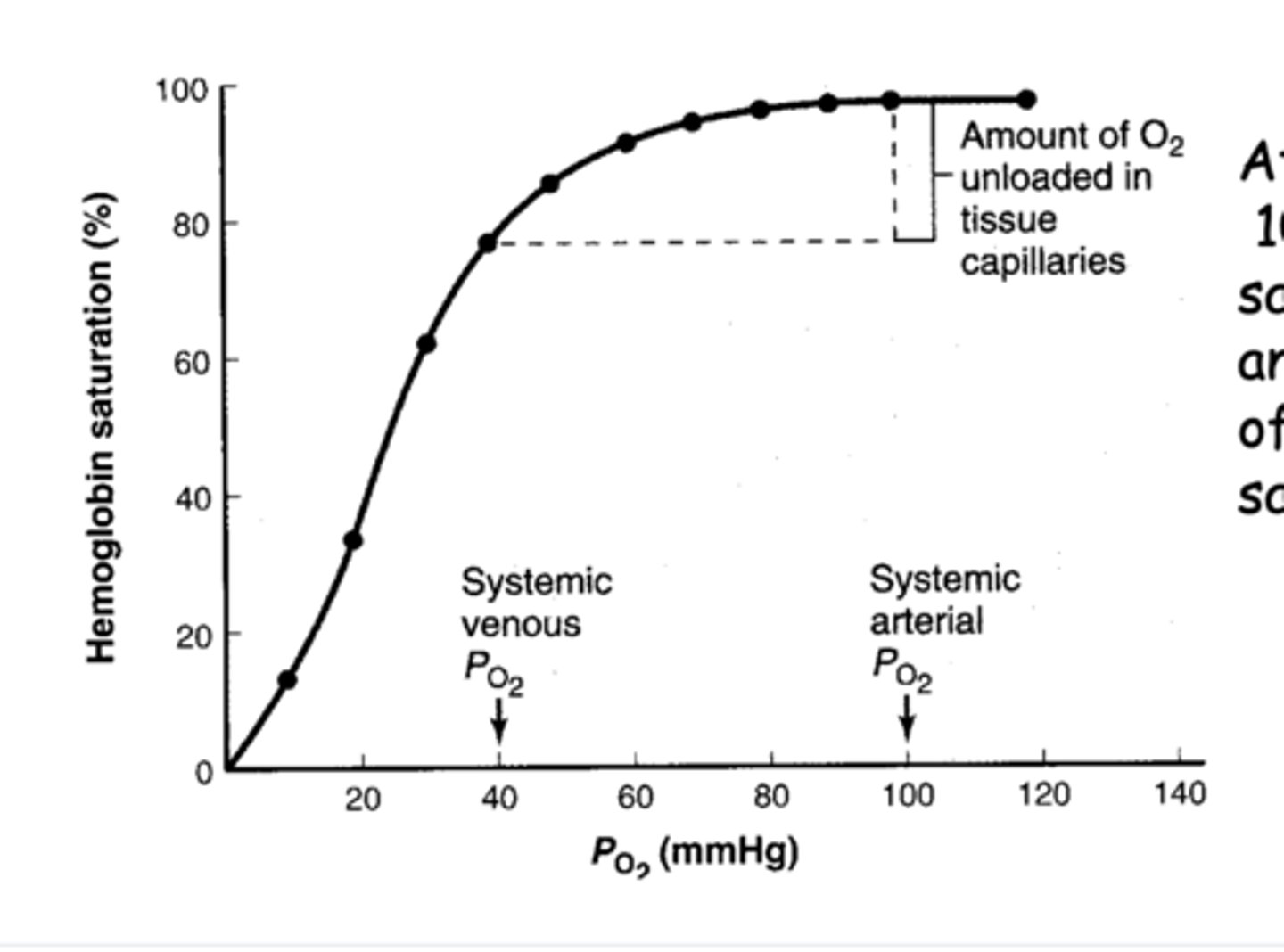
If only 1 O2 molecule is released from hemoglobin into tissues, what do the other 3 bound O2 molecules serve as?
they represent a reserve capacity '
how much O2 is dissolved in venous blood at 40mmHg?
0.003mLO2/dL/mmHg x 40 mmHg = 0.12 mLO2/DL
How much hemoglobin is in each dl of blood?
15g
1g of hemoglobin binds _________mL of O2 at 100% saturation
1.34
How much O2 is bound to hemoglobin in venous bloods?
1.34ml/g x 15g/dl x 0.975 = 19.6 mlO2/dl ==> 0.75 (19.6) = 15.08 ml
-1 g of hemoglobin binds 1.34ml of O2
-15g of hemoglobin in every dl of blood
-97.5% saturation
-only 75% of hemoglobin saturated w/ O2 (only 3 O2 bound in venous blood)
what is the total oxygen in venous blood?
dissolved O2 + hemoglobin bound O2
0.12ml/dl + 15.08ml/dl = 15.2mlO2/dl blood
-0.12ml/dl = dissolved O2 in venous blood
-15.08 ml/dl = hemoglobin bound O2 in venous blood
What is the amount of O2 delivered to resting tissue per deciliter of blood?
19.9ml/dl - 15.2ml/dl = 4.7 mlO2/dl of perfusion
-19.9 ml/dl = total O2 in arterial blood
-15.2ml/dl = total O2 in venous blood
At PaO2 of 100mmHg, what percent of O2 is dissolved in blood?
1.5 %
*other 98.5% is bound to hemoglobin
why is the O2 dissolved in blood critical?
-maintains the PO2 necessary to keep the hemoglobin saturated
-only free O2 can diffuse across cell membranes into tissues
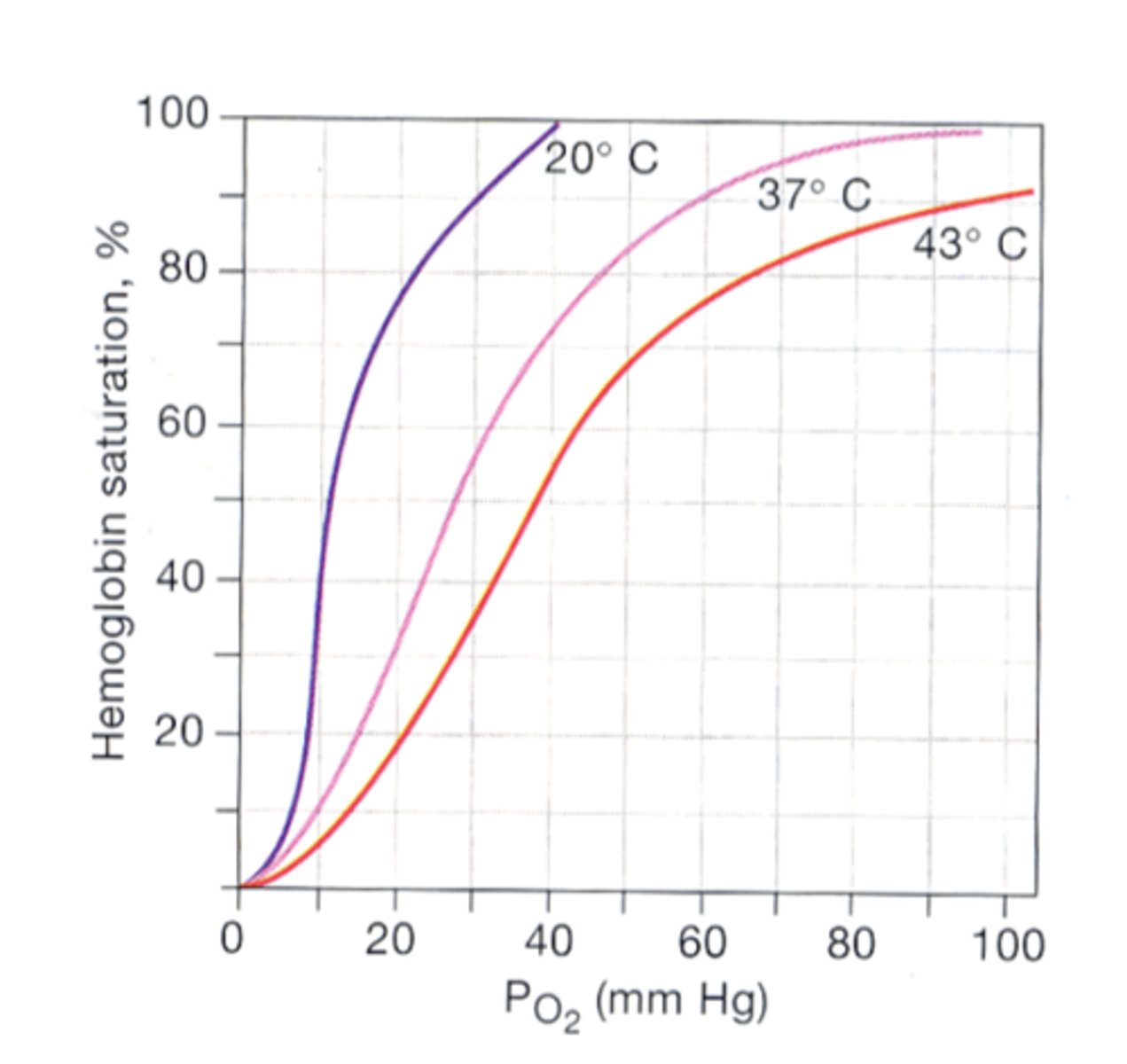
What is the effect of temperature on hemoglobin binding to O2?
-high Temp --> decreases binding affinity (curve shifts to the right)
>ex: high temp in active muscles or w/ fever *
-low temp --> increases binding affinity (curve shifts to the left)
>may be due to small shifts in amino acid side chain pK values that cause a conformational change in Hb*
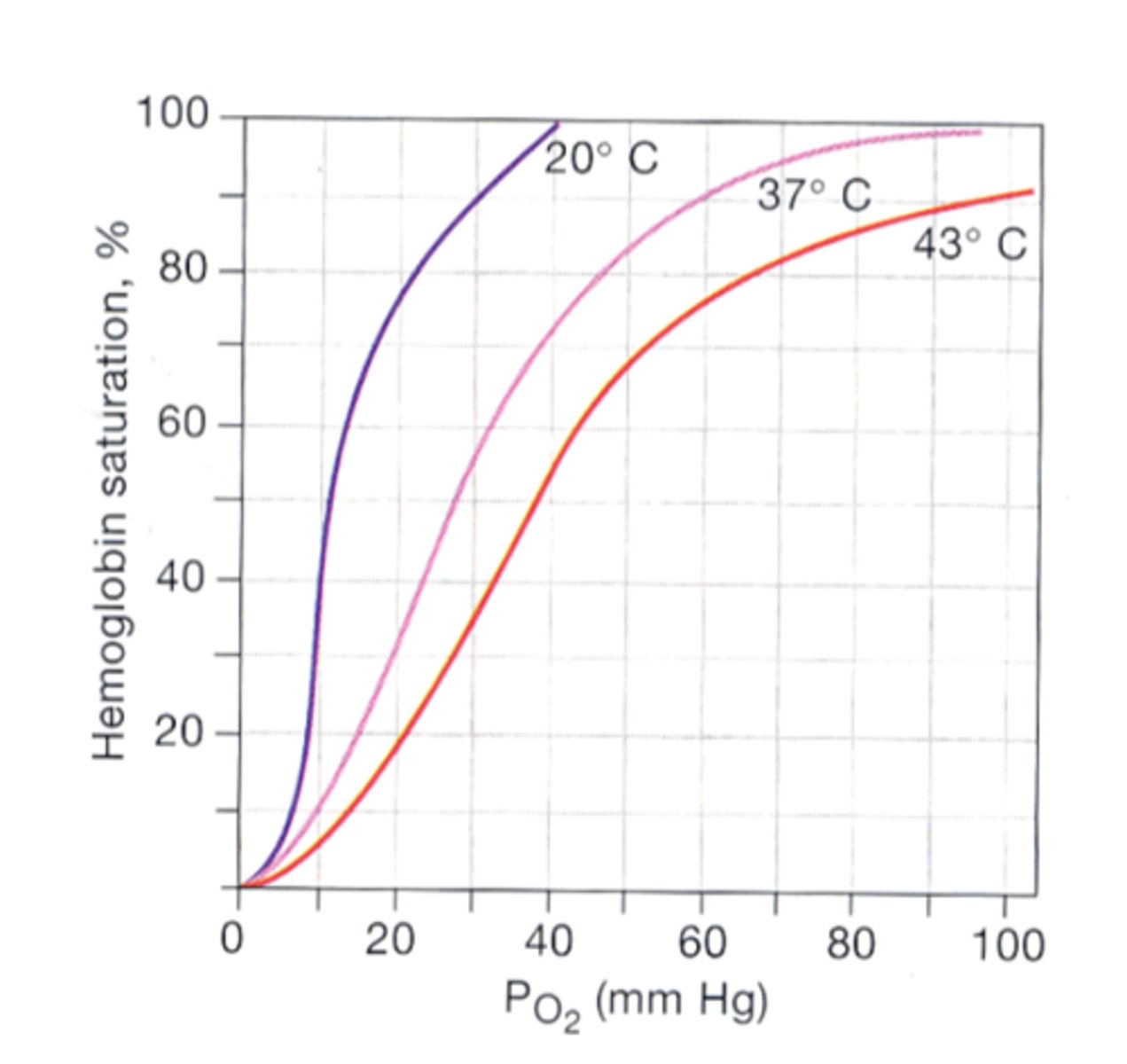
True or False: Fever decreases the binding affinity of hemoglobin for O2
True ==> high temp decreases binding affinity
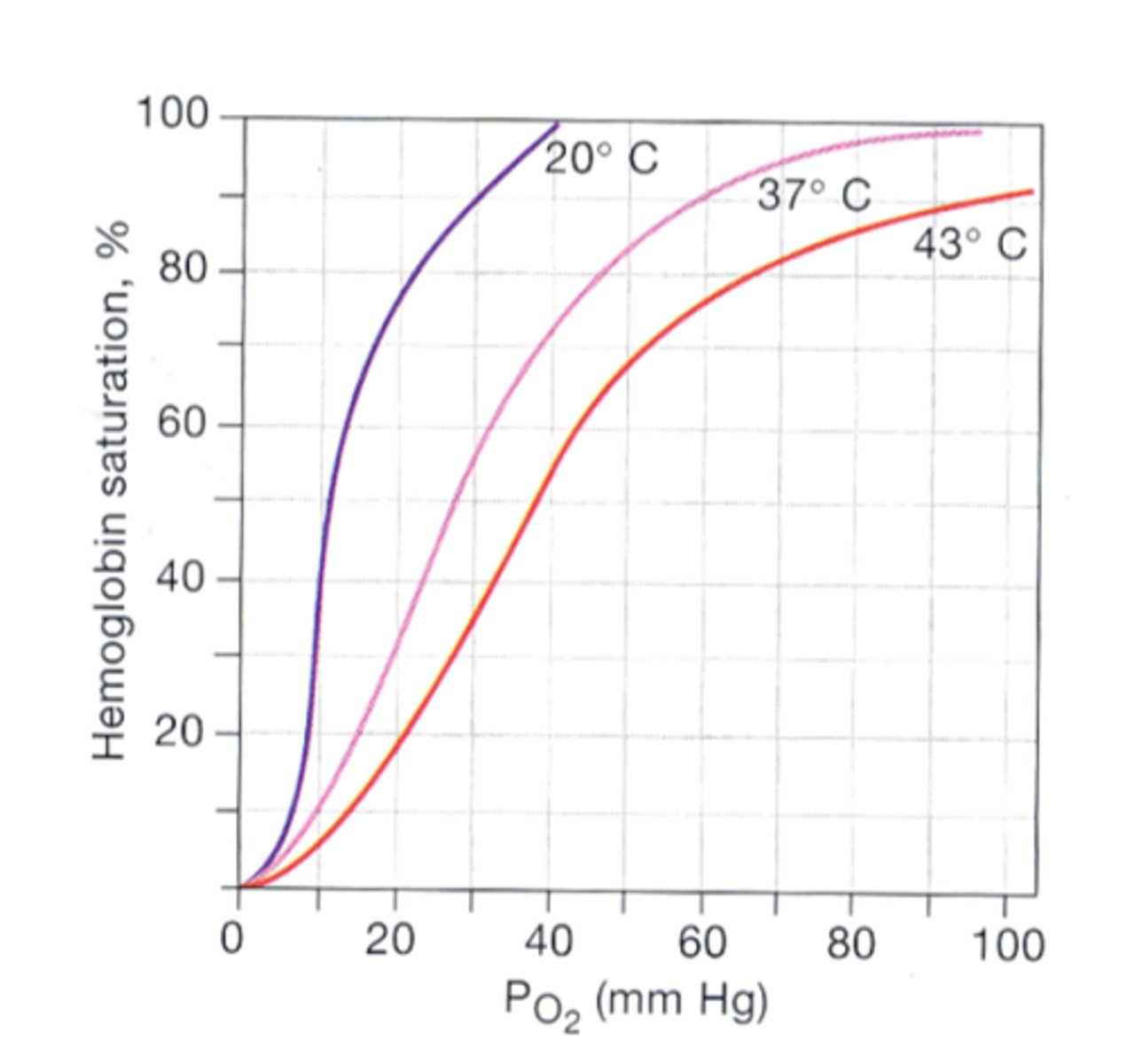
Why does low temperature increase the binding affinity of hemoglobin for O2?
may be due to small shifts in amino acid side chain pK values that cause a conformational change in Hb
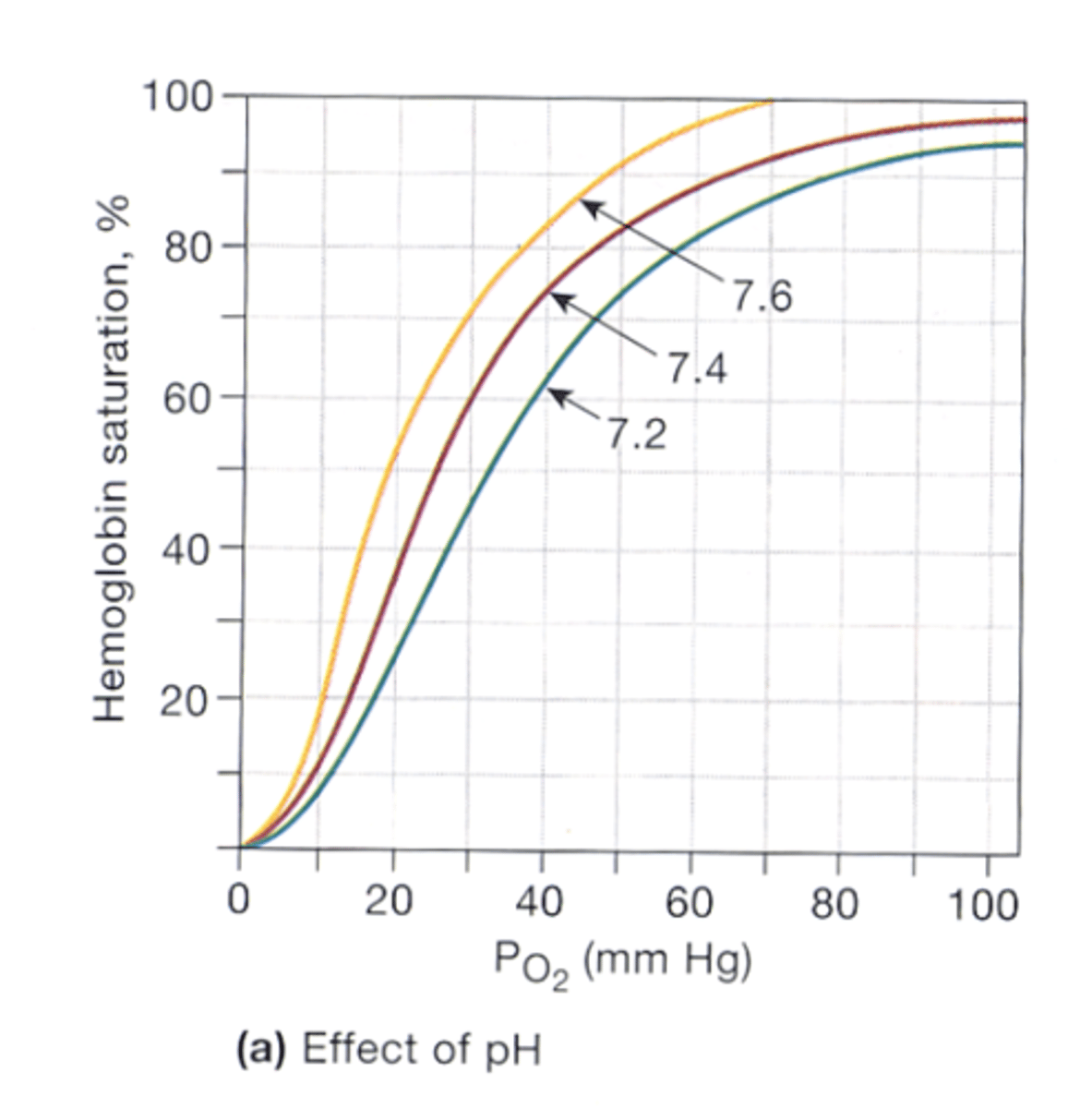
Bohr effect
respiratory acidosis (low pH) decreases the binding affinity of hemoglobin for O2 (shifts curve to the right)
*increased metabolism in active muscles generates acid = increased CO2 + lactic acid --> enter RBCS --> effect titratable groups on hemoglobin --> decreases O2 affinity
*the pH-induced changes in Hb are independent of PCO2
How does PCO2 affect binding affinity of hemoglobin for O2?
-increased PCO2 --> decrease Hb affinity for O2 (shifts curve right)
-decreased PCO2 --> increases Hb affinity for O2 (shifts curve left)
*these changes happen independently of pH changes
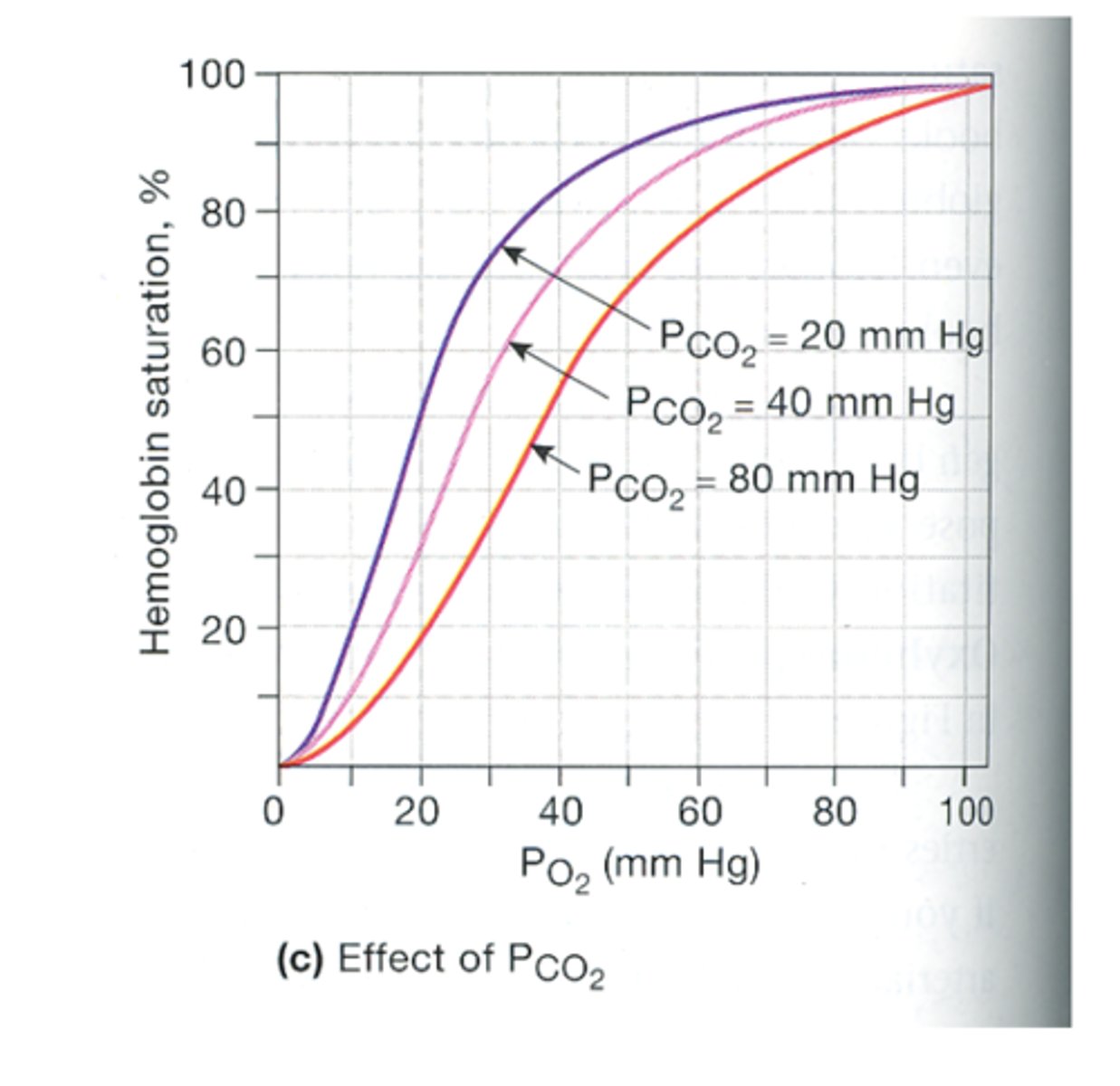
why does hemoglobin have an affinity for CO2?
CO2 binds free amino groups (N-terminal amino group) of 4 Hb chains --> generates carbamino groups
CO2 + Hb -NH2 = Hb-NH-COO-
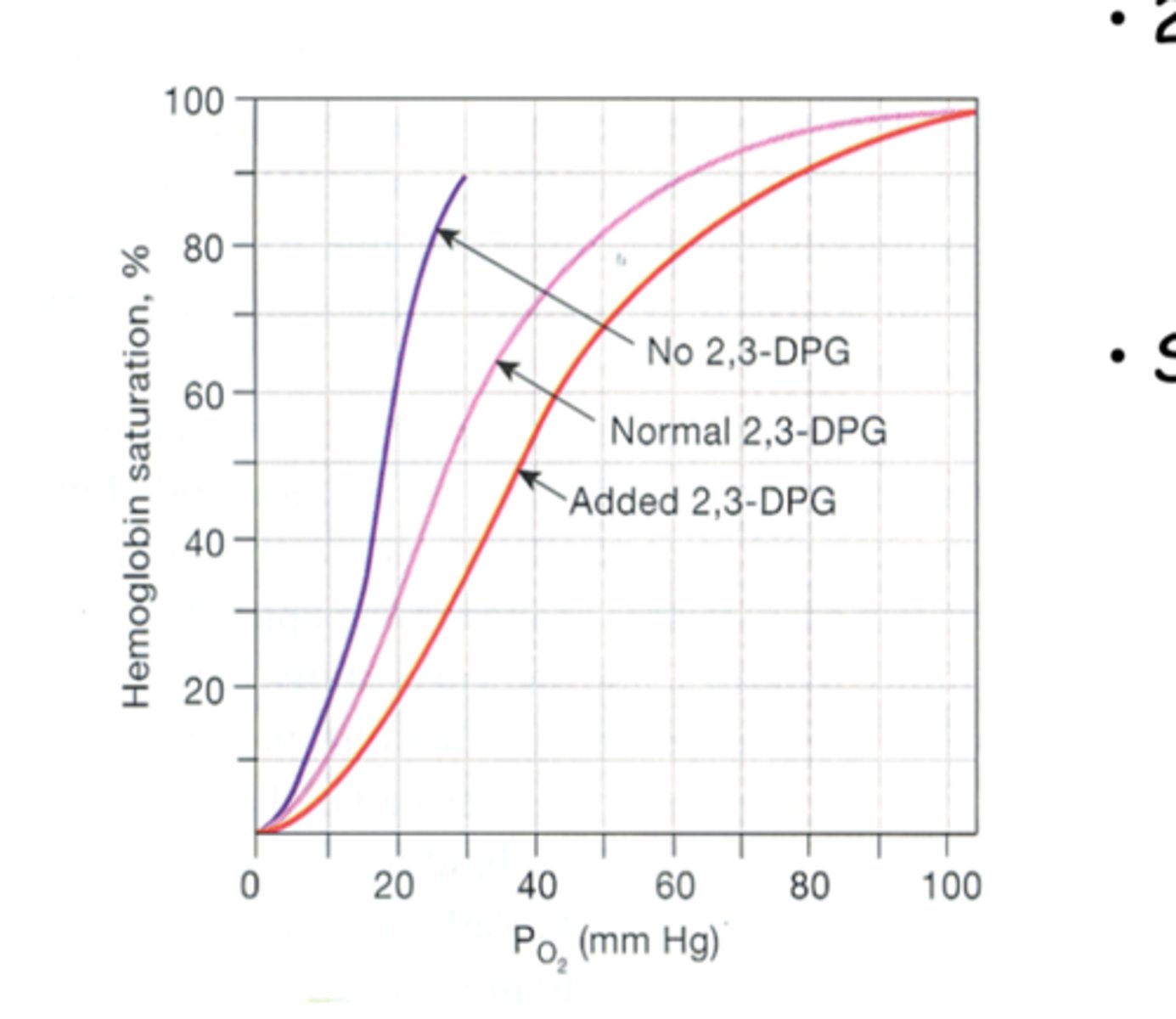
how does 2,3-diphoshoglycerate (2,3-DPG) affect the binding affinity of hemoglobin for O2?
-increased 2,3-DPG --> decreased affinity (shifts curve to the right)
-decreased/absent 2,3-DPG --> increased affinity (shifts curve to the left)
*stimulation of glycolysis in exercise increases 2,3-DPG to levels that decreased Hb affinity for O2
True or False: Fetal hemoglobin (HbF) has a higher affinity for O2 than adult hemoglobin (HbA)
True
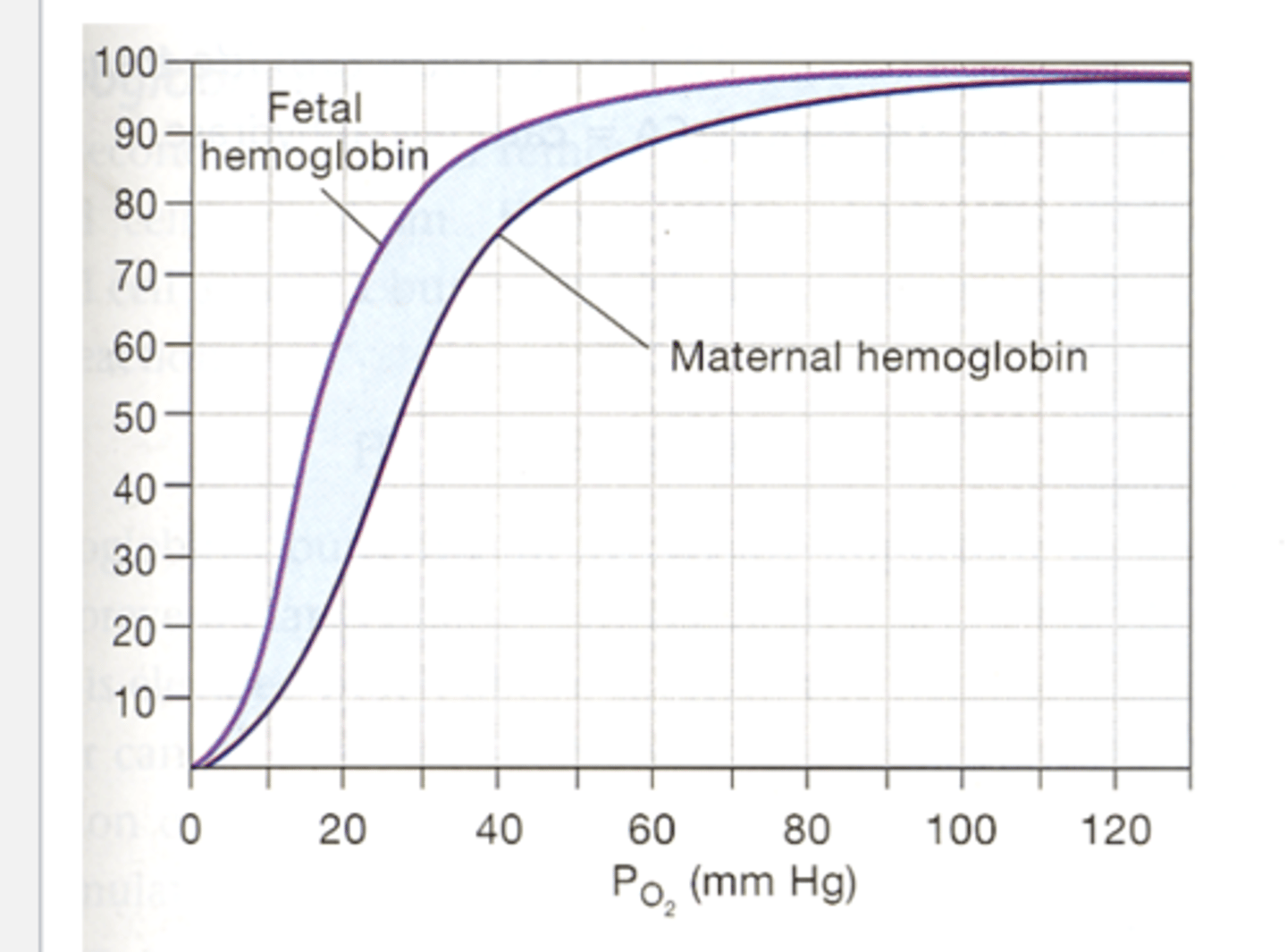
Why does fetal hemoglobin (HbF) have a higher affinity for O2 than adult hemoglobin (HbA)?
to facilitate the extraction of O2 by the fetus of maternal blood at the placenta
True or False: A newborn's blood has about equal amounts of HbF and HbA
True
*HbF falls to only 1-2% by the end of the 1st year
methemoglobin (Met-Hb)
hemoglobin who's ferrous ion (Fe2+) that got oxidized to ferric ion (Fe3+) ==> can't bind O2
-created by various drugs & chemicals oxides (ex: nitrites, sulfonamides)
-Met-Hb reductase = enzyme that converts Met-Hb back to ferrous ion
Met-Hb reductase
enzyme that converts Met-Hb back to ferrous ion